Abstract
Purpose
Tibio-femoral kinematics are clearly influenced by the bony morphology of the femur. Previous morphological studies have not directly evaluated relationships between morphology and knee kinematics. Therefore, the purpose of this study was to examine the relationship between distal femur bony morphology and in vivo knee kinematics during running. It was hypothesized that the posterior offset of the transcondylar axis would be related to the magnitude of anterior/posterior tibio-femoral translation and that the rotational angle of the transcondylar axis would be related to the magnitude of internal/external knee rotation.
Methods
Seventeen contralateral (uninjured) knees of ACL-reconstructed patients were used. Distal femoral geometry was analyzed from 3D-CT data by determining the anteroposterior location (condyle offset ratio—COR) and rotational angle (condylar twist angle—CTA) of the femoral transcondylar axis. Six degree-of-freedom knee kinematics were obtained during running using a dynamic stereo radiograph system. Knee kinematics were correlated with the femoral morphologic measures (COR and CTA) to investigate the influence of femoral geometry on dynamic knee function.
Results
Significant correlations were identified between distal femur morphology and knee kinematics. Anterior tibial translation was positively correlated with the condyle offset ratio (R2 = 0.41, P < 0.01). Internal tibial rotation was positively correlated with the condylar twist angle (R2 = 0.48, P < 0.01).
Conclusions
Correlations between knee kinematics and morphologic measures describing the position and orientation of the femoral transcondylar axis suggest that these specific measures are valuable for characterizing the influence of femur shape on dynamic knee function.
Level of evidence
III.
Keywords: Bony morphology, In vivo knee kinematics, Dynamic stereo radiograph (DSX) system, Transcondylar axis
Introduction
Knee kinematics are clearly influenced by bony morphology. Variation of femoral condyle morphology has been associated with anterior cruciate ligament (ACL) injury risk [9, 10, 19, 42] and is a factor for proper fitting of total knee arthroplasty (TKA) implants [8, 31]. Knee kinematics vary considerably between individuals during in vivo dynamic activity [48, 49], and it is reasonable to suggest that bony morphology might influence knee motion. However, little is known about how anatomic variation of the femur affects in vivo knee kinematics.
The transcondylar axis is the most common mechanical axis, which is set based on the bony geometry of the posterior condyles [6, 20, 24, 30, 34, 43, 48, 49, 51], and has been referred to as the “flexion facet center” or the “geometrical center axis” since it describes the axis of rotation (for unloaded cadaver knees) during the knee flexion of 10° or more [23]. This axis moves away from the center of flexion to the posterior in extension (less than 10° of flexion), when the flexion axis is aligned with the more anteriorly positioned “extension facet center”. This posterior shift of the transcondylar axis toward extension is associated with the anterior translation of the tibia relative to the femur [24]. Since the knee is typically near extension at heel strike during walking or running, this posterior shift would occur during a period of rapidly applied, high-magnitude loads, and the magnitude of the shift could have important implications for cartilage and ligament loading.
The second most common mechanical axis described for the distal femur is the transepicondylar axis, which runs through both medial and lateral epicondyles [10, 24, 29, 36, 37, 53]. Tibial rotation during flexion has similar trend of internal rotation based on both mechanical axes, but the range of tibial rotation is larger when calculated based on the transcondylar axis [24]. The condylar twist angle (CTA), defined as the angular difference between these two axes [52], varies considerably across individuals and may impact the magnitude of knee rotation.
The effects of the mechanical axes position and angle on functional knee kinematics should be evaluated during physiologically relevant loading. Dynamic stereo radiograph (DSX) can provide high-accuracy in vivo tibio-femoral kinematics during dynamic and functional activities [47–49] and is therefore well suited for this application.
The goals of this study were to examine the anteroposterior location and the rotational angle of the transcondylar axis within the femur and to compare it to in vivo knee kinematics during full weight-bearing dynamic activity for uninjured limbs. It was hypothesized that the posterior offset of the transcondylar axis would be related to the magnitude of anterior/posterior tibio-femoral translation and that the angular difference between the transcondylar and transepicondylar axes would be related to the magnitude of internal/external knee rotation.
Materials and methods
Data already available from a previous IRB-approved ACL reconstruction study were employed for this analysis. Computed tomography (CT) scans and knee kinematics were obtained for the contralateral (uninjured) knees of seventeen ACL reconstruction patients (35 ± 12 years; 9 men and 8 women). CT scans included high-resolution slices from 10 cm above to 10 cm below the joint line, along with single slices through femoral head and ankle joint to establish long bone axes. As described elsewhere and reviewed briefly below, the knee CT scans were reconstructed into three-dimensional (3D) bone models of the tibia and femur for morphological measurements, and the location and the rotational angle of the femoral transcondylar axis were measured by 3D-CT analysis. The tibial anterior/posterior translation and internal/external rotation during downhill running were measured using the DSX system, as previously reported [47–49].
3D-CT measurements
The 3D-CTs of the femur were segmented and analyzed using 3D imaging software (Geomagic Studio 10, Geomagic Inc., Research Triangle Park, NC).
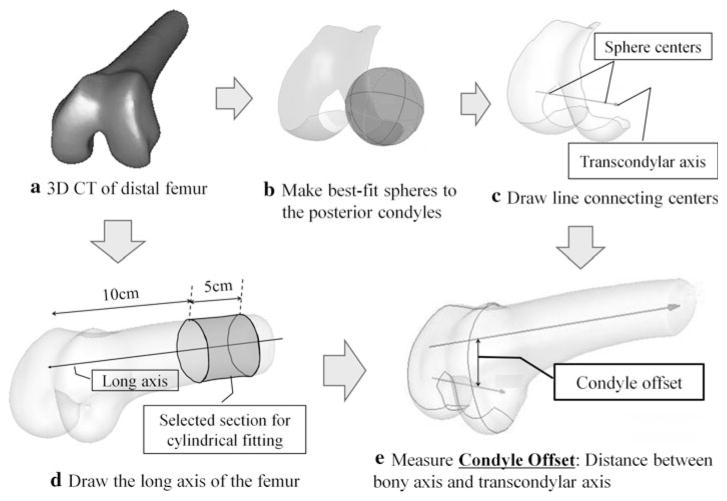
Condyle offset ratio (COR)
The condyle offset ratio (COR) is defined as the anteroposterior location of the transcondylar axis. Firstly, the articular surface area was extracted manually using the Geomagic angularity detection tool. Spheres were fitted to the regions of the medial and lateral posterior condyles between the top of the intercondylar notch and the posterior end (Fig. 1a, b). The transcondylar axis was defined as the line connecting the centers of both best-fit spheres (Fig. 1c). Next, the long axis of the femur was defined by fitting a cylinder to a section of the femoral shaft between 10 and 15 cm from the distal end (Fig. 1d). The condyle offset was calculated as the perpendicular distance between the transcondylar axis and the long axis of the femur (Fig. 1e). To normalize the condyle offset to femur size, the condyle offset ratio (COR) was calculated by dividing the condyle offset by the average radius of the two best-fit condyle spheres.
Fig. 1.
Definition of the condyle offset
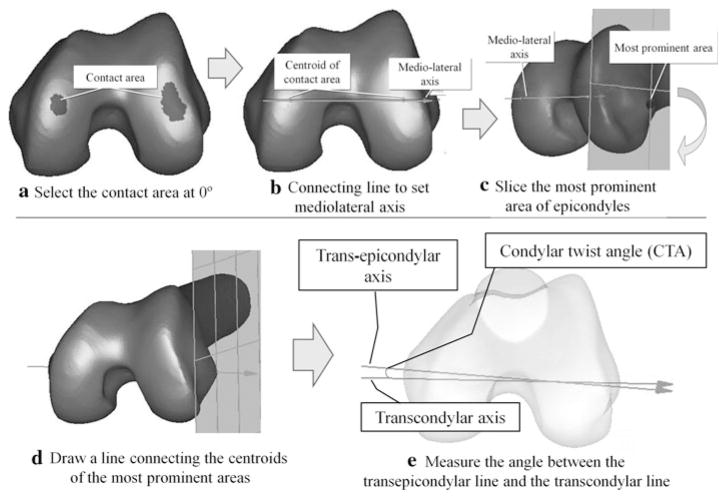
Condylar twist angle (CTA)
The two most common medial/lateral axes used for anatomic descriptions of the distal femur and knee kinematics studies are the transcondylar axis (as described above) and the transepicondylar axis, which connects the medial and lateral femoral epicondyles. The condylar twist angle (CTA) is defined as the angle between these two axes [52]. Clinically, the transepicondylar axis is defined as the line that connects the most prominent points of medial and lateral epicondyles [13, 35, 52]. The procedure to calculate the transepicondylar axis from 3D-CT is as follows. First, a temporary medial–lateral axis was defined by connecting a line between the centroid points of the medial and lateral condyle contact areas at 0 degree knee flexion, defined as the most distal area of the articular surface in the direction of femoral long axis (Fig. 2a, b). Then, a cutting plane perpendicular to this axis was translated medially and laterally to identify the most prominent areas of the both epicondyles (Fig. 2c). Lastly, the transepicondylar axis was defined by the line connecting the centroid points of the most prominent areas (Fig. 2d). The condylar twist angle (CTA) was then measured by projecting both axes (transcondylar and transepicondylar) onto a horizontal plane perpendicular to the long axis of the femur (Fig. 2e).
Fig. 2.
Definition of the condylar twist angle (CTA)
In vivo kinematics
Kinematics were evaluated during downhill running on a treadmill at a moderate speed (2.5 m/s) with 10° downward slope. Three trials were carried out for each subject. For each trial, kinematics data were collected from shortly before foot strike through midstance for one step of the tested leg (approximately 0.5 s duration).
Knee kinematics were assessed with a dynamic stereo radiograph (DSX) system [47–49]. The DSX system consisted of two gantries (each containing a 150-kW radiography source, 40-cm image intensifier, and 4-Mpixel digital video system), configured to provide two beams parallel to the ground with an inter-beam angle of 60°. Radiographic studies were performed using 90-kVp, 150-mA, and 1-ms pulsed exposures, at a frame rate of 150 Hz. Biplane images were collected for a total of 0.5 s, resulting in 75 image pairs per trial.
A model-based tracking technique was used to align 3D-CT bone models to the radiographic image pairs, defining the anatomical coordinate system and providing knee kinematics, as previously described [2]. Anatomic coordinate systems were defined from 3D bone models as described previously [48, 49]. Femoral origin was defined as the midpoint between the centers of the medial and lateral condyles. The vector from femoral origin to tibial insertion was defined and expressed in the tibial anatomical coordinate system. Thus, anteroposterior translation occurred along the tibia anatomical x-axis. This coordinate system was selected for translations because it was both orthogonal and fixed to the tibia with the anteroposterior and mediolateral axes approximately parallel to the tibial plateau. Tibio-femoral rotations were calculated using the conventions described by Grood and Suntay [17]. This kinematics measurement system has been previously used and is capable of evaluating in vivo joint motion with an accuracy of within ±0.1 mm [47–49].
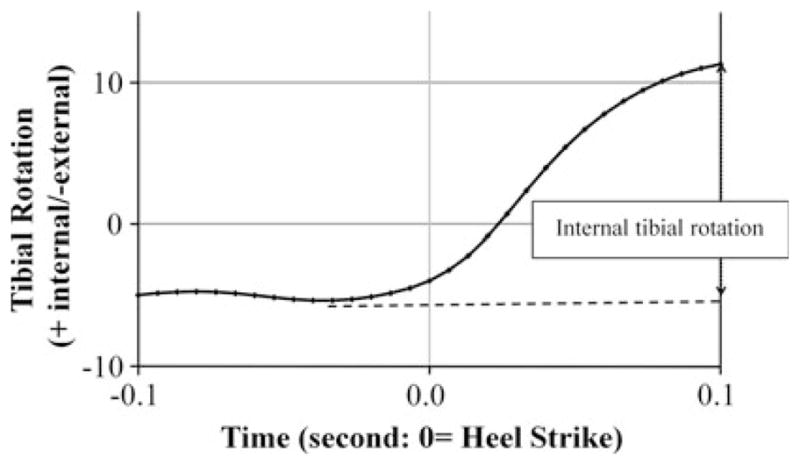
Typical examples of the measurement are shown in Figs. 3 and 4. The tibia moved anteriorly and rotated internally relative to the femur around heel strike. The most anterior and the most internally rotated tibial position was observed during the interval from 0 to 0.1 s after heel strike. For this analysis, anterior tibial translation range was determined as the distance from the most posterior to the most anterior position relative to the femur, while the internal tibial rotation range was calculated as angle from the most external to the most internal rotation.
Fig. 3.
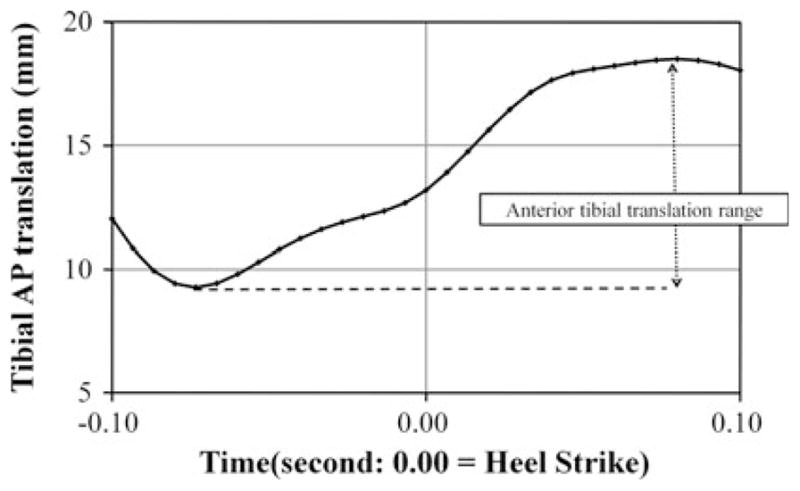
Example of the tibial anteroposterior translation during 0.1 s around heel strike. Plus means anterior direction. The distance from the most posterior position to the most anterior position of the tibia relative to the femur was defined as anterior tibial translation range
Fig. 4.
Example of the tibial rotational angle during 0.1 s around heel strike. Plus means internal rotation. The internal tibial rotation range was calculated as the angle from the most external to the most internal rotation of the tibia relative to the femur
Statistical analysis
Correlations between the morphological and kinematics measures were determined by linear regression analysis. The level of statistical significance was set at alpha = 0.05. Statistical calculations were performed using PASW Statistics 18 (formerly SPSS Statistics, SPSS Inc, Chicago, IL). Post hoc power of these statistical tests were also calculated using G*Power 3.1 when a significant difference or relationship was not observed.
Results
The COR was significantly larger in women than men (P < 0.05; Table 1). The tibial anteroposterior translation around heel strike is shown in Fig. 5. The anterior tibial translation range was 8.9 ± 1.2 (range 6.6–12.0) mm. A fair correlation was observed between the COR and the anterior tibial translation range (R2 = 0.41, P < 0.01; Fig. 6). Larger COR was associated with larger anterior tibial translation range after heel strike. A good correlation between COR and anterior tibial translation range was found for male subjects (R2 = 0.57, P < 0.05), but not for women (n.s., power = 0.78) (Fig. 7).
Table 1.
3D-CT measurement results
| Overall | Male | Female | Gender difference | |
|---|---|---|---|---|
| Condyle offset ratio (COR) | 1.03 ± 0.13 (range 0.81–1.24) | 0.92 ± 0.10 | 1.09 ± 0.18 | P < 0.05 |
| Condylar twist angle (CTA) | 5.4 ± 2.0° (range 2.4–8.5°) | 5.5 ± 2.0° | 5.3 ± 2.1° | n.s. Power = 0.49 |
Fig. 5.
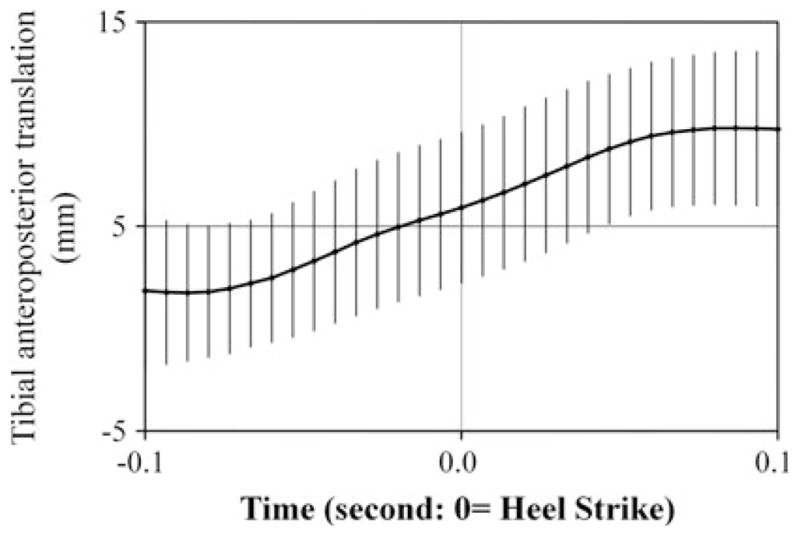
The tibial anteroposterior translation during 0.1 s around heel strike (time = 0.0). Plus means anterior direction. Average and ±1 standard deviation
Fig. 6.
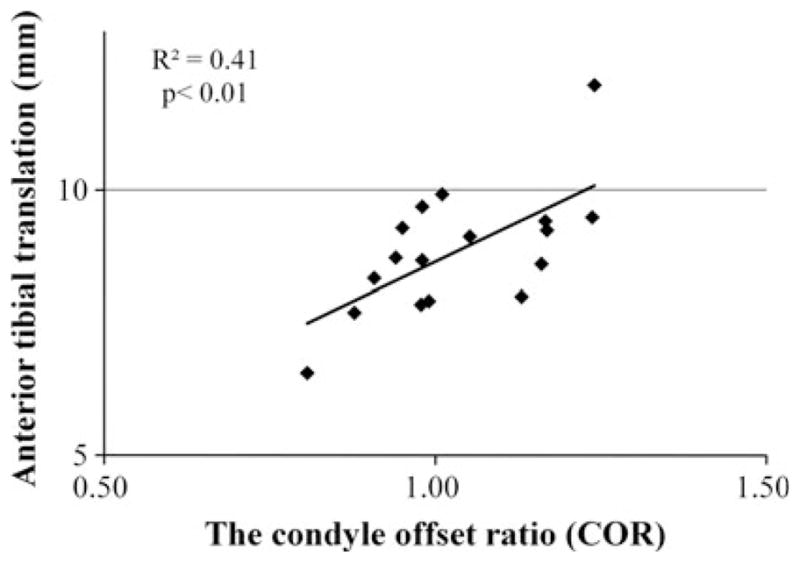
The relationship between anterior tibial translation during 0.1 s around heel strike and condyle offset ratio (COR)
Fig. 7.
The relationship between anterior tibial translation range during 0.1 s around heel strike and condyle offset ratio (COR) in each gender
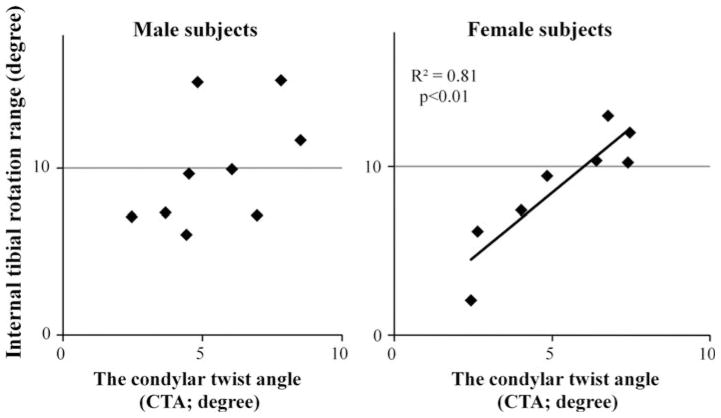
The condylar twist angle (CTA) has no significant difference between genders (n.s., power = 0.49; Table 1). The tibial rotation around heel strike is shown in Fig. 8. The internal tibial rotation range was 9.4 ± 3.4° (range 2.1–15.3°). The CTA was moderately correlated with internal tibial rotation range (R2 = 0.48, P < 0.01; Fig. 9), with larger CTA associated with larger internal rotation range.
Fig. 8.
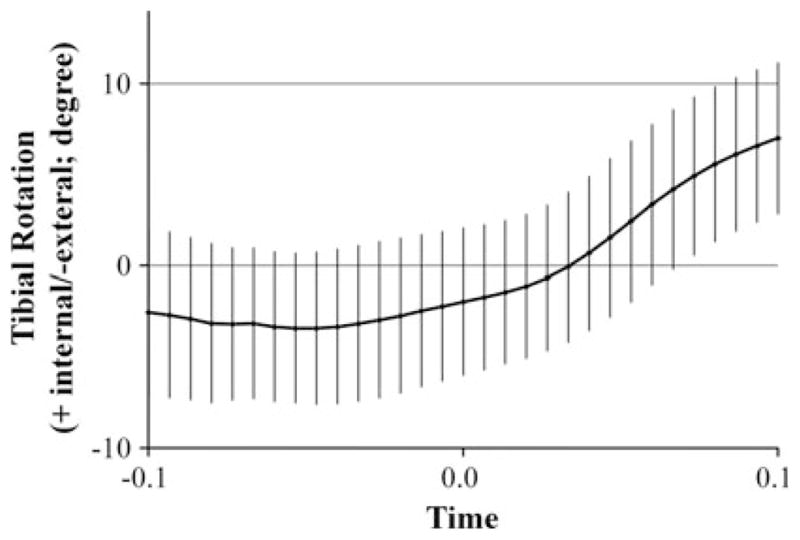
The tibial rotation during 0.1 s around heel strike (time = 0.0). Plus means internal rotation. Average and ±1 standard deviation
Fig. 9.

The relationship between tibial internal rotation range during 0.1 s around heel strike and the condylar twist angle (CTA)
The relationship between the CTA and the internal tibial rotation range was highly significant in women (R2 = 0.81, P < 0.01), but not in men (n.s., power = 0.76) (Fig. 10).
Fig. 10.
The relationship between tibial internal rotation range during 0.1 s around heel strike and the condylar twist angle (CTA) in each gender
Discussion
The most important finding of the present study was that there were specific relationships between the femur geometry and tibio-femoral kinematics. Specifically, the condyle offset ratio (COR) was related to tibial anteroposterior translation, while the condylar twist angle [52] was related to knee axial rotation.
This study showed that knees with larger COR tend to have greater anterior tibial translation during a stressful dynamic task (downhill running), while those with larger CTA have greater internal rotation. Given that the tibial anterior translation and internal rotation induce the tensile stress on the ACL [32, 33], these findings suggest that individuals with larger COR and/or larger CTA might generate higher ACL stresses and be more dependent on ACL function to maintain joint stability.
Differences between genders of both bony morphology and knee kinematics have been often reported [1, 7–9, 18, 31, 50, 52]. The results of this study suggest that the interactions between morphology and kinematics also differ between genders. A relationship between COR and tibial anteroposterior translation was identified in men but not in women. Conversely, the relationship between CTA and tibial rotation was significant in women but not in men. These results strongly suggest that morphological variation may be an important determinant of kinematic knee function, though a larger sample size might be needed to fully characterize the effects of gender on these morphology–kinematics relationships.
Bony anatomy has often been considered as a factor contributing to ACL injury risk [5, 9, 19, 42], but its effect on tibio-femoral kinematics has been unknown. A notable exception is posterior inclination of the tibial plateau, which has been identified as a risk factor for ACL injury [18, 46]; this hypothesis is supported by studies demonstrating increased anterior tibial translation associated with larger tibial slope [11, 14]. Studies focusing on the intercondylar notch size as a predictor of ACL injury risk (particularly in women) provided mixed results, with some studies finding a relationship [9, 19, 42, 45], while others have not [1, 7, 27]. In the meantime, no relationships between intercondylar notch dimension and knee kinematics have been reported. This study is the first to report a definitive relationship between femoral geometry and in vivo knee kinematics, which could be used for evaluating the risk of ACL injury and determining optimal treatment (e.g., identifying potential copers or non-copers [39]) based on individual anatomical variation.
Rotation is a critical component of knee kinematics, not only for ACL pathology [32, 33, 38, 48, 49] but also for TKA implant design and placement [3, 4]. Thus, morphological factors affecting rotation could have value for optimizing the treatment of ACL injury and designing TKA procedures. Larger range of the internal rotation during knee flexion was calculated based on the transcondylar axis than the transepicondylar axis [24]. The current study showed that increased angle between the two axes was related to greater tibial internal rotation. Since CTA is larger in women [52, 53] (who are at higher risk for ACL injury [16]), further research into the potential role of its effects on knee rotation, ACL strain and further injury risk are warranted.
A limitation of the study is that we investigated only two of many factors that could affect in vivo knee kinematics. Ligament injuries surely alter knee kinematics, [15, 26, 30, 41] though a recent report demonstrated that the early reconstruction after ACL injury could avoid the alteration of in vivo knee kinematics [22]. Healthy knee function can be affected by loading conditions [12, 20, 25], muscle force [21, 28], and activities [29, 34, 50]. Subjects were tested under a controlled loading environment to minimize the influence of these other factors. In addition, the investigated knees were contralateral healthy knees in ACL-reconstructed patients, whereas uninjured subjects might be preferable as control. However, the contralateral knee in the ACL-deficient/reconstructed patient has often used as a normal control [48, 49], since they have similar kinematics to the normal subject [24, 40, 41]. Also the femoral bony morphology is not different between ACL injured and contralateral knees [44]. There is, however, a possibility of bias with this sample, since individuals who have undergone ACL reconstruction (and were by inference at high risk of ACL injury) may have different morphology on average than an uninjured population.
The relationship between femoral bony morphology and in vivo knee kinematics should be acknowledged to assess the ACL injury risk and to design a knee replacement implant for the better in vivo knee kinematics.
Conclusions
The location and orientation of the transcondylar axis were significantly related to knee kinematics during a high-load functional activity. These relationships appear to be different between men and women, though further research is necessary to fully characterize gender effects. These results are the first to establish specific links between femoral morphology and in vivo dynamic knee function and may contribute to the development of a mechanistic basis for predicting ACL injury risk.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Yuichi Hoshino, Department of Orthopaedic Surgery, University of Pittsburgh, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA.
Joon Ho Wang, Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Ilwon-Dong, Kangnam-Ku, Seoul 135-720, South Korea.
Stephan Lorenz, Department of Orthopaedic Sports Medicine, Klinikum rechts der Isar, Technical University of Munich, Ismaninger Str. 22, 81675 Munich, Germany.
Freddie H. Fu, Department of Orthopaedic Surgery, University of Pittsburgh, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA
Scott Tashman, Email: tashman@pitt.edu, Department of Orthopaedic Surgery, University of Pittsburgh, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA. Orthopaedic Research Laboratories, 3820 South Water St., Pittsburgh, PA 15203, USA.
References
- 1.Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58–66. doi: 10.1177/03635465010290011501. [DOI] [PubMed] [Google Scholar]
- 2.Anderst W, Zauel R, Bishop J, Demps E, Tashman S. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009;31:10–16. doi: 10.1016/j.medengphy.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anglin C, Brimacombe JM, Hodgson AJ, Masri BA, Greidanus NV, Tonetti J, Wilson DR. Determinants of patellar tracking in total knee arthroplasty. Clin Biomech (Bristol, Avon) 2008;23:900–910. doi: 10.1016/j.clinbiomech.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;366:155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Brisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy. 2010;26:901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter RD, Majumdar S, Ma CB. Magnetic resonance imaging of 3-dimensional in vivo tibiofemoral kinematics in anterior cruciate ligament-reconstructed knees. Arthroscopy. 2009;25:760–766. doi: 10.1016/j.arthro.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Chandrashekar N, Slauterbeck J, Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med. 2005;33:1492–1498. doi: 10.1177/0363546504274149. [DOI] [PubMed] [Google Scholar]
- 8.Chin KR, Dalury DF, Zurakowski D, Scott RD. Intraoperative measurements of male and female distal femurs during primary total knee arthroplasty. J Knee Surg. 2002;15:213–217. [PubMed] [Google Scholar]
- 9.Davis TJ, Shelbourne KD, Klootwyk TE. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1999;7:209–214. doi: 10.1007/s001670050150. [DOI] [PubMed] [Google Scholar]
- 10.DeFrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G. The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency. An in vivo imaging analysis. Am J Sports Med. 2006;34:1240–1246. doi: 10.1177/0363546506287299. [DOI] [PubMed] [Google Scholar]
- 11.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg [Br] 1994;76:745–749. [PubMed] [Google Scholar]
- 12.Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. J Orthop Res. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, Reinig KD. Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg. 2001;83-A(Suppl 2):43–50. doi: 10.2106/00004623-200100021-00010. [DOI] [PubMed] [Google Scholar]
- 14.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 15.Gill TJ, Van de Velde SK, Wing DW, Oh LS, Hosseini A, Li G. Tibiofemoral and patellofemoral kinematics after reconstruction of an isolated posterior cruciate ligament injury: in vivo analysis during lunge. Am J Sports Med. 2009;37:2377–2385. doi: 10.1177/0363546509341829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 18.Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Jr, Mansouri H, Dabezies E. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg [Am] 2008;90:2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: part 1, mechanisms and risk factors. Am J Sports Med. 2006;34:299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 20.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg [Br] 2000;82:1196–1198. doi: 10.1302/0301-620x.82b8.10716. [DOI] [PubMed] [Google Scholar]
- 21.Hirokawa S, Solomonow M, Lu Y, Lou ZP, D’Ambrosia R. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20:299–306. doi: 10.1177/036354659202000311. [DOI] [PubMed] [Google Scholar]
- 22.Isberg J, Faxén E, Laxdal G, Eriksson BI, Kärrholm J, Karlsson J. Will early reconstruction prevent abnormal kinematics after ACL injury? Two-year follow-up using dynamic radiostereometry in 14 patients operated with hamstring autografts. Knee Surg Sports Traumatol Arthrosc. 2011 doi: 10.1007/s00167-011-1399-y. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Iwaki H, Pinskerova V, Freeman MAR. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg [Br] 2000;82:1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- 24.Kozanek M, Van de Velde SK, Gill TJ, Li G. The contralateral knee joint in cruciate ligament deficiency. Am J Sports Med. 2008;36:2151–2157. doi: 10.1177/0363546508319051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42:1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kvist J. Sagittal plane translation during level walking in poor-functioning and well-functioning patients with anterior cruciate ligament deficiency. Am J Sports Med. 2004;32:1250–1255. doi: 10.1177/0363546503262173. [DOI] [PubMed] [Google Scholar]
- 27.LaPrade RF, Burnett QM., 2nd Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1994;22:198–202. doi: 10.1177/036354659402200208. [DOI] [PubMed] [Google Scholar]
- 28.Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL. The importance of quadriceps and hamstring muscle loading on knee kinematics and in situ forces in the ACL. J Biomech. 1999;32:395–400. doi: 10.1016/s0021-9290(98)00181-x. [DOI] [PubMed] [Google Scholar]
- 29.Li G, Kozanek M, Hosseini A, Liu F, Van de Velde SK, Rubash HE. New fluoroscopic imaging technique for investigation of 6DOF knee kinematics during treadmill gait. J Orthop Surg Res. 2009;4:6. doi: 10.1186/1749-799X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Logan M, Dunstan E, Robinson J, Williams A, Gedroyc W, Freeman M. Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med. 2004;32:720–726. doi: 10.1177/0095399703258771. [DOI] [PubMed] [Google Scholar]
- 31.Lonner JH, Jasko JG, Thomas BS. Anthropomorphic differences between the distal femora of men and women. Clin Orthop Relat Res. 2008;466:2724–2729. doi: 10.1007/s11999-008-0415-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Markolf K, Burchfield D, Shapiro M, Shepard M, Finerman G, Slauterbeck J. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 33.Meyer EG, Haut RC. Anterior cruciate ligament injury induced by internal tibial torsion or tibiofemoral compression. J Biomech. 2008;41:3377–3383. doi: 10.1016/j.jbiomech.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 34.Moro-oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res. 2008;26:428–434. doi: 10.1002/jor.20488. [DOI] [PubMed] [Google Scholar]
- 35.Most E, Axe J, Rubash H, Li G. Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech. 2004;37:1743–1748. doi: 10.1016/j.jbiomech.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 36.Olcott CW, Scott RD. The Ranawat award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999;367:39–42. [PubMed] [Google Scholar]
- 37.Papannagari R, Gill TJ, DeFrate LE, Moses JM, Petruska AJ, Li G. In vivo kinematics of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2006–2012. doi: 10.1177/0363546506290403. [DOI] [PubMed] [Google Scholar]
- 38.Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1323–1329. doi: 10.1016/j.arthro.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 39.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. 1998 Basmajian student award paper: movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- 40.Scarvel JM, Smith PN, Refshauge KM, Galloway HR, Woods KR. Does anterior cruciate ligament reconstruction restore normal kinematics? A prospective MRI analysis over two years. J Bone Joint Surg [Br] 2006;88:324–330. doi: 10.1302/0301-620X.88B3.16787. [DOI] [PubMed] [Google Scholar]
- 41.Shefelbine SJ, Ma CB, Lee KY, Schrumpf MA, Patel P, Safran MR, Slavinsky JP, Majumdar S. MRI analysis of in vivo meniscal and tibiofemoral kinematics in ACL-deficient and normal knees. J Orthop Res. 2006;24:1208–1217. doi: 10.1002/jor.20139. [DOI] [PubMed] [Google Scholar]
- 42.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26:402–408. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 43.Shin CS, Carpenter RD, Majumdar S, Ma CB. Three-dimensional in vivo patellofemoral kinematics and contact area of anterior cruciate ligament-deficient and -reconstructed subjects using magnetic resonance imaging. Arthroscopy. 2009;25:1214–1223. doi: 10.1016/j.arthro.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 44.Siebold R, Axe J, Irrgang JJ, Li K, Tashman S, Fu FH. A computerized analysis of femoral condyle radii in ACL intact and contralateral ACL reconstructed knees using 3D CT. Knee Surg Sports Traumatol Arthrosc. 2010;18:26–31. doi: 10.1007/s00167-009-0969-8. [DOI] [PubMed] [Google Scholar]
- 45.Staeubli HU, Adam O, Becker W, Burgkart R. Anterior cruciate ligament and intercondylar notch in the coronal oblique plane: anatomy complemented by magnetic resonance imaging in cruciate ligament-intact knees. Arthroscopy. 1999;15:349–359. doi: 10.1016/s0749-8063(99)70051-4. [DOI] [PubMed] [Google Scholar]
- 46.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16:112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 47.Tashman S, Anderst W. In vivo measurement of dynamic joint motion using high speed biplane radiography and CT: application to canine ACL deficiency. J Biomech Eng. 2003;125:238–245. doi: 10.1115/1.1559896. [DOI] [PubMed] [Google Scholar]
- 48.Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975–983. doi: 10.1177/0363546503261709. [DOI] [PubMed] [Google Scholar]
- 49.Tashman S, Kolowich P, Collon D, Anderson K, Anderst W. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop Relat Res. 2007;454:66–73. doi: 10.1097/BLO.0b013e31802bab3e. [DOI] [PubMed] [Google Scholar]
- 50.Varadarajan KM, Gill TJ, Freiberg AA, Rubash HE, Li G. Gender differences in trochlear groove orientation and rotational kinematics of human knees. J Orthop Res. 2009;27:871–878. doi: 10.1002/jor.20844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J. A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Joint Surg [Br] 2009;91:683–690. doi: 10.1302/0301-620X.91B5.21827. [DOI] [PubMed] [Google Scholar]
- 52.Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16:493–497. doi: 10.1054/arth.2001.23621. [DOI] [PubMed] [Google Scholar]
- 53.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg [Am] 1987;69A:873–880. [PubMed] [Google Scholar]