Abstract
Purpose
Many techniques are available for closed reduction and percutaneous fixation of proximal humeral fractures. The palm tree technique was described by Kapandji in 1989. In that technique three curved wires are inserted through one hole at the V-shaped insertion of the deltoid muscle. It is a good technique but it has some disadvantages. In this study we introduced some modifications for the technique, and we evaluated the clinical results of the modified technique in treatment of 18 cases.
Methods
Eighteen patients with displaced proximal humeral fractures were treated by closed reduction and percutaneous fixation with the palm tree technique after minor modifications. The age of the patients ranged from 38 to 75 years with an average of 56 years. Eleven were females and seven were males. The fractures were two-part in 13 cases and three-part fractures in five cases.
Results
The average time of healing was seven weeks. The follow-up period ranged from 14 months to 39 months with an average of 22 months. The Constant score ranged from 45 to 88 with a mean of 73. The results were satisfactory in 77% and unsatisfactory in 23% of the cases. The complications included pin tract infection in two cases, intraarticular wire migration in one case, skin necrosis around the wires in three cases and malunion with varus deformity in one case. No cases were complicated by neurovascular injury, loss of fixation or avascular necrosis of the humeral head.
Conclusions
The palm tree technique is a good method for fixation of proximal humeral fractures. It produces good grip in both of the proximal and distal fragments and allows for early joint movements. Our modifications allow for easy insertion of the wires, increase the stability of fixation and minimize the risk of complications.
Introduction
Proximal humeral fractures account for 4–5% of all fractures [12]. It is the second most common fracture of the upper extremity, following distal forearm fractures [1]. About 80% of these fractures are undisplaced according to Neer's [16] criteria and can be managed nonoperatively. Only 20% are displaced and require operative interference. Several surgical techniques have been described for the management of such fractures. Open reduction and internal fixation has the advantages of anatomical reduction and stable fixation but it carries the risk of joint stiffness, implant failure and avascular necrosis of the humeral head [5]. Closed reduction and percutaneous fixation with straight wires has the advantage of a less invasive technique but it carries the risk of insecure fixation, loss of reduction and wire migration [4, 7]. The palm tree technique was described by Kapandji [9] in 1989. In his technique Kapandji inserts three curved wires through one hole at the V-shaped insertion of the deltoid muscle. The wires are made divergent and then driven into the suchondral bone of the proximal fragment to maximize the stability. It is a good technique but it has some problems. To reach the V-shaped insertion of the deltoid muscle a formal skin incision must be done (4 cm according to Kapandji). Insertion of the wires at the level of the deltoid tuberosity carries the risk of radial nerve injury especially if the drill bit slipped posteriorly. Kapandji [9] reported on two cases complicated by radial nerve injury due to improper insertion of the wires. Le Bellec et al. [11] also had two cases complicated by radial nerve injury in their series that were treated by the same technique. Insertion of the wires through one hole in the distal fragment does not eliminate rotation at the fracture site and acts as a stress riser that may predispose to fracture at the entry point. Le Bellec et al. [11] had one case of fracture at the site of wire insertion. Another problem with this technique is that if one wire migrated distally the other wires would be loose and eventually will migrate.
In this study we introduced some modifications for the technique to avoid these problems and we evaluated the clinical results of the modified technique in treatment of 18 cases. The modifications involve insertion of each wire through a separate hole in the distal fragment, the entry points for the wires are shifted proximal to the deltoid tuberosity to be safer and a small bend is made at the tips of the wires to facilitate their insertion.
Patients and methods
Between April 2006 and June 2009, 18 patients with displaced proximal humeral fractures were treated in our institution by closed reduction and percutaneous fixation with the modified palm tree technique. The age of the patients ranged from 38 to 75 with an average of 56 years. Eleven were females and seven were males. The right side was affected in eight cases and the left in ten cases. The mechanism of injury was a fall on outstretched hand in 12 cases and a direct trauma to the shoulder in six cases. Thirteen cases had two-part fractures and five had three-part fractures according to Neer [16] classification. Under general anaesthesia, a trial of closed reduction was attempted under C-arm control and then fixation was done according to the Kapandji [9] technique with some modifications described herein.
Preparation of the K-wires
Three K-wires of 2-mm thickness are usually used for fixation of the reduced fracture. The sharp tapering end of the wire is cut and the first 5 mm of the wire is bent by about 45 degrees followed by a smooth gentle curve over the next 10 cm of the wire (Fig. 1a).
Fig. 1.
a The sharp end of the wire is cut and the first 5 mm of the wire is bent by about 45 degrees followed by a smooth gentle curve over the next 10 cm of the wire. b Two drill holes are made in the lateral and anterolateral cortices of the distal fragment using a 2.5-mm drill bit directed obliquely from distal to proximal. c Two wires are inserted in the predrilled holes and advanced till the fracture site. d Reduction is adjusted and the wires are advanced into the subchondral bone of the proximal fragment. e A third wire is added to increase the stability of fixation
Predrilling of the distal fragment
Two snip incisions are made in the skin over the lateral and anterolateral aspects of the arm then blunt dissection is carried down to the bone. With the 2.5-mm drill bit two drill holes are made in the distal fragment through the previous incisions. The drill bit is directed obliquely from distal to proximal and only the near cortex is opened. The holes are made in the lateral and the anterolateral cortices in the area lying proximal to the deltoid tuberosity and about 3–5 cm distal to the fracture line. The drill holes are made at different levels to avoid stress risers (Fig. 1b).
Insertion of the wires
The prepared wires are inserted into the predrilled holes in the distal fragment and advanced by gentle hammering up to the fracture line. The wires are rotated gently to make their tips point in different directions (Fig. 1c). Reduction is done again and the wires are engaged into the proximal fragment and advanced into the subchondral bone by gentle hammering (Fig. 1d). For additional stability a third wire is added through a separate hole in the distal fragment (Fig. 1e). In the five cases with three part fractures the greater tuberosity was fixed by a separate straight wire inserted directly from the greater tuberosity towards the medial cortex of the distal fragment.
The stability of fixation is then checked under C-arm by rotating the humeral head in different directions. The wires are then bent and cut short outside the skin. Dressing around the wires is done in the usual way. The arm is supported in an arm sling. In the second postoperative day the patient is instructed to actively move the shoulder as pain tolerates. Pendulous exercise is encouraged from the second postoperative week. After healing of the fracture the wires are extracted in the outpatient clinic without anaesthesia.
Results
The period of hospital stay ranged from two to seven days with an average of three days. The time of healing ranged from five weeks to eleven weeks with an average of seven weeks. The follow-up period ranged from 14 months to 39 months with an average of 22 months. All the fractures healed within the expected time (Fig. 2). The Constant [2] score of the patients ranged from 45 to 88 with a mean of 73. According to this scoring system, the results were excellent in five cases (27%), good in nine cases (50%), fair in three cases (17%) and poor in one case (6%). Out of the 13 patients with two-part fractures, 11 had satisfactory results and two had unsatisfactrory results. Of the five patients with three-part fractures three had satisfactory and two had unsatisfactory results. All the patients with unsatisfactory results were above 65 years old. The range of shoulder movements was satisfactory in most of the cases (Table 1). The complications included pin tract infection in two cases (treated by local care and short course of systemic antibiotics), wire migration inside the shoulder joint in one case (treated by wire extraction), area of skin necrosis around the wires in three cases (treated by skin release and excision of the necrotic areas of the skin) and malunion with 20 degrees of varus deformity in one case. No cases were complicated by loss of fixation, deep infection, or avascular necrosis of the head humerus.
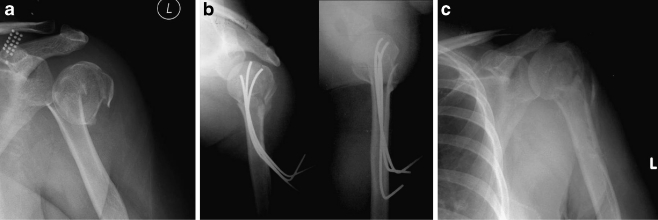
Fig. 2.
a A 53-year-old female patient with displaced proximal humeral fracture. b Closed reduction and fixation with the modified palm tree technique. c After healing of the fracture and removal of the wires
Table 1.
Range of shoulder movements at the final follow-up
| Patient number | Age (years) | Gender | Type of fracture | Range of shoulder movements at final follow-up | |||
|---|---|---|---|---|---|---|---|
| FF | AB | ER | IR (dorsum hand to) | ||||
| 1 | 52 | M | Two-part fracture | 150 | 130 | H above head, elbow forward | Waist (L3) |
| 2 | 39 | F | Two-part fracture | 170 | 160 | Full elevation of arm | T12 |
| 3 | 67 | F | Two-part fracture | 110 | 100 | H behind head, elbow back | SI joint |
| 4 | 44 | M | Two-part fracture | 180 | 180 | Full elevation of arm | Interscapular (T7) |
| 5 | 72 | F | Three-part fracture | 100 | 80 | H behind head, elbow forward | SI joint |
| 6 | 40 | F | Two-part fracture | 160 | 150 | H above head, elbow back | T12 |
| 7 | 42 | F | Two-part fracture | 180 | 170 | Full elevation of arm | Interscapular (T7) |
| 8 | 56 | F | Two-part fracture | 140 | 120 | H behind head, elbow back | Waist (L3) |
| 9 | 67 | M | Three-part fracture | 90 | 80 | H behind head, elbow forward | Buttock |
| 10 | 60 | F | Two-part fracture | 170 | 140 | H above head, elbow forward | T12 |
| 11 | 38 | M | Two-part fracture | 170 | 180 | Full elevation of arm | Interscapular (T7) |
| 12 | 69 | F | Three-part fracture | 130 | 140 | H above head, elbow forward | Waist (L3) |
| 13 | 53 | F | Two-part fracture | 170 | 170 | H above head, elbow back | Interscapular (T7) |
| 14 | 75 | M | Two-part fracture | 100 | 90 | H behind head, elbow forward | SI joint |
| 15 | 58 | M | Three-part fracture | 170 | 150 | H above head, elbow back | T12 |
| 16 | 66 | F | Two-part fracture | 150 | 130 | H above head, elbow forward | Waist (L3) |
| 17 | 59 | M | Three-part fracture | 160 | 140 | H above head, elbow back | T12 |
| 18 | 54 | F | Two-part fracture | 170 | 160 | Full elevation of arm | Interscapular (T7) |
M male, F female, FF forward flexion, AB abduction, ER external rotation, IR internal rotation, H hand, T12 thoracic 12 vertebra, T7 thoracic 7 vertebra, L3 lumbar 3 vertebra, SI sacroiliac
Discussion
Closed reduction and percutaneous pinning of proximal humeral fractures has the advantage of being both a less invasive and a simple procedure, but it carries the risk of certain disadvantages which include loss of reduction, wire migration and the possibility of neurovascular injury [4, 7]. With straight wires it is sometimes difficult to engage both of the proximal and distal fragments with the same wire. In his mechanical study, Vogel et al. [19] found that the straight wires tend to accumulate in the medial part of the proximal fragment which indicates poor rotational stability.
The palm tree technique avoids the disadvantages of the straight wires and allows for better distribution of the wires in the proximal fragment. Unlike straight wires the curved wires are less likely to migrate. The smooth curve in the proximal part of the wires produces the three-point fixation; one at the entry point, one at the summit of the curve and one at the tip of the wire. This is a well-known principle in management of fractures and it produces sufficient stability to allow for early joint movements [10, 13]. Several biomechanical studies had been done to compare different wire configurations in fixation of proximal humeral fractures. They found that a parallel configuration is better than a convergent configuration in both rotational and bending stresses and that a divergent configuration is better than a parallel configuration in rotational stresses [8, 14, 19]. The palm tree technique allows for insertion of the wires in a divergent manner that insures stable fixation. The Hackethal technique was described in fixation of the humeral shaft and proximal humeral fractures. It is done by multiple elastic nails inserted through a window in the distal humerus. Heterotropic ossification at the site of wire insertion and loss of elbow extension are common complications of the technique. Wire migration is another problem and some authors advise packing of the medulla with a large number of nails to avoid this complication [3, 6, 17]. The palm tree technique avoids the elbow complications associated with the Hackethal technique by shifting the wire insertion more proximally.
Although it overcomes the complications of both the straight wires and Hackethal techniques the palm tree technique still has some disadvantages which include the formal skin incision, the risk of radial nerve injury and the risk of fracture at the site of wire insertion. Our modifications further improve the stability of fixation with this technique and reduce the risk of its complications. Insertion of each wire through a separate hole avoids the stress riser created by a single big hole and minimizes rotation at the fracture site as the wires are distributed in both of the proximal and distal fragments and not accumulated at one point in any of them. The small bend at the tip of the wire allows for easy identification of the hole in the distal fragment and prevents impingement of the tip of the wire on the far cortex. The entry points in our study are usually distal to the surgical neck and proximal to the deltoid tuberosity. This area is considered to be safe for insertion of the lateral wires according to Rowles and McGrory [18] who did an atomic study to detect the risk of injury to neurovascular structures from percutaneous pinning of the proximal part of the humerus. In our study the distal parts of the wires are bent and cut outside the skin. This helps for easy removal of the wires after fracture healing without anaesthesia. The skin must be released around the wires to avoid any pressure over the skin. We had seven complications in our study, six of them improved during the course of treatment and they did not affect the final outcome. No cases were complicated by neurovascular injury, distal wire migration or fracture at the entry points. Most of the cases with two-part fractures had satisfactory results (85%) while 40% of the cases with three-part fractures had unsatisfactory results. This may be related to the nature of these fractures. Three- and four-part fractures of the proximal humerus are the most severe injuries to that structure. Evaluation and treatment can be challenging. However, a thorough knowledge of normal glenohumeral relationships and careful attention to factors such as fracture pattern, bone quality, patient motivation, and expectations will optimize treatment outcome. Patients who are physiologically young and have good bone quality will benefit from attempts to preserve the native anatomy with open reduction and internal fixation. Patients who are elderly and have poor bone quality are better treated with early hemiarthroplasty. Those who are medically unable to undergo the rigors of surgery or rehabilitation may be treated nonoperatively [15].
The weakness of our study is the small number of cases. In fact, the literature is not rich in the palm tree technique and further studies are required to assess the results of the technique and the value of these modifications.
Conclusion
The palm tree technique with these modifications is a good method for fixation of proximal humeral fractures. It is a minimally invasive technique and produces good grip in both of the proximal and distal fragments. It allows for early joint movements with subsequent good results.
Acknowledgments
Conflict of interest statement The author has not received any benefit for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996;18(Suppl 3):209S–213S. doi: 10.1016/8756-3282(95)00504-8. [DOI] [PubMed] [Google Scholar]
- 2.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–164. [PubMed] [Google Scholar]
- 3.Descamps PY, Fabeck L, Krallis P, Hardy D, Delincé P. Biomechanical evaluation of Hackethal's intramedullary bundle pin fixation of humeral neck fractures. Acta Orthop Belg. 2001;67(3):219–225. [PubMed] [Google Scholar]
- 4.Fenichel I, Oran A, Burstein G, Perry Pritsch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop. 2006;30(3):153–157. doi: 10.1007/s00264-005-0058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerber C, Werner CM, Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86:848–855. doi: 10.1302/0301-620X.86B6.14577. [DOI] [PubMed] [Google Scholar]
- 6.Henley MB, Chapman JR, Claudi BF. Closed retrograde hackethal nail stabilization of humeral shaft fractures. J Orthop Trauma. 1992;6:18. [PubMed] [Google Scholar]
- 7.Herscovici D, Jr, Saunders DT, Johnson MP, Sanders R, DiPasquale T. Percutaneous fixation of proximal humeral fractures. Clin Orthop Relat Res. 2000;375:97–104. doi: 10.1097/00003086-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Jiang C, Zhu Y, Wang M, Rong G. Biomechanical comparison of different pin configurations during percutaneous pinning for the treatment of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(2):235–239. doi: 10.1016/j.jse.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Kapandji A. Osteosynthesis using the "palm-tree" nail technic in fractures of the surgical neck of the humerus. Ann Chir Main. 1989;8(1):39–52. doi: 10.1016/S0753-9053(89)80044-4. [DOI] [PubMed] [Google Scholar]
- 10.Lascombes P, Prevot J, Ligier JN, Mataizeau JP, Poncelet T. Elastic stable intramedullary nailing in forearm shaft fractures in children: 85 cases. J Pediatr Orthop. 1990;10:167. [PubMed] [Google Scholar]
- 11.Bellec Y, Masmejean E, Cottias P, Alnot JY, Huten D. Internal fixation of proximal humerus fracture by "palm tree" pinning. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(4):342–348. [PubMed] [Google Scholar]
- 12.Lind T, Korner K, Jansen J. The epidemiologic features of the proximal humerus. Arch Orthop Trauma Surg. 1989;108:285. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 13.Metaizeau JP. Stable elastic intramedullary nailing for fractures of the femur in children. J Bone Joint Surg Br. 2004;86(7):954–957. doi: 10.1302/0301-620X.86B7.15620. [DOI] [PubMed] [Google Scholar]
- 14.Naidu SH, Bixler B, Capo JT, Moulton MJ, Radin A. Percutaneous pinning of proximal humerus fractures: a biomechanical study. Orthopedics. 1997;20(11):1073–1076. doi: 10.3928/0147-7447-19971101-13. [DOI] [PubMed] [Google Scholar]
- 15.Naranja RJ, Iannotti JP. Displaced three- and four-part proximal humerus fractures: evaluation and management. J Am Acad Orthop Surg. 2000;8:373–382. doi: 10.5435/00124635-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Neer CS., II Displaced proximal humerus fractures: part I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077. [PubMed] [Google Scholar]
- 17.Pospula W, Abu Noor T. Hackethal bundle nailing with intramedullary elastic nails in the treatment of two- and three-part fractures of the proximal humerus: initial experience at Al Razi Hospital, Kuwait. Med Princ Pract. 2009;18(4):284–288. doi: 10.1159/000215725. [DOI] [PubMed] [Google Scholar]
- 18.Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Jt Surg Am. 2001;83A(11):1695–1699. doi: 10.2106/00004623-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Vogel G, Chechick A, Perry Pritch M, Brosh T. Fixation of humeral surgical neck fracture using contoured pins versus straight pins: a mechanical study. Int Orthop (SICOT) 2007;31:811–815. doi: 10.1007/s00264-006-0266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]