Abstract
Objectives
Because audiometric evaluation, symptom histories, questionnaires, and similar standard assessment tools may not adequately sample the effects of chronic tinnitus on day-to-day activities, there is a need for alternative methodological approaches to study the impact of tinnitus on day-to-day life. An innovative methodological approach that has shown great promise in the study of chronic health problems characterized by reported temporal and/or situational variability in symptoms and distress is known as ecological momentary assessment (EMA). EMA involves the real time measurement of states, situational factors, and symptoms by individuals as they go about their day-to-day activities. The objective of this pilot investigation was to explore the feasibility of using EMA methods to examine within- and between-day effects of tinnitus.
Design
This study was conducted in three phases: (1) design and development of an EMA methodology that could be used to assess effects of tinnitus; (2) refinement of the methodology through the use of two focus groups; and (3) field-test the methodology with individuals who experienced bothersome tinnitus. For Phase 3, each of the 24 participants wore, throughout their waking hours for two weeks, a personal digital assistant that produced alerts four times a day. The alerts prompted participants to respond to 19 questions, including nine relating to situational and mood factors, and 10 comprising the Tinnitus Handicap Inventory - Screening version (THI-S). To evaluate for potential reactive effects of performing the EMA protocol, each participant completed the paper-and-pencil version of the full 25-item THI before and after the 2-week EMA period.
Results
Participants responded to the alerts with a 90% compliance rate, providing a total of 1210 completed surveys. At the time of their response, participants indicated they were in their house or apartment (67.7%), alone (50.2%), happy (50%), and calm (54.5%). Across most responses, participants could hear their tinnitus (97%), and the loudness of their tinnitus averaged 4.7 on a 7-point increasing-loudness scale. The mean THI-S index score (out of a possible maximum 40 points for greatest tinnitus severity) was 17.0 (moderate self-perceived tinnitus handicap). Repeated THI-S index scores varied considerably both within and between participants. Mean 25-item THI scores were not significantly different before and after the EMA period, suggesting little reactivity of the EMA.
Conclusions
The high compliance rate, positive feedback from participants, lack of reactivity as a result of performing the EMA protocol, and data collected indicate that EMA methodology is feasible with patients who have tinnitus. Outcome data obtained with this methodology cannot be obtained any other way because retrospective questionnaires cannot capture the day-to-day reactions. This methodology has the potential to provide more in-depth and accurate assessments of patients receiving therapy for tinnitus.
Keywords: hearing disorders, tinnitus, outcomes assessment
INTRODUCTION
Tinnitus is self-generated ear and/or head noise that is experienced by 10–15% of the adult population (Hoffman & Reed 2004). For most of these individuals the tinnitus is chronic, and their awareness of its presence generally increases in quiet environments. Fortunately, about 80% of people who experience tinnitus are not particularly bothered by it (Davis & Refaie 2000; Henry, Zaugg, Myers, & Schechter 2008; Jastreboff & Hazell 1998). For the remaining 20%, however, the tinnitus is “clinically significant,” i.e., it causes functional impairment to such a degree that clinical intervention is warranted (Henry, Zaugg, Myers, & Kendall 2010).
Numerous methods have been developed to provide therapy for tinnitus. The literature and the internet are rife with approaches to mitigate, alleviate, relieve, manage, treat, and even “cure” tinnitus. The great majority of these methods are not supported by rigorous scientific research. Occasionally, medical management is helpful for tinnitus (Wackym & Friedland 2004). Surgery, rarely an option, may be appropriate for somatically induced tinnitus (Levine 2004). Although there is no drug for tinnitus, drugs often are used to treat associated mental health conditions such as depression and anxiety (Dobie 2004a). Research is ongoing to find a cure for tinnitus but achieving this goal may be many years away. Thus, claims that treatment can quiet or eliminate tinnitus are unwarranted. For these reasons, most interventions focus on reducing reactions to tinnitus rather than attempting to mitigate the sensation (Dobie 2004b). These interventions generally involve some combination of education, stress reduction, and use of therapeutic sound (Henry et al. 2010). Empirically supported behavioral interventions include cognitive-behavioral therapy (Martinez Devesa, Waddell, Perera, & Theodoulou 2007), neuromonics tinnitus treatment (Davis, Paki, & Hanley 2007), progressive tinnitus management (Henry et al. 2010), tinnitus masking (Vernon & Meikle 2000), tinnitus retraining therapy (Jastreboff & Hazell, 2004), and the use of hearing aids (Searchfield, Kaur, & Martin 2010).
Difficulty in the assessment and further development of behavioral interventions for tinnitus stems from the limitations of techniques used to evaluate these interventions. It is well known that psychoacoustic measures of tinnitus sensation (loudness, pitch, and timbre) generally are unrelated to the impact of tinnitus on the individual (Henry & Meikle 2000; Jakes, Hallam, Chambers, & Hinchcliffe 1985; Meikle, Vernon, & Johnson 1984). For this reason, psychoacoustic testing to characterize these parameters usually is not helpful for diagnostic purposes, for guiding intervention, or for assessing outcomes of intervention (Henry et al. 2010).
Self-report measures (questionnaires) are relied upon to assess outcomes of intervention. We have previously described limitations of tinnitus questionnaires (Henry, Dennis, & Schechter 2005). Briefly, most of these questionnaires provide an index score to quantify the impact of tinnitus on the patient’s everyday activities. Although an index score assists in establishing the need for intervention, it can over- or under-estimate tinnitus severity. An examiner cannot rely solely on an index score to make an objective, clinical severity judgment. In addition, it is difficult to accurately identify and quantify each patient’s tinnitus-associated problems, primarily because (a) effects of tinnitus on an individual are often multidimensional, and (b) a limited set of questions is inherently weighted to addressing certain issues (which may or may not be relevant to an individual patient).
These kinds of problems with retrospective self-report measures are not unique to tinnitus. Collecting accurate and detailed self-reports for any chronic condition is challenging for a number of reasons (Stone & Shiffman 2002). The primary challenge is memory distortions that affect recall of past experiences. A large body of evidence (Erskine, Morley, & Pearce 1990; Gorin & Stone 2004; Schwarz & Sudman 1994; Stone, Turkkan, Jobe, & al. 2000) has shown that recalled information is subject to numerous biases, including: (a) A patient’s current circumstances affect interpretations of previous circumstances. (b) Recall is more of a mental “reconstruction” process rather than one of “retrieval.” (c) Summarizing the nature or severity of a condition can give undue weight to experiences that are more salient or more recent. (d) The recall environment, such as a research setting, can influence the responses.
A methodological approach has been developed to minimize recall biases that are inherent with traditional questionnaires that assess experiences and feelings retrospectively. These new methods involve reports of immediate experience, which are referred to as experience sampling or momentary assessments (reporting feelings or experiences at the moment) (Stone & Shiffman 2002). The approach, referred to broadly as ecological momentary assessment (EMA), circumvents the recall biases listed above because participants are asked about immediate experiences in their natural environment. EMA can involve random- or fixed-time sampling of experiences, events, circumstances, behaviors, and physiological measures. Most commonly, patients provide responses multiple times every day for a week or more.
Because of the weaknesses and limitations inherent in the use of questionnaires that retrospectively assess the effects of tinnitus, we designed and conducted a study that utilized EMA methodology with individuals who complained of bothersome tinnitus. This was a pilot study intended specifically to determine the feasibility of conducting momentary assessments with this target population, and to compare momentary assessments with a traditional tinnitus questionnaire administered before and after the use of EMA.
The primary aims of the study were to: (a) design an assessment battery for the study of reactions to tinnitus that can be used in a real-time situational context via EMA methodology; (b) refine the assessment battery by conducting focus groups with individuals experiencing bothersome tinnitus who would provide qualitative data regarding potential problematic issues surrounding EMA assessment, such as discomfort, embarrassment, or difficulties with use; and (c) assess the feasibility of using this EMA battery among individuals with bothersome tinnitus. The EMA battery was designed to obtain ratings of temporal and situational variability, and to obtain index scores from a validated tinnitus outcomes instrument. A further aim was to determine the variability of these repeated index scores and to compare those scores to scores obtained using the traditional retrospective method.
METHODS
This study was conducted in three phases over a 2-year period. Phase 1 involved the identification of an appropriate personal digital assistant (PDA) to implement EMA for the stated purpose, development of an EMA assessment battery, selection of an assessment schedule, and initial PDA programming. For Phase 2, focus groups were conducted as a forum for the further development and refinement of the momentary assessment protocol. Phase 3 involved active data-gathering.
The Institutional Review Boards of the Portland Veterans Affairs Medical Center (PVAMC) and Oregon Health & Science University approved this study. Signed informed consent was obtained from each candidate in Phases 2 and 3 before enrollment in the study.
Phase 1
Device Selection
Various PDAs were evaluated to determine the one that would be most suitable for this project. The PDA selected was a Palm Pilot Model Tungsten (Palm, Inc., Sunnyvale, California) that runs a program called CERTAS®, developed by Personal Improvement Computer Systems, Inc. (Reston, Virginia). CERTAS® is a self-monitoring program that facilitates the design and implementation of remote, electronic data collection protocols. The program is flexible to accommodate various research applications, and allows data collection questionnaires to be developed according to user requirements. A total of 14 PDAs were purchased.
Development of Sampling Protocol
“Sampling” refers to momentary assessments that are repeated both within and across days. Each sampling occasion was initiated by production of an audible “alert” from the PDA. Development of the sampling protocol for this study involved determining the number of survey items for each alert; whether responses would reflect conditions at the moment of alert or since the previous survey; the content and format of each item; and the sampling schedule.
It is essential that each sampling occasion be no more than 1–3 minutes to minimize the burden of responding and to maximize compliance (Stone & Shiffman 2002). It was determined that the number of survey items for each occasion should be 20 or less to meet this requirement.
EMA data can be obtained either with respect to the immediate experience, or as the recollection of experiences since the last sampling point. There are advantages and disadvantages to each strategy (Beal & Weiss 2003). While sampling the immediate experience eliminates recall bias, it potentially misses experiences the survey is intended to capture. On the other hand, asking participants to respond with respect to the interval of time since the last sampling point introduces memory biases and adds significant complexity to the response task. For this study it was determined that surveying the immediate experience would provide the most objective data for analysis. Hence, after an alert the first screen on the PDA instructed participants to respond to the questions about their experiences at that moment. Individual questions were worded similarly.
The survey items needed to obtain information sufficient to determine if and how the tinnitus was a problem, and the relevant circumstances at the time of assessment. Most importantly, it was essential to determine the effects of tinnitus at the time of each momentary survey. An appropriate tool had already been developed, which was adapted for this purpose. The 10-item screening version of the Tinnitus Handicap Inventory (THI-S) has been psychometrically validated for test-retest reliability and for measuring activity limitation and participation restriction as a result of tinnitus (Newman, Sandridge, & Bolek 2008). The THI-S contains a subset of questions from the full 25-item version of the THI (Newman, Jacobson, & Spitzer 1996; Newman, Sandridge, & Jacobson 1998), and the two versions have been shown to have high comparability. Both versions use the identical scoring method, i.e., a response of “yes” is assigned 4 points, “sometimes” is assigned 2 points, and “no” is assigned 0 points. The THI-S index score thus can range from 0 to 40 points, with higher scores representing greater self-perceived activity limitation and participation restriction due to tinnitus.
In addition to the 10 THI-S questions, nine questions were included for participants to report on their immediate context in terms of what they were doing and their perception of their tinnitus, environmental sounds, and mood (see Table 1 for the nine questions and their response choices). Participants who reported not hearing their tinnitus at that moment were not asked to rate perceived tinnitus loudness (achieved via branching capabilities of the software program). They were, however, asked all of the other questions.
Table 1.
Context-related questions and response choices for PDA. Responses to these questions were provided before completing the 10-item screening version of the Tinnitus Handicap Inventory (THI-S).
| Questions and response choices |
|---|
|
Decisions were made regarding the number of alerts per day (sampling density) and the schedule of survey administration. The sampling density needed to be sufficient to capture daily fluctuations in the tinnitus experience without imposing a burdensome response schedule. Previous studies using EMA generally have used between four and eight alerts per day (Beal & Weiss 2003). With respect to tinnitus, a variable that could affect momentary responses was fluctuations in the tinnitus percept (including loudness, pitch, timbre, and localization). Although some patients experience daily fluctuations in their tinnitus percept, the majority report that their tinnitus is essentially stable within and across days (Meikle, Schuff, & Griest 1987; Stouffer & Tyler 1990). It therefore was not necessary to impose a high sampling density to capture variations in responses that could be a result of tinnitus fluctuations. It was expected that responses would be influenced primarily by situational circumstances (location, activity, level of environmental sound) and mood factors—all of which can be highly variable and unpredictable in any population.
We determined that a minimum of four alerts would be appropriate for capturing a day’s experience of tinnitus, given that we wanted to examine and characterize daily and weekly variation of tinnitus but did not want to overburden participants with an intensive alert schedule (e.g., every 15 min) (Stone & Shiffman, 2002). It is possible that an intensive alert schedule for patients with tinnitus might result in a poor compliance rate and/or create reactivity in which the patients become more aware of their tinnitus and report an increase in perceived tinnitus severity.
The PDAs were programmed to signal participants with audible alerts that occurred randomly within time periods determined by the sampling density and scheduling parameters. Each day had a 12-hour testing period (8 A.M. to 8 P.M.). Scheduling parameters were developed so that four alerts would be created daily within roughly equal but random periods of time. These parameters included the first alert occurring within the first 15 minutes of the 8 A.M. hour. Subsequent alerts were programmed to occur at least 150 minutes apart (but no more than 180 minutes apart). In addition, up to four reminder alerts (occurring every 5 minutes) were programmed, which resulted in participants having a 20 minute window to respond to an initial alert. For most days, this sampling schedule resulted in four alerts. In some instances the randomized nature of the alerts resulted in a fifth alert being generated. Finally, it was determined that participants in Phase 3 would wear and respond to the device for 2 weeks, which was sufficient time to achieve the study objectives while minimizing the burden of responding. A 2-week time frame is commonly used with EMA studies (Stone, et al. 2003).
Phase 2
After the selection of devices and initial programming, the next step was to consult with members of the target population, i.e., to conduct focus groups (O'Brien 1993; Powell, Single, & Lloyd 1996; Vogt, King, & King 2004). “Focus groups generate qualitative data that can be used to both enrich and extend what is known about a concept and inform item development” (p. 233) (Vogt et al. 2004). Moderator-facilitated discussion was used to capture the full range of participants’ experiences and opinions. Sessions were audio-recorded, and recordings were transcribed by the “coder” (research assistant) who was instructed in methodology to capture the most relevant and useful information (Krueger 1998). Special attention was given to language and colloquialisms, which informed appropriate wording of item statements.
Two independent focus groups were conducted, separated by approximately one month. Focus group participants were recruited from a pool of individuals who had previously participated in tinnitus research conducted at the National Center for Rehabilitative Auditory Research (NCRAR). The first and second groups included five (mean age = 62.40 years; SD 4.28) and four (mean age = 51.0 years; SD 8.76) participants, respectively. In group 1, four members (80%) were Veterans; in group 2, two (50%) were Veterans. All group members were male except for one female in the first group. Each focus group lasted approximately 120 minutes. JAH and JAI served as group co-facilitators with assistance from two research assistants. Group members received $15 for their participation.
The PDAs, which had received initial programming, were demonstrated to the participants. Feedback from the participants informed the final device programming (e.g., length of period that participants have to respond, vibratory vs. audio alert, where and how they carry the device, number of questions, etc.). Participants also helped with the selection of the case/holster that was used to wear the PDAs. Further, the sampling density (i.e., four alerts per day) and daily schedule (i.e., 8 A.M. to 8 P.M.) were discussed with the participants. Overall, they were in agreement with the sampling density and time window proposed. EMA techniques can be a burden on participants because of the sheer number of responses they have to attend to. Therefore, every effort was made to accommodate the participants’ suggestions within the context of the study goals.
Phase 3
In addition to contacting previous NCRAR research participants, recruitment flyers were posted at the PVAMC with instructions to call the study coordinator. The primary inclusion criterion was tinnitus that was at least moderately bothersome as indicated by a response of “moderate” or worse to the question “How much of a problem is your tinnitus?” Individuals who engaged in activities on a daily basis that made it difficult to respond to or hear alerts (e.g., non-standard wake-sleep cycles; drove more than 2 hours per day) were excluded from the study.
The study protocol for each participant included: (a) an orientation session, (b) momentary assessments during the EMA period, and (c) a post-EMA debriefing session. Participants were paid $100 plus an additional $1 per alert that resulted in complete responses.
Orientation Session
During the orientation session, participants were first consented and then they completed the 25-item THI (Newman et al. 1996; 1998) and a basic tinnitus-characteristics questionnaire. The THI, one of the most commonly used tinnitus instruments, provides an index score (0–100, with higher scores reflecting greater perceived functional limitations as a result of tinnitus). After completing the questionnaires in the paper-and-pencil format, participants were shown the PDA (i.e., Palm Pilot Model Tungsten). Only study-relevant features of the PDA were explained (e.g., stylus pen, on/off button, silencing alarms, charging the battery). In addition, the alert sound was demonstrated so that participants would be familiar with the sound and know what to expect. Participants were instructed on how to use the stylus pen and tap the buttons on the screen to select a response and move on to the next question. Next, participants completed an example questionnaire using the PDA and were encouraged to ask questions. The orientation period lasted approximately 30 minutes.
Twenty four participants were enrolled. On average, the participants were 57.3 years of age (SD = 11.4; range 28–69). They predominantly were military Veterans (83.3%) and male (91.7%). Half were married (50.0%), many retired (41.7%), and the majority had a high school or higher education (95.8%). One participant (4.2%) reported unilateral tinnitus, 19 (79.2%) reported bilateral tinnitus (including three participants who reported the perceived tinnitus location as “inside head”), and four (16.7%) reported “other” location. Of those who responded, 38.1% reported that the tinnitus sensation was one sound, 52.4% reported hearing two or more sounds, and 9.5% reported “unsure” as to the number of sounds. Table 2 provides further characteristics of the participants.
Table 2.
Characteristics of participants (N = 24).
| Characteristics | n | % |
|---|---|---|
| Marital Status | ||
| Married living with spouse | 12 | 50.0 |
| Divorced | 8 | 33.3 |
| Never married | 4 | 16.7 |
| Employment Status | ||
| Employed | 6 | 25.0 |
| Unemployed | 2 | 8.3 |
| Retired | 10 | 41.7 |
| Looking for work | 4 | 16.7 |
| Other | 2 | 8.3 |
| Veteran Status | ||
| Veteran | 20 | 83.3 |
| Nonveteran | 4 | 16.7 |
| Education | ||
| Less than high school | 1 | 4.2 |
| Completed high school / vocational training | 5 | 20.8 |
| Some college / completed college | 18 | 75.0 |
| Awareness of tinnitus | ||
| <1 year | 1 | 4.2 |
| 3–5 years | 3 | 12.5 |
| 6–10 years | 5 | 20.8 |
| 11–20 years | 6 | 25.0 |
| 20 or more years | 9 | 37.5 |
| Temporal course of tinnitus | ||
| Suddenly (1 week or less) | 6 | 25.0 |
| More gradually | 15 | 62.5 |
| Do not know | 3 | 12.5 |
| Location of tinnitus | ||
| Right ear only | 1 | 4.2 |
| Both ears | 16 | 66.7 |
| Inside head | 3 | 12.5 |
| Other | 4 | 16.7 |
| Presence of tinnitus | ||
| Never | 0 | 0 |
| Occasionally | 0 | 0 |
| Some of the time | 0 | 0 |
| Most of the time | 6 | 25.0 |
| Always | 18 | 75.0 |
| Time thinking about tinnitus | ||
| Never | 0 | 0 |
| Occasionally | 2 | 8.3 |
| Some of the time | 14 | 58.3 |
| Most of the time | 7 | 29.2 |
| Always | 1 | 4.2 |
| Tinnitus as a problem | ||
| Not a problem | 0 | 0 |
| Slight problem | 1 | 4.2 |
| Moderate problem | 10 | 41.7 |
| Big problem | 12 | 50.0 |
| Very big problem | 1 | 4.2 |
EMA Period
During the EMA period, each participant carried the PDA device for 2 weeks, which was programmed to obtain momentary assessments as described above. The EMA period began immediately after the orientation session and ended when participants returned for the debriefing session.
Debriefing Session
After the EMA period, participants returned with the PDA for a debriefing session. In this stage, participants again completed the 25-item THI and answered questions as part of a debriefing interview. The interview questions were designed to elicit feedback regarding their general experience using the PDA and responding to the alerts. Participants were asked whether their feelings had changed regarding: their perception of their tinnitus; whether the PDA interfered with their daily routine; reactions from other people; whether the alerts were easy or hard to hear; and their perception of total responses they completed and the reasons they might have missed alerts. In addition, participants were allowed to see their responses and comment on their level of compliance with the alert schedule.
Data Analysis
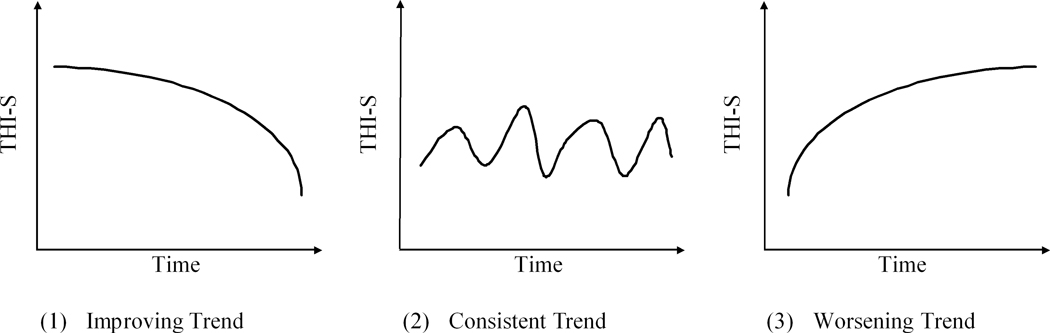
Descriptive analyses of the EMA data were conducted to determine the feasibility of conducting momentary assessments with this target population and to compare momentary assessments (THI-S index scores) with questionnaire scores (using the same subset of questions from THI) obtained before and after the use of EMA. Administering the THI before and after the use of EMA also enabled an analysis of potential reactivity effects. In addition, a graphical examination of the EMA data (THI-S index scores) was conducted to examine tinnitus severity chronologically across the study period for each participant. EMA data trends were analyzed by GG and EJT using the following criteria (see Fig. 1): (a) “Improving trend” characterized by an improvement in the scores (i.e., THI-S scores decreasing over the study period); (b) “Consistent trend” characterized by little variation in the scores (i.e., consistent THI-S scores over the study period); and (c) “Worsening trend” characterized by a decline in the scores (i.e., THI-S scores increasing over the study period).
Figure 1.
Graphical representations of repeated THI-S index scores reflecting three trends across the 2-week EMA sampling period: Improving trend is characterized by an improvement (reduction) in scores. Consistent trend is characterized by little to no directional variation in scores. Worsening trend is characterized by an increase in scores.
RESULTS
Participants responded to questions using the PDA over a period that was intended to last 14 days. However, because of scheduling constraints, some participants responded to the PDA for more or less than 14 days (M = 15.08, SD = 1.47; range = 12–16). The response rate for the participants was high. On average, based only on the responses within the 14 day period, participants responded to 90% of the alerts (M = 50.42, SD = 4.00) yielding a total of 1210 responses.
Descriptive Analyses of PDA Context Questions
Participants responded to questions regarding their immediate context, affect, and their tinnitus. Based on the total number of responses, the majority of responses indicated that participants were in their house or apartment (67.7%), somewhere else (15.4%), traveling (11.2%), or working outside the home (5.8%). In terms of what they were doing at the time the PDA alerted them, the participants reported other (38.5%), watching TV or computer (30.4%), physical activity (12.7%), eating a meal (11.7%), and working at a paid job (6.7%). Half of the participants were alone when they responded to the PDA (50.2%) or in a small group of one to two people (41.2%). Moreover, fewer participants were with many people (8.4%) when they responded to the alerts and even fewer were on the phone (0.3%).
In terms of affect, the average rating for “how happy or sad do you feel right now?” was 3.36 (SD = 1.13) on a 7-point likert scale (anchored by 1=“very happy” and 7=“very sad”). Overall, approximately 50% of the responses indicated participants feeling happy, about 36% reported a response between happy and sad (4 on the likert scale) and about 14% reported feeling sad. Similarly, the average rating for “how calm or anxious do you feel right now?” was 3.32 (SD = 1.29) on a 7-point likert scale (anchored by 1=“very calm” and 7=“very anxious”). More than half reported feeling calm (54.5%), about one third (29.0%) reported a response between calm and anxious (4 on the likert scale), and fewer reported feeling anxious (16.5%) when the PDA alerted them.
Participants were asked whether they could hear their tinnitus at the moment of being alerted. Based on the total number of responses, the majority of the responses indicated that participants could hear their tinnitus at the moment they were questioned (97.0%). For those who responded “yes,” a follow-up (branching) question asked how loud their tinnitus was at the moment using a 7-point likert scale (anchored by 1=“softest sound” and 7=“loudest sound”; please note that during the orientation session, participants were instructed to respond to this question with respect to the “softest sound imaginable” and the “loudest sound imaginable”—because of space limitations of the PDA screen and the CERTAS program, these full anchors could not be displayed). Out of 1174 responses, the average rating for the loudness of the participants’ tinnitus was 4.7 (SD = 1.5). Approximately 57% of the responses indicated that the loudness of their tinnitus was greater than the midpoint between the softest and loudest sound. About 22% reported softest sound and 20% reported ratings between the softest and loudest sounds imaginable (4 on the likert scale).
THI-S Index Scores
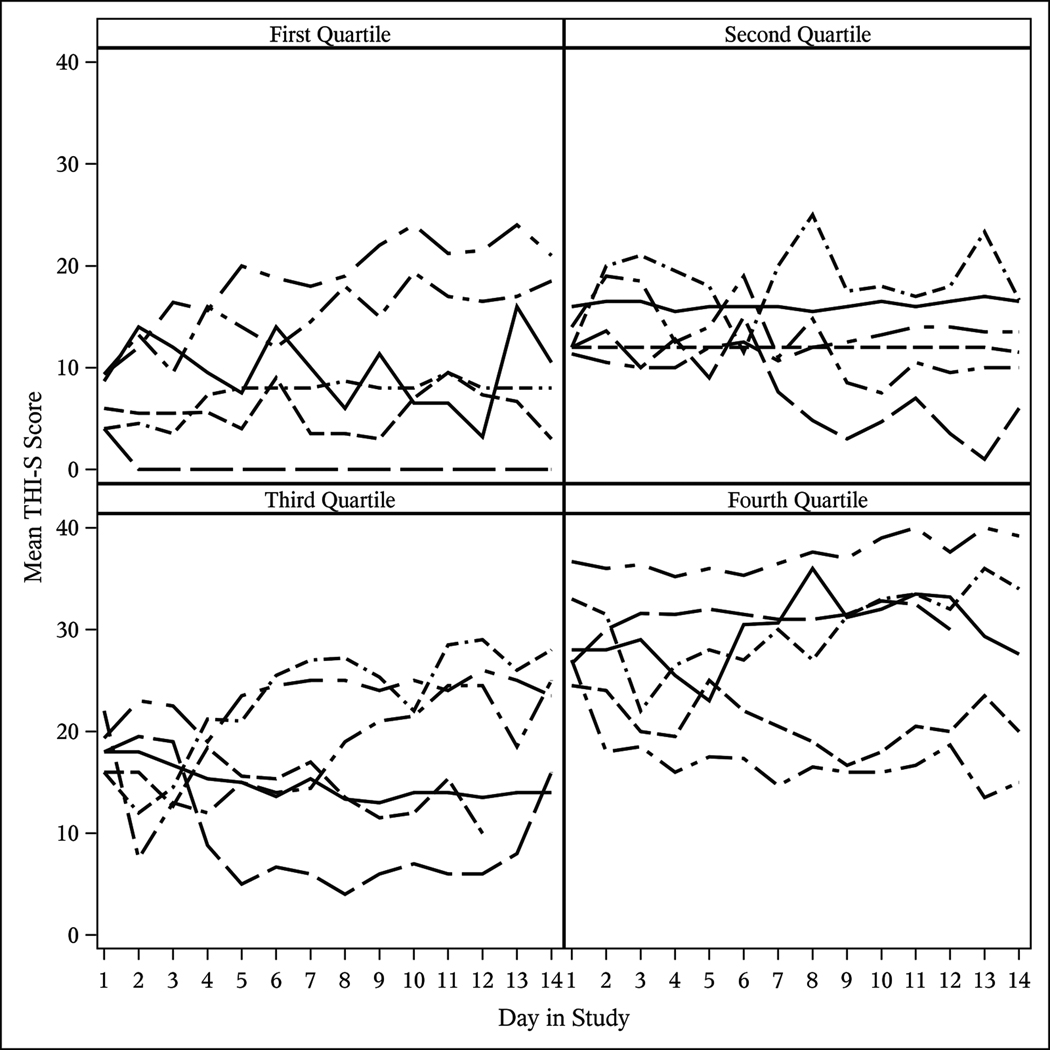
Self-perceived activity limitation and participation restriction as a result of tinnitus was assessed using the 10-item THI-S on the PDA. THI-S index scores can range between 0 and 40 with scores greater than 6 points indicating some degree of self-perceived limitation/restriction (Newman, et al. 2008). All index scores were summed and divided by the number of total alerts (1210) creating a mean score for the entire study period of 17.0 (SD = 9.9). A graphical examination of the data was conducted in order to examine tinnitus severity across the study period for each participant. Participants were grouped into quartiles based on the average THI-S score for the first day in the study (Fig. 2). Generally, wide variation in self perceived tinnitus activity limitation and participation restriction was observed over the two week period among all participants. To further evaluate the variation in tinnitus severity, EMA data trends of both individual scores (i.e., THI-S score for each alert—see Appendix A, Supplemental Digital Content 1) and daily averages (i.e., THI-S daily means—see Appendix B, Supplemental Digital Content 2) were analyzed for each participant.
Figure 2.
Each trace represents the mean daily THI-S scores obtained from participants across 14 days of responding to EMA alerts. Each point for each day indicates the mean TSI-S score derived from four individual TSI-S scores (except days when fewer than four responses were provided). Participants are grouped into quartiles according to their average THI-S score from the first day.
Two of the coauthors (GG and EJT) independently analyzed and rated each of the participants’ trends in THI-S scores over time (Fig. 1). These ratings for daily mean THI-S scores indicated that 54.2% of the participants were classified as “consistent trend,” 25.0% as “improving trend,” and 20.8% as “worsening trend.” The interrater reliability for the raters was found to be κ = 0.86 (p < 0.001) indicating almost perfect agreement between the two raters.
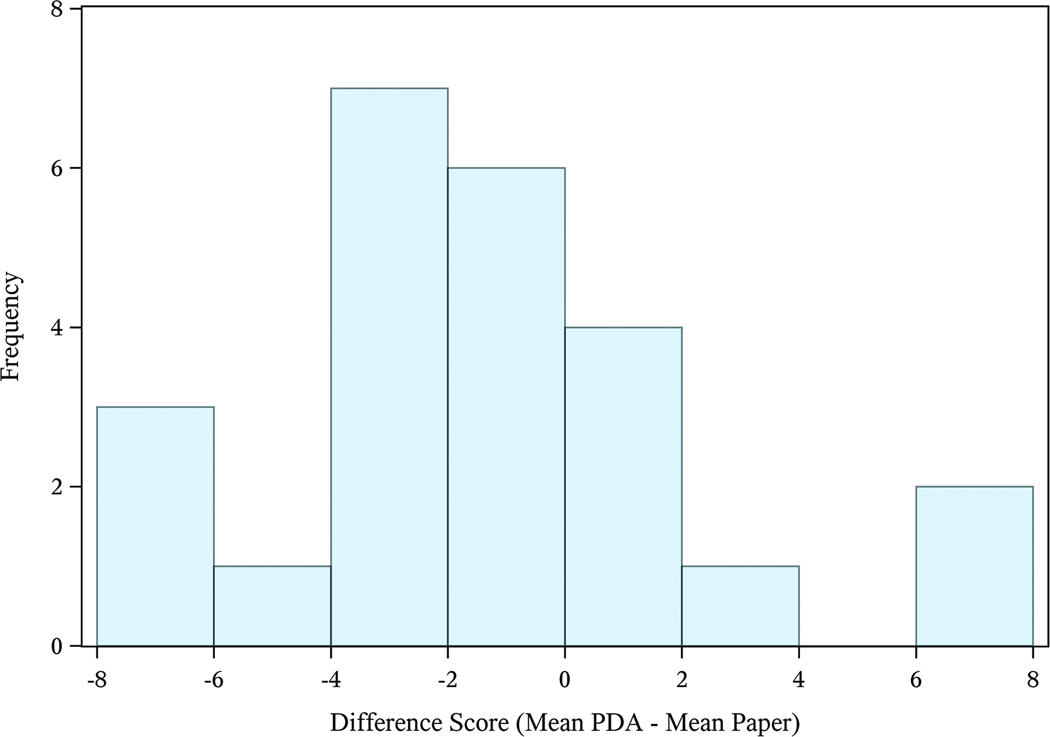
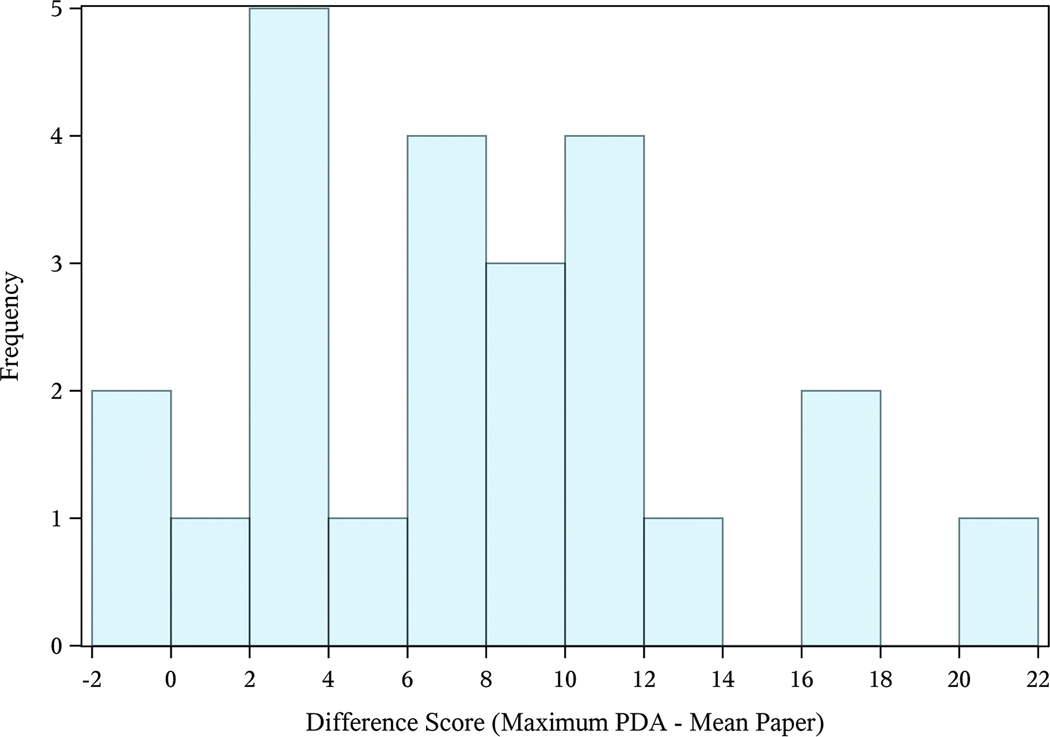
THI-S Scores: PDA versus Paper-and-Pencil
It was an objective of this study to compare THI-S index scores between those obtained on the PDA versus those obtained using paper-and-pencil during the orientation and debriefing sessions. Each participant’s mean THI-S responses (obtained repeatedly during the 2-week EMA period) were compared to the average of the two paper-and-pencil scores. Because the full 25-item THI was completed at the orientation and debriefing sessions, only the subset of the 10 questions that comprised the THI-S was used in this analysis to enable the most valid comparison. For each participant, the analysis involved taking the average of the PDA scores and subtracting the average of the orientation and debriefing scores. A negative difference score meant that the paper-and-pencil format produced a higher score (indicating greater tinnitus severity) than the PDA format for that participant. If the difference was positive, then the PDA format resulted in a higher score than the paper-and-pencil format.
Figure 3a shows the results of this analysis. It can be seen that many of the difference scores were close to zero, indicating close agreement between the two formats. Eleven participants showed differences less than −2. For these participants, the paper-and-pencil format overestimated tinnitus severity relative to the PDA scores. Only three participants had differences greater than +2. For these participants, the paper-and-pencil format underestimated tinnitus severity relative to the PDA.
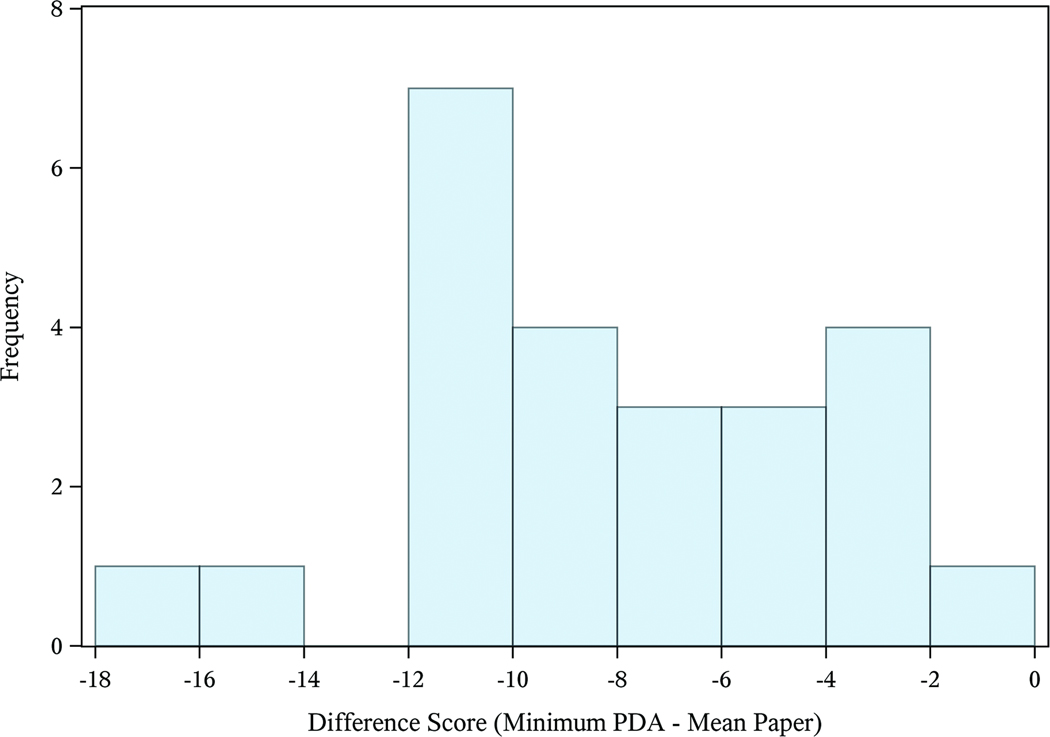
Figure 3.
These figures are based on difference scores calculated to reflect the correspondence between paper-and-pencil and PDA formats of obtaining THI-S scores. The height of each bar reflects the number of participants for each range of difference scores. These differences were calculated individually for each of the 24 participants by subtracting the average of the two THI-S scores obtained during the orientation and debriefing sessions from: (a) the average of all of the THI-S scores obtained with the PDA over 14 days of EMA testing; (b) the minimum THI-S score obtained with the PDA; (c) the maximum THI-S score obtained with the PDA.
The multiple responses obtained with the PDA enabled further comparisons. Each participant had a range of THI-S index scores. For the previous analysis, we used the average across all of the PDA responses. It also was of interest to make similar comparisons using the minimum and maximum THI-S scores obtained with the PDA. Figures 3b and 3c, respectively, show the results of these analyses. When using the minimum THI-S score, Figure 3b shows that all of the difference scores were negative, indicating that every participant had at least one THI-S index score that was lower than the paper-and-pencil version. When using the maximum THI-S score, Figure 3c shows that most of the difference scores were positive, indicating that most participants had at least one THI-S index score that was higher than the paper-and-pencil version.
Responses by Time Block and Location
Two linear mixed models were fit to the THI-S scores to assess the effects of time of day and location on responses. Each model included random participant-level intercepts and day effects, allowing for overall variability in mean THI-S among participants, as well as serial correlation in mean THI-S across days of measurement (Fitzmaurice, Laird, & Ware 2004). Table 3 shows means and standard deviations from these analyses. Time of day was divided into four 3-hour time blocks: 8 A.M.–11 A.M., 11 A.M.–2 P.M., 2 P.M.–5 P.M., and 5 P.M.–8 P.M. The results of the time of day model indicate that THI-S scores did not vary by time of day, F(3, 1160) = 0.29, p = 0.83. The second analysis, testing the effects of physical location on mean THI-S, had a similar random effects structure with fixed-effect categories for physical location that included work, home, traveling, and somewhere else. The mean score for the THI-S: (a) while traveling was 17.5 (N = 135; SD = 10.3); (b) while at their house or apartment was 17.4 (N = 819; SD = 10.0); (c) while somewhere else was 15.8 (N = 186; SD = 9.8); and (d) while at work was 15.1 (N = 70; SD = 7.7). Using a random coefficient model, an analysis of variance indicated a significant main effect for location: F(3, 1164) = 4.06, p < 0.01. Contrasts indicated a significant (p < .01) effect for “somewhere else” resulting in a decrease of 0.99 THI-S score when compared to THI-S score at home. A significant (p < .05) effect was found for “traveling” resulting in a decrease of 0.77 THI-S score when compared to THI-S score “at home.” THI-S scores for “work” were not significantly different when compared to THI-S score “at home.”
Table 3.
Descriptive statistics of PDA questions by time block and location.
| Environment Loudness |
Happy - Sad |
Calm - Anxious |
Tinnitus Problem |
Tinnitus Loudness |
THI-S | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Block | Location | N | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD |
| 8am – 11am | Work | 12 | 3.8 | 1.3 | 2.6 | 1.0 | 2.9 | 1.3 | 2.8 | 1.2 | 4.5 | 1.3 | 17.3 | 10.0 |
| Home | 269 | 2.5 | 1.1 | 3.5 | 1.0 | 3.2 | 1.2 | 2.4 | 1.1 | 4.7 | 1.4 | 16.8 | 9.8 | |
| Traveling | 30 | 4.7 | 1.4 | 3.6 | 1.4 | 3.8 | 1.5 | 2.7 | 0.9 | 4.9 | 1.3 | 19.3 | 8.4 | |
| Somewhere Else | 26 | 4.0 | 1.5 | 3.5 | 1.4 | 3.6 | 1.6 | 2.8 | 1.2 | 4.8 | 1.6 | 18.3 | 9.2 | |
| 11am – 2pm | Work | 28 | 4.0 | 1.5 | 2.7 | 1.0 | 2.9 | 1.0 | 2.6 | 1.0 | 4.7 | 1.1 | 14.5 | 7.7 |
| Home | 171 | 2.8 | 1.2 | 3.5 | 1.2 | 3.4 | 1.4 | 2.6 | 1.2 | 4.8 | 1.5 | 17.5 | 10.3 | |
| Traveling | 41 | 3.9 | 1.6 | 3.3 | 1.2 | 3.2 | 1.4 | 2.5 | 1.1 | 4.3 | 1.5 | 17.2 | 10.8 | |
| Somewhere Else | 54 | 3.8 | 1.6 | 3.4 | 1.1 | 3.3 | 1.2 | 2.1 | 1.0 | 4.4 | 1.5 | 15.9 | 9.6 | |
| 2pm – 5pm | Work | 22 | 3.8 | 1.5 | 2.7 | 0.9 | 2.8 | 1.0 | 2.5 | 1.1 | 4.6 | 1.4 | 15.3 | 7.7 |
| Home | 158 | 3.1 | 1.2 | 3.5 | 1.1 | 3.4 | 1.2 | 2.5 | 1.1 | 4.8 | 1.3 | 17.1 | 10.0 | |
| Traveling | 38 | 4.4 | 1.5 | 3.1 | 1.0 | 3.5 | 1.4 | 2.3 | 1.1 | 4.4 | 1.9 | 17.5 | 10.7 | |
| Somewhere Else | 64 | 3.9 | 1.4 | 3.4 | 1.3 | 3.3 | 1.4 | 2.1 | 1.2 | 4.5 | 1.6 | 16.6 | 9.2 | |
| 5pm – 8pm | Work | 8 | 4.6 | 1.6 | 2.3 | 1.0 | 2.6 | 1.1 | 2.5 | 1.1 | 4.9 | 1.0 | 13.5 | 3.3 |
| Home | 221 | 3.1 | 1.3 | 3.3 | 1.2 | 3.4 | 1.3 | 2.6 | 1.2 | 4.7 | 1.5 | 18.2 | 9.9 | |
| Traveling | 26 | 4.2 | 1.5 | 3.4 | 1.1 | 3.3 | 1.3 | 2.2 | 1.1 | 4.2 | 2.0 | 15.7 | 11.3 | |
| Somewhere Else | 42 | 3.7 | 1.6 | 3.0 | 0.9 | 2.9 | 1.2 | 2.2 | 1.2 | 4.1 | 1.6 | 13.2 | 11.2 | |
| All | 1210 | 3.2 | 1.4 | 3.4 | 1.1 | 3.3 | 1.3 | 2.5 | 1.1 | 4.7 | 1.5 | 17.0 | 9.9 | |
Note. Tinnitus loudness = How loud is your tinnitus right now? 7-point likert scale; Tinnitus problem = How mch of a problem is your tinnitus right now? 7-point likert scale; Environment loudness = How loud is your environment right now? 7-point likert scale; Happy – Sad = How happy or sad do you feel right now? 7-point likert scale, 5–7 scores indicate sadness; Calm – Anxious = How calm or anxious do you feel right now? 7-point likert scale, 5–7 scores indicate anxiousness.
Interrelationships Between PDA Responses
Correlations were conducted to examine relationships between the other PDA questions as well as THI-S scores (see Table 4). Questions that were examined as part of this analysis included “How loud is your tinnitus right now?” (question #5 in Table 1), “How much of a problem is your tinnitus right now?” (#6), “How loud is your environment right now”? (#7), “How happy or sad do you feel right now?” (#8), and “How calm or anxious do you feel right now?” (#9). Responses to each of these items were correlated with each other as well as with the THI-S. Pearson r’s ranged from −0.03 to 0.87. Significant (p<0.01) correlations were seen between: THI-S and tinnitus loudness (r=0.57); THI-S and tinnitus problem (r=0.76); THI-S and calm-anxious; tinnitus loudness and tinnitus problem (r=0.77); and happy-sad and calm-anxious (r=0.87).
Table 4.
Correlation matrix for PDA questions.
| Tinnitus Loudness |
Tinnitus Problem |
Environment Loudness |
Happy - Sad |
Calm - Anxious |
|
|---|---|---|---|---|---|
| THI-S | 0.57* | 0.76** | −0.15 | 0.34 | 0.56* |
| Tinnitus Loudness | - | 0.77** | −0.08 | −0.03 | 0.07 |
| Tinnitus Problem | - | - | −0.10 | 0.06 | 0.28 |
| Environment Loudness | - | - | - | 0.18 | 0.08 |
| Happy - Sad | - | - | - | - | 0.87** |
Note.
p = < .01,
p = < .001;
Tinnitus loudness = How loud is your tinnitus right now? Tinnitus problem = How much of a problem is your tinnitus right now? Environment loudness = How loud is your environment right now? Happy – Sad = How happy or sad do you feel right now? Calm – Anxious = How calm or anxious do you feel right now?
Reactivity Analysis
To determine if the EMA intervention had an effect on the participants’ self-perceived tinnitus activity limitation and participation restriction, the mean 25-item THI scores were compared between the pre- and post-EMA assessments. The mean THI score at the orientation session was 41.58 (SD = 21.79) indicating “moderate handicap.” [A THI index score of 18 or more indicates some degree of self-perceived handicap (Newman et al. 1998)]. The mean THI score assessed during the debriefing session was 43.29 (SD = 19.99) also indicating a “moderate handicap.” A t-test was conducted to determine if THI scores from the orientation and debriefing sessions were significantly different. The difference in means was 1.71 units, which was not significant, t(23) = −0.68, p = 0.502, suggesting little, if any, reactivity.
Qualitative Data from Debriefing Session
Individual interviews were conducted during the debriefing session to elicit feedback from participants regarding their general experience of using the PDA. Over 91.7% (22) of participants reported becoming more aware of their tinnitus as a result of being in the study. Only two participants reported no change. Most comments referred to becoming more aware of their tinnitus and how it impacted their lives. For example, one participant said, “It asked questions that brought me into awareness, emotional things that were disturbing to me but didn’t know why. For me that’s a plus, to understand myself.” In addition, all participants were asked whether the change (i.e., increased awareness of their tinnitus) was positive or negative. Fifteen (68.2%) reported positive, three (12.5%) reported negative, three (12.5%) reported both, and one (4.5%) reported neither.
Twenty-two (91.7%) participants reported that responding to the PDA did not interfere with their daily routine. In terms of other people’s reaction to them carrying and responding to a PDA, 17 (81%) reported that people did not change their behavior toward them. In most cases, the use of the PDA went unnoticed by other people. Four (19%) participants reported that other people changed their behaviors toward them. In these cases, positive interactions with other people regarding the use of a PDA in a study were discussed (e.g., PDA as a conversation piece, people’s curiosity) as well as friends realizing that the participant had a serious hearing problem.
Furthermore, participants reported whether the PDA alerts were easy or hard to hear. Fourteen (58.3%) participants reported that the alerts were easy to hear, seven (29.2%) reported hard to hear, and three (12.5%) reported both easy and hard to hear. In these latter cases, participants described situational environment noise that affected their ability to hear the PDA alerts. For example, one participant said, “In my pocket, easy. On a nightstand or close to the TV, I would miss the first alert, it became harder to hear.” Lastly, the participants had a good sense of the number of PDA alerts they completed throughout the study period. On average they thought they had completed 89% (SD = 8.90) of the PDA alerts, which is comparable with the actual response rate of 90% (M = 50.42, SD = 4.00).
DISCUSSION
Auditory problems can be episodic—due either to day-to-day variability in symptoms or because situations or experiences that pose a challenge to an individual may occur infrequently or only in particular settings. Thus, symptom histories and questionnaire and interview methods may not be well suited to discovering the impact of auditory disorders on daily life. EMA is a method that shows great promise in capturing what “really” happened in the course of day-to-day events, whereas appraisals provided by retrospective interviews or questionnaires provide a view through a lens tinted by an individual’s ability to recall, summarize, and evaluate their experiences. This pilot study was designed to determine the feasibility of utilizing EMA methodology with individuals who are bothered by chronic tinnitus. A second arm of this study was to use the same methodology with individuals who were hearing aid users, to determine the feasibility of EMA methodology to assess momentary hearing challenges with this population (Galvez, Turbin, Thielman, Istvan, Andrews, & Henry 2011).
The use of EMA methods in populations that experience tinnitus problems is novel, and, before conducting this pilot study, it seemed possible that there may be unforeseen and/or uncontrollable concerns with the use of EMA methods or PDA devices specifically. The debriefing sessions with participants revealed that technical problems, practical issues, ease of use, or discomfort and embarrassment were not concerns. These findings are consistent with studies that have shown that participation in EMA assessments has null effects on the behaviors under examination (e.g., Hufford, Shields, Shiffman, Paty, & Balabanis 2002).
Another concern was the potential for a high proportion of missing data in the EMA records. Unlike paper-and-pencil methods, the rate of compliance with EMA devices is generally high—in a study of symptom report in chronic pain patients, only 6% of all records were missing vs. 89% for patients using a standard paper-and-pencil method (Stone, Shiffman, Schwartz, Broderick, & Hufford 2002). Our participants revealed a 90% compliance rate. There further was the concern of a high rate of loss or damage to the instruments provided to the participants. We urged research participants to handle the PDA devices with prudence, and in fact none of the devices was lost or damaged.
The sampling density factors selected for this study were designed to optimize compliance. These factors included testing for 2 weeks, obtaining four samples per day, and limiting the survey to 19 questions. Total average time for participants to respond to the questions associated with a single alert was 1 min, 20 sec (range: <1 min to 4 min), which was well within the recommended range (Stone & Shiffman 2002). The high compliance rate amongst the participants suggests that EMA methodology can be used with this population. It of course is possible that increasing the sampling density would reduce compliance accordingly (Stone et al. 2003). A logical next step would be to conduct a study with different sampling density groups, and to compare compliance between groups.
Compliance was also optimized by the incentive structure for the study. In fact, it might be questioned if the high compliance was a result of the payment amount. However, such incentives are very common in EMA studies. Reis and Gable (2000) noted, “Incentives should be commensurate with workload: not so large as to attract freeloaders but not so small as to only attract research-eager volunteers.” (p. 207) Stone and Shiffman (2002) stated, “Beyond assessing and recording compliance, investigators should do what they can to achieve high compliance. This often requires a combination of participant training, monitoring and feedback, incentives, and other procedures.” (p. 241) Scollon, Kim-Prieto, and Diener (2003) concurred with these other investigators, noting that a previous study (Stone, Kessler, & Haythornthwaite 1991) overpaid subjects, resulting in poor quality data. We consulted with an EMA expert to determine the payment schedule, which was designed to maximize compliance without degrading data quality.
An important concern addressed by this study was the potential for reactivity, i.e., whether performing the EMA protocol itself could lead to a heightened perception of tinnitus and consequent effects. To evaluate for reactivity, data were analyzed to determine if THI scores were significantly different between the Phase 3 orientation and debriefing sessions. The difference in means was not significant, suggesting that responding to the PDA questions over the 2-week period did not create reactivity for the participants in terms of their self-perceived tinnitus activity limitation and participation restriction. This lack of reactivity is consistent with EMA studies with individuals experiencing chronic pain (Cruise, Broderick, Porter, Kaell, & Stone 1996; Stone et al. 2003). Although the EMA protocol did not result in reactivity, the majority of participants reported that using the PDA and responding to questions about their tinnitus increased their overall awareness of their auditory disorder. This increased awareness was rated mostly as a positive change. Hence, these participants experienced essentially no adverse effects as a result of performing the protocol.
We have presented both group data and individual data. Analysis of group data alone masks results that take place at the individual level. Appendices are provided showing all of the THI-S results for individual participants (Appendix A, Supplemental Digital Content 1, and Appendix B, Supplemental Digital Content 2). The individual traces of THI-S results over time reveal that participants differed substantially in the variability of their responses. Rating these individual traces determined that the participants could be grouped in three categories with regard to the trend of their responses: improving, consistent, and worsening. In general, about half of the participants showed responses that were consistent over time, whereas about one-fourth showed improvement and one-fourth showed worsening. This distribution of trends is interesting and warrants further study to determine why individuals reveal different temporal patterns with respect to scores that describe the impact of their tinnitus.
We also presented data showing comparisons of THI-S index scores obtained with the PDA versus those obtained using paper-and-pencil before and after the EMA period. These comparisons showed that the paper-and-pencil (traditional) score was within 1–2 points of the PDA average of scores for 41.7% of the participants (Fig. 3a). However, for 45.8% the traditional method overestimated tinnitus severity compared to the PDA scores, while for 12.5% the traditional method underestimated tinnitus severity compared to the PDA scores. These are not straightforward comparisons because of the high variability of the repeated scores obtained with the PDA. This high variability resulted in at least one PDA score that was lower than the traditional score for all of the participants (Fig. 3b), and in at least one PDA score that was higher than the traditional score for most of the participants (Fig. 3c). Based on these comparisons, it appears that administering a retrospective tinnitus questionnaire does a reasonable job of estimating the average life impact of tinnitus for many/most patients, but for a subset of patients the questionnaire score over- or underestimates life impact. Further, the variability in how tinnitus affects an individual over time is not captured with a retrospective questionnaire that relies on recall.
Potential Use of EMA to Assess Outcomes of Intervention for Tinnitus
The EMA protocol we have tested exemplifies how EMA can potentially be used to assess outcomes of tinnitus intervention studies. An important question in this regard is whether the fluctuations seen in the THI-S index score (see Appendix A, Supplemental Digital Content 1) represent actual changes in the degree of tinnitus impact versus normal test-retest variability of the measure.
The test-retest reliability of a questionnaire reflects the instrument’s ability to provide equivalent scores when an individual completes the test multiple times—in the absence of any intervention that might be expected to affect the score. Normally, an instrument is administered to individuals on two occasions separated by about 2 weeks. The authors of the THI-S conducted such testing, with a mean of 16 days between the two administrations (Newman et al. 2008). Results of their testing revealed a test-retest reliability coefficient of 0.81 for the THI-S, which, according to the authors (p. 279) “met the established statistical criteria (r > 0.80) (Newman et al. 2008) for a test to be considered acceptable for clinical purposes (Nunnally 1978a).” The authors further determined that a change of more than 10 points was necessary “to demonstrate a true change in global perceived tinnitus before and after clinical intervention” (Newman et al. 2008) (p. 280).
Many tinnitus questionnaires require patients to provide responses reflecting a specified period of time leading up to the moment of assessment. In essence, patients are asked to average their experiences and feelings over a time period. With the THI-S, no such instructions are provided (Newman et al. 2008), so patients can respond with respect to any time period they feel is appropriate. Participants in the present study completed the THI-S repeatedly during EMA testing, and were instructed to respond to the questions with respect to the present moment. When responding in this manner, the index scores varied widely for most of the participants, as seen in Appendix A, Supplemental Digital Content 1. In fact, most of the participants provided scores over a range exceeding 10 points, which met the THI-S criteria for “true change in global perceived tinnitus” (Newman et al. 2008) (p. 280). Because these scores reflected the exact moment of testing, and because no intervention was provided, this variation can reasonably be assumed to indicate variation in tinnitus impact across the different times of testing.
In spite of the large variability in individual scores, when these scores were averaged they closely corresponded with the average scores obtained with the paper-and-pencil versions of the THI-S (i.e., from the 10 THI-S questions culled from the 25-item THI that was administered pre- and post-EMA). These results support the validity of EMA testing as an outcome measure to evaluate the variability in distress associated with tinnitus. Thus, for tinnitus intervention studies EMA testing might provide an additional level of detail that could elucidate daily fluctuations in how patients are bothered by tinnitus. These results also have implications for clinical application, i.e., patients undergoing intervention for tinnitus could eventually be assessed using some type of an EMA protocol.
Limitations of the Study
An inherent limitation with EMA in general is that each assessment must be completed in 3 minutes or less to minimize the burden of responding (Stone & Shiffman 2002). Each assessment thus is limited with respect to the amount of information that can be obtained. In spite of this limitation, each assessment needed to determine: (a) tinnitus-relevant circumstances; (b) tinnitus characteristics; (c) emotional affect; and (d) an index score from a validated tinnitus questionnaire. Nine questions were developed to accomplish objectives a, b, and c (Table 1). For objective d, we chose the THI-S (Newman et al. 2008) from numerous questionnaires having validated psychometric properties. The THI-S uses only 10 questions to generate an index score, in contrast with the 25–50 questions that are included in most of the other questionnaires (Newman & Sandridge 2004).
A disadvantage of using the THI-S was its limited number of response items, which cannot adequately address the multiplicity of problems that can be associated with problematic tinnitus (Meikle & Walsh 1984; Stouffer & Tyler 1990). Further, it has been argued that the response format of the THI-S (as well as the THI) does not adequately discriminate between different levels of tinnitus impact (Tyler, Oleson, Noble, Coelho, & Ji 2007). That is, the response choices of “yes,” “sometimes,” and “no” limit the instrument’s ability to determine gradations of tinnitus severity that exist on a continuum. As recommended by Nunnally (1978b), a response scale of 7 to 11 levels may be optimal for maximum reliability when discriminating different severity levels. In spite of these limitations, the THI-S is documented for psychometric adequacy, and compares well with the full 25-item THI (Newman et al. 2008).
We have mentioned that EMA responses can reflect either the moment of responding or the time period since the last momentary assessment. We opted to assess the immediate experience to ensure that responses were unaffected by recall bias and thus were as accurate as possible. A concern with this immediate-experience strategy is that sleep disturbance is one of the most common problems reported by patients with tinnitus (Axelsson & Ringdahl 1989; Tyler & Baker 1983). Further, patients who report sleep disturbance tend to be the most impacted by their tinnitus (Erlandsson, Hallberg, & Axelsson 1992; Folmer & Griest 2000). Thus, any tinnitus assessment should include questions about sleep. The THI-S includes the question “Because of your tinnitus, do you have trouble falling asleep at night?” This question was asked with each momentary assessment, but did not address whether sleep was disrupted by tinnitus the previous night. EMA has the capability of assessing problems both falling asleep and staying asleep during the previous night. Since these problems are so commonly reported by patients with tinnitus it is essential that further use of EMA to evaluate effects of tinnitus assessed upon awakening include questions that assess sleep disturbances caused by tinnitus during the previous night.
The convenience sample used in this study imposed limitations that should be mentioned. The participants were predominantly male Veterans. These Veterans tended to be older (50s and 60s) and only 25% of them were employed. This sample thus represented a group that may have been ideal for complying with the EMA protocol. Future studies should include equal numbers of women and men who are distributed across age decades. It also would be important to determine age limits and other factors that would determine suitability for EMA testing. For example, children below a certain age would not be able to perform the task, and work and lifestyle factors would preclude testing during certain periods of time.
Future Directions
In spite of this study’s limitations, the positive findings suggest that it would be appropriate to conduct studies that further verify the use of EMA with individuals who experience bothersome tinnitus. The use of EMA methodology eventually could have application for routine assessment of patients who receive hearing health care services for tinnitus. The advantages of such an approach would be to obtain real-life measures of tinnitus distress, and to determine within- and between-day variability in this distress and associated factors. Such information currently is not available from patients who seek tinnitus services. It seems likely that having this information would lead to more targeted interventions and improved outcomes.
Similarly, EMA protocols could be used to assess outcomes of hearing aid use and of auditory rehabilitation. Such assessments would provide intra- and inter-day data describing circumstances of use (and non-use) of hearing aids, satisfaction/dissatisfaction with hearing aids, difficulties encountered, tools used, and any other information considered important to optimize the benefit of hearing aids and auditory rehabilitation. EMA protocols could be designed to perform standardized assessments or to obtain specific information to assist in identifying areas of difficulty for patients. This kind of detailed information collected in the patient’s normal listening environment is currently not available to audiologists and could be of significant value for optimizing outcomes.
We anticipate the technological underpinnings of portable computing devices will continue to converge with those of ear-level tinnitus devices and hearing aids (e.g., Bluetooth capability or real-time data storage; see Boothroyd et al. 2007), thus it will soon be possible to integrate such therapeutic devices with assessment tools used in EMA. This could give us opportunities to observe simultaneous streams of objective data (e.g., measures of ambient noise, indicators of physiological stress) and subjective data (e.g., reports of listening effort or behaviors for modifying environmental conditions to improve communication). Such findings could dramatically improve understanding of real life circumstances and facilitate the development and selection of rehabilitation interventions.
The availability of EMA technology has the potential to greatly advance hearing health care. Portable, pocket-sized electronic devices have become ubiquitous during the last decade with public use of MP3 players and cell phones now commonplace. The more recent proliferation of smartphones (cell phones with internet connectivity and programmability) has created the means to incorporate EMA into devices that are already in use by patients. It is thus envisioned that, in the future, patients complaining of hearing loss or tinnitus could download an application onto their smartphone supporting automatic administration of patient-guided momentary assessments. Results of these assessments would be made available to the audiologist at each clinical appointment, providing a complete and accurate description of the patient’s auditory difficulties during their full course of treatment. Such a protocol would greatly improve on the normal clinical procedures of obtaining case history and patients completing questionnaires, changing hearing aid settings, and for counseling individuals about communication strategies specific to their life style and listening situations.
Assessment of outcomes in tinnitus research is limited to the use of questionnaires that assess experiences and feelings retrospectively. The approach of ecological momentary assessment (EMA) circumvents recall biases because participants are asked about immediate experiences in their natural environment. This pilot study was conducted to explore the feasibility of using EMA methods to examine within- and between-day effects of tinnitus. A personal digital assistant (PDA) was programmed to perform EMA four times per day for 14 days. Twenty-four participants completed testing and demonstrated the feasibility of using this approach.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Erin Conner for her work as a research assistant during the first half of this project. The contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government.
Sources of support:
Research Grant from the National Institute on Deafness and Other Communications Disorders (1R03DC009012-01A1)
Research Career Scientist Award from VA Rehabilitation Research and Development Service for JAH (F7070S)
Administrative support and facilities provided by:
VA National Center for Rehabilitative Auditory Research, Portland, OR
Oregon Health & Science University, Portland, OR
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Appendix A, Supplemental Digital Content 1. For each of the 24 Phase 3 participants, individual THI-S scores obtained from the PDA are plotted across the 14-day EMA period.
Appendix B, Supplemental Digital Content 2. For each of the 24 Phase 3 participants, daily means of the THI-S scores obtained from the PDA are plotted across the 14-day EMA period. Each mean normally consists of the mean of four THI-S index scores obtained for a single day. In some cases there were less than four means, depending on how many times the participant completed the surveys. Since compliance was approximately 90%, only about 10% of the points reflect means based on less than four THI-S scores.
REFERENCES
- Axelsson A, Ringdahl A. Tinnitus: A study of its prevalence and characteristics. British Journal of Audiology. 1989;23:53–62. doi: 10.3109/03005368909077819. [DOI] [PubMed] [Google Scholar]
- Beal DJ, Weiss HM. Methods of ecological momentary assessment in organizational research. Organizational Research Methods. 2003;6(4):440–464. [Google Scholar]
- Boothroyd A, Fitz K, Kindred J, Kochkin S, Levitt H, Moore B, et al. Hearing aids and wireless technology. Hearing Review. 2007;14(6):44–47. [Google Scholar]
- Cruise CE, Broderick J, Porter L, Kaell A, Stone AA. Reactive effects of diary self-assessment in chronic pain patients. Pain. 1996;67(2–3):253–258. doi: 10.1016/0304-3959(96)03125-9. [DOI] [PubMed] [Google Scholar]
- Davis A, Refaie AE. Epidemiology of tinnitus. In: Tyler R, editor. Tinnitus Handbook. San Diego: Singular Publishing Group; 2000. pp. 1–23. [Google Scholar]
- Davis PB, Paki B, Hanley PJ. Neuromonics tinnitus treatment: Third clinical trial. Ear and Hearing. 2007;28(2):242–259. doi: 10.1097/AUD.0b013e3180312619. [DOI] [PubMed] [Google Scholar]
- Dobie RA. Clinical trials and drug therapy for tinnitus. In: Snow JB, editor. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004a. pp. 266–277. [Google Scholar]
- Dobie RA. Overview: suffering from tinnitus. In: Snow JB, editor. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004b. pp. 1–7. [Google Scholar]
- Erlandsson SI, Hallberg LRM, Axelsson A. Psychological and audiological correlates of perceived tinnitus severity. Audiology. 1992;31:168–179. doi: 10.3109/00206099209072912. [DOI] [PubMed] [Google Scholar]
- Erskine A, Morley S, Pearce S. Memory for pain: a review. Pain. 1990;41(3):255–265. doi: 10.1016/0304-3959(90)90002-U. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons, Inc.; 2004. [Google Scholar]
- Folmer RL, Griest SE. Tinnitus and insomnia. American Journal of Otolaryngology. 2000;21(5):287–293. doi: 10.1053/ajot.2000.9871. [DOI] [PubMed] [Google Scholar]
- Galvez G, Turbin MB, Thielman EJ, Istvan JA, Andrews JA, Henry JA. Feasibility of ecological momentary assessment of hearing difficulties encountered by hearing aid users. Ear & Hearing (in review) 2011 doi: 10.1097/AUD.0b013e3182498c41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Stone AA. Recall biases and cognitive errors in retrospective self-reports: A call for momentary assessments. In: Baum A, Revenson T, Singer J, editors. Handbook of Health Psychology. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2004. pp. 405–413. [Google Scholar]
- Henry JA, Dennis K, Schechter MA. General review of tinnitus: Prevalence, mechanisms, effects, and management. Journal of Speech, Language, and Hearing Research. 2005;48(5):1204–1234. doi: 10.1044/1092-4388(2005/084). [DOI] [PubMed] [Google Scholar]
- Henry JA, Meikle MB. Psychoacoustic measures of tinnitus. Journal of the American Academy of Audiology. 2000;11:138–155. [PubMed] [Google Scholar]
- Henry JA, Zaugg TL, Myers PJ, Schechter MA. The role of audiologic evaluation in Progressive Audiologic Tinnitus Management. Trends in Amplification. 2008;12(3):169–184. doi: 10.1177/1084713808319941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JA, Zaugg TL, Myers PM, Kendall CJ. Progressive Tinnitus Management: Clinical Handbook for Audiologists. San Diego, CA: Plural Publishing; 2010. [Google Scholar]
- Hoffman HJ, Reed GW. Epidemiology of tinnitus. In: Snow JB, editor. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004. pp. 16–41. [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: an example using undergraduate problem drinkers. Psychol Addict Behav. 2002;16(3):205–211. [PubMed] [Google Scholar]
- Jakes SC, Hallam RS, Chambers C, Hinchcliffe R. A factor analytical study of tinnitus complaint behaviour. Audiology. 1985;24:195–206. doi: 10.3109/00206098509070103. [DOI] [PubMed] [Google Scholar]
- Jastreboff PJ, Hazell JWP. Treatment of tinnitus based on a neurophysiological model. In: Vernon JA, editor. Tinnitus Treatment and Relief. Needham Heights: Allyn & Bacon; 1998. pp. 201–217. [Google Scholar]
- Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. New York: Cambridge University Press; 2004. [Google Scholar]
- Krueger RA. Analyzing and reporting focus group results. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Levine RA. Somatic tinnitus. In: Snow JB, editor. Tinnitus: Theory and management. Lewiston, NY: BC Decker Inc.; 2004. pp. 108–124. [Google Scholar]
- Martinez Devesa P, Waddell A, Perera R, Theodoulou M, editors. Cognitive behavioural therapy for tinnitus (Review), Cochrane Database of Systematic Reviews 2007, Issue 1. 2007 doi: 10.1002/14651858.CD005233.pub2. [DOI] [PubMed] [Google Scholar]
- Meikle M, Schuff N, Griest S. Intra-subject variability of tinnitus: observations from the tinnitus clinic. In: Feldmann H, editor. Proceedings III International Tinnitus Seminar, Münster. Karlsruhe: Harsch Verlag; 1987. pp. 175–180. [Google Scholar]
- Meikle M, Walsh ET. Proceedings of the Second International Tinnitus Seminar, New York 1983The Journal of Laryngology and Otology. Ashford, Kent: Invicta Press; 1984. Characteristics of tinnitus and related observations in over 1800 tinnitus patients; pp. 17–21. [DOI] [PubMed] [Google Scholar]
- Meikle MB, Vernon J, Johnson RM. The perceived severity of tinnitus. Otolaryngology–Head and Neck Surgery. 1984;92(6):689–696. doi: 10.1177/019459988409200617. [DOI] [PubMed] [Google Scholar]
- Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology–Head and Neck Surgery. 1996;122:143–148. doi: 10.1001/archotol.1996.01890140029007. [DOI] [PubMed] [Google Scholar]
- Newman CW, Sandridge SA. Tinnitus questionnaires. In: Snow JB, editor. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004. pp. 237–254. [Google Scholar]
- Newman CW, Sandridge SA, Bolek L. Development and psychometric adequacy of the screening version of the tinnitus handicap inventory. Otol Neurotol. 2008;29(3):276–281. doi: 10.1097/MAO.0b013e31816569c4. [DOI] [PubMed] [Google Scholar]
- Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. Journal of the American Academy of Audiology. 1998;9:153–160. [PubMed] [Google Scholar]
- Nunnally JC. 2 ed. New York, NY: McGraw Hill; 1978. Psychometric Theory. [Google Scholar]
- O'Brien K. Improving survey questionnaires through focus groups. In: Morgan DL, editor. Successful focus groups: Advancing the state of the art. Thousand Oaks, CA: Sage; 1993. pp. 105–117. [Google Scholar]
- Powell RA, Single HM, Lloyd KR. Focus groups in mental health research: Enhancing the validity of user and provider questionnaires. Intern J Soc Psychiat. 1996;42:193–206. doi: 10.1177/002076409604200303. [DOI] [PubMed] [Google Scholar]
- Reis HT, Gable SL. Event-sampling and other methods for studying everyday experience. In: Reis HT, Judd C, editors. Handbook of Research Methods in Social and Personality Psychology. Cambridge, England: Cambridge University Press; 2000. pp. 190–223. [Google Scholar]
- Schwarz N, Sudman S. Autobiographical Memory and the Validity of Retrospective Reports. New York: Springer-Verlag; 1994. [Google Scholar]
- Scollon CN, Kim-Prieto C, Diener E. Experience sampling: Promises and pitfalls, strengths and weaknesses. Journal of Happiness Studies. 2003;4:5–34. [Google Scholar]
- Searchfield GD, Kaur M, Martin WH. Hearing aids as an adjunct to counseling: tinnitus patients who choose amplification do better than those that don't. Int J Audiol. 2010;49(8):574–579. doi: 10.3109/14992021003777267. [DOI] [PubMed] [Google Scholar]
- Stone A, Turkkan J, Jobe J. The Science of Self Report. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2000. al., E. [Google Scholar]
- Stone AA, Broderick JE, Schwartz JE, Shiffman S, Litcher-Kelly L, Calvanese P. Intensive momentary reporting of pain with an electronic diary: reactivity, compliance, and patient satisfaction. Pain. 2003;104(1–2):343–351. doi: 10.1016/s0304-3959(03)00040-x. [DOI] [PubMed] [Google Scholar]
- Stone AA, Kessler RC, Haythornthwaite JA. Measuring daily events and experiences: decisions for the researcher. J Pers. 1991;59(3):575–607. doi: 10.1111/j.1467-6494.1991.tb00260.x. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Capturing momentary, self-report data: a proposal for reporting guidelines. Ann Behav Med. 2002;24(3):236–243. doi: 10.1207/S15324796ABM2403_09. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. BMJ. 2002;324(7347):1193–1194. doi: 10.1136/bmj.324.7347.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. Journal of Speech and Hearing Disorders. 1990;55:439–453. doi: 10.1044/jshd.5503.439. [DOI] [PubMed] [Google Scholar]
- Tyler RS, Baker LJ. Difficulties experienced by tinnitus sufferers. Journal of Speech and Hearing Disorders. 1983;48:150–154. doi: 10.1044/jshd.4802.150. [DOI] [PubMed] [Google Scholar]
- Tyler RS, Oleson J, Noble W, Coelho C, Ji H. Clinical trials for tinnitus: study populations, designs, measurement variables, and data analysis. Prog Brain Res. 2007;166:499–509. doi: 10.1016/S0079-6123(07)66048-8. [DOI] [PubMed] [Google Scholar]
- Vernon JA, Meikle MB. Tinnitus masking. In: Tyler RS, editor. Tinnitus Handbook. San Diego: Singular Publishing Group; 2000. pp. 313–356. [Google Scholar]
- Vogt DS, King DW, King LA. Focus groups in psychological assessment: enhancing content validity by consulting members of the target population. Psychol Assess. 2004;16(3):231–243. doi: 10.1037/1040-3590.16.3.231. [DOI] [PubMed] [Google Scholar]
- Wackym PA, Friedland DR. Otologic evaluation. In: Snow JB, editor. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004. pp. 205–219. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.