Abstract
Background & Aims
Endoscopic findings such as esophageal rings, strictures, narrow-caliber esophagus, linear furrows, white plaques, and pallor or decreased vasculature might indicate the presence of eosinophilic esophagitis (EoE). We aimed to determine the prevalence and diagnostic utility of endoscopic features of EoE.
Methods
We conducted a systematic review and meta-analysis. PubMed, EMBASE, and GI meeting abstracts were searched to identify studies that included ≥ 10 patients with EoE and reported endoscopic findings. Pooled prevalence, sensitivity, specificity, and predictive values were calculated using random- and mixed-effects models.
Results
The search yielded 100 articles and abstracts on 4678 patients with EoE and 2742 without (controls). In subjects with EoE, the overall pooled prevalence of esophageal rings was 44%, strictures 21%, narrow-caliber esophagus 9%, linear furrows 48%, white plaques 27%, and pallor/decreased vasculature 41%. Substantial heterogeneity existed among studies. Results from endoscopy examinations were normal in 17% of patients, but this number decreased to 7% when the analysis was limited to prospective studies (P<.05). Overall levels of sensitivity were modest, ranging from 15% to 48%, whereas levels of specificity were greater, ranging from 90% to 95%. Positive predictive values ranged from 51% to 73% and negative predictive values ranged from 74% to 84%.
Conclusions
There is heterogeneity among studies in the reported prevalence of endoscopic findings in patients with EoE, but in prospective studies, at least 1 abnormality was detected by endoscopy in 93% of patients. The operating characteristics of endoscopic findings alone are inadequate for diagnosis of EoE. Esophageal biopsies should be obtained from all patients with clinical features of EoE, regardless of the endoscopic appearance of the esophagus.
Keywords: esophagus, inflammation, immune response, detection
Introduction
Eosinophilic esophagitis (EoE) is a clinicopathological disease first described in 1978 that is characterized by esophageal dysfunction and marked esophageal eosinophilic infiltration.1, 2 Presenting symptoms differ among patient populations. Adults typically present with symptoms of dysphagia, food impactions, and heartburn.3, 4 Although children can also present with swallowing difficulties, they most commonly have non-specific symptoms such as abdominal pain, vomiting, and failure to thrive.5–7 EoE is a relatively new disease, so our understanding is limited; because patients often present with nonspecific symptoms, it can be a challenge to diagnose.8
Diagnostic guidelines for EoE were created by participants of the First International Gastrointestinal Eosinophil Research Symposium (FIGERS) in 2007, and updates to these guidelines were published in the spring of 2011.2, 9 These diagnostic guidelines include features of the clinical presentation and histologic findings characteristic of the disease, but there are currently no recommendations regarding the role of endoscopic findings in the diagnosis of EoE.2, 9
Endoscopic findings of EoE include esophageal rings, strictures, narrow-caliber esophagus, linear furrows, white plaques or exudates, and pallor or decreased vasculature.4, 10 Some studies have reported abnormal results from endoscopic examinations in as few as 33% of cases,11–13 but other studies have reported endoscopic findings in as many as 95% of patients.14, 15 Although some studies have reported the sensitivity, specificity, and predictive values of the presence of classic endoscopic findings of EoE,16–19 the operating characteristics of these endoscopic findings are poorly described. We aimed to determine the prevalence, operating characteristics, and diagnostic utility of individual endoscopic features of EoE by performing a systematic review and meta-analysis of the literature.
Methods
Search Strategy and Data Collection
Two authors (HPK, RBV) independently searched the MEDLINE-indexed literature using the PubMed search engine from the National Center for Biotechnology Information (www.pubmed.gov). All studies with a print or electronic publication date from January 1, 1950 through June 30, 2011 were eligible for inclusion. To identify all relevant articles, the following search terms were used: eosinophilic esophagitis, allergic esophagitis, corrugated esophagus, ringed esophagus, eosinophil AND gastrointestinal, eosin* AND esoph*. The search was repeated in the EMBASE search engine to ensure that all eligible papers were reviewed, and the bibliographies of identified articles were hand searched. We also searched the published proceedings from the annual national meetings of the American Gastroenterological Association (AGA) and the American College of Gastroenterology (ACG) from 2000 to 2011.
After the search was complete, both authors reviewed each abstract to determine eligibility for inclusion. If there was any discrepancy, the full article was reviewed. Exclusion criteria comprised nonhuman studies, basic science/nonclinical studies, letters to the editor, editorials, review and summary articles, case reports, non-English studies without available translations, studies with <10 patients diagnosed with EoE, and studies that did not report upper endoscopy (EGD) findings. If studies reported a composite endoscopic score, primary authors were contacted to request original data regarding specific findings. We included case series, cross-sectional and cohort studies, case-control studies, and clinical trials. All eligible studies were included in the prevalence analysis, while the analysis of operating characteristics was restricted to studies that had a non-EoE control group.
Pertinent data were extracted from each study and organized into evidence tables independently by 2 authors. Data collected included year of publication, study design, study population (adults versus children defined as <18 years of age), number of patients in the study diagnosed with EoE, numbers of control participants (without EoE) if applicable, patients’ sex and age, and all reported endoscopic findings. Endoscopic findings included: esophageal rings (which could be termed rings, felinization, trachealization, or corrugation), strictures (defined as a focal narrowing of the esophagus), narrow-caliber esophagus (defined as a diffusely narrowed esophagus without clear focal stricture), linear furrows (longitudinal grooves or crevices parallel to the length of the esophagus which could be termed linear furrows, linear fissures, or tram tracks), white plaques or exudates, pallor or decreased vasculature (defined as abnormal color, granularity, or congestion of the esophageal mucosa with loss of the normal vascular pattern), and erosive esophagitis (defined as erosions and erythema in the area of the distal esophagus and gastroesophageal junction). The number of normal endoscopies per study was also recorded. All extracted data was collected and reviewed by both authors, with discrepancies reviewed and reconciled by all of the authors.
Statistical analysis
All study findings were compiled in tabular form, and the prevalence, sensitivity, specificity, and positive and negative predictive values were calculated for each finding by study. Overall unweighted prevalence and operating characteristics were also calculated using the raw data.
Statistical analysis was performed using Stata software (version 12.0; StataCorp LP, College Station, TX). Meta-analysis was performed to determine pooled prevalence rates and 95% confidence intervals using a random-effects model and with I2 as the measure of heterogeneity. The I2statistic estimates the percentage of total variation across studies that is secondary to study heterogeneity. An I2 statistic of 0% indicates no observed heterogeneity, and that all variation can be attributed to chance, whereas larger values indicate increasing heterogeneity. I2 of 25%, 50% and 75% are considered to represent low, moderate, and high levels of heterogeneity, respectively.20 The pooled operating characteristics (sensitivity, specificity, predictive values, and corresponding 95% confidence intervals) were determined using a mixed-effects model. To assess for sources of heterogeneity, stratified analyses were performed by age (adults vs children), study design (retrospective vs prospective), publication date (before vs after publication of guidelines), and study size (NEoE<30, NEoE≥30). Stratification for publication was set at 2008, due to publication of the initial diagnostic guidelines for EoE in late 2007.
Results
Search Results
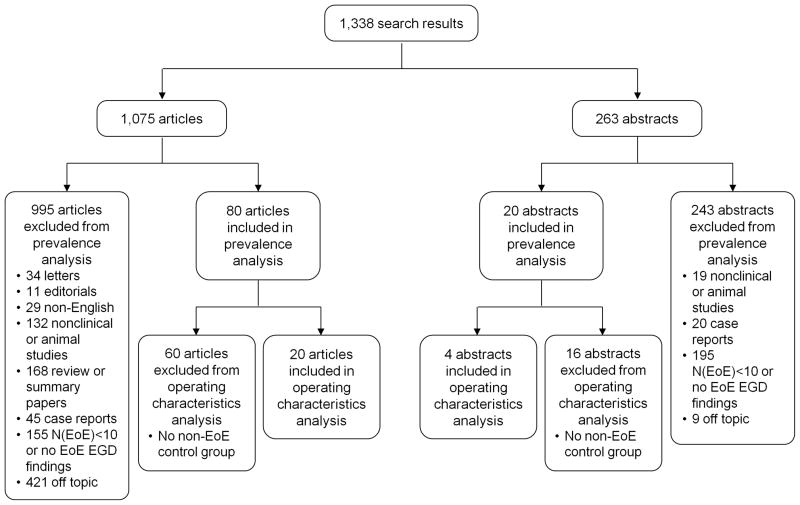
Of the 1338 publications initially identified, 80 original articles and 20 abstracts were included in the prevalence analysis, including more than 4600 patients with EoE (Figure 1). A total of 995 articles were excluded: 34 letters, 11 editorials, 29 papers that were not in the English language, 151 nonclinical or nonhuman studies, 168 review or summary articles, 65 case reports, 350 studies with less than 10 patients with EoE or no reported endoscopic findings, and 430 off-topic publications. A total of 20 original articles and 4 abstracts included patients with EoE and control groups (without EoE); these were included in the operating characteristics analysis. After all data was extracted from the studies, a 10% sample of extracted data was examined and agreement between authors was excellent (kappa=0.98).
Figure 1.
Flow diagram delineating the inclusion and exclusion of studies from the prevalence and operating characteristics analyses.
Prevalence
There was a broad overall range of findings reported among the 100 publications included in this analysis (Appendix 1). After meta-analysis, the overall pooled prevalence of esophageal rings was 44%, strictures 21%, narrow-caliber esophagus 9%, linear furrows 48%, white plaques or exudates 27%, pallor or decreased vasculature 41%, and erosive esophagitis 17% (Table 1). The endoscopic examination was normal in 17% of cases. After stratification by study design, prospective studies reported a greater prevalence of at least one abnormal endoscopic finding than retrospective studies (93% vs 80%; P<.05). Although not statistically significant, a greater prevalence of each of the individual endoscopic findings was reported in prospective, compared with retrospective, studies for rings, linear furrows, white plaques or exudates, and pallor or decreased vasculature (Table 1).
Table 1.
Prevalence of Endoscopic Findings by Study Characteristics
| Endoscopic Findings
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Rings | Stricture | Narrow Caliber Esophagus | Linear Furrows | White Plaques/Exudates | Pallor/Decreased Vasculature | Erosive Esophagitis | Normal | |
| Overall | ||||||||
| Prev % [95% CI]* | 44 [36, 51] | 21 [17, 25] | 9 [7, 12] | 48 [40, 56] | 27 [23, 30] | 41 [25, 57] | 17 [13, 22] | 17 [13, 22] |
| Nfinding/NEoE | 1828/4313 | 483/2597 | 126/1186 | 1588/3967 | 718/4071 | 264/740 | 257/1308 | 838/3296 |
| I2 (%) | 97.7 | 90.2 | 54.4 | 97.9 | 94.4 | 98.0 | 87.3 | 94.6 |
| # of studies | 85 | 46 | 27 | 77 | 74 | 21 | 37 | 66 |
| Adults | ||||||||
| Prev % [95% CI]* | 57 [49, 64] | 25 [19, 30] | 9 [6, 12] | 48 [37, 59] | 19 [16, 22] | 18 [0, 37] | 16 [11, 20] | 15 [9, 21] |
| Nfinding/NEoE | 1647/3149 | 439/2153 | 102/975 | 953/2555 | 331/2681 | 52/337 | 182/954 | 556/2159 |
| I2 (%) | 95.9 | 91.9 | 51.4 | 98.3 | 90.2 | 97.6 | 82.1 | 95.6 |
| # of studies | 60 | 35 | 20 | 47 | 44 | 9 | 28 | 41 |
| Children | ||||||||
| Prev % [95% CI]* | 11 [8, 15] | 8 [4, 12] | 11 [5, 18] | 46 [34, 58] | 36 [26, 45] | 58 [40, 76] | 15 [7, 23] | 21 [14, 29] |
| Nfinding/NEoE | 134/1015 | 35/348 | 24/211 | 540/1263 | 344/1241 | 212/403 | 65/343 | 281/1126 |
| I2 (%) | 64.2 | 58.2 | 62.6 | 96.6 | 94.3 | 95.7 | 85.3 | 92.2 |
| # of studies | 26 | 11 | 8 | 31 | 30 | 12 | 11 | 27 |
| Retrospective | ||||||||
| Prev % [95% CI]* | 39 [33, 46] | 22 [17, 27] | 9 [7, 12] | 44 [36, 51] | 22 [19, 26] | 36 [19, 53] | 18 [13, 24] | 20 [14, 25] |
| Nfinding/NEoE | 1572/3861 | 432/2333 | 114/1097 | 1322/3526 | 567/3727 | 183/607 | 213/1047 | 801/2918 |
| I2 (%) | 96.8 | 91.6 | 53.9 | 96.7 | 93.3 | 97.6 | 88.9 | 94.8 |
| # of studies | 66 | 36 | 22 | 59 | 58 | 16 | 27 | 51 |
| Prospective | ||||||||
| Prev % [95% CI]* | 59 [43, 75] | 17 [9, 25] | 11 [2, 21] | 61 [46, 77] | 44 [29, 59] | 57 [11, 102] | 15 [7, 22] | 7 [3, 10] |
| Nfinding/NEoE | 256/452 | 51/264 | 12/89 | 266/441 | 151/344 | 81/133 | 44/261 | 37/378 |
| I2 (%) | 96.6 | 77.5 | 63.7 | 97.2 | 92.1 | 98.9 | 78.0 | 63.7 |
| # of studies | 19 | 10 | 5 | 18 | 16 | 5 | 10 | 15 |
| Before 2008 | ||||||||
| Prev % [95% CI]* | 38 [27, 49] | 27 [20, 34] | 13 [9, 18] | 50 [37, 64] | 26 [18, 34] | 42 [19, 65] | 22 [14, 30] | 16 [10, 21] |
| Nfinding/NEoE | 427/1312 | 189/715 | 44/300 | 595/1349 | 284/1298 | 154/494 | 107/529 | 274/1367 |
| I2 (%) | 96.7 | 82.0 | 31.7 | 98.1 | 93.2 | 98.5 | 88.7 | 93.2 |
| # of studies | 31 | 20 | 11 | 28 | 26 | 11 | 17 | 31 |
| After 2008 | ||||||||
| Prev % [95% CI]* | 47 [37, 56] | 17 [12, 22] | 8 [5, 10] | 46 [37, 56] | 27 [23, 31] | 39 [14, 64] | 14 [9, 19] | 18 [12, 25] |
| Nfinding/NEoE | 1401/3001 | 294/1882 | 82/886 | 993/2618 | 434/2773 | 110/246 | 150/779 | 564/1929 |
| I2 (%) | 97.8 | 91.7 | 55.9 | 97.3 | 93.8 | 97.5 | 85.2 | 95.2 |
| # of studies | 54 | 26 | 16 | 49 | 48 | 10 | 20 | 35 |
| NEoE <30 | ||||||||
| Prev % [95% CI]* | 43 [32, 53] | 25 [15, 34] | 14 [9, 19] | 54 [44, 64] | 36 [27, 46] | 40 [17, 64] | 17 [10, 24] | 17 [10, 25] |
| Nfinding/NEoE | 344/816 | 90/380 | 53/314 | 377/715 | 237/665 | 87/210 | 61/376 | 106/602 |
| I2 (%) | 95.7 | 92.1 | 48.9 | 91.7 | 90.4 | 96.8 | 82.5 | 92.4 |
| # of studies | 46 | 21 | 18 | 40 | 39 | 12 | 21 | 36 |
| NEoE ≥30 | ||||||||
| Prev % [95% CI]* | 45 [34, 55] | 19 [15, 23] | 7 [4, 10] | 42 [30, 53] | 19 [16, 23] | 41 [18, 64] | 18 [12, 24] | 18 [12, 24] |
| Nfinding/NEoE | 1484/3497 | 393/2217 | 73/872 | 1211/3252 | 481/3406 | 128/355 | 196/932 | 732/2694 |
| I2 (%) | 98.5 | 88.5 | 58.4 | 98.8 | 94.4 | 98.7 | 90.8 | 96.0 |
| # of studies | 40 | 26 | 9 | 38 | 35 | 9 | 17 | 31 |
Pooled prevalence values and 95% CIs are the result of a random-effects meta-analysis.
There was also a difference in the prevalence of findings by age. Rings and strictures were more prevalent in adults (57% and 25%, respectively) than in children (11% and 8%; P<.05 for each). On the other hand, white plaques and pallor or decreased vasculature were more prevalent in children (36% and 58%) than in adults (19% and 18%; P<.05 for each). No differences according to publication date or study size were observed.
Operating Characteristics
Twenty original articles and 4 abstracts, representing more than 950 patients with EoE and 2700 controls, were included in the analysis to determine the operating characteristics of rings, strictures, linear furrows, white plaques or exudates, and pallor or decreased vasculature. Operating characteristics for each finding by study, as well as overall unweighted operating characteristics are described in Appendices 2 and 3.
For individual findings, overall pooled sensitivities were modest and ranged from 15% to 48%, whereas pooled specificities were greater and ranged from 90% to 95% (Table 2). Overall pooled positive predictive values (PPV) ranged from 51% to 73%, and pooled negative predictive values (NPV) ranged from 74% to 84%. Rings had overall sensitivity, specificity, PPV, and NPV of 48%, 91%, 64%, and 84%, respectively. The overall sensitivity, specificity, PPV, and NPV for strictures were 15%, 95%, 51%, and 76%, and for white plaques were 27%, 94%, 67%, and 74%, respectively. The operating characteristics were slightly higher for linear furrows with a sensitivity of 40%, specificity 95%, PPV 73%, and NPV 83%. For pallor/decreased vasculature, the sensitivity, specificity, PPV, and NPV were 43%, 90%, 65%, and 79%, respectively. In contrast to the low sensitivity of individual endoscopic findings, when examining the presence of at least 1 endoscopic finding, an abnormal endoscopy had a sensitivity of 87%, specificity of 47%, PPV of 42%, and NPV of 89%.
Table 2.
Overall Pooled Sensitivity, Specificity, and Predictive Values of Endoscopic Findings
| Endoscopic Findings
|
||||||
|---|---|---|---|---|---|---|
| Rings | Stricture | Linear Furrows | White Plaques/Exudates | Pallor/Decreased Vasculature | Abnormal endoscopy (≥1 finding) | |
| Sens % [95% CI] | 48 [32, 65] | 15 [10, 21] | 40 [31, 51] | 27 [17, 41] | 43 [20, 69] | 87 [80, 92] |
| Spec % [95% CI] | 91 [81, 96] | 95 [90, 97] | 95 [91, 97] | 94 [89, 97] | 90 [82, 95] | 47 [27, 67] |
| PPV % [95% CI] | 64 [48, 81] | 51 [46, 57] | 73 [64, 84] | 67 [57, 81] | 65 [42, 91] | 42 [35, 47] |
| NPV % [95% CI] | 84 [74, 89] | 76 [71, 78] | 83 [79, 85] | 74 [69, 77] | 79 [71, 84] | 89 [69, 109] |
| Prevalence of EoE %* | 25 | 26 | 25 | 31 | 30 | 31 |
| # of studies | 19 | 11 | 19 | 14 | 7 | 14 |
| I2 % [95% CI] | 99 [99, 100] | 96 [92, 99] | 98 [97, 99] | 97 [95, 99] | 97 [95, 99] | 98 [97, 99] |
Prevalence is equivalent to the pre-test probability of having EoE, and was calculated using a mixed-effects meta-analysis.
There were significant differences in the operating characteristics of these findings by patient population according to age. Rings had greater sensitivity in adults than in children (64% vs 17%; P<.05; Appendix 4), whereas pallor/decreased vasculature had greater sensitivity in children than in adults (57% vs. 14%; p<0.05). Predictive values also differed between these patient populations. Rings, strictures, white plaques/exudates, and pallor/decreased vasculature had greater PPVs in children (79%, 75%, 89%, 74%, respectively) than in adults (56%, 43%, 40%, 28%, respectively; P<.05 for all comparisons). In contrast, the NPVs for these findings were greater in adults (89%, 81%, 82%, 89%, respectively) than in children (64%, 54%, 63%, 74%, respectively; P<.05 for all comparisons).
Heterogeneity Between Studies
There was substantial heterogeneity in the overall prevalence of endoscopic findings with I2 values ranging from 54.4% to 98.0% (Table 1). After stratification of data, heterogeneity decreased in some categories, including esophageal rings, strictures, and narrow-caliber esophagus, but remained substantial with I2 values ranging from 31.7% to 98.9% (Table 1). Pooled prevalence of individual endoscopic findings significantly varied by patient age (as described above, rings and strictures were significantly more prevalent in adults than in children, and white plaques/exudates and pallor/decreased vasculature were significantly more prevalent in children than in adults), indicating that a proportion of the heterogeneity among studies could be attributed to the age of the study population. No significant difference in the prevalence of individual endoscopic findings was observed according to study design, publication date, or study size, and these factors did not explain additional heterogeneity.
Discussion
EoE is an emerging disease that has increased in incidence and prevalence over the past decade.12, 21–23 Because the clinical presentation is non-specific and there are significant variations in esophageal biopsy protocols and eosinophil counting methods, EoE can be a challenge to diagnose.24, 25 Although endoscopic features of EoE such as esophageal rings, linear furrows, and white plaques or exudates are often considered to be typical features of EoE, these are not always identified by endoscopists.26, 27 We conducted this systematic review and meta-analysis to determine the prevalence and operating characteristics of individual endoscopic features found in patients with EoE to assess their diagnostic utility.
This study revealed that although the prevalence of any 1 individual finding may be low, 83% of individuals reported in the literature to have EoE had at least 1 endoscopic feature of this disease. When the analysis was limited to prospective studies, which are not complicated by recall bias or errors inherent to medical record review, this number increased to 93%. The increased prevalence values calculated for prospective studies indicates that with careful assessment, endoscopic abnormalities are more likely to be found in patients with EoE, and that most patients with EoE have abnormal findings from upper endoscopy examinations. However, the sensitivity values of individual endoscopic findings were modest, and although the specificity values were higher, the predictive values were inadequate for diagnostic purposes.
The predictive values of diagnostic tests vary with disease prevalence. The prevalence of EoE depends on the population studied. For example, the prevalence of EoE has been estimated to be 0.4%–1.1% in the general population.28, 29 In patients who present for routine endoscopy for any indication, however, the prevalence of EoE increases to approximately 6.5%, and in those undergoing an EGD for dysphagia, the prevalence is 10%–15%.16, 26, 27
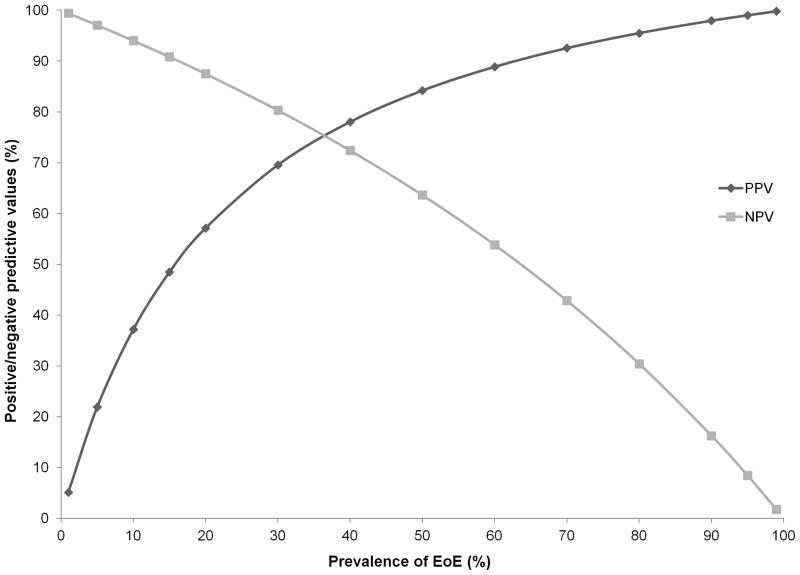
As the prevalence of EoE decreases, the PPV (defined as the probability of disease in those with a positive test result) decreases and the NPV (defined as the probability of no disease in those with a negative test result) increases. Figure 2 illustrates this point with data from the current study. If esophageal rings were used as a diagnostic tool (sensitivity 48%, specificity 91%), the positive and negative predictive values of esophageal rings in patients presenting for EGD with dysphagia (predicted probability of EoE 10%–15%) would be 37%–48% and 91%–94%, respectively. In the general population, the prevalence of EoE is much lower, and the PPV and NPV of esophageal rings would be 5% and 99%, respectively. Therefore, the presence or absence of esophageal rings would not change the pre-test probability significantly, bringing into question the utility of any individual endoscopic finding for the diagnosis of EoE or for making decisions about obtaining esophageal biopsies in the general population. However, although the sensitivity of any individual finding is low, the literature indicates that endoscopic detection of any one of the several associated abnormalities has some clinical utility.
Figure 2.
The effect of EoE prevalence on the positive and negative predictive values of esophageal rings for diagnosing EoE. The sensitivity and specificity of esophageal rings are held constant at 48% and 91%, respectively, (these are the values calculated with a random-effects meta-analysis in this study), the prevalence of EoE is varied on the x-axis, and the resulting PPV or NPV are noted on the y-axis.
The other major finding from this study was the substantial heterogeneity among endoscopic findings in reported in the literature for patients with EoE. This is not surprising given that the studies included in our analysis were conducted over more than 20 years, incorporated a variety of EoE case definitions, used different study designs, and investigated different populations in different settings. To address the issue of heterogeneity, we performed analyses stratifying studies by patient age (adult vs. pediatric), study type (retrospective vs. prospective), size, and year of publication (before/after first consensus guidelines). The results indicated that a proportion of the heterogeneity can be attributed to differences in the endoscopic presentation of EoE according to patient age. We observed differences in endoscopic findings between children and adults, with rings and strictures more frequently observed in adults, whereas white plaques and pallor/decreased vasculature were more frequently found in children. in endoscopic appearance of EoE with age could result from changes that occur in the esophageal mucosa as the disease progresses, with inflammatory processes occurring at earlier stages of the disease and fibrotic processes occurring later. There are limited data on disease progression to support this hypothesis,30–34 although a similar association has been shown from analysis of cross-sectional data.10 We also observed differences in the sensitivities and predictive values of individual endoscopic findings between children and adults. Certain endoscopic findings might therefore have more or less diagnostic utility, depending on the age of the patient. However, because of the heterogeneity and variability among studies, the role of age in the interpretation of endoscopic findings remains unclear
It is important to acknowledge several limitations of our study. Although our search strategy was broad, it is possible that some relevant studies were not identified or included. However, 2 databases were each searched independently by 2 investigators; additional sources were identified by reviewing bibliographies and including abstracts from major gastroenterology meetings. We also minimized possible misclassification of endoscopic findings during data extraction by having 2 investigators independently extract and then reconcile the data from each study; the level of agreement between the investigators was excellent. However, because there are not widely-accepted a priori definitions for the endoscopic findings of EoE, findings from each study could not be standardized beyond the judgment of the endoscopist(s) that performed each study. In addition, we were unable to comment on the role of findings in patients who could have had esophageal eosinophilia that responded to proton pump inhibitor (PPI) therapy. A broad range of studies were included in this meta-analysis, and although many of the patients had confirmed EoE, given that many of the studies were performed before consensus guidelines for the diagnosis of EoE were established, it is possible that some patients might have had PPI-responsive eosinophilia. These factors could all contribute to the substantial heterogeneity observed among studies.
In conclusion, in a systematic review and meta-analysis of endoscopic findings from patients with EoE, we found that there is a high pooled prevalence of at least 1 endoscopic finding in patients with EoE, though prevalence rates for individual findings varied and could be low. Although individual endoscopic findings had high levels of specificity, the low sensitivity and variable predictive values make them inadequate both for the diagnosis of EoE and for the decision of whether or not to obtain biopsies. There was also substantial heterogeneity in the prevalence of these findings in the medical literature; this was due, in part, to the ages of the populations studied and also probably due to variations in the definitions of EoE. A large prospective study that includes a clear atlas of endoscopic findings, to standardize nomenclature, would be required to clarify these issues.
Our findings indicate that although a high degree of suspicion for EoE must be maintained for patients that have endoscopic features of this disease, the presence or absence of endoscopic findings is insufficient to make a diagnosis. Esophageal biopsies should be obtained from all patients who present with symptoms of EoE, regardless of the endoscopic appearance of the esophagus.
Figure 3.
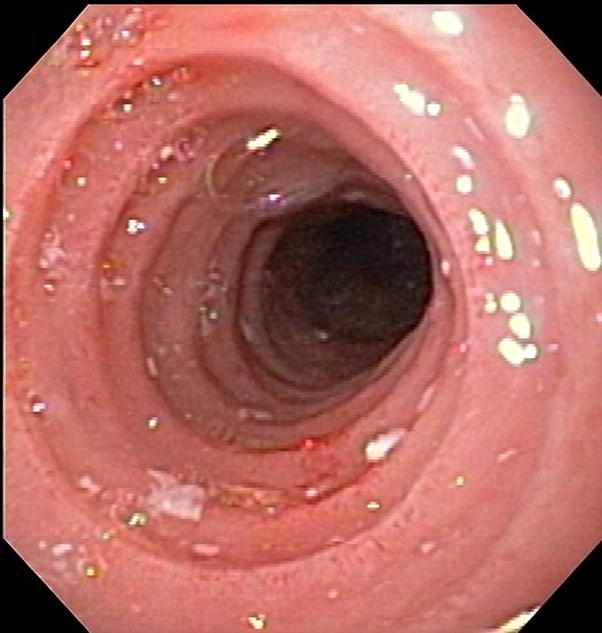
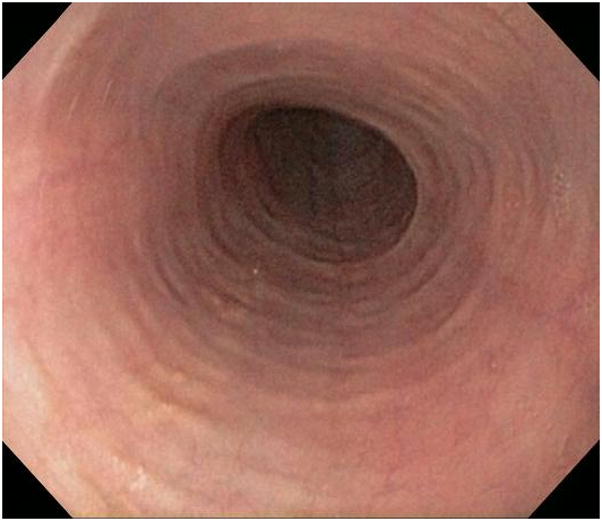

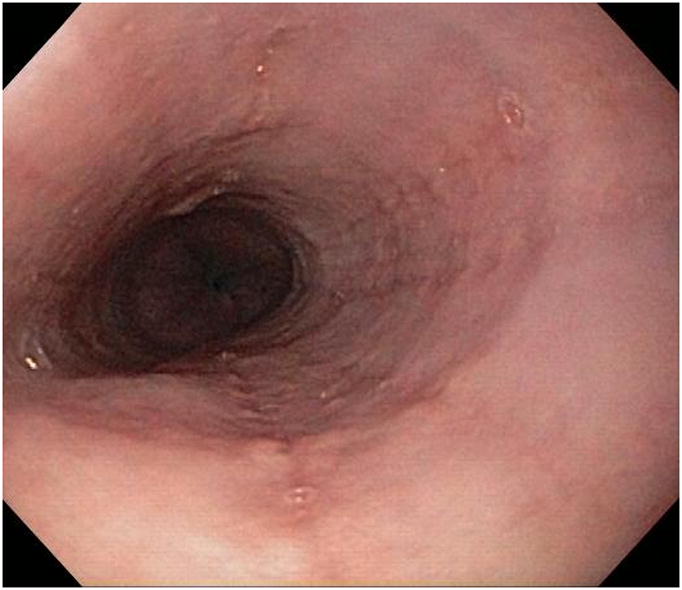
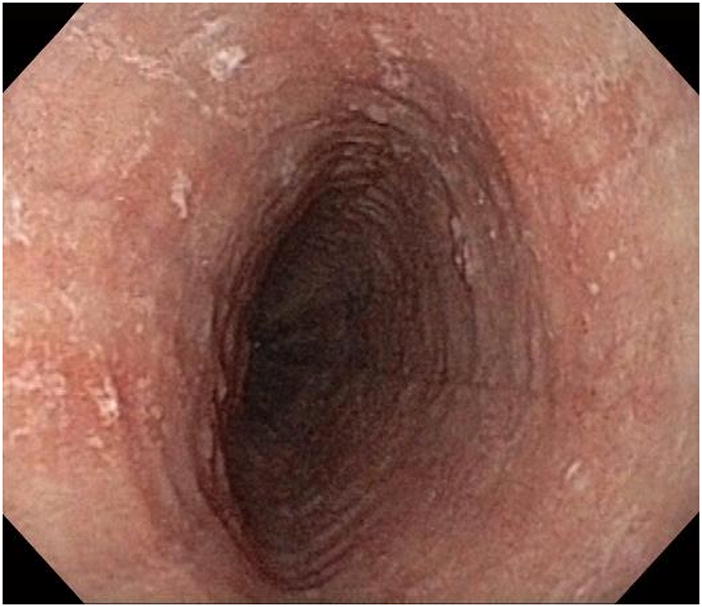
Typical endoscopic findings of EoE. (A) Prominent and fixed esophageal rings and narrow caliber esophagus. (B) Subtle rings. (C) Rings and linear furrows, as well as mucosal pallor and decreased vasculature. (D) Linear furrows, mucosal pallor, and decreased vasculature. (E) Linear furrows and white plaques or exudates, as well as mucosal pallor and decreased vasculature.
Acknowledgments
Grant support: This work was supported by a grant from the Doris Duke Charitable Foundation to the University of North Carolina-Chapel Hill (HPK) and NIH award number 1K23 DK090073-01 (ESD)
Abbreviations
- ACG
American College of Gastroenterology
- AGA
American Gastroenterological Association
- EGD
upper endoscopy, esophagogastroduodenoscopy
- EoE
eosinophilic esophagitis
- FIGERS
First International Gastrointestinal Eosinophil Research Symposium
Footnotes
Disclosures: None of the authors have disclosures pertinent to this paper
Author contributions:
- Kim: Acquisition of data; analysis and interpretation of data; drafting/revision of the manuscript; final approval
- Vance: Acquisition of data; critical revision of the manuscript; final approval
- Shaheen: Conception and design; critical revision of the manuscript; final approval
- Dellon: Study concept and design; analysis and interpretation of data; drafting/revision of the manuscript; final approval
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Landres RT, Kuster GG, Strum WB. Eosinophilic esophagitis in a patient with vigorous achalasia. Gastroenterology. 1978;74(6):1298–301. Epub 1978/06/01. [PubMed] [Google Scholar]
- 2.Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133(4):1342–63. doi: 10.1053/j.gastro.2007.08.017. Epub 2007/10/09. [DOI] [PubMed] [Google Scholar]
- 3.Ferre-Ybarz L, Nevot Falco S, Plaza-Martin AM. Eosinophilic oesophagitis: clinical manifestations and treatment options. The role of the allergologist. Allergologia et immunopathologia. 2008;36(6):358–65. doi: 10.1016/s0301-0546(08)75869-5. Epub 2009/01/20. [DOI] [PubMed] [Google Scholar]
- 4.Sgouros SN, Bergele C, Mantides A. Eosinophilic esophagitis in adults: a systematic review. European journal of gastroenterology & hepatology. 2006;18(2):211–7. doi: 10.1097/00042737-200602000-00015. Epub 2006/01/06. [DOI] [PubMed] [Google Scholar]
- 5.Liacouras CA. Clinical presentation and treatment of pediatric patients with eosinophilic esophagitis. Gastroenterology & hepatology. 2011;7(4):264–7. Epub 2011/08/23. [PMC free article] [PubMed] [Google Scholar]
- 6.Berthet S, Triolo V, Bourrier T, Descos B, De Smet S, Berard E, et al. [Eosinophilic esophagitis. Clinical presentation, allergology and treatment: a series of 22 children] [in French with English abstract] Archives de pediatrie : organe officiel de la Societe francaise de pediatrie. 2011;18(1):7–14. doi: 10.1016/j.arcped.2010.10.002. Epub 2010/11/30. L’oesophagite a eosinophiles. Presentation, bilan allergologique et traitement : a propos de 22 cas. [DOI] [PubMed] [Google Scholar]
- 7.Hasosah MY, Sukkar GA, Alsahafi AF, Thabit AO, Fakeeh ME, Al-Zahrani DM, et al. Eosinophilic esophagitis in Saudi children: symptoms, histology and endoscopy results. Saudi journal of gastroenterology : official journal of the Saudi Gastroenterology Association. 2011;17(2):119–23. doi: 10.4103/1319-3767.77242. Epub 2011/03/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doyle LA, Odze RD. Eosinophilic esophagitis without abundant eosinophils? The expanding spectrum of a disease that is difficult to define. Digestive diseases and sciences. 2011;56(7):1923–5. doi: 10.1007/s10620-011-1715-x. Epub 2011/05/03. [DOI] [PubMed] [Google Scholar]
- 9.Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. The Journal of allergy and clinical immunology. 2011;128(1):3–20. e6. doi: 10.1016/j.jaci.2011.02.040. quiz 1–2. Epub 2011/04/12. [DOI] [PubMed] [Google Scholar]
- 10.Dellon ES, Gibbs WB, Fritchie KJ, Rubinas TC, Wilson LA, Woosley JT, et al. Clinical, endoscopic, and histologic findings distinguish eosinophilic esophagitis from gastroesophageal reflux disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009;7(12):1305–13. doi: 10.1016/j.cgh.2009.08.030. quiz 261. Epub 2009/09/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ravi K, Talley NJ, Smyrk TC, Katzka DA, Kryzer L, Romero Y, et al. Low grade esophageal eosinophilia in adults: an unrecognized part of the spectrum of eosinophilic esophagitis? Digestive diseases and sciences. 2011;56(7):1981–6. doi: 10.1007/s10620-011-1594-1. Epub 2011/02/08. [DOI] [PubMed] [Google Scholar]
- 12.Prasad GA, Alexander JA, Schleck CD, Zinsmeister AR, Smyrk TC, Elias RM, et al. Epidemiology of eosinophilic esophagitis over three decades in Olmsted County, Minnesota. Clin Gastroenterol Hepatol. 2009;7(10):1055–61. doi: 10.1016/j.cgh.2009.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin de Carpi J, Gomez Chiari M, Castejon Ponce E, Masiques Mas ML, Vilar Escrigas P, Varea Calderon V. [Increasing diagnosis of eosinophilic esophagitis in Spain] [in Spanish with English abstract] An Pediatr (Barc) 2005;62(4):333–9. doi: 10.1157/13073246. Epub 2005/04/14. Aumento del diagnostico de esofagitis eosinofilica en nuestro medio. [DOI] [PubMed] [Google Scholar]
- 14.Pasha SF, DiBaise JK, Kim HJ, De Petris G, Crowell MD, Fleischer DE, et al. Patient characteristics, clinical, endoscopic, and histologic findings in adult eosinophilic esophagitis: a case series and systematic review of the medical literature. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus / ISDE. 2007;20(4):311–9. doi: 10.1111/j.1442-2050.2007.00721.x. Epub 2007/07/10. [DOI] [PubMed] [Google Scholar]
- 15.Lai AL, Girgis S, Liang Y, Carr S, Huynh HQ. Diagnostic criteria for eosinophilic esophagitis: a 5-year retrospective review in a pediatric population. Journal of pediatric gastroenterology and nutrition. 2009;49(1):63–70. doi: 10.1097/MPG.0b013e318184c917. Epub 2009/05/26. [DOI] [PubMed] [Google Scholar]
- 16.Gupta SK, Fitzgerald JF, Chong SK, Croffie JM, Collins MH. Vertical lines in distal esophageal mucosa (VLEM): a true endoscopic manifestation of esophagitis in children? Gastrointestinal endoscopy. 1997;45(6):485–9. doi: 10.1016/s0016-5107(97)70178-0. Epub 1997/06/01. [DOI] [PubMed] [Google Scholar]
- 17.Lim JR, Gupta SK, Croffie JM, Pfefferkorn MD, Molleston JP, Corkins MR, et al. White specks in the esophageal mucosa: An endoscopic manifestation of non-reflux eosinophilic esophagitis in children. Gastrointestinal endoscopy. 2004;59(7):835–8. doi: 10.1016/s0016-5107(04)00364-5. Epub 2004/06/03. [DOI] [PubMed] [Google Scholar]
- 18.Potter JW, Saeian K, Staff D, Massey BT, Komorowski RA, Shaker R, et al. Eosinophilic esophagitis in adults: an emerging problem with unique esophageal features. Gastrointestinal endoscopy. 2004;59(3):355–61. doi: 10.1016/s0016-5107(03)02713-5. Epub 2004/03/05. [DOI] [PubMed] [Google Scholar]
- 19.Veerappan GR, Perry JL, Duncan TJ, Baker TP, Maydonovitch C, Lake JM, et al. Prevalence of eosinophilic esophagitis in an adult population undergoing upper endoscopy: a prospective study. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009;7(4):420–6. 6 e1–2. doi: 10.1016/j.cgh.2008.10.009. Epub 2009/01/24. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in medicine. 2002;21(11):1539–58. doi: 10.1002/sim.1186. Epub 2002/07/12. [DOI] [PubMed] [Google Scholar]
- 21.Straumann A, Simon HU. Eosinophilic esophagitis: escalating epidemiology? The Journal of allergy and clinical immunology. 2005;115(2):418–9. doi: 10.1016/j.jaci.2004.11.006. Epub 2005/02/08. [DOI] [PubMed] [Google Scholar]
- 22.Kapel RC, Miller JK, Torres C, Aksoy S, Lash R, Katzka DA. Eosinophilic esophagitis: a prevalent disease in the United States that affects all age groups. Gastroenterology. 2008;134(5):1316–21. doi: 10.1053/j.gastro.2008.02.016. Epub 2008/05/13. [DOI] [PubMed] [Google Scholar]
- 23.Hruz P, Straumann A, Bussmann C, Heer P, Simon HU, Zwahlen M, et al. Escalating incidence of eosinophilic esophagitis: A 20-year prospective, population-based study in Olten County, Switzerland. The Journal of allergy and clinical immunology. 2011;128(6):1349–50. e5. doi: 10.1016/j.jaci.2011.09.013. Epub 2011/10/25. [DOI] [PubMed] [Google Scholar]
- 24.Dellon ES, Aderoju A, Woosley JT, Sandler RS, Shaheen NJ. Variability in diagnostic criteria for eosinophilic esophagitis: a systematic review. The American journal of gastroenterology. 2007;102(10):2300–13. doi: 10.1111/j.1572-0241.2007.01396.x. Epub 2007/07/10. [DOI] [PubMed] [Google Scholar]
- 25.Sperry SL, Shaheen NJ, Dellon ES. Toward uniformity in the diagnosis of eosinophilic esophagitis (EoE): the effect of guidelines on variability of diagnostic criteria for EoE. The American journal of gastroenterology. 2011;106(5):824–32. doi: 10.1038/ajg.2011.10. quiz 33. Epub 2011/02/10. [DOI] [PubMed] [Google Scholar]
- 26.Peery AF, Cao H, Dominik R, Shaheen NJ, Dellon ES. Variable reliability of endoscopic findings with white-light and narrow-band imaging for patients with suspected eosinophilic esophagitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2011;9(6):475–80. doi: 10.1016/j.cgh.2011.02.026. Epub 2011/03/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moy N, Heckman MG, Gonsalves N, Achem SR, Hirano I. Inter-Observer Agreement on Endoscopic Esophageal Findings in Eosinophilic Esophagitis (EoE) Gastroenterology. 2011;140(5, Supplement 1):S-236. [Google Scholar]
- 28.Almansa C, Devault KR, Achem SR. A comprehensive review of eosinophilic esophagitis in adults. Journal of clinical gastroenterology. 2011;45(8):658–64. doi: 10.1097/MCG.0b013e318211f95b. Epub 2011/08/13. [DOI] [PubMed] [Google Scholar]
- 29.Ronkainen J, Talley NJ, Aro P, Storskrubb T, Johansson SE, Lind T, et al. Prevalence of oesophageal eosinophils and eosinophilic oesophagitis in adults: the population-based Kalixanda study. Gut. 2007;56(5):615–20. doi: 10.1136/gut.2006.107714. Epub 2006/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spergel JM, Brown-Whitehorn TF, Beausoleil JL, Franciosi J, Shuker M, Verma R, et al. 14 years of eosinophilic esophagitis: clinical features and prognosis. Journal of pediatric gastroenterology and nutrition. 2009;48(1):30–6. doi: 10.1097/MPG.0b013e3181788282. Epub 2009/01/28. [DOI] [PubMed] [Google Scholar]
- 31.Assa’ad AH, Putnam PE, Collins MH, Akers RM, Jameson SC, Kirby CL, et al. Pediatric patients with eosinophilic esophagitis: an 8-year follow-up. The Journal of allergy and clinical immunology. 2007;119(3):731–8. doi: 10.1016/j.jaci.2006.10.044. Epub 2007/01/30. [DOI] [PubMed] [Google Scholar]
- 32.Teitelbaum JE. Natural history of primary eosinophilic esophagitis: a follow up of 30 adult patients for up to 11.5 years. Journal of pediatric gastroenterology and nutrition. 2004;38(3):358–9. doi: 10.1097/00005176-200403000-00024. Epub 2004/04/13. [DOI] [PubMed] [Google Scholar]
- 33.Straumann A, Spichtin HP, Grize L, Bucher KA, Beglinger C, Simon HU. Natural history of primary eosinophilic esophagitis: a follow-up of 30 adult patients for up to 11.5 years. Gastroenterology. 2003;125(6):1660–9. doi: 10.1053/j.gastro.2003.09.024. Epub 2004/01/16. [DOI] [PubMed] [Google Scholar]
- 34.Straumann A. The natural history and complications of eosinophilic esophagitis. Thoracic surgery clinics. 2011;21(4):575–87. doi: 10.1016/j.thorsurg.2011.09.004. Epub 2011/11/02. [DOI] [PubMed] [Google Scholar]
- 35.Rizo Pascual JM, De La Hoz Caballer B, Redondo Verge C, Terrados Cepeda S, Roy Arino G, Riesco Lopez JM, et al. Allergy assessment in children with eosinophilic esophagitis. J Investig Allergol Clin Immunol. 2011;21(1):59–65. Epub 2011/03/05. [PubMed] [Google Scholar]
- 36.Abe M, Mashiba T, Zeniya M, Yamamoto K, Onji M, Tsubouchi H. Present status of autoimmune hepatitis in Japan: a nationwide survey. Journal of gastroenterology. 2011;46(9):1136–41. doi: 10.1007/s00535-011-0421-y. Epub 2011/05/21. [DOI] [PubMed] [Google Scholar]
- 37.Jung KW, Gundersen N, Kopacova J, Arora AS, Romero Y, Katzka D, et al. Occurrence of and risk factors for complications after endoscopic dilation in eosinophilic esophagitis. Gastrointestinal endoscopy. 2011;73(1):15–21. doi: 10.1016/j.gie.2010.09.036. Epub 2010/11/12. [DOI] [PubMed] [Google Scholar]
- 38.Madanick RD, Shaheen NJ, Dellon ES. A novel balloon pull-through technique for esophageal dilation in eosinophilic esophagitis (with video) Gastrointestinal endoscopy. 2011;73(1):138–42. doi: 10.1016/j.gie.2010.09.034. Epub 2010/12/28. [DOI] [PubMed] [Google Scholar]
- 39.Abu-Sultaneh SM, Durst P, Maynard V, Elitsur Y. Fluticasone and food allergen elimination reverse sub-epithelial fibrosis in children with eosinophilic esophagitis. Digestive diseases and sciences. 2011;56(1):97–102. doi: 10.1007/s10620-010-1259-5. Epub 2010/05/12. [DOI] [PubMed] [Google Scholar]
- 40.Ricker J, McNear S, Cassidy T, Plott E, Arnold H, Kendall B, et al. Routine screening for eosinophilic esophagitis in patients presenting with dysphagia. Therapeutic advances in gastroenterology. 2011;4(1):27–35. doi: 10.1177/1756283X10384172. Epub 2011/02/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwiatek MA, Hirano I, Kahrilas PJ, Rothe J, Luger D, Pandolfino JE. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140(1):82–90. doi: 10.1053/j.gastro.2010.09.037. Epub 2010/09/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li-Kim-Moy JP, Tobias V, Day AS, Leach S, Lemberg DA. Esophageal subepithelial fibrosis and hyalinization are features of eosinophilic esophagitis. Journal of pediatric gastroenterology and nutrition. 2011;52(2):147–53. doi: 10.1097/MPG.0b013e3181ef37a1. Epub 2011/01/06. [DOI] [PubMed] [Google Scholar]
- 43.Roman S, Hirano I, Kwiatek MA, Gonsalves N, Chen J, Kahrilas PJ, et al. Manometric features of eosinophilic esophagitis in esophageal pressure topography. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society. 2011;23(3):208–14. e111. doi: 10.1111/j.1365-2982.2010.01633.x. Epub 2010/11/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bohm M, Sebastiano C, Malik ZA, Thomas R, Richter J. Sa1173 Racial Differences in Symptoms and Endoscopic Findings in Adults With Eosinophilic Esophagitis: A 10 Year Experience in an Urban Hospital. Gastroenterology. 2011;140(5, Supplement 1):S-244. [Google Scholar]
- 45.Malik ZA, Bohm M, Sebastiano C, Thomas R, Richter J. Sa1174 Symptoms and Endoscopic Findings in Children With Eosinophilic Esophagitis Differ by Race: A 7 Year Experience in an Urban Hospital. Gastroenterology. 2011;140(5, Supplement 1):S-244–S-5. [Google Scholar]
- 46.Moawad FJ, Maydonovitch CL, Veerappan GR, Bassett JT, Lake JM, Wong RK. Esophageal motor disorders in adults with eosinophilic esophagitis. Digestive diseases and sciences. 2011;56(5):1427–31. doi: 10.1007/s10620-011-1655-5. Epub 2011/03/19. [DOI] [PubMed] [Google Scholar]
- 47.Achem SR, Almansa C, Krishna M, Heckman MG, Wolfsen HC, Talley NJ, et al. Oesophageal eosinophilic infiltration in patients with noncardiac chest pain. Alimentary pharmacology & therapeutics. 2011;33(11):1194–201. doi: 10.1111/j.1365-2036.2011.04652.x. Epub 2011/04/07. [DOI] [PubMed] [Google Scholar]
- 48.Lucendo AJ, De Rezende LC, Jimenez-Contreras S, Yague-Compadre JL, Gonzalez-Cervera J, Mota-Huertas T, et al. Montelukast Was Inefficient in Maintaining Steroid-Induced Remission in Adult Eosinophilic Esophagitis. Digestive diseases and sciences. 2011 doi: 10.1007/s10620-011-1775-y. Epub 2011/06/16. [DOI] [PubMed] [Google Scholar]
- 49.Martin Martin L, Santander C, Lopez Martin MC, Espinoza-Rios J, Chavarria-Herbozo C, Gisbert JP, et al. Esophageal motor abnormalities in eosinophilic esophagitis identified by high-resolution manometry. Journal of gastroenterology and hepatology. 2011;26(9):1447–50. doi: 10.1111/j.1440-1746.2011.06770.x. Epub 2011/05/18. [DOI] [PubMed] [Google Scholar]
- 50.Vindigni C, Villanacci V, Marini M, Rocca BJ, Frosini G, Pedruzzi E, et al. Eosinophilic esophagitis: an Italian experience. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva. 2010;102(1):15–9. doi: 10.4321/s1130-01082010000100003. Epub 2010/03/02. [DOI] [PubMed] [Google Scholar]
- 51.Penfield JD, Lang DM, Goldblum JR, Lopez R, Falk GW. The role of allergy evaluation in adults with eosinophilic esophagitis. Journal of clinical gastroenterology. 2010;44(1):22–7. doi: 10.1097/MCG.0b013e3181a1bee5. Epub 2009/07/01. [DOI] [PubMed] [Google Scholar]
- 52.Krarup AL, Villadsen GE, Mejlgaard E, Olesen SS, Drewes AM, Funch-Jensen P. Acid hypersensitivity in patients with eosinophilic oesophagitis. Scandinavian journal of gastroenterology. 2010;45(3):273–81. doi: 10.3109/00365520903469931. Epub 2009/12/17. [DOI] [PubMed] [Google Scholar]
- 53.Dellon ES, Gibbs WB, Rubinas TC, Fritchie KJ, Madanick RD, Woosley JT, et al. Esophageal dilation in eosinophilic esophagitis: safety and predictors of clinical response and complications. Gastrointestinal endoscopy. 2010;71(4):706–12. doi: 10.1016/j.gie.2009.10.047. Epub 2010/02/23. [DOI] [PubMed] [Google Scholar]
- 54.Leslie C, Mews C, Charles A, Ravikumara M. Celiac disease and eosinophilic esophagitis: a true association. Journal of pediatric gastroenterology and nutrition. 2010;50(4):397–9. doi: 10.1097/MPG.0b013e3181a70af4. Epub 2009/10/21. [DOI] [PubMed] [Google Scholar]
- 55.Robles-Medranda C, Villard F, le Gall C, Lukashok H, Rivet C, Bouvier R, et al. Severe dysphagia in children with eosinophilic esophagitis and esophageal stricture: an indication for balloon dilation? Journal of pediatric gastroenterology and nutrition. 2010;50(5):516–20. doi: 10.1097/MPG.0b013e3181b66dbd. Epub 2009/11/26. [DOI] [PubMed] [Google Scholar]
- 56.Binkovitz LA, Lorenz EA, Di Lorenzo C, Kahwash S. Pediatric eosinophilic esophagitis: radiologic findings with pathologic correlation. Pediatric radiology. 2010;40(5):714–9. doi: 10.1007/s00247-009-1484-2. Epub 2009/12/19. [DOI] [PubMed] [Google Scholar]
- 57.Peterson KA, Thomas KL, Hilden K, Emerson LL, Wills JC, Fang JC. Comparison of esomeprazole to aerosolized, swallowed fluticasone for eosinophilic esophagitis. Digestive diseases and sciences. 2010;55(5):1313–9. doi: 10.1007/s10620-009-0859-4. Epub 2009/06/18. [DOI] [PubMed] [Google Scholar]
- 58.Dias JA, Moawad FJ, Veerappan GR, Maydonovitch CL, Lake JM, Wong R. S1074 Differences Between Blacks and Whites With Eosinophilic Esophagitis. Gastroenterology. 2010;138(5, Supplement 1):S-173. [Google Scholar]
- 59.Moy N, Miller FH, Hirano I. S1094 Limited Accuracy of Upper GI Studies in the Diagnosis of Eosinophilic Esophagitis in Adults. Gastroenterology. 2010;138(5, Supplement 1):S-178. [Google Scholar]
- 60.Bohm M, Richter JE, Kelsen S, Thomas R. Esophageal dilation: simple and effective treatment for adults with eosinophilic esophagitis and esophageal rings and narrowing. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus / ISDE. 2010;23(5):377–85. doi: 10.1111/j.1442-2050.2010.01051.x. Epub 2010/04/01. [DOI] [PubMed] [Google Scholar]
- 61.Kanakala V, Lamb CA, Haigh C, Stirling RW, Attwood SE. The diagnosis of primary eosinophilic oesophagitis in adults: missed or misinterpreted? European journal of gastroenterology & hepatology. 2010;22(7):848–55. doi: 10.1097/MEG.0b013e32832c7709. Epub 2010/05/11. [DOI] [PubMed] [Google Scholar]
- 62.Dohil R, Newbury R, Fox L, Bastian J, Aceves S. Oral viscous budesonide is effective in children with eosinophilic esophagitis in a randomized, placebo-controlled trial. Gastroenterology. 2010;139(2):418–29. doi: 10.1053/j.gastro.2010.05.001. Epub 2010/05/12. [DOI] [PubMed] [Google Scholar]
- 63.Hejazi RA, Reddymasu SC, Sostarich S, McCallum RW. Disturbances of esophageal motility in eosinophilic esophagitis: a case series. Dysphagia. 2010;25(3):231–7. doi: 10.1007/s00455-009-9248-6. Epub 2009/08/27. [DOI] [PubMed] [Google Scholar]
- 64.Enns R, Kazemi P, Chung W, Lee M. Eosinophilic esophagitis: clinical features, endoscopic findings and response to treatment. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2010;24(9):547–51. doi: 10.1155/2010/341925. Epub 2010/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Malhotra A, Dhadham GC, Galeano N, Akmal A, Baddoura W. 65 Is There a Seasonal Variation in Eosinophilic Esophagitis? - A Single Center Experience [abstract] The American journal of gastroenterology. 2010;105(Supplement 1s):S24. [Google Scholar]
- 66.Jacob S, Jackson C, Barrett J, Low K. 1366 A Retrospective Review of the Prevalence of Eosinophilic Esophagitis in Male Veterans [abstract] The American journal of gastroenterology. 2010;105(Supplement 1s):S505–S6. [Google Scholar]
- 67.Straumann A, Conus S, Degen L, Felder S, Kummer M, Engel H, et al. Budesonide is effective in adolescent and adult patients with active eosinophilic esophagitis. Gastroenterology. 2010;139(5):1526–37. 37, e1. doi: 10.1053/j.gastro.2010.07.048. Epub 2010/08/05. [DOI] [PubMed] [Google Scholar]
- 68.Shah A, Kagalwalla AF, Gonsalves N, Melin-Aldana H, Li BU, Hirano I. Histopathologic variability in children with eosinophilic esophagitis. The American journal of gastroenterology. 2009;104(3):716–21. doi: 10.1038/ajg.2008.117. Epub 2009/02/12. [DOI] [PubMed] [Google Scholar]
- 69.Achem SR, Almansa C, Heckman MG, Talley NJ, DeVault KR. W1336 Diagnostic Value of Endoscopic Signs in Suspected Eosinophilic Esophagitis [abstract] Gastroenterology. 2009;136(5, Supplement 1) [Google Scholar]
- 70.Garrean CP, Patil D, Gonsalves N, Yang GY, Hirano I. S1860 Comparison of Endoscopic and Histologic Response in Patients with Eosinophilic Esophagitis Treated with Proton Pump Inhibition, Topical Fluticasone, and Dietary Elimination [abstract] Gastroenterology. 2009;136(5, Supplement 1):A-279. [Google Scholar]
- 71.Almansa C, Cano S, DeVault KR, Wolfsen HC, Talley NJ, Achem SR. S1862 Overlapping Features Between Eosinophilic Esophagitis and Gastroesophageal Reflux [abstract] Gastroenterology. 2009;136(5, Supplement 1):A-280. [Google Scholar]
- 72.Miller SM, Tatel SF, Lee SJ, Boike JR, Kim J, Gonsalves N, et al. S1864 The Utility of Specific Symptoms and Endoscopic Features As Predictors of Eosinophilic Esophagitis (EoE) in Adults [abstract] Gastroenterology. 2009;136(5, Supplement 1):A-280. [Google Scholar]
- 73.Chaves DM, Imada RR, Felipe-Silva AS, Nakao FS, Rodrigues RA, Assef MS, et al. S1885 Eosinophilic Esophagitis: Counting of the Numbers of Eosinophils in the Three Segments of the Esophagus and Clinical Aspects [abstract] Gastroenterology. 2009;136(5, Supplement 1):A-285. [Google Scholar]
- 74.Karakelides M, Kopacova J, Enders F, Dierkhising RA, Talley NJ, Weiler C, et al. 4 Eosinophilic Esophagitis in Adults Lacks Seasonal Correlation [abstract] The American journal of gastroenterology. 2009;104(Supplement 3s):S1–S2. [Google Scholar]
- 75.Sayej WN, Patel R, Baker RD, Tron E, Baker SS. Treatment with high-dose proton pump inhibitors helps distinguish eosinophilic esophagitis from noneosinophilic esophagitis. Journal of pediatric gastroenterology and nutrition. 2009;49(4):393–9. doi: 10.1097/MPG.0b013e31819c4b3e. Epub 2009/07/28. [DOI] [PubMed] [Google Scholar]
- 76.Eroglu Y, Lu H, Terry A, Tendler J, Knopes B, Corless C, et al. Pediatric eosinophilic esophagitis: single-center experience in northwestern USA. Pediatrics international : official journal of the Japan Pediatric Society. 2009;51(5):612–6. doi: 10.1111/j.1442-200X.2008.02796.x. Epub 2009/10/06. [DOI] [PubMed] [Google Scholar]
- 77.Aceves SS, Newbury RO, Dohil MA, Bastian JF, Dohil R. A symptom scoring tool for identifying pediatric patients with eosinophilic esophagitis and correlating symptoms with inflammation. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2009;103(5):401–6. doi: 10.1016/S1081-1206(10)60359-6. Epub 2009/11/26. [DOI] [PubMed] [Google Scholar]
- 78.Schoepfer AM, Gschossmann J, Scheurer U, Seibold F, Straumann A. Esophageal strictures in adult eosinophilic esophagitis: dilation is an effective and safe alternative after failure of topical corticosteroids. Endoscopy. 2008;40(2):161–4. doi: 10.1055/s-2007-995345. Epub 2008/02/07. [DOI] [PubMed] [Google Scholar]
- 79.Ferreira CT, Vieira MC, Vieira SM, Silva GS, Yamamoto DR, Silveira TR. [Eosinophilic esophagitis in 29 pediatric patients] [in Portuguese with English abstract] Arquivos de gastroenterologia. 2008;45(2):141–6. doi: 10.1590/s0004-28032008000200010. Epub 2008/07/16. Esofagite eosinofilica em 29 pacientes pediatricos. [DOI] [PubMed] [Google Scholar]
- 80.Garrean C, Gonsalves N, Hirano I. S1971 Comparison of Demographic, Endoscopic and Histologic Features in EoE Patients with and Without GERD [abstract] Gastroenterology. 2008;134(4, Supplement 1):A-288. [Google Scholar]
- 81.Eswaran SL, Gonsalves N, Hirano I. S1983 Narrow Band Imaging May Improve the Sensitivity of Endoscopy for Diagnosing Eosinophilic Esophagitis [abstract] Gastroenterology. 2008;134(4, Supplement 1):A-291. [Google Scholar]
- 82.Gonsalves N, Yang G-Y, Doerfler B, Ritz S, Ditto AM, Hirano I. 727 A Prospective Clinical Trial of Six Food Elimination Diet and Reintroduction of Causative Agents in Adults with Eosinophilic Esophagitis (EE) Gastroenterology. 2008;134(4, Supplement 1):A-104–A-5. [Google Scholar]
- 83.Collins MH, Blanchard C, Abonia JP, Kirby C, Akers R, Wang N, et al. Clinical, pathologic, and molecular characterization of familial eosinophilic esophagitis compared with sporadic cases. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2008;6(6):621–9. doi: 10.1016/j.cgh.2008.01.004. Epub 2008/04/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin Martin L, Santander Vaquero C, Sanchez Prudencio S, Cantero Perona J, Gisbert JP, Moreno-Otero R. [Eosinophilic esophagitis in the adult--clinical, endoscopic, pH-metric, and manometric findings] [in Spanish with English abstract] Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva. 2008;100(8):476–80. doi: 10.4321/s1130-01082008000800006. Epub 2008/10/24. Esofagitis eosinofilica en el adulto: aspectos clinicos, endoscopicos, pH-metricos y manometricos. [DOI] [PubMed] [Google Scholar]
- 85.Mackenzie SH, Go M, Chadwick B, Thomas K, Fang J, Kuwada S, et al. Eosinophilic oesophagitis in patients presenting with dysphagia--a prospective analysis. Alimentary pharmacology & therapeutics. 2008;28(9):1140–6. doi: 10.1111/j.1365-2036.2008.03795.x. Epub 2008/07/16. [DOI] [PubMed] [Google Scholar]
- 86.Pentiuk SP, Miller CK, Kaul A. Eosinophilic esophagitis in infants and toddlers. Dysphagia. 2007;22(1):44–8. doi: 10.1007/s00455-006-9040-9. Epub 2006/10/07. [DOI] [PubMed] [Google Scholar]
- 87.Lee GS, Craig PI, Freiman JS, de Carle D, Cook IJ. Intermittent dysphagia for solids associated with a multiringed esophagus: clinical features and response to dilatation. Dysphagia. 2007;22(1):55–62. doi: 10.1007/s00455-006-9043-6. Epub 2007/01/12. [DOI] [PubMed] [Google Scholar]
- 88.Aceves SS, Newbury RO, Dohil R, Schwimmer J, Bastian JF. Distinguishing eosinophilic esophagitis in pediatric patients: clinical, endoscopic, and histologic features of an emerging disorder. Journal of clinical gastroenterology. 2007;41(3):252–6. doi: 10.1097/01.mcg.0000212639.52359.f1. Epub 2007/04/12. [DOI] [PubMed] [Google Scholar]
- 89.Muller S, Puhl S, Vieth M, Stolte M. Analysis of symptoms and endoscopic findings in 117 patients with histological diagnoses of eosinophilic esophagitis. Endoscopy. 2007;39(4):339–44. doi: 10.1055/s-2007-966216. Epub 2007/04/12. [DOI] [PubMed] [Google Scholar]
- 90.Kerlin P, Jones D, Remedios M, Campbell C. Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus. Journal of clinical gastroenterology. 2007;41(4):356–61. doi: 10.1097/01.mcg.0000225590.08825.77. Epub 2007/04/07. [DOI] [PubMed] [Google Scholar]
- 91.Jabeen SA, Hashmi SM, Hughes L, Choudary S, Mann J, Ryan BE, et al. T2040 A Case-Control Study to Differentiate Allergic / Idiopathic Eosinophilic Esophagitis (Aee/Iee) from Gastroesophageal Reflux Disease in Adults [abstract] Gastroenterology. 2007;132(4, Supplement 2):A-608–A-9. [Google Scholar]
- 92.Almansa C, DeVault KR, Buchner AM, Achem SR. T2044 The Faces of Eosinophilic Esophagitis (Eoe) in Adults and Children [abstract] Gastroenterology. 2007;132(4, Supplement 2):A-609–A-10. [Google Scholar]
- 93.Hashmi H, Baker SS, Baker RJ, Tran E. T2046 Association of Eosinophilic Esophagitis with Furrows [abstract] Gastroenterology. 2007;132(4, Supplement 2):A-610. [Google Scholar]
- 94.Gangotena F, Mackenzie S, Go M, Thomas K, Fang J, Peterson K. 79 Eosinophilic Esophagitis/Ringed Esophagus: The Diagnostic Conundrum [abstract] The American journal of gastroenterology. 2007;102(Supplement 2s):S145–S6. [Google Scholar]
- 95.Chehade M, Sampson HA, Morotti RA, Magid MS. Esophageal subepithelial fibrosis in children with eosinophilic esophagitis. Journal of pediatric gastroenterology and nutrition. 2007;45(3):319–28. doi: 10.1097/MPG.0b013e31806ab384. Epub 2007/09/18. [DOI] [PubMed] [Google Scholar]
- 96.Lucendo AJ, Pascual-Turrion JM, Navarro M, Comas C, Castillo P, Letran A, et al. Endoscopic, bioptic, and manometric findings in eosinophilic esophagitis before and after steroid therapy: a case series. Endoscopy. 2007;39(9):765–71. doi: 10.1055/s-2007-966738. Epub 2007/08/21. [DOI] [PubMed] [Google Scholar]
- 97.Cohen MS, Kaufman AB, Palazzo JP, Nevin D, Dimarino AJ, Jr, Cohen S. An audit of endoscopic complications in adult eosinophilic esophagitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2007;5(10):1149–53. doi: 10.1016/j.cgh.2007.05.017. Epub 2007/08/09. [DOI] [PubMed] [Google Scholar]
- 98.Aceves SS, Bastian JF, Newbury RO, Dohil R. Oral viscous budesonide: a potential new therapy for eosinophilic esophagitis in children. The American journal of gastroenterology. 2007;102(10):2271–9. doi: 10.1111/j.1572-0241.2007.01379.x. quiz 80. Epub 2007/06/22. [DOI] [PubMed] [Google Scholar]
- 99.Prasad GA, Talley NJ, Romero Y, Arora AS, Kryzer LA, Smyrk TC, et al. Prevalence and predictive factors of eosinophilic esophagitis in patients presenting with dysphagia: a prospective study. The American journal of gastroenterology. 2007;102(12):2627–32. doi: 10.1111/j.1572-0241.2007.01512.x. Epub 2007/09/04. [DOI] [PubMed] [Google Scholar]
- 100.Parfitt JR, Gregor JC, Suskin NG, Jawa HA, Driman DK. Eosinophilic esophagitis in adults: distinguishing features from gastroesophageal reflux disease: a study of 41 patients. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2006;19(1):90–6. doi: 10.1038/modpathol.3800498. Epub 2005/11/01. [DOI] [PubMed] [Google Scholar]
- 101.Remedios M, Campbell C, Jones DM, Kerlin P. Eosinophilic esophagitis in adults: clinical, endoscopic, histologic findings, and response to treatment with fluticasone propionate. Gastrointestinal endoscopy. 2006;63(1):3–12. doi: 10.1016/j.gie.2005.07.049. Epub 2005/12/27. [DOI] [PubMed] [Google Scholar]
- 102.De Angelis P, Markowitz JE, Torroni F, Caldaro T, Pane A, Morino G, et al. Paediatric eosinophilic oesophagitis: towards early diagnosis and best treatment. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. 2006;38(4):245–51. doi: 10.1016/j.dld.2005.08.004. Epub 2005/10/04. [DOI] [PubMed] [Google Scholar]
- 103.Gonsalves N, Policarpio-Nicolas M, Zhang Q, Rao MS, Hirano I. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointestinal endoscopy. 2006;64(3):313–9. doi: 10.1016/j.gie.2006.04.037. Epub 2006/08/23. [DOI] [PubMed] [Google Scholar]
- 104.Konikoff MR, Noel RJ, Blanchard C, Kirby C, Jameson SC, Buckmeier BK, et al. A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis. Gastroenterology. 2006;131(5):1381–91. doi: 10.1053/j.gastro.2006.08.033. Epub 2006/11/15. [DOI] [PubMed] [Google Scholar]
- 105.Cherian S, Smith NM, Forbes DA. Rapidly increasing prevalence of eosinophilic oesophagitis in Western Australia. Archives of disease in childhood. 2006;91(12):1000–4. doi: 10.1136/adc.2006.100974. Epub 2006/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Desai TK, Stecevic V, Chang CH, Goldstein NS, Badizadegan K, Furuta GT. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointestinal endoscopy. 2005;61(7):795–801. doi: 10.1016/s0016-5107(05)00313-5. Epub 2005/06/04. [DOI] [PubMed] [Google Scholar]
- 107.Zimmerman SL, Levine MS, Rubesin SE, Mitre MC, Furth EE, Laufer I, et al. Idiopathic eosinophilic esophagitis in adults: the ringed esophagus. Radiology. 2005;236(1):159–65. doi: 10.1148/radiol.2361041100. Epub 2005/06/29. [DOI] [PubMed] [Google Scholar]
- 108.Huang L, Fields AC, Reinertson TE. 2 Clinical Presentation, Endoscopic Findings and Treatment of Eosinophilic Esophagitis in Adults: An Analysis of 61 Consecutive Cases [abstract] The American journal of gastroenterology. 2005;100(Supplement 9s):S23. [Google Scholar]
- 109.Dauer EH, Freese DK, El-Youssef M, Thompson DM. Clinical characteristics of eosinophilic esophagitis in children. The Annals of otology, rhinology, and laryngology. 2005;114(11):827–33. doi: 10.1177/000348940511401103. Epub 2005/12/20. [DOI] [PubMed] [Google Scholar]
- 110.Liacouras CA, Spergel JM, Ruchelli E, Verma R, Mascarenhas M, Semeao E, et al. Eosinophilic esophagitis: a 10-year experience in 381 children. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2005;3(12):1198–206. doi: 10.1016/s1542-3565(05)00885-2. Epub 2005/12/20. [DOI] [PubMed] [Google Scholar]
- 111.Sundaram S, Sunku B, Nelson SP, Sentongo T, Melin-Aldana H, Kumar R, et al. Adherent white plaques: an endoscopic finding in eosinophilic esophagitis. Journal of pediatric gastroenterology and nutrition. 2004;38(2):208–12. doi: 10.1097/00005176-200402000-00020. Epub 2004/01/22. [DOI] [PubMed] [Google Scholar]
- 112.Straumann A, Spichtin HP, Bucher KA, Heer P, Simon HU. Eosinophilic esophagitis: red on microscopy, white on endoscopy. Digestion. 2004;70(2):109–16. doi: 10.1159/000080934. Epub 2004/09/24. [DOI] [PubMed] [Google Scholar]
- 113.Sant’Anna AM, Rolland S, Fournet JC, Yazbeck S, Drouin E. Eosinophilic esophagitis in children: symptoms, histology and pH probe results. Journal of pediatric gastroenterology and nutrition. 2004;39(4):373–7. doi: 10.1097/00005176-200410000-00013. Epub 2004/09/28. [DOI] [PubMed] [Google Scholar]
- 114.Khan S, Orenstein SR, Di Lorenzo C, Kocoshis SA, Putnam PE, Sigurdsson L, et al. Eosinophilic esophagitis: strictures, impactions, dysphagia. Digestive diseases and sciences. 2003;48(1):22–9. doi: 10.1023/a:1021769928180. Epub 2003/03/21. [DOI] [PubMed] [Google Scholar]
- 115.Attwood SE, Lewis CJ, Bronder CS, Morris CD, Armstrong GR, Whittam J. Eosinophilic oesophagitis: a novel treatment using Montelukast. Gut. 2003;52(2):181–5. doi: 10.1136/gut.52.2.181. Epub 2003/01/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Markowitz JE, Spergel JM, Ruchelli E, Liacouras CA. Elemental diet is an effective treatment for eosinophilic esophagitis in children and adolescents. The American journal of gastroenterology. 2003;98(4):777–82. doi: 10.1111/j.1572-0241.2003.07390.x. Epub 2003/05/10. [DOI] [PubMed] [Google Scholar]
- 117.Arora AS, Perrault J, Smyrk TC. Topical corticosteroid treatment of dysphagia due to eosinophilic esophagitis in adults. Mayo Clinic proceedings Mayo Clinic. 2003;78(7):830–5. doi: 10.4065/78.7.830. Epub 2003/07/04. [DOI] [PubMed] [Google Scholar]
- 118.Croese J, Fairley SK, Masson JW, Chong AK, Whitaker DA, Kanowski PA, et al. Clinical and endoscopic features of eosinophilic esophagitis in adults. Gastrointestinal endoscopy. 2003;58(4):516–22. doi: 10.1067/s0016-5107(03)01870-4. Epub 2003/10/02. [DOI] [PubMed] [Google Scholar]
- 119.Cheung KM, Oliver MR, Cameron DJ, Catto-Smith AG, Chow CW. Esophageal eosinophilia in children with dysphagia. Journal of pediatric gastroenterology and nutrition. 2003;37(4):498–503. doi: 10.1097/00005176-200310000-00018. Epub 2003/09/26. [DOI] [PubMed] [Google Scholar]
- 120.Walsh SV, Antonioli DA, Goldman H, Fox VL, Bousvaros A, Leichtner AM, et al. Allergic esophagitis in children: a clinicopathological entity. The American journal of surgical pathology. 1999;23(4):390–6. doi: 10.1097/00000478-199904000-00003. Epub 1999/04/13. [DOI] [PubMed] [Google Scholar]
- 121.Straumann A, Spichtin HP, Bernoulli R, Loosli J, Vogtlin J. [Idiopathic eosinophilic esophagitis: a frequently overlooked disease with typical clinical aspects and discrete endoscopic findings] [in German with English abstract] Schweizerische medizinische Wochenschrift. 1994;124(33):1419–29. Epub 1994/08/20. Idiopathische, eosinophile Osophagitis: eine haufig verkannte Krankheit mit typischer Klinik und diskretem endoskopischem Bild. [PubMed] [Google Scholar]
- 122.Attwood SE, Smyrk TC, Demeester TR, Jones JB. Esophageal eosinophilia with dysphagia. A distinct clinicopathologic syndrome. Digestive diseases and sciences. 1993;38(1):109–16. doi: 10.1007/BF01296781. Epub 1993/01/01. [DOI] [PubMed] [Google Scholar]
- 123.Lee RG. Marked eosinophilia in esophageal mucosal biopsies. The American journal of surgical pathology. 1985;9(7):475–9. doi: 10.1097/00000478-198507000-00002. Epub 1985/07/01. [DOI] [PubMed] [Google Scholar]