Abstract
Study Objectives:
o advance our understanding of the interplay of socioeconomic factors, occupational exposures, and race/ethnicity as they relate to sleep duration. We hypothesize that non Hispanic African/Caribbean immigrant employees in long term health care have shorter sleep duration than non Hispanic white employees, and that low education, low income, and occupational exposures including night work and job strain account for some of the African/Caribbean immigrant–white difference in sleep duration.
Design:
Cross sectional
Setting:
Four extended care facilities in Massachusetts, United States
Participants:
340 employees in extended care facilities
Measurements and Results:
Sleep duration was assessed with wrist actigraphy for a mean of 6.3 days. In multivariable regression modeling controlling for gender and age, African/Caribbean immigrants slept 64.4 fewer minutes (95% CI: −81.0, −47.9) per night than white participants; additional control for education and income reduced the racial gap to 50.9 minutes (−69.2, −32.5); additional control for the occupational factors of hours worked per week and working the night shift reduced the racial gap to 37.7 minutes (−57.8, −17.6).
Conclusions:
his study provides support for the hypothesis that socioeconomic and occupational characteristics explain some of the African/ Caribbean immigrant–white difference in sleep duration in the United States, especially among health care workers.
Citation:
Ertel KA; Berkman LF; Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immi grants and US white health care workers. SLEEP 2011; 34(4):509-518.
Keywords: Racial and ethnic disparities, health, sleep duration, occupation, work family, actigraphy
INTRODUCTION
Short sleep duration is associated with weight gain, obesity, type 2 diabetes, elevated blood pressure, cardiovascular disease, and premature mortality.1–6 Together, these health outcomes represent a large portion of the burden of morbidity and mortality, both in the United States7 and across the world.8
In the United States, sleep duration has been found to vary by race, with most studies using polysomnography or actigraphy to assess objective sleep duration reporting that black Americans have shorter sleep durations than white Americans.9–12 However, at least one study, using polysomnography in an inpatient research setting, reported longer sleep for blacks.13 It may be that black Americans tend to have “extremes” of sleep duration, either short or long.14,15 In samples of sufficient size, both long and short sleep duration are related to increased health risks.5,14,16,17 It has been suggested that sleep durations at both ends of the sleep duration distribution may help account for racial disparities in a broad array of health outcomes.14
Central to understanding why non-Hispanic blacks have suboptimal sleep duration is the identification of social and environmental conditions that may account for the associations between race/ethnicity and patterns of sleep. Hypothesized explanations for racial differences in sleep have focused on socioeconomic position and the living environment.9,14 While these factors may be associated with sleep outcomes, few studies have examined directly whether they explain racial differences in sleep and relatively few studies are poised to address questions regarding such differences in sleep.
Another complicating factor is that groupings according to race often conceal important heterogeneity within the group. Important considerations in racial/ethnic groupings as they relate to sleep may be immigrant status, country of origin, and acculturation.18–21 For example, among black Americans living in Brooklyn, New York, Caribbean Americans reported fewer sleep complaints compared to US-born African Americans, while immigrant European Americans reported more sleep complaints than US-born European Americans.19 Financial hardship has been explicitly linked to sleep loss in African migrants to Canada22 but did not explain the shorter polysomnographic-measured sleep duration in African Americans compared to whites.11 Very little is known about black immigrants to the US and how their sleep patterns may differ from US-born blacks or other racial/ethnic groups.
In this paper, we explore the interplay of race/ethnicity, socioeconomic factors, occupational characteristics, and sleep duration in a diverse, generally low-wage cohort of employees in the health care sector. The non-Hispanic black participants are primarily immigrants, with the majority born in Haiti. Thus, we refer to this grouping as African/Caribbean immigrants. We compare sleep duration between African/Caribbean immigrants and US whites and investigate whether socioeconomic and occupational factors help explain observed differences in sleep duration. While this study is cross-sectional and cannot reveal temporal or causal links between social conditions and health outcomes, it can provide important clues as to why African/Caribbean black men and women working in the health care sector may have poorer patterns of sleep that put them at risk for subsequent increases in morbidity and mortality.
Socioeconomic Status and Sleep Duration
A number of studies have reported an association between sleep duration and various indicators of socioeconomic status (SES); though there are important exceptions.10,23 Paralleling patterns in racial differences in sleep, it appears that individuals at the lowest SES levels (indicated by education, income, and employment status) are more likely to have both long and short sleep duration than individuals with higher SES.24,25 Considering differences in income and education according to race/ethnicity in the US, it has been suggested that these factors may explain racial/ethnic differences in sleep. Few studies have examined this directly, and these studies have produced conflicting results.9–11,14,26
Occupational Exposures and Sleep Duration
In addition, and related, to education and income disparities, black Americans and other minority groups tend to occupy different jobs with different occupational exposures, conditions, and stressors. Industry and occupation are increasingly recognized as important factors in shaping sleep patterns among employees.27 A number of occupations have well-characterized working conditions that are likely to affect sleep outcomes. These include shift work generally but night shift specifically, working very long hours, and job strain.28–34 Surprisingly, sleep duration per se has seldom been examined in relation to occupational factors. Further, occupational factors have never, to our knowledge, been examined as potential explanatory factors in racial differences in sleep.
The goal of this study is to advance our understanding of the interplay of socioeconomic factors, occupational exposures, and race/ethnicity as they relate to measured sleep duration. We also studied 3 family-related factors as they relate to sleep duration: presence of a child in the household, self-reported work-to-family spillover, and whether the participant was the primary wage earner in the household. This study used wrist actigraphy devices over a week to measure daily sleep duration. The long-term care sector is particularly interesting for sleep studies, as the around the clock nature of the work requires shift work and there are a range of very different occupations within an institution (including health care workers, administration, and dietary, maintenance and janitorial staff).
We hypothesized that adverse socioeconomic and occupational exposures as well as shorter sleep duration are associated with non-white race/ethnicity. Specifically, we think African/ Caribbean immigrant employees are more likely than non-Hispanic whites to have low income, low education, work the night shift, and report high job strain. Finally, we hypothesized that socioeconomic factors and occupational exposures account for at least some of the difference in sleep duration between US white and African/Caribbean immigrant employees.
METHODS
Sample and Data Collection
Subjects were employees from 4 extended-care facilities in Massachusetts who took part in a cross-sectional survey of employee experiences with workplace policies and informal practices. We chose extended-care facilities due to interest in the health care sector and interest in small-sized businesses that employ lower-wage and racially/ethnically diverse work-forces. Trained research assistants administered the survey in English, Spanish, and Haitian Creole between September 2006 and July 2007. We conducted interviews during employees' work shifts; interviews took approximately 40 minutes. We invited all eligible employees at each worksite to participate in the survey (n = 590), with a response rate of 76.6% (n = 452). In addition to the survey, we invited employees to wear a wrist actigraphy device to measure sleep duration. Of the 452 subjects who responded to the survey, we obtained wrist actigraph data from 365 participants. We excluded 4 outliers with long sleep duration (≥ 700 min) because of uncertainty about the validity of these recordings, as well as the probability that they would unduly influence linear regression results. We also excluded 21 subjects because of missing exposure and covariate information, resulting in a sample size of 340. Informed consent was obtained from each study participant. This study was approved by the Institutional Review Board at the Dana Farber Cancer Institute, Boston MA.
Measures
Sleep duration
We measured sleep duration with wrist actigraphy (AW-64, Minimitter, Bend OR). An actigraphic recorder is a small (17 grams) wrist-worn device that measures activity over extended periods in a noninvasive and discreet manner. Actigraphy represents a generally reliable, valid measure of sleep duration35 useful in large-scale studies.9,6,37 We instructed participants to wear the wrist actigraphy monitor continuously for a week. Valid data were defined as complete 24-h recordings with < 30 min of missing data. Total sleep duration per day was estimated for visually defined sleep periods using the Actiware Sleep software provided by the manufacturer. We use total sleep duration (instead of sleep at night) in order to include naps and daytime sleep that are critical for employees who work the night shift or have rotating shift work. Participants wore the actigraphy monitor for an average of 6.3 valid days (median = 7, range: 1-10); 96% (n = 326) had ≥ 3 valid days of actigraphy data.
Race/ethnicity
We assessed race/ethnicity with 2 questions: “Are you Hispanic or Latino” and “Which of the following describes you?” with possible responses: American Indian or Alaska Native, Asian, black or African American, Native Hawaiian/other Pacific Islander, white, other. The 26 participants who identified themselves as “Hispanic or Latino” were classified as Hispanic. Of the 126 non-Hispanic black subjects, 118 (94%) were foreign-born; among foreign-born blacks, the majority (n = 70, 56%) were born in Haiti, and the rest were from other Caribbean or African nations. Thus, we use the term African/Caribbean immigrant instead of “black” or “African American” to more accurately describe the racial/ethnic make-up of this group. Of the 144 non-Hispanic white subjects, 130 (90%) were born in the United States. The “other” group included 9 subjects who were born in Cape Verde, 7 subjects who were born in Haiti, 6 subjects born in the Philippines, and 12 subjects who were born in the US; no other country of birth in this category had more than 3 subjects represented. Due to sample size considerations, we focus our interpretation of results on comparisons between non-Hispanic whites (hereafter referred to as white) and African/Caribbean immigrants.
Occupational characteristics
We examined 4 types of occupational exposures: (1) hours worked per week and whether subjects worked any overtime; (2) shift work, specifically whether they usually worked the night shift and whether they reported usually working more than one shift (such as the day and the evening shift); (3) occupation; and (4) job strain. All were obtained by self-report. Hours worked per week was the sum of the average number of hours worked at the extended-care facility and the average number of hours worked at other jobs. We assessed overtime in the past 4 weeks as extra hours not usually worked. Subjects were asked which shift(s) they usually work, with response options: day (07:00-15:00), evening (15:00-23:00), and night (23:00-07:00). Subjects who selected more than one shift were coded as working multiple shifts. Subjects were coded as working the night shift if they had worked a night shift (defined as ≥ 6 h between 22:00 and 08:00) at any job in the past 4 weeks. Occupation was coded as one of 4 broad occupational categories that capture a constellation of workplace exposures. Healthcare practitioners have professional degrees (Registered Nurses or Licensed Practical Nurses) associated with their skill and have direct contact with patients. Health-care support staff are care workers in support of the practitioners; their tasks are more hands-on and do not require a professional degree beyond high school and technical training certification (certified nurse assistant). Managers/office/administrative workers primarily work at a desk and have little to no direct patient contact as a requirement of their job. Food service and maintenance are manual labor positions that include food service, housekeeping, grounds and maintenance jobs. We assessed exposure to job strain with questions derived from the theoretical and empirical work of Karasek and Theorell.38 We created scales for job demands and job control as the sum of the ordinal response options (items reverse coded where necessary) and dichotomized each of these measures at the 50th percentile. The combination of job demands and job control resulted in 4 quadrants of exposure to job strain: (1) High strain—high job demands and low control; (2) Active jobs—high job demands and high control; (3) Passive jobs—low job demands and low control; (4) Low strain—low job demands and high control.
Demographic, socioeconomic, health, and family characteristics
We included age as a continuous variable, centered at its mean. We categorized education into 4 groups: less than high school, high school diploma or GED, some college, college degree or more. We computed adjusted household income as the total household income divided by the square root of the number of individuals supported by this income; we centered this variable at its mean. Nativity was a binary variable: born in the United States or not. Health behaviors of interest were smoking (current smoker if smoke cigarettes every day or some days; otherwise not current smoker) and alcohol intake (3 categories based on number of drinks per week: 0, 1-4, 5+). We assessed symptoms of apnea with 3 items from the multivariable apnea risk index39: past-month frequency of loud snoring, snorting or gasping, and breathing stops or struggle breathing. If subjects reported experiencing these symptoms an average of ≥ 1-2 times per week, we considered them to have apnea symptoms. Family characteristics of interest were marital status, whether there was a child < 18 years in the household (binary yes/no), whether the respondent was the primary wage earner in the household (binary yes/no), and a measure of work-family spillover (a single item: In the last month, I was preoccupied with my work while I was at home. Respondents who answered “often” were coded as experiencing work-family spillover; all other responses (sometimes, rarely, and never) were coded as not experiencing work-family spillover).
Statistical Analysis
The primary outcome for this analysis is average daily minutes of total sleep time. The secondary outcome is short sleep duration, defined as average daily sleep duration ≤ 6 hours. Due to the small number of participants with long sleep (≥ 9 h; n = 15) in this working population, we were not able to study predictors of long sleep duration. We examined univariate and bivariate relations of the variables included in our analysis. We conducted bivariate analyses to compare the distribution of all variables according to racial/ethnic groups using χ2 tests for categorical variables and analysis of variance (ANOVA) tests for continuous variables. To address the primary aim of this paper, we built sequential linear regression models predicting sleep duration. In preparation for model building, we examined correlations between predictor variables; pair-wise correlations did not raise concerns about collinearity between variables. The base model, Model 1, shows the estimated association between race/ethnicity and sleep duration controlling for only gender and age. Model 2 additionally controls for the socioeconomic factors of education and household income. Model 3 adds 2 occupational factors: night work and hours worked per week. Model 4 includes all sociodemographic, occupational, and family characteristics. To test for the presence of multicol-linearity, we calculated variance inflation factors (VIF).40 No VIF exceeded 3; thus, multicollinearity was not an appreciable concern in our regression models. For all continuous predictors, we examined the distribution of residuals to determine if transformation or categorization was necessary. Residual plots revealed no breach of model assumptions.
To examine if the demographic, socioeconomic, and occupational factors had similar relations with sleep duration for African/Caribbean immigrants and US whites, we ran the primary regression model (Model 3 in Table 3) in each group separately. To predict short sleep duration (≤ 6 h), we used the same covariates and model sequence in logistic regression analysis. For model parsimony, variables that were not of primary interest and did not confound the association between race/ethnicity and sleep duration (as assessed by a 10% change in the estimate of race/ethnicity upon addition to the model) were not included in the models presented here; these variables were marital status, foreign-born, alcohol intake, and apnea symptoms. In addition to potentially being a confounding factor, place of birth (US- or foreign-born) may be an effect modifier. Though we were limited in our ability to test for effect modification because immigrant status aligned so closely with racial group (94% of African/Caribbean black subjects were foreign-born and 90% of white subjects were US-born), we examined multivariable regression results when we excluded US-born black subjects as well as foreign-born white subjects. Additionally, because of the small number of males, we were not able to stratify analyses by gender; to examine if effects differed by gender, we repeated all models among females only. All statistical analyses were performed in SAS, version 9.1.3 (SAS Institute, Cary, NC, USA).
Table 3.
Multivariable linear regression models predicting mean daily sleep duration in minutes (n = 340)
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |||||
| Intercept | 449.8 | 438.3 | 461.3 | 442.8 | 421.1 | 464.5 | 441.6 | 419.7 | 463.5 | 441.8 | 411.2 | 472.5 |
| Race/ethnicity | ||||||||||||
| NH White | 0(ref) | 0(ref) | 0(ref) | 0(ref) | ||||||||
| NH Afr/Crb Immigrant | -64.4 | -81.0 | -47.9 | -50.9 | -69.2 | -32.5 | -37.7 | -57.8 | -17.6 | -39.6 | -60.9 | -18.3 |
| Hispanic | -33.9 | -62.8 | -5.0 | -22.8 | -52.5 | 6.9 | -13.6 | -43.6 | 16.5 | -20.0 | -50.9 | 10.8 |
| Other | -38.4 | -61.0 | -15.9 | -30.6 | -53.8 | -7.4 | -23.3 | -46.8 | 0.1 | -25.7 | -49.7 | -1.7 |
| Gender | ||||||||||||
| Male | -28.2 | -47.2 | -9.2 | -29.1 | -48.0 | -10.3 | -25.6 | -44.3 | -7.0 | -31.0 | -52.8 | -9.1 |
| Female | 0(ref) | 0(ref) | 0(ref) | 0(ref) | ||||||||
| Age (years) | -0.3 | -0.8 | 0.3 | -0.2 | -0.8 | 0.3 | -0.1 | -0.7 | 0.4 | -0.2 | -0.8 | 0.4 |
| Education | ||||||||||||
| Less than high school | -6.5 | -35.5 | 22.6 | -12.6 | -41.3 | 16.0 | -20.6 | -51.3 | 10.2 | |||
| High school of GED | -1.1 | -25.2 | 22.9 | -3.4 | -27.3 | 20.5 | -10.2 | -36.2 | 15.7 | |||
| Some college | 5.4 | -17.4 | 28.1 | 3.1 | -19.3 | 25.5 | 0.0 | -22.8 | 22.9 | |||
| College or more | 0(ref) | 0(ref) | 0(ref) | |||||||||
| Household Income (per $1,000) | 0.8 | 0.2 | 1.5 | 0.9 | 0.3 | 1.5 | 1.0 | 0.3 | 1.7 | |||
| Currently smokes | 3.0 | -16.0 | 22.0 | 5.3 | -14.1 | 24.7 | ||||||
| Worked night shift in past 4weeks | -14.9 | -31.4 | 1.6 | -14.8 | -32.2 | 2.5 | ||||||
| Work hours per week (hours) | -1.1 | -1.8 | -0.5 | -1.1 | -1.7 | -0.4 | ||||||
| Worked overtime in past 4weeks | -11.1 | -25.8 | 3.6 | |||||||||
| Worked multiple shifts | 5.3 | -24.9 | 35.4 | |||||||||
| Job strain category | ||||||||||||
| Passive | 6.0 | -16.8 | 28.9 | |||||||||
| Active | 0.8 | -19.7 | 21.3 | |||||||||
| High Strain | 16.8 | -6.2 | 39.7 | |||||||||
| Low Strain | 0(ref) | |||||||||||
| Occupational category | ||||||||||||
| Healthcare Practitioner (RN or LPN) | 0.0 | -24.6 | 24.6 | |||||||||
| Healthcare support (CNA) | 0(ref) | |||||||||||
| Office and administrative | -1.0 | -31.9 | 29.9 | |||||||||
| Food Service and maintenance | 14.0 | -8.0 | 35.9 | |||||||||
| Primary wage earner in household | 11.3 | -4.7 | 27.3 | |||||||||
| Often preoccupied with work while at home | -12.4 | -38.5 | 13.8 | |||||||||
| Child under 19years in household | -4.5 | -20.2 | 11.1 | |||||||||
CI, confidence interval; GED, graduate equivalency degree; RN, registered nurse; LPN, licensed practical nurse; CNA, certified nursing assistant.
RESULTS
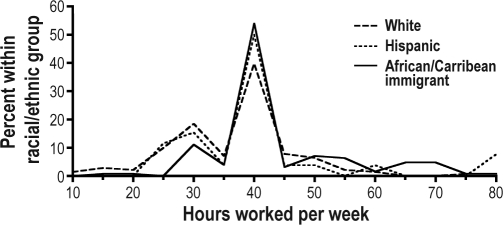
Descriptive statistics for all variables are presented in Table 1. On average, study subjects slept 413 minutes, or 6 h 53 min (SD 74 min). The sample was predominantly female (82%). Results from analyses restricted to females were very similar to results including the whole sample. Thus, we present results for the whole sample and we control for the effect of gender in all multivariable models. Non-Hispanic African/ Caribbean immigrant employees had less income and less education (P < 0.01 for both) than non-Hispanic white employees (Table 2). African/Caribbean immigrant and white participants were also significantly (P < 0.05) different according to all occupational characteristics, with the exception of working overtime (Table 2). African/Caribbean immigrant and Hispanic employees were twice as likely to work the night shift as non-Hispanic white employees. African/Caribbean immigrant participants dominated the Healthcare Support (CNA) occupational category, non-Hispanic white participants dominated the Healthcare Practitioner (RN, LPN) category, and Hispanic participants dominated Food Service and Maintenance staff positions. Nearly 45% of non-Hispanic white participants reported low job strain, whereas 41% of African/Caribbean immigrants reported high job strain. Compared to white and Hispanic participants, a higher proportion of African/Caribbean immigrant participants worked > 40 h/week (Figure 1).
Table 1.
Study population characteristics (n = 340)
| Overall |
Females |
Males |
||||
|---|---|---|---|---|---|---|
| n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | |
| Sociodemographic and Health Characteristics | ||||||
| Mean age | 41.2 | 13.3 | 41.9 | 13.2 | 37.7 | 13.5 |
| Gender | ||||||
| Female | 279 | 82.1 | ||||
| Male | 61 | 17.9 | ||||
| Race/ethnicity | ||||||
| Non-Hispanic White | 141 | 41.5 | 124 | 44.4 | 17 | 27.9 |
| Non-Hispanic African/Caribbean Immigrant | 126 | 37.1 | 101 | 36.2 | 25 | 41.0 |
| Hispanic | 26 | 7.7 | 18 | 6.5 | 8 | 13.1 |
| Other | 47 | 13.8 | 36 | 12.9 | 11 | 18.0 |
| Mean household income (adj for # supported) | 28340.9 | 13655.1 | 28564.8 | 13559.8 | 27316.8 | 14152.4 |
| Education | ||||||
| Less than high school | 52 | 15.3 | 44 | 15.8 | 8 | 13.1 |
| High school or GED | 106 | 31.2 | 88 | 31.5 | 18 | 29.5 |
| Some college | 136 | 40.0 | 110 | 39.4 | 26 | 42.6 |
| College or more | 46 | 13.5 | 37 | 13.3 | 9 | 14.8 |
| Married or living with partner (n, %yes) | 192 | 56.5 | 155 | 55.6 | 37 | 60.7 |
| Smoker (n, %yes) | 69 | 20.3 | 54 | 19.4 | 15 | 24.6 |
| Number of alcoholic drinks/week | ||||||
| 0 | 245 | 72.1 | 209 | 74.9 | 36 | 59.0 |
| 1-4 | 53 | 15.6 | 39 | 14.0 | 14 | 23.0 |
| 5+ | 42 | 12.4 | 31 | 11.1 | 11 | 18.0 |
| Foreign-born (n, %yes) | 188 | 55.3 | 149 | 53.4 | 39 | 63.9 |
| Mean hourly wage* | 15.4 | 7.2 | 15.8 | 7.3 | 13.4 | 6.3 |
| Mean body mass index* | 27.9 | 5.7 | 28.2 | 5.8 | 26.9 | 5.0 |
| Apnea* (n, %yes) | 16 | 4.8 | 15 | 5.4 | 1 | 1.7 |
| Occupational Characteristics | ||||||
| Number of hours worked/week | 40.1 | 11.9 | 39.5 | 12.1 | 43.0 | 10.4 |
| Any night shift in past 4weeks (n, %yes) | 87 | 25.6 | 68 | 24.4 | 19 | 31.2 |
| Job strain category | ||||||
| Low Strain | 97 | 28.5 | 81 | 29.0 | 16 | 26.2 |
| Passive | 75 | 22.1 | 59 | 21.2 | 16 | 26.2 |
| Active | 85 | 25.0 | 73 | 26.2 | 12 | 19.7 |
| High Strain | 83 | 24.4 | 66 | 23.7 | 17 | 27.9 |
| Occupation | ||||||
| Healthcare Practitioner (RN or LPN) | 72 | 21.2 | 65 | 23.3 | 7 | 11.5 |
| Healthcare support (CNA) | 162 | 47.7 | 147 | 52.7 | 15 | 24.6 |
| Office and administrative | 29 | 8.5 | 28 | 10.0 | 1 | 1.6 |
| Food Service and maintenance | 77 | 22.7 | 39 | 14.0 | 38 | 62.3 |
| Worked overtime in past 4weeks (n, %yes) | 161 | 47.4 | 121 | 43.4 | 40 | 65.6 |
| Worked multiple shifts (n, %yes) | 21 | 6.2 | 17 | 6.1 | 4 | 6.6 |
| Work-family Characteristics | ||||||
| Child in household (n, %yes) | 180 | 52.9 | 150 | 53.8 | 30 | 49.2 |
| Often preoccupied with work while at home (n, %yes) | 29 | 8.5 | 24 | 8.6 | 5 | 8.2 |
| Primary wage earner (n, %yes) | 184 | 54.1 | 153 | 54.8 | 31 | 50.8 |
| Outcome | ||||||
| Mean daily sleep duration (minutes) | 413.2 | 73.7 | 419.4 | 70.9 | 385.0 | 80.3 |
Sample sizes are slightly different due to missing data: wage n = 335; BMI n = 319; apnea n = 334.
GED, graduate equivalency degree; RN, registered nurse; LPN, licensed practical nurse; CNA, certified nursing assistant.
Table 2.
Bivariate associations between race/ethnicity and all study variables
| NHWhite (n = 141) |
NHAfr/Crb (n = 126) |
Hispanic (n = 26) |
Other (n = 47) |
P-value** |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n or mean | % or SE | n or mean | % or SE | n or mean | % or SE | n or mean | % or SE | |||
| Sociodemographic and Health Characteristics | ||||||||||
| Mean age | 44.5 | 14.7 | 39.1 | 11.2 | 35.3 | 11.8 | 40.2 | 13.2 | 0.00 | |
| Female (n, %yes) | 124 | 87.9 | 101 | 80.2 | 18 | 69.2 | 36 | 76.6 | 0.06 | |
| Household income (adj for # supported) | 34542 | 12908 | 21757 | 11381 | 24911 | 13875 | 29287 | 12895 | < 0.01 | |
| Education | < 0.01 | |||||||||
| Less than high school | 7 | 5.0 | 30 | 23.8 | 3 | 11.5 | 12 | 25.5 | ||
| High school or GED | 31 | 22.0 | 45 | 35.7 | 14 | 53.9 | 16 | 34.0 | ||
| Some college | 77 | 54.6 | 42 | 33.3 | 6 | 23.1 | 11 | 23.4 | ||
| College or more | 26 | 18.4 | 9 | 7.1 | 3 | 11.5 | 8 | 17.0 | ||
| Married or living with partner (n, %yes) | 76 | 53.9 | 76 | 60.3 | 12 | 46.2 | 28 | 59.6 | 0.48 | |
| Smoker (n, %yes) | 51 | 36.2 | 7 | 5.6 | 3 | 11.5 | 8 | 17.0 | < 0.01 | |
| Number of drinks/week | < 0.01 | |||||||||
| 0 | 79 | 56.0 | 112 | 88.9 | 19 | 73.1 | 35 | 74.5 | ||
| 1-4 | 34 | 24.1 | 9 | 7.1 | 5 | 19.2 | 5 | 10.6 | ||
| 5+ | 28 | 19.9 | 5 | 4.0 | 2 | 7.7 | 7 | 14.9 | ||
| Foreign-born (n, %yes) | 11 | 7.8 | 118 | 93.7 | 21 | 80.8 | 38 | 80.9 | < 0.01 | |
| Mean hourly wage* | 18.5 | 8.1 | 12.9 | 4.8 | 13.1 | 5.7 | 13.7 | 7.3 | < 0.01 | |
| Mean body mass index* | 27.1 | 5.9 | 28.7 | 5.6 | 29.0 | 4.7 | 27.8 | 5.7 | 0.12 | |
| Apnea* (n, %yes) | 5 | 3.6 | 8 | 6.5 | 2 | 7.7 | 1 | 2.3 | ||
| Occupational Characteristics | ||||||||||
| Total hours worked/week | 36.8 | 9.9 | 43.9 | 11.3 | 40.9 | 13.7 | 39.6 | 15.1 | < 0.01 | |
| Any night shift in past 4weeks (n, %yes) | 22 | 15.6 | 41 | 32.5 | 9 | 34.6 | 15 | 31.9 | 0.01 | |
| Job strain category | < 0.01 | |||||||||
| Low Strain | 62 | 44.0 | 22 | 17.5 | 3 | 11.5 | 10 | 21.3 | ||
| Passive | 20 | 14.2 | 32 | 25.4 | 9 | 34.6 | 14 | 29.8 | ||
| Active | 48 | 34.0 | 21 | 16.7 | 5 | 19.2 | 11 | 23.4 | ||
| High Strain | 11 | 7.8 | 51 | 40.5 | 9 | 34.6 | 12 | 25.5 | ||
| Occupation | < 0.01 | |||||||||
| Healthcare Practitioner (RN or LPN) | 49 | 34.8 | 13 | 10.3 | 3 | 11.5 | 7 | 14.9 | ||
| Healthcare support (CNA) | 40 | 28.4 | 91 | 72.2 | 9 | 34.6 | 22 | 46.8 | ||
| Office and administrative | 25 | 17.7 | 1 | 0.8 | 2 | 7.7 | 1 | 2.1 | ||
| Food Service and maintenance | 27 | 19.2 | 21 | 16.7 | 12 | 46.2 | 17 | 36.2 | ||
| Worked overtime in past 4weeks | 62 | 44.0 | 62 | 49.2 | 14 | 53.9 | 23 | 48.9 | 0.73 | |
| Worked multiple shifts | 4 | 2.8 | 14 | 11.1 | 1 | 3.9 | 2 | 4.3 | 0.04 | |
| Work-family Characteristics | ||||||||||
| Child in household (n, %yes) | 60 | 42.6 | 83 | 65.9 | 12 | 46.2 | 25 | 53.2 | < 0.01 | |
| Often preoccupied with work while at home | 14 | 9.9 | 8 | 6.4 | 2 | 7.7 | 5 | 10.6 | 0.70 | |
| Primary wage earner (n, %yes) | 71 | 50.4 | 73 | 57.9 | 17 | 65.4 | 23 | 48.9 | 0.34 | |
| Outcome | ||||||||||
| Mean daily sleep duration (minutes) | 445.8 | 62.1 | 380.6 | 75.8 | 409.0 | 57.9 | 405.3 | 68.3 | < 0.01 | |
Sample sizes are slightly different due to missing data: wage n = 335; BMI n = 319; apnea n = 334.
Overall chi-square or t-test P-value.
GED, graduate equivalency degree; NH, non-Hispanic; RN, registered nurse; LPN, licensed practical nurse; CNA, certified nursing assistant.
Figure 1.
Hours worked per week according to racial/ethnic group. he reported total hours per week at all jobs are depicted for each racial and ethnic group as a proportion of the total participants within that racial and ethnic group. Non Hispanic white participants (dashed line), non-Hispanic African/Caribbean immigrant participants (solid line), Hispanic participants (dotted line). For the purpose of illustration, hours worked per week are depicted in centered, half hour bins.
As hypothesized, African/Caribbean immigrants had shorter sleep durations than white participants (Table 2, Figure 2). As displayed in Figure 2, the whole distribution of sleep among white participants was shifted towards longer sleep than African/Caribbean immigrant participants. When adjusted for gender and age (Model 1, Table 3), the African/Caribbean immigrant–white difference in sleep duration was > 1 h (estimate = −64.4 min [95% CI: −81.0, −47.9]). Hispanic and non-Hispanic other participants also had, on average, significantly less sleep than non-Hispanic white participants, though their sleep was intermediary between whites and African/Caribbean immigrants. Further adjustment for the socioeconomic indicators of education and income (Model 2, Table 3) attenuated the African/Caribbean immigrant–white difference in sleep duration, with the estimated gap decreasing to −50.9 (−69.2, −32.5) minutes. The addition of 2 occupational variables: working the night shift and total hours worked per week (Model 3, Table 3) further attenuated the African/Caribbean immigrant–white gap to −37.7 (−57.8, −17.6) minutes. Further addition of occupational characteristics and work-family characteristics (Model 4, Table 3) did not attenuate the African/Caribbean immigrant– white gap any further. Restriction to foreign-born blacks and US-born whites did not alter observed associations in multivariable modeling. Overall, the addition of socioeconomic and workplace conditions contributed to a substantial reduction in the difference in sleep duration between African/Caribbean immigrant and non-Hispanic white employees in the long-term care settings. While there continues to be a large difference in average sleep duration between African/Caribbean immigrants and whites, the difference was reduced by 41% in these analyses, suggesting that a large portion of the gap is attributable to socioeconomic conditions and work environment.
Figure 2.
Daily sleep duration according to racial/ethnic group. he daily sleep duration assessed by wrist actigraphy is depicted for each racial and ethnic group as a proportion of the total participants within that racial and ethnic group. Non Hispanic white participants (dashed line), non Hispanic African/Caribbean immigrant (solid line), Hispanic participants (dotted line). For the purpose of illustration, hours of sleep/ day are depicted in centered, half hour bins.
In race/ethnicity stratified models, gender, night work, and total hours worked/week were particularly salient predictors of shorter sleep duration in African/Caribbean immigrants. In a model controlling for age, education, income, smoking status, night work, and total hours worked/week, the estimated association with sleep duration for male gender was −39.51 (−73.14, −5.89) in African/Caribbean immigrants, and −22.69 (−56.12, 10.73) in whites. In that same model, the estimate for working the night shift was −20.55 (−49.23, 8.12) in African/Caribbean immigrants, and 0.95 (−28.21, 30.11) in whites, while the estimate for work hours/week was −1.09 (−2.27, 0.08) in African/ Caribbean immigrants and −0.23 (−1.33, 0.87) in whites.
In addition to understanding racial differences in average sleep duration, it is important to examine the extremes of sleep duration because of their implications for health outcomes. In the present study, we were not able to study long sleep duration (only 15 employees slept ≥ 9 h), but could examine short sleep duration. Models predicting short sleep duration showed a similar pattern to results for average sleep duration, with the odds of short sleep duration for African/Caribbean immigrants compared to whites attenuated by income, education, night work, and work hours. Using the same models as above, the odds of short sleep duration for African/Caribbean immigrants compared to whites was 9.85 (95% confidence interval: 4.49, 21.63) in Model 1 and 5.95 (2.19, 16.15) in Model 4 (Table 4).
Table 4.
Multivariable logistic regression models predicting short sleep duration (< = 6 hours)(n = 340)
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| Race/ethnicity | ||||||||||||
| NH White | (ref) | (ref) | (ref) | (ref) | ||||||||
| NH Afr/Crb Immigrant | 9.85 | 4.49 | 21.63 | 6.49 | 2.79 | 15.09 | 5.10 | 1.99 | 13.07 | 5.95 | 2.19 | 16.15 |
| Hispanic | 2.42 | 0.65 | 8.96 | 1.68 | 0.42 | 6.68 | 1.42 | 0.34 | 5.94 | 1.59 | 0.36 | 7.03 |
| Other | 4.69 | 1.80 | 12.21 | 3.72 | 1.35 | 10.26 | 3.14 | 1.08 | 9.11 | 3.43 | 1.14 | 10.35 |
| Gender | ||||||||||||
| Male | 3.52 | 1.81 | 6.86 | 3.74 | 1.88 | 7.44 | 3.65 | 1.82 | 7.35 | 4.25 | 1.73 | 10.44 |
| Female | (ref) | (ref) | (ref) | (ref) | ||||||||
| Age (years) | 1.03 | 1.00 | 1.05 | 1.03 | 1.00 | 1.05 | 1.02 | 1.00 | 1.05 | 1.02 | 1.00 | 1.05 |
| Education | ||||||||||||
| Less than high school | 1.28 | 0.40 | 4.08 | 1.52 | 0.47 | 4.88 | 1.90 | 0.53 | 6.82 | |||
| High school of GED | 1.32 | 0.46 | 3.78 | 1.38 | 0.48 | 4.01 | 1.60 | 0.49 | 5.22 | |||
| Some college | 1.14 | 0.40 | 3.24 | 1.19 | 0.41 | 3.43 | 1.29 | 0.42 | 3.94 | |||
| College or more | (ref) | (ref) | (ref) | |||||||||
| Household Income (per $1,000) | 0.97 | 0.95 | 1.00 | 0.97 | 0.94 | 0.99 | 0.97 | 0.94 | 1.00 | |||
| Currently smokes | 1.12 | 0.45 | 2.77 | 1.08 | 0.42 | 2.77 | ||||||
| Worked night shift in past 4weeks | 1.81 | 0.96 | 3.40 | 1.75 | 0.90 | 3.42 | ||||||
| Work hours per week (hours) | 1.03 | 1.01 | 1.06 | 1.03 | 1.00 | 1.05 | ||||||
| Worked overtime in past 4weeks | 1.53 | 0.82 | 2.85 | |||||||||
| Worked multiple shifts | 0.70 | 0.22 | 2.26 | |||||||||
| Job strain category | ||||||||||||
| Passive | 0.73 | 0.27 | 1.96 | |||||||||
| Active | 0.84 | 0.33 | 2.14 | |||||||||
| High Strain | 0.40 | 0.15 | 1.06 | |||||||||
| Low Strain | (ref) | |||||||||||
| Occupational category | ||||||||||||
| Healthcare Practitioner (RN or LPN) | 0.72 | 0.22 | 2.38 | |||||||||
| Office and administrative | 0.41 | 0.04 | 3.71 | |||||||||
| Food Service and maintenance | 0.63 | 0.25 | 1.61 | |||||||||
| Healthcare support (CNA) | (ref) | |||||||||||
| Primary wage earner in household | 1.06 | 0.54 | 2.08 | |||||||||
| Often preoccupied with work while at home | 0.86 | 0.27 | 2.76 | |||||||||
| Child under 19years in household | 0.92 | 0.47 | 1.80 | |||||||||
NH, non-Hispanic; Afr/Crb, African/Caribbean Immigrant; OR, odds ratio; CI, confidence interval; GED, graduate equivalency degree; RN, registered nurse; LPN, licensed practical nurse; CNA, certified nursing assistant.
DISCUSSION
African/Caribbean immigrant employees had shorter sleep durations than non-Hispanic white employees. As hypothesized, socioeconomic factors (education and household income) accounted for some of the African/Caribbean immigrant–white gap in sleep duration and occupational factors (night work and hours worked per week) accounted for an additional amount of the gap in sleep duration. Together, these factors reduced the African/Caribbean immigrant–white gap in sleep duration by 41%. This serves as a beginning to identification of other social and environmental conditions that may help us understand the racial/ethnic variations in sleep duration that have been previously reported.
Our finding of an hour difference in sleep duration between races is consistent with a middle-aged sample from the Coronary Artery Risk Development in Young Adults (CARDIA) site in Chicago,9 though larger than several other studies that report something more on the order of a half-hour difference.10,11,19 At tenuation of the racial difference in sleep duration upon control for socioeconomic variables was also seen in the CARDIA study9 and a National Health Interview Survey analysis.14 In CARDIA, a study of middle-aged adults, black-white differences in actigraphy-assessed sleep duration were reduced, though remained large, after statistical control for income, education, and employment status.9 Using self-report from the National Health Interview Survey,14 there was some attenuation of racial/ethnic differences in short (≤ 6 h) and long (≥ 9 h) sleep duration with the inclusion of marital status, education, family income, family size, and employment status. However, other studies reported that their measures of socioeconomic status did not help explain racial differences in sleep duration: Mezick et al. reported that a composite socioeconomic measure (education and income standardized and averaged) did not help explain racial differences in sleep duration,10 and Hall et al. reported that PSG-measured sleep was a half-hour shorter in African American women, but inclusion of SES measures of financial strain and education did not attenuate this relationship.11,26 Divergent findings may be explained by the use of different samples, including different ethnic and immigrant make-up of racial/ethnic groupings and community versus occupational samples, different indicators of socioeconomic status, different statistical model-building strategies, or differences in the underlying racial disparities in sleep duration.
Our finding that working the night shift and a greater number of hours predicted reduced sleep duration is consistent with several studies in occupational cohorts examining various sleep outcomes.29,33,34 The American Time Use Survey, a cross-sectional study of a nationally representative sample of Americans, found that compensated work time was the most important determinant of sleep duration, with sleep duration decreasing as work time increased31; full-time employment may also be related to the increasing trend in short sleep duration.32 Also consistent with other studies,33 after controlling for night shift and hours worked, other occupational characteristics were not particularly important in predicting sleep duration. This is the first study that we are aware of that provides evidence that night work and hours worked may help explain immigrant and racial differences in sleep outcomes.
This study extends our understanding of determinants of sleep, particularly those related to racial/ethnic differences in sleep duration in several ways. First, we add to the growing body of evidence that sleep duration varies systematically according to race in the US context. Second, we examine racial differences in sleep duration in an occupational sample in the health care setting. Health care, and particularly extended care, is an increasingly important part of US economy. In 2008 there were 3,008,000 employees in the nursing and residential care facilities industry, with an expected increase of 21.2% by 2018.41 A particularly salient characteristic of health care is the need for workers around the clock. Shift work and night work have important implications for both the health of the employees and the care provided to patients. Health care settings may offer important avenues for preventive interventions to improve employee health and well-being: a clinical trial in a medical workplace setting demonstrated that reducing work hours could improve sleep duration, workplace productivity, and patient safety.42,43 Third, we directly examined the joint actions of socioeconomic status and occupational characteristics in explaining racial/ethnic differences in sleep duration, finding that both may help explain some of the observed differences in sleep.
Limitations
Though use of an occupational cohort allowed thorough characterization of work characteristics, an occupational cohort is by definition not representative of the general population. All participants were employed, and there was a restricted range in age and income and possible healthy worker effects. The majority of the non-Hispanic black participants in this study were immigrants of Caribbean descent. Restriction to foreign-born blacks did not alter observed associations, though we did not have adequate sample sizes to determine if our findings were specific to immigrants from specific regions, nor do we have data on acculturation. Our findings may not generalize to the larger US African American population. Other researchers have found a race-related difference in sleep medication use by African American women compared to white women that may in part explain the measured difference in sleep duration,44 but we did not include questions on sleep medication use. Additionally, the range of sleep duration was restricted compared to community samples. In particular, there were few individuals with long sleep duration, which precluded analysis of both extremes of sleep duration. The majority of employees were female, limiting our ability to examine gender differences in interaction with racial differences. There is some evidence that the racial difference in sleep may be largest among men.9,19 As discussed above, we found no evidence for effect modification by gender in our sample.
Residual confounding as well as additional unmeasured conditions may have influenced associations in this study. There is always the possibility of residual effects of control variables due to imprecision in construct measurement and this is likely often the case when focusing on a complex, multidimensional construct such as socioeconomic status. We used education and income to measure SES (with additional control for occupation) which are standard indicators of SES. Use of additional indicators of SES, including wealth, and more refined measures of education (more than 4 categories) may reveal that more of the racial difference in sleep is attributable to SES. We did not have information about neighborhood or the home sleeping environment that may affect sleep duration. We captured some home and family exposures, though they did not play a large role in this analysis. It is possible that more detailed descriptions of home and family stressors in future research may reveal important influences on sleep.
CONCLUSIONS
In summary, this study provides evidence that socioeconomic and occupational characteristics explain some of the African/Caribbean immigrant–white difference in sleep, but there are also other factors at play. After statistically controlling for sociodemographic, occupational, and home characteristics, the African/Caribbean immigrant–white difference in sleep duration was reduced by 41%. Male gender, night work, and total hours worked/week were particularly salient predictors of shorter sleep duration in African/Caribbean immigrants. While we cannot establish causality in this cross sectional study, we can start to identify conditions that are associated with poor outcomes. Further longitudinal or intervention studies can evaluate the causal pathways linking race/ethnicity, sleep duration, and adverse health outcomes. Due to the role of sleep for many health outcomes, it is important to understand systematic differences in sleep duration. Understanding the causes and processes that afford adequate sleep duration may inform interventions and policies aimed at promoting optimal sleep duration and the workplace may be an ideal setting for such interventions.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Buxton has received the use of equipment from Philips/Respironics, research support from Sepracor and has consulted for Sepracor and Dinsmore. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The work reported herein was conducted at the Harvard School of Public Health. This research was conducted as part of the Work, Family and Health Network (www.WorkFamily-HealthNetwork.org), which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: National Institute of Child Health and Human Development (Grant # U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (Grant # U01AG027669), Office of Behavioral and Science Sciences Research, and National Institute for Occupational Safety and Health (Grant # U010H008788). Grants from the William T. Grant Foundation and the Administration for Children and Families have provided additional funding. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices. Special acknowledgment goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, PhD, and Lynne Casper, PhD, for design of the original Work-place, Family, Health and Well-Being Network Initiative. We wish to thank Michael Ostler for assistance with data collection and Emily Reid for assistance with data collection and analysis.
REFERENCES
- 1.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27:205–11. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 3.Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J. Work schedule, needle use, and needlestick injuries among registered nurses. Infect Control Hosp Epidemiol. 2007;28:156–64. doi: 10.1086/510785. [DOI] [PubMed] [Google Scholar]
- 4.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 5.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010 doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 6.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–7. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. Nutrition and over-weight. Tracking Healthy People 2010. Washington, DC: U.S. Government Printing Office; 2000. pp. B19-1–B19-42. [Google Scholar]
- 8.World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 9.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 10.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008;70:410–6. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 12.Walsleben JA, Kapur VK, Newman AB, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep. 2004;27:293–8. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 13.Profant J, Ancoli-Israel S, Dimsdale JE. Are there ethnic differences in sleep architecture? Am J Hum Biol. 2002;14:321–6. doi: 10.1002/ajhb.10032. [DOI] [PubMed] [Google Scholar]
- 14.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: results of the National Health Interview Survey. J Natl Med Assoc. 2008;100:317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 16.Lieberman HR, Tharion WJ, Shukitt-Hale B, Speckman KL, Tulley R. Effects of caffeine, sleep loss, and stress on cognitive performance and mood during U.S. Navy SEAL training. Sea-Air-Land. Psychopharmacology (Berl.) 2002;164:250–61. doi: 10.1007/s00213-002-1217-9. [DOI] [PubMed] [Google Scholar]
- 17.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 18.Voss U, Tuin I. Integration of immigrants into a new culture is related to poor sleep quality. Health Qual Life Outcomes. 2008;6:61. doi: 10.1186/1477-7525-6-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jean-Louis G, Kripke DF, Ancoli-Israel S, Klauber MR, Sepulveda RS. Sleep duration, illumination, and activity patterns in a population sample: Effects of gender and ethnicity. Biol Psychiatry. 2000;47:921–7. doi: 10.1016/s0006-3223(99)00169-9. [DOI] [PubMed] [Google Scholar]
- 20.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2009 Sep 1; doi: 10.1007/s10903-009-9284-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33:962–7. doi: 10.1093/sleep/33.7.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simich L, Hamilton H, Baya BK. Mental distress, economic hardship and expectations of life in Canada among Sudanese newcomers. Transcult Psychiatry. 2006;43:418–44. doi: 10.1177/1363461506066985. [DOI] [PubMed] [Google Scholar]
- 23.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;64:337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Troxel WM, Buysse DJ, Matthews KA, et al. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33:973–81. doi: 10.1093/sleep/33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luckhaupt SE, Tak S, Calvert GM. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep. 2010;33:149–59. doi: 10.1093/sleep/33.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med (Lond) 2003;53:89–94. doi: 10.1093/occmed/kqg046. [DOI] [PubMed] [Google Scholar]
- 29.Åkerstedt T. Shift work and disturbed sleep/wakefulness. Sleep Med Rev. 1998;2:117–28. doi: 10.1016/s1087-0792(98)90004-1. [DOI] [PubMed] [Google Scholar]
- 30.Härmä M, Tenkanen L, Sjöblom T, Alikoski T, Heinsalni P. Combined effects of shift-work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scand J Work Environ Health. 1998;24:300–7. doi: 10.5271/sjweh.324. [DOI] [PubMed] [Google Scholar]
- 31.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: Sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ribet C, Derriennic F. Age, working conditions, and sleep disorders: a longitudinal analysis in the French cohort E.S.T.E.V. Sleep. 1999;22:491–504. [PubMed] [Google Scholar]
- 34.Akerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Work organisation and unintentional sleep: results from the WOLF study. Occup Environ Med. 2002;59:595–600. doi: 10.1136/oem.59.9.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Littner M, Hirshkowitz M, Kramer M, et al. Practice parameters for using polysomnography to evaluate insomnia: an update. Sleep. 2003;26:754–60. doi: 10.1093/sleep/26.6.754. [DOI] [PubMed] [Google Scholar]
- 36.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Stability of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Questionnaires over 1 year in early middle-aged adults: the CARDIA study. Sleep. 2006;29:1503–6. doi: 10.1093/sleep/29.11.1503. [DOI] [PubMed] [Google Scholar]
- 37.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-individual daily and yearly variability in actigraphically recorded sleep measures: the CARDIA study. Sleep. 2007;30:793–6. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karasek R, Theorell T. Healthy work: Stress, productivity, and the reconstruction of working life. New York, NY: Basic Books; 1990. [Google Scholar]
- 39.Maislin G, Pack AI, Kribbs NB, et al. A survey screen for prediction of apnea. Sleep. 1995;18:158–66. doi: 10.1093/sleep/18.3.158. [DOI] [PubMed] [Google Scholar]
- 40.Belsley DA, Kuh E, Welsch RE. Regression diagnostics: identifying influential data and sources of collinearity. New York: Wiley-Interscience; 1980. [Google Scholar]
- 41.Bureau of Labor Statistics, U. S. Department of Labor. Career Guide to Industries: Healthcare. 2010. http://www.bls.gov/oco/cgs035.htm (2010-11). 6-2-2010.
- 42.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 43.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 44.Allen KD, Renner JB, DeVellis B, Helmick CG, Jordan JM. Racial differences in sleep medication use: a cross-sectional study of the Johnston County Osteoarthritis Project. Ann Pharmacother. 2008;42:1239–4. doi: 10.1345/aph.1L111. [DOI] [PMC free article] [PubMed] [Google Scholar]