Abstract
Evidence for a bi-directional relationship of depression and type 2 diabetes suggests that social distress plays a role in depression among people with diabetes. In this work, we examine the relationship between subjective distress and depression in 121 first and second generation Mexican immigrant women seeking diabetes care at a safety-net hospital in Chicago. We used a mixed-methods approach including narrative interview, survey, and finger stick blood HbA1c data. Using grounded theory analysis we identified seven life stressors from narrative interviews: interpersonal abuse, stress related to health, family, neighborhood violence, immigration status, and work, and feeling socially detached. Women reported unusually high rates of interpersonal abuse (65%) and disaggregated physical abuse (54%) and sexual abuse (23%). We evaluated depression using CES-D cut-off points of 16 and 24 and assessed rates to be 49% and 34%, respectively. We found that interpersonal abuse was a significant predictor of depression (CESD≥24) in bivariate (OR 3.97; 95% CI 1.58–10.0) and multivariate (OR 5.51; 95% CI 1.85,16.4) logistic regression analyses. These findings suggest that interpersonal abuse functions as an important contributor to depression among low-income Mexican immigrant women and should be recognized and addressed in diabetes care.
Keywords: depression, psychosocial stress, interpersonal abuse, diabetes, Mexican immigrants, women
Introduction
“The stress of problems, of paying rent, of men, of bringing the children to school…And I had too many stresses at the same time,” commented María, a women who suffered from depression much of her life, worsening upon diagnosis of type 2 diabetes in her early fifties. Mental distress among Mexican immigrant women like María often come to a front in later age, which has been attributed to social support, worsening physical health, and other factors related to depression (Black 1999; Gerst, Al-Ghatrif et al. 2010). Epidemiologists have demonstrated that Mexican-Americans report higher rates of mental distress in the United States compared to other ethnic groups, and that U.S.-born Mexican-Americans report higher rates of psychiatric distress compared to Mexican immigrants (Burnam, Hough et al. 1987; Alderete, Vega et al. 2000; Alderete, Vega et al. 2000; Escobar, Hoyos Nervi et al. 2000; Allegria, Mulvaney-Day et al. 2007; Allegria, Canino et al. 2008). Some have argued that this disproportionate burden of mental distress among people of Mexican descent may be attributed to poor access to mental health care and resultant chronicity of mental distress (Castañeda 2010; Gonzalez, Tarraf et al. 2010).
In this study we examined depression among late-adult first and second generation Mexican immigrant women living with type 2 diabetes (also known as Non-Insulin Dependent Diabetes Mellitus, hereafter “diabetes”) in Chicago. National surveillance data suggest that the incidence of diabetes is increasing among Mexican-Americans, and that the prevalence of diabetes in this population is twice that of the general population (Cowie, Rust et al. 2010). Co-morbid depression among Mexican Americans with diabetes is extremely high: one in three individuals within this population who have diabetes also report symptoms of depression (deGroot, Pinkerman et al. 2006). Even though rate of co-morbid depression is only slightly higher than whites, the rate of diabetes-related disability and death as a result of poor depression care is much higher (Ibid). Depression among those with diabetes is particularly troubling because depression is associated with hyperglycemia which, in turn, increases the likelihood of macro-vascular complications, such as cardiovascular disease and high blood pressure, and micro-vascular complications, such as retinopathy, neuropathy, and nephropathy (deGroot, Anderson et al. 2001).
Epidemiologists and clinical investigators interested in the interaction of depression and diabetes have largely focused on how the debilitating and distressing aspects of diabetes contribute to depression. However, recent work has documented a possible bidirectional relationship between diabetes and depression, which may decrease self-management activities and may elevate glucose even more; in this way depression may herald the diagnosis of diabetes (Talbot and Nouwen 2000; Knol, Twisk et al. 2006; Golden, Chang et al. 2007; Golden, Lazo et al. 2008; Pan, Lucas et al. 2010). As a result, there have been recent calls for more studies that examine the social and emotional contributors to mental distress among people with diabetes (Fisher, Chesla et al. 2001; Rock 2003; Fisher, Skaff et al. 2008; Pouwer, Kupper et al. 2010). This research is necessary to understand how psychosocial stress may contribute to the higher rates of depression among those with diabetes, particularly in populations with high incident diabetes. Our objective in this study was to elucidate the range of stressors in the lives of first and second generation Mexican immigrant women with diabetes and how they relate to depression in this population.
Background
Ethnographic studies reveal that poor Mexican and immigrant Mexican women in the United States experience severe social stress in their everyday lives. Specifically, domestic violence has been well-documented in the Mexican context (Baker, Norris et al. 2005) and largely framed around constructions of gender and power in Mexican marriages and associated with alcohol abuse among men (Finkler 1994; Finkler 1997; Gutmann 1999; Hirsch 2003). Kaja Finkler’s (1994, 1997) research on married Mexican women describes domestic violence as a fundamental stress, including both physical and sexual abuse that is not only a problem of gender but also class. Finkler comments (1994): “The suffering and afflictions of women living in miserable poverty are as much connected with economic scarcity as they are with inimical social relationships with mates, family, and neighbors” (33). Jennifer Hirsch (2003) found domestic violence similarly to be a problem for married women in Mexico, and argued that the balance of gender and power within Mexican couples was shifting with modernity and migration to the U.S. (Hirsch 2003). Interestingly, evidence in the U.S. suggests that Mexican immigrant populations report higher rates of abuse compared to the general population, and those in Mexico, and that incidence of abuse is higher still among those who are low-income second, third, and fourth generation Mexican-Americans (Holman, Silver et al. 2000; Lown and Vega 2001; Heilemann, Kury et al. 2005; Baker, Norris et al. 2009).
In our previous ethnographic work, we found both structural violence and interpersonal violence to be major contributors to people’s well-being, in addition to depression specifically (Mendenhall, Seligman et al. 2010). This works prompted us to further explore this association in a larger sample, as the relationship of interpersonal abuse and depression is a core concern of psychology and psychiatry, and particularly salient among Mexican-Americans. Multiple studies have demonstrated that women of Mexican descent living in the U.S. experience higher rates of psychiatric distress when compared to other ethnic groups, and to women living in Mexico (Vega, Kolody et al. 1986; Burnam, Hough et al. 1987; Vega, Kolody et al. 1998; Heilemann, Kury et al. 2005; Smith, Poschman et al. 2006; Fisher, Skaff et al. 2008). In a clinical study of 315 low-income women of Mexican descent in California, Heilemann and colleagues (2005) found high rates of depression, which strongly correlated with reporting post-traumatic stress disorder, and these women were more likely to report more traumatic experiences throughout the life course. Importantly, few of these women received the mental health care that they needed due to language barriers and limited access to health care generally. Moreover, a substantial body of research suggests that myriad stresses contribute to poor mental health among immigrant Mexicans in the U.S., including acculturative stress, linguistic and social isolation, work-related stress, and living in unhealthy, and sometimes unsafe, social and physical environments (Vega, Kolody et al. 1986; Moscicki, Locke et al. 1989; Stern, Gonzalez et al. 1992; Vega, Kolody et al. 1998; Hovey 2000; Abraido-Lanza, Chao et al. 2005; Lara, Gamboa et al. 2005; Vega, Ang et al. 2011).
This study was designed to explore the social stressors that are at the center of women’s life stories and to examine major contributors to depression among first and second generation Mexican immigrant women with diabetes in Chicago. In this study, we explore patterns in reporting subjective experiences of social stress in life history narratives. We then examine the association between individuals’ past experiences of social stress with depression. We focus on women specifically because our previous work suggested that women of Mexican descent are more likely to experience the prolonged forms of emotional distress linked with depression compared to men (Mendenhall, Seligman et al. 2010). The focus on women is important, as well, due to the disproportionate number of women with diabetes who suffer diabetes complications as a result of poor mental health care. We hypothesize that prolonged stresses, and particularly a history of interpersonal abuse, identified in women’s life stories would be associated with depression even when controlling for diabetes-related stress. By understanding the social factors that contribute to depression we can develop better strategies for providing the critical social and psychological interventions needed to mitigate the effects of such problems and, potentially in turn, improve their diabetes.
Methods
Data Source
We conducted a cross-sectional study of 121 first and second generation Mexican immigrant women seeking diabetes care in a hospital-based safety-net clinic in Chicago. The primary purpose of the study was to investigate the interface between stress, emotion, mental health, and diabetes control in this population. We recruited a convenience sample of female patients who self-identified as Mexican or Mexican-American, were between the ages of 40 and 65, and could consent in English or Spanish. We excluded patients who did not meet our inclusion criteria or who had cognitive impairment, active substance abuse, or psychosis severe enough to interfere with interviewing or survey administration.
The first author approached patients in the clinic and invited them to participate in a study that they were told was about stress and diabetes. After providing informed consent in English or Spanish, participants were scheduled to complete an in-person interview with the first author. They participated in a two to three hour interview that involved an in-depth qualitative interview followed by the administration of the Center for Epidemiological Studies Depression Scale (CES-D), standardized sociodemographic questions, and finger-stick blood collection. Recruitment and interview administration occurred between February and July 2010. The Institutional Review Boards at Cook County Health and Hospitals System and Northwestern University approved the study.
Qualitative Analysis
We used a systematic analysis of qualitative data to identify stresses in participants’ lives and how they had an impact on women’s every day experiences. Each narrative interview began with: “Can you tell me about your childhood?” Targeted probing included “where did you grow up?” and “can you tell me about your family?” Oftentimes these simple questions launched women into in depth life stories. If family relationships, emotion, past trauma, mental health, and diabetes management did not come up through the iterative process of qualitative interviewing, we followed up with these key questions: “Have you ever been married?” “What age were your first married, can you tell me about that relationship?” “Can you tell me about your family, your children?” “Have you ever experienced strong emotions (like rage-anger/coraje)? If so, what caused these emotions?” “Do any emotions affect your diabetes?” “What caused your diabetes?” “How do you manage your diabetes?” and “Have you been depressed or hopeless in the last month?” If a traumatic experience was not mentioned in the interview, then the following question was asked at the end: “Have you experienced any major stress or trauma in your life?” Because our preliminary ethnographic data indicated that gender-based violence was a major issue among socially disadvantaged Mexican-American women, we asked a specific follow-up question if mistreatment or abuse was not mentioned. However, there rarely was a need for follow-up questions, as most women who experienced trauma or mistreatment brought it up during the natural course of the interview.
The qualitative interviews were transcribed into English or Spanish. Based on the literature review and exploratory ethnographic research, we identified four overarching themes that we predicted would be central to women’s stories: (1) diabetes stress, (2) gender-based violence, (3) family stress, and (4) immigration stress. Through grounded theory analysis of the narrative text we better defined and broke down these codes into seven key sub-codes to represent the most stressful and sometimes traumatic factors represented in the 121 life history narratives collected for this study (Strauss and Corbin 1990). Seven narrative themes (sub-codes) emerged from open coding: (1) interpersonal abuse; (2) health stress; (3) family stress; (4) financial stress; (5) neighborhood violence; (6) immigration stress; and (7) feelings of social isolation. In addition, specific mention of physical and sexual abuse were measured apart from the larger category of interpersonal abuse, which measured any mention of verbal, emotional, physical, or sexual abuse. Exemplar quotations of each category were excerpted for inclusion in this paper and the first author translated the Spanish-language quotes. Qualitative data was reviewed, analyzed, and themes identified before analysis of the quantitative data to avoid any bias in looking for particular stressors or frequency of stressors in women identified as depressed in the quantitative analysis.
Quantitative Measures
Each stressor from qualitative interviews was used as a dichotomous variable (0=No mention of that stress, 1=One or more mention of that stress) for the quantitative analyses.
Depression was measured by administering the Center for Epidemiological Studies Depression Scale (CES-D). The CES-D is a widely used 20-item questionnaire designed to assess the major symptoms of depression in English, and has been validated in Spanish (Radloff 1977; Soler, Perez-Sola et al. 1997). A reliable and well-validated instrument, the CES-D’s targeted symptoms include depressed mood, changes in appetite and sleep, low energy, feelings of hopelessness, low self-esteem and loneliness. Respondents were asked to consider the presence and duration of each item/symptom over the past week and to rate each along a 4-point scale from 0 (rarely or never) to 3 (most or all of the time). Possible scores range from 0 to 60. We present data for two different cut-off scores for the CES-D: (1) ≥16 validated for use as a screen for “likely depression” in community population (Vega and colleagues 1986) to be an acceptable predictive validity as a community screen for depression and (2) ≥24, which is recommended for use to screen for depression in clinical populations; but only use the higher cut-off in our regression analyses because our sample was clinical population.
Diabetes duration was measured by subtracting age of diagnosis from current age. Diabetes severity measured how many symptoms an individual experienced in the past four weeks from a list of six: pins and needles in both feet, a low blood sugar reaction, limb amputation, kidney problems, retinopathy, and neuropathy (0–6). Diabetes distress was measured by a standardized Diabetes Distress Scale that evaluated the mean of responses to five key questions (0–6) (Polonsky, Fisher et al. 2005). Questions from this scale included in this study are: 1) Feeling that diabetes is taking up too much of my mental and physical energy; 9) Feeling angry, scared, and/or depressed when I think about living with diabetes; 17) Feeling that diabetes controls my life; 21) Feeling that I will end up with serious long-term complications, no matter what I do; and 25) Feeling overwhelmed by the demands of living with diabetes.
Finger stick blood samples were collected in conclusion of each interview and analyzed to evaluate hemoglobin (Hb)A1c, a standard measurement for glycemic control in both clinic- and population-based studies (Peterson, Pavlovich et al. 1998; McCarter, Hempe et al. 2006). We dichotomized HbA1c into groups of controlled (less than 7.5) and uncontrolled (7.5 or more).
Analyses were adjusted for independent variables known to be associated with depression including age, education level, income, primary language, birthplace, and acculturation. Age was divided into 2 categories: 40–50 and 50–65 years of age. Family income categories were less than $9,999 (0), $10,000 to $24,999 (1), and $25,000 or more (2). Education ranged from (0) no degree earned, (1) high school diploma or GED, to (2) more than high school. Language preference use was categorized as Spanish or English, according to the language utilized in the qualitative interview; many, but not all, English speakers were bilingual. Birthplace was categorized as either Mexico or the U.S. The Acculturation Rating Scale for Mexican-Americans (ARSMA)-II was used to measure Mexican versus Anglo Orientation, assessing four factors: a) language use and preference, b) ethnic identity and clarification, c) cultural heritage and ethnic behaviors, and d) ethnic interaction (Cueller, Arnold et al. 1995). The linear acculturation scale was derived from subtracting the mean of the Mexican Orientation Scale from the mean of the Anglo Orientation Scale; a negative score indicates that an individual is more Mexican-oriented and a positive score indicates an Anglo orientation.
Quantitative Analysis
First, we conducted bivariate analyses to explore the relationship between each of the stressors and having a CES-D score >24. Second, we examined whether or not psychosocial stressors that were significantly associated with depression correlated with one another and the strength of that correlation. We then used multivariate logistic regression to examine the association of reporting any abuse or physical and sexual abuse alone with depression, adjusting for stressors we found to be significantly associated with depression in bivariate analyses in a stepwise fashion. We excluded feelings of social isolation from this analysis because it represented a small, select group of Mexican immigrant women (n=18). In Model 1 we examined the relationship of abuse with depression, in Models 2 and 3 we examined the relationship between abuse and depression while adjusting for health stress and diabetes distress, respectively; in the final model we adjusted for both stressors. All models were adjusted for age, income, education, acculturation, and glycemic control. Because the results for sexual and physical abuse were very similar to “any abuse”, we present only the data for “any abuse” in Table 4.
Table 4.
Relationship between Reported Stressors and Depression (CESD≥24) in Multivariate Analyses§
| Model 1 OR (95%CI) |
Model 2 OR (95%CI) |
Model 3 OR (95%CI) |
Model 4 OR (95%CI) |
|
|---|---|---|---|---|
| Interpersonal Abuse | 4.49** (1.67–12.1) | 4.28** (1.57,11.6) | 5.75** (1.93,17.1) | 5.51** (1.85,16.4) |
| Health Stress | - | 2.14 (0.91,5.05) | - | 1.53 (0.59,3.99) |
| Diabetes Distress | - | - | 1.85*** (1.36,2.51) | 1.81*** (1.32,2.46) |
p<0.05
p<0.01
p<0.001
All models are adjusted for age, income, education, acculturation, and glycemic control
Results
Table 1 presents the demographic make-up of the women in this study. The women interviewed were 55 years of age on average, with an even distribution between 40 and 65 years. Eighty-two percent of women had an annual household income below the poverty line and less than half completed secondary school. Eighty-nine percent of women were ever married, 65 percent were born in Mexico, and 52 percent spoke Spanish as their primary language. The average number of years spent in the United States among those born in Mexico was 28 years. The average score on the ARSMA-II was −0.97, indicating that the sample was slightly oriented toward Mexican values and beliefs; this finding is not surprising given that two-thirds of these women were Mexican immigrants and one-third were second-generation Mexican-Americans. One in four women were undocumented immigrants.
Table 1.
Sample Characteristics (n=121)
| Variable | Total sample |
|---|---|
| Demographics | |
| Age (years) (mean +/− SD) | 54.42 +/− 8.38 |
| No Educational Degree Earned (n,%) | 70 (58%) |
| Household income Less than $25,000 (n,%) | 99 (82%) |
| Ever Married | 108 (89%) |
| Spanish as Primary Language (n,%) | 63 (52%) |
| Birthplace (Mexico) (n,%) | 79 (65%) |
| Years in the U.S. among Mexican-born (mean +/− SD) | 28 +/−14.9 |
| Acculturation Continuum Scale (ARSMA-II) (mean +/− SD) | −0.97 +/− 1.82 |
| Undocumented Status (n,%) | 33 (27%) |
| Diabetes Measures | |
| Diabetes Duration (years) (mean +/− SD) | 11.18 +/− 9.07 |
| Diabetes Severity (mean +/− SD) | 2.13 +/− 1.61 |
| Diabetes Control (hemoglobin A1c=7.5+) (n,%) | 93 (77%) |
| Diabetes Distress (mean +/− SD) | 3.70 +/− 1.72 |
| Depression Measures | |
| Depression (CESD=16+) (n,%) | 59 (49%) |
| Depression (CESD=24+) (n,%) | 41 (34%) |
The women in our sample had diabetes for an average of eleven years and had an average of two diabetes-related problems. Retinopathy and neuropathy were the most commonly reported diabetes complications. On average, the women reported slightly more than moderate diabetes-related distress, as the mean value of Diabetes Distress Scale was 3.70.
The mean CES-D score was 18.3 (SD+/−14.7). One in every two women (49%) reported a CES-D score above the cut-off point traditionally used in community-based samples to screen for depressive symptoms (CES-D≥16). One-third of the sample (34%) presented very high risk for depression according to a higher cut-off for depression (CES-D≥24).
Qualitative Findings
There were seven life stressors found to be most prevalent among life history narratives (Figure 1). The most frequently reported life stressor was interpersonal abuse, which was reported by two-thirds of the sample. This category was broken down into two additional categories: physical abuse and sexual abuse. Fifty-four percent of women reported physical abuse and 23 percent reported sexual abuse. More than half of the women in this study reported a health-related stress, and just under half the sample reported family stress. One in three women reported financial insecurity as a stress, and one in six women described neighborhood violence, immigration, work, and feelings of social isolation as a source of stress. The average number of qualitatively reported stresses was 3.04 (SD +/−1.51).
Figure 1.
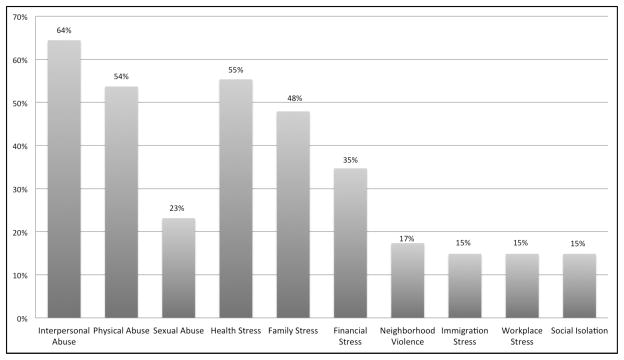
Major Life Stresses Reported in Life History Narratives*
*More than one stressor could be reported
Interpersonal Abuse
Two-thirds of the women interviewed discussed a history of interpersonal abuse. The broad abuse category captured any reported history of emotional neglect, repeated verbal ragging, spousal battering, and childhood sexual violence. While some women only experienced one type of abuse in their lifetimes, many described repeated experiences of mistreatment and had endured more than one form of abuse. Sixty-five percent reported any interpersonal abuse exposure, 54 percent reported physical abuse, and 23 percent reported sexual abuse; 86 percent of women who reported sexual abuse also reported physical abuse (n=24). Ten percent of women reported exposure to verbal and/or emotional abuse only. Below are some representative quotes coded as verbal, emotional, physical, or sexual abuses:
My first marriage “lasted like six and a half years and I finally left. It was—it was—it was [pause] I got beat up, almost every day.” English-speaking Mexican-American woman
“P: My dad’s cousin abused me when I was small. I told my mom, but my mom didn’t want to tell my dad.
EM: Like sexual abuse?
P: Yeah. I was eight.” English-speaking Mexican-American woman
“I separated from him [my first husband] because he drank too much. He would begin to drink and it made him very aggressive. One day I had to call the police. He put a knife to my neck.” Spanish-speaking Mexican woman
Health Stress
The general health stress category captures women’s concerns with physical pain and was the second most commonly reported stressor in the dataset (55%; n=67). While this category incorporated diabetes talk, it was not limited to it, as women described stress due to the management of other physical ailments, including chronic pain, the repercussions of stroke, breast cancer, liver cancer, heart disease, fibromyalgia, and so on, as demonstrated by the following narrative excerpts:
My stress is “from all of the diseases that have developed. Because imagine; I have rheumatism, diabetes, high blood pressure, and asthma.” Spanish-speaking Mexican woman
“I started gaining lots of weight and I ended up having hypo-thyroid. And I think that led up to diabetes and diabetes led up to heart problems and that led up to, you know, the neuropathy and fibromyalgia and [pause] all that.” English-speaking Mexican-American woman
Family Stress
Stress related to family members’ struggles, behaviors, illnesses, and needs was the third most commonly reported narrative theme in the dataset, mentioned by almost half the sample (n=58). Women primarily reported family stress in relation to their caretaker role for grandchildren or sick parents and/or siblings, mothers of disobedient children, and/or wives of husbands who were unfaithful, sick, or drug abusers. As one woman described:
“Watching my mom and my grandma—taking care of—being with two older women, it just—really, it’s very stressful. Like, taking care of them, their medical problems, their every day daily activities.” English-speaking Mexican-American woman
Feelings of Social Isolation
Many women spoke about feeling socially isolated while at the same time being surrounded by family members. Some women spoke of longing to spend time with their family in Mexico, and others said that their family in the U.S. didn’t understand them. Some women relayed that they felt taken advantage of in the U.S.; many of these women moved to the U.S. to be with their grown children and took care of the house, cooking, and childcare (n=18). As such, twenty percent of women born in Mexico reported feeling lonely, compared to only five percent of women born in the U.S.
“I came here to be here with my two daughters. Nothing else. I should have stayed there [in Mexico]… sometimes I feel like leaving. And my kids say to me, ‘No where would you go?’ They say that because who is going to cook, who is going to look after the [kids]? No, no. [pause] Yes, I want to go. Already I am tired of the cold, I can’t leave the house in all this snow.” Spanish-speaking Mexican woman
Financial Stress
This category captures those who reported financial struggle as a principle stress (n=42); these women were more likely to have higher education and be employed.
“I feel a little worried about my situation right now because I have so many bills for food, for bus fair, and my sales [in my job] are not good.” Spanish-speaking Mexican woman
The Stresses of Neighborhood Violence, Immigration, and Work
Women described neighborhood violence as an everyday stress that permeated their lives both acutely (e.g., shootings) and chronically via gang or drug influence on children and/or reduced exercise due to living in unsafe environments (n=21).
“We weren’t afraid of walking in the street, back in the days. Now, you can’t walk in the—not even half-block and you’re being attacked, raped, killed, you know—here in Chicago it is [pause] I don’t go out here in Chicago.” English-speaking Mexican-American woman
While sixty percent of women (n=72) reported that they were citizens, forty percent (n=49) reported that they were not. Of these women who were not citizens, 67 percent (n=33) were undocumented immigrants. This category captures immigration-related stress only, such as memory of a traumatic border crossing and/or the stress of having a family member deported (n=18):
“They took my son to jail and gave him to immigration.” Spanish-speaking Mexican woman
Finally, women reported stress related to previous or current work-related grievances (e.g., work-related injury or through negative emotion associated with racism or unfair compensation) (n=18).
“When I was working for Fannie Mae there was too much stress, too much pressure. The job was very fast, there were many problems. And there, since I was having to work there, I think that I developed hypertension, and that was because of the pace of the job.” Spanish-speaking Mexican woman
Quantitative Findings
The results of the bivariate analysis of the relationship between psychosocial stressors and depression are presented in Table 2. The odds of being depressed were significantly higher for women who reported any abuse, physical abuse, sexual abuse, social isolation, health stress, and diabetes distress. Stress related to finances, family, work, immigration, and neighborhood violence were not significantly associated with depression in these analyses.
Table 2.
Relationship between Reported Stressors and Depression (CESD≥24) in Unadjusted Analyses
| Depression | |||
|---|---|---|---|
| OR | 95% CI | P-values | |
| Any abuse | 3.97 | 1.58–10.0 | 0.00 |
| Physical abuse | 2.95 | 1.32–6.60 | 0.01 |
| Sexual abuse | 3.63 | 1.51–8.72 | 0.00 |
| Social Isolation | 3.82 | 1.35–10.8 | 0.01 |
| Health stress | 2.26 | 1.03–4.99 | 0.04 |
| Family Stress | 1.64 | 0.77–3.51 | 0.20 |
| Financial Stress | 0.96 | 0.44–2.13 | 0.93 |
| Neighborhood Violence | 1.25 | 0.47–3.31 | 0.65 |
| Immigration Stress | 1.29 | 0.46–3.63 | 0.63 |
| Work Stress | 1.29 | 0.46–3.63 | 0.63 |
| Diabetes Distress | 1.67 | 1.28–2.19 | 0.00 |
p<0.05
p<0.01
p<0.001
We examined correlations between the stressors that were significantly associated with depression (Table 3). Feelings of social isolation strongly correlated with interpersonal abuse category, in addition to sexual abuse, but not with physical abuse. Health stress correlated with physical abuse only, and with diabetes distress. Social isolation also positively correlated with diabetes distress. Diabetes distress correlated with health stress.
Table 3.
Correlations Among Reported Stressors
| Sexual Abuse | Social Isolation | Health Stress | Diabetes Distress | |
|---|---|---|---|---|
| Interpersonal Abuse | - | 0.21* | 0.13 | −0.10 |
| Physical Abuse | 0.35* | 0.16 | 0.20* | 0.00 |
| Sexual Abuse | - | 0.21* | 0.14 | 0.15 |
| Social Isolation | - | - | 0.10 | 0.20* |
| Health Stress | - | - | - | 0.21* |
p<0.05
The results from the adjusted multivariate analyses investigating the association between interpersonal abuse and depression are shown in Table 4. We found that the odds of having depression were significantly greater for those women who had experienced interpersonal abuse (Model 1) and that this relationship persisted after adding health stress (Model 2) or diabetes distress (Model 3) alone or together (Model 4) into the model.
DISCUSSION AND CONCLUSIONS
To our knowledge, this study is the first to use life history narratives to examine social stressors among low-income first and second generation Mexican immigrant women with diabetes and how they relate to depression in this population. We have highlighted the seven most commonly reported stresses in women’s stories to reveal how social distress might contribute to depression. The data confirm several expectations, but bring to light other issues that better elucidate the relationship between depression and the forms of social distress that are most significant to the lives of low-income Mexican immigrant women with diabetes. Our data suggest that both past and current life experiences are important determinants of depression in this population. We found that both past traumatic experience and current social isolation and health stress are important determinants of depression in this vulnerable population of women with diabetes. We also found much higher rates of depression and reported interpersonal abuse than in previous studies focusing on Latinos, which we believe highlights the particular vulnerability of Mexican American women with diabetes seeking medical care at safety-net clinics.
First, prevalence of interpersonal abuse found within this sample suggests that the conditions in which women live may facilitate in some sense increased risk for and experience of abuse. Specifically, abuse prevalence within this sample was substantially higher than population-based studies of Mexican-Americans diverse in socioeconomic status. For example, Lown and Vega (2001) found a 10.7 percent prevalence of physical abuse in a socioeconomically diverse population of Mexican-American women, compared to the 54 percent of physical abuse exposure in the present sample. A study focused on similarly impoverished women of Mexican descent seeking primary care at a safety-net clinic in California found comparable rates of physical violence to the present study (Heilemann, Kury et al. 2005). It is crucial to identify such intra-ethnic differences because they demonstrate that high rates of interpersonal abuse may stem from contextual factors, such as poverty and immigration stress (see Benson, Wooldredge et al. 2004), as opposed to Mexican or Mexican-American ethnicity. While there certainly are cultural factors that contribute to the manner in which individuals cope with and manage stress, salience of such social distress at the population level must be understood as interlinked with structural inequalities. As such, interpersonal abuse, which is often gender-based, may be understood to be one manifestation of such inequities (Bourgois 2009).
Second, on average women reported two to four major life stressors and many of the narrative themes were correlated with one another. Understanding the interactions between and effects of two or more stresses in the life course is essential, as we have learned from The ACE Study that stressful experiences rarely occur in isolation (Dong, Anda et al. 2004). By examining the relationships between narrative themes, we can develop a better understanding of their intersection within the dataset at large. For example, while the broad category of interpersonal abuse correlated strongly with feelings of social isolation, there was some variability between physical and sexual abuse. Sexual abuse strongly correlated with feelings of social isolation, but physical abuse did not (and in contrast uniquely correlated with health stress). Such findings might suggest that women who have experienced sexual abuse are more likely to socially isolate from arterial social networks. Also, because sixteen of the eighteen women who reported feelings of social isolation were Mexican immigrants, it may be that changing familial, cultural, and social structures affect coping strategies linked with interpersonal abuse. At the same time, many of these women reported more general family stress, which may figure into their tendency to socially isolate, in addition to their diabetes distress; such findings may further indicate that these women are less likely to seek support and care from family and friends for their emotional needs, or diabetes care.
Third, through examination of these narrative themes the macro-level political-economic and social inequalities that facilitate these micro-level stresses become clearer. For example, financial stress and the breakdown of social networks resulting from immigration played a powerful role in cultivating the conditions in which women experienced abuse and social detachment. At the same time, women described everyday struggles with economic insecurity, work stress, and family stress. They communicated fears rooted in the deleterious environments in which they lived, often linking gang- and drug-related violence with family and immigration stress. Additionally, many immigrant women feared every day for the safety of family members while at the same time struggling with family discord. Understanding these interconnections is critical for studies of mental health because the confluence of structural violence, poverty, and stress together contribute to significant burden of depression and cannot be dissociated from self-care corollary to diabetes management.
In sum, the unique social experiences of the women in our sample are likely what contributed to high rates of psychosocial stress and depression. At the same time, these higher rates of depression may be rooted in poor access to mental health care and the fact that social stresses such as interpersonal abuse frequently goes unnoticed in primary care settings where much of the attention is devoted to the physical problems associated with diabetes (Weiner, Schwartz et al. 2007; Weiner, Schwartz et al. 2010). Moreover, scholars suggest that individuals who internalize the negative side of themselves and the world are more likely to report past experiences with and psychological symptoms of distress (Dohrenwend, Dodson et al. 1984; Watson and Clark 1984). In other words, individuals in this sample might have been more prone to negative affect, defined as someone who experiences a wide variety of unpleasant states (e.g., distressed, nervous, angry, guilty, scornful) (Watson and Clark 1984), which would contribute to increased rate of reporting social stress in life history narratives and depression according to the CES-D. On the other hand, it may be that in addition to chronic adversity, individuals who experience stressful life experiences in childhood and throughout adulthood are more likely to internalize negative experiences, socially isolate from family and friends, dwell on stressful aspects of their lives, and develop diabetes. Hence, sampling women with diabetes might have contributed to the higher rates of reporting interpersonal abuse and depressive symptoms.
Nevertheless, compared to the surprisingly high rates of interpersonal abuse reported and the cumulative impact of social distress revealed through women’s life history narratives, we might expect depression to be even higher. In fact, the more conservative measure of high likelihood of depression (CES-D≥24) indicated that our findings may resemble depression among Latinos with diabetes more broadly (deGroot, Pinkerman et al. 2006). In this sense, we might consider the rate of depression within this population to be somewhat low when we compare it to the high rates of abuse, and sexual abuse in particular. As such, we must consider that the majority of these women have social network resources that sustain them emotionally and financially, as they are the ones who are able to seek medical care at the clinic itself. Indeed, depression prevalence may be much higher among women who do not make it to a safety-net medical clinic for diabetes and/or depression care.
This work is not without limitations. We interviewed a convenience sample of patients at a safety-net clinic in Chicago, which limits its broad generalizability. However, this allowed us to conduct in-depth interviews and gain a more comprehensive understanding of what stressors impact vulnerable Mexican immigrant women with diabetes. Indeed, as with any interview that involved memory work of life events, recall bias must be considered as a potential limitation. Moreover, this is a cross-sectional mixed qualitative and survey study so we are unable to assign causality between stressors and depression and some of our measures, while validated, may be limited by their use in the context of a survey. That said our study suggests an important link between social suffering and depression in this vulnerable group of women.
There is a need to understand parallels among documented increases of interpersonal abuse and depression among Mexican immigrant women with diabetes in the United States. Future studies require systematic collection of both histories of traumatic experience and treatment histories so that we can understand the interactions of past exposure to interpersonal abuse – including both severe experiences such as childhood sexual abuse and more moderate stress related to verbal ragging – and depression care that might mitigate the effects of such experiences at a young age. Indeed, both the extended period of time through which the women in this study have suffered alone with their stories of abuse and the lack of mental health care available to them likely have contributed significantly to the progression of their depression, and potentially of their diabetes. Additionally, a study comparing people with and without diabetes would provide insight into the role of severe social stress as a contributor to depression and the development of type 2 diabetes. Such an approach would provide an in depth understanding of social and emotional experiences of those who are both exposed to traumatic experiences in childhood and early adulthood, and who have increased risk for chronic disease (Felitti, Anda et al. 1998).
Our study highlights the link between depression and social problems among low-income population, in addition to the potential impact of such interaction among people with diabetes. Asking about and mitigating social stress within the clinical encounter may be a more relevant target than focusing on the treatment of diabetes and diabetes distress alone. Policy-makers need to recognize this and improve mental health care and social services for this population focused on the prevention and mitigation of interpersonal abuse. Connecting such services with diabetes care is crucial. Looking forward, these findings suggest that earlier psychological and social service intervention has the potential to make a major impact in the adult mental and physical health of the socially disadvantaged. In addition to this study that focuses on the contributors to depression among women with diabetes, studies are beginning to explore the effect of emotional stressors on diabetes onset (Pan, Lucas et al. 2010; Pouwer, Kupper et al. 2010). More qualitative and context-specific data is needed to understand what forms of stress affect the health and well-being of specific populations, and what age is most productive for intervention.
Acknowledgments
The authors wish to thank the women at John H. Stroger, Jr. Hospital of Cook County for participating in this study and sharing so openly their stories. Additionally, thank you to the staff at the GMC for providing support and space for this study amidst their busy schedules. Thank you to Erin P. Finley and Kenneth Maes for reading early drafts of the manuscript and to the anonymous reviewers for their insightful comments. Emily Mendenhall was supported by the National Science Foundation (Grant #1024116), Cells to Society at Northwestern University, and The Graduate School at Northwestern University. We are also grateful to the Russell Sage Foundation because they supported Dr. Elizabeth Jacob and the preliminary work that inspired this work.
References
- Abraido-Lanza A, Chao M, et al. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science and Medicine. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderete E, Vega W, et al. Effects of time in the United States and Indian ethnicity on DSM-III-R psychiatric disorders among Mexican Americans in California. Journal of Nervous and Mental disease. 2000;188(2):90–100. doi: 10.1097/00005053-200002000-00005. [DOI] [PubMed] [Google Scholar]
- Alderete E, Vega W, et al. Lifetime prevalence of and risk factors for psychiatric disorder among Mexican migrant farm workers in California. American Journal of Public Health. 2000;90(4):608–614. doi: 10.2105/ajph.90.4.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegria M, Canino G, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino Groups. The American Journal of Pyschiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegria M, Mulvaney-Day N, et al. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007;97(1):68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker C, Norris F, et al. Violence and PTSD in Mexico: gender and regional differences. Social Psychiatry and Psychiatric Epidemiology. 2005;40(7):519–528. doi: 10.1007/s00127-005-0921-2. [DOI] [PubMed] [Google Scholar]
- Baker C, Norris F, et al. Childhood trauma and adulthood physical health in Mexico. Journal of behavioral medicine. 2009 doi: 10.1007/s10865-009-9199-2. pub online 28 Jan. [DOI] [PubMed] [Google Scholar]
- Benson ML, Wooldredge J, et al. The Correlation between Race and Domestic Violence is Confounded with Community Context. Social Problems. 2004;51(3):326–342. [Google Scholar]
- Black S. Increased health burden associated with comorbid depression in older diabetic Mexican Americans. Results from the Hispanic Established Population for the Epidemiologic Study of the Elderly survey. Diabetes Care. 1999;22(1):56–64. doi: 10.2337/diacare.22.1.56. [DOI] [PubMed] [Google Scholar]
- Bourgois P. Recognizing Invisible Violence. In: Rylko-Bauer B, Whiteford L, Farmer P, editors. Global Health in Times of Violence. Santa Fe, NM: School for Advanced Research Press; 2009. pp. 17–40. [Google Scholar]
- Burnam M, Hough R, et al. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of health and social behavior. 1987;28:89–102. [PubMed] [Google Scholar]
- Castañeda H. Im/migration and Health: Conceptual, Methodological, and Theoretical Propositions for Applied Anthropologyby. Annals of Applied Anthropology (Formerly NAPA Bulletin) 2010;34(1):6–27. [Google Scholar]
- Cowie CC, Rust KF, et al. Prevalence of Diabetes and High Risk for Diabetes using A1C Criteria in the U.S. Population in 1988–2006. Diabetes Care. 2010;33(3):562–568. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cueller I, Arnold B, et al. Acculturation rating scale for Mexican Americans II. Hispanic Journal of Behavioral Sciences. 1995;17(3):275–304. [Google Scholar]
- deGroot M, Anderson RJ, et al. Association of Depression and Diabetes Complications: A Meta-Analysis. Psychosomatic Medicine. 2001;63:619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- deGroot M, Pinkerman B, et al. Depression treatment and satisfaction in a multicultural sample of type 1 and type 2 diabetic patients. Diabetes Care. 2006;29:549–553. doi: 10.2337/diacare.29.03.06.dc05-1396. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Dodson M, et al. Symptoms, Hassles, Social Supports, and Life Events: Problem of Confounded Measures. Journal of Abnormal Psychology. 1984;93(2):222–230. doi: 10.1037//0021-843x.93.2.222. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Escobar JI, Hoyos Nervi C, et al. Immigration and mental health: Mexican Americans in the United States. Harvard Review of Psychiatry. 2000;8:64–72. [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, et al. Relationship of childhood abuse and household dysrunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkler K. Women in Pain: Gender and Morbidity in Mexico. Philadelphia: University of Philadelphia Press; 1994. [Google Scholar]
- Finkler K. Gender, Domestic Violence and Sickness in Mexico. Social Science and Medicine. 1997;45(8):1147–1160. doi: 10.1016/s0277-9536(97)00023-3. [DOI] [PubMed] [Google Scholar]
- Fisher L, Chesla C, et al. Contributors to depression in Latino and European American patients with type 2 diabetes. Diabetes Care. 2001;24:1751–1757. doi: 10.2337/diacare.24.10.1751. [DOI] [PubMed] [Google Scholar]
- Fisher L, Skaff M, et al. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with Type 2 diabetes. Diabetic Medicine. 2008;25(9):1096–1101. doi: 10.1111/j.1464-5491.2008.02533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerst K, Al-Ghatrif M, et al. High depressive symptomatology among older community-dwelling Mexican-Americans: The impact of immigration. Aging Mental Health. 2010;14(3):347–354. doi: 10.1080/13607860903292578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden S, Lazo M, et al. Examining a bidirectional association between depressive symptoms and diabetes. Journal of the American Medical Association. 2008;299(23):2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden SH, Chang BLH, et al. Depression and Type 2 Diabetes Mellitus: The Multiethnic Study of Atherosclerosis. Psychosomatic Medicine. 2007;69:529–536. doi: 10.1097/PSY.0b013e3180f61c5c. [DOI] [PubMed] [Google Scholar]
- Gonzalez HM, Tarraf W, et al. The epidemiology of major depression and ethnicity in the United States. Journal of Psychiatric Research. 2010 doi: 10.1016/j.jpsychires.2010.03.017. epub: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutmann MC. Ethnicity, alcohol, and acculturation. Social Science & Medicine. 1999;48:173–84. doi: 10.1016/s0277-9536(98)00325-6. [DOI] [PubMed] [Google Scholar]
- Heilemann MV, Kury FS, et al. Trauma and Posttraumtaic Stress Disorder Symptoms among Low Income Women of Mexican Descent in the United States. The Journal of Nervous and Mental Disease. 2005;193(10):665–672. doi: 10.1097/01.nmd.0000180741.93635.ab. [DOI] [PubMed] [Google Scholar]
- Hirsch J. A Courtship After Marriage: Sexuality and Love in Mexican Transnational Families. Berkeley: University of California Press; 2003. [Google Scholar]
- Holman EA, Silver RC, et al. Traumatic Life Events in Primary Care Patients: A Study in an Ethnically Diverse Sample. Archives of Family Medicine. 2000;9(9):802–810. doi: 10.1001/archfami.9.9.802. [DOI] [PubMed] [Google Scholar]
- Hovey J. Acculturative Stress, Depression and Suicidal Ideation in Mexican Immigrants. Cultural Diversity and Ethnic Minority Psychology. 2000;6(2):134–151. doi: 10.1037/1099-9809.6.2.134. [DOI] [PubMed] [Google Scholar]
- Knol M, Twisk J, et al. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–845. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, et al. Acculturation and Latino Health in the United States: A Review of the Literature and its Sociopolitical Context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lown EA, Vega WA. Prevalence and Predictors of Physical Partner Abuse Among Mexican American Women. American Journal of Public Health. 2001;91(3):441–445. doi: 10.2105/ajph.91.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarter R, Hempe J, et al. Mean Blood Glucose and Biological Variation Have Greater Influence on HbA1c Levels than Glucose Instability. Diabetes Care. 2006;29:352–355. doi: 10.2337/diacare.29.02.06.dc05-1594. [DOI] [PubMed] [Google Scholar]
- Mendenhall E, Seligman R, et al. Speaking through Diabetes: Rethinking the Significance of Lay Discourses on Diabetes. Medical Anthropology Quarterly. 2010;24(2):220–239. doi: 10.1111/j.1548-1387.2010.01098.x. [DOI] [PubMed] [Google Scholar]
- Moscicki E, Locke B, et al. Depressive symptoms among Mexican Americans: The Hispanic Health and Nutrition Examination Survey. American Journal of Epidemiology. 1989;130:348–360. doi: 10.1093/oxfordjournals.aje.a115341. [DOI] [PubMed] [Google Scholar]
- Pan A, Lucas M, et al. Bidirectional Association Between Depression and Type 2 Diabetes Mellitus in Women. Archives of Internal Medicine. 2010;170(21):1884–1891. doi: 10.1001/archinternmed.2010.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson K, Pavlovich J, et al. What is hemoglobin A1c? An analysis of glycated hemoglobins by electrospray ionization mass spectrometry. Clinical Chemistry. 1998;44(9):1951–1958. [PubMed] [Google Scholar]
- Polonsky WH, Fisher L, et al. Assessing Psychosocial Distress in Diabetes. Diabetes Care. 2005;28:626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- Pouwer F, Kupper N, et al. Does Emotional Stress Cause Type 2 Diabetes Mellitus? A Review from the European Depression in Diabetes EDID Research Consortium. Discovery Medicine. 2010;9(45):112–118. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Rock M. Sweet Blood and Social Suffering: Rethinking Cause-Effect relationships in Diabetes, Distress and Duress. Medical Anthropology. 2003;22:131–174. doi: 10.1080/01459740306764. [DOI] [PubMed] [Google Scholar]
- Smith MV, Poschman K, et al. Symptoms of Posttraumatic Stress Disorder in a Community Sample of Low-Income Pregnant Women. American Journal of Psychiatry. 2006;163:881–884. doi: 10.1176/ajp.2006.163.5.881. [DOI] [PubMed] [Google Scholar]
- Soler J, Perez-Sola V, et al. Validation Study of the Center for Epidemiological Studies-Depression of a Spanish population of patients with affective disorders. Actas Luso Esp Neurol Psiquiatr Cienc Afines. 1997;25(4):243–249. [PubMed] [Google Scholar]
- Stern M, Gonzalez C, et al. Genetic and environmental determinants of type II diabetes in Mexico City and San Antonio. Diabetes. 1992;41(4):484–492. doi: 10.2337/diab.41.4.484. [DOI] [PubMed] [Google Scholar]
- Strauss AL, Corbin JM. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Talbot F, Nouwen A. A Review of the Relationship between Depression and Diabetes in Adults: Is There a Link? Diabetes Care. 2000;23(10):1556–1562. doi: 10.2337/diacare.23.10.1556. [DOI] [PubMed] [Google Scholar]
- Vega W, Ang A, et al. Neighborhood protective effects on depression in Latinos. American Journal of Community Psychology. 2011;47(1–2):114–126. doi: 10.1007/s10464-010-9370-5. [DOI] [PubMed] [Google Scholar]
- Vega W, Kolody B, et al. Depressive Symptoms and Their Correlates Among Immigrant Mexican Women in the United States. Social Science & Medicine. 1986;22(6):645–652. doi: 10.1016/0277-9536(86)90037-7. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, et al. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55:771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative Affectivity: The Disposition to Experience Aversive Emotional States. Psychological Bulletin. 1984;96(3):465–490. [PubMed] [Google Scholar]
- Weiner S, Schwartz A, et al. Evaluating physician performance at individualizing care: a pilot study tracking contextual errors in medical decision making. Medical Decisiom Making. 2007;27:726–734. doi: 10.1177/0272989X07306113. [DOI] [PubMed] [Google Scholar]
- Weiner SJ, Schwartz A, et al. Contextual Errors and Failures in Individualizing Patient Care. Annals of Internal Medicine. 2010;153(2):69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]


