Abstract
Sister Mary Joseph nodule or Sister Mary Joseph Sign refers to a palpable nodule bulging into the umbilicus as a result of metastasis of a malignant cancer in the pelvis or abdomen. A rare case of Sister Mary Joseph nodule, manifesting as ascites, cachexia and bleeding per rectum, is presented without any primary tumor despite extensive search for the same.
Keywords: Umbilical Nodule, Metastasis, FNAC
Sister Mary Joseph nodule or Sister Mary Joseph Sign refers to a palpable nodule bulging into the umbilicus as a result of metastasis of a malignant cancer in the pelvis or abdomen. Gastrointestinal malignancies account for about half of the underlying sources (gastric, colonic, pancreatic cancer), gynecologic (ovarian, uterine cancer), unknown primary tumors and rarely bladder or respiratory malignancies cause umbilical metastasis. Mechanism of spread of cancer to the umbilicus is unknown but proposed mechanisms include direct transperitoneal spread via lymphatic running along the obliterated umbilical vein, hematogenous spread or via remnant structures like the falciform ligament, median umbilical ligament or a remnant of the umbilical duct. Sister Mary Joseph nodule is associated with multiple peritoneal metastases and signifies a poor prognosis. A rare case of Sister Mary Joseph nodule, manifesting as ascites, cachexia and bleeding per rectum, is presented without any primary tumor despite extensive search for the same.
Case Report
A 75 year old woman presented to the emergency room with a seven months history of increased fatigability, loss of appetite, weight loss and progressive abdominal distension. On examination the patient was markedly pale, asthenic, dehydrated and febrile and had altered mental status. Her general physical examination revealed anemia and pedal edema without any lymphadenopathy. On inspection abdomen was distended, without any visible vessel, scar or sinus. A periumblical bluish violet swelling 5 cm in diameter was also noted (Figure 1). On palpation a firm liver edge 4 cm below the right costal margin with a hard periumblical swelling was also found. Percussion of the abdomen revealed ascitis with shifting dullness. Auscultation of the abdomen did not reveal any abnormality. Examination of the chest revealed a left sided pleural effusion. The cardiovascular system was normal except for a systolic flow murmur at the apex and base. Investigations revealed a low hemoglobin of 3%, microcytic hypochromic type with a reticulocyte count of 5% and no abnormal cells on peripheral blood smear. Kidney function tests, electrolytes, blood sugar, urine examination and septic screen (blood, urine and asitic fluid cultures) were normal. Liver function tests revealed hypoalbuminemia with normal enzyme and alkaline phosphatase levels. Ascites and pleural taps revealed a lymphocytic exudate without malignant cells and adenosine deaminase in a suspect range. CA-125 and CEA levels were normal. Ultrasound of the abdomen revealed ascites with an enlarged liver, normal pancreas, gall bladder, adnexae and no para-aortic lymphadenopathy. CT scan of the abdomen revealed thickened peritoneum studded with metastatic lesions. Upper and lower gastrointestinal endoscopy was normal. Fine needle aspiration cytology (FNAC) of the umbilical nodule done showed metastatic deposits of well-differentiated adenocarcinoma (Figure 2). A diagnosis of Sister Mary Joseph's nodule was made. Despite extensive search a primary could not be located. The patient succumbed to massive rectal bleeding and despite all measures could not be resuscitated.
Figure 1.

A visible periumblical bluish violet swelling suggestive of a Sister Mary Joseph nodule
Figure 2.
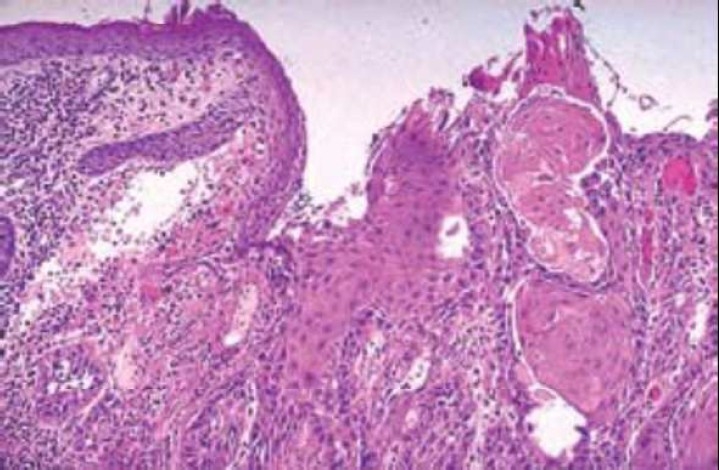
Metastatic deposits of a well differentiated adenocarcinoma documented by FNAC
Discussion
Umbilical tumors are relatively rare and can be classified as benign or malignant.1 Malignant tumors can be primary or metastatic tumors. Metastatic tumors arise from a variety of primary malignant tumors. The term “Sister Mary Joseph nodule” is used to describe a malignant umbilical tumor usually associated with advanced metastasizing intra-abdominal cancer and generally indicating a poor prognosis. This sign was first identified by Sister Mary Joseph (1856-1939) who as a surgical assistant to Dr William James Mayo drew attention to the presence of a hard umbilical nodule in a patient being prepared for surgery in 1928. Sir Hamilton Bailey coined the term “Sister Mary Joseph nodule” in the 11th edition of his textbook “Demonstrations of Physical Signs in Clinical Surgery” in 1949. The nodule usually presents as a firm, indurate often vascular swelling which may be fissured or ulcerated and may have serous, mucinous, purulent or bloody discharge. The nodule has been described as white, bluish violet and brownish red and is occasionally pruritic. It is usually irregular in shape, generally painless when palpated except if the overlying skin has ulcerated. It is typically less than 5 cm in diameter but occasionally enlarges enough to form a protruding tumor. Patients with Sister Mary Joseph nodule present with a number of clinical symptoms consistent with intra-abdominal cancer including epigastric pain, abdominal distension, weight loss, nausea, ascites and bleeding per rectum.2 The sign of Sister Mary Joseph nodule has been extensively described in literature. Its occurrence is uncommon and as a first sign of malignancy is rare. The evaluation of an umbilical mass should be directed by suspicion of its being a metastatic deposit keeping in mind its potential to be either a primary malignant umbilical lesion or a benign disease. In a patient with a known malignancy an umbilical mass represents a spread or seeding of the primary tumor and thus can influence therapeutic decision making.3 The most common origins of Sister Mary Joseph nodule are gastrointestinal (52%), gynecologic (28%), stomach (23%) and ovarian (16%) carcinomas. About 15-29% of all cases have an unknown origin (as depicted by the presented case) and 3% originate from the thoracic cavity. Primary tumors in many other sites like gall bladder, uterus, liver, endometrium, small intestine, fallopian tube, appendix, cervix, penis, prostrate, urinary bladder, breast, lung and kidneys have also been reported to cause Sister Mary Joseph nodules. Histology of the metastatic umbilical tumor usually reveals adenocarcinoma but rare reports of umbilical metastasis from sarcomas, mesotheliomas and melanomas have also been seen.2–4 CT Scan (abdomen and chest) and Fine Needle Aspiration Cytology (FNAC) of the tumor are invaluable in the diagnosis of Sister Mary Joseph nodule and help to exclude a primary benign umbilical neoplasm. In 14-33% of cases, umbilical metastases lead to the diagnosis of previously occult neoplasms.5 In 40% of patients with a known neoplasm the nodule was an early sign of relapse.6 Spread of metastatic carcinoma to the umbilical region has been hypothesized to occur by either contiguous spread of peritoneal cancer, hematogenous spread through arterial and venous systems or lymphatic spread (mainly pancreatic carcinoma) with extension along ligaments of embryonic origin (round ligament of liver, urachus, vitello intestinal duct reminant and the obliterated vitelline artery).6,7 The presence of a Sister Mary Joseph nodule verified histological signifies advanced metastatic carcinoma and a poor prognosis with a survival time of 10 months (range 2-17 months) and inoperability. Treatment of established Sister Mary Joseph nodule is palliative as wide excision, surgery and radiotherapy have all proved ineffective. Nevertheless a Sister Mary Joseph nodule is a time tested, honored clinical sign emphasizing the importance of a careful physical examination of the abdomen. It still remains an interesting and useful diagnostic tool in modern medicine.
Authors’ Contributions
MAK initially examined and admitted the patient. IHD examined, planned the work up, executed the investigative profile and wrote the manuscript. SHS and FAK collected the reference material. All authors have read and approved the content of final manuscript.
Footnotes
Conflict of Interests:
Authors have no conflict of interests.
References
- 1.Steck WD, Helwig EB. Tumors of the umbilicus. Cancer. 1965;18(7):907–15. doi: 10.1002/1097-0142(196507)18:7<907::aid-cncr2820180721>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 2.Urbano FL. Sister Joseph's nodule. (44).Hospital Physician. 2001;37(5):33–5. [Google Scholar]
- 3.Larentzakis A, Theodorou D, Fili K, Manataki A, Bizimi V, Tibishrani M, et al. Sister Mary Joseph's nodule: three case reports. Cases Journal. 2008;1:182. doi: 10.1186/1757-1626-1-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galvan VG. Sister Mary Joseph's nodule. Ann Intern Med. 1998;128(5):410. doi: 10.7326/0003-4819-128-5-199803010-00017. [DOI] [PubMed] [Google Scholar]
- 5.Majumdar B, Wiskind AK, Croft BN, Dudley AG. The Sister (Mary) Joseph nodule: its significance in gynecology. Gynecol Oncol. 1991;40(2):152–9. doi: 10.1016/0090-8258(91)90108-h. [DOI] [PubMed] [Google Scholar]
- 6.Srinivasan R, Ray R, Nijhawan R. Metastatic cutaneous and subcutaneous deposits from internal carcinoma. An analysis of cases diagnosed by fine needle aspiration. Acta Cytol. 1993;37(6):894–8. [PubMed] [Google Scholar]
- 7.Powell FC, Cooper AJ, Massa MC, Goellner JR, Su WP. Sister Mary Joseph's nodule: a clinical and histologic study. J Am Acad Dermatol. 1984;10(4):610–5. doi: 10.1016/s0190-9622(84)80265-0. [DOI] [PubMed] [Google Scholar]


