Abstract
Objective: This study evaluated the safety and efficacy of sublative fractional bipolar radiofrequency and bipolar radio frequency combined with diode laser for the treatment of both superficial and deep acne scars in patients with skin types II to V. Design: Prospective, single-center study. Subjects received up to five treatments with sublative fractional bipolar radiofrequency and bipolar radiofrequency combined with diode laser. Treatments were directed to at least two facial (forehead, perioral, cheeks) and/or neck areas with acne scars at four-week intervals. Treatment parameters on each subject were based on skin type and on skin responses to test spots on the target area just before treatment. Setting: Physician office. Participants: Subjects (n=20, aged 40.7±10.5 years [mean ± SD], skin types II–V) with acne scars and without acne lesions enrolled in this prospective study. Measurements: Results were evaluated just before each treatment and at four and 12 weeks after the final treatment using the Goodman Scar Scale, a quantitative method of evaluating scars that attempts to reduce grading subjectivity, as well as by patient satisfaction. Results: Acne scars improved significantly one month after three treatments and improvement persisted for at least 12 weeks after the fifth treatment. Improvement was not affected by skin type. Adverse effects were limited to transient erythema and edema. Conclusion: The combination of diode laser and bipolar radiofrequency energy device in addition to fractionated sublative radiofrequency is a safe and statistically significantly effective combined modality for the treatment of both superficial and deep acne scars in patients with skin types II to V with minimal downtime and no significant side effects.
Introduction
Acne scars have multiple morphologies1 and often require different technical approaches to achieve an optimal cosmetic outcome, especially in dark-skinned subjects.2 Acne scars are commonly classified as ice pick, rolling, or boxcar.1 Ice pick scars have traditionally been treated by punch excision, subcision, or chemical reconstruction of skin scars (CROSS) technique with 100% trichloroacetic acid3; rolling scars by subcision and/or laser resurfacing; boxcar scars by punch elevation, subcision, and/or laser resurfacing; deep boxcar scars by punch excision; and shallow boxcar scars by laser resurfacing. Combinations of modalities may also be required.4
Dermabrasion is very effective in the treatment of scars, but is not widely used due to blood spattering and the need for a high skill level to produce excellent results. Chemical peels, which are most effective against macular scars,5 are associated with variable levels of improvement. Biomaterials such as collagen, hyaluronic acid (HA), autologous fat, or other fillers offer transient improvement,4,6–8 but are often used for focal rolling scars. Subdermal minimal surgery has recently been introduced,9 which is performed by pneumatically accelerating a carrier fluid jet containing high-mass molecules of HA. These molecules then disperse into the skin under the targeted scar.
For the past 10 years, the mainstays of acne scarring therapy have been nonablative and ablative lasers. Newer fractional technologies have advanced the treatment of acne scarring significantly, as they are able to reach the dermal layer yet have a relatively low side-effect profile. These technologies may even be used safely in dark skin.2 Laser procedures are effective against boxcar scars and rolling scars.5 The ablative devices, such as the CO2 and erbium-doped yttrium aluminium garnet (Er:YAG) lasers,10 are effective, but may be associated with long recovery times and side effects including postinflammatory hyperpigmentation. They can, however, be used successfully in dark skin.11
Nonablative devices include the neodymium-doped yttrium aluminium garnet (Nd:YAG) and diode lasers, long-pulsed 1450nm diode, the 1320 and 1064nm Nd:YAG, and 1540nm erbium glass lasers,5,12 although careful attention must be paid to parameters in Asian skin types.13 Although side effects and recovery times with nonablative lasers are reduced compared to ablative lasers, multiple treatments are required to reach significant efficacy. Examples include the 1550nm fractional erbium-doped laser14–16 and the 1540nm fractional laser.17
Recent reports have presented objective evidence of the efficacy of devices that combine ablative with nonablative fractional technology for the treatment of acne scars.18–23 A relatively new modality uses fractionated bipolar radiofrequency (RF) energy, which has been shown to improve mild rhytids, skin texture, smoothing, and tightening.24,25 This treatment—sublative rejuvenation (SR)—provides a coagulative (nonablative) effect limited to the mid-dermis in addition to an ablative injury to less than five percent of the epidermis. The advantages of this modality are reduced down time, lack of interaction with melanin, and low side-effect profile. One prior evaluation with similar technology has been published for acne scars.26
The current article seeks to ascertain the efficacy and safety of SR in addition to a diode laser/bipolar RF (DLRF) energy for the treatment of both superficial and deep acne scars in skin types II to V.
Methods
Subjects. Healthy men and women (n=20, 8 men/12 women, aged 40.7±10.5 years [mean ± SD], skin types II–V) with acne scars successfully enrolled in the study. All female subjects were postmenopausal, surgically sterilized, or used an acceptable form of birth control for at least three months before the study began. All subjects provided signed informed consent. Exclusion criteria were active acne; pregnancy; breastfeeding; active electrical implant; permanent facial implant; injectable filler in area to be treated within nine months of investigation; surgical, chemical, or light-based facial treatments in the past six months; isotretinoin treatment within six months; immunosuppression; currently tanned or unable to refrain from tanning within the investigation period; or any dermatological, hormonal, or medical condition (or history) or therapy that might compromise a subject's safety or interfere with interpretation of the study results.
Treatment device. Treatment of acne scars consisted of irradiation with a combination of biopolar RF and 915nm diode laser energy (Matrix IR, Syneron Medical Ltd., Yokneam, Israel) (DLRF) followed by sublative bipolar RF energy (Matrix RF, Syneron)(SR). Both applicator handpieces derived energy from a common platform (eLaser, Syneron).
The DLRF device was designed to create a focal coagulation of tissue at approximately 1.5mm skin depth to stimulate collagenesis (Figure 1), thereby elevating the deeper area of the scar.27 The SR energy enters the dermis through ablation caused by rows of electrode pins on the square disposable tip (Figure 2). The nonablative dermal heating is a combination of coagulative damage and a subcoagulative heat effect (Figure 3), causing dermal remodeling. DLRF was included in this study because the authors hypothesized that this could be beneficial in treating ice pick scars due to the device design since these types of scars have proven particularly difficult to treat28 and many individuals presenting for treatment of acne scarring have multiple types of scarring (i.e., rolling, ice pick, boxcar).
Figure 1.
Schematic of Combination Bipolar Matrix Array and Bi-Polar RF (DLRF). The intersection of the two modalities creates thermal bands at 1.5mm into the dermis causing collagen contraction. Figure courtesy of Syneron Medical LTD.
Figure 2.
Sublative Rejuvenation Disposable Tips and Schematic. Radiofrequency current flows between the positive and negative mini-electrodes. Control of this current allows varying degrees of tissue impact. In the space of no current flow a healing reservoir is obtained. Image courtesy of Syneron Medical LTD.
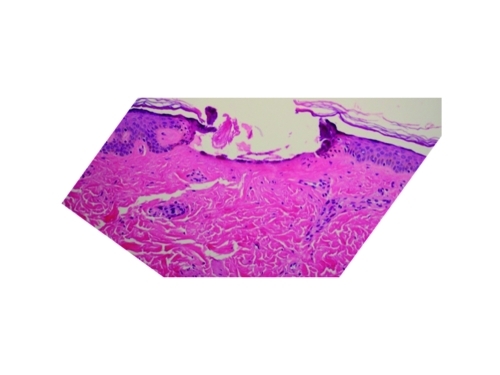
Figure 3.
Photomicrograph of skin wound taken immediately after sublative rejuvenation pulse. Note clean ablation of epidermis and upper dermis with slight coagulation of the upper dermis. Photomicrograph courtesy of Syneron Medical LTD.
Study design. In this prospective study, subjects with acne scars received up to five treatments in at least two facial (or neck) areas at four-week intervals. Areas treated included the cheeks, forehead, perioral, and neck. Target areas were washed with mild soap and water before DLRF treatment. After a layer of conductive gel was applied to the target areas, subjects received 3 to 4 lesional passes. Treatment parameters on each subject were based on skin type and skin responses to test spots on the target area just before treatment, with clinical endpoints being erythema and edema. DLRF laser fluence ranged from 40 to 85J/cm2 and RF fluence ranged from 50 to 100J/cm3. No anesthetic was used for this portion of the treatment. When DLRF treatment was completed, the conductive gel was removed and the treated areas were allowed to cool at room temperature for 30 minutes, after which topical anesthesia (prilocaine [7%] and lidocaine [7%]) was applied for 30 minutes. The skin was then cleansed with acetone, alcohol, and water; patted dry; and left to air dry for 10 minutes. These areas were then treated with SR with fluence (17–25J/cm3/pin) determined by skin response to a test spot. Epidermal ablation was five percent in each area treated, with dermal coagulation area directly proportional to the energy of the RF (Figure 4).
Figure 4.
Thirty-six hours after treatment, note crust formation and deep dermal coagulation and remodeling. Reprinted with permission from: Hruza G, et al. Skin rejuvenation and wrinkle reduction using a fractional radiofrequency system.
J Drugs Dermatol. 2009;8(3): 259–265.
Post-treatment care consisted of application of petrolatum and sunscreen. Subjects were instructed to avoid exfoliants, to not excoriate healing lesions, to avoid tanning salons and sun, and to use sunscreen (sun protection factor [SPF 30]) during the entire study period.
Evaluation of results. Efficacy and adverse effects were assessed by physical examination at each treatment visit and at the 4- and 12-week follow-up visits. The evaluation was one month after treatment three and immediately before treatment four. Other assessments were made as shown in Table 1. Scars were evaluated at each time point using the scale in Table 2. Differences were evaluated for significance by Friedman's test, the Wilcoxon Signed-Rank test, the Mann-Whitney test, and Pearson's chi square test.
TABLE 1.
Study protocol
| EVALUATION TOOL | VISIT | ||||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T5 | 4-WEEK FOLLOW UP | 12-WEEK FOLLOW UP | |
| *Photography | X | X | X | X | X | X | X |
| *Assessment of scars and texture | X | X | X | X | X | X | X |
| †Comfort during treatment | X | X | X | X | X | ||
| *Subject satisfaction, improvement | X | X | X | X | |||
| Adverse events | X | X | X | X | X | X | X |
Before treatment
After treatment
- T
treatment
TABLE 2.
Global acne scarring classification29
| (GRADE) TYPE | NUMBER OF LESIONS 1 (1–10) | NUMBER OF LESIONS 2 (111–0) | NUMBER OF LESIONS 3 (>20) |
|---|---|---|---|
| (A) Milder scarring (1 point each) | |||
| • Macular erythematous or pigmented | 1 point | 2 points | 3 points |
| • Mildly atrophic dish-like | |||
| (B) Moderate scarring (2 points each) | |||
| • Moderately atrophic dish-like | |||
| • Punched out with shallow bases small scars (< 5mm) | 2 points | 4 points | 6 points |
| • Shallow but broad atrophic areas | |||
| (C) Severe scarring (3 points each) | |||
| • Punched out with deep but normal bases, small scars (< 5mm) | |||
| • Punched out with deep abnormal bases, small scars (<5 mm) | 3 points | 6 points | 9 points |
| • Linear or troughed dermal scarring | |||
| • Deep, broad atrophic areas | |||
| (D) Hyperplastic papular scars | 2 points | 4 points | 6 points |
| (D) Hyperplastic keloidal, hypertrophic scars | Area <5cm2 6 points | Area 5–20 cm2 12 points | Area >20 cm2 18 points |
Reproduced with permission from Goodman GJ, Baron JA. Postacne scarring—a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5(1):48–52.29
Results
Scar and scar texture scores.
Scars. Scars on the cheeks, perioral area, forehead, and neck were assessed at each visit according to the scale in Table 2. Scores of the four anatomical areas were combined for non-parametric statistical analysis. The median scar assessment scores at each visit are shown in Table 3. A graph of the scar scores is presented in Figure 5.
TABLE 3.
Median (IQR) scar scores (cheek, perioral, forehead, neck) at each visit
| VISIT | SCAR SCORE | PVALUE* |
|---|---|---|
| T1 | 15.0 (8.3) | — |
| T2 | 11.0 (6.0) | 0.0775 (ns) |
| T3 | 11.0 (6.7) | 0.0100 (ns) |
| T4 | 9.0 (5.7) | 0.0002 (s) |
| T5 | 9.5 (6.3) | <0.0001 (s) |
| 4-WEEK FOLLOW UP | 9.5 (4.6) | <0.0001 (s) |
| 12-WEEK FOLLOW UP | 9.0 (6.0) | 0.0001 (s) |
- IQR
interquartile range, a measure of dispersion
- T
treatment
- s
significant
- ns
not significant
Compared with baseline (T1), Wilcoxon Signed-Rank test
Figure 5.
Average Goodman Scar Score Over Time. Patients with at least three treatments versus patients with five treatments. *=statistical significance.
Friedman's test (a nonparametric equivalent to the repeated measures analysis of variance) for the treatment 1 (T1) through T5, four-week follow-up, and 12-week follow-up visit groups showed that the median scar assessments among the seven groups differed significantly (p<0.0001). Friedman's test, however, does not specify which among the six non-baseline groups differs significantly from baseline (T1). Wilcoxon Signed-Rank Rank comparisons of each treatment group with baseline (T1) revealed treatment groups in which the median scar assessment score differed significantly from baseline. The p values are presented in Table 3.
The data show that the median scar scores at the T4, T5, four-week follow-up, and 12-week follow-up visits were significantly lower than the median scar score at baseline. Since six comparisons with baseline were made, the Bonferroni correction was applied to obtain the appropriate cutoff level. The traditional level (p=0.05) was adjusted by dividing 0.05 by six, the number of comparisons with baseline. With the new p=0.0083 cutoff level, the median scar scores of only the four previously mentioned groups differed significantly from baseline.
The effect of skin type on improvement in scar assessment scores at 12 weeks compared to baseline was evaluated by the Mann-Whitney test. Data were divided into two categories: Skin types II through III and skin types IV through VI. The analysis showed that the median scores of the two groups did not differ significantly (p=0.9758), indicating that the scar assessment scores are not affected by skin type. Early in the study it appeared that people with darker skin types were getting better results than Caucasians (Figure 6), but this difference did not persist after the treatments were completed. Clinical examples of patients after treatment series are presented in Figures 7, 8, and 9.
Figure 6.
The mean acne score for each ethnicity at baseline is compared to the mean acne scar for each ethnicity one month after completing three treatments. The number of patients in each ethnicity group was Caucasian=10, Hispanic/Latino=4, Asian/Pacific Islander=3, Indian/Middle Eastern=2, and Caucasian and Middle Eastern (she is Fitzgerald skin type III)=1.
Figure 7.
Hispanic study patient before and one month after three treatments of SR and DLRF
Figure 8.
Same patient as Figure 7, opposite cheek view. Hispanic patient before and one month after three treatments
Figure 9.
East Indian study patient before and one month after five treatments of SR and DLRF
Scar texture. Pearson's chi square test was used to evaluate scar texture because texture consisted only of two groups—rough and regular. The comparative data are presented in Table 4.
TABLE 4.
Distribution of subjects among rough and regular scar texture groups and comparison with baseline (T1)
| TEXTURE | VISIT | ||||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T5 | 4-WEEK FOLLOW UP | 12-WEEK FOLLOW UP | |
| ROUGH | 19 | 13 | 12 | 7 | 1 | 2 | 1 |
| REGULAR | 8 | 14 | 15 | 20 | 23 | 22 | 24 |
| P value | p=0.0966 (ns) | p=0.0541 (ns) | p=0.0011 (s) | p=<0.0001 (s) | p=<0.0001 (s) | p=<0.0001 (s) | |
- T
treatment
- s
significant
- ns
not significant
The analyses show that the proportions of scar texture scores at the T4 (1 month after the 3rd treatment and just before the 4th treatment), T5, four-week follow-up, and 12-week follow-up visits all differed significantly from baseline (T1). The data indicate that texture improves for more subjects with continued treatment up to T5, in which all but one subject achieved regular texture, and that the effects persist for at least 12 weeks after T5 in nearly all subjects.
Subject grading. Subjects graded acne scars, skin texture, coloration, and overall improvement at T3, T5, four weeks, and 12 weeks, using the following scale: 0=no improvement, worsening; 1=slight improvement; 2=moderate improvement; 3=good improvement; 4=excellent improvement.
For acne scars, at least moderate improvement was achieved by 50 percent of subjects at T3, 75 percent of subjects at T5, 58 percent of subjects at four weeks, and 63 percent of subjects at 12 weeks. These data suggest a trend toward maximum improvement in acne scars at T5 and persistence of the improvement in most subjects for at least 12 weeks. For skin texture, at least moderate improvement was achieved by 60 percent of subjects at T3, 62 percent of subjects at T5, 68 percent of subjects at four weeks, and 60 percent of subjects at 12 weeks.
For coloration, at least moderate improvement was achieved by 43 percent of subjects at T3, 46 percent of subjects at T5, 58 percent of subjects at four weeks, and 58 percent of subjects at 12 weeks. These data suggest a trend toward maximum improvement in coloration at four weeks and persistence of this level of improvement in most subjects for at least an additional eight weeks. For overall improvement, at least moderate improvement was achieved by 50 percent of subjects at T3, 69 percent of subjects at T5, 58 percent of subjects at four weeks, and 62 percent of subjects at 12 weeks. These data suggest a trend toward maximum overall improvement at T5 and persistence of the improvement in most subjects for at least 12 weeks.
Subject satisfaction. Subject satisfaction with the treatment and results was evaluated at T3, T5, four weeks, and 12 weeks. Subject responses included “not satisfied,” “somewhat satisfied,” “satisfied,” “very satisfied,” or “extremely satisfied.” The percentage of responses of “satisfied” or better, however, was 55 percent at T3, 69 percent at T5, 58 percent at four weeks, and 50 percent at 12 weeks, suggesting a trend toward peak satisfaction at T5, which may begin to decline at four and 12 weeks.
Tolerance. Discomfort during treatment was evaluated for each modality (DLRF and SR) at each treatment visit using a 5-point scale in which 0=no pain and 4=maximum tolerable pain. Data were evaluated by nonparametric statistics. Median pain scores were usually higher during DLRF treatment than during SR treatment. The median pain scores for DLRF decreased from 2.6 for treatment 1 and to 1.75 for treatment 5. The median scores for SR decreased from 1.55 to 0.75 from treatment 1 to 5.
Side effects and complications. Crust formation and shedding. The duration of the appearance and shedding of treatment-induced crusts was recorded at each treatment visit. Crusts on average appeared within 1 to 2 days after treatment and were shed by 3 to 4 days. Subjects were able to apply makeup effectively on Days 2 to 3.
Edema and erythema. Edema was noted in almost all patients and resolved in 1 to 3 days. Erythema was observed in all patients and resolved within 1 to 2 days. Post-inflammatory hyperpigmentation occurred in one patient with skin type IV but resolved after the next treatment without intervention other than reminding the patient to use sunscreen. No ulcerations, scars, infections, or prolonged or delayed evidence of hyper or hypopigmentation was noted in any patient.
Discussion
To the authors' knowledge, this is the first study to evaluate the combination of diode laser and fractional bipolar RF with sublative fractionated RF for the treatment of acne scars. Ramesh et al26 treated acne scars of 30 subjects (skin types IV–VI) with a Matrix tunable RF device similar to the RF device used in the present study. All subjects were pretreated with oral antibiotics and the acne scars of eight subjects were subjected to subcision before RF treatment. Subjects received up to four treatments at one-month intervals. Adverse effects included a transient burning sensation, edema, and erythema. Crusting was observed on the treated areas. Improvement ranged from 10 to 50 percent at two months and from 20 to 70 percent at six months. Improvement in this study was based on comparison of photographs by two independent observers using a visual analog scale. Subcision appeared to enhance outcomes as reported by patients who had undergone subcision versus patients who had not.
Bipolar RF with a diode laser has been used for nonablative treatment of concave skin irregularities such as atrophic acne scars.30 Unlike laser energy, RF energy is not absorbed by melanin, making this modality potentially safer in subjects with dark skin. Sublative rejuvenation technology attempts to blend ablative and nonablative modalities to create a more effective therapy with less downtime. As with all acne scarring treatments, the deepest and most “bound down” scars are the most difficult to treat. These scars have been treated in the past with punch elevation, excision, subcision, or a combination of these modalities. The bipolar RF device with diode laser is designed to remodel these scars without an epidermal wound by creating a coagulative focal point at 1.5mm where the RF and laser meet, stimulating collagen synthesis at the depth of the scar.27
As stated previously, acne scars have been successfully treated with nonablative and ablative fractional lasers. Prior evaluation of nonablative therapies showed modest success.31–34 The development of the 1550nm Er:YAG laser was an important advance in the treatment of acne scarring by nonablative fractional photothermolysis35 as well as for the treatment of darker skin. However, multiple treatment sessions are necessary to achieve 50- to 75-precent improvement. Ablative lasers have also been successfully utilized in the hopes of reducing the number of treatments required.36 One study showed that combining nonablative with ablative resurfacing produced a better result with fewer complications than ablative resurfacing alone.18 Another study37 compared nonablative (fractional erbium glass) with ablative (fractional carbon dioxide) laser. The ablative laser produced better results after one session, but with considerably more discomfort and downtime.
Additionally, safe and effective treatments for skin of color have become increasingly sought after, leading to usage of other modalities than light in order to avoid the frequent problem of postinflammatory hyperpigmentation. Trying to balance the social downtime, discomfort, efficacy, and safety of energy-based aesthetic treatments has been an important theme over the last 10 years. Sublative rejuvenation is a modality that attempts to answer these aesthetic needs in a different way by utilizing mainly RF and harnessing the novel concept of ablative RF, something that is used frequently in other areas of medicine.
Acne scars are principally dermal. The resurfacing, chemical peels, and diamond fraises of the past aimed to wound the epidermis and the superficial dermis profoundly and thus secondarily promote dermal remodeling. Nonablative erbium glass resurfacing or ablative fractional treatments can penetrate deeply into the dermis making this a more direct method, while promoting faster healing from the reservoir of untreated skin.38 These wounds tend to be straight columns into the dermis, whereas the sublative fractional bipolar RF current creates small epidermal wounds that are much wider in the dermis (Figure 10). The advantage of this in relation to scarring is that the downtime is limited due to minimizing epidermal injury, yet the scar remodeling is still maximized due to the profound direct impact on the dermis. The DLRF combination has a focal point of about 1.5mm, where the laser and RF energies merge and create a focal coagulation at a deep level effect that is probably most important in the treatment of punched out, ice pick, or troughed scars. The nonablative dermal injuries create collagen remodeling that is delayed, mirroring the delayed results in the subjects of the present study.
Figure 10.
Thermal profile at different energies Sublative 64 (.86W/electrode). As the energy is increased, both the depth and diameter of affected tissue increases.
The main advantages of the RF modalities are their lack of side effects, especially in darker skin, and the low social downtime. Although there is crusting for a number of days, it is relatively easy to cover with makeup. Even without makeup, the crusting is not significantly disfiguring. The RF modalities require multiple treatments and the treatments require time before results are seen due to the need for collagen regeneration, which takes 1 to 6 months. The platform used for this study was a prototype; the newer generations have energies that are more than twice the energies that were available to us at the time.
Conclusion
The combination of diode laser and bipolar RF energy along with sublative bipolar RF is a safe and effective modality for the treatment of both superficial and deep acne scars. The encouraging results warrant additional studies to further characterize this modality.
Biography
Dr. Taub is founder and medical director of Advanced Dermatology, Lincolnshire, Illinois; Northwestern University Department of Dermatology, Chicago, Illinois. Dr. Garretson is from Northwestern Memorial Physicians Group; Northwestern University Department of Dermatology, Chicago, Illinois. Disclosure: Dr. Taub was paid to perform the research for this study. The fees were commensurate with only the actual work performed. Dr. Garretson reports no relevant conflicts of interest. This study, as well as the manuscript and statistical assistance, was funded by Syneron Medical LTD.
References
- 1.Jacob CE, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109–117. doi: 10.1067/mjd.2001.113451. [DOI] [PubMed] [Google Scholar]
- 2.Taub AF. Fractionated delivery systems for difficult to treat clinical applications: acne scarring, melasma, atrophic scarring, striae distensae, and deep rhytides. J Drugs Dermatol. 2007;6(11):1120–1128. [PubMed] [Google Scholar]
- 3.Lee JB, Chung WG, Kwahck H, Lee KH. Focal treatment of acne scars with trichloroacetic acid: chemical reconstruction of skin scars method. Dermatol Surg. 2002;28(11):1017–1021. doi: 10.1046/j.1524-4725.2002.02095.x. discussion 1021. [DOI] [PubMed] [Google Scholar]
- 4.Shamban AT, Narurkar VA. Multimodal treatment of acne, acne scars and pigmentation. Dermatol Clin. 2009;27(4):459–471. doi: 10.1016/j.det.2009.08.010. vi. [DOI] [PubMed] [Google Scholar]
- 5.Fabbrocini G, Annunziata MC, D'Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol ResPract. 2010;2010:893080. doi: 10.1155/2010/893080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jemec GB, Jemec B. Acne: treatment of scars. Clin Dermatol. 2004;22(5):434–438. doi: 10.1016/j.clindermatol.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Lee DH, Choi YS, Min SU, et al. Comparison of a 585nm pulsed dye laser and a 1064-nm Nd:YAG laser for the treatment of acne scars: A randomized split-face clinical study. J Am Acad Dermatol. 2009;60(5):801–807. doi: 10.1016/j.jaad.2008.11.883. [DOI] [PubMed] [Google Scholar]
- 8.Beer K. A single-center, open-label study on the use of injectable poly-L-lactic acid for the treatment of moderate to severe scarring from acne or varicella. Dermatol Surg. 2007;33(Suppl 2):S159–S167. doi: 10.1111/j.1524-4725.2007.33356.x. [DOI] [PubMed] [Google Scholar]
- 9.Lee JW, Kim BJ, Kim MN, Lee CK. Treatment of acne scars using subdermal minimal surgery technology. Dermatol Surg. 2010;36(8):1281–1287. doi: 10.1111/j.1524-4725.2010.01623.x. [DOI] [PubMed] [Google Scholar]
- 10.Kutlubay Z, Gokdemir G. Treatment of atrophic facial acne scars with the Er:YAG laser: a Turkish experience. J Cosmet Laser Ther. 2010;12(2):65–72. doi: 10.3109/14764171003706141. [DOI] [PubMed] [Google Scholar]
- 11.Manuskiatti W, Triwongwaranat D, Varothai S, et al. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63(2):274–283. doi: 10.1016/j.jaad.2009.08.051. [DOI] [PubMed] [Google Scholar]
- 12.Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysisfor the treatment of atrophic scars. Dermatol Surg. 2007;33(3):295–299. doi: 10.1111/j.1524-4725.2007.33059.x. [DOI] [PubMed] [Google Scholar]
- 13.Chan HH, Manstein D, Yu CS, et al. The prevalence and risk factors of postinflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2007;39(5):381–385. doi: 10.1002/lsm.20512. [DOI] [PubMed] [Google Scholar]
- 14.Hu S, Chen MC, Lee MC, et al. Fractional resurfacing for the treatment of atrophic facial acne scars in asian skin. Dermatol Surg. 2009;35(5):826–832. doi: 10.1111/j.1524-4725.2009.01139.x. [DOI] [PubMed] [Google Scholar]
- 15.Chrastil B, Glaich AS, Goldberg LH, Friedman PM. Second-generation 1,550-nm fractional photothermolysis for the treatment of acne scars. Dermatol Surg. 2008;34(10):1327–1332. doi: 10.1111/j.1524-4725.2008.34284.x. [DOI] [PubMed] [Google Scholar]
- 16.Mahmoud BH, Srivastava D, Janiga JJ, et al. Safety and efficacy of erbium-doped yttrium aluminum garnet fractionated laser for treatment of acne scars in type IV to VI skin. Dermatol Surg. 2010;36(5):602–609. doi: 10.1111/j.1524-4725.2010.01513.x. [DOI] [PubMed] [Google Scholar]
- 17.Yoo KH, Ahn JY, Kim JY, et al. The use of 1540nm fractional photothermolysis for the treatment of acne scars in Asian skin: a pilot study. Photodermatol Photoimmunol Photomed. 2009;25(3):138–142. doi: 10.1111/j.1600-0781.2009.00430.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim S, Cho KH. Clinical trial of dual treatment with an ablative fractional laser and a nonablative laser for the treatment of acne scars in Asian subjects. Dermatol Surg. 2009;35(7):1089–1098. doi: 10.1111/j.1524-4725.2009.01193.x. [DOI] [PubMed] [Google Scholar]
- 19.Chapas AM, Brightman L, Sukal S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40(6):381–385. doi: 10.1002/lsm.20659. [DOI] [PubMed] [Google Scholar]
- 20.Waibel J, Beer K, Narurkar V, Alster T. Preliminary observations on fractional ablative resurfacing devices: clinical impressions. J Drugs Dermatol. 2009;8(5):481–485. [PubMed] [Google Scholar]
- 21.Hantash BM, Bedi VP, Kapadia B, et al. In-vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39(2):96–107. doi: 10.1002/lsm.20468. [DOI] [PubMed] [Google Scholar]
- 22.Hantash BM, Bedi VP, Chan KF, Zachary CB. Ex-vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39(2):87–95. doi: 10.1002/lsm.20405. [DOI] [PubMed] [Google Scholar]
- 23.Wang YS, Tay YK, Kwok C. Fractional ablative carbon dioxide laser in the treatment of atrophic acne scarring in Asian subjects: a pilot study. J Cosmet Laser Ther. 2010;12(2):61–64. doi: 10.3109/14764171003706166. [DOI] [PubMed] [Google Scholar]
- 24.Brightman L, Goldman MP, Taub AF. Sublative rejuvenation: experience with a new fractional radiofrequency system for skin rejuvenation and repair. J Drugs Dermatol. 2009;8(11 Suppl):S9–S13. [PubMed] [Google Scholar]
- 25.Hruza G, Taub AF, Collier SL, Mulholland SR. Skin rejuvenation and wrinkle reduction using a fractional radiofrequency system. J Drugs Dermatol. 2009;8(3):259–265. [PubMed] [Google Scholar]
- 26.Ramesh M, Gopal M, Kumar S, Talwar A. Novel Technology in the Treatment of Acne Scars: the Matrix-tunable Radiofrequency Technology. J Cutan Aesthet Surg. 2010;3(2):97–101. doi: 10.4103/0974-2077.69021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammes S, Greve B, Raulin C. Electrooptical synergy (ELOS) technology for nonablative skin rejuvenation: a preliminary prospective study. J Eur Acad Dermatol Venereol. 2006 Oct.20(9):1070–1075. doi: 10.1111/j.1468-3083.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- 28.Khunger N, Bhardwaj D, Khunger M. Evaluation of CROSS technique with 100% TCAin the management of ice pick acne scars in darker skin types. J Cosmet Dermatol. 2011;10(1):51–57. doi: 10.1111/j.1473-2165.2010.00526.x. [DOI] [PubMed] [Google Scholar]
- 29.Goodman GJ, Baron JA. Postacne scarring—a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5(1):48–52. doi: 10.1111/j.1473-2165.2006.00222.x. [DOI] [PubMed] [Google Scholar]
- 30.Sadick NS, Trelles MA. Nonablative wrinkle treatment of the face and neck using a combined diode laser and RF technology. Dermatol Surg. 2005;31(12):1695–1699. doi: 10.2310/6350.2005.31310. [DOI] [PubMed] [Google Scholar]
- 31.Keller R, Belda Júnior W, Valente NY, Rodrigues CJ. Nonablative 1,064-nm Nd:YAG laser for treating atrophic facial acne scars: histologic and clinical analysis. Dermatol Surg. 2007;33(12):1470–1476. doi: 10.1111/j.1524-4725.2007.33318.x. [DOI] [PubMed] [Google Scholar]
- 32.Yaghmai D, Garden JM, Bakus AD, Massa MC. Comparison of a 1064nm laser and a 1320nm laser for the nonablative treatment of acne scars. Dermatol Surg. 2005;31(8) Pt 1:903–909. doi: 10.1097/00042728-200508000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Chua SH, Ang P, Khoo LS, Goh CL. Nonablative 1450nm diode laser in the treatment of facial atrophic acne scars in type IV to V Asian skin: a prospective clinical study. Dermatol Surg. 2004;30(10):1287–1291. doi: 10.1111/j.1524-4725.2004.30402.x. [DOI] [PubMed] [Google Scholar]
- 34.Tanzi EL, Alster TS. Comparison of a 1450nm diode laser and a 1320nm Nd:YAG laser in the treatment of atrophic facial scars: a prospective clinical and histologic study. Dermatol Surg. 2004;30(2 Pt 1):152–157. doi: 10.1111/j.1524-4725.2004.30078.x. [DOI] [PubMed] [Google Scholar]
- 35.Sherling M, Friedman PM, Adrian R, et al. Consensus recommendations on the use of an erbium-doped 1550nm fractionated laser and its applications in dermatologic laser surgery. Dermatol Surg. 2010;36(4):461–469. doi: 10.1111/j.1524-4725.2010.01483.x. [DOI] [PubMed] [Google Scholar]
- 36.Chapas AM, Brightman L, Sukal S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40(6):381–386. doi: 10.1002/lsm.20659. [DOI] [PubMed] [Google Scholar]
- 37.Cho SB, Lee SJ, Cho S, et al. Nonablative 1550nm erbium-glass and ablative 10 600nm carbon dioxide fractional lasers for acne scars: a randomized split-face study with blinded response evaluation. J Eur Acad Dermatol Venereol. 2010;24(8):921–925. doi: 10.1111/j.1468-3083.2009.03551.x. [DOI] [PubMed] [Google Scholar]
- 38.Saedi N, Petelin A, Zachary C. Fractionation: a new era in laser resurfacing. Clin Plast Surg. 2011;38(3):449–461. doi: 10.1016/j.cps.2011.02.008. [DOI] [PubMed] [Google Scholar]