Abstract
Background
Musculoskeletal disorders are the most common cause of disability in many industrial countries. Recurrent and chronic pain accounts for a substantial portion of workers' absenteeism. Neck pain seems to be more prominent in the general population than previously known.
Objectives
To determine the effectiveness of workplace interventions (WIs) in adult workers with neck pain.
Search methods
We searched: CENTRAL (The Cochrane Library 2009, issue 3), and MEDLINE, EMBASE, CINAHL, PsycINFO, ISI Web of Science, OTseeker, PEDro to July 2009, with no language limitations;screened reference lists; and contacted experts in the field.
Selection criteria
We included randomised controlled trials (RCT), in which at least 50% of the participants had neck pain at baseline and received interventions conducted at the workplace.
Data collection and analysis
Two review authors independently extracted data and assessed risk of bias. Authors were contacted for missing information. Since the interventions varied to a large extend, International Classification of Functioning, Disability and Health (ICF) terminology was used to classify the intervention components. This heterogeneity restricted pooling of data to only one meta‐analysis of two studies.
Main results
We identified 1995 references and included10 RCTs (2745 workers). Two studies were assessed with low risk of bias. Most trials (N = 8) examined office workers. Few workers were sick‐listed. Thus, WIs were seldom designed to improve return‐to‐work. Overall, there was low quality evidence that showed no significant differences between WIs and no intervention for pain prevalence or severity. If present, significant results in favour of WIs were not sustained across follow‐up times. There was moderate quality evidence (1 study, 415 workers) that a four‐component WI was significantly more effective in reducing sick leave in the intermediate‐term (OR 0.56, 95% CI 0.33 to 0.95), but not in the short‐ (OR 0.83, 95% CI 0.52 to 1.34) or long‐term (OR 1.28, 95% CI 0.73 to 2.26). These findings might be because only a small proportion of the workers were sick‐listed.
Authors' conclusions
Overall, this review found low quality evidence that neither supported nor refuted the benefits of any specific WI for pain relief and moderate quality evidence that a multiple‐component intervention reduced sickness absence in the intermediate‐term, which was not sustained over time. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. There is an urgent need for high quality RCTs with well designed WIs.
Keywords: Adult, Humans, Occupational Health, Ergonomics, Neck Pain, Neck Pain/rehabilitation, Occupational Diseases, Occupational Diseases/rehabilitation, Posture, Randomized Controlled Trials as Topic, Relaxation Therapy
Workplace interventions for workers with neck pain
Studies have shown that musculoskeletal disorders are the most common cause of sick‐leave and disability in many industrial countries. Neck pain is more common in the general population than previously known.This Cochrane review presents what we know from research about the effect of workplace interventions for workers with neck pain who, for the most part, are not sick‐listed.
Ten trials with 2745 participants were included in this review. Two studies were rated as having low risk of bias. The workplace interventions comprised education about stress management, principles of ergonomics, anatomy, musculoskeletal disorders, and the importance of physical activity. They taught 'pause gymnastics', how to use a relaxed work posture, proper positioning, the importance of rest breaks, and strategies to improve relaxation. Some studies also included how to modify work tasks, work load, working techniques, working positions, and working hours. Several studies suggested how to make adjustments and recommended alternatives to the existing furniture and equipment at the workplace.
The present review found low quality evidence that those who received workplace interventions did not get more pain relief than those who received no interventions. We found moderate quality evidence (1 trial, 415 workers) that workplace interventions reduced sick leave among the workers at six month‐, but not at three‐ and 12‐month follow‐ups. This could be due to the fact that few participants in the study were sick‐listed. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate for both pain and sickness absence.
Summary of findings
Summary of findings for the main comparison.
workplace interventions compared to no intervention for neck pain
| workplace interventions compared to no intervention for neck pain | ||||||
| Patient or population: patients with neck pain Settings: work places Intervention: workplace interventions Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| no intervention | workplace interventions | |||||
| Current pain at 10/12 months follow‐up VAS and five‐point scale. Scale from: 0 to 5/10. Follow‐up: 10‐12 months | The mean Current pain at 10/12 months follow‐up in the intervention groups was 0.12 standard deviations lower (0.36 lower to 0.2 higher) | 267 (2 studies) | ⊕⊕⊝⊝ low1,2 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Uncertain allocation concealment, no participant and care provider blinding. 2 95% confidence interval includes no effect.
Background
Neck pain in workers
Musculoskeletal disorders (MSD) are the most common causes of long‐term sick‐leave and disability pension in several industrial countries. Lost days due to MSD are 42%, 40% and 33% in Norway, Sweden and the United States, respectively (Nordlund 2004; Statistics Norway 2004; US Dept Labor 2004). Recurrent and chronic pain account for a substantial portion of worker absenteeism (Nachemson 2000; Nordlund 2004) and the low‐back and neck comprise the most common pain locations. In addition to personal consequences, such disorders represent a large economic loss for society (Hansson 2005).
Neck pain seems to be more prominent in the general population than previously known (Lidgren 2008). A recent review showed that neck pain is common in the adult population; in the majority of studies included in the review, the annual prevalence was between 20% and 50% (Hogg‐Johnson 2008). In another large review, the annual prevalence of neck pain among workers varied considerably across countries, from 27.1% in Norway and 33.7% in the UK, to 47.8% in Quebec, Canada (Côté 2008). In single studies, totally different occupations, such as dentists, nurses, office workers and crane operators have been shown to have a prevalence of neck pain above 50%, while the annual prevalence of sick leave due to neck pain varies in available studies from 5% to10% (Côté 2008). Office and computer workers had the highest incidence of neck disorders (Côté 2008) amongst all occupations studied, which is higher than the prevalence in the general population (Hush 2006).
The causes for musculoskeletal disorders, including neck pain, are multifactorial (Bongers 2006; Côté 2008; Punnet 2004). Self‐reported physical exposure such as sedentary positions in prolonged periods, repetitive work, cervical spine in flexion for prolonged time, working in awkward positions, inadequate keyboard and mouse position, no chair armrest, and upper extremity posture have been shown to be risk factors for neck pain (Ariens 2001; Côté 2008; van der Windt 2000). Self‐reported psychosocial work exposure such as job strain, low co‐worker support, decreased job security and overall stress at work have also been shown to be risk factors for neck pain (Ariens 2000; Bongers 2002; Boyle 2008; Côté 2008; van der Windt 2000). Individual factors such as age, gender, education (Côté 2008; Linton 2000) and non‐work‐related factors also contribute to the explanation of the prevalence of neck pain (Bongers 2002; Boyle 2008; Côté 2008). Neck pain is a condition characterised by lapses and relapses (Guzman 2008) that sometimes, but not always, result in episodes of sick leave. Due to this complexity, the contribution of different risk factors in the development and exacerbation of problems in the neck and shoulder may be difficult to explain.
Workplace interventions
Four premises have made the workplace a more focused arena for interventions. First, the responsibility for health and sick leave has gradually been transferred from the healthcare system to the employer. This has also been expressed though the model of Corporate Social Responsibilities (CRS), which, among other factors, targets the company's responsibilities towards their own employees' health and absence. Accordingly, new social policies and systems highlight a more spacious or inclusive working life (Norwegian Government 2005), where the stakeholders' involvement and closer contact between the employee and employer are anticipated (Aas 2008). An implication is that the workplace is a core intervention arena in western health and social policy. This development has been further expanded by promotion of the Disability Management (DM) movement (Westmorland 2004). Second, the understanding of work disability has gradually changed. It is now understood to be the result of a complex interaction between components at the body, individual and societal levels (WHO 2001), or the result of the interaction between the health care, the workplace and the social security system (Aas 2009; Loisel 2001). As a result, the workplace has become more important as an intervention arena. Third, workers who have not returned to work within two to three months are at high risk for developing disability and dropping out of the work arena (Frank 1996). Therefore, encouraging early return‐to‐work by intervening at the workplace level has been seen as an efficient way to reduce socioeconomic and personal consequences of musculoskeletal disorders (Elders 2004) and crucial for reducing the distance between the workplace and the sick‐listed worker. Finally, the paradigm shift within the occupational rehabilitation field from "train‐then‐place" to "place‐then‐train" approaches (Corrigan 2001; Fadyl 2009) has strengthened the value of placement in a real context (e.g. the workplace) early in the rehabilitation process.
In this review, 'workplace interventions' (WI) were defined as: 'any action at the workplace with the aim of preventing health problems and disability, maintaining participation in work and reducing sickness absences, or facilitating early return‐to‐work. These interventions seek to modify the employees' physical or mental functions, their activity performance, participation challenges or the physical, social or attitudinal environment'. We did not include workplace interventions that focused on preventing health problems in this review.
Workplace intervention outcomes
Complex phenomena such as neck pain and sickness absence (Côté 2008) often require complex approaches. Therefore, evidence from multi‐component interventions is often needed and answering the question of which interventions work in combination becomes crucial. Multidimensional intervention strategies require the evaluation of many underlying concepts (Staal 2002). The International Classification of Functioning, Disability and Health (ICF) (WHO 2001) offers a conceptual biopsychosocial model that describes health and function (Figure 1). The ICF and the International Classification of Diseases (ICD‐10) make up the two core classification systems of the World Health Organization (WHO), where diseases, disorders and disabilities are included. The ICF codifies disabilities on different health and health‐related dimensions within a framework of up to 1424 codes. For example, in the field of occupational health, the ICF has been used: to describe work‐related factors that influence the health of employees (Heerkens 2004), to describe the content of specific outcome questionnaires (Grotle 2005), to assess function in relation to sick leave and disablement pension (Brage 2004), and as a conceptual framework to guide the development of a broader perspective of ergonomic interventions (Leyshon 2008). The ICF includes health factors that can be modified by interventions (Verbeek 2004). Therefore, in this review, we used the ICF as a conceptual framework to describe, sort and analyse workplace interventions, according to whether the intervention was trying to change or modify body function (physical or mental), activity, participation, environmental factors (physical, social or attitudinal), personal factors, or a combination of these.
Figure 1.
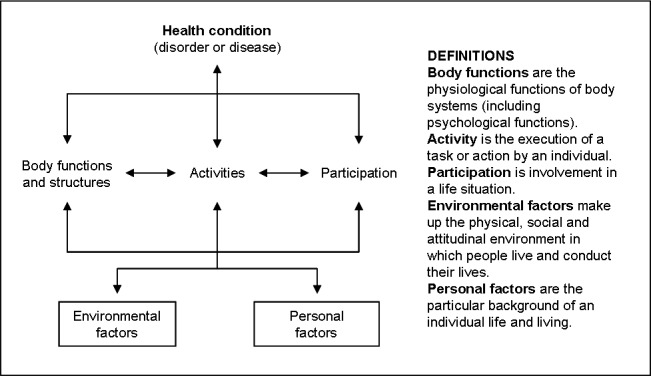
International Classification of functioning, disability and Health, ICF (WHO 2001). The model and definitions of the health and health‐related components in ICF
A focus on reducing the consequences of musculoskeletal disorders (disability prevention) is proposed as a paradigm within occupational medicine (Loisel 2001). Thus, we envisioned that some of the workplace interventions would target the underlying causes of both pain and sickness absence, to enable workers to return to work in spite of their pain. Although there are no systematic reviews examining how the workplace affects sickness absence due to neck pain, studies have shown that the workplace does have an impact (Bergstrom 2007).
Objectives
The objective of this review was to determine the effectiveness of workplace interventions compared to no treatment, usual care or other workplace interventions for adult workers with neck pain.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCT) were included. There were no language limitations on the literature search.
Types of participants
Inclusion criteria:
Age: Working age male and female adults (18 to 67 years).
Working status: Workers at work or absent from work (on sick leave, early retirement or disability pension), but still connected to a workplace by employment agreements (permanent or temporary).
Job sectors: All sectors, branches and types of jobs.
Conditions: Workers with reported neck pain of acute (less than six weeks), subacute (six to 12 weeks) or chronic (12 weeks or more) duration were included. Shoulder pain was only included when it was described in conjunction with neck pain, otherwise, it was excluded. The fluctuating nature of neck pain led to a challenge when defining the target group for this review. We solved this by including studies where at least 50% of the baseline population had neck pain. The rationale for this strategy was that since neck pain is characterised by lapses and relapses, even if 100% of the study participants had neck pain at baseline, a lower percentage would have pain at short‐, intermediate‐ and long‐term follow‐up, just by the nature of neck pain. Therefore, we also wanted to include studies where neck pain was not an inclusion criteria, but the annual prevalence of neck pain in the participants surpassed 50% at baseline.
Exclusion criteria:
Neck pain due to specific pathological conditions (e.g. fractures, tumours, infections, inflammatory processes, ankylosing spondylitis).
Studies with a baseline prevalence of neck pain below 50%.
Types of interventions
Inclusion criteria
Setting: Both group‐based and individual interventions conducted at the workplace were included; interventions could be aimed at modifying:
Body function (both physical and mental function; i.e. education and advice about workplace challenges, stress management and advice on correct positions, changing positions, relaxation, breaks)
Activity performance (i.e. graded activity (only work‐task performance adjustments, not exercises), methods of working, biomechanical work techniques, lifting, pushing and pulling techniques (actual changes not just advice), job rotation, task adjustments)
Participation (i.e. workload modifications, lighter work, work duration, reduced working hours, part‐time work, flexible working hours, active sick leave, sick leave)
Environmental (physical, social and attitudinal factors, i.e. workstation design, work layout changes, new equipment (chairs, tables, light, computer mouse, keyboard, lifting aid, office design, work space changes, communication and contact between supervisor and employee about social and attitudinal aspects, early contact, supervisor's and colleagues' abilities and attitudes, workplace culture, occupational health services, organizational changes, offer of work accommodation)
Personal factors (i.e. life cycle adaptation, lifestyle redesign, changed habits, age‐related adjustments)
The interventions could be a single strategy, or a combination of strategies, named with different intervention program labels (i.e. modified work, participatory ergonomic, ergonomic workplace visit, return‐to‐work interventions, multidisciplinary ergonomic interventions).
We performed these broad comparisons:
workplace intervention versus no interventions,
workplace intervention versus usual care,
comparison of two or more workplace interventions.
Exclusion criteria:
Setting:Clinical and healthcare interventions conducted outside the workplace were excluded.
Covered in other Cochrane Reviews:
Exercise (also group gymnastics, fitness programs, aerobics, spinning, graded exercise programs) (Kay 2005; Schonstein 2003)
Multidisciplinary biopsychosocial rehabilitation (Karjalainen 2003)
Types of outcome measures
Harms and adverse effects were included if reported in the included studies. The timing of outcome measures was reported according to the descriptions used in the included studies. They were grouped as short‐term (measured closest to four weeks post‐randomisation), intermediate‐term (measured closest to six months post‐randomisation) and long‐term (measured one year or longer post‐randomisation) (Furlan 2009).
Primary outcomes
Trials measuring at least one of the following outcomes recommended by the Cochrane Back Review Group (Furlan 2009) were included:
Pain severity or pain prevalence (self‐reported on a VAS or NSR scale, or measured as the proportion of those with pain)
Work absenteeism (time on benefits, number of hours/days on sick leave/lost time, proportion of individuals returning to work, employment status, and shift in employment status to working/part‐time working/sick listed, disability pension and early retirement)
Secondary outcomes
Global improvement (proportion of participants recovered or improved, measured by an overall judgment of improvement or treatment effectiveness)
Functional status
Well‐being / Quality of Life
Search methods for identification of studies
The search strategies for MEDLINE and EMBASE were developed according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) and the 2009 Updated method guidelines for systematic reviews in the Cochrane Back Review Group (Furlan 2009). Searches for CINAHL and PsychINFO were based on RCT search filters used at the Norwegian Knowledge Centre for the Health Services. Searches in the other databases were adapted as indicated from the search strategy for MEDLINE.
Electronic searches
Potential trials were identified with computer‐aided searches (to July 2009) in these electronic bibliographic databases:
CENTRAL (The Cochrane Library 2009, issue 3; Appendix 1)
MEDLINE (Appendix 2)
EMBASE (Appendix 3)
CINAHL (Appendix 4)
PsychINFO (Appendix 5)
ISI Web of Science (Appendix 6)
OTseeker (Occupational Therapy Systematic review of Evidence) (Appendix 7)
PEDro (The Physiotherapy Evidence database) (Appendix 8)
The intervention section of the searches was purposely left open, because of the diversity of terms used to describe workplace interventions.
Searching other resources
We screened references cited in included trials, and contacted experts in the field for further studies.
Data collection and analysis
We followed the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) and the 2009 Updated method guidelines for systematic reviews in the Cochrane Back Review Group (Furlan 2009) for these steps.
Selection of studies
The titles and abstracts (if available) of all identified studies were collected and duplicates were removed before study selection. We pilot tested our interpretation of the inclusion criteria on a sample of ten articles, including some considered to be definitely eligible, some definitely not eligible and some questionable. Thereby, the inclusion form was revised. The full text of articles whose abstracts appeared to meet our inclusion criteria, those for which we could not make a decision based on the abstract, or articles for which there were no abstracts, were obtained and independently screened by the same two review authors to determine if they met our inclusion criteria. Consensus was used to solve disagreements; if disagreements persisted, a third review author was consulted.
Data extraction and management
Two review authors independently extracted the data from the included studies onto a standardised form that included characteristics of the participants, interventions, outcomes and results. The form was developed on the basis of experiences of others. Consensus was used to solve disagreements; if disagreements persisted, a third review author was consulted.
Assessment of risk of bias in included studies
The risk of bias in the included studies was assessed using 12 criteria recommended by the Cochrane Back Review Group (Furlan 2009) and based on The Cochrane Handbook (Higgins 2008) and are defined in Appendix 9. The criteria were scored ’yes’, ’no’ or ‘unclear’ and are reported in the Risk of Bias tables. A trial with low risk of bias was defined as a trial that met, at a minimum, criteria 1 (randomisation), 2 (allocation concealment), 5 (outcome assessor blinding) and any three of the other criteria. Two review authors independently assessed a selection of trials for risk of bias and reached consensus on the final results. A third review author assessed the risk of bias for all included studies.
Measures of treatment effect
Due to between‐study diversity of interventions, outcomes and outcome measures, type of workers and follow‐up times, only one meta‐analysis could be performed. In that case, the two studies were homogeneous in their goal: both focused on the body function level. We calculated odds ratios (OR) for dichotomous data and mean differences (MD) for continuous data with 95% confidence intervals (CI) for the outcomes.
Approximately half of the results were from continuous outcomes (musculoskeletal discomfort, pain intensity (worst pain, average pain, current pain), and days on sick leave), and the other half were dichotomous outcomes (prevalence of: neck pain, discomfort, those reporting much stress, recovered, disabled, months without symptoms, and musculoskeletal sick leave).
Some of the studies tested a single intervention; some tested a set of interventions. Therefore, a content analysis of the interventions as outlined in the text of the included papers was performed to describe the exact content of the intervention. For this analysis, we used the ICF (WHO 2001) as a conceptual framework to help describe the intervention components in the included studies. As an overview, we presented the components, techniques and doses of the combined interventions in Table 8, using the ICF terminology.
Table 1.
Description of interventions in included studies
| Study | Intervention | Control |
Interventions targeting mental body functions [BF‐mental health education] |
Interventions targeting musculoskeletal body functions [BF‐physical education] [BF‐relaxation‐breaks] |
Interventions modifying activity performance [A‐ modification] |
Interventions modifying physical environment [E‐ physical modification] | Intensity / frequency | Descriptions and aims |
| Bernaards 2007 | Intervention 1 WS: Work style group (WS) Intervention 2 WSPA: Work style (WS) + lifestyle physical activity (PA)‐group |
No intervention | WS: increasing awareness of coping with high work demands and adjustments of workplace accordingly | WS: awareness of taking break, body posture and workplace adjustments PA: moderate to heavy intensive physical activities |
6 meetings/ 15 to 60 minutes each, during 6 months | Four large meetings <10 persons, two small meetings <3 persons. Trained counsellor / standardised protocol. Aim for both was behavioural change | ||
| Fostervold 2006 | Computer screen angle ‐high line of sight (HLS) | Computer screen angle ‐low line of sigh (LLS) | HLS: 15 º lower than a horizontal line to the midpoint of the screen LLS: low line of sight: 30 º lower than a horizontal line to the midpoint of the screen |
Permanent | Aim is to reduced subjective symptoms, optometric status, musculoskeletal load and other health‐related variables | |||
| Haukka 2008 | Participatory ergonomic intervention (PEI) | No intervention | Phase 1: pre‐implementation: active workshop identifying mental workload | Phase 1: pre‐implementation: active workshop with ergonomic identification of risks and problems, and planning solutions | Phase 2: implementation of 402 ergonomic changes (how many targeted the tasks) |
Phase 2: implementation of 402 ergonomic changes (how many targeted the environment?) | 11 months, 6 workshops a 3 hours each, during 9 to12 months | Built on a Finnish Participatory Ergonomic model. Aim was to prevent musculoskeletal disorders |
| Horneij 2001 | Workplace stress management group | No intervention (live as usual) | Identify and reach goals and strategies for stress (from lack of social support, low decision latitude, high psychological work load) | 12 groups, 7 meetings over 7 weeks, 1.5 hours each. Two follow‐up meetings after 3 and 6 months. | Immediate supervisors invited to join the 6th and/or 7th meeting. All participants from one workplace. Aim was to reach goals and strategies to reduce perceived stress. | |||
| Hedge 1999 | Downward tilted computer keyboard on a tray | Conventional keyboard on a flat tray | Downward tilted computer keyboard on a tray |
Permanent | ||||
| Kamwendo 1991 | Intervention 1: Traditional neck school (TNS) Intervention 2: Reinforced neck school (RNS) |
No care | RNS: interview by a psychologist on psychosocial work factors to arrive at a personal coping strategy | TNS: education about body function and ergonomics, included pause‐gymnastics and relaxation | RNS: workplace visit, discussion of ergonomic adjustments |
TNS: 4 hours RNS: 4 hours + 2 hours |
TNS: To provide them with knowledge of appropriate measures to prevent work‐related neck and shoulder pain | |
| Ketola 2002 | Intervention 1: Intensive ergonomics (IE) Intervention 2: Ergonomic education (EE) |
No care, received a leaflet | IE: work site visit including; to take breaks during work, pay attention to work posture.The worker could participate actively EE: group training session: Encourage to take short pauses |
IE: Worksite visit including; layout environmental conditions of the workroom, and adjustments of the workstation. EE: group training session: Encourage to evaluate their own workstation and implement change, and ask for equipment if needed |
IE: 1.5 to 2 hours EE: 1 hour |
|||
| Morken 2002a | Coping group sessions of MSD at the workplace | No care | Group meeting aimed at coping with MSD. Ten different topics; as musculoskeletal disorders, coping with MSD symptoms | Group meeting aimed at coping with MSD. Ten different topics; as working technique, working positions | Group meeting aimed at coping with MSD. Ten different topics; as optimal design of the workplace |
10 meetings | Three intervention groups receiving the same interventions but containing different stakeholders + changes in working environment. | |
| van den Heuvel 2003 | Intervention 1: Rest breaks (RB) Intervention 2: Rest breaks (RB) + exercise (E) |
C: Usual care | RB: five minutes rest every 35 minutes introduced by a computer program. E: four physical exercises of 45 seconds duration |
|
RB: 5 min rest every 35 min and 7 sec rest every 5 min. E: As above + physical exercises of 45 sec duration |
|||
| Voerman 2007 | MTEC: Ambulant myo‐feedback training (MT) and ergonomic counselling (EC) |
Ergonomic counselling (EC) | MTEC: Instructed to relax as a response to the myo‐feedback | EC: workplace visit included ergonomic investigation (work task, work hour, work load) | EC: workplace visit included ergonomic investigation and modifying the existing work station | MTEC and EC: 4 weeks | Myofeedback training: Sounds that are playing when muscles need relaxation. Ergonomic counselling: visited weekly by a therapist |
Physical exercises are not further described as these are not included in this review (only included when provided in combination with included interventions).
Assessing whether a specific intervention makes a clinical difference should not be based only on statistically significant findings. Thus, we tried to address five questions in order to determine the clinical relevance of the intervention (Furlan 2009), see (Appendix 10).
Dealing with missing data
We dealt with missing data according to the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008); we contacted original investigators to request missing data, we made any assumptions of methods used to cope with missing data explicit, and we addressed the potential impact of missing data.
Data synthesis
Whether we had sufficient data to combine the results statistically or not, we assessed the overall quality of the evidence for our primary outcomes by using an adapted GRADE approach (Furlan 2009). The quality of the evidence for a specific outcome was based on the performance against five domains: limitations of the study design, inconsistency, indirectness (inability to generalise) and imprecision (insufficient or imprecise data) of results and publication bias across all studies that measured that particular outcome. Two review authors independently performed the GRADE analysis.
The quality started at high when at least two RCTs with a low risk of bias provided results for the outcome, and reduced by one level for each of the domains not met.
High quality evidence = there were consistent findings among at least 75% of RCTs with no limitations of the study design, consistent, direct and precise data and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results.
Moderate quality evidence = one of the domains was not met. Further research is likely to have an important impact on our confidence in the estimate of effect and might change the estimate.
Low quality evidence = two of the domains were not met. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality evidence = three of the domains were not met. We are very uncertain about the estimate.
No evidence = no RCTs were identified that addressed this outcome
Subgroup analysis and investigation of heterogeneity
No subgroup analysis or investigation of heterogeneity was performed.
Sensitivity analysis
There were no data available with which to perform a sensitivity analysis.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
The search strategy identified 1995 references. The searches were performed up to July 2009, according to the guidelines from the Cochrane Back Review Group. In total, the search identified 182 references in CENTRAL, 439 references in MEDLINE, 672 references in EMBASE, 167 references in CINAHL, 120 references in PsycINFO, 249 references in ISI Web of Science, 118 references in OTseeker, and 48 references in PEDro. After removing duplicates, 1427 references remained.
The titles and abstracts were scrutinized and assessed by two reviewer authors, and when information necessary for inclusion was lacking, the full‐text articles were read. The full text of 26 articles was obtained. Of these, nine articles were included (see Characteristics of included studies). Handsearching the reference lists of included studies identified three additional references to be scrutinised by full‐text; one of them was included (Hedge 1999). Contacts were made with eight experts in the field, but they did not generate additional studies. Therefore, a total of ten studies were included.
Included studies
Participants and type of jobs
The total number of participants in the ten included studies was 4179. In one study, one of the intervention arms was physical activity (Horneij 2001), and was not included in the analyses because it met the exclusion criteria for physical exercises. In another study, one of the control groups was not randomised, so this group was also excluded from the review (Morken 2002a). When subtracting these participants (90 and 1344 respectively), the remaining number of participants in the included studies became 2745.
Table 9 gives an overview of the characteristics of the included studies. Seven of the studies dealt mainly with computer workers (Bernaards 2007; Fostervold 2006; Hedge 1999; Kamwendo 1991; Ketola 2002; Voerman 2007; van den Heuvel 2003), but they had different type of jobs: social security workers, secretaries, technicians, engineers, drafts people, and architects. One of these studies dealt with office workers who were medical secretaries, but the trial was performed before computers were a common work tool (Kamwendo 1991). The dominant gender varied according to type of work. In the aluminium industry, the participants were 84% male (Morken 2002a), and in the study in hospitals and municipal home‐care, the participants were all female (Horneij 2001). In the remaining studies, gender was more equally distributed.
Table 2.
Descriptions of included studies
| Study | Country | Region | Branches | Type of workers | Work status and sickness absence | Basis for inclusion |
| Bernaards 2007 | The Netherlands | Different regions | Head offices of seven companies | Computer workers | Working mean 4 1/2 days/week. Sickness absence: working at least 50% of total working time (inclusion criteria), sick leave not reported at baseline, or later | 1 |
| Fostervold 2006 | Norway | Oslo | National Insurance Office | Computer workers | Working between 70‐100% av normal working hours. Sickness Absence: Not reported | 2 |
| Haukka 2008 | Finland | Four large cities | Schools, nursery, nursing homes | Kitchen workers; service managers, chefs, cooks, kitchen aids | Working > 6 hours a day. Sickness absence: Between 16‐19% had MSD‐related sick leave at 3 month follow‐up | 2 |
| Hedge 1999 | US | Phoenix | Large office building | Computer workers | Full time workers. Sickness absence not reported. | 2 |
| Horneij 2001 | Sweden | A medium sized city | Homebased care | Nurising aids and assistant nurses | 25% working full time / 75% 50‐94%. 13% had been on sick leave the preceding 12 months, but not reported during the study | 2 |
| Kamwendo 1991 | Sweden | Not known | Hospital | Medical secretaries | Working 73% full time, e.g. 40 h/w, 27% < 30 h/w. Sick absence: Almost nothing 6 months before and after the program. | 1 |
| Ketola 2002 | Finland | One medium sized city in Southern Sweden | Administrational units | Computer‐/ VDU‐workers; secretaries, technicians, engineers, draft persons | Working status: Not reported. Sick absence status: Not reported. | 1 |
| Morken 2002a | Norway | Not known | Eight aluminium plants | Operators (67%), office workers (20%), managers (N=8%) | Work status: Not reported. Sickness absence: All participants are assumed working, not being sick listed | 2 |
| van den Heuvel 2003 | The Netherlands | Not known | Social security insurance offices (N=22) | Computer workers | Working at least four days a week. Sick absence: 6,3‐9,5% of participants were sick listed before, and 3.8‐6.2% after intervention. | 1 |
| Voerman 2007 | The Netherlands and Sweden | Area of Enschede (the Netherlands) and area of Goteborg (Sweden) | Recruitment and health care | Job counsellors, medical secretaries | Working > 20 hours a week. Sick absence status: Not reported | 1 |
1= inclusion criteria = all participants must have neck pain. 2= inclusion criteria = each participant did not have to have neck pain, but > 50% of the participants had neck pain at baseline
Eight of the articles reported prevalence of neck pain at baseline, which varied from 54% to 90%. One study reported a 54% to 61% prevalence of neck pain during the preceding year (Horneij 2001). One article did not report neck prevalence, but according to information from the author, the cumulative prevalence of neck pain in the past week was 100% (van den Heuvel 2003). None of the studies had sickness absence as an inclusion criterion. In all studies, participants were assumed to be working full‐ or part‐time; however, status on sickness absence was not reported.
The interventions
Altogether, six types of intervention combinations were used in six studies. These where: one four‐component combination (Haukka 2008), one three‐component combination (Morken 2002a), and four different two‐component combinations (Bernaards 2007; Kamwendo 1991; Ketola 2002; Voerman 2007). Five studies provided single component workplace interventions: mental health education (Horneij 2001), physical education, relaxation and breaks (Kamwendo 1991; van den Heuvel 2003), and physical environmental modifications (Fostervold 2006; Hedge 1999). Table 8 gives an overview of the interventions in the ten included studies using the authors` own terms mapped onto uniform terminology of the ICF (WHO 2001).
Three types of interventions targeting the Body Functions domain were examined in the included studies; education for mental health, education for physical health and relaxation breaks. The last two were combined into one group (Table 8), as they both targeted musculoskeletal body functions.The mental health education interventions were aimed at behavioural change and coping with high work demands. Interventions targeting the Activity domain were seen less often. These interventions were described as modifying work tasks, work load, work techniques, work positions, and work hours. They were defined during group meetings or workplace visits. Interventions targeting the Environmental domain modified the physical environment. These were often individually‐tailored interventions following an assessment during a workplace visit or a group session that identified individual needs. Sometimes they were also given to all employees (for example, downward tilted computer keyboards or screen angle modifications). In most cases, several adjustments and alterations of the existing furniture and work equipment were provided. Education for physical health, relaxation, breaks and physical modifications to the environment were the most often examined interventions in the included studies. No interventions targeted modifications of social or attitudinal environments, participation or personal factors domains. These interventions were given separately, or provided as different combinations of intervention programs.
The control groups
In seven studies, the control group received no intervention (Bernaards 2007; Haukka 2008; Hedge 1999; Horneij 2001; Kamwendo 1991; Ketola 2002; Morken 2002a). However, in one of these studies, an information leaflet was given (Ketola 2002). In the analyses, this was regarded as no intervention. In another study, the control group received ergonomic adjustments of the workplace and received a booklet (van den Heuvel 2003). This was regarded as usual care. Finally, three studies compared two workplace interventions (Fostervold 2006; Hedge 1999, Voerman 2007).
The comparisons included in the studies varied to a large extent. Several studies compared two intervention groups to one control group (Bernaards 2007; Horneij 2001; Kamwendo 1991; Ketola 2002; van den Heuvel 2003). One of these studies (Horneij 2001) had a control group with no intervention and another intervention arm that provided an individual physical training program, which was excluded from further analysis in this review, according to our exclusion criteria. One study (Morken 2002a) had three intervention groups providing the same interventions, but to different participants; e.g. in two of the groups the supervisors and/or managers also participated. This study had two control groups, but one of the control groups was not randomised and was excluded from the review.
Outcomes
Outcome measures and their timing are described in Table 10. All ten studies reported pain severity or pain prevalence, while only three studies measured sickness absence. However, data were available for further analysis (after contacting the authors) for only seven of them; seven on pain and only one on sickness absence. No studies reported harms or adverse effects.
Table 3.
Descriptions of outcomes in included studies
|
Included studies author (Year) |
Outcome group | Relevant outcome reported | Short‐term | Intermediate‐term | Long‐term |
| Bernaards 2007 | Pain severity |
average pain last 4 weeks | 6m | 12m | |
| current pain1 | 6m | 12m | |||
| worst pain last 4 weeks | 6m | 12m2 | |||
| Functional or disability status | prevalence recovered | 6m | 12m | ||
| prevalence disabled | 6m | 12m | |||
| Pain severity | 0, 1‐2, 3‐6 months without symptoms | 6m | 12m3 | ||
| Fostervold 2006 | Pain severity | discomfort in neck/shoulder | 12m | ||
| Haukka 2008 | Pain severity | prevalence of neck pain | 3m | 6m,9m | 12m,15m, 18m,21m,24m |
| Well being | prevalence reporting "much stress" | pi4 | 12m | ||
| Work absenteeism | prevalence of MS‐sick leave past 3 months | 3m | 6m5, 9m | 12m,15m, 18m, 21m, 24m | |
| Hedge 1999 | Pain severity | prevalence of neck pain | 3w | ||
| Ketola 2002 | Pain severity | MSD discomfort in neck1 | 2m6 | 10m | |
| Morken 2002a | Pain severity | MSD discomfort in neck last 12 months | 16m | ||
| Horneij 2001 | Pain severity | Change in interference due to neck‐shoulder pain previous month | 12m, 18m | ||
| Pain severity | Change in pain drawing, neck‐shoulder previous month | 12m |
Notes: Data for analysis of intervention effects were available for seven out of ten studies. Abbreviations: w = weeks, m = months MS = Musculoskeletal, MSD = Musculoskeletal disorders, pi = post intervention. 1These outcomes were pooled (meta‐analysis), 2Significance favours control vs. intervention 2 (P < 0.00001), 31 to 2 month without symptoms: Significance favours experimental, both intervention 1 (P = 0.05) and intervention 2 (P = 0.05), 4Significance favours controls (P = 0.05), 5Significance favours experimental (P = 0.03) 6Significance favours experimental, intervention I (P = 0.03) and intervention 2 (P = 0.007)
Excluded studies
Eighteen studies were excluded after reading the full text of the articles and receiving unpublished information from the authors. See Characteristics of excluded studies which describes the reason for exclusion.
Risk of bias in included studies
In all studies, the first author was contacted for missing information concerning risk of bias criteria (see Figure 2 for individual risk of bias assessments). Two of the studies were rated as having low risk of bias (Bernaards 2007; Haukka 2008).
Figure 2.
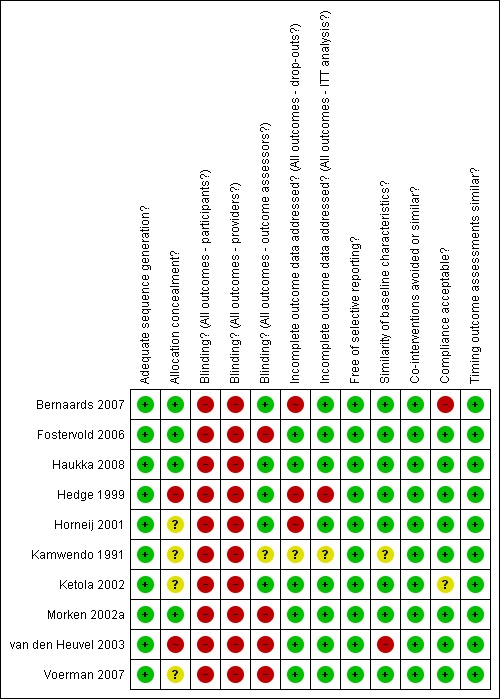
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
All studies had adequate sequence generation as this was an inclusion criterion (only RCT‐design). Only one article reported concealed allocation. When the other authors were asked to clarify this, three authors reported adequately performed allocation concealment, and two authors reported inadequately concealed allocation. In four articles, this issue remains unclear.
Blinding
Lack of blinding of participants and care providers was the most common shortcoming, since this was not possible in any of the studies. When it came to blinding of the outcome assessor, blinding was performed in five studies, not performed in four studies and unclear in one study.
Incomplete outcome data
The dropout rate was acceptable in six studies, not acceptable in three studies, and unclear in one study. Intention‐to‐treat analyses were performed in eight studies, not performed in one study, and unclear in one study.
Selective reporting
All studies appeared to be free from selective outcome reporting.
Other potential sources of bias
Timing of outcomes assessment was similar in all groups within the studies. Co‐interventions were avoided or similar in all studies. Compliance to the intervention was acceptable in eight studies, not acceptable in one study, and unclear in one study. Finally, similarity of baseline characteristics was acceptable in eight studies, unacceptable in one study and unclear in one study.
Effects of interventions
See: Table 1
Data for analysis of intervention effects were available for seven out of ten studies. The results of the three studies that were not analysed due to lack of data, are summarised in the text when relevant, but conclusions are not given. Only between‐group results are presented (showing differences between index and control intervention), even though the authors included within group changes in the original papers. All the results of the relevant outcomes are given in Table 10. The quality of the evidence is presented in Table 11, along with the reasons for downgrading.
Table 4.
Grade of evidence analysis (GRADE)
| GRADE criteria | ||||||
| Study | 1. Limitation of the study design | 2. Inconsistency | 3. Indirectness (inability to generalize) |
4. Imprecision of results (insufficient or imprecise data) |
5. Publication bias (across all studies assessing the outcome) | Conclusion from the GRADE‐ assessment |
| Four‐component workplace intervention versus no intervention | ||||||
| Haukka 2008 | No | No | No | Serious (‐1)1 | Unlikely | Pain: Moderate quality evidence Sickness absence: Moderate quality evidence |
| Three‐component workplace intervention versus no intervention | ||||||
| Morken 2002a | Serious (‐1)3 | No | No | Serious (‐1)5 | Unlikely | Pain: Low quality evidence Sickness absence:No evidence² |
| Two‐component workplace intervention versus no intervention | ||||||
| Bernaards 2007 | No | No | No | Serious (‐1)1 | Unlikely | Pain: Moderate quality evidence Sickness absence: No evidence² |
| Ketola 2002 | Serious (‐1)7 | No | No | Serious (‐1)5 | Unlikely | Pain: Low quality evidence Sickness absence:No evidence |
| Kamwendo 1991 | Very serious (‐2)6 | No | No | Serious (‐1)5,1 | Unlikely | Pain: Very low quality evidence Sickness absence: Very low |
| One‐component workplace intervention versus no intervention | ||||||
| Horneij 2001 | Serious (‐1)4 | No | No | Serious (‐1)5 | Unlikely | Pain: Low quality evidence Sickness absence: No evidence² |
| Kamwendo 1991 | Very serious (‐2)6 | No | No | Serious (‐1)5,1 | Unlikely | Pain: Very low quality evidence Sickness absence: Very low |
| Physical health education, relaxation and breaks versus usual care | ||||||
| van den Heuvel 2003 | Serious (‐1)8 | No | No | Serious (‐1)5,1 | Unlikely | Pain: Low quality evidence Sickness absence: Low quality evidence |
| Activity modifications and physical environmental modifications versus physical health education, relaxation and breaks | ||||||
| Voerman 2007 | Serious (‐1)9 | No | No | Serious (‐1)5 | Unlikely | Pain: Low quality evidence Sickness absence: No evidence² |
| Physical environment modifications versus another physical environment modification | ||||||
| Fostervold 2006 | Serious (‐1)3 | No | No | Serious (‐1)1 | Unlikely | Pain: Low quality evidence Sickness absence:No evidence² |
| Hedge 1999 | Serious (‐1)4 | No | No | Serious (‐1)1 | Unlikely | Pain: Low quality evidence Sickness absence:No evidence² |
1.Total number of events being < 300 and thus have wide confidence intervals and likelihood of random errors, 2. Sickness absence is not an outcome in this study, 3. Lack of blinding of participants, care providers and outcome assessors, 4. Lack of concealed allocation, lack of/unclear blinding of participants and care provider, and large loss to follow up, 5. Total number of participants being < 400 and thus have wide confidence intervals and likelihood of random errors, 6. Unclear allocation concealment, lack of blinding of participants and care provider, unclear blinding of outcome assessor, and unclear addressing of incomplete outcome data, 7. Unclear allocation concealment and lack of blinding of participants and care provider, 8. Lack of concealed allocation, and lack of blinding of participants, care provider and outcome assessor, 9. Unclear allocation concealment and lack of blinding of participants, care provider and outcome assessor.
1. Workplace intervention versus no interventions
Quantiative results
Only two of the studies comparing workplace interventions with no interventions had comparable type of workers (computer/VDU workers) (Bernaards 2007; Ketola 2002), follow‐up time, and outcome of pain severity, and therefore, were pooled. The meta‐analysis (Table 1) revealed no significant differences in pain prevalence in the long‐term (MD ‐0.12, 95% CI ‐0.36 to 0.12).
Conclusion: There is low quality evidence (2 trials, 267 people), that there is little or no difference between a two‐component workplace intervention and no intervention on pain severity at long‐term follow‐up.
Qualitative descriptive results
The narrative analysis using ICF revealed different types of four‐, three‐, and two components workplace interventions compared to no interventions.
a. Four‐component workplace intervention versus no intervention
ai. Mental health education, physical health education, relaxation & breaks, activity modifications, and physical environmental modifications
One study (Haukka 2008) assessed the effect of combining four intervention components; (1) mental health education, (2) physical health education, relaxation and breaks, (3) activity modifications, and (4) physical environmental modifications, compared to no interventions.The program was a so‐called 'participatory ergonomic intervention' program. There were no significant differences in pain prevalence in the short‐term (OR 1.43; 95% CI 0.95 to 2.14), intermediate‐term (OR 0.80, 95% CI 0.52 to 1.21) or long‐term (OR 1.13, 95% CI 0.69 to 1.87). There was a significant difference in sick leave (Figure 3) in the intermediate‐term (OR 0.56, 95% CI 0.33 to 0.95), but not in the short‐term (OR 0.83, 95% CI 0.52 to 1.34) or long‐term (OR 1.28, 95% CI 0.73 to 2.26). These results on sick leave were not presented in the included paper, but found by the review team after analysing the sickness absence data we received from the authors.
Figure 3.
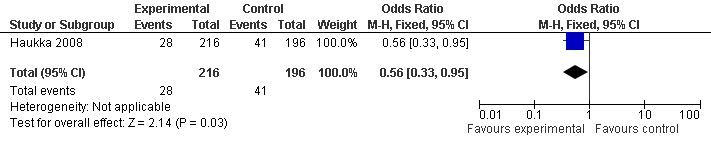
Forest plot of comparison: Four component workplace intervention versus no intervention. Intermediate‐term effect: Prevalence of musculoskeletal sick leave past 3 months
Conclusion: There is moderate quality evidence (1 trial, 295 people) that there were no significant differences in short‐, intermediate‐ or long‐term follow‐up for the prevalence of neck pain between those who received this four‐component workplace intervention and those who received no interventions. There is moderate quality evidence (1 trial, 415 people) that those who received this workplace intervention were significantly less likely to be sick‐listed in the intermediate‐term then those who received no interventions. The differences were not significant at short‐term and long‐term follow‐up.
b. Three‐component workplace intervention versus no interventions
bi. Physical health education, relaxation & breaks, activity modifications, and physical environmental modifications
One study evaluated a three‐component workplace intervention (Morken 2002a) that combined (1) physical health education, relaxation and breaks, (2) activity modifications, and (3) physical environmental modifications versus no interventions. This was a one‐year group training program for three groups; employees only, employees and supervisors, supervisors only. None of the between‐group differences in pain prevalence were significant between groups (employees only: MD 0.01, 95% CI ‐0.21 to 0.23, employees and supervisors: MD 0.12, 95% CI ‐0.11 to 0.35, supervisors only; MD ‐0.04, 95% CI ‐0.24 to 0.16) on long term follow‐up.
Conclusion: There is low quality evidence (1 trial, three arms; 601, 599 and 629 people) that there is no significant difference in pain severity between the group who received the three‐component intervention and those who received no intervention.There is no evidence on sickness absence.
c. Two‐component workplace interventions versus no intervention
Three studies evaluated different two‐component intervention programs.
c1. Mental health education, and physical health education, relaxation and breaks
One of the studies (Bernaards 2007) combined (1) mental health education, with (2) physical health education, relaxation and breaks, and compared them to no intervention. The study had two arms; (i) a work style group, and (ii) a work style plus lifestyle physical activity group, both with the same intervention combination. There were no significant differences in pain severity in the intermediate‐term (arm 1: MD 0.30, 95% CI ‐0.26 to 0.86, arm 2: MD 0.20, 95% CI ‐0.37 to 0.77) or long‐term (arm 1: MD ‐0.20, 95% CI ‐0.84 to 0.44, arm 2: MD ‐0.10, 95% CI ‐0.73 to 0.53). For the outcome ''time without symptoms', those with one to two months without symptoms at the assessment time had significant differences at long‐term (arm 1: OR 2.01, 95% CI 1.00 to 4.03, arm 2: OR 2.03, 95% CI 1.01 to 4.08), but the differences were smaller and not significant at intermediate‐term (arm 1: OR 1.32, 95% CI 0.73 to 2.41, arm 2: OR 1.18, 95% CI 0.64 to 2.19). For the rest of the outcomes measured in this study, the results showed small or no differences between the experimental and control groups, at both intermediate‐term and long‐term.
Conclusion: There is moderate quality evidence that there is no significant difference in current neck pain, measured at intermediate‐term (1 trial, two arms; 266 and 259 people) or at long‐term follow‐up (1 study, two arms; 210 and 209 people). There is conflicting evidence (1 study, two arms; 264 and 257) for time without symptoms (no time, one to two months, three to six months), at both intermediate‐ and long term follow‐up. There is no evidence on sickness absence for this type of intervention.
c2. Physical health education, relaxation & breaks, and physical environment modifications
The second study (Ketola 2002) combined (1) physical health education, relaxation and breaks with (2) physical environment modifications, and compared them to no intervention. The study had two intervention arms: (i) intensive ergonomics, and (ii) ergonomic education, both with the same intervention combination. The study revealed significant differences in pain severity for both intervention arms in the short‐term (arm 1: MD ‐0.60, 95% CI ‐1.15 to ‐0.05; Figure 4, arm 2: MD ‐0.60, 955 CI ‐1.04 to ‐0.16; Figure 5), but not at intermediate‐term follow‐up (arm 1: MD ‐0.30, 95% CI ‐0.85 to 0.25; and arm 2: MD ‐0.25‐0.77 to 0.28).
Figure 4.
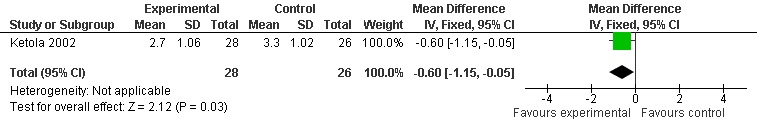
Forest plot of comparison: Two component workplace intervention versus no intervention. Short‐term effect. Outcome:Musculoskeletal discomfort in the neck (Arm: Intensive ergonomic).
Figure 5.
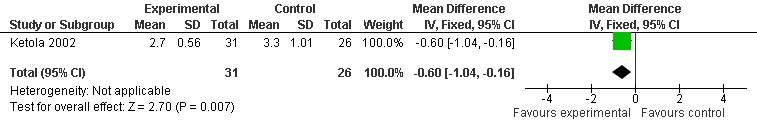
Forest plot of comparison: Two component workplace intervention versus no intervention. Short‐term effect: Outcome: Musculoskeletal discomfort in the neck (Arm: Ergonomic education)
Conclusion: There is low quality evidence (1 trial ‐ two arms; 54 and 57 people) that a two‐component workplace intervention is more effective than no intervention in pain severity in the short‐term. However, there were no significant differences at the intermediate‐term (1 study, 54 and 57 people).There is no evidence on sickness absence for this type of intervention.
c3. Mental health education, and physical environment modifications
The third study (Kamwendo 1991) contained a two‐component intervention program consisting of (1) mental health education, and (2) physical environment modifications versus no interventions. The study had two arms. According to the article reporting this study (Kamwendo 1991), they found no significant differences between the interventions and control group on pain and sick leave. As we did not have statistics from this study, no conclusion has been drawn.
d. One component workplace interventions versus no intervention
di. Mental health education
One study (Horneij 2001) assessed the effect of mental health education versus no intervention on pain prevalence. In the long‐term, no significant differences in pain severity (MD 7.70, 95% CI ‐13.73 to 29.13) were found.
Conclusion: There is low quality evidence from one trial (43 people) that there is no significant difference in neck pain between those receiving workplace interventions and those receiving no interventions at long‐term follow‐up.
dii. Physical health education, relaxation and breaks
One study (Kamwendo 1991) assessed the effect of physical health education and/or relaxation and breaks versus no interventions on pain prevalence or pain severity. According to the authors, their study revealed no significant differences between the intervention and control group on pain and sick leave. As we did not have statistics from this study, no conclusion has been drawn.
2. Workplace intervention versus usual care
Quantitative results
It was not possible to pool the results for this comparison, due to lack of statistics.
Qualitative descriptive results
a. Physical health education, relaxation and breaks versus usual care
One study (van den Heuvel 2003) assessed the effect of (i) physical health education, (ii) relaxation and breaks compared to usual care. Arm I only included rest breaks, while arm II included rest breaks with exercises. Data were not available for further analysis of intervention effects, but the authors reported that more subjects in the intervention groups than in the control group reported change in their complaints (55% versus 34%) at short‐term follow‐up, but no differences were seen in self‐reported sick leave. As we did not have statistics from this study, no conclusion has been drawn.
3. Comparison of two or more workplace interventions
Quantiative results
It was not possible to pool the results for this comparison, due to lack of statistics, and different follow‐up times.
Qualitative descriptive results
a. Activity modifications and physical environmental modifications versus physical health education, relaxation and breaks
One study (Voerman 2007) assessed the effect of two‐component combinations, containing activity modifications and physical environmental modifications versus physical health education, relaxation and breaks (ambulant myo‐feedback training and ergonomic counselling). The authors reported that none of the between‐group differences for pain prevalence or disability were significant. As we did not have statistics from this study, no conclusion has been drawn.
b. Physical environment modifications versus another physical environment modification
Two studies (Fostervold 2006; Hedge 1999) assessed the effect of one physical environment modification versus another physical environment modification (computer equipment adjustments of screen and table) on pain severity. Both studies focused on computer workers. The results from these two studies were not pooled because they used different follow‐up times. There were small but not significant differences between the two groups in pain prevalence at short‐term (Hedge 1999: OR 0.47, 95% CI 0.12 to 1.76) and long‐term follow‐up (Fostervold 2006: OR 0.48, 95% CI 0.22 to1.02) (Figure 6).
Figure 6.
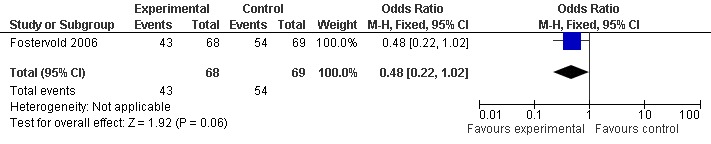
Forest plot of comparison: Physical environment modification versus another physical environment modification. Long‐term effect: Prevalence of discomfort in neck/shoulder (Computer screen angle, high vs. low line‐of‐sight)
Conclusion: There is low quality evidence that there is no significant difference at short‐term follow‐up (1 trial; 37 people) or at long‐term follow‐up (1 study, 137 people) in the prevalence of neck pain for those who received one workplace intervention versus those who received another workplace intervention.
Discussion
The objective of this review was to determine the effectiveness of workplace interventions in working age adults with neck pain compared to no interventions, usual care or other workplace interventions.
Summary of main results
The search strategy identified 1995 references. Ten RCTs were included (2745 workers). Two studies were rated as having low risk of bias. Most trials (N = 8) examined office workers. Only a few workers were sick‐listed. Thus, workplace interventions were seldom aimed at return‐to‐work. For the most part, there was low quality evidence (10 trials, 2745 workers) showing no significant differences between workplace interventions and no interventions for pain prevalence or pain severity. None of the significant results for pain, in favour of workplace interventions, were sustained across different follow‐up times. Only one study, with a low risk of bias, had data available on sickness absence, and provided moderate quality evidence (1 study, 415 workers) that a four‐component workplace intervention was significantly more effective in reducing sick leave in the intermediate‐term, but not in the short‐ and long‐term. The negative results on sickness absence might be because only a small proportion of the workers included in the study were sick‐listed.
Overall completeness and applicability of evidence
An overall result from this Cochrane review is a message of: ".. low quality evidence that there are no significant differences in the reduction of pain and sickness absence between workers with neck pain receiving workplace interventions versus those who did not receive any interventions". How should this type of result be understood and applied? Does this document the ineffectiveness of workplace interventions, or is it a message about not yet having reliable evidence on workplace interventions for this group? To discuss this, we need to divide the message into two parts. First; "low quality evidence" should be regarded as inconclusive evidence, and generate a demand for high quality trials in which adequate sequence generation, allocation concealment and assessor blinding are performed, and also where more participants or events are included in the trials to reduce the wide confidence intervals and thereby the risk of random error. The problem of low power was also a consequence of an inability to pool data across trials, due to diversity in interventions, outcomes, and follow‐up times. The second part of the message: "there are no significant differences" opens up more interpretations. First, are the content, dose and expected responses of the workplace interventions in these ten studies adequate for reducing neck pain and sickness absence? Are the outcome measures relevant to catch the present effect, or are the relevant outcome measures used? Is the timing of the outcome assessment relevant and in accordance with expected effects? This will be discussed below.
The target of most of the interventions in the included trials was musculoskeletal body functions, with some trying to modify the physical environment. However, the specific content, duration, intensity and methodology of the interventions varied considerably. Some were single interventions, others complex combinations. There were also differences in whether the interventions were individually adjusted or standardised and/or delivered in groups. In all studies, workplace adjustment strategies were to some extend individually tailored, based either on existing knowledge or on experimental ideas. However, in most cases, educational approaches were used. It could be questioned whether education alone is enough to change behaviour. Many of the interventions in the studies did not seem to be based on cumulative traditions. Some of the tested interventions seemed to be based on hypotheses and models that were developed on an ad hoc basis, rather than on evidence that had already been published. In addition, few multi‐targeted interventions were conceptualised. The use of WHO's ICF (WHO 2001) could have contributed to a conceptual frame of reference based on common terminology.
There seems to be quite a range of interventions, from studies testing a single modification to the physical environment to those having four‐component interventions targeting mental and physical body functions, activities and environmental changes. Hence, when trying to conduct analyses regarding the effect of interventions on specific outcomes, most of the results were based on single studies. When the number of trials increases in future updates of this review, meta‐analysis will more likely be an option.
This review shows infrequent effects in favour of the experimental group, on a few outcomes, in only some studies. However, a systematic pattern was neither found across studies nor over time, i.e. a significant effect found at one point in time was non‐existent at another follow‐up. This may have to do with a number of factors. The first is that studies that look at reasonably effective interventions have not yet been carried out. Another reason may be that the interventions examined in the studies included in this review were not appropriate for the goal to alleviate neck pain. This involves the methodology of interventions, intensity or duration of the means, but it may also have to do with the fact that at least some of the neck pain may have different causes than work postures or physical environmental factors, as confirmed in several studies documenting that risk factors for neck pain are also psychosocial (Aas 2011; Ariens 2000; Côté 2008; Linton 2000 ). A few of these included studies have such components, but they seem to be less dominant than the ones focusing on the physical exposures. Thus, the fact that the interventions take place during a part of a work day within a small fraction of a person's life reduces the efficiency and the probable effect. Another reason might be due to the chosen follow‐up times. With a short follow‐up time, the effect of an intervention may be limited, since it usually takes time for affected musculoskeletal systems to recover. With a long follow‐up time, the problem is that a number of other influences may occur during the follow‐up time, which reduces the ability to determine if the intervention was the main or only cause of the outcome. The lack of interventions targeting the ICF‐domains "attitudinal‐ and social environment" may also have led to the lack of effectiveness. Employers' involvement in workplace intervention programs has gradually become more important (Lambeek 2010; Aas 2008), even though this is not new in the return‐to‐work literature (Franche 2005; Loisel 2001; Franche 2005). The lack of clinical interventions, such as cognitive therapy, combined with workplace interventions, diagnostic assessments followed by the reassurance that there was no harm in being active, and the active involvement of stakeholders might also be plausible causes for these inconclusive results. By using the psychosocial flag framework for identifying psychosocial obstacles for musculoskeletal disorders such as neck pain, the awareness of the wide spectrum of risk factors for neck pain could be strengthened in the future. Most of the included studies in this review did not included employer involvement in their intervention. Finally, another plausible reason might be that these were just chance findings, because most studies analysed several outcome measures at several follow‐up moments.
The measurement of outcomes varied considerably between the ten studies. Pain, musculoskeletal discomfort, prevalence of disability, periods without symptoms or similar concepts were used in the different studies, along with sick leave and prevalence of persons recovered. No dominant or standardised methodology to measure neck pain/discomfort/symptoms and sickness absence seems to exist, and different scales for measuring subjective pain were used in the studies. The follow‐up time varied considerably between the studies. No study discussed whether the interventions were expected to have long‐term, intermediate‐ or short‐ term effects. The follow‐up times seemed to be determined more on research procedures than on ideas about the time it would take to get effects of the interventions on pain, discomfort or sick leave.
Quality of the evidence
The GRADE‐analyses revealed that these studies provided low quality evidence, which means that further research is very likely to have an important impact on the confidence in the estimate of effect, and will likely change the estimate.
As expected, blinding is a challenge in this type of research, and with the nature of these interventions, it is not possible to blind healthcare providers or participants. One cannot avoid that their expectations may influence the effect of the interventions. However, there should not be any obstacle prohibiting blinding of the outcome assessor. Nevertheless, less than 50% of the studies provided blinded outcome evaluation. In addition, incomplete outcome data, low compliance and differences in baseline characteristics of the participants introduce a high risk of bias in several of the included studies. The number of participants in each intervention was low in several of the studies. In addition, the diversity of settings, participants and interventions hampered pooling of data and the overall robustness of the evidence gained from results that are repeated across studies.
In addition, the diversity of primary studies regarding interventions and outcomes is a typical challenge for conducting meta‐analysis on workplace interventions in general (Conn 2009).
The significant result on sickness absence is promising, as the study had low risk of bias (Haukka 2008), and also used a more broad targeted four‐component intervention, built on participatory ergonomics methodology, with high involvement of stakeholders. Still, these results were from a study of kitchen workers, while most workplace interventions targeting neck pain are for computer workers. This may reduce the clinical relevance and generalisability of this result.
Potential biases in the review process
There is no universally accepted definition of workplace interventions. In the present review, the main prerequisite was that the intervention was conducted at the workplace. Of course, interventions that aim to modify physical, or social and attitudinal factors in the work environment cannot be applied elsewhere. However, modification of personal factors, like exercise and other health promotion activities, may be as feasibly conducted outside the workplace. Comparison of their effectiveness across the setting , that is, within or outside the workplace, has not been applied as far as we know. Another potential bias might be caused by our inclusion criteria of studies where at least 50% of the participants had neck pain at baseline, in both the intervention and control groups. Would a review that only included studies where all or 75% of the participants had neck pain at baseline give other results? Even though some of these studies only included participants with neck pain, not all had pain at baseline, due to the fluctuating nature of neck pain.
Agreements and disagreements with other studies or reviews
The results of the symptom outcomes will be discussed first. In this review, we tried to find relief of neck pain, among workers with such pain. The prognosis for neck pain, and the effects of treatment are generally less optimistic than for low‐back pain (Borghouts 1998; Carroll 2008; Côté 2008; Hill 2004). However, several risk factors related to intensive computer work, like keyboard position with small elbow angles, inadequate mouse position, high screen placement and chairs that do not have arm rest have been identified (Ariens 2000). Psychosocial factors such as high demand, low control and low support at work also influence the incidence of health problems in workplace settings (Lau 2008). Thus, one could hope that intervening against these factors would reduce neck pain. The present review indicates no strong evidence for mostly educational workplace interventions aimed at reducing these identified risk factors. However, the results should be interpreted with caution because of the small number of studies and participants included in the analysis, and because only two of the ten studies had a low risk of bias. A review conducted at the Institute for Work & Health in Canada among computer users found moderate evidence that workstation adjustments, and rest breaks together with exercise had no impact on pain symptoms, while alternative pointing devises had a positive impact (van Eerd 2006). For the rest of the different ergonomic interventions in this review (van Eerd 2006), there were inconsistent findings, or insufficient evidence. Another Cochrane review focusing on several types of MSD also found that workplace interventions failed to reduce symptoms (van Oostrom 2009). We could question whether we experience an implementation challenge with using the risk‐literature directly when designing and implementing interventions in complex contexts such as the workplace. According to the PARiSH framework, successful implementation is a function of the nature and type of evidence, the qualities of the context in which the evidence is being introduced, and the way the implementation is facilitated (Kitson 2008). If the context is not ready or actively involved, we could question if workplace interventions alone are likely to result in a sustainable effect. A literature review on health effects of workplace interventions revealed a lack of reporting on how the interventions actually were implemented (Egan 2009). This might be crucial information in the future.
When discussing the results on sickness absence, it is important to have in mind that the effort of reducing sick leave was not a high priority in any of the included studies, and that few of the participants in the studies were actually sick‐listed. To expect to reduce a phenomenon (e.g. sickness absence) that almost does not exist, seems demanding. Still, one of the included studies revealed a significant finding on sickness absence. Studies focusing on workplace interventions targeting sick‐listed workers, often call these 'RTW‐workplace interventions'. Is this the same type of workplace intervention provided in the studies in this review, but with another aim? RTW‐workplace interventions have been found to significantly reduce sick leave (Franche 2005; Lambeek 2010; van Oostrom 2009,). In a review of 10 studies among sick‐listed employees with MSD, Franche et al (Franche 2005) found strong evidence that offers of work accomodation and early contact between healthcare providers and the workplace, and moderate evidence that early contact with the worker by the workplace, ergonomic work site visits, and the presence of a RTW‐coordinator significantly improved RTW for workers with MSD and other pain‐related conditions. The determinants of sick leave are complex. Any attempt to understand them must take into account interactions between individual and environmental factors and how tasks are executed, over a large variety of occupations. Therefore, effective interventions may represent a combination of processes where the workers, employers, health professionals, and employment system must interact (Anema 2007). With the growing evidence‐base supporting RTW‐workplace interventions, should we question if these two types of workplace interventions should interact more, when designing efficient workplace interventions for the future? Still, many guidelines for MSD only include interventions aiming at symptom reduction, without offering recommendations for workplace interventions. Implementing effective organisational and collaborative workplace interventions for those who remain at work and in pain, will be challenging but necessary for the future.
Authors' conclusions
This review neither supports nor refutes any specific workplace intervention.Therefore, whether a specific workplace intervention is likely to reduce pain or not is still unknown. Based on the current literature, there is low quality evidence that there is little or no difference in pain relief for workers with neck pain who do or do not receive workplace interventions and moderate evidence from only one trial that multi‐component workplace interventions might be effective in reducing sick leave in the intermediate‐term, although the effect is not sustained over time. Further research is very likely to have an important impact on our confidence in the estimate of effect, and is likely to change the estimate.
The large variations in target groups, interventions, follow‐ups and outcome measurements restricted pooling of data across studies. Hence, there is an urgent need for randomised controlled trials with well‐designed multi‐dimensional interventions, tailored towards neck pain and conducted at the workplace. We recommend that researchers use the ICF terminology to ensure that all relevant dimensions of health and functioning are addressed in further trials. In addition, the two main outcomes, pain relief and reduced sickness absence/return‐to‐work, would benefit from standardisation, and should always be included in this types of study. Hence, there is an urgent need for randomised controlled trials with well designed intervention components tailored towards each individual and the multifactorial etiology of neck pain.
Acknowledgements
A warm thanks goes to colleagues who contributed with smaller amounts of work, mainly in the inclusion/exclusion process and assessment process; Brit Hege Skaugen (BHS), Merete Labriola (ML) and Kjersti Lunde Ellingsen (KLE). Besides the important help from the Cochrane Back Review Group, especially Victoria Pennick, the review authors would like to thank Andrew D. Oxman at the Norwegian Knowledge Centre for Health Services and Jos Verbeek at the Finnish Institute of Occupational Health for helpful advice; our Librarians Marit Johansen, at the Norwegian Directorate for the Health and Social Affairs, Oslo, Susanne Tidblom‐Kjellberger, Librarian at the Nordic School of Public Health, Gotenborg, and Rachel Couban at the Cochrane Back Review Group for valuable advice on search strategies and search performance; and Allison Kelly administrative Editorial Assistant at the Cochrane Back Review Group, Institute for Work & Health for graphic adjustments of the figures.
Appendices
Appendix 1. CENTRAL Search Strategy
#1 MeSH descriptor Neck Pain explode all trees #2 neck pain #3 (#1 OR #2) #4 MeSH descriptor Workplace explode all trees #5 workplace #6 worksite #7 MeSH descriptor Sick Leave explode all trees #8 sick leave #9 (#4 OR #5 OR #6 OR #7 OR #8)
Appendix 2. MEDLINE Search Strategy
1 randomized controlled trial.pt. 2 controlled clinical trial.pt. 3 randomized.ab. 4 placebo.ab,ti. 5 drug therapy.fs. 6 randomly.ab,ti. 7 trial.ab,ti. 8 groups.ab,ti. 9 or/1‐8 10 (animals not (humans and animals)).sh. 11 9 not 10 12 neck muscles.sh. 13 exp Neck/ 14 exp neck pain/ 15 whiplash injuries.sh. 16 neck.ti,ab. 17 exp Musculoskeletal System/ 18 musculoskeletal disorder$.mp. 19 or/12‐18 20 11 and 19 21 exp Workplace/ 22 exp Sick Leave/ 23 exp Work/ 24 or/21‐23 25 24 and 20
Appendix 3. EMBASE Search Strategy
1 Clinical Article/ 2 exp Clinical Study/ 3 Clinical Trial/ 4 Controlled Study/ 5 Randomized Controlled Trial/ 6 Major Clinical Study/ 7 Double Blind Procedure/ 8 Multicenter Study/ 9 Single Blind Procedure/ 10 Phase 3 Clinical Trial/ 11 Phase 4 Clinical Trial/ 12 crossover procedure/ 13 placebo/ 14 or/1‐13 15 allocat$.mp. 16 assign$.mp. 17 blind$.mp. 18 (clinic$ adj25 (study or trial)).mp. 19 compar$.mp. 20 control$.mp. 21 cross?over.mp. 22 factorial$.mp. 23 follow?up.mp. 24 placebo$.mp. 25 prospectiv$.mp. 26 random$.mp. 27 ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp. 28 trial.mp. 29 (versus or vs).mp. 30 or/15‐29 31 14 and 30 32 human/ 33 Nonhuman/ 34 exp ANIMAL/ 35 Animal Experiment/ 36 33 or 34 or 35 37 32 not 36 38 31 not 36 39 37 and 38 40 38 or 39 41 neck muscles.mp. 42 exp NECK/ 43 whiplash injuries.mp. 44 neck.mp. 45 exp neck pain/ 46 exp neck muscle/ 47 musculoskeletal disorder$.mp. 48 or/41‐47 49 40 and 48 50 exp workplace/ 51 worksite.mp. 52 sick leave.mp. or exp medical leave/ 53 or/50‐52 54 53 and 49
Appendix 4. CINAHL Search Strategy
S37 S31 and S36 S36 S32 or S33 or S34 or S35 S35 (MH "Sick Leave") S34 (MH "Work Environment+") S33 "worksite" S32 "workplace" S31 S23 and S30 S30 S24 or S25 or S26 or S27 or S28 or S29 S29 "musculoskeletal disorder*" S28 (MH "Whiplash Injuries") S27 (MH "Cervical Vertebrae") S26 (MH "Neck Pain") S25 (MH "Neck") S24 ("neck muscles") or (MH "Neck Muscles+") S23 S21 not S22 S22 (MH "Animals+") S21 S20 or S19 or S18 or S17 or S16 or S15 or S14 or S13 or S12 or S11 or S10 or S9 or S8 or S7 or S6 or S5 or S4 or S3 or S2 or S1 S20 "volunteer*" S19 prospectiv* S18 "control*" S17 "follow‐up stud*" S16 (MH "Prospective Studies+") S15 (MH "Evaluation Research+") S14 (MH "Comparative Studies") S13 "latin square" S12 (MH "Study Design+") S11 (MH "Random Sample+") S10 "random*" S9 "placebo*" S8 (MH "Placebos") S7 (MH "Placebo Effect") S6 "triple‐blind" S5 "single‐blind" S4 "double‐blind" S3 ""clinical W8 trial"" S2 "randomi?ed controlled trial*" S1 (MH "Clinical Trials+")
Appendix 5. PsycInfo Search Strategy
((KW=(Randomi?ed controlled trial*) OR KW=(clinical trial*) OR KW=(clin* near trail*) OR KW= (sing* near blind*) OR KW=(sing* near mask*) OR (doub* near blind*) OR KW=(doubl* NEAR mask*) OR KW=(trebl* near mask*) OR KW=(trebl* near mask*) OR KW=(tripl* near blind*) OR KW=(tripl* near mask*) OR KW=(placebo*) OR KW=(random*) OR DE=(research design) OR KW=(Latin square) OR KW=(comparative stud*) OR KW=(evaluation stud*) OR KW=(follow up stud*) OR DE=(prospective stud*)OR KW=(control*) OR KW=(prospective*) OR KW=(volunteer*)) AND DE=(neck)) and (KW=(workplace or worksite or (sick leave)))
Appendix 6. ISI Web of Science Search Strategy
# 23 #22 AND #17 # 22 #21 OR #20 OR #19 OR #18 # 21 Topic=(sickness absence) # 20 Topic=(sick leave) # 19 Topic=(worksite) # 18 Topic=(workplace) # 17 #16 AND #12 # 16 #15 OR #14 OR #13 # 15 Topic=(neck* pain) # 14 Topic=(musculosk* disorder*) # 13 Topic=(musculosk* syst*) # 12 #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 # 11 Topic=(prospective stud*) # 10 Topic=(follow up stud*) # 9 Topic=(controlled trial) # 8 Topic=(comparative stud*) # 7 Topic=(research design) # 6 Topic=(controlled clinical trial) # 5 Topic=(random*) # 4 Topic=(placebo*) # 3 Topic=(clinical trial*) # 2 Topic=(double blind*) # 1 Topic=(single blind*)
Appendix 7. OTseeker (Occupational Therapy Systematic review of Evidence)
Keywords: work OR worksite OR workplace Diagnosis/Subdiscipline: Musculoskeletal or connective tissue injuries/ disorders/ procedures Method: Clinical Trial
Appendix 8. PEDro (The Physiotherapy Evidence database)
Abstract & Title: work Body Part: head or neck Subdiscipline: musculoskeletal Method: clinical trial Match all search terms (AND)
Appendix 9. Criteria for risk of bias assessment for RCTs
1. Was the method of randomisation adequate? A random (unpredictable) assignment sequence. Examples of adequate methods are coin toss (for studies with two groups), rolling a dice (for studies with two or more groups), drawing of balls of different colours, drawing of ballots with the study group labels from a dark bag, computer‐generated random sequence, pre‐ordered sealed envelops, sequentially‐ordered vials, telephone call to a central office, and pre‐ordered list of treatment assignments
Examples of inadequate methods are: alternation, birth date, social insurance/security number, date in which they are invited to participate in the study, and hospital registration number
2. Was the treatment allocation concealed? Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient.
Was knowledge of the allocated interventions adequately prevented during the study? 3. Was the patient blinded to the intervention? This item should be scored “yes” if the index and control groups are indistinguishable for the patients or if the success of blinding was tested among the patients and it was successful.
4. Was the care provider blinded to the intervention? This item should be scored “yes” if the index and control groups are indistinguishable for the care providers or if the success of blinding was tested among the care providers and it was successful
5. Was the outcome assessor blinded to the intervention? Adequacy of blinding should be assessed for the primary outcomes. This item should be scored “yes” if the success of blinding was tested among the outcome assessors and it was successful or:
for patient‐reported outcomes in which the patient is the outcome assessor (e.g., pain, disability): the blinding procedure is adequate for outcome assessors if participant blinding is scored “yes”
for outcome criteria assessed during scheduled visit and that supposes a contact between participants and outcome assessors (e.g., clinical examination): the blinding procedure is adequate if patients are blinded, and the treatment or adverse effects of the treatment cannot be noticed during clinical examination
for outcome criteria that do not suppose a contact with participants (e.g., radiography, magnetic resonance imaging): the blinding procedure is adequate if the treatment or adverse effects of the treatment cannot be noticed when assessing the main outcome
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between patients and care providers (e.g., co‐interventions, hospitalisation length, treatment failure), in which the care provider is the outcome assessor: the blinding procedure is adequate for outcome assessors if item “4” is scored “yes”
for outcome criteria that are assessed from data of the medical forms: the blinding procedure is adequate if the treatment or adverse effects of the treatment cannot be noticed on the extracted data
Were incomplete outcome data adequately addressed? 6. Was the drop‐out rate described and acceptable? The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and does not lead to substantial bias a 'yes' is scored. (N.B. these percentages are arbitrary, not supported by literature).
7. Were all randomised participants analysed in the group to which they were allocated? All randomised patients are reported/analysed in the group they were allocated to by randomisation for the most important moments of effect measurement (minus missing values) irrespective of non‐compliance and co‐interventions.
8. Are reports of the study free of suggestion of selective outcome reporting? In order to receive a ‘yes’, the review author determines if all the results from all pre‐specified outcomes have been adequately reported in the published report of the trial. This information is either obtained by comparing the protocol and the report, or in the absence of the protocol, assessing that the published report includes enough information to make this judgment.
Other sources of potential bias: 9. Were the groups similar at baseline regarding the most important prognostic indicators? In order to receive a “yes”, groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms, and value of main outcome measure(s).
10. Were co‐interventions avoided or similar? This item should be scored “yes” if there were no co‐interventions or they were similar between the index and control groups.
11. Was the compliance acceptable in all groups? The reviewer determines if the compliance with the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). For example, physiotherapy treatment is usually administered over several sessions; therefore it is necessary to assess how many sessions each patient attended. For single‐session interventions (for ex: surgery), this item is irrelevant.
12. Was the timing of the outcome assessment similar in all groups? Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments.
Appendix 10. Questions to determine clinical relevance
Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?
Are the interventions and treatment settings described well enough so that you can provide the same for your patients?
Were all clinically relevant outcomes measured and reported?
Is the size of the effect clinically important?
Are the likely treatment benefits worth the potential harms?
Data and analyses
Comparison 1.
Four‐component workplace intervention versus no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term effect: Prevalence of neck pain | 1 | 469 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.95, 2.14] |
| 2 Intermediate‐term effect: Prevalence of neck pain | 1 | 412 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.52, 1.21] |
| 3 Long‐term effect: Prevalence of neck pain | 1 | 295 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.69, 1.87] |
| 4 Short‐term effect: Prevalence of musculoskeletal sick leave past 3 months | 1 | 469 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.52, 1.34] |
| 5 Intermediate‐term effect: Prevalence of musculoskeletal sick leave past 3 months | 1 | 412 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.33, 0.95] |
| 6 Long‐term effect: Prevalence of musculoskeletal sick leave past 3 months | 1 | 295 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.73, 2.26] |
Analysis 1.1.
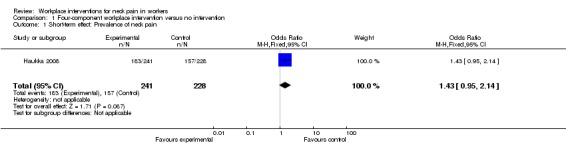
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 1 Short‐term effect: Prevalence of neck pain.
Analysis 1.2.
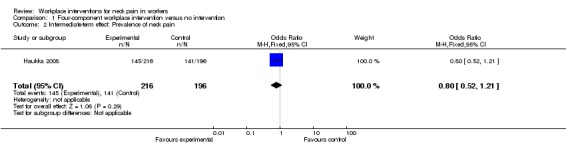
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 2 Intermediate‐term effect: Prevalence of neck pain.
Analysis 1.3.
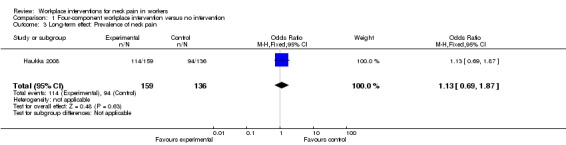
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 3 Long‐term effect: Prevalence of neck pain.
Analysis 1.4.
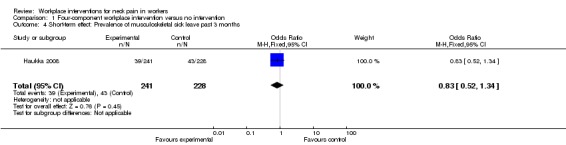
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 4 Short‐term effect: Prevalence of musculoskeletal sick leave past 3 months.
Analysis 1.5.
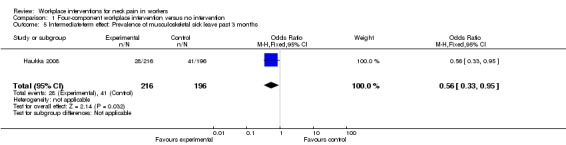
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 5 Intermediate‐term effect: Prevalence of musculoskeletal sick leave past 3 months.
Analysis 1.6.
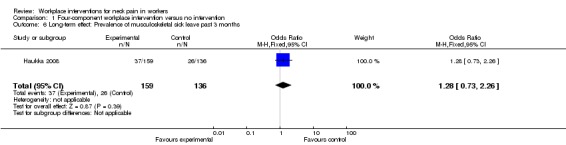
Comparison 1 Four‐component workplace intervention versus no intervention, Outcome 6 Long‐term effect: Prevalence of musculoskeletal sick leave past 3 months.
Comparison 2.
Three‐component workplace intervention versus no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Long‐term effect: Musculoskeletal discomfort (Arm: Operators with supervisors) | 1 | 601 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.11, 0.35] |
| 2 Long‐term effect: Musculoskeletal discomfort (Arm: Operators without supervisors) | 1 | 599 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.21, 0.23] |
| 3 Long‐term effect: Musculoskeletal discomfort (Arm: Managers only) | 1 | 629 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.24, 0.16] |
Analysis 2.1.
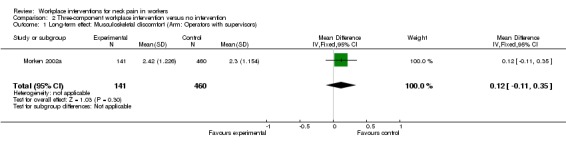
Comparison 2 Three‐component workplace intervention versus no intervention, Outcome 1 Long‐term effect: Musculoskeletal discomfort (Arm: Operators with supervisors).
Analysis 2.2.
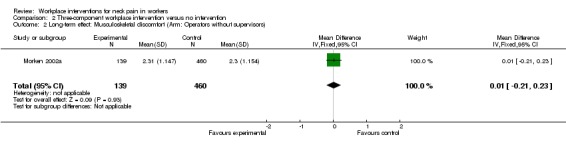
Comparison 2 Three‐component workplace intervention versus no intervention, Outcome 2 Long‐term effect: Musculoskeletal discomfort (Arm: Operators without supervisors).
Analysis 2.3.
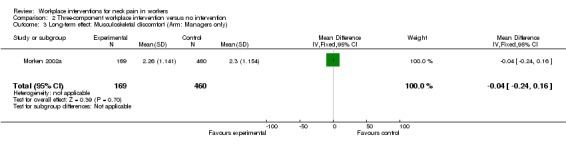
Comparison 2 Three‐component workplace intervention versus no intervention, Outcome 3 Long‐term effect: Musculoskeletal discomfort (Arm: Managers only).
Comparison 3.
Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention
Analysis 3.1.
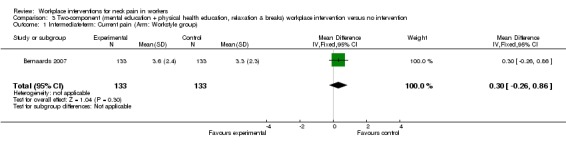
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 1 Intermediate‐term: Current pain (Arm: Workstyle group).
Analysis 3.2.
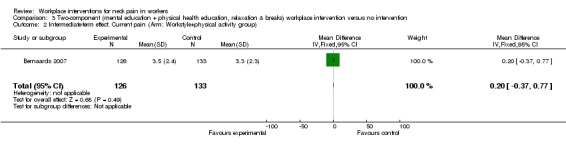
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 2 Intermediate‐term effect: Current pain (Arm: Workstyle+physical activity group).
Analysis 3.3.
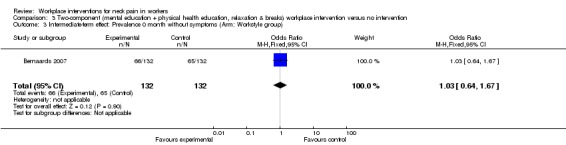
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 3 Intermediate‐term effect: Prevalence 0 month without symptoms (Arm: Workstyle group).
Analysis 3.4.
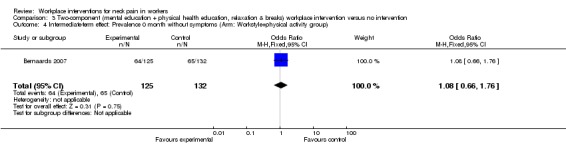
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 4 Intermediate‐term effect: Prevalence 0 month without symptoms (Arm: Workstyle+physical activity group).
Analysis 3.5.
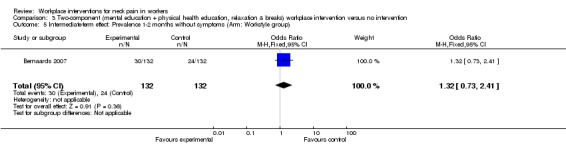
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 5 Intermediate‐term effect: Prevalence 1‐2 months without symptoms (Arm: Workstyle group).
Analysis 3.6.
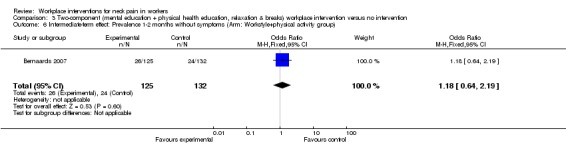
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 6 Intermediate‐term effect: Prevalence 1‐2 months without symptoms (Arm: Workstyle+physical activity group).
Analysis 3.7.
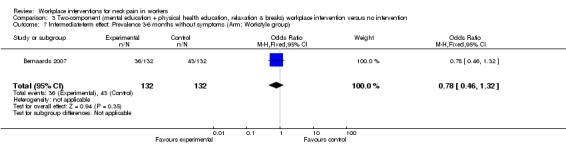
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 7 Intermediate‐term effect: Prevalence 3‐6 months without symptoms (Arm: Workstyle group).
Analysis 3.8.
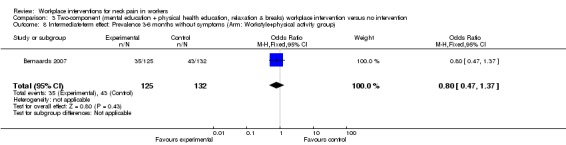
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 8 Intermediate‐term effect: Prevalence 3‐6 months without symptoms (Arm: Workstyle+physical activity group).
Analysis 3.9.
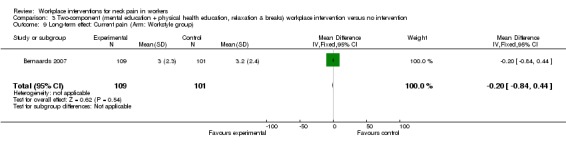
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 9 Long‐term effect: Current pain (Arm: Workstyle group).
Analysis 3.10.
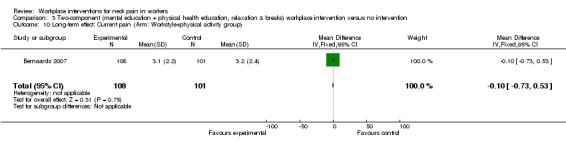
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 10 Long‐term effect: Current pain (Arm: Workstyle+physical activity group).
Analysis 3.11.
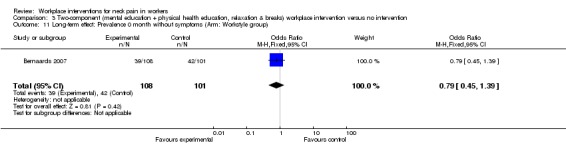
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 11 Long‐term effect: Prevalence 0 month without symptoms (Arm: Workstyle group).
Analysis 3.12.
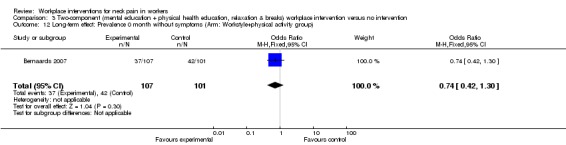
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 12 Long‐term effect: Prevalence 0 month without symptoms (Arm: Workstyle+physical activity group).
Analysis 3.13.
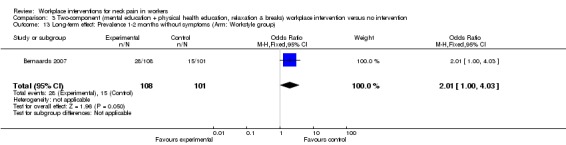
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 13 Long‐term effect: Prevalence 1‐2 months without symptoms (Arm: Workstyle group).
Analysis 3.14.
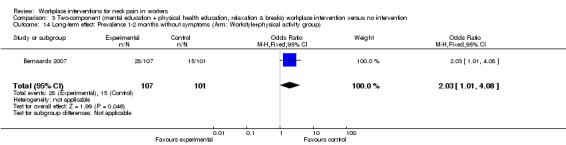
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 14 Long‐term effect: Prevalence 1‐2 months without symptoms (Arm: Workstyle+physical activity group).
Analysis 3.15.
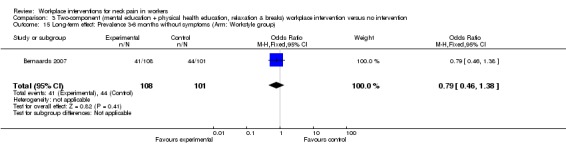
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 15 Long‐term effect: Prevalence 3‐6 months without symptoms (Arm: Workstyle group).
Analysis 3.16.
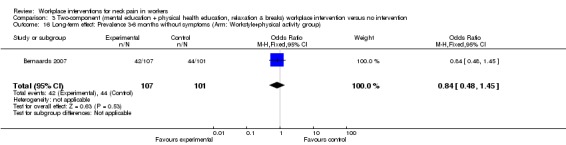
Comparison 3 Two‐component (mental education + physical health education, relaxation & breaks) workplace intervention versus no intervention, Outcome 16 Long‐term effect: Prevalence 3‐6 months without symptoms (Arm: Workstyle+physical activity group).
Comparison 4.
Two‐component workplace intervention (physical health education, relaxation & breaks + physical environment modifications) versus no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term effect: Musculoskeletal discomfort in the neck (Arm: Intensive ergonomic) | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐1.15, ‐0.05] |
| 2 Short‐term effect: Musculoskeletal discomfort in the neck (Arm: Ergonomic education) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐1.04, ‐0.16] |
| 3 Intermediate‐term effect: Musculoskeletal discomfort (Arm: Intensive ergonomics) | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.85, 0.25] |
| 4 Intermediate‐term effect: Musculoskeletal discomfort (Arm: Ergonomic education) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.64, 0.24] |
Analysis 4.1.
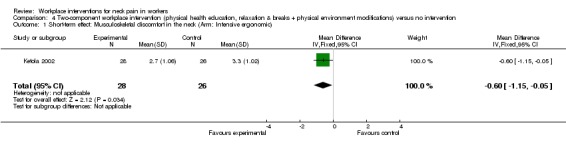
Comparison 4 Two‐component workplace intervention (physical health education, relaxation & breaks + physical environment modifications) versus no intervention, Outcome 1 Short‐term effect: Musculoskeletal discomfort in the neck (Arm: Intensive ergonomic).
Analysis 4.2.
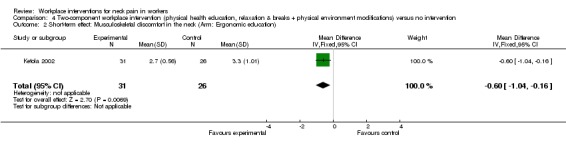
Comparison 4 Two‐component workplace intervention (physical health education, relaxation & breaks + physical environment modifications) versus no intervention, Outcome 2 Short‐term effect: Musculoskeletal discomfort in the neck (Arm: Ergonomic education).
Analysis 4.3.
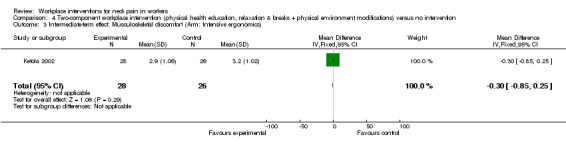
Comparison 4 Two‐component workplace intervention (physical health education, relaxation & breaks + physical environment modifications) versus no intervention, Outcome 3 Intermediate‐term effect: Musculoskeletal discomfort (Arm: Intensive ergonomics).
Analysis 4.4.
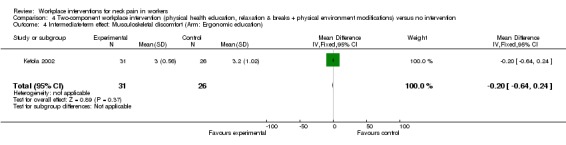
Comparison 4 Two‐component workplace intervention (physical health education, relaxation & breaks + physical environment modifications) versus no intervention, Outcome 4 Intermediate‐term effect: Musculoskeletal discomfort (Arm: Ergonomic education).
Comparison 5.
Mental health education vs. no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Long‐term effect: Change in pain drawing neck/shoulder | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐1.39, 1.19] |
| 2 Long‐term effect: Change in interference due to neck‐shoulder pain last month | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 7.70 [‐13.73, 29.13] |
Analysis 5.1.
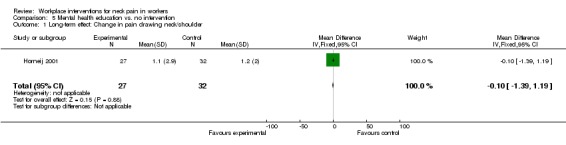
Comparison 5 Mental health education vs. no intervention, Outcome 1 Long‐term effect: Change in pain drawing neck/shoulder.
Analysis 5.2.
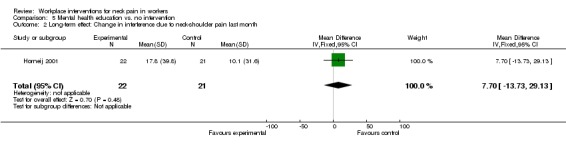
Comparison 5 Mental health education vs. no intervention, Outcome 2 Long‐term effect: Change in interference due to neck‐shoulder pain last month.
Comparison 6.
Physical environment modification versus another physical environment modification
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term effect: Prevalence of neck pain (Downward‐tilted vs. flat keyboard in computer work) | 1 | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.76] |
| 2 Long‐term effect: Prevalence of discomfort in neck/shoulder (Computer screen angle, high vs. low line‐of‐sight) | 1 | 137 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.02] |
Analysis 6.1.

Comparison 6 Physical environment modification versus another physical environment modification, Outcome 1 Short‐term effect: Prevalence of neck pain (Downward‐tilted vs. flat keyboard in computer work).
Analysis 6.2.
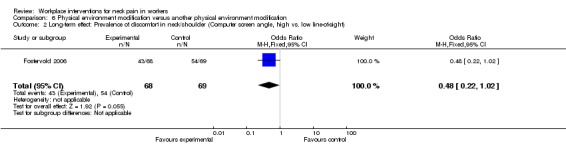
Comparison 6 Physical environment modification versus another physical environment modification, Outcome 2 Long‐term effect: Prevalence of discomfort in neck/shoulder (Computer screen angle, high vs. low line‐of‐sight).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | The study is a randomised controlled trial with a block‐randomised design. The study had two intervention groups and one control group. To prevent unbalanced randomisation, participants were pre‐stratified by company and self‐reported sports participation. The intervention period lasted six months in the years of 2004‐2005 and took place in the Netherlands. | |
| Participants | The participants were computer workers from head‐offices of seven companies in various branches (insurance, science, energy, transportation policy and taxes). The companies were located in different regions in the Netherlands. The inclusion criteria were: Frequent (i.e. at least once a week) long‐term pain, stiffness and tingles in neck, shoulders, arms, wrists and/or hands in the preceding six months and/or the last two weeks. Performing computer work for at least three days a week during at least three hours a day. Having a working contract until the last follow‐up measurement. Not being under treatment of a doctor or (physical) therapist for complaints in the neck, shoulders, arms, wrists and/or hands. Not having non‐work‐related or clear somatic diseases (e.g. rheumatoid arthritis, cervical hernia, tennis elbow, carpal tunnel syndrome). Finally, having sickness absence of less than 50% of the total working time (i.e. worker was working at least 50% of the hours he or she was supposed to work according to his or her working contract). Excluded were women who were pregnant in the start of the study. A short questionnaire was sent to 8000 workers. The number of workers who responded was 1875, of which 466 met the inclusion criteria and were randomised into three groups. The intervention group 1 (work style group) had 152 participants, the intervention group 2 (work style and physical activity group) had 156 participants and the control group had 158 participants. The follow‐up rate at 12 months was 68%. Mean age was 43.8, 43.6 and 44.4 years in the intervention group 1, intervention group 2 and control group respectively. Male sex was 54.6%, 53.8% and 58.2% respectively. Mean workdays a week were 4.5 days. MSD is described as symptoms in neck and upper limbs. The distribution of average pain at baseline was 4.1, 3.9 and 3.7 in intervention group 1, intervention group 2 and control group respectively on a scale from 0 'no pain' to 10 'worst pain ever'. Median duration of pain at baseline was 36 months, 30 months and 36 months respectively. Accordingly, prevalence of neck shoulder symptoms at baseline was 87.4%, 86.2% and 90.3% in the three groups. |
|
| Interventions | The intervention for the two intervention groups both consisted of six interactive group meetings of 15 to 60 minutes duration in a six‐month period. Four group meetings were large (with maximally ten participants) and two group meetings were small (with maximally three participants). The goal of all group meetings was behavioural change with regard to physical activity and/or work style. All group meetings took place at the workplace during work time under the supervision of a specially trained counsellor. The counsellors used standardised protocols. Intervention group 1: Work style group. The goal of the intervention was to stimulate work place adjustment and to improve body posture, the number and quality of breaks, and coping behaviour with regard to high work demands. Intervention group 2: Work style and physical activity group. In the combined intervention the additional goal was to increase moderate to heavy intensity physical activities, in addition to the interventions presented above. Performing physical exercise was not part of the intervention itself. Control group: The control group did not attend any of the group meetings, no intervention was given. |
|
| Outcomes | All outcomes except degree of recovery, were measured at baseline (October 2004). In addition, all outcomes were measured at six months follow‐up (April 2005) and twelve months follow‐up (October 2005). The primary outcomes were: Recovery: Degree of recovery from neck and upper limb symptoms was assessed using a seven‐point Visual Analogue Scale ranging from 'much worse' to 'completely recovered'. Pain intensity: Current pain, average pain and worst pain in the past four weeks were assessed using a validated eleven‐points numerical scale ranging from 0 'no pain' to 10 'worst pain ever'. Disability at work: Change in ability to work in the past four weeks was assessed with a validated eleven‐point scale ranging from 0 'no change' to 10 'extreme change'. Number of days with neck and upper limb symptoms: Participants reported the number of days with neck/shoulder symptoms and arm/wrist/hand symptoms in the past six months (no symptoms, 1‐7 days, 8‐30 days, 31‐90 days, 91‐180 days) and the past week (no symptoms, 1 day, 2‐3 days, 4‐7 days) using the validated Dutch Musculoskeletal Questionnaire. Number of months without symptoms: The number of months without neck and upper limb symptoms in the past six months was assessed using one question: “In how many of the past six months did you have no symptoms in neck and upper extremities?” |
|
| Notes | Additional information about the trial was found in two other publications (Bernaards 2006; Bernaards 2008). First author was contacted for missing information and responded. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “An independent statistician prepared the randomisation by using a computer‐generated randomisation.... Furthermore, block randomisation with blocks of three was used”. According to the first author, the generated sequences were like 123, 213, 321 etc, where number 1 was referring to group 1, 2 was referring group 2, and 3 was referring to group 3. The numbers were put in envelopes in this order. The first participants was given the first envelope, the second participant was given the second envelope etc. To conclude, this is an adequate method computer‐generated block randomisation. |
| Allocation concealment? | Low risk | Information about treatment allocation was kept in envelopes. The researchers were not aware of numbers inside the envelopes. After baseline measurements, the researchers opened the envelopes and informed the workers about group allocation. Some workers were informed about their treatment allocation by phone. This was the case when the participants were unable to collect their number themselves. The envelopes were opened during the call. The description above is based on information from the article and information given by author. To conclude, it is our impression that the allocation was adequately concealed. |
| Blinding? All outcomes ‐ participants? | High risk | Quote: "Unfortunate, it was impossible to blind participants and counsellors for the treatment allocation”. Blinding of participants to the intervention was not performed. |
| Blinding? All outcomes ‐ providers? | High risk | Blinding of care providers to the intervention was not performed either. |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | The researchers who performed the follow‐up were not aware of the treatment allocation of participants, except for the counsellors who also performed part of the measurements. According to the author the counsellors could have known treatment allocation for less than 10% of the participants. Since the outcomes assessors were blinded in more than 90% of the cases, we score 'yes' here. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | The drop‐out rate at 12 months follow‐up was 32 %, which is considered to be too high. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Quote. “Intention‐ to‐treat analyses were used to estimate the effect of the intervention. This means that all participants who were randomly assigned to one of the two intervention groups, were included in the analyses regardless of whether they attended the group meetings”. Intention‐to‐treat analyses were performed. |
| Free of selective reporting? | Low risk | All outcomes are reported thoroughly. There is no reason to suspect selective outcome reporting. |
| Similarity of baseline characteristics? | Low risk | According to table 1 in the article, the baseline characteristics of the participants were largely similar in all three study groups. |
| Co‐interventions avoided or similar? | Low risk | According to author all companies were instructed not to start any co‐interventions during the intervention period. If there were co‐interventions by means of discussions between the groups, they were similar in index groups and control group. |
| Compliance acceptable? | High risk | The main part of the intervention was attending group meetings. Compliance to the group meetings is reported in table 2 in the article in form of number of participants who attended the six meetings. Even though the compliance was quite similar in the two intervention groups, it was not high (less than 50% attended the meetings). Hence, compliance was not acceptable. |
| Timing outcome assessments similar? | Low risk | All groups were assessed simultaneously at baseline, 6 months and 12 months follow‐up. |
| Methods | The study is a randomised controlled trial with two interventions groups. A stratified randomisation procedure was used, where gender and age were regarded as potentially important prognostic factors and used as strata. The study was conducted in The National Insurance Services in Norway in 1999. | |
| Participants | The participants were recruited from employees at The National Insurance Services in Oslo, Norway. To be included in the study, the participants had to be between 18 and 62 years old and working between 70% and 100% of normal hours. Excluded were employees with known illness, planning to leave job or planning pregnancy. In total 150 employees out of 500 were selected. There were 75 participants in each group. All participants were experienced video display unit (VDU) users and used VDU above 50% of their working time. Thirteen workers left the study, giving a dropout rate of 9%. Mean age was 41.1 years and 40.8 years in intervention group 1 and intervention group 2 respectively. Hundred and eleven female workers and 39 male workers participated in the study. Sex distribution was 55 females in intervention group 1 and 56 females in intervention group 2. MSD was assessed by a symptom questionnaire measuring 14 different symptoms. Prevalence of discomfort in neck and shoulder at baseline was 75% and 73.5% in intervention group 1 and 2 respectively. |
|
| Interventions | The intervention was installation of a new desktop with a submerged VDU screen into the table top. The computer screen was lowered and tilted backwards in two different angles. Intervention group 1 had a high line of sight (HLS) α = ‐15º, which means a line of sight 15º lower than a horizontal line. Intervention group 2 had downward line of sight (DLS) α = ‐30º, which means a line of sight 30º lower than a horizontal line. |
|
| Outcomes | The following outcomes were measured at baseline and after 12 months: Subjective symptoms: A symptom questionnaire developed in‐house assessing 14 different symptoms was used. The symptoms were: Focusing difficulties, headache, discomfort in the neck and shoulder, discomfort in the back, discomfort in the arm, discomfort of the leg, skin symptoms, dizziness, nausea, concentration problems, general feeling of fatigue, discomfort in eyes, tired eyes, and reading problems. Each symptom was assessed by seven items. The first one categorical, determining whether or not the participant had experienced symptoms during the last three weeks. The remaining items were intensity and duration of that symptom. This was assessed on a seven‐step numeric scale with semantic descriptors at both ends and in the middle. Health examination (included number of days absent due to illness during last six months): The examination comprised the following health indicators: Musculoskeletal tender or trigger points, neck mobility, presence of and intensity of any pain during neck movements, isometric/endurance test, palpation of tendon attachments, mobility in the shoulder joint and symptoms of carpal‐tunnel syndrome. In addition a structured clinical interview identified these issues: Known disease, prescribed medication, use of painkillers, received physiotherapeutic or chiropractic treatment, smoking, height, weight, number of days absent due to illness during last six months, and number of work days absent due to musculoskeletal problems in previous six months. Optometric status: This outcome was assessed by measuring refraction, contrast sensitivity, and the zone of clear single vision. Musculoskeletal load: EMG (electrode electromyography) was used to measure muscle activity of neck and shoulder area. Control measures: Individual psychological states, satisfaction with the physical work environment and perceived work strain were measured to control for potential confounding factors. Control measurements of lighting, screen distance, and working hours in front of the VDU, were also recorded. |
|
| Notes | First author was contacted for missing information and responded. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | According to first author it was used a between subjects design between units and a stratified design within each unit. Stratifying factors were gender and age. Block randomisation with a block size of four was used as randomisation procedure between units. A simple stratified lottery technique was used as assignment procedure. Drawing of lots is an adequate method of randomisation. |
| Allocation concealment? | Low risk | After recruitment each participant was allocated a case number comprising individual identification number and unit identification number. The people carrying out the assignment procedure did not conduct the number allocation. Neither were they part of the recruitment process. Information about the case number, age and gender were then handed over to the staff conducting the randomisation procedure. All this according to first author. This is an adequate method of allocation concealment. |
| Blinding? All outcomes ‐ participants? | High risk | It was impossible to blind the worker. |
| Blinding? All outcomes ‐ providers? | High risk | It was also impossible to blind the care provider to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | High risk | The study contained measures like self‐assessed questionnaire, optometric examination, health examination and musculoskeletal load. According to author, outcome assessors were blinded to the intervention except for measures of musculoskeletal load. Without all measurements blinded, it is not possible to score ´yes´. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | In total 9% of the participants dropped out of the study. They were evenly distributed between the groups. This is an acceptable drop‐out rate. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Author has confirmed that all randomised participants were analysed in the group to which they were allocated. |
| Free of selective reporting? | Low risk | All outcomes are reported thoroughly. Based on an overall impression, ´yes´ is scored. |
| Similarity of baseline characteristics? | Low risk | Stratified randomisation was performed to ensure equally distribution of gender and age. Author provided information about sex distribution between the groups. The groups were similar at baseline regarding the important indicators; age and sex. |
| Co‐interventions avoided or similar? | Low risk | Co‐interventions were avoided according to author. |
| Compliance acceptable? | Low risk | Due to the nature of the interventions, the participants in both groups had to comply when doing computer work. |
| Timing outcome assessments similar? | Low risk | Author has confirmed that the timing of the outcomes assessments was similar in both groups. |
| Methods | The study is a cluster‐randomised trial consisting of two groups. Randomisation was carried out using an assignment algorithm called Alternate Ranks Design (ARD) and stratification by area (city district) and type of kitchen (school, nursery, home for senior citizens, other institution). The study was conducted in different institution‐based kitchens in four large cities in Finland in the years 2002‐2005. The duration of the intervention was 11 to 14 months. |
|
| Participants | Out of 202 eligible municipal kitchens, 80 kitchens refused to participate either collectively or based on individual workers refusal. Thus, 122 kitchens were randomised to intervention group and control group. However three kitchens dropped out. Of the remaining 119 kitchens, the intervention group consisted of 59 kitchens and the control of 60 kitchens. The total number of workers was 504 (263 in intervention group, 241 in control group). Inclusion criteria were having at least three full‐time workers in each kitchen and employees working for at least six hours per day. Exclusion criteria are not stated. There were different kinds of kitchens: School (intervention group 43, control group 42), nursery (intervention group 10, control group 11), nursing home (intervention group 5, control group 6), and other (intervention group 1, control group 1). The workers were food service managers, chefs, cooks, kitchen aids and others. Distribution of female sex was 96% and 98% in the intervention group and control group respectively. Accordingly, range of age (median) was 19‐63 (46) years and 19‐62 (47) years. Distribution of full time work was 95% and 97% in the two groups respectively. Prevalence of neck pain at baseline was 71%. |
|
| Interventions |
Intervention group: The intervention was carried out in a participatory way based on active group work. The workers were actors identifying problems, planning and evaluating changes, and implementing them in collaboration with management and technical staff. The researcher acted as a consultant and trainer, promoting, guiding, and training the workers during the development work and taking care of progress of the implementation of changes. Regular meetings were held to standardise the working methods of the teams. In addition, a project coordinator participated in the workshops, observed the working of the researchers, and provided them with feedback. The intervention phase was composed of a 2‐month pre‐implementation phase and a 9‐12‐month implementation phase. In the pre‐implementation phase all workers participated in a two days (10 hours) workshop where they initially were taught basic principles of ergonomics and the functions of musculoskeletal system. In the second workshop every kitchen decided on their primary targets to improve ergonomics and planned the implementation. In the implementation phase ergonomics changes were carried out, promoted by 18 hours of workshops. Each of the three workshops had a specific thematic element related to ergonomics, and the process of intervention was thoroughly discussed. Control group: In the control kitchens normal activity was going on. No intervention was given. |
|
| Outcomes | All measurements were collected by a questionnaire at baseline and every three months during the intervention (3, 6, 9 and 12 months), and post intervention measures were taken at 3, 6, 9 and 12 months. In all, measurements were collected nine times. The outcomes were: Prevalence of musculoskeletal pain (included prevalence of neck pain): This outcome was measured in seven anatomical sites (neck, shoulders, forearms/hands, low back, hips, knees and ankles/feet). Trouble caused by pain during the past three months: This outcome was measured ranging from 1 (not at all), to 7 ( very much). Local fatigue after the work day during the past seven days: Was measured on a scale from 1 (not at all) to 6 (very much). Prevalence of musculoskeletal sick leave during past three months: This outcome was measured as 'yes' or 'no'. Changes in perceived physical workload: Was measured ranging from 1 (not at all) to 7 (very strenuous). Prevalence of stress: Psychosocial factors such as stress was measured during the past month ranging from 1 (no stress at all) to 3 (much stress). Mental strenuousness at work: Was measured ranging from 1 (not at all) to 3 (very strenuous). Job satisfaction: Was measured as 1 (satisfied), 2 (undecided) and 3 (dissatisfied). |
|
| Notes | Additional information about the study was found in two other publications (Haukka 2006; Pekhonen 2009). First author was contacted and gave us missing information. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote:”Randomisation was carried out using an assignment algorithm (Alternate Ranks Design (ARD) and stratification by area (city district) and type of kitchen (school, nursery, home for senior citizens, other institution). Kitchens in each stratum were ranked in descending order by number of staff. A person not otherwise involved in the study during the field phase performed the randomisation”. This is an adequate method of avoiding selection bias. |
| Allocation concealment? | Low risk | Concealment of allocation is not reported. When asked, first author informs that the person who carried out the randomisation and assignment to the study arms, was an independent person with no information about the persons included in the trial and no influence on the assignment sequence or on the decision about eligibility of the participant. This is an adequate method of concealed allocation. |
| Blinding? All outcomes ‐ participants? | High risk | Participants were not blinded to the intervention. |
| Blinding? All outcomes ‐ providers? | High risk | Care providers were not blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | Data were collected from the participants by questionnaire. The researchers were blinded in the following respect: they had no access to the questionnaire data during the data collection, and data analysis was started only after the whole follow‐up data was collected. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | At 12 months follow‐up 82 out of 504 participants had dropped out. This gives a drop out rate of 16%, which is acceptable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | All kitchens were analysed into the group they were allocated, except three kitchens that dropped out. We consider this situation analogous to the case in which the patients dies before starting the medication/treatment, This is not generally considered as a situation that destroys the intention‐to‐treat principle. The amount of dropouts were minor in relation to the total number of kitchens and does not threaten the comparability of the groups. |
| Free of selective reporting? | Low risk | There is no reason to suspect selective outcome reporting. |
| Similarity of baseline characteristics? | Low risk | According to table 1 in the article the groups were similar at baseline regarding important indicators. |
| Co‐interventions avoided or similar? | Low risk | “All the participants were asked not to talk about the study process in case they changed kitchen. Only two workers were transformed from an intervention to a control kitchen during the intervention, so that contamination was probably minor”. In addition, it was a cluster randomised trial with participants from the two arms of the study working at separate locations. |
| Compliance acceptable? | Low risk | Quote: “On average 73% of the workers participated in the workshops”. Based on this, we think that the compliance was acceptable. |
| Timing outcome assessments similar? | Low risk | According to table 2 in the article, the timing of the outcome assessment was similar in both groups. |
| Methods | The study is a randomised controlled trial consisting of two groups. The study was conducted in a large office building in Phoenix, USA in 1995. The intervention period lasted three weeks. | |
| Participants | Recruitment of participants is not reported, however 46 participants were included in the study. By the end of the study eight participants had either moved their work location or moved to another company. Thus, only 38 participants were left at three weeks follow‐up. Inclusion criterion was being a full time office employee. Exclusion criteria are not stated. All participants were working by computer. They were engineers constructing Boeing airplanes. The participant's age ranged from 24 to 57 years, with a mean age of 37.4 years. Seventy‐four percent of the participants were female. The average amount of time using computer each day was 5.4 hours. The Intervention group had 23 participants, the same as the control group. Neck pain prevalence at baseline 70% and 54% in the intervention group and control group respectively. |
|
| Interventions |
Intervention group: The intervention consisted of using a downward tilted computer keyboard on a tray. Control group: The control group used a conventional keyboard placed on a flat keyboard tray. |
|
| Outcomes | All outcomes were measured at baseline and after three weeks. Physical dimensions of the workstation: This outcome was measured (home/row height; distance from the floor to the top of the home row keys; keyboard slope angle of the keyboard at the home row, measured with an inclinometer; seat pan height; distance from the floor to the lower edge of the seat pan fabric; monitor distance; distance from the centre of the monitor to the eyes when sitting in front of the computer with fingers on the home row keys). Presence of wrist rest and/or foot rest (yes/no) was noted. VDU work: The participants were asked for the following information: Job tenure (months); daily VDT use (hours); mouse use (never, occasionally, fairly often, very often); frequency of data entry (never, occasionally, fairly often, very often); use of wrist rest (yes/no); use of foot rest (yes/no). Participants were asked about their knowledge of ergonomics (none, a little, moderate, very knowledgeable, expert). Workstation comfort: Was measured using a self‐report questionnaire on physical comfort of keyboard use, mouse use and chair comfort (very uncomfortable, fairly uncomfortable, fairly comfortable, very comfortable). Musculoskeletal discomfort (included prevalence of neck pain): Was measured with a self‐reported, not validated questionnaire that was developed in‐house. This questionnaire asked participants to rate discomfort in all body regions on the following scales: frequency of ache, pain, discomfort (never, 1 ‐ 2 times last week, 3 ‐ 4 times last week, once every day, several times every day); intensity of ache, pain, discomfort (slightly uncomfortable, moderately uncomfortable, very uncomfortable); ache, pain, discomfort interference with work (not at all, slightly interfered, substantially). |
|
| Notes | First author was contacted for missing information and responded. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "Pretest measures were taken for all subjects after which they were randomly assigned to either a control or a test group". When asked, first author informs that there was a list with names of participants giving each participant a number. Randomisation was performed by selecting numbers from an opaque bag of labels. This method is in principle the same as drawing of lots, which is an acceptable method of randomisation. |
| Allocation concealment? | High risk | Concealment of allocation is not reported. When asked, author could not verify adequate concealment. |
| Blinding? All outcomes ‐ participants? | High risk | The participants were not blinded to the intervention. |
| Blinding? All outcomes ‐ providers? | High risk | The care providers were not blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | When asked, author informs that the participants completed their own surveys and placed them into sealed envelopes. Other outcomes were collected online without influence of outcomes assessor. To conclude, outcome assessors were blinded to the intervention. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | The dropout rate varied in the two groups. All eight participants who dropped out came from the control group, giving a dropout rate of 35 % in this group, which is unacceptable in a three weeks intervention period. To conclude, the drop out rate was too high for such a short intervention period. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | Intention‐to‐treat is not reported. When asked, author informs that the eight participants that dropped out, were excluded from analyses. Hence, intention‐to‐treat is not accomplished. |
| Free of selective reporting? | Low risk | There is no reason to suspect selective outcome reporting. |
| Similarity of baseline characteristics? | Low risk | Baseline data such as sex‐ and age distribution of the two groups are missing. According to the memory of author, there were no significant differences between the groups at baseline regarding important indicators. |
| Co‐interventions avoided or similar? | Low risk | According to author no other interventions occurred at the time of the study. |
| Compliance acceptable? | Low risk | Due to the nature of the intervention; downward tilted keyboard on tray, the participants had to comply in order to do their jobs. |
| Timing outcome assessments similar? | Low risk | The timing of outcome assessments was similar in both groups. |
| Methods | The study is a randomised controlled trial consisting of three groups. The study was conducted in five municipal home‐care services in a medium sized city in southern Sweden in the year 1996‐1997. The follow‐up period was 18 months. | |
| Participants | Female nursing aides and assistant nurses working in the home‐care service were invited to participate in the study. In all, 659 women were invited to participate and 534 (81%) accepted. Due to recourses available, only 282 participants were randomised into the three groups. Intervention group 1 had 93 participants, intervention group 2 had 99 participants and the control group had 99 participants. Only 169 participants completed follow‐up at both 12 and 18 months. The inclusion criteria were Swedish speaking, permanently employed, female nursing aides and assistants working at least 50% of full time, not pregnant and not suffering from intercurrent disease. Mean age was 45, 43 and 44 years in intervention group 1, intervention group 2 and control group respectively. Prevalence of neck pain during the preceding year was 54 to 61%. Sick leave due to neck, shoulder and/or back pain during the last year was reported by 13% of the participants. |
|
| Interventions |
Intervention group 1 ‐ Stress Management Programme in Groups (SM): The purpose of this intervention was primarily to identify and reach goals and strategies for perceived stress induced by lack of social support, low decision latitude/work control, and perceived high psychological work load. The intervention was based on group instruction. Each group consisted of participants from one work place. In all, 12 groups were involved. Every group met 7 times over a period of 7 weeks, each time for 1.5 hours. Two follow‐ups were carried out after about 3 and 6 months. The meetings covered both theory and practice. An important part involved interactive talks among the participants concerning their experience of stress in general and at work, and how to handle these problems. At the seventh meeting a stress‐reducing goal for the entire workplace was formulated by the participants. The aim was to fulfil the goal within the follow‐up 3 months later. Furthermore, the participants formulated an individual goal in order to reduce perceived stress at work and/or at home. The goal was to be concrete and attainable within 6 months. The immediate supervisors were invited to join the sixth or/and the seventh meeting if the participants agreed. Intervention group 2 ‐ Individual Physical Training Programme (IT): The participants underwent initially a clinical physical examination. In connection with this examination all participants received an individually designed training programme. The exercises were individually adapted and individual goals were formulated. The majority of the exercises were taken from a manual specially designed for this purpose. The participants were asked to take notes every time they did their exercises and every time they exercised for more than 20 minutes and perceived the training “somewhat hard”. Control group ‐ The Non‐Intervention Group: This group was to function as a check for environmental changes during the follow‐up period. Participants were requested to live as usual. If, however, the physical examination indicated a condition which could risk the participant’s further health, e.g. increased blood pressure or severe musculoskeletal disorders, she was recommended to contact a physician. |
|
| Outcomes | The following measurements were conducted at baseline, and at 12 and 18 months follow‐up: Musculoskeletal pain: Neck, shoulder and back symptoms were assessed using the Nordic Musculoskeletal Questionnaire (NMQ). The response options were 'yes' and 'no'. Perception of pain during the previous 6 months: This outcome had 5 scores: Much better, better, same, worse, much worse. Perceived interference with work and/or leisure activities due to discomfort: Those who in NMQ had indicated pain the neck/shoulders and/or back were asked to rate how much these problems had interfered with work and/or leisure activities. Rating was done on a 100mm visual analogue scale. Changes from baseline to follow‐up above 10mm were considered as a change. Pain‐drawing: The extension of pain during the previous month was described on a pain‐drawing. The extension of pain was evaluated by the sum of areas marked. The neck/shoulder region was covered by 12 areas. Perceived physical exertion at work: This outcome was measured on a Borg scale. The question asked was: “How physically demanding do you in general perceive your work to be?” The rating was from 6 to 20, where 6 meant 'less than very, very easy' and 20 meant 'more than very, very hard'. Perceived work‐related psychosocial factors: This outcome was assessed with the questionnaire developed by Rubenowitz comprising five psychosocial factors, namely 1) Influence on and control over work, 2) Supervisor climate, 3) Stimulation from work itself, 4) Relations with fellow workers, and 5) Psychological workload. Each factor comprised five items and each item had five responses, where 1 meant 'very unsatisfactory' and 5 meant 'entirely satisfactorily'. Physical activities and fitness training the previous 6 months: A question about physical exercise from Wiktorin was modified: “To what extent have you performed physical activities of fitness training during the previous six months?” The scores were rated from 1 to 8, where 1 meant 'no exercise, and very little physical activity' and 8 meant 'hard physical exercise with vigorous exertion and training/competition at top level'. The following outcome was measured at 12 and 18 months follow‐up: Perceived amount of training: This outcome reported to what extent the participants had performed any training during the last 6 months compared with previously. The following outcome was only measured at 18 months follow‐up: Question about applied relaxation and home exercise: At 18 month the participants were asked to what extent they had performed any relaxation and home exercises during the preceding 6 months. |
|
| Notes | Since physical activity is an intervention outside the scope of this review, we disregard this intervention in analyses. First author was contacted for missing information and responded. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | According to first author the randomisation was made by computer in two steps: In step one randomisation was done at group level to one of the three interventions to avoid co‐interventions within each of the five home‐care units. This was possible as each caring unit comprised several work places and each work‐place had its own leader. In step two randomisation was made on individual level in order to decide which participants should be included. To conclude, generation by computer is an adequate method of randomisation. |
| Allocation concealment? | Unclear risk | Author could not confirm adequate concealment of allocation. |
| Blinding? All outcomes ‐ participants? | High risk | It was not possible to blind the workers in this type of interventions. |
| Blinding? All outcomes ‐ providers? | High risk | Care providers could not be blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | Quote: “The questionnaires were administrated by the project nurse, who was not involved in the intervention programmes, and blinded to group allocation”. Outcome assessor was blinded to group allocation. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | Out of 282 participants, 169 completed all follow‐ups. This gives a drop‐out rate of 40%, which is not acceptable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Author confirms that all randomised participants were analysed in the group to which they were allocated. |
| Free of selective reporting? | Low risk | Since all outcomes are reported, the article appears to be without selective reporting. |
| Similarity of baseline characteristics? | Low risk | Quote: “There were no differences between the groups at baseline for any demographic or outcome variable”. The groups were similar at baseline. |
| Co‐interventions avoided or similar? | Low risk | Quote: “To avoid interference bias between the programmes, the randomisation comprised two steps: (1) all work places at each unit were randomised to one of three groups (...). 2) Individuals were randomly assigned from their designated workplaces”. Measurements were taken to avoid co‐interventions within each unit. Treatment outside the study might have occurred, but was most likely similar in all groups. |
| Compliance acceptable? | Low risk | Quote: “Besides the first examination, the IT programme included four sessions and the SM programme seven sessions and two follow‐ups. Only six participants of the IT group and nine participants of the SM group attended fewer than 50% of the sessions”. Since the groups consisted of 90 and 93 participants respectively, this is considered to be good compliance to the intervention. |
| Timing outcome assessments similar? | Low risk | Outcomes were evaluated at simultaneously in all groups. |
| Methods | The study claims to be a controlled trial with randomly assigned participants. The study had two intervention groups and one control group. The intervention period lasted four weeks and follow‐up was conducted after six months. The study took place in Sweden. The year the study was conducted is not stated, but it must have been before 1991 when the article was published. | |
| Participants | Medical secretaries were invited to be part of the study. The setting was a hospital where both interventions and follow‐up took place. The secretaries' major tasks were typing patient journals, letters and reports, in addition to telephone, mail an appointment duties. Inclusion criteria were having experienced some pain in either the neck or shoulder region during the previous year, and having estimated their average time of sitting during working hours to be a minimum of five hours daily. In addition, the inclusion criteria were having worked at least 30 hours a week and not being under medical treatment for their neck and shoulder problems. From a study of 420 medical secretaries, 119 fulfilled the initial inclusion criteria. After further screening 40 secretaries were excluded for different reasons, hence 79 secretaries were included in this trial. The participants were all females and the mean age was 39.4. They had worked as secretaries for an average of 9.6 years and 73% of them worked full time. The number of participants was 25, 28 and 26 in the intervention group 1, intervention group 2 and control group respectively. Three secretaries went on maternity leave during the study period and thus 76 remained at six months follow‐up. There is no information about how pain was defined in the selection of participants. During the previous year 63% of the 420 secretaries had experienced neck pain. Of the sample of 119 participants all had experienced some pain in the neck or the shoulder region during the previous year. |
|
| Interventions |
Intervention group 1: Traditional neck school. Participants in this group attended a four‐hour traditional neck school conducted by a therapist. Lectures were given twice weekly during working hours and consisted of a series of slides which included anatomy, aetiology of musculoskeletal disorders, ergonomics and self‐care measures. Part of each lecture was used to pause‐gymnastics in form of exercises using the neck and shoulder followed by relaxation. In addition, ergonomics of the workplace was demonstrated. Intervention group 2: Reinforced neck school. In addition to the above described neck school, the participants in this group received a variety of measures to enhance compliance. The participants were visited by a therapist at the workplace. Ergonomic adjustments were discussed. They were also interviewed by a psychologist on psychosocial and organizational factors. The total additional time allotted to this group was two hours per individual. Other methods to enhance compliance in this group were: 1) Only measures that the participants agreed upon were included in their individual program. 2) The participants received written information for a pause‐gymnastics program. 3) A written list of all measures agreed upon was given to the participants. 4) Participants were contacted for a follow‐up after three months. Control group: The control group was not offered any intervention until after completion of all follow‐up assessments. |
|
| Outcomes | Measurements were made baseline, after the four‐week intervention period and at six months follow‐up. The outcomes were: Expectancy: Four questions were used to measure expected outcome. The questions asked were how relevant the program was, whether it could be recommended to others, and how successful it might be for neck and shoulder, as well as for back pain. Each question had a ten‐point scale ranging from 1 'not at all relevant' to 10 'very relevant'. Ergonomic knowledge: A multiple choice questionnaire was constructed with 13 questions (range 0‐49 points) covering the neck school material. This test was applied in both intervention groups before and after neck‐school. The control group did not receive the test. Fatigue and pain: Daily ratings of muscular neck and shoulder fatigue and pain was carried out at work for a five days period. Ratings were conducted three or four times a day. A ten cm Visual Analogue Scale anchored by 'no pain' to ' considerable pain' was used. Work load: Estimated workload was rated daily using ten cm Visual Analogue Scale anchored by 'usually little to do' to 'unusually mush to do'. Range of motion: Active range of motion was measured at pre‐, post‐, and follow‐up periods, according to American Academy of Orthopedic Surgeons recommendations by means of a Myrin goniometer. Headache and low back pain: This was rated at pre‐, post, and follow‐up periods using a. ten cm Visual Analogue Scale anchored by 'no pain' to ' considerable pain'. Sickness absence: Information about sick leaves was obtained from the Swedish Social Insurance Agency. Diagnoses, number of sick leave occasions, and number of days on sick leave were registered. Interview information at follow‐up: Number of ergonomic changes the participants had implemented at work, number of pieces of equipment acquired, and number of visits to a physician, therapist or chiropractor for neck and shoulder pain or headache after the four week programme were registered. Adherence to individual programs for intervention group B was also registered. |
|
| Notes | Additional information about the study was found in another publication (Kamwendo 1991B). First author was contacted for missing information, but could not respond our questions, since the study is rather old. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote:“The subjects were randomly assigned to a control group or one of two interventions groups.” No details are given on how the randomisation procedure was performed. First author was contacted for clarification, but could not respond, since the study is rather old. We think that the method of randomisation most likely was adequate, but the information available is limited. |
| Allocation concealment? | Unclear risk | No information is given on allocation concealment in the article or provided by author on request. |
| Blinding? All outcomes ‐ participants? | High risk | No detailed information is given, but it is not likely that the participants could be blinded to the intervention. |
| Blinding? All outcomes ‐ providers? | High risk | No detailed information is given, but it is not likely that the care providers could be blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | The outcome assessor may have been blinded, but it is not clear in the text if the research team and the intervention team were separate. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Unclear risk | Even though 76 out of 79 participants remained in the study at the end, it is quite uncertain that there is data for all the 76 individuals regarding the main outcome variable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Intention‐to‐treat analyses are not reported. Author could not clarify this matter. |
| Free of selective reporting? | Low risk | No selective reporting is suspected in this article. |
| Similarity of baseline characteristics? | Unclear risk | No information comparing the three groups at baseline is given. |
| Co‐interventions avoided or similar? | Low risk | No information is given on co‐interventions, but it seems unlikely. |
| Compliance acceptable? | Low risk | Quote: “Consequently, the failure of this study to demonstrate a decrease in neck or shoulder discomfort did not occur as a result of poor compliance, rather despite good compliance”. Attendance to neck school was 100% in intervention group 1 and 98% in intervention group 2, which is very acceptable. |
| Timing outcome assessments similar? | Low risk | The timing of the outcomes was the same for all three groups. |
| Methods | The study is a randomised controlled design with a block‐randomised design having two intervention groups and one control group. The study was conducted in three administrational units in a medium‐sized city in Finland in 1998‐1999. The administrational units were used as stratum for the block randomisation, which was done on an individual level. The duration of follow‐up period was ten months. | |
| Participants | The employees were mainly secretaries, technicians, architects, engineers and draftspersons, all working at video display units. The inclusion criteria were symptoms in the neck, shoulders, or upper‐limb in one to eight anatomical areas, out of eleven areas all together, during the preceding 30 days. In addition, the inclusion criteria were computer work for more than four hours per week, mouse use for more than 5% of the work time and age under 61 years. A number of 515 employees were asked to fill out a questionnaire, of which 416 employees returned the formulae. One hundred and twenty‐four participants met the inclusion criteria and were randomised into three groups, however only 109 participants were left at baseline. At ten months follow‐up there were 102 participants left. Intervention group 1: Intensive, (N=39), had 60% women, with a mean age of 46 years. Intervention group 2: Education, (N=35), had 60% women and a mean age of 49 years. The control group, (N= 35), had 54% women and a mean age of 49 years. MSD was described as symptoms in the neck, shoulders, or upper‐limb region in one to eight anatomical areas during the preceding 30 days. The prevalence of neck pain at baseline was 78%, 77% and 77% in the three groups respectively. |
|
| Interventions | All participants were given a one‐page leaflet on musculoskeletal health in association with computer work. Intervention group 1: Intensive ergonomics. Physiotherapists visited the work site of every member of the intensive ergonomics group. They introduced an ergonomic checklist for computer work. The checklist emphasised the following three items: the layout and environmental conditions of the workroom, adjustments of the workstation, and breaks during work. The participants independently assessed their workstations with the aid of the list and answered the questions. Adjustments and alterations in the existing furniture and work equipment were performed. The worker was also encouraged to participate actively in the redesign and rearrangement of his or her workstation. New forearm and wrist rests were available if needed. In addition, the participants were advised to pay attention to their work postures and to add short pauses into their work. The ergonomic evaluation and the implementation of the immediate changes for a workstation took approximately 1.5‐2 hours. Intervention group 2: Ergonomic education. The participants attended a 1‐hour training session in ergonomics in groups of two to six persons. A trainer in ergonomics instructed the workers concerning the principles of ergonomics in computer work. They received the same checklist as the intensive ergonomics group and were encouraged to evaluate their own workstation, implement changes, and ask for new equipment and furniture if needed. Moreover, the participants were instructed to add short pauses and adopt relaxed work postures. Control group: The group received no intervention, except for the one‐page leaflet. |
|
| Outcomes | Measurements were taken at baseline, at two months follow‐up and at ten months follow‐up, for the outcomes called diary of discomfort, musculoskeletal strain and pain, and level of ergonomics. The outcome called workload was only measured at baseline. Musculoskeletal discomfort: The participants were asked to keep a diary of discomfort three times a day. The diary consisted of questions of discomfort in different anatomical areas. The rating had a five‐point scale from 1 'feel good' to 5 'feel very uncomfortable'. A manikin (modified from Nordic Questionnaire) was used to define anatomical areas. Musculoskeletal strain and pain (included current pain): Strain after a usual workday during the preceding 30 days was assessed by a five‐point scale ranging from 1 'no strain' to 5 'very much strain'. The questions of pain during the preceding 30 days addressed the number of days with pain. The answers were classified into 'no pain' (0 day) and 'pain' (>1 days). Level of ergonomics: This was measured by use of video recordings of the participants performing their daily tasks. A continuous four minutes extract of each participant was chosen to represent the person’s most common computer tasks. Two researchers analysed these extracts and gave them an overall ergonomic rating from 4 'poor' to 10 'excellent' using a scale from the Finnish educational system. Workload: For the assessment of the amount of daily work load, daily computer usage in minutes was calculated. This was done by using a special software program monitoring key board and mouse usage continuously. |
|
| Notes | First author was contacted and filled in missing information. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | According to first author randomisation was performed using a computer program. Using a computer random number generator is an adequate method of randomisation. |
| Allocation concealment? | Unclear risk | Allocation concealment is not reported. When asked, author could not verify that allocation was adequately concealed. |
| Blinding? All outcomes ‐ participants? | High risk | Participants could not be blinded to the intervention. |
| Blinding? All outcomes ‐ providers? | High risk | Care providers could not be blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | Quote: “Data on workplace layout and dimensions were collected before the intervention and also 2 and 10 months after it by two experts in ergonomics. They were blinded to the group assignment of study subjects”. Outcome assessors were blinded to the intervention. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | Out of 109 participants at baseline, 102 were left at ten months follow‐up. This gives a drop‐out rate of 6% which is very acceptable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Author confirms that all randomised participants were analysed in the group to which they were allocated.. |
| Free of selective reporting? | Low risk | There is no reason to suspect selective outcome reporting. |
| Similarity of baseline characteristics? | Low risk | Quote: "The strength of our study was that all three groups were comparable as regards to demographic characteristics and occupational factors measured at the beginning of the study”. According to table 1, the groups were largely similar at baseline. |
| Co‐interventions avoided or similar? | Low risk | Quote: “On the other hand it was practically impossible to prevent personal interaction between the groups" (....). "Ten subjects in the intensive group, seven in the education group, and eight in the reference group contacted the occupational therapist to get ergonomic advice during the 10‐month follow‐up”. Co‐interventions were not avoided, but were similar in all groups. |
| Compliance acceptable? | Unclear risk | Compliance is not reported in the article. When asked, author could not verify acceptable compliance. |
| Timing outcome assessments similar? | Low risk | The timing of the outcome assessment was similar in all groups. |
| Methods | The study is designed as a cluster‐randomised controlled trial consisting of three intervention groups and two control groups. One control group (group B) was not randomised. The study was performed for a period of 16 months, from 1998‐2000 in eight aluminium plants in Norway. | |
| Participants | For intervention group 1, 2, 3 and control group A, the inclusion criterion was workers who could shift groups of operators in the production line. Exclusion criterion was other functions/types of jobs. The excluded participants constituted control group B. All employees in the eight aluminium plants were recruited by participating in the baseline survey, where 92% (N=5654) filled out the questionnaire satisfactorily. Among them 67% were operators, 20% were office workers and 8% were managers. Mean age was 40 years with a range from 18‐69 years. Eighty‐six per cent were men and 14% were women. Mean duration of employment at the plant was 16 years. Of those completing the post intervention questionnaire (N=5143, 94% of all workers), 3321 participants were so‐called matched individuals with completed questionnaire in 1998 and 2000. Of those matched participants, 837 were operators in the production line which were randomised on group level to three intervention groups and control group A. The rest (N= 1344) constituted control group B. A number of 414 participants received the intervention. In intervention group 1 operators and supervisors participated (20 shift groups, N=132). In intervention group 2 operators only participated (18 shift groups, N=135). In intervention group 3, two groups of supervisors and managers and ten groups of operators participated (N= 147). A total number of 423 workers from the production line were in control group A. At 16 months follow‐up there were 2181 participants left. The production line was chosen for intervention due to high prevalence of MSD, well‐known risk factors and similar and comparable job content. Work in the production line was physically demanding. At baseline 94 had experienced pain in one of more of body parts the last 12 months (range 87‐95%). The prevalence of participants with neck pain was 68%. |
|
| Interventions |
The intervention groups:The intervention was developed specifically for the needs of the aluminium industry. The intervention was similar in the three intervention groups. The reason for three groups receiving the same intervention was to examine the potential differing results according to who participated in the process; the operators and their supervisors (group 1), the operators only (group 2) or the managers and supervisors only (group 3). The company physiotherapists were the providers of the intervention, which included ten meetings aimed at coping with MSD at the workplace. Important components were learning by conversation and acting within the context of the environment. Each session had different topics. They lasted 2 hours; 1 hour and 15 minutes of didactics about knowledge from the topics and 45 minutes of discussion about solutions of work environment problems. Changes in the working environment were implemented after the sessions. The control groups: The control groups did not receive any special attention or information. |
|
| Outcomes | Measurements were made at baseline (1998) and 16 months after, with the following three main outcomes: Musculoskeletal symptoms (included musculoskeletal discomfort): The prevalence of musculoskeletal symptoms was assessed using Standard Nordic Questionnaire (SNQ) with modifications. Musculoskeletal symptoms were described as pain, discomfort or reduced mobility. The body parts examined were neck, shoulders, elbows, hands, upper neck, lower back, hips, knees and feet. Furthermore, the body part “head” was specially added to the bodily items. A five‐point scale (from 'never' to 'very often', instead of 'yes' and 'no') was used. Coping with musculoskeletal symptoms: An index of eleven coping strategy items was used. The questions concerned what the participants did when they experienced troublesome bodily pain or stiffness. The index had a three‐point scale ranging from 1 'seldom or never' to 3 'often'. The eleven scores were summarised to one score. Psychosocial work factors: A job content questionnaire (JCQ) was used to test psychosocial work factors such as job demands, job control and social support. It was a short Swedish version of the questionnaire, which was translated to Norwegian. The questionnaire consisted of 17 questions scored on a four‐point scale. |
|
| Notes | The project was initiated by the involved companies and funded by them. The planners, providers and assessors were having the same employer as the participants in the study. Additional information about the trial was found in two other publications (Morken 2000; Morken 2002b). First author was contacted for missing information and responded. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “All the shift groups were randomised at the group level into three types of intervention groups or control group A". According to first author randomisation was performed by drawing of lots, which is an adequate method of randomisation. However, control group B was not randomised. Despite this we score 'yes' since we are disregarding control group B in further analyses. |
| Allocation concealment? | Low risk | According to author the allocation to the different groups was performed prior to the intervention by researchers who did not know the workers in the aluminium plants. The researchers had no knowledge of the health condition or work conditions in the different shifts. In other words, they had no possibility to lead the shifts into groups that "fitted". Based on information from author, even if some details are lacking, we choose to consider the allocation adequately concealed. |
| Blinding? All outcomes ‐ participants? | High risk | It was not possible to blind the intervention to the participants. |
| Blinding? All outcomes ‐ providers? | High risk | Companies' physiotherapists, planned the study, developed the program, and provided the intervention. Hence, the personnel were not blinded. |
| Blinding? All outcomes ‐ outcome assessors? | High risk | Quote: “Physiotherapists from the occupational health services distributed and collected the questionnaires in special meetings at the plants”. Outcome assessors were most likely not blinded. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | Quote: “Many of the respondents were lost due to the matching procedure when matching the data of the pre‐intervention and the post‐intervention survey”. A number of 804 participants were lost to follow‐up, of which 713 were lost due problems with the matching procedure. This represents a drop‐out rate of 32‐ 39%, which is too high. However, additional analyses demonstrated that the lack of data from unmatched participants did not introduce any major bias. Hence, the score is 'yes'. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Information provided by author confirms that all randomised participants were analysed in the group to which they were allocated. |
| Free of selective reporting? | Low risk | The results are reported and the findings were not in favour of the intervention. Based on an overall impression we score 'yes' here. |
| Similarity of baseline characteristics? | Low risk | Control group B had a significant higher control and coping at baseline. They also had higher age, and more years of experience. However, since we are disregarding control group B we score 'yes' here. |
| Co‐interventions avoided or similar? | Low risk | Possible co‐interventions were similar in index groups and control groups. |
| Compliance acceptable? | Low risk | Quote: ”The participation in the session for each groups varied from 70% to 100%”. Compliance was acceptable. |
| Timing outcome assessments similar? | Low risk | Author has confirmed that the timing of the outcome assessment was similar in all groups. |
| Methods | The study is a randomised controlled trial using a cluster‐randomised design. The study had two intervention groups and one control group. Randomisation was done on group level using a spreadsheet program. The duration of the intervention period was eight weeks. The study took place in the Netherlands. The year the study was conducted is not known, however it had to be before 2003. | |
| Participants | The participants were computer workers from a large office organisation dealing with social security allowances. Twenty‐two office locations were included. Inclusion criteria were working at least four days a week, having computer work at least five hours a day, and having their own computer at work. Other inclusion criteria were having complaints in neck, shoulders, arms, wrists, hands and fingers, having current pain neck/upper extremities lasting more than 14 days, considering the complaints work‐related, and finally having age between 18‐50 years. Workers needing medical treatment according to judgement by physician were excluded. Also excluded were workers having other health problems, including medication that might influence behaviour at work. The number of employees requested to answer a short questionnaire was 12000. A total number of 1700 workers returned the questionnaire, of which 1000 workers were included in the study. The number of participants who returned the consent form and were randomised into groups was 268 participants, of which 219 participants completed the observation period and returned the final questionnaire. In intervention group 1 ‐ Breaks group (N=97), the mean age was 39 years, and there were 46 % males. In the interventions group 2 ‐ Breaks and exercise group (N=81,) the mean age was 42 years, and there were 66 % males. In the control group (N=90), the mean age was 37 year, and 43 % were males. MSD is described as self‐reported frequency and severity of pain in defined upper extremity regions (neck, shoulders, upper arms, forearms, wrists, hands and fingers). All groups had complaints about neck pain at baseline. According to information from author the prevalence of cumulative neck pain last week was 100%. |
|
| Interventions | Ergonomics of the workplace was checked before the intervention for all three groups and if necessary individually adjusted. In addition, all groups received a small booklet with general information on neck and upper limb disorders, as well as a neck and upper‐limb disorder risk test. Intervention group 1: Breaks. Rest breaks were introduced by a computer program (five minutes rest every 35 minutes and seven seconds rest every five minutes of computer use). The computer was blocked during the breaks. Intervention group 2: Breaks + exercises. This group received the same procedure of rest breaks as the other intervention group. In addition, they received four physical exercises of 45 seconds duration. Control group: Intervention was given in form of ergonomic adjustments of the work place and the receiving of the booklet was given. Besides that, no extra intervention was given. |
|
| Outcomes | Measurements were made three weeks before the intervention period and again after three months. The primary outcome was: Overall recovery from complaints. This was measured with a questionnaire with a seven‐point scale from 'complete recovery' to 'worse than ever before'. The secondary outcomes were : Frequency and severity of complaints: The frequency of complaints were measured by asking how often they felt discomfort or pain in their neck, shoulders, upper arms, elbows, forearms, wrists and hands or fingers during the previous week. The alternatives were 'no pain', '1 day', '2‐3 days' or '4‐7 days'. The severity of complaints was measured by asking the participants to rate it on a ten‐point scale from 1 'no complaints' to 10 'sever complaints'. Sick leave: This was measured with a questionnaire where the participants were asked if they had been on sick leave as a result of their complaints during the last three months. Productivity: This outcome was measured as mean number of computer key strokes a day. Accuracy rate was computed using this equation: Accuracy rate = 1‐ (number of backspace + delete key strokes) / total number of key strokes. Computer usage was recorded online. |
|
| Notes | Since physical exercises are outside the scope of this review, we disregard this intervention in analyses. First and second author was contacted for missing information, but could not be reached in this phase of the review process. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “A randomisation procedure in a spreadsheet program was used that randomly assigned each location on a figure between 1 and 3”. This is an adequate method of cluster randomisation. |
| Allocation concealment? | High risk | Since no information about concealment of allocation is given in the article, we have no reason to believe that concealment was performed adequately. Neither first nor second author could be reached to clarify this matter in this phase of the process. |
| Blinding? All outcomes ‐ participants? | High risk | As the intervention consisted of breaks or breaks and exercise versus no intervention, blinding of participants was not possible. |
| Blinding? All outcomes ‐ providers? | High risk | Blinding of care providers being in contact with the participants is not described. However, care providers could not have been blinded when performing adjustments of the workplace. |
| Blinding? All outcomes ‐ outcome assessors? | High risk | The outcome assessor is not stated, nor his/hers blinding status. However, we assume if the outcome assessors were blinded, it would have been reported. Neither first nor second author could be reached to clarify this matter. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | Out of 268 participants at baseline, 219 completed the study at three months follow‐up. This gives a drop‐out rate of 18%, which is acceptable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | Even though performing an intention‐to‐treat analysis is not stated explicitly, we score 'yes' here since no changes of participants between groups were done in the analyses. |
| Free of selective reporting? | Low risk | Since all outcomes were reported, there is no reason to suspect selective outcome reporting. |
| Similarity of baseline characteristics? | High risk | Intervention group 2 had 66% men, compared to 43% and 46% for control group and intervention group 1 respectively. Hence, all the groups were not similar at baseline. |
| Co‐interventions avoided or similar? | Low risk | Possible co‐interventions are not reported. However, there is reason to believe that possible co‐interventions would have been similar in all groups. |
| Compliance acceptable? | Low risk | Quote: According to the answers in the general questionnaire, 74% of the participants performed the exercises most of the time. According to the questions posed after each rest break; all the exercises were performed in 78% of all rest breaks...”. Compliance to exercises (intervention group 2) was fairly good. When it comes to compliance to rest breaks (intervention group 1), the computer was blocked during breaks, hence compliance for this group is assumed to have been better. To conclude, compliance was acceptable in all groups. |
| Timing outcome assessments similar? | Low risk | All groups were assessed simultaneously. |
| Methods | The study is a randomised controlled trial using a block‐randomisation design consisting of two groups. Both groups received an intervention. The intervention period lasted for four weeks. The study was performed in the years 2003 to 2005 in the Netherlands (area of Enschede) and in Sweden area of Goteborg. | |
| Participants | Computer workers like job counsellors and medical secretaries were approached by telephone and announcements, and sent a screening questionnaire. To be included in the study the participants had to work at least 20 hours a week and have had perpetuating work‐related complaints in the neck and/or shoulder region for at least 30 days during the last year. Excluded were participants who reported pain in more than three body regions, who suffered from severe arthrosis or joint disorders, who were using muscle relaxants, or if they reported other complaints in the upper extremity not related to computer work. The participants were all female workers over 45 years old. Mean age was 52 years in intervention group 1 (N=42) and 50.7 years in the intervention group 2 (N=37). Mean working hours per week was 32.8 in both groups. Participants were recruited between March 2003 and June 2005. Total number of participants recruited is not stated, but 79 workers met the inclusion criteria, of which 65 participants completed the study at six months follow‐up. Forty‐one participants were recruited in Sweden, while the remaining 38 participants were recruited in the Netherlands. MSD was assessed as pain in neck, shoulder and upper back for at least 30 days during last year. The amount of participants with complaints and trouble in neck last year (measured from baseline) was 92.9% in the intervention group 1 and 91.9% in the intervention group 2. |
|
| Interventions |
Intervention group 1: Myofeedback and ergonomic counselling.The participants received ambulant myo‐feedback training combined with ergonomic counselling. Immediately after baseline, participants were given a myo‐feedback device and they were explained the working mechanism and background of the myo‐feedback training. They were instructed to respond to the feedback by relaxation. The participants wore the device for four weeks, for at least eight hours a week, (distributed over two hours a day and two days a week as a minimum), while performing their regular work. During the weekly visits by their therapist the electronic data from last week were scrutinized and discussed to give the participants insight in their relaxation patterns and to identify possible situations of concern. The content of ergonomic counselling intervention is described below. Intervention group 2: Ergonomic counselling. Participants received four weeks of intervention during which they kept a diary of activities and pain intensity scores. In this period they were visited weekly by their therapist. The first visit comprised an ergonomic workplace investigation by means of the risk inventory. This checklist contained questions to evaluate work tasks, working hours, work load, work station, and working methods. Based on the outcome, possible improvements were discussed with the participants. With regard to the work station, the focus was primarily on modifying the existing work station rather than providing new equipment. The remaining visits were used to further discuss the ergonomic aspects, the consequences of possible ergonomic adjustments etc. This was done according to a manual to guarantee a uniform intervention. |
|
| Outcomes | Measurements were performed at baseline, immediately after intervention, and at three months and six months after the intervention. The outcomes were: Pain intensity: Pain intensity in the neck, shoulder (left and right), and upper back at time of the measurement was assessed by means of four Visual Analogue Scales. Participants were instructed to rate their subjectively experienced level of pain intensity at that moment for each body region. Pain intensity was scored on a ten cm scale ranging from 'no discomfort at all' to 'as much discomfort as possible'. Disability: The level of subjectively experienced disability was assessed with the Pain Disability Index, a self‐rating scale that measures the impact of pain on the abilities to participate in life activities. Disability was scored on an eleven‐point scale ranging from 'not disabled' to 'fully disabled'. |
|
| Notes | Additional information about the Swedish branch of the study was found in another publication (Larsman 2009). We were able to reach the second author, who respond to our questions concerning missing information. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “Block‐randomisation was used to assign subjects to either Mbf or Ec. When a new group of subjects started the intervention, half of them were assigned to Mfb and half of them were assigned to Ec”. (MbF is intervention group 1 and Ec is intervention group 2). When asked, second author informs that randomisation was performed using a random function in Excel. Using a computer random number generator is an adequate method of sequence generation. |
| Allocation concealment? | Unclear risk | Despite thorough explanation from second author, we are not convinced that the allocation was adequately concealed in the Dutch branch of the study. |
| Blinding? All outcomes ‐ participants? | High risk | Quote: "The character of the intervention made blinding of the therapists and the subjects to the intervention impractical. To prevent from information bias, subjects were informed that the aim of the study was to compare the effects of two interventions and that there was no evidence favouring one of these interventions”. Participants were not blinded to the intervention. |
| Blinding? All outcomes ‐ providers? | High risk | Care providers were not blinded to the intervention. |
| Blinding? All outcomes ‐ outcome assessors? | High risk | When asked, the second author confirms that in Sweden the outcome assessors never met the participants. However, in the Dutch branch of the study the outcome assessor and care provider was the same person. Hence, all outcome assessors were not blinded to the intervention. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | According to diagram 1 in the article, 79 participants were included in the study and 65 participants completed the study at six months follow‐up. This gives a drop‐out rate of 18%, which is acceptable. |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | According to second author all randomised participants were analysed in the group to which they were allocated. |
| Free of selective reporting? | Low risk | All outcomes are reported thoroughly. Besides, both groups were given an occupational intervention and no differences were found between the groups. Hence, there is no reason to suspect selective reporting. |
| Similarity of baseline characteristics? | Low risk | Quote: “Despite extensive standardisation, the recruitment of subjects in two different study groups (Sweden and the Netherlands) resulted in heterogeneity of the subject populations with regard to age, working hours, seniority, and working posture. To correct for this, the factor study group was considered a confounder need to control for during analyses”. Since the baseline imbalance was corrected for in analyses, we consider this criterion to be met. |
| Co‐interventions avoided or similar? | Low risk | When asked, the second author confirms that co‐interventions were equally distributed between the two intervention groups. |
| Compliance acceptable? | Low risk | Second author writes that in intervention group 1 the participants had to wear the myo‐feedback device at least eight hours a week for four weeks; in other words they had to comply. The participants in intervention group 2 were considered to comply if they took part in all weekly meetings, and all participants did so. Hence, compliance was acceptable in both groups. |
| Timing outcome assessments similar? | Low risk | According to diagram 1 in the article, the timing of outcomes assessment was identical in the two groups. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aarås 1999 | Method of randomisation is not reported. When asked, first author writes that every second participant was allocated to the same group as soon as the questionnaire reached the medical department. Allocation by availability of participants is not an adequate method of randomisation. Hence, the study is not an RCT. |
| Arnetz 2003 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50% at baseline. The intervention group had a 27.7% prevalence of neck pain, the control group had 20.8%. |
| Borgchrevink 1998 | Excluded due to type of participants: 25 % of the included not working (student, housewives, militaries) |
| Brisson 1999 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50%. In total the prevalence of neck pain at baseline was 12.8%. |
| Bultmann 2009 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50%. The total prevalence of neck pain at baseline was 18.6%. |
| Cook 2004 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50% at baseline.The prevalence of discomfort in intervention group was 21%. In the control group the prevalence was 18%. |
| DeKraker 2008 | Excluded due to type of participants: Information about neck pain at baseline lacking. Main author contacted. |
| Greene 2005 | Randomisation it not reported in the article. When asked, author writes that assignment of participants to groups occurred in an alternating fashion; one participant to the control group and the next to the interventions group. This is not an adequate method to ensure random sequence generation. In addition, author writes that a couple of participants were purposely assigned to group allocation. |
| Haldorsen 1998 | Excluded due to lack of workplace component in the intervention. Main author contacted. |
| Haldorsen 2002 | Excluded due to lack of workplace component in the intervention. Main author contacted. |
| Henning 1997 | Excluded due to type of participants: Information about neck pain at baseline lacking. |
| Jensen 2005 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50% at baseline. The prevalence of neck pain varied from 26‐50% within the four groups. |
| Li‐tsang 2008 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50% at baseline. The intervention group had a prevalence of 18.8%, and the control group had a prevalence of 25.8%. |
| Meijer 2006 | Excluded due to dealing with pain in upper extremities, not neck pain. |
| Peper 2003 | Excluded due to type of participants: Information about neck pain at baseline lacking. |
| Rempel 2006 | Excluded due to type of participants: Information about neck pain at baseline lacking. Main author contacted. |
| Skouen 2006 | Excluded due to lack of workplace component in the intervention. Main author contacted. |
| Veiersted 2008 | Excluded due to type of participants: Proportion of included in the study with neck pain below 50% at baseline. The intervention group had a prevalence of 56% (N=18), and the control group (N=20) had a prevalence of 40%. |
Contributions of authors
The lead review author (RWA) initiated and planned the review, and administrated the review process.
One review author (RWA) planned the search strategy and two review authors (RWA and KAH) undertook the search the first time. Updated searches were done by the Cochrane Back Review Group's Trials Search Co‐ordinator, Rachel Couban.
Two review authors, and two assistant scientists participated in the decision‐making process regarding inclusion and exclusion of trials (RWA, KAH, BHS, KLE).
One author developed the inclusion/exclusion‐ and quality assessment standardised forms (RWA). Eight review authors participated in the data extraction and assessment of risk of bias of the ten included studies, constituting four reading couples (SM+RWA), (AM+KAH), (HT+CR) and (TL+ML). One author performed quality assurance of the risk of bias assessment of the included studies, and collected missing information from the trials' first author (HT). One review author did a qualitative content analysis, to identify the interventions in the studies, and sorted these results according to the ICF (RWA). One review author collected the result data from the authors of the included studies (TL). Another author conducted all the analyses of treatment effects, in line with the ICF‐classification of the interventions (RWA).Two authors conducted the GRADE analysis (RWA, HT).
The lead review author (RWA) wrote drafts of the review and sent them to all co‐authors and to our mentor, Andrew Oxman and advisor, Jos Verbeek for comment and input.
Sources of support
Internal sources
PreSenter, International Research Institute of Stavanger (IRIS), Norway.
Bergen University College, Norway.
Nordic Ministries`Nordic School of Public Health, Sweden.
Division of Insurance Medicine, Dep. of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden.
Oslo University hospital, Department of Physical Medicine and Rehabilitation, Norway.
External sources
Norwegian Research Counsil, The Oil and Gas Program: Health, Safety and Environment, Norway.
Declarations of interest
None known.
New
References
References to studies included in this review
- Bernaards CM, Ariens GAM, Knol DL, Hildebrandt VH. The effectiveness of a work style intervention and a lifestyle physical activity intervention on the recovery from neck and upper limb symptoms in computer workers. Pain 2007;132:142‐53. [DOI] [PubMed] [Google Scholar]
- Fostervold KI, Aarås A, Lie I. Work with visual display units: Long‐term health effects of high and downward line‐of‐sight in ordinary office environments. International Journal of Industrial Ergonomics 2006;36:331‐43. [Google Scholar]
- Haukka E, Leino‐Arjas P, Viikari‐Juntura E, Takala EP, Malmivaara A, Hopsu L, et al. A randomised controlled trial on whether a participatory ergonomics intervention could prevent musculoskeletal disorders. Occupational and Environmental Medicine 2008;65:849‐56. [DOI] [PubMed] [Google Scholar]
- Hedge A, Morimoto S, McCrobie D. Effects of keyboard tray geometry on upper body posture and comfort. Ergonomics 1999;42(10):1333‐49. [DOI] [PubMed] [Google Scholar]
- Horneij E, Hernborg B, Jensen I, Ekdahl C. No significant differences between intervention programmes on neck, shoulder and low back pain: A prospective randomized study among home‐care personnel. J Rehabil Med 2001;33:170‐6. [PubMed] [Google Scholar]
- Kamwendo K, Linton SJ. A controlled study of the effect of neck school in medical secretaries. Scandinavian Journal of Rehabilitation Medicine 1991;23:143‐52. [PubMed] [Google Scholar]
- Ketola RK, Toivonen R, Hakkanen M, Luukkonen R, Takala EP, Viikari‐Juntura E, et al. Effects of ergonomic intervention in work with video display units. Scandinavian Journal of Work, Environment & Health 2002;28(1):18‐24. [DOI] [PubMed] [Google Scholar]
- Morken T, Moen B, Riise T, Hauge SHV, Holien S, Langedrag A, et al. Effects of a training program to improve musculoskeletal health among industrial workers‐ effects of supervisors role in the intervention. International Journal of Industrial Ergonomics 2002;30:115‐27. [Google Scholar]
- Heuvel SG, Looze MP, Hildebrandt VH, The KH. Effects of software programs stimulating regular breaks and exercises on work‐related neck and upper‐limb disorders. Scandinavian Journal of Work, Environment & Health 2003;29(2):106‐16. [DOI] [PubMed] [Google Scholar]
- Voerman GE, Sandsjo L, Vollenbroek‐Hutten MMR, Larsman P, Kadefors R, Hermens HJ. Effects of ambulant myofeedback training and ergonomic counselling in female computer workers with work‐related neck‐shoulder complains: A randomized controlled trial. Journal of Occupational Rehabilitation 2007;17:137‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
- Aarås A, Ro O, Thorsen M. Can a More Neutral Position of the Forearm When Operating a Computer Mouse Reduce the Pain Level for Visial Display Unit Operators? A Prospective Epidemiological Intervention Study. International Journal of Human‐Computer Interaction 1999;11(2):79‐94. [Google Scholar]
- Arnetz BB, Sjögren B, Rydēhn B, Meisel R. Early workplace intervention for employees with musculoskeletal ‐related absenteeism: A prospective controlled intervention study. Journal of occupational and environmental medicine 2003;45(5):499‐506. [DOI] [PubMed] [Google Scholar]
- Borchgrevink GE, Kaasa AA, McDonagh D, Stiles TC, Haraldseth O, Lereim I. Acute treatment of whiplash neck sprain injuries. Spine 1998;23(1):25‐31. [DOI] [PubMed] [Google Scholar]
- Brisson C, Montreuil S, Punnett L. Effects of an ergonomic training program on workers with video display units. Scandinavian Journal of Work Environment and Health 1999;25(3):255‐63. [DOI] [PubMed] [Google Scholar]
- Bultmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. Journal of Occupational Rehabilitation 2009;19(1):81‐93. [DOI] [PubMed] [Google Scholar]
- Cook C, Burgess‐Limerick R. The effect of forearm support on musculoskeletal discomfort during call centre work. Ergonomics 2004;35:337.342. [DOI] [PubMed] [Google Scholar]
- Kraker H, Korte EM, Mil FL, Bongers PM. The effect of a feedback signal in a computer mouse on hovering behaviour, productivity, comfort and usability in a field study. Ergonomics 51;2:140‐55. [DOI] [PubMed] [Google Scholar]
- Greene BL, DeJoy DM, Olejnik S. Effects of an ergonomic training program on risk exposure, worker beliefs, and symptoms in computer use. Work 2005;24:41‐52. [PubMed] [Google Scholar]
- Haldorsen EMH, Kronholm K, Skouen JS, Ursin H. Multimodal Cognitive Behavioral Treatment of patients sick‐listed for musculoskeletal pain a randiomized controlled study. Scandinavian Journal of Rheumatology 1998;27:16‐25. [DOI] [PubMed] [Google Scholar]
- Håland Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment and extensive multidisciplinary treatment for long‐term sick‐listed employees with musculoskeletal pain. Pain 2002;95:49‐63. [DOI] [PubMed] [Google Scholar]
- Henning RA, Jacques P, Kissel GV, Sullivan AB, Alteras‐Webb SM. Frequent short rest breaks from computer work: effects on productivity and well‐being at two field sites. Ergonomics 1997;40(1):78‐91. [DOI] [PubMed] [Google Scholar]
- Jensen IB, Bergström G, Ljungquist T, Bodin L. A 3‐year follow‐up of a multidisciplinary rehabilitation programme for back and neck pain. Pain 2005;115:273‐83. [DOI] [PubMed] [Google Scholar]
- Li‐Tsang CW, Li EJ, Lam CS, Hui KY, Chan CC. The effect of a job replacement and support program for workers with musculoskeletal injuries: a randomized control trial (RCT) study. Journal of Occupational Rehabilitation 2008;18(3):299‐306. [DOI] [PubMed] [Google Scholar]
- Meijer EM, Sluiter KJ, Heyma A, Sadiraj K, Frings‐Dresen MHW. Cost‐effectiveness of multidisciplinary treatment in sick‐listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one‐year follow‐up. International Archives of Occupational and Environmental Health 2006;79:654‐64. [DOI] [PubMed] [Google Scholar]
- Peper E, Wilson VS, Gibney KH, Huber K, Harvey R, Shumay DM. The integration of electromyography (SEMG) at the workstation: assessment, treatment and prevention of repetitive strain injury (RSI). Applied Psychophysiology and Biofeedback 2003;28(2):167‐82. [DOI] [PubMed] [Google Scholar]
- Rempel DM, Krause N, Goldberg R, Benner D, Hudes M, Goldner GU. A randomised controlled trial evaluating the effects of two workstation interventions on upper body pain and incident musculoskeletal disorders among computer operators. Occupational and Environmental Medicine 2006;63:300‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skouen JS, Grasdal A, Haldorsen EMH. Return to work after comparing outpatient multidisciplinary treatment programs versus treatment in general practice for patients with chronic widespread pain. European Journal of Pain 2006;10:145‐52. [DOI] [PubMed] [Google Scholar]
- Veiersted KB, Gould KS, Osteras N, Hansson GA. Effects of an intervention addressing working technique on the biomechanical load of the neck and shoulders among hairdressers. Applied Ergonomics 2008;39(2):183‐90. [DOI] [PubMed] [Google Scholar]
Additional references
- Aas RW, Elliningsen KL, Lindøe P, Moller A. Leadership qualities in the return to work process: A content analysis. Journal of Occupational Rehabilitation 2008;18(4):335‐46. [DOI] [PubMed] [Google Scholar]
- Aas RW. Fast return. Evidence‐based rehabilitation of sick listed [Raskt tilbake. Kunnskapsbasert rehabilitering av sykmeldte]. [Raskt tilbake. Kunnskapsbasert rehabilitering av sykmeldte] Norwegian. Oslo: Gyldendal Akademisk, 2009. [Google Scholar]
- Aas RW, Thingbø C, Holte KA, Lie K, Lode IA. On long term sick leave due to musculoskeletal diseases and disorders. Experiences of work demands. Work. A journal of Prevention, Assessment and Rehabilitation 2011;(In press). [DOI] [PubMed] [Google Scholar]
- Anema JR, Steenstra IA, Bongers PM, Vet HC, Knol DL, Loisel P, Mechelen W. Multidisiplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine 2007;32(3):291‐98. [DOI] [PubMed] [Google Scholar]
- Ariens GA, Mechelen W, Bongers PM, Bouter LM, Wal G. Physical risk factors for neck pain. Scand J Work Environ Health 2000;26(1):7‐19. [DOI] [PubMed] [Google Scholar]
- Ariens GA, Bongers PM, Hoogendoorn WE, Houtman IL, Wal G, Mechelen W. High quantitative job demands and low coworker support as risk factors for neck pain: results of a prospective cohort study. Spine 2001;26(17):1896‐901. [DOI] [PubMed] [Google Scholar]
- Bergstrom G, Bodin L, Bertilsson H, Jensen IB. Risk factors for new episodes of sick leave due to neck or back pain in a working population. A prospective study with an 18‐month and a three‐year follow‐up. Occupational and Environmental Medicine 2007;64:279‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernaards CM, Ariëns GA, Hildebrandt VH. Study protocol. The (cost‐) effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on the recovery from neck and upper limb symptoms in computer workers. BMC Musculoskeletal disorders 2006;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernaards CM, Ariëns GA, Simons M, Knol DL, Hildebrandt VH. Improving work style behaviour in computer workers with neck and upper limb symptoms. Journal of Occupational Rehabilitation 2008;18(1):87‐101. [DOI] [PubMed] [Google Scholar]
- Bongers PM, Kremer AM, ter Laak J. Are psychosocial factors risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist? A review of the epidemiological literature. Am J Ind Med 2002;41(5):315‐42. [DOI] [PubMed] [Google Scholar]
- Bongers PM, Ljmker S, Heuvel S, Blatter BM. Epidemiology of work related neck and upper limb problems: psychosocial and personal risk factors (part I) and effective interventions from a bio behavioural perspective (part II). Journal of Occupational Rehabilitation 2006;16:279‐302. [DOI] [PubMed] [Google Scholar]
- Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of non‐specific neck pain: a systematic review. Pain 1998;77(1):1‐13. [DOI] [PubMed] [Google Scholar]
- Boyle EP, Côté PD, Grier ARD, Cassidy JDD. Examining Vertebrobasilar Artery Stroke in Two Canadian Provinces. Spine 2008;33:170‐5. [DOI] [PubMed] [Google Scholar]
- Brage S, Fleten N, Knudsrod OG, Reiso H, Ryen A. Norwegian Functional Scale ‐ a new instrument in sickness certification and disability assessments. Tidsskr Nor Laegeforen 2004;124(19):2472‐4. [PubMed] [Google Scholar]
- Carroll LJ, Hogg‐Johnson S, Cote P, van d, V, Holm LW, Carragee EJ, Hurwitz EL, Peloso PM, Cassidy JD, Guzman J, Nordin M, Haldeman S. Course and prognostic factors for neck pain in workers: results of the Bone and Joint Decade 2000‐2010 task Force on neck pain and its Associated disorders. Spine 2008;33(4):93‐100. [DOI] [PubMed] [Google Scholar]
- Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta‐analysis of workplace physical activity interventions. AM J Prev Med 2009;37(4):330‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW. Place‐than‐train: An alternative service paradigm for persons with psychiatric disabilities. Clinical Psychological Science Practice 2001;8:334‐49. [Google Scholar]
- Côté PD, Velde GD, Cassidy JDD, Carroll LJP, Hogg‐Johnson SP, Holm LWD, et al. The Burden and Determinants of Neck Pain in Workers: Results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(S4):S60‐S74. [DOI] [PubMed] [Google Scholar]
- Egan M, Bambra C, Petticrew M, Whitehead M. Reviewing the evidence on complex social interventions: Appraising implementation in systematic review of the health effects of organisational‐level workplace interventions. Journal of epidemiology and community health 2009;63(1):4‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elders LAM, Burdorf A. Workplace interventions. Occupational Environmental Medicine 2004;61:287‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadyl JK, McPherson M. Approaches to vocational rehabilitation after traumatic brain injury: A review of the evidence. Journal of head trauma Rehabilitation 2009;24(3):195‐212. [DOI] [PubMed] [Google Scholar]
- Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J, and IWH review team. Workplace‐based return to work interventions: A systematic review of the quantitative literature. Journal of Occupational Rehabilitation 2005;15(4):607‐31. [DOI] [PubMed] [Google Scholar]
- Frank JW, Brooker AS, DeMaio SE, Kerr MS, Maetzel A, Shannon HS, et al. Disability resulting from occupational low back pain. Part II: What do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine 1996;21(24):2918‐29. [DOI] [PubMed] [Google Scholar]
- Furlan AD, Pennick V, Bombardier C, van Tulder MW on behalf of the Editorial Board of the Cochrane Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34(18):1929‐1941. [DOI] [PubMed] [Google Scholar]
- Grotle M, Brox AS, Vollestad NK. Functional status and disability questionnaires: What do they assess?. Spine 2005;30(1):130‐140. [PubMed] [Google Scholar]
- Guzman J, Hurwitz EL, Caroll LJ, Haldeman S, Côtė P, Carragee EJ, Peloso PM, Velde G, Holm LW, Hogg‐Johnson S, Nordin M, Cassidy JD. A New Conceptual Model of Neck Pain. Linking Onset, Course, and Care: The Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S14‐S23. [DOI] [PubMed] [Google Scholar]
- Hansson EK, Hansson TH. The costs for persons sick‐listed more than one month because of low back or neck problems. A two‐year prospective study of Swedish patients. Europ Spine J 2005;14:337‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haukka E, Arja PL, Solovieva S, Ranta R, Viikari‐Juntura E, Riihimäki H. Co‐occurrence of musculoskeletal pain among female kitchen workers. International Arch Occup Environ Health 2006;80:141‐48. [DOI] [PubMed] [Google Scholar]
- Heerkens YF, Engels J, Kupier C, Gulden J, Oostendorp RAB. The use of the ICF to describe work related factors influencing the health of employees. Disability and Rehabilitation 2004;26(17):1060‐6. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.0 [updated February 2008]. The Cochrane Collaboration (www.cochrane.org/resources/handbook/index.htm)2008.
- Hill J, Lewis M, Papageorgiou AC, Dziedzic K, Croft P. Predicting persistent neck pain : a 1‐year follow‐up of a population cohort. Spine 2004;29(15):1648‐54. [DOI] [PubMed] [Google Scholar]
- Hogg‐Johnson SP, Velde GD, Carroll LJP, Holm LWD, Cassidy JDD, Guzman JMMF, et al. The Burden and Determinants of Neck Pain in the General Population: Results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S39‐S51. [DOI] [PubMed] [Google Scholar]
- Hush JM, Maher CG, Refshauge KM. Risk factors for neck pain in office workers: A prospective study. BMJ Musculoskeletal Disorders 2006;7:81. [DOI: 10.1186/1471-2474-7-81] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamwendo, K. Neck and Shoulder Disorders in Secretaries. Prevalence, Risk Factors and Neck School Intervention. Sweden: University of Lund, 1991. [Google Scholar]
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD002194] [DOI] [PubMed] [Google Scholar]
- Kay TM, Gross A, Goldsmith CH, Hoving JL, Brønfort G. Exercises for mechanical neck disorders. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004250.pub3] [DOI] [PubMed] [Google Scholar]
- Kitson AL, Rycroft‐Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiSH framework: theoretical and practical challenges. Implementation science 2008;3(1). [DOI: 10.1186/1748-5908-3-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambeek LC, Bosmans JE, Royen BJ, Tulder MW, Mechelen W, Anema JR. Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial. British Medical Journal 2010;341. [DOI: 10.1136/bmj.c6414] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsman P, Sandsjö L, Kadefors R, Voerman G, Vollenbroek‐Hutten M, Hermens H. Prognostic Factors for Intervention Effect of Neck/Shoulder Symptoms Intensity and Disability among Female Computer Workers. Journal of Occupational Rehabilitation 2009;19:300‐11. [DOI: 10.1007/s10926-009-9186-z.] [DOI] [PubMed] [Google Scholar]
- Lau B, Knardal S. Perceived job insecurity, job predictability and health. J Occup Envirion Med 2008;50(2):172‐81. [DOI] [PubMed] [Google Scholar]
- Leyshon RT, Shaw LE. Using the ICF as a conceptual framework to guide ergonomic intervention in occupational rehabilitation. Work 2008;31(1):47‐61. [PubMed] [Google Scholar]
- Lidgren LM. Preface: Neck Pain and the Decade of the Bone and Joint 2000‐2010. Spine 2008;33(4S):S1‐S2. [DOI] [PubMed] [Google Scholar]
- Linton SJ. A review of psychological risk factors in back and neck pain. Spine 2000;25(9):1148‐56. [DOI] [PubMed] [Google Scholar]
- Loisel P, Durand MJ, Berthelette D, Vezina N, Baril R, Gagnon D. Disability prevention‐New paradigm of the management of occupational back pain. Disease Management & Health Outcomes 2001;9(7):351‐60. [Google Scholar]
- Morken T, Moen B, Riise T, Bergum O, Bua L, Vigeland HS, et al. Prevalence of musculoskeletal symptoms among aluminium workers. Occupational. Medicine 2000;50(6):414‐21. [DOI] [PubMed] [Google Scholar]
- Morken T, Riise T, Moen B, Bergum O, Vigeland Hauge SH, Holien S, et al. Frequent musculoskeletal symptoms and reduced health‐related quality of life among industrial workers. Occupational Medicine 2002;52(2):91‐8. [DOI] [PubMed] [Google Scholar]
- Nachemson AL, Waddell G, Nordlund AL. Epidemiology for neck and low back pain. In: Nachemson AL, Jonsson E editor(s). Neck and back pain: The scientific evidence of causes, diagnosis and treatment. Philadelphia: Lippincott Williams & Wilkins, 2000:165‐88. [Google Scholar]
- Nordlund A, Ekberg K. Self reported musculoskeletal symptoms in the neck/shoulders and/or arms and general health (SF‐36): Eight year follow up of a case‐control study. Occup Environ Med 2004;61(3):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwegian Government. Letter of intent regarding a more inclusive working life 2006‐2009. The Ministry of Labour and Inclusion2005.
- Pehkonen I, Takala E‐P, Ketola R, Viikari‐Juntura E, Leino‐Arjas P, Hopsu L, et al. Evaluation of a participatory ergonomic intervention process in kitchen work. Applied Ergonomics 2009;40:115‐23. [DOI] [PubMed] [Google Scholar]
- Punnett L, Wegman DH. Work‐related musculoskeletal disorders: the epidemiologic evidence and the debate. Journal of Electromyograpy and Kinesiology 2004;14(1):13‐23. [DOI] [PubMed] [Google Scholar]
- Schonstein E, Kenny DT, Keating JL, Koes BW. Work conditioning, work hardening and functional restoration for workers with back and neck pain. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD001822] [DOI] [PubMed] [Google Scholar]
- Staal JB, Hlobil H, Tulder MW, Koke AJ, Smid T, Mechelen W. Return‐to‐work interventions for low back pain: a descriptive review of contents and concepts of working mechanisms. Sports Med 2002;32(4):251‐67. [DOI] [PubMed] [Google Scholar]
- Central statistics on sickness absence. Labour Market Statistics Division, Statistics Norway2004.
- Bureau of Labor Statisitics. Lost work‐time injuries and illnesses: Characteristics and resulting days away from work, 2003. Washington D.C.: United States Department of Labor, 2004. [Google Scholar]
- Windt DA, Thomas E, Pope DP, Winter AF, Macfarlane GJ, Bouter LM, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med 2000;57(7):433‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eerd D, Brewer S, Amick BC, Irvin E, Daum K, Gerr G, et al. Workplace interventions to prevent musculoskeletal and visual symptoms and disorders among computer users: A systematic review. Institute for Work & Health, Toronto, Canada2006. [DOI] [PubMed]
- Oostrom SH, Driessen MT, Vet HCW, Franche RL, Shonstein E, Loisel P, et al. Workplace interventions for preventing work disability. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
- Verbeek J, Husman K, Dijk F, Jauhiainen M, Pasternack I, Vainio H. Building an evidence base for occupational health interventions. Scandinavian Journal of Work Enviroment and Health 2004;30(2):164‐8. [PubMed] [Google Scholar]
- Westmorland MG, Buys N. A comparison of disability management practices in Australian and Canadian workplaces. Work 2004;23:31‐41. [PubMed] [Google Scholar]
- World Health Organization. International classification of functioning, disability and health (ICF). 2001. Available at: http://www.who.int/classifications/icf/en/ (accessed August 23, 2005).


