A 44-year-old woman presented to our emergency department complaining of mild abdominal pain of three days duration. The pain had started in the epigastrium and progressively migrated to the lower quadrants of the abdomen. She did not have nausea, diarrhea or fever and her last menstrual period had finished five days before admission. On clinical examination the abdomen was tender to deep with superficial palpation, and rebound tenderness was found in the right iliac fossa. The abdomen was not distended, and peristalsis was normal. Laboratory analysis showed a leukocyte count of 9 800/mm3, without any other significant findings. Because of the long duration of pain and the absence of leucocytosis, a diagnosis of acute appendicitis could not be made with confidence, so a computed tomography (CT) scan of the abdomen was ordered. The CT scan showed an oval-shaped lesion with inflammatory changes in the surrounding fat in the ascending colon, compatible with epiploic appendagitis (Figure 1). The patient was managed with oral nonsteroidal anti inflammatory drugs and discharged home, with complete resolution of pain upon follow-up examination five days later.
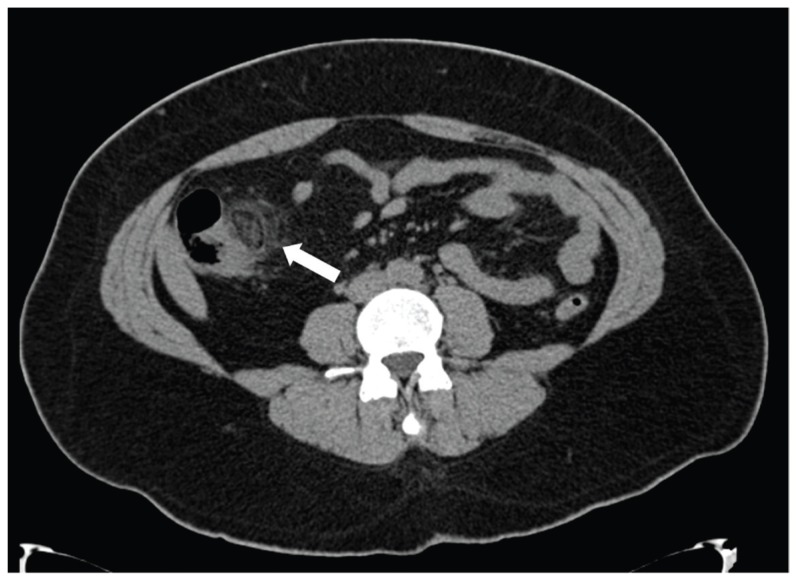
Figure 1.
Noncontrast computed tomography scan of the abdomen showing an oval lesion with fat attenuation and surrounded by inflammatory changes (arrow) characteristic of epiploic appendagitis at the ascending colon.
Epiploic appendagitis is a rare nonsurgical cause of acute abdomen, characterized by a sudden onset of abdominal pain. This condition is caused by the torsion of an epiploic appendage, which is a peritoneal fat pouch attached to the colon and supplied by a vascular stalk.1 The impairment of vascular supply to the appendage causes ischemia, which in turn leads to necrosis. The pain is sharp and sudden, and it is not accompanied by nausea, vomiting, fever or diarrhea.2 Depending on the localization of the appendage the pain can be referred to virtually any part of the abdomen, particularly the lower quadrants. This can be explained by the fact that the most common site of appendagitis is the sigmoid colon, and thus it is usually mistakenly diagnosed as diverticulitis.3 This condition, however, can also mimic acute appendicitis,1,3,4 cholecystitis5 and virtually any other cause of acute abdomen. Laboratory examination is typically normal, and only a few patients present with leucocytosis.1 Historically, the diagnosis of epiploic appendagitis has been made at the time of laparotomy, 4 but currently imaging techniques have made it possible to diagnose this condition before surgery. Although ultrasound examination of the abdomen has been used with good results in the diagnosis of epiploic appendagitis, the imaging modality of choice is CT.2 The typical tomographic sign is an oval-shaped lesion with central hyperattenuation and inflammatory changes of the surrounding fat.2 Epiploic appendagitis is a self-limiting condition, and the course of the disease is benign. As such, the preferred treatment is the administration of non-steroidal anti-inflammatory drugs, with very good long-term results.3 Some authors, however, advocate surgical therapy using the laparoscopic approach in order to reduce the possibility of recurrence.1 Diagnosing epiploic appendagitis is virtually impossible by physical examination alone, and thus awareness and proper usage of radiological studies are essential for its diagnosis. Even though a CT scan should be omitted in cases in which the clinical picture clearly points to acute appendicitis, it can be particularly useful when the clinical examination or history are unrevealing and laboratory analyses are normal, as in our patient. Recognizing epiploic appendagitis preoperatively can spare patients unnecessary surgical intervention, and save thousands of dollars, but due to its rarity it should not be routinely sought in every patient with abdominal pain. The various presentations of this condition make it very important for any clinician dealing with patients in an emergency department, and it should at least be considered in the differential diagnosis of more common causes of the acute abdomen, particularly in patients with an unconventional presentation.
REFERENCES
- 1.Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, Mann B. Epiploic appendagitis–clinical characteristics of an uncommon surgical diagnosis. BMC Surg. 2007;7:11. doi: 10.1186/1471-2482-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25:1521–34. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 3.Rodríguez Gandía MA, Moreira Vicente V, Gallego Rivera I, Rivero Fernández M, Garrido Gómez E. Epiploic appendicitis: the other appendicitis. Gastroenterol Hepatol. 2008;31:98–103. doi: 10.1157/13116074. [DOI] [PubMed] [Google Scholar]
- 4.Sangha S, Soto JA, Becker JM, Farraye FA. Primary epiploic appendagitis: an underappreciated diagnosis. A case series and review of the literature. Dig Dis Sci. 2004;49:347–50. doi: 10.1023/b:ddas.0000017463.46961.94. [DOI] [PubMed] [Google Scholar]
- 5.Lien WC, Lai TI, Lin GS, Wang HP, Chen WJ, Cheng TY. Epiploic appendagitis mimicking acute cholecystitis. Am J Emerg Med. 2004;22:507–8. doi: 10.1016/j.ajem.2004.07.018. [DOI] [PubMed] [Google Scholar]