Abstract
Despite prophylaxis with immunosuppressive agents or a variety of other approaches, many patients suffer from acute graft-versus-host disease after allogeneic hematopoietic cell transplantation. Although consensus has emerged supporting the use of high-dose methylprednisolone or prednisone for initial treatment of acute GVHD, practices differ among centers with respect to the initial glucocorticoid dose, the use of additional immunosuppressive agents, and the approach to withdrawal of treatment after initial improvement. Despite many studies, practices vary considerably with respect to the selection of agents for treatment of glucocorticoid-resistant or refractory GVHD. Investigators and clinicians have recognized the lack of progress and lamented the absence of an accepted standard of care for secondary treatment of acute GVHD. The American Society of Blood and Marrow Transplantation has developed recommendations for treatment of acute GVHD to be considered by care providers, based on a comprehensive and critical review of published reports. Since the literature provides little basis for a definitive guideline, this review also provides a framework for the interpretation of previous studies and the design of future studies.
Keywords: acute graft-versus-host disease, hematopoietic cell transplantation, treatment
INTRODUCTION
Despite prophylactic treatment with immunosuppressive agents, 20% to 80% of recipients develop acute graft-versus-host disease (GVHD) after allogeneic hematopoietic cell transplantation (HCT). The incidence and severity of acute GVHD depend on a variety of risk factors (reviewed in ref 1). Acute GVHD occurs more frequently and is more severe after HCT from HLA-non-identical or unrelated donors as compared to HLA-matched sibling donors.
The severity of acute GVHD should be graded according to the Keystone Consensus 1994 criteria [2] or according to CIBMTR criteria [3] (see on-line appendix for summary). Whenever possible, the clinical diagnosis of acute GVHD should be confirmed by biopsy of an affected end organ, and other complications affecting the skin, liver and gastrointestinal tract should be ruled out by appropriate testing. Decisions to begin systemic treatment depend not only on the severity of GVHD manifestations but also on their rate of progression. Rapidly progressive GVHD manifestations and any proven intestinal or liver involvement require prompt treatment. Cases characterized by indolent progression of rash without intestinal or liver involvement require more careful consideration of the benefits and risks of systemic immunosuppressive treatment. Survival correlates directly with the response to initial therapy. Second-line treatment is characterized by high failure rates, significant toxicities, and poor survival.
This review is intended to serve 3 goals: 1) provide an introductory guide to systemic treatment of acute GVHD, 2) establish a framework for evaluating previously published results, and 3) offer benchmarks for complete response (CR) and complete plus partial response (CR/PR) rates and survival rates that could be used in the design of future clinical trials.
Treatment suggestions in this review must be implemented in a medically reasonable way that accounts for the specific situation of the individual patient. Since the United States Food and Drug Administration has not approved any products for treatment of acute GVHD, all applications suggested in this review are acknowledged as “off-label” uses administered according to the discretion and judgment of physicians responsible for the care of individual patients. Applications are suggested only for marketed products with systemic activity. Numerous reports describing results of treatment for acute GVHD have been published in the medical literature. Details from selected individual studies that inform the recommendations are discussed in this review. Agents used for topical or non-systemic treatment will not be discussed in this review. The literature reviewed in this report does not support the use of agents other than prednisone or methylprednisolone for first-line treatment of acute GVHD or the use of any specific agent for second-line treatment of acute GVHD. In the absence of evidence to support any specific recommendation, this review can offer only general considerations for therapy.
METHODS
We searched the Medline (PubMed) database using a broad search strategy to identify studies evaluating treatment of acute GVHD with reports published between 1990 and 2011. The primary search was conducted using the terms “Graft-versus-host disease” and “Treatment” excluding ‘”Review.” Relevant references in the publications identified were also reviewed. Both retrospective and prospective studies were included, but studies with cohorts containing fewer than 10 patients, case reports and studies of agents that are not commercially available were excluded from consideration.
The literature search identified 13 reports summarizing results of initial systemic treatment for acute GVHD, including 2 studies comparing treatment with prednisone at different doses, 5 studies comparing prednisone with other agents versus prednisone alone, 3 single arm studies summarizing the results with the use of agents added to prednisone, 1 study summarizing results with sirolimus alone, and 2 large studies summarizing results with prednisone alone. The literature search identified 67 reports summarizing results of secondary systemic treatment for acute GVHD, but many of these reports had numerous deficiencies. In order to make recommendations based on reports with fewer deficiencies, we used a rating system that had been previously applied to reports of treatment for chronic GVHD [4]. The same method was applied to studies of treatment for acute GVHD [5]. The rating system assessed published reports according to the following 10 indicators: 1) adequately defined eligibility criteria; 2) documented minimization of bias in the selection of patients; 3) a consistent treatment regimen; 4) objective criteria for assessment of response in organs affected by GVHD; 5) unambiguous criteria for assessment of overall response; 6) assessment of response at a specified time after enrollment; 7) an accounting for effects of concomitant treatment; 8) identification of a well-established control benchmark; 9) a formal statistical hypothesis and consideration of statistical power; 10) display of overall survival, ideally with at least 6 months of follow-up. Two individuals independently evaluated reports identified in the literature search according to whether each criterion was met or not. Differences in scores were reconciled by joint review to arrive at a consensus. Results of the review suggested a bimodal distribution in the overall scores, with one peak including 38 reports that met between 0 and 4 of the indicators and another peak including 29 reports that met between 5 and 8 of the indicators. The 29 studies that met at least 5 criteria were included in the current review.
For both initial and secondary treatment, reports were reviewed to extract information regarding the CR rate, the CR/PR rate, and the 6-month Kaplan-Meier estimate of overall survival. These results were plotted against the number of patients enrolled in each study. In addition, aggregated CR and CR/PR rates for initial treatment with prednisone were derived from results of all studies, and the aggregated 6-month survival estimate after treatment with prednisone was likewise derived from the weighted average of the estimates from all reports. Aggregated results after secondary systemic treatment were derived by using the same methods. In order to determine whether the result with a given endpoint in any individual study differed statistically from the overall aggregated result, we used the binomial distribution to determine the 95% confidence limits with any number of patients and with the aggregated result as the probability of success. Individual studies with results above the upper boundary of the 95% confidence interval or below the lower boundary of the 95% confidence interval are statistical outliers, as shown in the figures. These studies were reviewed further in order to elucidate causes that could explain the results.
FIRST-LINE SYSTEMIC THERAPY
Treatment with methylprednisolone at 2 mg/kg/day or prednisone at 2.0 to 2.5 mg/kg/day has long been accepted as a standard first-line systemic therapy for acute GVHD. An exception is acute GVHD of the upper GI tract, a distinct clinical entity of anorexia, nausea, vomiting and dyspepsia that is more responsive to lower-dose systemic corticosteroids and topical steroid therapy [6]. A reasonable initial approach to treatment of acute GVHD of the upper GI tract is methylprednisolone or prednisone at 1 mg/kg/day. Table 1 summarizes results of previous studies addressing the dose of steroids to be used for initial treatment of acute GVHD and studies testing the effects of combined systemic agents for first-line therapy.
Table 1.
Summary of Studies Evaluating Systemic Agents for Initial Therapy of Acute GVHD*
| Reference | Agent | Phase | No. of patients | Response Assessment | CR Proportion | CR or PR Proportion | 6-month Survival |
|---|---|---|---|---|---|---|---|
| Comparative studies | |||||||
| [7] | High-dose Pred | 3 | 48 | 0.74 | |||
| Pred | 47 | 0.63 | |||||
| [8] | Low-dose Pred | Retro | 347 | 0.77 | |||
| Pred | 386 | 0.69 | |||||
| [10] | Basiliximab Pred | 3 | 35 | Day 20 | 0.54 | 0.63 | 0.78 |
| Pred | 34 | Day 20 | 0.44 | 0.71 | 0.66 | ||
| [12] | Horse ATG Pred | 3 | 50 | Day 42 | 0.27‡ | 0.48 | |
| Pred | 46 | Day 42 | 0.55 | 0.65 | |||
| [11]† | Daclizumab Pred | 3 | 53 | Day 42 | 0.43 | 0.51 | 0.53‡ |
| Pred | 49 | Day 42 | 0.49 | 0.53 | 0.76 | ||
| [13]† | Etanercept Pred | 2 | 61 | Day 28 | 0.69‡ | 0.69 | |
| Pred | Retro | 99 | Day 28 | 0.33 | 0.55 | ||
| [14]† | Infliximab Pred | 3 | 29 | Day 28 | 0.55 | 0.52 | |
| Pred | 28 | Day 28 | 0.54 | 0.54 | |||
| Single arm studies | |||||||
| [17] | MMF Pred | Pilot | 17 | 0.65 | 0.80 | ||
| [18]† | Etanercept Pred | 2 | 46 | Day 28 | 0.26 | 0.48 | 0.56 |
| [18]† | MMF Pred | 2 | 45 | Day 28 | 0.60 | 0.78 | 0.71 |
| [18]† | Denileukin Pred | 2 | 47 | Day 28 | 0.53 | 0.60 | 0.58 |
| [18]† | Pentostatin Pred | 2 | 42 | Day 28 | 0.38 | 0.62 | 0.56 |
| [32] | Sirolimus | Pilot | 10 | Best | 0.50 | ||
| Results with prednisone | |||||||
| [15] | Pred | 3 | 114 | Day 28 | 0.25 | 0.59 | 0.73 |
| [16] | Pred | Retro | 864 | Day 28 | 0.53 | 0.65 | 0.65 |
Non-steroid treatment results that fall outside the 95% confidence interval for the aggregated overall average of all studies are shown in bold. See Figures 1, 2 and 3.
Rationale for planned sample size and corresponding power estimates are reported.
statistically significant difference compared to controls, as reported by the study authors
Initial dose of glucocorticoids
Two studies have evaluated outcomes according to the initial dose of glucocorticoids (Table 1). One was a prospective study comparing 6-methylprednisolone at 10 mg/kg/day for 5 days with subsequent tapering versus standard therapy with 6-methylprednisolone at 2 mg/kg/day (equivalent to prednisone at 2.5 mg/kg/day) [7]. The primary endpoint was response to treatment such that patients could comply with a taper schedule that prescribed a 50% reduction in steroid dose every 5 days. By this definition, 13 of 47 (28%) of the patients in the high-dose arm responded, compared to 14 of 46 (30%) patients in the standard-dose arm. Rates of progression to grade III – IV GVHD and overall survival were similar between the two arms. The other was a retrospective study comparing low-dose glucocorticoid therapy at a 1.0 mg/kg prednisone-equivalent dose versus standard glucocorticoid therapy at a 2 mg/kg/day prednisone-equivalent dose [8]. The cumulative glucocorticoid dose across time was reduced by 48% in the low-dose arm but risks of overall mortality, relapse, non-relapse mortality, chronic GVHD and secondary therapy were similar in the two groups. The number of patients with grade III – IV GVHD was too small for definitive conclusions.
Summary conclusions for first-line systemic treatment of acute GVHD
Taken together, these two studies have shown no advantage of initial treatment with prednisone-equivalent steroid doses higher than 2.5 mg/kg/day and, at least in patients with grade II GVHD, no disadvantage of lower-dose initial treatment at 1.0 mg/kg/day. Experience with lower-dose steroids in patients with grade III – IV GVHD is limited. The use of lower-dose steroids has been evaluated in only a single retrospective study. A prospective randomized study addressing this question is in progress (NCT00929695).
Taper of steroid doses after initial response
Only a single study has attempted to define the appropriate glucocorticoid taper rate after treatment for acute GVHD [9]. In this study, 30 patients with response after 14 days of treatment with prednisone at 60 mg/m2 were randomized to either a “short” or “long” taper of the prednisone dose. The 14 patients in the short taper arm were scheduled to receive a total prednisone dose of 2275 mg/m2 over 86 days, and the 16 patients in the long taper arm were scheduled to receive a total prednisone dose of 6300 mg/m2 over 147 days. The median time to resolution of GVHD was 30 days in the long taper arm and 42 days in the short taper arm (p = 0.01). The incidence rates of GVHD reactivation during the taper, chronic GVHD, and infectious and non-infectious glucocorticoid-related complications were similar in the 2 arms. Likewise, the numbers of hospital days during the first 6 months and survival rates at 6 months were similar in the 2 arms.
Summary conclusions for tapering steroid doses
The optimal rate for tapering steroid doses has not been defined. Appropriate behavior of physicians in adjusting the taper rate according to the resolution or persistence of GVHD manifestations might explain why a nearly 3-fold range of total steroid doses did not affect outcomes. Tapering of steroid doses should begin as soon as GVHD manifestations show major improvement. Inappropriately rapid taper rates carry a risk of GVHD exacerbation or recurrence, while inappropriately slow taper rates increase the risk of steroid-related complications., When GVHD manifestations are under good control, taper rates that initially decrease the dose of prednisone by 0.2 mg/kg/day every 3 to 5 days and the taper schedules provided in national, multicenter trials for acute GVHD such as BMT CTN 0302 or 0802 reflect current practice and are appropriate. Taper rates should be slowed after the prednisone dose has been decreased to less than 20 – 30 mg/day.
Combined systemic agents for first-line therapy
Five studies have evaluated a variety of agents added to prednisone compared to prednisone alone for initial therapy of acute GVHD (Table 1). The agents evaluated included antibodies against IL-2R, [10,11] horse anti-thymocyte globulin (ATG) [12], etanercept [13], and infliximab [14]. Table 1 summarizes the available CR rates, CR/PR rates and 6-month survival estimates for each of these studies. The results showed no advantage or disadvantage with respect to CR at day 28 or survival rates when infliximab was added to prednisone, although response rates at 1 week were inferior among patients treated with infliximab plus prednisone, as compared to those treated with prednisone alone. Survival results with the use of IL-2R-specific antibodies were mixed. One study was closed prematurely because of inferior survival among patients treated with the antibody [11], but inferior survival with a different IL-2R-specific antibody was not observed in the other study [10]. In one randomized trial, the use of horse ATG plus prednisone was associated with a statistically significant lower CR/PR rate at day 42, as compared to prednisone alone, when secondary therapy was considered as treatment failure [12]. In addition, the use of ATG was associated with a higher risk of infections. The use of etanercept in the study by Levine et al. [13] was associated with a statistically significant higher CR rate at day 28 compared to historical controls treated with prednisone alone.
Five studies have evaluated agents added to prednisone without a formal comparison to a control group (Table 1). In order to interpret these results, data from the control arms of 6 prospective studies [7,10–12,14,15] and 3 retrospective studies [8,13,16] were aggregated. Survival is the most robust of the 3 endpoints summarized in Table 1, since this endpoint is entirely objective and can therefore be assessed in a consistent manner across all studies, although results can be profoundly affected by the characteristics of patients in the study cohort. This endpoint is not entirely satisfactory, since patients who survive after secondary treatment are counted as success. CR can be objectively defined, but the time points for assessment of CR vary considerably among the reports for different studies. Since the proportion of patients with CR increases across time, these differences must be taken into account when results are evaluated. CR/PR is the least robust of the 3 endpoints, since results are affected not only by the specific time point of assessment but also by the criteria used to define PR. In many studies, PR was defined as any reduction of the overall GVHD grade. This definition, however, is not entirely satisfactory, because a trivial decrease in GVHD severity can result in a reduction of the overall GVHD grade.
The aggregated results of standard treatment with prednisone showed an overall CR rate of 48%, an overall CR/PR rate of 64% and a weighted 6-month survival estimate of 0.66. The overall CR and CR/PR rates were 36% and 59% for the 6 prospective studies, somewhat lower than the respective 51% and 65% CR and CR/PR rates for the 3 retrospective studies. On the other hand, the weighted averages of the 6-month survival estimates for the 6 prospective and retrospective studies were similar, 0.68 and 0.65, respectively. The lower response rates after standard treatment with prednisone in prospective studies as compared to retrospective studies could reflect more stringent criteria for response or possibly some selection bias toward enrollment of patients perceived to have GVHD that is less likely to respond to conventional steroid treatment.
By far the largest study analyzing conventional steroid treatment was reported by MacMillan et al. [16] Results of this study show a CR rate of 53% and a CR/PR rate of 65% at day 28, and a 6-month survival estimate of 0.65. Hence, this study can be used as a convenient reference point for the interpretation of results in the 5 single-arm studies of agents added to prednisone and in the experimental arms of the 5 comparative studies.
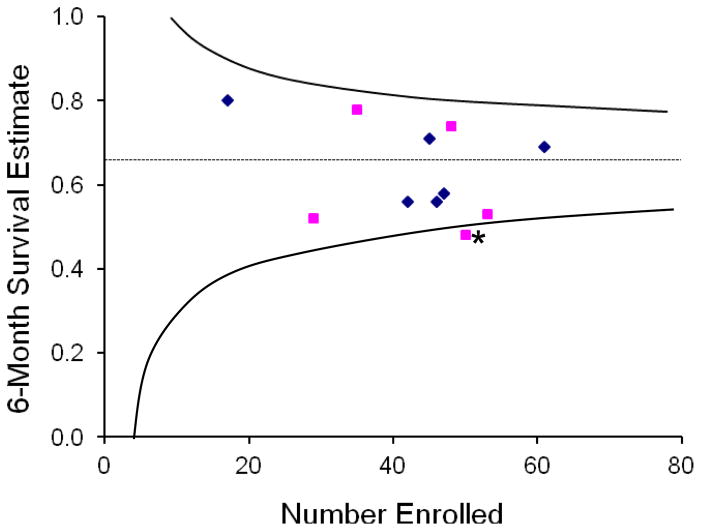
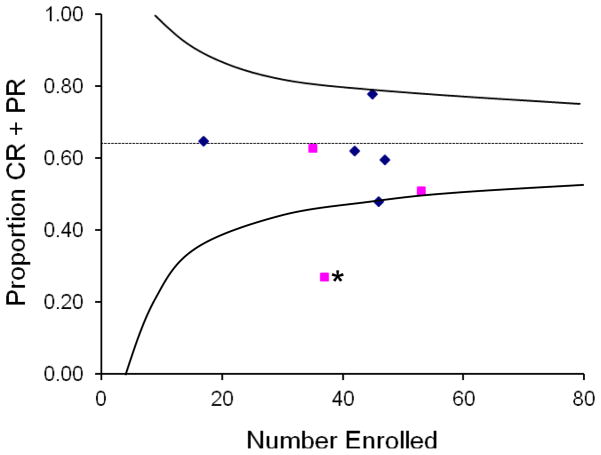
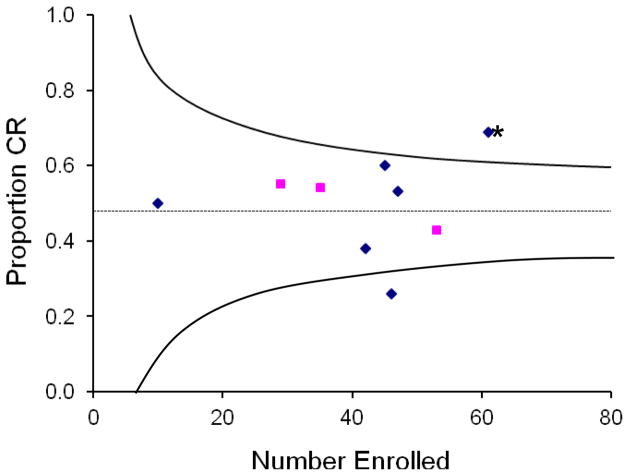
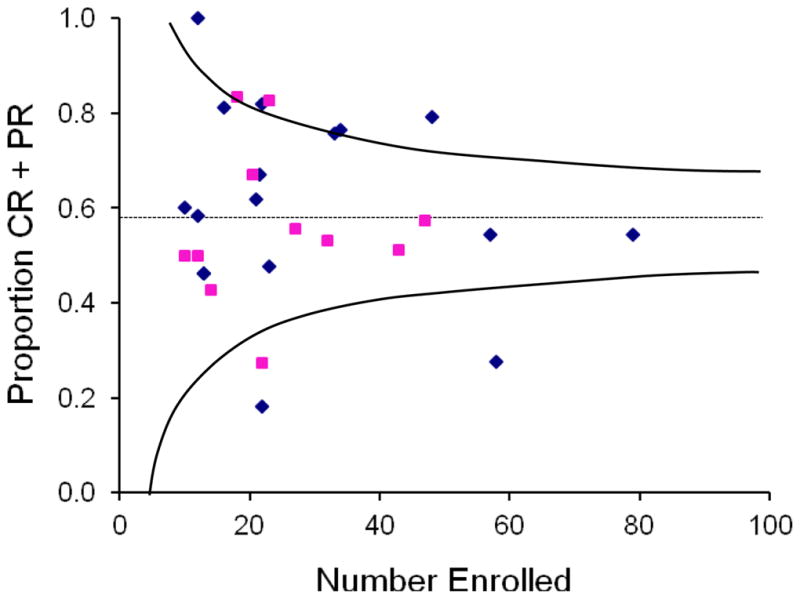
The agents evaluated in combination with prednisone in the 5 single-arm studies included mycophenolate mofetil (MMF) [17,18], etanercept [18], denileukin diftitox [18], and pentostatin [18]. As shown in Table 1 and Figures 1 – 3, results of these studies did not show outlier high results for any of the three endpoints. The 26% CR rate at day 28 in the evaluation of etanercept by Alousi et al. [18] was the only outlier low result. This result differs from the outlier high CR rate in the etanercept arm of the study by Levine et al. [12]. Reasons for the striking difference in CR rates between these 2 studies are not clear, since characteristics of the patients enrolled in the 2 studies were similar.
Figure 1.
Relationship between number of patients enrolled and the Kaplan-Meier estimate of survival at 6 months for each study of initial systemic therapy. The dotted line shows the weighted average 6-month survival estimate for all studies with standard-dose glucocorticoid treatment. Curved lines approximate the upper and lower boundaries of the 95% confidence interval for the weighted average at any given number of patients enrolled in a study. Squares indicate results of the experimental arms in phase 3 studies, and diamonds indicate results of prospective phase 2 studies and pilot studies. Points between the upper and lower boundaries identify studies with results that are statistically consistent with the weighted average. The point below the lower boundary identifies a study with outlier 6-month survival results that are statistically inconsistent with the weighted average. The asterisk indicates a phase III study that showed a statistically significant difference in survival between the 2 arms. The other phase III study with outlier low survival did not show a statistically significant difference between the two arms.
Figure 3.
Relationship between number of patients enrolled and the overall CR/PR rate for each study of initial systemic therapy. The dotted line shows the overall PR/CR rate for all studies with standard-dose glucocorticoid treatment. Curved lines approximate the 95% confidence limits for the overall PR/CR rate at any given number of patients enrolled. Squares indicate results of the experimental arm in phase 3 studies, and diamonds indicate results of prospective phase 2 studies and pilot studies. The asterisk indicates a phase III study that showed a statistically significant difference in survival between the 2 arms.
Figures 1 – 3 also show results for the experimental arms in the 5 comparative studies summarized in Table 1 [10–14]. These results confirm that the CR/PR rate in the horse ATG study was lower than expected [12]. The results also show that the 6-month survival estimate in this group was lower than expected, considering that median patient age of 23 years was somewhat lower than in the MacMillan study [16] and considering that only 6% of the patients had grade III – IV GVHD at the onset of treatment. These unfavorable results suggest that the regimen of horse ATG used in this study should not be added to prednisone for initial treatment of GVHD.
Results in Figure 1 also confirm that the CR rate in the etanercept study by Levine et al. [13] was higher than expected and that the CR rate in the etanercept arm of the study by Alousi et al.[18] was lower than expected. The patients treated with etanercept in these studies were older than those in the MacMillan study (median 51 and 50 years vs. 32 years), and a higher proportion had grade III – IV GVHD at the onset of treatment (33% and 26% vs. 15%) [16].
Summary conclusions for first-line therapy with combined systemic agents
The use of 6-methylprednisolone or prednisone alone as described above remains the standard of care for initial treatment of acute GVHD. The survival and response data from studies combining the use of other immunosuppressive agents together with glucocorticoid treatment do not support this approach as the standard of care. Combined treatment with multiple agents should be limited to patients who agree to participate in well-designed phase II or phase III studies. Currently, the design of these studies is hampered by the absence of prognostic factors that can accurately distinguish patients with higher-risk acute GVHD who might benefit from intensified initial treatment from those with standard-risk acute GVHD who are much less likely to benefit or who could be harmed by unnecessarily intensive treatment.
SECOND-LINE SYSTEMIC THERAPY
Criteria and indications for secondary systemic therapy of acute GVHD have not been systematically defined. Both the severity and duration of manifestations should be taken into account in deciding that initial glucocorticoid treatment has not adequately controlled GVHD. In general, decisions to initiate secondary therapy should be made sooner for patients with more severe GVHD. For example, secondary therapy may be indicated after 3 days with progressive manifestations of GVHD, after 1 week with persistent, unimproving grade III GVHD or after 2 weeks with persistent, unimproving grade II GVHD. Secondary systemic therapy may be indicated earlier in patients who cannot tolerate high-dose glucocorticoid treatment.
Very few prospective comparative studies have been carried out to assess the efficacy and safety of second-line therapy for acute GVHD. Hence, clinicians must rely on reports of retrospective studies and single-arm phase II studies to evaluate the merits of any given treatment. Comparison of results between these studies is complicated by the lack of standardized endpoints and the small numbers of patients included in most reports.
Table 2 summarizes results of 29 studies evaluating products that are commercially available for secondary therapy of acute GVHD. The review was limited to published studies that enrolled at least 10 patients and met at least 5 criteria, as described above. The table summarizes the total number of patients included in each study, the proportion of all patients who had a CR, the proportion of patients who had a complete or partial response, and the Kaplan-Meier estimate of survival at 6 months after starting secondary therapy.
Table 2.
Summary of Studies Evaluating Agents for Second-line Therapy of Acute GVHD*
| Ref. | Agent | Phase | No. of patients | Response Assessment | CR Proportion | CR or PR Proportion | 6-month Survival |
|---|---|---|---|---|---|---|---|
| [33] | Methotrexate | Retro | 12 | Day 28† | 0.42 | 0.58 | 0.58 |
| [34] | MMF | Retro | 13 | Best | 0.15 | 0.46 | 0.66 |
| [35] | MMF | Retro | 10 | Best | 0 | 0.60 | 0.77 |
| [30] | MMF | Retro | 48 | Best | 0.31 | 0.79 | 0.47 |
| [36] | MMF | Retro | 27 | Best | 0.26 | 0.52 | |
| [20] | ECP | Retro | 33 | Best† | 0.55 | 0.76 | 0.76 |
| [21] | ECP | Retro | 23 | Best† | 0.48 | 0.48 | 0.57 |
| [37] | Basiliximab | 2 | 23 | Day 7† | 0.17 | 0.83 | 0.55 |
| [38] | Daclizumab | 2 | 43 | Day 43 | 0.37 | 0.51 | |
| [39] | Daclizumab | 2 | 12 | Day 28† | 0.08 | 0.50 | 0.33 |
| [23] | Daclizumab | Retro | 57 | Day 43 | 0.33 | 0.54 | 0.28 |
| [40] | Inolimomab | 2 | 14 | Best† | 0.14 | 0.43 | 0.36 |
| [41] | Denileukin diftitox | 1 | 32 | Best | 0.38 | 0.53 | |
| [42] | Denileukin diftitox | 2 | 22 | Best | 0.18 | 0.27 | |
| [25] | Alemtuzumab | 2 | 18 | Day 28† | 0.33 | 0.83 | 0.71 |
| [24] | Alemtuzumab | 2 | 10 | Best† | 0.20 | 0.50 | 0 |
| [26] | Alemtuzumab | Retro | 18 | Day 56† | 0.28 | 0.62 | 0.61 |
| [31] | Horse ATG | Retro | 22 | Day 28 | 0.18 | ||
| [22] | Horse ATG | Retro | 58 | Day 21† | 0.07 | 0.28 | 0.17 |
| [19] | Horse ATG | Retro | 79 | Day 28 | 0.20 | 0.54 | 0.44 |
| [43] | Horse ATG | 2/3 | 47 | Best† | 0.32 | 0.57 | 0.45 |
| [44] | Horse ATG | 3 | 27 | Best† | 0.33 | 0.56 | 0.55 |
| [45] | Etanercept | Retro | 13 | Day 56 | 0.38 | 0.46 | 0.77 |
| [27] | Infliximab | Retro | 21 | Day 7† | 0.62 | 0.67 | 0.52 |
| [28] | Horse ATG + Etanercept | Retro | 16 | Best† | 0.69 | 0.81 | 0.56 |
| [46] | Dacliz+Etanercept | 2 | 21 | Best† | 0.38 | 0.67 | 0.57 |
| [47] | Dacliz+Infliximab | Retro | 22 | Day 42† | 0.45 | 0.82 | 0.86 |
| [29] | Dacliz/Inflix/Horse ATG | Retro | 12 | Best† | 1.00 | 1.00 | 0.73 |
| [48] | Sirolimus | Retro | 34 | Best | 0.44 | 0.76 | 0.48 |
Treatment results that fall outside the 95% confidence interval for the aggregated overall average of all studies are shown in bold. See Figures 4, 5 and 6.
The report did not indicate whether absence of further systemic treatment was a criterion for response. In all other reports, patients who had further systemic treatment were classified as not having a complete or partial response.
Analysis of 6-month survival
The weighted average 6-month survival estimate across the 25 studies that reported this endpoint was 0.49 (Figure 4). Sixteen studies had higher reported survival estimates, and 9 had lower reported survival estimates. The overall distribution of 6-month survival rates was similar for prospective and retrospective studies. The largest study was reported by MacMillan et al. [19] This study tested horse ATG and included 79 patients. The 6-month survival estimate for this study was 0.44, close to the weighted mean for all studies. Hence, the horse ATG study by MacMillan et al. [19] can be used as a convenient reference point for the interpretation of results in other studies.
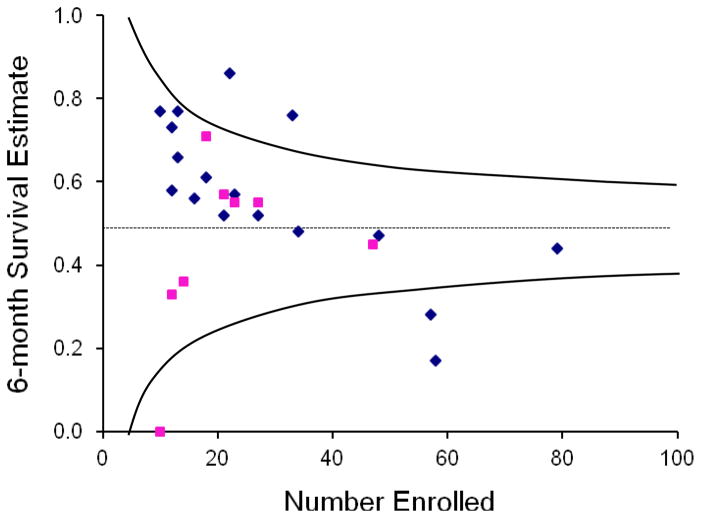
Figure 4.
Relationship between number of patients enrolled and the Kaplan-Meier estimate of survival at 6 months for each study of second-line therapy. The dotted line shows the weighted average 6-month survival estimate for all studies. Curved lines approximate the 95% confidence limits for the weighted average at any given number of patients enrolled. Squares indicate prospective studies, and diamonds indicate retrospective studies.
As shown in Figure 4, 5 studies had outlier 6-month survival results. In one of the two studies with outlier high survival, patients were treated with both daclizumab and infliximab and had a median age of 5.6 years [19]. In the other study with outlier high survival, patients were treated with extracorporeal photopheresis (ECP) and had a median age of 9.6 years [20]. In contrast, the median age of patients in the horse ATG study was 27 years [19]. These outlier results could reflect age differences between patient cohorts. Hence, it cannot be concluded that results with ECP or the combination of daclizumab and infliximab are likely to be superior to those with horse ATG. The conclusion that ECP does not yield superior 6-month survival is supported by the more typical results of one other study that evaluated ECP [21].
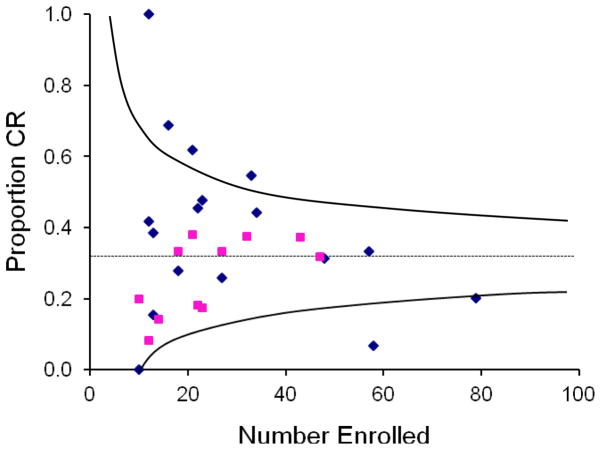
Figure 5.
Relationship between number of patients enrolled and the overall CR rate for each study of second-line therapy. The dotted line shows the overall CR rate for all studies. Curved lines approximate the 95% confidence limits for the overall CR rate at any given number of patients enrolled. Squares indicate prospective studies, and diamonds indicate retrospective studies.
In one of the 3 studies with outlier low survival, the patients were treated with horse ATG [22]. Patients in this study had a median age of 36 years. At the beginning of secondary therapy, 54% had grade IV GVHD, and 52% had liver involvement, compared to 5% with grade IV GVHD and 11% with liver involvement in the study by MacMillan et al. [19] The outlier results could reflect these differences in patient characteristics. Hence, it cannot be concluded that the poor survival was related specifically to the use of horse ATG. In another study with outlier low survival, the patients were treated with daclizumab [23]. The median age of patients in this study was 28 years, similar to the MacMillan study [19], but 26% of the patients had grade IV GVHD, and 32% had liver involvement, again suggesting that the inferior results could reflect differences in patient characteristics as opposed to differences in the efficacy of treatment. In the third study with outlier low survival, the patients were treated with alemtuzumab [24]. At the beginning of secondary therapy, all of the patients had grade III or IV GVHD, compared to 43% in the study by MacMillan et al. [19], and 50% had liver involvement, again suggesting that the inferior results reflected differences in patient characteristics as opposed to differences in the efficacy of treatment. Likewise, the conclusion that alemtuzumab does not yield inferior 6-month survival is supported by the much more favorable results of two other studies that evaluated alemtuzumab [25,26].
Summary conclusion for second-line therapy, based on survival results
The evaluation of 6-month survival estimates does not support the choice of any specific agent for secondary therapy of acute GVHD. The results also provide no evidence that any specific agent should be avoided for secondary therapy of acute GVHD.
Analysis of CR rates
Sixteen of the 29 studies reported “best response,” whereas others reported responses at day 7 (N = 2), 21 (N = 1), 28 (N = 4), 42 or 43 (N = 3) or 56 (N = 2). Response rates are likely to be inflated to some extent when “best response” is used as opposed to response at any given time point, since not all responses are durable. Seventeen of the reports did not indicate whether absence of further systemic treatment was a criterion for response, although it seems logical to assume that follow-up ended at the onset of subsequent treatment in studies that used “best response” as the endpoint.
The overall CR rate for the aggregated 28 studies that reported this endpoint was 32% (Figure 5). Twelve studies had higher CR rates, 11 had lower response rates, and the remaining 5 had results that were very close to the overall CR rate. The overall distribution of CR rates was lower among prospective studies was lower than among retrospective studies, suggesting that the distinction between CR and PR was more rigorously applied in prospective studies. For this reason, caution should be exercised in the interpretation of CR rates in retrospective studies. Results of the study by Perales et al. [23] evaluating daclizumab was the largest of these 5 studies and can therefore be used a convenient reference point for the interpretation of results in other studies.
As shown in Figure 5, 5 retrospective studies had outlier CR rates. One of the 4 studies with outlier high response rates was also the ECP study with outlier high survival [20]. The median age of patients in this study was 9.6 years, compared to 29 years in the daclizumab study [23]. The ECP study used “best response” as the outcome criteria, whereas the daclizumab study defined response at day 43 and specified that patients who had further systemic treatment were classified as not having a CR. Thus, the younger age of patients and the less stringent definition of CR could account for the outlier high CR rate in the ECP study [20]. This conclusion is supported by the more typical CR rate reported in the other study that evaluated ECP [21].
A second study with an outlier high CR rate evaluated infliximab [27]. The median age of patients in this study was 47 years, considerably higher than in the daclizumab study, but only 19% had grade III – IV GVHD at the onset of secondary treatment, compared to 51% in the daclizumab study [23]. The infliximab study evaluated response at day 7, but the report indicates that 3 of the 13 patients subsequently required additional treatment. From this information, it appears that 10 of the 21 (48%) patients had a response at day 43. Thus, it is likely that the lower severity of GVHD at the onset of treatment and the less stringent response definition account for the outlier high response rate in the infliximab study.
A third study with an outlier high CR rate evaluated horse antithymocyte globulin plus etanercept with or without mycophenolate mofetil [28]. The median age of patients in this study was 46 years, considerably higher than in the daclizumab study, and 81% had grade III – IV GVHD at the onset of treatment, which was also considerably higher than in the daclizumab study [23]. On the other hand, the horse ATG plus etanercept study [28] used the less stringent “best response” definition as the outcome criterion. Other reasons that might account for the higher CR rate after treatment with horse ATG and etanercept are not obvious when the two reports are compared. Despite the older age of patients and the higher severity of GVHD at the onset of treatment, patients treated with horse ATG and etanercept had better survival at 6 months than those treated with daclizumab. Taken together, these results suggest that the combination of horse ATG and etanercept might yield a higher than expected CR rate, but uncertainty remains because of the less stringent definition of CR used in this study and because of the small size of the study cohort. The interpretation of results in this study is also clouded by the inconsistent use of MMF in the treatment regimen.
A fourth study with an outlier high CR rate evaluated various combinations of daclizumab, infliximab and horse antithymocyte globulin [29]. The median age of patients in this study was 44 years, considerably higher than in the daclizumab study, and all had grade III – IV GVHD at the onset of treatment, which was also considerably higher than in the daclizumab study [23]. Although the less stringent “best response” definition was used as the outcome criterion in this study, complete responses were durable in 10 of the 12 patients. The problem with this study is that the 12 patients were treated with 4 different regimens. Five patients were treated with daclizumab alone, 2 were treated with daclizumab plus ATG, 4 were treated with daclizumab plus infliximab, and 1 was treated first with daclizumab and then with the combination of daclizumab plus infliximab. Although both the CR and 6-month survival rates were high, the lack of a consistent treatment regimen completely negates the value and impact of this study.
The one study with an outlier low CR rate evaluated horse ATG also had an outlier low 6-month survival rate [22]. At the beginning of secondary treatment, 93% of the patients in this study had grade III – IV GVHD, considerably higher than in the daclizumab study, and 52% had liver involvement, compared to 32% in the daclizumab study [23]. Response was assessed at day 21 in the horse ATG study, much earlier than the day 43 time point used in the daclizumab study. Given the differences in patient characteristics and time points of assessment, it cannot be concluded that the low CR rate was specifically related to the use of horse ATG.
Summary conclusion for second-line therapy, based on CR rates
With one possible exception, the evaluation of CR rates does not support the choice of any specific agent for secondary therapy of acute GVHD. The results also provide no evidence that any specific agent should be avoided for secondary therapy of acute GVHD. Although results with the combination of horse ATG and etanercept were encouraging, no other study has evaluated this combination of agents for secondary treatment of acute GVHD. For this reason, the available evidence is not sufficient to endorse this regimen as a recommendation or as the standard of care.
Analysis of CR/PR rates
Caution should be exercised in the interpretation of CR/PR rates. As discussed above, a trivial decrease in GVHD severity can produce a decrease in GVHD grade. Studies that use a reduction in GVHD grade to measure PR could inflate the proportion of patients who experience true benefit. In addition, studies that use “best response” would be expected to have higher response rates than studies that define response at a specific time point. Taken together, these considerations suggest that the bar of success with a best CR/PR criterion is so low that this measure cannot be used in isolation to identify promising agents for secondary treatment of GVHD.
The overall CR/PR rate for the aggregated 29 studies that reported this endpoint was 58% (Figure 6). Twelve studies had higher CR/PR rates, 13 had lower response rates, and the remaining 3 had results that were very close to the overall CR/PR rate. The overall distribution of CR/PR rates was similar in prospective and retrospective studies. The CR/PR rate in the study by MacMillan et al. [19] was 54% and can therefore be used a convenient reference point for the interpretation of results in other studies.
Figure 6.
Relationship between number of patients enrolled and the CR/PR rate for each study of second-line therapy. The dotted line shows the overall PR/CR rate for all studies. Curved lines approximate the 95% confidence limits for the overall PR/CR rate at any given number of patients enrolled. Squares indicate prospective studies, and diamonds indicate retrospective studies.
As shown in Figure 6, 4 studies had outlier CR/PR rates. In 1 of the studies with an outlier high CR/PR rate, patients were treated with the combination of daclizumab, infliximab and horse anti-thymocyte globulin, as discussed above [29]. In the other study with an outlier high CR/PR rate, patients were treated with mycophenolate mofetil (MMF) [30], and 23% had grade III – IV GVHD, compared to 43% in the study by MacMillan et al. [19] The MMF study used best response as the criterion of success, whereas the study by MacMillan et al. [19] evaluated the response on day 28. Thus, it is likely that the lower severity of GVHD at the onset of treatment and the less stringent response definition account for the outlier CR/PR rate in the MMF study. The similar 6-month survival estimates in the two studies support the conclusion that results with MMF [30] were not superior to those with horse ATG in the study by MacMillan et al. [19]
In both studies with outlier low CR/PR rates, patients were treated with horse ATG. One of these was a study that also had an outlier low CR rate, as discussed above [22]. The other [31] was a predecessor of the study by MacMillan et al. [19] The difference in CR/PR rates could reflect the periods when the patients were treated. The study with an outlier low PR/CR rate enrolled patients between 1985 and 1990 [31], whereas the study by MacMillan et al. [19] enrolled patients between 1990 and 1998.
Summary conclusion for second-line therapy, based on overall response rates
Taken together, the evaluation of CR/PR rates does not support the choice of any specific agent for secondary therapy of acute GVHD. The results also provide no evidence that any specific agent should be avoided for secondary therapy of acute GVHD.
Recommendations regarding second-line therapy
Since comparative data demonstrating superior efficacy for any particular agent over others are not available, the choice of a second-line regimen should be guided by the effects of any previous treatment and by considerations of potential toxicity, interactions with other agents, including those used for prophylaxis, convenience, expense, the familiarity of the physician with the agent, the prior experience of the physician (Table 3). When agents that cause profound depression of T-cell function (i.e., anti-thymocyte globulin, alemtuzumab, daclizumab, pentostatin) are administered, strategies for intensified surveillance and prophylaxis for opportunistic infections must be implemented when possible. For example, cytomegalovirus (CMV)-seropositive patients require increased monitoring for CMV reactivation, and the threshold for starting treatment with ganciclovir or foscarnet should be low. Long-term prophylaxis with mold-active antifungal agents should be administered. Since profound T-cell suppression increases the risk of Epstein-Barr virus (EBV)-lymphoproliferative disorders, adenovirus and human herpes virus 6 infections, the viral loads should be monitored during administration of second-line treatment for acute GVHD until the number of T cells in the blood has begun to recover. Data are not available to indicate whether the agents used for treatment of GVHD or the intensity of immunosuppression might attenuate graft-versus-leukemia effects. Hence, the extent to which decisions regarding treatment should be influenced by concern about recurrent malignancy is not known.
Table 3.
Considerations for Use of Agents in Second-line Treatment of Acute GVHD*
| Glucocorticoids | |
| Mechanism of action | Broad anti-inflammatory and lymphocytoxic effects |
| Toxicity concerns | Hyperglycemia, hypertension, insomnia, labile mood, gastritis, osteopenia, avascular bone necrosis, myopathy, impaired wound healing, secondary adrenal insufficiency |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | High when doses > 2 mg/kg/day |
| Convenience | Easy to prescribe |
| Expense concerns | Inexpensive |
|
| |
| Mycophenolate Mofetil (CellCept®, Myfortic®) | |
| Mechanism of action | Non-competitive inhibitor of IMPDH, the rate limiting step for de novo purine synthesis on which lymphocytes depend |
| Toxicity concerns | Dose related cytopenia and gastrointestinal toxicity; consider risk: benefit carefully when treating gastrointestinal GVHD. Enteric-coated mycophenolic acid (Myfortic®) may be better tolerated. |
| Significant interactions | May compound cytopenia when used with other myelosuppressive drugs |
| Viral reactivation concerns | Moderately high, especially if used with high dose steroids; lower cumulative incidence of severe/life-threatening infections compared to pentostatin or denileukin diftitox in the randomized phase II BMT CTN 0302 study |
| Convenience | Smallest pill formulations are 250 mg (mycophenolate mofetil, MMF) or 180 mg (Myfortic®). IV formulation of MMF is available |
| Expense concerns | Moderately expensive |
|
| |
| Denileukin diftitox (Ontak®) | |
| Mechanism of action | Recombinant fusion molecule of human IL-2 and diphtheria toxin that binds to the IL-2R-α and triggers apoptosis in activated T cells |
| Toxicity concerns | Dose limiting elevation of hepatic transaminases |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | High; higher cumulative incidence of severe/life-threatening infections compared to MMF or etanercept in the randomized phase II BMT CTN 0302 study |
| Convenience | IV formulation only and complex schedule: 9 micrograms/kg on days 1, 3, 5, 15, 17, and 19 |
| Expense concerns | Very expensive |
|
| |
| Sirolimus (Rapamune®) | |
| Mechanism of action | Binds to FK-binding protein complex and blocks mTOR, ultimately causing cell cycle arrest in G1; T cells are the most sensitive. Other mechanisms include: blocking co-stimulation via CD28, prevention of dendritic cell antigen presentation and maturation, and impairment of B cell activation and immunoglobulin production |
| Toxicity concerns | The most clinically relevant toxicities include reversible cytopenia, hypertriglyceridemia, and nephrotoxicity (HUS/TMA) and neurotoxicity (TTP) when combined with calcineurin inhibitors. Less common clinically relevant toxicities are transaminase elevations, edema, arthralgias, and non-infectious pneumonitis |
| Significant interactions | Sirolimus is a substrate for CYP3A4 and P-glycoprotein so that careful attention to concomitant therapies that interact with CYP3A or P-glycoprotein is necessary. Critical interaction mandates an initial 90% dose reduction in sirolimus when combining with voriconazole (75% reduction for posaconazole, 25% reduction for fluconazole). Sirolimus may increase the risk for rhabdomyolysis if used with HMG-CoA reductase inhibitors. In patients who develop HUS, calcineurin inhibitor therapy should be stopped and the dose of sirolimus should be adjusted to ensure that the trough level < 10 ng/mL. In patients with a serum total bilirubin >2 mg/dL, the sirolimus dose should be reduced by 30%. |
| Viral reactivation concerns | Moderate |
| Convenience | Oral formulations only: 0.5 mg, 1 mg and 2 mg tablets as well as a 1 mg/mL oral solution. Target levels of 3–12 ng/mL but <10 ng/mL when combined with calcineurin inhibitor. Consider terminal half-life of 57–62 hours when adjusting dose and checking levels |
| Expense concerns | Moderately expensive |
|
| |
| Infliximab (Remicade®) | |
| Mechanism of action | Chimeric murine/human monoclonal antibody that binds with high affinity to soluble and membrane-bound TNFα, resulting in clearance of both circulating TNFα and T cells. |
| Toxicity concerns | Generally well tolerated. Anaphylaxis is uncommon, but epinephrine should be available at beside. |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | Very high in secondary therapy; weekly PCR monitoring for EBV, adenovirus and CMV PCR for at least 6 months after last dose of Thymoglobulin or until absolute lymphocyte count >300 per microliter. No apparent increase in infections compared to steroids alone in single center phase III study of primary therapy versus steroids alone. |
| Convenience | IV formulation only; dosed at 10 mg/kg/week for at least 4 doses |
| Expense concerns | Very expensive |
|
| |
| Etanercept (Enbrel®) | |
| Mechanism of action | Soluble dimeric fusion protein consisting of the extracellular ligand-binding portion of the human TNFR linked to the Fc portion of human IgG133It competes for TNF-α binding and renders it inactive |
| Toxicity concerns | Subcutaneous injections are generally well tolerated |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | High; but lower overall cumulative incidence of severe/life-threatening infections compared to pentostatin or denileukin diftitox in the randomized phase II BMT CTN 0302 study |
| Convenience | Subcutaneous route only given twice weekly for 8 weeks at a dose of 0.4 mg/kg per dose (maximum dose, 25 mg); IV formulation only and complex schedule: Days 1, 4, 8, 15 and 22 |
| Expense concerns | Very expensive |
|
| |
| Pentostatin (Nipent®) | |
| Mechanism of action | Nucleoside analog that potently inhibits adenosine deaminase. Broad activities in GVHD include marked reduction of CD4 and CD8 T cells, significant B-cell depletion and lowering of IgG levels |
| Toxicity concerns | Myelosuppression; advisable to reduce dose by 50% if ANC <1000 per μL and discontinue therapy until recovery if ANC < 500 μL. Reversible elevation of liver function test results may occur. Dose reduction to 0.75 mg/m2 is recommended if creatinine clearance reduced to between 30 mL/min and 50 mL/min and discontinued if < 30 mL/min/1.73 m2. Stop or withhold therapy for neurotoxicity. |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | Very high; higher overall cumulative incidence of severe/life-threatening infections compared to MMF or etanercept in the randomized phase II BMT CTN 0302 study. Weekly PCR monitoring for EBV, adenovirus and CMV PCR for at least 6 months after last dose of Thymoglobulin or until absolute lymphocyte count >300 per microliter |
| Convenience | IV formulation only and complex schedule: 1.5 mg/m2 on days 1 to 3 and 15 to 17 |
| Expense concerns | Very expensive |
|
| |
| Horse antithymocyte globulin (ATGAM®) | |
| Mechanism of action | Antilymphocytic, primarily monomeric IgG, from hyperimmune serum of horses immunized with human thymus lymphocytes. It also contains low concentrations of antibodies against other formed elements of the blood. In rhesus and cynomolgus monkeys, horse ATG reduces lymphocytes in thymus-dependent areas of spleen and lymph nodes but ordinarily does not cause severe lymphopenia. |
| Toxicity concerns | Intradermal skin testing (0.1 mL of 1:1000) is advised before the first infusion to detect for any systemic (anaphylaxis) reaction that precludes further administration. Anaphylaxis is uncommon but epinephrine should be available at the bedside. Post marketing reports show fever 51% and chills 16% (due to release of endogenous leukocyte pyrogens), thrombocytopenia 30%, leukopenia 14%, and rash 27%. Five percent to 10% of patients experience serum sickness (lower if premedicated with steroids), dyspnea/apnea, arthralgia, chest, back, or flank pain; diarrhea and nausea and/or vomiting |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | Very high. Weekly PCR monitoring for EBV, adenovirus and CMV PCR for at least 6 months after last dose of Thymoglobulin or until absolute lymphocyte count >300 per microliter |
| Convenience | Intense clinical and vital sign monitoring required; IV infusion only. Regimens vary for GVHD: 15 mg/kg every other day × 6 doses to 15 mg per kg twice daily × 5 days. |
| Expense concerns | Expensive |
|
| |
| Rabbit antithymocyte globulin (Thymoglobulin®) | |
| Mechanism of action | Antilymphocytic globulin from hyperimmune serum of rabbits immunized with human thymus lymphocytes. It is thought to clear T-cells from the circulation, to down modulate inflammation, T-cell activation, homing, and cytotoxic activities. T-cell depletion is deeper and longer than with horse ATG and is usually observed within one day from starting therapy. |
| Toxicity concerns | Skin testing is not considered necessary but must monitor closely for anaphylaxis or cytokine release syndrome, the latter being more common particularly if first infusion runs < 6 hours. Premedication includes methylprednisolone. Thrombocytopenia and opportunistic infections are common. |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | Very high. Weekly PCR monitoring for EBV, adenovirus and CMV PCR for at least 6 months after last dose of Thymoglobulin or until absolute lymphocyte count >300 per microliter |
| Convenience | Intense clinical and vital sign monitoring required; IV infusion only. Variable 4 to 7 dose course with complex schedule for GVHD. It is advisable to start with 0.5 mg/kg for the first infusion and increase to 1–1.5 mg/kg for subsequent doses (max. is 1.5 mg/kg in a given day); total cumulative dose is 6–7.5 mg/kg |
| Expense concerns | Expensive |
|
| |
| Alemtuzumab (Campath®) | |
| Mechanism of action | Humanized IgG1monoclonal antibody targeting the non-modulating CD52 antigen on normal and malignant T- and B-cells, NK cells, monocytes, macrophages and a subpopulation of granulocytes. Proposed mechanism of action is the antibody-dependent lysis of cells expressing CD52. A proportion of bone marrow cells, including some CD34+ cells, express variable levels of CD52. |
| Toxicity concerns | Serious and, in rare instances fatal, cytopenia and marrow hypoplasia. Autoimmune thrombocytopenia and hemolytic anemia have occurred. Higher incidence of pancytopenia if exceed single doses > 30 mg or cumulative doses > 90 mg per week which are not recommended and such doses are unnecessary to induce profound lymphopenia in GVHD. Most commonly reported infusion-related adverse events are rigors and fever (80%-90%), nausea and vomiting (30%-50%). Other frequently reported (10%-15%) infusion-related events include rash, fatigue, hypotension, urticaria, dyspnea, pruritus, headache, and diarrhea. Premedication, which includes steroids, helps to prevent infusion-related events. Prolonged CD4 lymphopenia means that prophylaxis against Pneumocystis jirovecii pneumonia and herpes virus infections is advised. |
| Significant interactions | Not usually clinically significant |
| Viral reactivation concerns | Very high. Weekly PCR monitoring for EBV, adenovirus and CMV PCR for at least 6 months after last dose of Thymoglobulin or until absolute lymphocyte count >300 per microliter. |
| Convenience | IV infusional therapy is given over 2 hours and should not be begin at doses > 3 mg. If tolerated, daily doses may increase to 10 mg but higher doses are not likely to be necessary for GVHD therapy. The schedule and number of doses for GVHD therapy is unclear. The overall average half-life (t1/2) is about 12 days |
| Expense concerns | Expensive |
|
| |
| Extracorporeal photopheresis (ECP) | |
| Mechanism of action | Direct apoptosis of leukocytes (especially lymphocytes) and reinfusion of these cells appears to generate tolerogenic responses by reported mechanisms that have included: interference with dendritic cell maturation, modulation of cytokine production, and expansion of regulatory T cells (Tregs) |
| Toxicity concerns | Limited and includes: blood loss from the extracorporeal circuit, hypocalcemia due to anticoagulant, mild cytopenia, catheter-associated bacteremia but overall infection risks do not appear to be increased beyond standard therapy |
| Significant interactions | None |
| Viral reactivation concerns | Not increased |
| Convenience | Inconvenient; requires travel to ECP centers for up to many months. Complex schedule typically 3 per week (Week 1), 2 per week (Weeks 2–12) and 2 per 4 weeks thereafter |
| Expense concerns | Very expensive |
Daclizumab has been withdrawn from the market for commercial reasons and is therefore not included in this table.
Abbreviations: ANC, absolute neutrophil count; BMT CTN, Blood and Marrow Transplant Clinical Trials Network; EBV, Epstein Barr Virus; HUS, hemolytic uremic syndrome; IV, intravenous; mTOR, mammalian target of rapamycin; TMA, thrombotic microangiopathy; TNF-α, tumor necrosis factor alpha; TNFR, tumor necrosis factor receptor; TTP, thrombotic thrombocytopenic purpura.
Enrollment in well-designed clinical trials should be encouraged, since no standard, effective second line therapy for steroid-refractory acute GVHD has been identified, and since no treatment has been definitively demonstrated to be superior to any others. When a clinical trial is not open for accrual, a variety of therapeutic options can be considered. Corticosteroid treatment should be continued after starting a second-line agent for treatment of steroid-refractory acute GVHD. Corticosteroid doses should be tapered as clinical manifestations improve, but earlier tapering should be considered in order to minimize the risk of opportunistic infection or other toxicity.
Design considerations for future treatment trials
Development of effective agents for second-line treatment of acute GVHD will require well-designed prospective phase II studies. As discussed elsewhere [5], the most frequent deficiencies in the designs of previous studies were the absence of well-established benchmarks of success, failure to formulate null and alternative statistical hypotheses, insufficient statistical power due to small cohort size, and the lack of consideration given to differences in patient characteristics or response definitions that might explain outlier results. Patient characteristics that should be taken into account include age, pretransplant disease risk, recipient HLA-mismatching or the use of an unrelated donor, intensity of the conditioning regimen, type of graft (marrow, mobilized blood cells, cord blood), and severity of GVHD and involved sites at the onset of treatment.
Many of these deficiencies could easily be remedied by improvements in study design, but problems will persist until the primary endpoint for GVHD treatment studies has been standardized. Several groups have proposed that CR + PR at day 28 without prior secondary treatment should be used as the primary outcome measure for studies of initial treatment for GVHD, since this endpoint showed closer correlation with subsequent survival than other more stringent endpoints such as CR or very good PR [16,49–50]. Whether any of these endpoints will be acceptable to regulatory authorities remains to be determined.
As suggested previously [51], survival for 6 months without resort to a different systemic treatment could serve as an excellent endpoint for acute GVHD treatment trials. Resort to a different systemic treatment implies that the original treatment did not provide the desired benefit. Survival for 6 months with uncontrolled GVHD would be unusual, and most deaths caused by infection related to excessive immunosuppression would be expected to occur within 6 months, while longer-term results could be confounded by events occurring after recurrent malignancy. With this approach, systemic treatment for chronic GVHD within 6 months after enrollment would have to be treated as a competing risk. Benchmarks for this outcome have not been established. Other endpoints such as disease-free survival, non-relapse mortality and overall survival do not include subsequent systemic treatment as events and are therefore less specific to outcomes related to the success of treatment for GVHD. These endpoints and other outcomes such as chronic GVHD and immunosuppressant-free survival should nonetheless be evaluated as secondary endpoints. The overall 6-month survival estimates and CR and CR/PR rates summarized above could potentially be used as benchmarks for future studies with one-sample statistical designs, and the studies identified as having representative results could be used to evaluate whether outlier results could be explained by differences in patient characteristics. At the same time, it should be recognized, however, that publication bias could have distorted the overall results, such that they are not actually representative of results for the much larger population of patients with results that have never been published. Retrospective reviews of results in large cohorts of patients from single centers or registries could help to determine whether the overall results summarized from the literature are truly representative or not.
Supplementary Material
Figure 2.
Relationship between number of patients enrolled and the overall CR rate for each study of initial systemic therapy. The dotted line shows the overall CR rate for all studies with standard-dose glucocorticoid treatment. Curved lines approximate the 95% confidence limits for the overall CR rate at any given number of patients enrolled. Squares indicate results of the experimental arm in phase 3 studies, and diamonds indicate results of prospective phase 2 studies and pilot studies. The asterisk indicates a phase II study that showed a statistically significant improvement in survival compared to historical controls at the same institution.
Acknowledgments
This report was approved by the ASBMT Board of Directors on February 3, 2012.
We thank Stuart Tenney for assistance in preparing the manuscript.
Funding for this work was provided in part by CA18029 (P.J.M.) from the Department of Health and Human Services.
Footnotes
The other authors declared no conflict of interest.
Financial disclosure: P.J.M. has received research support from Soligenix, Inc. and Roche Laboratories, administered through the Fred Hutchinson Cancer Research Center. P.J.S. has received honoraria from Millenium, Otsuka and Sanofi/Genzyme.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Flowers MED, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. 2011;117:3214–3219. doi: 10.1182/blood-2010-08-302109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–828. [PubMed] [Google Scholar]
- 3.Rowlings PA, Przepiorka D, Klein JP, et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol. 1997;97:855–864. doi: 10.1046/j.1365-2141.1997.1112925.x. [DOI] [PubMed] [Google Scholar]
- 4.Martin PJ, Inamoto Y, Carpenter PA, Lee SJ, Flowers MED. Treatment of chronic graft-versus-host disease: past, present and future. Korean Journal of Hematology. 2011;46:153–163. doi: 10.5045/kjh.2011.46.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin PJ, Inamoto Y, Lee SJ, Flowers MED, Carpenter PA. Secondary treatment of acute graft-versus-host disease: a critical review. Biol Blood Marrow Transplant. doi: 10.1016/j.bbmt.2012.04.006. Companion manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hockenbery DM, Cruickshank S, Rodell TC, et al. A randomized, placebo-controlled trial of oral beclomethasone dipropionate as a prednisone-sparing therapy for gastrointestinal graft-versus-host disease. Blood. 2007;109:4557–4563. doi: 10.1182/blood-2006-05-021139. [DOI] [PubMed] [Google Scholar]
- 7.van Lint MT, Uderzo C, Locasciulli A, et al. Early treatment of acute graft-versus-host disease with high- or low-dose 6-methylprednisolone: a multicenter randomized trial from the Italian Group for Bone Marrow Transplantation. Blood. 1998;92:2288–2293. [PubMed] [Google Scholar]
- 8.Mielcarek M, Storer BE, Boeckh M, et al. Initial therapy of acute graft-versus-host disease with low-dose prednisone does not compromise patient outcomes. Blood. 2009;113:2888–2894. doi: 10.1182/blood-2008-07-168401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hings IM, Filipovich AH, Miller WJ, et al. Prednisone therapy for acute graft-versus-host disease: short- versus long-term treatment. A prospective randomized trial. Transplantation. 1993;56:577–580. doi: 10.1097/00007890-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Cahn JY, Bordigoni P, Tiberghien P, et al. Treatment of acute graft-versus-host disease with methylprednisolone and cyclosporine with or without an anti-interleukin-2 receptor monoclonal antibody. A multicenter phase III study. Transplantation. 1995;60:939–942. [PubMed] [Google Scholar]
- 11.Lee SJ, Zahrieh D, Agura E, et al. Effect of up-front daclizumab when combined with steroids for the treatment of acute graft-versus-host disease: results of a randomized trial. Blood. 2004;104:1559–1564. doi: 10.1182/blood-2004-03-0854. [DOI] [PubMed] [Google Scholar]
- 12.Cragg L, Blazar BR, DeFor T, et al. A randomized trial comparing prednisone with antithymocyte globulin/prednisone as an initial systemic therapy for moderately severe acute graft-versus-host disease. Biol Blood Marrow Transplant. 2000;6:441–447. doi: 10.1016/s1083-8791(00)70036-x. [DOI] [PubMed] [Google Scholar]
- 13.Levine JE, Paczesny S, Mineishi S, et al. Etanercept plus methylprednisolone as initial therapy for acute graft-versus-host disease. Blood. 2008;111:2470–2475. doi: 10.1182/blood-2007-09-112987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Couriel DR, Saliba R, de Lima M, et al. A phase III study of infliximab and corticosteroids for the initial treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009;15:1555–1562. doi: 10.1016/j.bbmt.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin PJ, Nelson BJ, Appelbaum FR, et al. Evaluation of a CD5-specific immunotoxin for treatment of acute graft-versus-host disease after allogeneic marrow transplantation. Blood. 1996;88:824–830. [PubMed] [Google Scholar]
- 16.MacMillan ML, Defor TE, Weisdorf DJ. The best endpoint for acute GVHD treatment trials. Blood. 2010;115:5412–5417. doi: 10.1182/blood-2009-12-258442. [DOI] [PubMed] [Google Scholar]
- 17.Basara N, Blau WI, Romer E, et al. Mycophenolate mofetil for the treatment of acute and chronic GVHD in bone marrow transplant patients. Bone Marrow Transplant. 1998;22:61–65. doi: 10.1038/sj.bmt.1701281. [DOI] [PubMed] [Google Scholar]
- 18.Alousi AM, Weisdorf DJ, Logan BR, et al. Etanercept, mycophenolate, denileukin, or pentostatin plus corticosteroids for acute graft-versus-host disease: a randomized phase 2 trial from the Blood and Marrow Transplant Clinical Trials Network. Blood. 2009;114:511–517. doi: 10.1182/blood-2009-03-212290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacMillan ML, Weisdorf DJ, Davies SM, et al. Early antithymocyte globulin therapy improves survival in patients with steroid-resistant acute graft-versus-host disease. Biol Blood Marrow Transplant. 2002;8:40–46. doi: 10.1053/bbmt.2002.v8.pm11858189. [DOI] [PubMed] [Google Scholar]
- 20.Messina C, Locatelli F, Lanino E, et al. Extracorporeal photochemotherapy for paediatric patients with graft-versus-host disease after haematopoietic stem cell transplantation. Br J Haematol. 2003;122:118–127. doi: 10.1046/j.1365-2141.2003.04401.x. [DOI] [PubMed] [Google Scholar]
- 21.Perfetti P, Carlier P, Strada P, et al. Extracorporeal photopheresis for the treatment of steroid refractory acute GVHD. Bone Marrow Transplant. 2008;42:609–617. doi: 10.1038/bmt.2008.221. [DOI] [PubMed] [Google Scholar]
- 22.Khoury H, Kashyap A, Adkins DR, et al. Treatment of steroid-resistant acute graft-versus-host disease with anti-thymocyte globulin. Bone Marrow Transplant. 2001;27:1059–1064. doi: 10.1038/sj.bmt.1703032. [DOI] [PubMed] [Google Scholar]
- 23.Perales MA, Ishill N, Lomazow WA, et al. Long-term follow-up of patients treated with daclizumab for steroid-refractory acute graft-vs-host disease. Bone Marrow Transplant. 2007;40:481–486. doi: 10.1038/sj.bmt.1705762. [DOI] [PubMed] [Google Scholar]
- 24.Martinez C, Solano C, Ferra C, Sampol A, Valcarcel D, Perez-Simon JA. Alemtuzumab as treatment of steroid-refractory acute graft-versus-host disease: results of a phase II study. Biol Blood Marrow Transplant. 2009;15:639–642. doi: 10.1016/j.bbmt.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 25.Gomez-Almaguer D, Ruiz-Arguelles GJ, Carmen Tarin-Arzaga L, et al. Alemtuzumab for the treatment of steroid-refractory acute graft-versus-host disease. Biol Blood Marrow Transplant. 2008;14:10–15. doi: 10.1016/j.bbmt.2007.08.052. [DOI] [PubMed] [Google Scholar]
- 26.Schub N, Gunther A, Schrauder A, et al. Therapy of steroid-refractory acute GVHD with CD52 antibody alemtuzumab is effective. Bone Marrow Transplant. 2011;46:143–147. doi: 10.1038/bmt.2010.68. [DOI] [PubMed] [Google Scholar]
- 27.Couriel D, Saliba R, Hicks K, et al. Tumor necrosis factor-alpha blockade for the treatment of acute GVHD. Blood. 2004;104:649–654. doi: 10.1182/blood-2003-12-4241. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy GA, Butler J, Western R, Morton J, Durrant S, Hill GR. Combination antithymocyte globulin and soluble TNFalpha inhibitor (etanercept) +/− mycophenolate mofetil for treatment of steroid refractory acute graft-versus-host disease. Bone Marrow Transplant. 2006;37:1143–1147. doi: 10.1038/sj.bmt.1705380. [DOI] [PubMed] [Google Scholar]
- 29.Srinivasan R, Chakrabarti S, Walsh T, et al. Improved survival in steroid-refractory acute graft versus host disease after non-myeloablative allogeneic transplantation using a daclizumab-based strategy with comprehensive infection prophylaxis. Br J Haematol. 2004;124:777–786. doi: 10.1111/j.1365-2141.2004.04856.x. [DOI] [PubMed] [Google Scholar]
- 30.Furlong T, Martin P, Flowers MED, et al. Therapy with mycophenolate mofetil for refractory acute and chronic graft-versus-host disease. Bone Marrow Transplant. 2009;44:739–748. doi: 10.1038/bmt.2009.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roy J, McGlave PB, Filipovich AH, et al. Acute graft-versus-host disease following unrelated donor marrow transplantation: failure of conventional therapy. Bone Marrow Transplant. 1992;10:77–82. [PubMed] [Google Scholar]
- 32.Pidala J, Kim J, Anasetti C. Sirolimus as primary treatment of acute graft-versus-host disease following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:881–885. doi: 10.1016/j.bbmt.2009.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Lavallade H, Mohty M, Faucher C, Furst S, El Cheikh J, Blaise D. Low-dose methotrexate as salvage therapy for refractory graft-versus-host disease after reduced-intensity conditioning allogeneic stem cell transplantation. Haematologica. 2006;91:1438–1440. [PubMed] [Google Scholar]
- 34.Kim JG, Sohn SK, Kim DH, et al. Different efficacy of mycophenolate mofetil as salvage treatment for acute and chronic GVHD after allogeneic stem cell transplant. Eur J Haematol. 2004;73:56–61. doi: 10.1111/j.1600-0609.2004.00247.x. [DOI] [PubMed] [Google Scholar]
- 35.Krejci M, Doubek M, Buchler T, Brychtova Y, Vorlicek J, Mayer J. Mycophenolate mofetil for the treatment of acute and chronic steroid-refractory graft-versus-host disease. Ann Hematol. 2005;84:681–685. doi: 10.1007/s00277-005-1070-0. [DOI] [PubMed] [Google Scholar]
- 36.Pidala J, Kim J, Perkins J, et al. Mycophenolate mofetil for the management of steroid-refractory acute graft vs host disease. Bone Marrow Transplant. 2010;45:919–924. doi: 10.1038/bmt.2009.252. [DOI] [PubMed] [Google Scholar]
- 37.Schmidt-Hieber M, Fietz T, Knauf W, et al. Efficacy of the interleukin-2 receptor antagonist basiliximab in steroid-refractory acute graft-versus-host disease. Br J Haematol. 2005;130:568–574. doi: 10.1111/j.1365-2141.2005.05631.x. [DOI] [PubMed] [Google Scholar]
- 38.Przepiorka D, Kernan NA, Ippoliti C, et al. Daclizumab, a humanized anti-interleukin-2 receptor alpha chain antibody, for treatment of acute graft-versus-host disease. Blood. 2000;95:83–89. [PubMed] [Google Scholar]
- 39.Willenbacher W, Basara N, Blau IW, Fauser AA, Kiehl MG. Treatment of steroid refractory acute and chronic graft-versus-host disease with daclizumab. Br J Haematol. 2001;112:820–823. doi: 10.1046/j.1365-2141.2001.02582.x. [DOI] [PubMed] [Google Scholar]
- 40.Cuthbert RJ, Phillips GL, Barnett MJ, et al. Anti-interleukin-2 receptor monoclonal antibody (BT 563) in the treatment of severe acute GVHD refractory to systemic corticosteroid therapy. Bone Marrow Transplant. 1992;10:451–455. [PubMed] [Google Scholar]
- 41.Ho VT, Zahrieh D, Hochberg E, et al. Safety and efficacy of denileukin diftitox in patients with steroid-refractory acute graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Blood. 2004;104:1224–1226. doi: 10.1182/blood-2004-01-0028. [DOI] [PubMed] [Google Scholar]
- 42.Shaughnessy PJ, Bachier C, Grimley M, et al. Denileukin diftitox for the treatment of steroid-resistant acute graft-versus-host disease. Biol Blood Marrow Transplant. 2005;11:188–193. doi: 10.1016/j.bbmt.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 43.MacMillan ML, Couriel D, Weisdorf DJ, et al. A phase 2/3 multicenter randomized clinicl trial of ABX-CBL versus ATG as secondary therapy for steroid-resistant acute graft-versus-host disease. Blood. 2007;109:2657–2662. doi: 10.1182/blood-2006-08-013995. [DOI] [PubMed] [Google Scholar]
- 44.van Lint MT, Milone G, Leotta S, et al. Treatment of acute graft-versus-host disease with prednisolone: significant survival advantage for day +5 responders and no advantage for nonresponders receiving anti-thymocyte globulin. Blood. 2006;107:4177–4181. doi: 10.1182/blood-2005-12-4851. [DOI] [PubMed] [Google Scholar]
- 45.Busca A, Locatelli F, Marmont F, Ceretto C, Falda M. Recombinant human soluble tumor necrosis factor receptor fusion protein as treatment for steroid refractory graft-versus-host disease following allogeneic hematopoietic stem cell transplantation. Am J Hematol. 2007;82:45–52. doi: 10.1002/ajh.20752. [DOI] [PubMed] [Google Scholar]
- 46.Wolff D, Roessler V, Steiner B, et al. Treatment of steroid-resistant acute graft-versus-host disease with daclizumab and etanercept. Bone Marrow Transplant. 2005;35:1003–1010. doi: 10.1038/sj.bmt.1704929. [DOI] [PubMed] [Google Scholar]
- 47.Rao K, Rao A, Karlsson H, Jagani M, Veys P, Amrolia PJ. Improved survival and preserved antiviral responses after combination therapy with daclizumab and infliximab in steroid-refractory graft-versus-host disease. J Pediatr Hematol Oncol. 2009;31:456–461. doi: 10.1097/MPH.0b013e31819daf60. [DOI] [PubMed] [Google Scholar]
- 48.Hoda D, Pidala J, Salgado-Vila N, et al. Sirolimus for treatment of steroid-refractory acute graft-versus-host disease. Bone Marrow Transplant. 2010;45:1347–1351. doi: 10.1038/bmt.2009.343. [DOI] [PubMed] [Google Scholar]
- 49.Levine JE, Logan B, Wu J, et al. Graft-versus-host disease treatment: Predictors of survival. Biol Blood Marrow Transplant. 2010;16:1693–1699. doi: 10.1016/j.bbmt.2010.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saliba RM, Couriel DR, Giralt S, et al. Prognostic value of response after upfront therapy for acute GVHD. Bone Marrow Transplant. doi: 10.1038/bmt.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martin PJ. Study design and endpoints in graft-versus-host disease. Best Prac & Res Clin Hematol. 2008;21:357–372. doi: 10.1016/j.beha.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.