Abstract
Follicular thyroid carcinoma (FTC) is the second most common thyroid cancer (TCs) after papillary carcinoma, but it is ranked first in producing distant metastases among TCs. It accounts for 10 – 20% of all thyroid malignancies and is most often seen in patients over 40 years of age. Distant metastases at the time of diagnosis are reported in 11 – 20% of the patients and may be the reason for presentation. There have been less than 30 reported cases of cutaneous metastases from FTC in the English Literature, a majority affecting the scalp. We present an unusual aggressive, hypervascular FTC in a 58-year-old man with a previous diagnosis of multinodular goiter. The difficulty in gaining his acceptability of orthodox management resulted in the development of multiple giant scalp and right facial metastatic masses associated with lytic calvarial destruction and the involvement of frontal and right maxillary sinuses. These imposed serious challenges in managing him in a resource-poor community.
Keywords: Multinodular goiter, skull metastasis, thyroid follicular carcinoma
INTRODUCTION
Thyroid carcinomas (TCs) are well-documented, uncommon malignancies, accounting for 1 – 2% of all new cancer cases.[1–5] However, TC is the most common endocrine malignancy (90% of all endocrine cancers) and is responsible for more deaths than all other endocrine cancers combined[1,4,6] The annual incidence varies worldwide, but is estimated to be between 0.5 – 10 per 100,000 population[4] Epidemiologically ascertained risk factors are ionizing radiation, the presence of thyroid adenoma, and multinodular goiter (MNG).[5] The incidence of carcinoma in MNG is reported to range between 7 – 17%.[5]
Generally, TCs are derived from follicular epithelial cells and the variances include papillary carcinomas, follicular carcinoma, poorly differentiated carcinoma (also known as ‘insular’ carcinoma) and anaplastic carcinoma. Follicular thyroid carcinoma (FTC) is the second most common thyroid cancer after papillary carcinoma, but it is ranked first in producing distant metastases among TCs[4,5] It accounts for 10 – 20% of all thyroid malignancies and is most often seen in patients over 40 years of age[1,6] The most common sites of metastases of FTC are the bones, the lungs, and the central nervous system
Distant metastases at the time of diagnosis are reported in 11 – 20% of patients and may be the reason for presentation. [1–6] There have been fewer than 30 reports of cutaneous metastases in the literature, a majority are to the scalp. Skull metastases are a rare presentation in 2.5 – 5.8% of FTCs. [1–7] An unusual hypervascular metastatic FTC, producing aggressive, multiple, giant scalp and facial masses, lytic calvarial lesion, and goiter in a 58-year-old man is presented along with the challenges of managing him in a resource-poor community.
CASE REPORT
A 58-year-old man presented to the Surgical Outpatient Department of a Nigerian teaching hospital with a history of painless and slowly progressive neck and multiple scalp and facial swellings of 16-years and two-year duration, respectively.
There was no associated dyspnea, dysphagia, dysphonia or symptoms suggestive of hyperthyroidism. He had reported to the hospital when the neck swelling was of a five-year duration and a diagnosis of multinodular goiter was made, but he absconded from the clinic without doing the necessary investigations requested. This he attributed to poverty.
On examination, he was mildly pale, afebrile, anicteric, conscious, and alert. He was neither emaciated nor in distress. He had an anterior neck swelling to the right side of the midline [Figure 1a] that moved with swallowing. The swelling was hard in consistency, extended retrosternally, and demonstrated a positive Berry's sign. He had no palpable cervical lymph node, clinical evidence of thyrotoxicosis or hypothyroidism and his examination of the central nervous system, chest, and cardiovascular system were normal. The scalp masses were fluctuant and pulsatile. He had a tracheal deviation to the left.
Figure 1.

(a,b) Photographs of the 58-year-old man with metastatic follicular thyroid carcinoma showing multiple scalp and facial masses. Note in a and b the tortuous and engorged superficial vessels on the left upper aspect of the face and in (b) the right sided thyroid swelling
Plain skull radiographs [Figure 2a and b] showed multiple lytic skull vault lesions with ragged edges and bony strands extending into the skull masses, from the vault. There was a prominence of vascular markings in the direction of the lytic lesion and the overlying masses, suggesting hypervascularity. The frontal and the right maxillary sinuses were involved .There were also soft masses within the nasal cavity, with ill-definition of the nasal septum. The thyroid mass was essentially to the right of the midline, in the lower aspect of the neck. It caused tracheal deviation to the left and coronal tracheal narrowing. There was also retrosternal extension and associated mild hilar soft tissue masses with lobulated margins, presumed to be lymphadenopathy [Figure 3].
Figure 2.
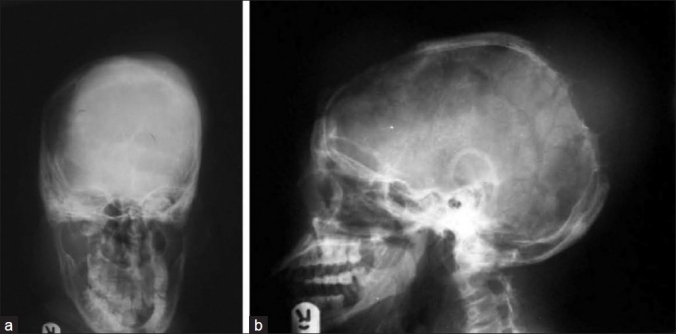
(a,b) Skull radiographs of the same patient. (a) Occipitofrontal view showing overlapping shadows of the skull masses and masses within the nasal cavity causing ill-definition of the nasal septum. (b) Multiple lytic skull vault lesions with ragged edges and radiating bony stands from the vault into the skull masses. Note the branching lucencies to the direction of the lytic lesion and the overlying masses, suggesting hypervascularity
Figure 3.
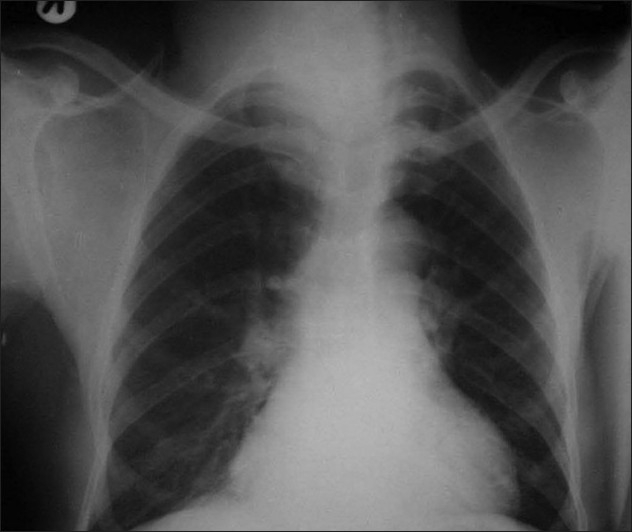
Patient chest radiograph showing thyroid mass essentially to the right of midline in the lower aspect of the neck, tracheal deviation to the left, coronal tracheal narrowing and retrosternal extension. Note the hilar soft tissue masses with lobulated margin presumed to be lymphadenopathy
B-mode ultrasound scans of the mass demonstrated hypervascularity and some area of cystic changes. There was right carotid vessel compression leading to a turbulent flow on Doppler interrogation.
The complete blood count, serum electrolyte urea and creatinine, abdominopelvic ultrasound, and thyroid function tests were normal.
Fine needle aspiration cytology of the thyroid showed malignant tumor and the histology of the scalp metastasis showed follicular carcinoma.
The patient was planned for neurosurgical and maxillofacial /plastic surgery consultation and further investigation that included computerized tomographic (CT) scans of the head and neck, CT-angiography before total thyroidectomy, External Radiation Beam Therapy (EBRT), and TSH-suppressive maintenance with l-thyroxine, but he declined and absconded.
DISCUSSION
The worldwide literature review reveals that follicular carcinoma has a greater preponderance than papillary carcinoma for cutaneous metastases, with the majority localized to the head and neck. Besides the scalp, the most commonly affected areas of cutaneous metastases of FTC that have been described are, various locations such as abdomen, back, thigh and pelvis. [1–5] Although bone metastasis has been reported in 10 – 40% of FTC, only 2.5 – 5.8% skull metastasis has been documented. [1–7] Multiple metastatic cutaneous FTC to the skull, scalp, paranasal sinuses, and face as in this case are rare exceptions in the literature. We did not find a case with such a wide and multiple lytic skull metastatic involvement [Figure 1] with follicular carcinoma documented in the literature.
Metastasis to the scalp usually presents with scalp swellings as had occurred in this patient. The plain skull radiograph and ultrasound scans demonstrated hypervascularity, which was also found in some reported cases.
Advance stage at presentation and proportionately high rates of cutaneous and bony metastases of FTC, as in this patient, have contributed to poor outcome of FTC in developing countries.[7,8] Despite the dismal outcome reported with late presentation of metastatic FTC, total thyroidectomies have been reported to prevent thyroid bed recurrence in surviving patients.[3,8,9] The treatment of patients with head metastases included a total thyroidectomy, an excision of the skull lesion, and the administration of radioiodine therapy, as well as thyroid-stimulating hormone (TSH) suppression Therapy.[2]
Some authors support the use of external beam radiation therapy (EBRT) for both locoregional control and control of inoperable metastases.[9,10] However, cases with radiographic metastatic changes are known not to respond well to iodine therapy.[8]
The best treatment for skull metastases, as extensive as in our patient, remains to be determined, but in this patient probably the treatment would have been total thyroidectomy with or without excision of the skull lesion, TSH-suppressive maintenance dosing with l-thyroxine, and EBRT.
We classify this patient as high risk, with probable poor prognosis for surgical management because of the extensive demonstrable radiographic skull involvement, and this was explained to the patient as part of counseling. Attempting excision of the multiple hypervascular skull lesions with facial involvement in our patient might not have been rewarding. In four patients presented by Dahl et al,[1] the average length of survival after diagnosis of cutaneous metastases was 19 months. Our patient's survival, despite disseminated malignancy, without appropriate management, supported the findings of long-term survival rates in up to 43% of the documented patients. [2–6]
In conclusion, we have presented an unusual case of aggressive FTC in a previous case of MNG, where poverty and difficulty in gaining his acceptability of orthodox management imposed serious treatment limitations, resulting in wide spread scalp and skull metastases. Multinodularity of goiter should no longer be considered an indicator of probable benign disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dahl PR, Brodland DG, Goellner JR, Hay ID. Thyroid carcinoma metastatic to the skin: a cutaneous manifestation of a widely disseminated malignancy. J Am Acad Dermatol. 1997;36:531–7. doi: 10.1016/s0190-9622(97)70239-1. [DOI] [PubMed] [Google Scholar]
- 2.Cupisti K, Ramp U, Raffel A, Krausch M, Rehders A, Knoefel WT. Multiple giant scalp metastases of a follicular thyroid carcinoma. World J Surg Oncol. 2008;6:82. doi: 10.1186/1477-7819-6-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab. 2006;91:2892–9. doi: 10.1210/jc.2005-2838. [DOI] [PubMed] [Google Scholar]
- 4.Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1998. CA Cancer J Clin. 1998;48:6–29. doi: 10.3322/canjclin.48.1.6. [DOI] [PubMed] [Google Scholar]
- 5.Gandolfi PP, Frisina A, Raffa M, Renda F, Rocchetti O, Ruggeri C, et al. The incidence of thyroid carcinoma in multinodular goiter: retrospective analysis. Acta Biomed. 2004;75:114–7. [PubMed] [Google Scholar]
- 6.Agarwal S, Rao S, Arya A, Gupta K, Arora R, Dhawan I. Follicular thyroid carcinoma with metastasis to skin diagnosed by fine needle aspiration cytology. Indian J Pathol Microbiol. 2008;51:430–1. doi: 10.4103/0377-4929.42552. [DOI] [PubMed] [Google Scholar]
- 7.Abdulkareem FB, Banjo AA, Elesha SO. Histological Review of Thyroid Lesions: A 13 year Retrospective study (1989-2001) Nig Postgrad Med J. 2005;12:210–4. [PubMed] [Google Scholar]
- 8.Ogawa Y, Sugawara T, Seki H, Sakuma T. Thyroid follicular carcinoma metastasized to the lung, skull, and brain 12 years after initial treatment for thyroid gland--case report. Neurol Med Chir (Tokyo) 2006;46:302–5. doi: 10.2176/nmc.46.302. [DOI] [PubMed] [Google Scholar]
- 9.Brierley J, Tsang R, Panzarella T, Bana N. Prognostic factors and the effect of treatment with radioactive iodine and external beam radiation on patients with differentiated thyroid cancer seen at a single institution over 40 years. Clin Endocrinol (Oxf) 2005;63:418–27. doi: 10.1111/j.1365-2265.2005.02358.x. [DOI] [PubMed] [Google Scholar]
- 10.Meadows KM, Amdur RJ, Morris CG, Villaret DB, Mazzaferri EL, Mendenhall WM. External beam radiotherapy for differentiated thyroid cancer. Am J Otolaryngol. 2006;27:24–8. doi: 10.1016/j.amjoto.2005.05.017. [DOI] [PubMed] [Google Scholar]