Abstract
Toxoplasmosis in immune competent patients usually causes asymptomatic infection or mild symptoms, while in immunocompromised and AIDS patients it can be a life threatening condition. We report a case of cerebral toxoplasmosis in a patient with AIDS and review the causes of brain ring enhancing lesions.
Background
Although our case is a fairly straightforward case of cerebral toxoplasmosis, we believe that it is a good teaching point for junior doctors, especially those working in the emergency department (ED).
Case presentation
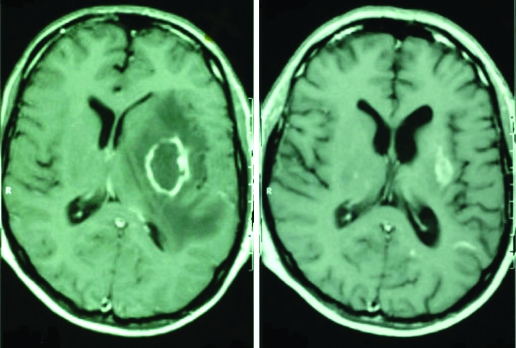
A 45-year-old bank manager was admitted to the emergency department with progressive confusion and difficulty speaking of 3 days’ duration. He was accompanied by his wife who reported that her husband had complained of poor appetite and diarrhoea for 2 weeks previously. The patient had no significant past medical history. He had been married for 20 years, drank moderate amounts of alcohol and had no illicit drug history. The patient denied any extra-marital relationship, blood transfusions or travel abroad. He kept no pets. The positive findings in his clinical examination were a right facial palsy and oral thrush. His chest x-ray and routine blood tests were normal. The patient was admitted to hospital for investigations but refused HIV testing. Two days after admission the patient had a generalised tonic-clonic seizure. He was commenced on anticonvulsant therapy. His brain MRI scan showed a single 2–3 cm ring enhancing lesion in the left frontal lobe suggesting a cerebral tumour or abscess. Once again the patient refused HIV testing but agreed to have a brain biopsy. The latter was inconclusive showing necrotic tissue only. After the biopsy the patient agreed to have an HIV test, which was positive with HIV-viral load (VL) 41 800 (4.6 log); T lymphocyte CD4 count was 75 cells/mm3 (reference range 500–1100). The patient was referred to the HIV team, who commenced him on co-trimoxazole for Pneumocystis carinii pneumonia (PCP) prophylaxis and planned to start the patient on anti-toxoplasmosis therapy the next day. However, the patient’s general condition and his Glasgow Coma Scale deteriorated rapidly next morning. He also developed an erythmatous maculopapular skin rash over his upper chest and upper arms. His co-trimoxazole was discontinued and he was admitted to the intensive care unit, intubated and ventilated. He was commenced on clindamycin, pyrimethamine and on highly active antiretroviral therapy (HAART) consisting of zidovudine, lamivudine and nevirapine. Further investigation showed the patient’s Toxoplasma IgG serology was positive, and the IgM negative. Screening tests for other opportunistic infections (cytomegalovirus, Cryptococcus neoformans), and viral hepatitis A, B and C and syphilis were negative. Three weeks later the patient was extubated and transferred to the medical unit where he spent 2 weeks before discharge from hospital. Figure 1 shows his brain MRI before treatment (left image) and 18 months after HAART and anti-toxoplasmosis therapy (right image).
Figure 1.
Patient’s brain MRI before treatment (left image) and 18 months after HAART and anti-toxoplasmosis therapy (right image).
Outcome and follow-up
The patient returned to work approximately 2 years after his initial admission. His facial droop improved but he was left with a loss of pain sensation over his right leg.
Discussion
A solitary cerebral lesion presents a diagnostic dilemma, especially in a heterosexual patient who claims to be in a long term monogamous relationship. Cerebral toxoplasmosis and primary cerebral lymphoma are the common causes of ring enhancing lesions of the central nervous system in a patient with AIDS. Toxoplasma encephalitis usually causes multiple lesions in the basal ganglia. However, it is often difficult to distinguish between these two conditions clinically and radiographically.1 An empiric trial of anti-toxoplasma therapy for 2–3 weeks can improve the patient’s symptoms and reduce the size of the brain abscesses in patients with toxoplasma encephalitis, the radiographic improvement often occurring after clinical improvement.2 Initially, our patient declined HIV testing and anti-toxoplasmosis therapy but agreed to have a brain biopsy. The latter may be indicated in such cases in order to clarify the diagnosis.3 Other less common conditions that can cause ring enhancing lesions in a patient with AIDS include progressive multifocal leukoencephalopathy, tuberculosis, granulomata, HIV and cytomegalovirus encephalitis, herpes simplex and varicella-zoster virus encephalitis, gliomas and other primary CNS neoplasms, metastases, cerebral infarction, contusion, demyelination, resolving haematoma and abscesses. The latter may include pyogenic abscess caused by bacterial, fungal or parasitic pathogens.3
Toxoplasmosis is a common worldwide zoonosis, caused by a coccidian parasite Toxoplasma gondii. The parasite infects all orders of mammals, but cats are the definitive hosts. They excrete the parasite’s oocysts in their faeces. Humans are usually infected by ingestion of faecally contaminated materials or by eating or handling uncooked or contaminated meat. The parasite can be also transmitted vertically causing birth defects. The infection causes no symptoms or a mild glandular fever-like illness in immune competent adults. However, in immunocompromised and AIDS patients toxoplasmosis may be life threatening. Disease in these individuals is rarely caused by new infection and is more commonly due to reactivation of a latent infection. Although any organ may be involved, encephalitis is the predominant presentation of toxoplasmosis in AIDS patients and may cause cranial nerve palsy, focal neurological lesions, confusion, stroke, seizures and neuropsychiatric disorders. Other presentations of toxoplasmosis in AIDS patients may include pneumonitis, chorioretinitis, myositis, myocarditis and skin rash.4 The diagnosis of toxoplasmosis can be made by serology, Toxoplasma DNA-PCR in the serum, cerebrospinal fluid and several types of body fluids and tissues. The presence of multiple Toxoplasma tissue cysts in an inflammatory brain lesion at brain biopsy is highly suggestive of toxoplasma encephalitis and the demonstration of Toxoplasma tachyzoites can establish the diagnosis. Clinical and radiographic response to 2–3 weeks of anti-toxoplasmosis therapy then supports this.2 Treatment of cerebral toxoplasmosis includes a combination of sulfadiazine 4–8 g per day and pyrimethamine 50–100 mg per day. The latter is a folic acid antagonist and should be administered concomitantly with folinic acid to prevent bone marrow suppression. Clindamycin 300–900 mg every 6 h may be used in combination with pyrimethamine as alternatives to sulfadiazine if a patient is allergic to or can not tolerate sulphadiazine. However, it has been reported that pyrimethamine/sulfadiazine is superior to pyrimethamine/clindamycin.5 Azithromycin, clarithromycin, dapsone and atovaquone may also be used in patients who are allergic to sulfonamide based drugs. Corticosteroids may be used when there is oedema around the abscesses and increased intracranial pressure. Antiretrovial therapy can be commenced together with anti-toxoplasmosis therapy, or soon after the patient’s clinical improvement. Our case reflects the high risk of morbidity in HIV infected patients with late presentation or with AIDS. Opportunistic infections including toxoplasma encephalitis are common in HIV patients with a CD4 count of less than 200 cells/mm3. Offering PCP prophylaxis therapy can prevent toxoplasmosis in patient with AIDS and this therapy can be discontinued after immune recovery on HAART.5
Although our patient returned back to work 2 years after his illness, he was left with loss of pain sensation over his right foot and ankle. The refusal of our patient to give consent for HIV testing indirectly led to a brain biopsy for diagnosis. However, patient consent for HIV testing is an important part of the management of HIV patients, and it must be addressed sensitively within the context of the presenting condition. After further counselling following the brain biopsy, our patient agreed to have an HIV test and thence to inform his wife about his diagnosis. She agreed to have the same test and her result was negative.
Learning points
It can be difficult to reach a diagnosis of cerebral toxoplasmosis and/or AIDS in a heterosexual patient who claims to be in a long term monogamous relationship.
There is a lack of HIV counselling and communication skills that could have helped our patient accept the HIV test and avoid a brain biopsy.
The stigma of HIV infection can discourage patients from seeking early medical care in order to avoid AIDS related consequences.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Schroeder PC, Post MJ, Oschatz E, et al. Analysis of the utility of diffusion-weighted MRI and apparent diffusion coefficient values in distinguishing central nervous system toxoplasmosis from lymphoma. Neuroradiology 2006; 48: 715–20 [DOI] [PubMed] [Google Scholar]
- 2.Cunha BA. Central nervous system infections in the compromised host: a diagnostic approach. Infect Dis Clin North Am 2001; 15: 567–90 [DOI] [PubMed] [Google Scholar]
- 3.Rosenow JM, Hirschfeld A. Utility of brain biopsy in patients with acquired immunodeficiency syndrome before and after introduction of highly active antiretroviral therapy. Neurosurgery 2007; 61: 130–41 [DOI] [PubMed] [Google Scholar]
- 4.Antinori A, Larussa D, Cingolani A, et al. Prevalence, associated factors, and prognostic determinants of AIDS-related toxoplasmic encephalitis in the era of advanced highly active antiretroviral therapy. Clin Infect Dis 2004; 39: 1681–91 [DOI] [PubMed] [Google Scholar]
- 5.Katlama C, De Wit S, O’Doherty E, et al. Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for toxoplasmic encephalitis in patients with AIDS. Clin Infect Dis 1996; 22: 268–75 [DOI] [PubMed] [Google Scholar]