Abstract
Tuberculosis is a major cause of morbidity and mortality worldwide. It is a chronic granulomatous disease that can affect any part of the body, including the oral cavity. Oral lesions of tuberculosis, though uncommon, are seen in both the primary and secondary stages of the disease. This article presents a case of tuberculosis of the buccal mucosa, manifesting as non-healing, non-painful ulcer. The diagnosis was confirmed based on histopathology, sputum examination and immunological investigation. The patient underwent anti-tuberculosis therapy and her oral and systemic conditions improved rapidly. Although oral manifestations of tuberculosis are rare, clinicians should include them in the differential diagnosis of various types of oral ulcers. An early diagnosis with prompt treatment can prevent complications and potential contaminations.
Keywords: Buccal mucosa, Oral lesion, Tuberculosis
Introduction
Tuberculosis (TB) is a communicable chronic granulomatous disease caused by Mycobacterium tuberculosis.1 Tuberculosis is a global health problem with 8 million people infected annually and 3 million people dying from the disease related to TB complications.2 India alone accounts for nearly one fifth of the global burden of tuberculosis.3 The incidence of TB in underdeveloped countries is increasing, and this is thought to be associated with poor hygiene conditions and the greater prevalence of acquired immunodeficiency syndrome (AIDS).4,5 TB is usually acquired by mycobacterium tuberculosis and less frequently by ingestion of unpasteurized cow's milk that is infected by Mycobacterium bovis or by other atypical Mycobacteria.6
Depending on the organ system involved, tuberculosis is classified clinically as pulmonary and extra-pulmonary. Pulmonary tuberculosis remains the most common form of the disease. Extra-pulmonary involvement in tuberculosis is uncommon, accounting for approximately 10% to 15% of all the patients.7 TB mainly affects the lungs but also affects intestine, meninges, bones, joints, lymph glands, skin and other tissues of the body.8 Oral tuberculosis lesions are infrequent and it is estimated that only 0.05- 5% of total tuberculosis cases may be presented with oral manifestations.9 The aim of this article is to report a case of primary tuberculosis and to emphasize the importance of early diagnosis with various diagnostic tests so as to lessen the risk of exposure to an infected patient's contact.
Case Report
A 35 year old female was referred to the oral and maxillofacial pathology department with a chief complaint of painless, non healing oral ulcers on the left buccal mucosa for the last five months duration, which had increased in size. Her detailed medical history revealed that she had experienced regular weight loss (around 3 kg) over the past three to four months. She also complained of cough and feeling of malaise during the past 15 to 20 days. However, her family history was not contributory and she was not on any kind of systemic medication.
On extra oral examination, a single cervical lymph node of left side was palpable and enlarged; however, there was no sign of tenderness or fixation to the surrounding tissues (Figure 1A). Intra orally, there was an ulcer on the right buccal mucosa measuring about 1.5 × 1.5 cm in dimension with a shallow ulcerated base and well defined margins. The ulcer was covered by a yellow pseudomembrane and surrounded by an erythematous halo (Figure 1B). There was no other abnormality elsewhere in the oral cavity. Based upon the clinical examination, a differential diagnosis included aphthous ulcer, traumatic ulcer, infections (bacterial, fungal and viral), drug reaction and malignancy, including primary squamous cell carcinoma and lymphoma. Since there was no history of any kind of trauma and the ulcers were chronic, painless and non recurrent, the possibility of traumatic or aphthous ulcers were ruled out. Moreover, the patient was not on any systemic medication; thus the possibility of ulcer due to drug reaction was also ruled out.
Figure 1.
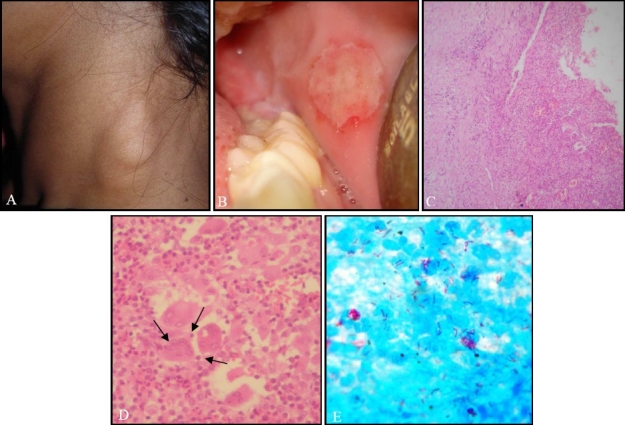
(A) Extraoral photograph shows enlarged cervical lymph node, (B) Intra orally photograph shows an ulcer with well defined margins on the right buccal mucosa covered by a yellow pseudomembrane, (C) Histopathological slide shows granulomatous inflammation with Langhans giant cells and focal caseous necrosis (hematoxylin and eosin stain), (D) Langhans cells containing nuclei arranged in a horseshoe shaped pattern at cell periphery (arrow), (E) Several acidfast bacilli in the sputum (Ziehl-Neelsen stain).
An incisional biopsy of the ulcer under local anesthesia was performed. Histopathologic examination of the excised specimen showed an ulcerated stratified squamous surface epithelium in association with fibro vascular connective tissue. The connective tissue exhibited granulomatous inflammation containing epithelioid cells, Langhans giant cells and lymphocytic infiltrate with areas of necrosis (Figures 1C and 1D). This raised the possibility of granulomatous infection, including tuberculosis, sarcoidosis or fungal infection. Subsequent stains for fungi (PAS and Grocott's Silver) and bacteria (Gram stain) were negative. However several acid-fast bacilli were identified with a Ziehl-Neelsen stain, in the sputum (Figure 1E).
Blood tests were within normal limits except for a raised white cell count (11.1× 109) and raised erythrocyte sedimentation rate (95 mm/hour). The hepatitis C virus test, VDRL (Venereal Disease Research Laboratory) and HIV test were negative. An ELISA (Enzyme-Linked Immunosorbent Assay) test confirmed the presence of antibodies against mycobacterium tuberculosis. However chest X ray did not reveal any characteristic finding. These features were consistent with those of tuberculous granulomatous lesion.
Based on all the above observations, patient was referred to a physician who initiated a WHO recommended category 1 anti-tubercular therapy DOTS (Directly Observed Treatment, Short Course) with rifampicin (450 mg), isoniazid (600 mg), ethambutol (1200 mg) and pyrazinamide (1500 mg) for two months with three times doses per week, followed with continuation phase with isoniazid (300 mg) and thioacetazone (150 mg) for six months. The patient was reported to our department after 6 months with relatively normal buccal mucosa.
Discussion
Tuberculosis is a major cause of ill health and death worldwide. The risk of infection however is much greater among people in lower socioeconomic groups.9 Every year, approximately 2.2 million individuals develop tuberculosis in India of which around 0.87 million are infectious cases and it is estimated that annually there are around 330,000 deaths due to TB.3 TB has become the most common opportunistic infection in areas where HIV infection is prevalent.4
Tuberculosis of the oral cavity is an uncommon occurrence, might be because of an intact squamous epithelium of the oral mucosa which makes tuberculosis bacilli penetration difficult and provides protection against the infection.10 Although the mechanism of primary inoculation has not been definitely established yet, it appears that the organisms are carried most likely in the sputum and enter the mucosal tissue through a small tear in the oral mucosa as a result of chronic irritation or inflammation which may favor the localization of organism.6 Local predisposing factors include poor hygiene, local trauma, dental extraction, leukoplakia, jaw fracture, cyst and abscess.11 In the present case, bacteria might have spread through local trauma or poor oral hygiene.
The primary form of the disease most often is localized to the lungs. In most patients, the infection does not spread and as host immunity develops the primary lesion heal by fibrosis and calcification.12 The other type of this disease is known as secondary tuberculosis which occurs from a healed primary focus or due to endogenous spread of the infection. Secondary TB is usually chronic in nature and can cause considerable destruction of the involved tissue with caseation, cavity formation and fibrosis.9
Primary oral TB lesions are extremely rare and usually seen in children but may also be seen in adults. It typically involves the gingiva and is associated with regional lymphadenopathy.
Secondary oral TB can occur in all age groups but most common in middle and older age groups.8 The most common occurring lesion is an ulcer, characterized by irregular edges with minimal induration.13 The base of an ulcer may be granular or covered with pseudomembrane. Tongue is most affected followed by palate, buccal mucosa and lips. Other sites can be salivary glands, tonsils, uvula and mandibular ridge.9,14,15 Sometimes oral TB ulcer can be seen as superficial ulcers, patches, indurated soft tissue lesions or even lesions within the jaw that may be in the form of TB osteomyelitis.7,16]
This case is unusual in the sense that a painless ulcer on the buccal mucosa led to the diagnosis of tuberculosis. Primary lesions of TB manifest in the oral cavity as non-healing chronic ulcers. Clinician should be aware when diagnosing such lesions with non-healing tendency, tuberculosis should be considered in the differential diagnosis. Sezer et al.9, Von Arx and Husain13 reported a non-healing ulcer on the buccal mucosa which is consistent with the present case. Ebenezer et al.12 reported two cases of oral TB, first one on labial mucosa and second on ingival, both presented as non healing ulcer. It is vital for clinician to conduct a complete physical examination including signs and symptoms of pulmonary TB with various diagnostic tests as listed in Table 1 and by performing a biopsy. Histopathological study is needed to exclude carcinomatous changes and to confirm the diagnosis of TB. In the present case, the most likely differential diagnosis included aphthous ulcer, traumatic ulcer, infections (bacterial, fungal and viral), drug reaction and malignancy, including primary squamous cell carcinoma, lymphoma and metastases. A negative history about trauma, non recurrent ulcer and any systemic medication helped to rule out traumatic, aphthous ulcer and ulcer due to drug reaction respectively.
Table 1.
Diagnostics techniques in tuberculosis

As reported here, the most likely clinical diagnosis is that of squamous cell carcinoma, in which case biopsy is mandatory. The histopathology revealed a granulomatous lesion. This raised the possibility of other orofacial granulomatous conditions such as tuberculosis, sarcoidosis, tertiary syphilis, deep mycoses and foreign body reaction. Subsequent stains for fungi (PAS and Grocott Silver) and bacteria (Gram stain) were negative along with negative VDRL (Venereal Disease Research Laboratory) and HIV test. The diagnosis of tuberculosis was confirmed by the presence of several acid-fast bacilli in the sputum and antibodies against mycobacterium tuberculosis by ELISA.
To conclude, tuberculosis of the oral cavity is relatively rare and has largely become a forgotten diagnosis of oral lesions. Dental practitioners need to be aware that TB may occur in the oral cavity and should be considered in the differential diagnosis of any ulcerated, indurated non-healing lesion of the oral cavity especially in lower socioeconomic groups. In addition, efforts should be made to control oral TB by early detection and referral of the patient to a physician for proper management. Also appropriate and effective infection control programs in dental surgery should be encouraged.
References
- 1.Wang WC, Chen JY, Chen YK, Lin LM. Tuberculosis of the head and neck: a review of 20 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):381–6. doi: 10.1016/j.tripleo.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Yepes JF, Sullivan J, Pinto A. Tuberculosis: medical management update. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(3):267–73. doi: 10.1016/j.tripleo.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Tuberculosis-the global burden. Trends in TB incidence in 9 regions of the world [Online] [cited 2005]. Available from: http://www.who.int/tb/publications/global_report/en/index.html .
- 4.Miziara ID. Tuberculosis affecting the oral cavity in Brazilian HIV-infected patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(2):179–82. doi: 10.1016/j.tripleo.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 5.John M. Risk of bacterial transmission in dental practice. J Can Dent Assoc. 2000;66(10):550–2. [PubMed] [Google Scholar]
- 6.Mignogna MD, Muzio LL, Favia G, Ruoppo E, Sammartino G, Zarrelli C, et al. Oral tuberculosis: a clinical evaluation of 42 cases. Oral Dis. 2000;6(1):25–30. doi: 10.1111/j.1601-0825.2000.tb00317.x. [DOI] [PubMed] [Google Scholar]
- 7.Umadevi M, Ranganathan K, Saraswathi TR, Uma R, Elizabeth J. Primary Tuberculous Osteomyelitis of the Mandible. Asian J Oral Maxillofac Surg. 2003;15:208–13. [Google Scholar]
- 8.Shafer WG, Hine MK, Levy BM. Bacterial Infection of the Oral Cavity. In: Shafer WG, Hine MK, Levy BM, editors. Textbook of Oral Pathology. 6th ed. Philadelphia: W.B. Saunders Company; 2011. pp. 313–7. [Google Scholar]
- 9.Sezer B, Zeytinoglu M, Tuncay U, Unal T. Oral mucosal ulceration: a manifestation of previously undiagnosed pulmonary tuberculosis. J Am Dent Assoc. 2004;135(3):336–40. doi: 10.14219/jada.archive.2004.0184. [DOI] [PubMed] [Google Scholar]
- 10.Pekiner FN, Erseven G, Borahan MO, Gumru B. Natural barrier in primary tuberculosis inoculation: oral mucous membrane. Int J Tuberc Lung Dis. 2006;10(12):1418. [PubMed] [Google Scholar]
- 11.Rodrigues G, Carnelio S, Valliathan M. Primary isolated gingival tuberculosis. Braz J Infect Dis. 2007;11(1):172–3. doi: 10.1590/s1413-86702007000100037. [DOI] [PubMed] [Google Scholar]
- 12.Ebenezer J, Samuel R, Mathew GC, Koshy S, Chacko RK, Jesudason MV. Primary oral tuberculosis: report of two cases. Indian J Dent Res. 2006;17(1):41–4. doi: 10.4103/0970-9290.29893. [DOI] [PubMed] [Google Scholar]
- 13.Von Arx DP, Husain A. Oral tuberculosis. Br Dent J. 2001;190(8):420–2. doi: 10.1038/sj.bdj.4800991. [DOI] [PubMed] [Google Scholar]
- 14.Carnelio S, Rodrigues G. Primary lingual tuberculosis: a case report with review of literature. J Oral Sci. 2002;44(1):55–7. doi: 10.2334/josnusd.44.55. [DOI] [PubMed] [Google Scholar]
- 15.Kilic A, Gul U, Gonul M, Soylu S, Cakmak SK, Demiriz M. Orificial tuberculosis of the lip: a case report and review of the literature. Int J Dermatol. 2009;48(2):178–80. doi: 10.1111/j.1365-4632.2009.03942.x. [DOI] [PubMed] [Google Scholar]
- 16.Cakan A, Mutlu Z, Ozsoz A, Erbaycu AE, Unal T, Koyuncu BO. Tuberculosis of oral mucosa. Monaldi Arch Chest Dis. 2001;56(4):315–7. [PubMed] [Google Scholar]
- 17.Control and prevention of tuberculosis in the United Kingdom: code of practice 2000. Joint Tuberculosis Committee of the British Thoracic Society. Thorax. 2000;55(11):887–901. doi: 10.1136/thorax.55.11.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Overby K. Pediatric Health Supervision. In: Rudolph A, Kamei R, Overby K, editors. Rudolph's Fundamentals of Pediatrics. 3rd ed. New York: McGraw-Hill Medical; 2002. pp. 52–3. [Google Scholar]
- 19.Harisinghani MG, McLoud TC, Shepard JA, Ko JP, Shroff MM, Mueller PR. Tuberculosis from head to toe. Radiographics. 2000;20(2):449–70. doi: 10.1148/radiographics.20.2.g00mc12449. [DOI] [PubMed] [Google Scholar]
- 20.Selvakumar N, Rahman F, Rajasekaran S, Narayanan PR, Frieden TR. Inefficiency of 0.3% carbol fuchsin in ziehl-neelsen staining for detecting acid-fast bacilli. J Clin Microbiol. 2002;40(8):3041–3. doi: 10.1128/JCM.40.8.3041-3043.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anthony RM, Kolk AH, Kuijper S, Klatser PR. Light emitting diodes for auramine O fluorescence microscopic screening of Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2006;10(9):1060–2. [PubMed] [Google Scholar]
- 22.Ohyashiki K, Ohyashiki JH, Tauchi T, Fujieda H, Hojo H, Ohtaka M, et al. Treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia: a pilot study which raises important questions. Leukemia. 1991;5(7):611–4. [PubMed] [Google Scholar]
- 23.Richeldi L. An update on the diagnosis of tuberculosis infection. Am J Respir Crit Care Med. 2006;174(7):736–42. doi: 10.1164/rccm.200509-1516PP. [DOI] [PubMed] [Google Scholar]
- 24.Rodrigues C, Shenai S, Sadani M, Sukhadia N, Jani M, Ajbani K, et al. Evaluation of the bactec MGIT 960 TB system for recovery and identification of Mycobacterium tuberculosis complex in a high through put tertiary care centre. Indian J Med Microbiol. 2009;27(3):217–21. doi: 10.4103/0255-0857.53203. [DOI] [PubMed] [Google Scholar]
- 25.Sankar S, Balakrishnan B, Nandagopal B, Thangara-ju K, Natarajan S. Comparative evaluation of nested PCR and conventional smear methods for the detection of Mycobacterium tuberculosis in sputum samples. Mol Diagn Ther. 2010;14(4):223–7. doi: 10.1007/BF03256377. [DOI] [PubMed] [Google Scholar]
- 26.Negi SS, Khan SF, Gupta S, Pasha ST, Khare S, Lal S. Comparison of the conventional diagnostic modalities, bactec culture and polymerase chain reaction test for diagnosis of tuberculosis. Indian J Med Microbiol. 2005;23(1):29–33. doi: 10.4103/0255-0857.13869. [DOI] [PubMed] [Google Scholar]


