Abstract
Odontoma, complex type is an agglomerate of all the dental tissues that are characterized by normal histodifferentiation but abnormal morphodifferentiation producing little or no resemblance to normal tooth form. They are usually asymptomatic but often associated with eruption disturbances. An interesting case of unusually large complex odontoma that was associated with pain and an impacted as well as missing molar is reported.
Keywords: Odontoma, Complex odontome, Compound, Infected, Erupting, Impacted tooth
Introduction
The term odontoma (or odontome) firstly described by Paul Broca in 1867 was originally used as a general descriptive for any tumor (in its broadest sense) of odontogenic origin. However, owing to their composition and behavior, odontomas have become known as hamartomatous lesions or malformations rather than true neoplasms; the epithelial and the ectomesenchymal tissues along with their respective cells may appear normal, but they seem to have a deficit in the structural arrangement [1, 2]. On the basis of gross, radiographic, and microscopic features, two types of odontoma are recognized: the compound and the complex [3]. The compound odontome has all the dental tissues represented in a more orderly fashion, so that the lesion consists of many small tooth like structures each having enamel, dentin, cementum and pulp arranged as in a normal tooth. The odontoma, complex type (ODCx) is a hamartomatous lesion in which all the dental tissues are represented, individual hard tissues being mainly well formed but occurring in a more or less disorderly pattern [2].
The ODCxs are slow growing, expanding lesions that are usually detected in the second decade of life [1, 2]. The lesions are invariably asymptomatic and are usually discovered on routine radiographic examinations. Most of the odontomas are associated with pathologic changes such as malformation, impaction, delayed eruption, malpositioning, cyst formation or displacement and resorption of adjacent teeth, but only rarely are they seen to be associated with the absence of one or more contiguous teeth [1, 4]. Both kinds of odontomas are generally present with in the jaw bones with only eight cases reported as peripheral developing odontomas [5]. Some are reported to be found in the maxillary sinus, or subcondylar regions [6]. In extremely rare instances they may seem to erupt into the oral cavity [3, 7–9]. One such unusual case of erupting ODCx associated with pain is reported and discussed.
Case Report
A 17 year old male was referred to the department of oral and maxillofacial surgery, with pain in the posterior mandible on the right side. The patient was afebrile past medical and family histories were unremarkable. There was no history of trauma or swelling of the maxillofacial region and this was the patients’ first visit to a dentist. The right submandibular lymph nodes were palpable, tender and movable. Intraoral examination revealed slightly expanded buccal cortex distal to the permanent mandibular right first molar (46) with apparent absence of the right mandibular second (47) and third molars (48). A firm mass in the gingiva distal to 46 was found on palpation with pus discharging through a sinus opening over the alveolar mucosa.
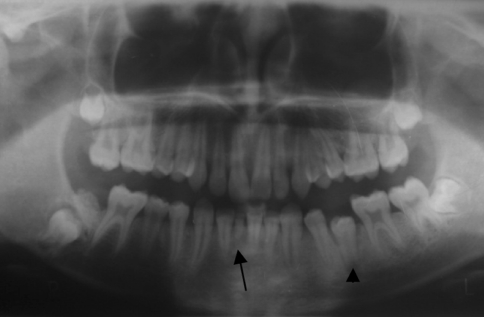
Panoramic radiograph showed a predominantly radio-opaque mass similar in density to calcified dental tissues, with small radiolucencies within, located distal to 46 and coronal to impacted and displaced 47 (Fig. 1). Radiograph also revealed incompletely formed roots of 47, missing 48 tooth bud, missing permanent mandibular right central incisor (41), with its deciduous predecessor retained (81) and submerged permanent mandibular left first premolar (35) with open apex.
Fig. 1.
Radiographs showing an erupting irregular calcified mass of tooth radiodensity present coronal to the impacted 47, retained 81 (arrow) and 35 (arrow head) with an open apex
Taking into account the clinical and radiological presentations, a provisional diagnosis of infected erupting complex odontome was determined and the case was planned for surgical excision under local anesthesia. A triangular mucoperiosteal flap was raised to expose the very superficially located mass that was removed and submitted for histopathological examination (Fig. 2). The tooth beneath was left in place undisturbed for further eruption into the oral cavity (Fig. 3). Pain was relieved and the postoperative healing was uneventful. The patient was explained about the second surgery and or orthodontic intervention if necessary to facilitate the eruption of 47 and advised for regular follow-up. Histopathological examination of the excised mass showed irregularly arranged dental hard tissues with areas of cell rich pulpal tissue. Clear spaces and clefts representing the mature enamel that is lost in the process of decalcification are often seen confirming the diagnosis of a complex odontoma (Fig. 4). Few islands of odontogenic epithelium along with thin fibrous capsule surrounding the lesion are evident. The adjacent tissue showed profuse chronic inflammatory cell infiltrate; suggestive of the lesion being secondarily infected.
Fig. 2.
Gross specimen––the completely excised irregular calcified mass
Fig. 3.
Pre and post operative (8 weeks follow-up) intraoral peri-apical radiographs depicting the calcified mass being removed and tooth left undisturbed for eruption because of its favorable position
Fig. 4.
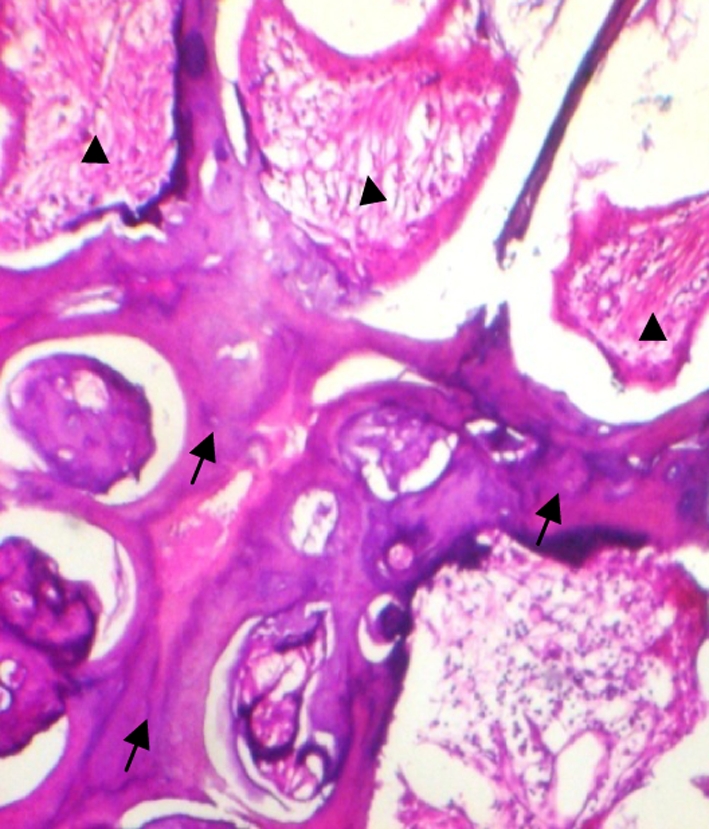
Decalcified hematoxylin and eosin stained section showing irregularly arranged dental tissues principally dentine (arrow) and pulp (arrow head)
Discussion
The etiology of ODCx is unknown. Several theories have been proposed, including local trauma, infection, family history, and genetic mutation. It has also been suggested that odontomas are inherited from a mutant gene or interference, possibly postnatal with the genetic control of tooth development [2].
Though it is agreed that ODCx tend to occur in the posterior regions of the mandible, differences exist in the literature regarding their prevalence [1, 2]. With a slight preponderance to females, the relative frequency of occurrence varies between 5 and 30% [2]. They may be discovered at any age, while the majority of cases (84%) occur before the age of 30. With a peak in the second decade of life, less than 10% are only found in the patients over 40 years of age [1, 7]. Unerupted teeth are associated with 10–44% of ODCx and delayed eruption of at least one permanent tooth, mostly being canines account to 74% [2].
Although they are usually asymptomatic and often detected on routine radiographs [2] clinical indicators of odontoma may include retention of deciduous teeth, non-eruption of permanent teeth, expansion of the cortical bone and tooth displacement. While few presented with other symptoms include paresthesia of the lower lip, headache in the frontal area of the skull and swelling in the affected area [1, 10], pain associated primarily with odontomas seems rather rare [3, 4, 7, 10].
The radiological appearance of ODCx depends on their stage of development and degree of mineralization. The first stage is characterized by radiolucency due to lack of calcification. Partial calcification is observed in the intermediate stage, while in the third stage the lesion usually appears radiopaque with amorphous masses of dental hard tissue surrounded by a thin radiolucent zone corresponding to the connective capsule histologically [2].
In our case, the lesion is found distal to 46 and overlying the crown of an impacted 47 and missing 48. Odontoma associated with the absence of one or more contiguous teeth seems to be rare. The radiolucencies found with in the lesion may very well correlate with the pulp like soft tissue seen histologically and we consider the present lesion to be not completely matured––the intermediate stage.
The present case is exceptional not only because of the size of the tumor and its association with pain and infection, but also because of its apparent eruption and location. Most of the erupted odontomas are reported to be compound and are often found in the maxilla with very few being complex [3, 7–9]. The proximity of the lesion to the surface of gingiva (erupting) and its closeness to the distal surface of first molar could very well be causative of the symptoms.
However, in the case of odontomas erupting into the oral cavity, the mechanism behind the eruption remains uncertain. It appears to be different from tooth eruption because of the lack of periodontal ligament in odontoma. Although there is no root formation in odontoma, its increasing size may lead to the sequestration of the overlying bone and, hence, occlusal movement or eruption [7]. It is likely that resorption of the edentulous part of the alveolar process as seen in older individuals may play a role, but it is also possible that reactive growth of the capsule contributes to this phenomenon [8]. Another reason for odontoma eruption could be the bony remodeling of the jaws. Eruption at a young age is possible through bone remodeling that might have resulted from the presence of dental follicles [7].
If the lesion is located at pericoronal level as with our case, presenting as mixed radiolucencies, it should be differentiated from adenomatoid odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibrodentinoma or odontoameloblastoma. Presence of disorderly arranged well formed dental tissues on histopathological examination will confirm the diagnosis of complex odontome.
The steps in removal of an odontoma in close relation to an adjacent impacted normal tooth should comprise removal of tumor and exposure of the impacted tooth. Orthodontic therapy may be applied. Removal of the odontome in the primary operation led to the eruption of the impacted tooth in 45% of cases, with a second surgical and/or orthodontic intervention giving better results. The morphology of the tooth, its location and position in the jaw and the available space in the dental arch should be examined radiographically, which will determine the treatment [11].
Conclusion
We present a rare case of erupting, complex odontome that was secondarily infected and associated with an impacted second molar and a missing third molar. Although rare, recognition of the potential of complex odontomas to form in association with impacted and missing teeth is important and the authors stress upon the importance of routine use of panoramic radiography for early detection of such dental abnormalities and prevention of adverse effects.
References
- 1.Budnick SD. Compound and complex odontomas. Oral Surg Oral Med Oral Pathol. 1976;42(4):501–506. doi: 10.1016/0030-4220(76)90297-8. [DOI] [PubMed] [Google Scholar]
- 2.Reichart AP, Philipsen HP. Odontogenic tumors and allied lesions. London: Quintessence; 2004. [Google Scholar]
- 3.Kaneko M, Fukuda M, Sano T, Ohnishi T, Hosokawa Y. Microradiographic and microscopic investigation of a rare case of complex odontoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(1):131–134. doi: 10.1016/S1079-2104(98)90163-9. [DOI] [PubMed] [Google Scholar]
- 4.Lee CH, Park GJ. Complex and compound odontomas are clinico-pathological entities. Basic Appl Pathol. 2008;1:30–33. doi: 10.1111/j.1755-9294.2008.00008.x. [DOI] [Google Scholar]
- 5.Ide F, Mishima K, Saito I, Kusama K. Rare peripheral odontogenic tumors: report of 5 cases and comprehensive review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):e22–e28. doi: 10.1016/j.tripleo.2008.05.064. [DOI] [PubMed] [Google Scholar]
- 6.Visscher JG, Güven O, Elias AG. Complex odontoma in the maxillary sinus. Report of 2 cases. Int J Oral Surg. 1982;11(4):276–280. doi: 10.1016/S0300-9785(82)80081-1. [DOI] [PubMed] [Google Scholar]
- 7.Vengal M, Arora H, Ghosh S, Pai KM. Large erupting complex odontoma: a case report. J Can Dent Assoc. 2007;73(2):169–173. [PubMed] [Google Scholar]
- 8.Ragalli CC, Ferreria JL, Blasco F. Large erupting complex odontoma. Int J Oral Maxillofac Surg. 2000;29(5):373–374. doi: 10.1016/S0901-5027(00)80056-9. [DOI] [PubMed] [Google Scholar]
- 9.Amado Cuesta S, Gargallo Albiol J, Berini Aytés L, Gay Escoda C. Review of 61 cases of odontoma. Presentation of an erupted complex odontoma. Med Oral. 2003;8(5):366–373. [PubMed] [Google Scholar]
- 10.Tüzüm MS. Orofacial pain associated with an infected complex odontome case report. Aust Dent J. 1990;35(4):352–354. doi: 10.1111/j.1834-7819.1990.tb00784.x. [DOI] [PubMed] [Google Scholar]
- 11.Morning P. Impacted teeth in relation to odontomas. Int J Oral Surg. 1980;9(2):81–91. doi: 10.1016/S0300-9785(80)80043-3. [DOI] [PubMed] [Google Scholar]