Abstract
Obesity in Chilean children has increased markedly over the past decades. School-based obesity prevention interventions have been launched by the Ministry of Health and academic groups to tackle this condition. We summarize the main characteristics of the interventions that we have conducted and reflect on the lessons learned. Since 2002, we conducted 1 pilot study, a 2-y controlled intervention including 6- to 12–y-old children (Casablanca), another pilot study, and a 2-y controlled intervention including teachers and their 4- to 9–y-old students (Macul). Both interventions consisted of training teachers to deliver contents on healthy eating, increasing physical education classes, and, additionally in Macul, teachers participated in a wellness program. BMI Z-score and obesity prevalence were compared among children in intervention and control schools by year and among students of intervention and control teachers. In the Casablanca study, the impact was greatest on the younger children during the first school year when the study received the full funding that was required. In Macul, although intervention teachers exhibited improvements in anthropometry and blood measures, the impact on the children was not related to their results. The main lessons learned from these experiences are random allocation of schools, although methodologically desirable, is not always possible; participation of parents is very limited; obesity is not recognized as a problem; and increasing physical activity and implementing training programs for teachers is difficult due to an inflexible curriculum and lack of teachers’ time. Unless these barriers are overcome, obesity prevention programs will not produce positive and lasting outcomes.
Introduction
In Chile, the prevalence of childhood obesity has increased sharply over the past 3 decades. In 6-y-old children (first grade) attending public schools, obesity has increased from 7% in 1987 to 22% in 2010 (1). The causes of this exponential increase are likely due to the combined effects of an increase in energy intake and a decrease in physical activity, both consequences of the rapid epidemiological-nutrition transition affecting most urban Latin America. In Chile, per capita income has more than doubled and poverty levels have dropped significantly (2); simultaneously, the consumption of energy-dense foods has increased, whereas the intake of fiber nutrient–rich low-energy foods has remained unchanged or has actually decreased (3). Recent data indicate that ∼88% of Chileans now live in urban areas and ∼90% are sedentary (4).
In 1997, the Ministry of Health launched a National Health Promotion Program (Vida Chile) with specific goals for each stage of the life course. For children, the goal for the decade was to reduce obesity at school entry, from 16% observed in 2000 to 12% in 2010 and to reduce sedentary behavior in the population older than 15 y of age from 91% who were initially classified as sedentary to 84%. These goals were not reached; on the contrary, obesity increased significantly to 22% in 2010, and sedentary behavior remained unchanged (5).
From 1999, Vida Chile included a “Healthy School Program” to address the rapid increase in childhood obesity considering that school programs might have a lifelong influence on physical activity and healthy eating. Until 2009, ∼25% of all public elementary schools in the country were accredited as “ healthy schools,” that is, they complied with implementing activities in at least 3e areas defined by Vida Chile (e.g., healthy eating, physical activity, tobacco control, alcohol and drugs). However, the criteria for accreditation only included process indicators and were poorly standardized (6). The continuing increase in childhood obesity was instrumental in the launching by the Ministry of Health in 2006 of another school-based initiative as part of its Global Strategy of Obesity (EGO schools) to specifically target obesity (7). An evaluation undertaken in 2009 that included 1000 EGO schools showed that between 2005 and 2008, the prevalence of obesity in 6-y-old children increased from 19.1% to 21.3% and that the degree of implementation of specific activities related to healthy eating and increased physical activity was not only insufficient, but when checked if they corresponded to what schools indicated, there was a huge gap. Only 40% of the schools indicated that the activities recommended in these 2 areas were in place; however, when checked on the ground, in one fourth of them, these activities were actually being implemented (8). One of the initiatives in which their effort was fruitless was in influencing what is being sold at the school kiosks (every school has at least 1 privately owned kiosk that mostly sells processed foods and provides a small amount of money to the school monthly).
Parallel efforts undertaken by researchers at the Institute of Nutrition and Food Technology, University of Chile, included several diet and physical activity interventions in elementary schools to reduce overweight and obesity under standardized, nonrandomized, controlled conditions with a strong evaluation component. Here we summarize the main characteristics of these interventions, the nature of the assessments components, and the results, and we look back at the lessons learned from these experiences.
We report here a summary of the main intervention studies we conducted.
Six-month pilot test of potential actions to address obesity in elementary schools in 3 cities: Santiago, Curicó and Casablanca (2002)
We developed and assessed the effectiveness of a 6-mo intervention to lower the BMI Z-score of 6- to 12–y-old children in 5 elementary schools. School authorities designated 3 schools in 3 cities (Santiago, Curicó, and Casablanca) as intervention schools (1 per city), whereas 2 schools were designated as controls (1 per city in Santiago and Curicó). The intervention included education in healthy eating for children and parents, a behavioral program to increase physical activity, and doubling of time devoted to physical education (PE) classes. Results from 2141 children in the intervention and 945 children in the control schools showed that BMI Z-score decreased from 0.63 to 0.51 in boys from intervention schools, whereas it remained unchanged in boys from control schools (Δ for BMI change between both groups of boys was significant, P < 0.001). In girls, the BMI Z-score remained unchanged. A differential effect on the BMI Z-score was observed according to baseline nutritional status; obese and overweight decreased by −0.16 and −0.15, respectively; normal children lost 0.07 BMI Z score units, whereas those who were underweight gained +0.15 BMI Z score units. This is relevant because it demonstrates that the intervention improved their weight status. No significant changes in BMI were observed in the control schools (9). Finally, we failed to gradually change the types of food sold at the kiosk because this was opposed by school directors and/or teachers.
Two-year intervention in 6- to 12-y-old children in 3 elementary schools located in the city of Casablanca (2003–2004)
On completion of the pilot study, the educational authorities in Casablanca requested the continuation of our program in all 3 elementary schools in the city for an additional 2 y. A comparison school with similar socioeconomic characteristics was selected from a nearby city as a control comparison group. We determined the effectiveness of this 2-y nonrandomized, controlled study in terms of changes in obesity prevalence and in anthropometric measurements in 1466 children from the intervention schools and 573 children from the control school (10).
We analyzed the results by period year (academic time and summer recess), considering school year 2003 as period 1, summer recess as period 2, and school year 2004 as period 3. The intervention included education for children and their parents, and several physical activity–related initiatives listed in the following. During period 1, teachers trained by the research nutritionist provided educational contents on healthy eating to the children; this activity was supervised periodically. Parents of participating children attended 2 sessions in which the nutritionist explained the most important aspects of the intervention. During period 3, due to funding limitations, only half of the educational activities for children and parents were implemented.
The physical activity program during period 1 consisted of a) the application of the Canadian Active Living Challenge, a practical behavioral resource designed to instill a healthy and active lifestyle for children; b) the provision of an extra 90 min per week of physical activity to children from third to eighth grade as PE classes; c) active recess (with music and dancing) for 4 mo; and d) out of school activities including the families of the children (mostly bicycle rides and walks). During period 3, only the extra weekly 90-min PE class was kept.
The impact of this intervention was assessed by comparison of changes in BMI Z-score and obesity prevalence between intervention and control children by period and sex and by age categories (<8, 8–10, 10–12, and >12 y). Table 1 shows a significant decrease in the BMI Z-score for periods 1 and 2 relative to baseline in boys from both intervention and control groups; however, the decrease was greater for the intervention group. At the end of period 3, values relative to baseline were significantly lower in the intervention group and significantly higher in the control group. In girls from the intervention schools, BMI Z-scores decreased from 0.64 to 0.52, remained unchanged, and increased back to 0.6 during period 3. In girls from the control school, BMI Z-scores also decreased in period 1, albeit less so, and a greater increase was observed during the last period. Obesity prevalence in boys in the intervention group decreased significantly during the first period compared with changes in the control group (17–11.4% vs. 21.6–19.7%). In girls, the decrease in obesity prevalence during period 1 was similar between groups. In period 3, this change was similar in both groups and in both sexes. When comparing the obesity prevalence between the end of study period and baseline, the decrease in the intervention group was significant for both sexes, whereas it remained practically unchanged in both sexes of the control group.
Table 1.
Changes in BMI Z-score and obesity prevalence in intervention and control children over 2 y: Casablanca 2003–2004
| Intervention Group |
||||||||
| Period 2 |
||||||||
| Period 1 |
Period 3 |
|||||||
| Boys (n = 750) |
Girls (n = 717) |
Boys |
Girls |
|||||
| Mar 03 | Nov 03 | Mar 03 | Nov 03 | Mar 04 | Nov 04 | Mar 04 | Nov 04 | |
| Age1 | 10.0 (2.3) | 10.6 (2.2) | 9.8 (2.3) | 10.4 (2.3) | 11.2 (2.3) | 11.6 (2.2) | 11 (2.3) | 11.4 (2.3) |
| BMI Z-score1 | 0.62 (1) | 0.442 (1) | 0.64 (0.95) | 0.512 (0.92) | 0.423 (1) | 0.534 (0.95) | 0.53 (0.93) | 0.584 (0.9) |
| % Obese | 17 | 11.4 | 14.1 | 10.35 | 11.46 | 12.35 | 9.9 | 10.3 |
| Control Group | ||||||||
| Period 2 |
||||||||
| Period 1 |
Period 3 |
|||||||
| Boys (n = 348) |
Girls (n = 224) |
Boys |
Girls |
|||||
| Mar 03 | Nov 03 | Mar 03 | Nov 03 | Mar 04 | Nov 04 | Mar 04 | Nov 04 | |
| Age1 | 9.9 (2.1) | 10.4 (2.1) | 9.9 (2.2) | 10.5 (2.2) | 11.1 (2.1) | 11.5 (2.1) | 11.2 (2.2) | 11.5 (2.2) |
| BMI Z-score1 | 0.67 (1) | 0.652 (1) | 0.64 (1) | 0.59 (1) | 0.653 (1) | 0.724 (1) | 0.573 (0.9) | 0.724 (0.9) |
| % Obese | 21.6 | 19.7 | 14.7 | 12.6 | 19.4 | 21.4 | 11.8 | 15.2 |
Values are mean (SD). Adapted from Reference 10 with permission.
Significant difference between March 03 and November 03.
Significant difference between March 03 and March 04.
Significant difference between March 03 and November 04.
Significant difference in changes in percentage of obese between intervention and control groups over 2 y.
Significant difference in changes in percentage of obese between intervention and control groups in period 1.
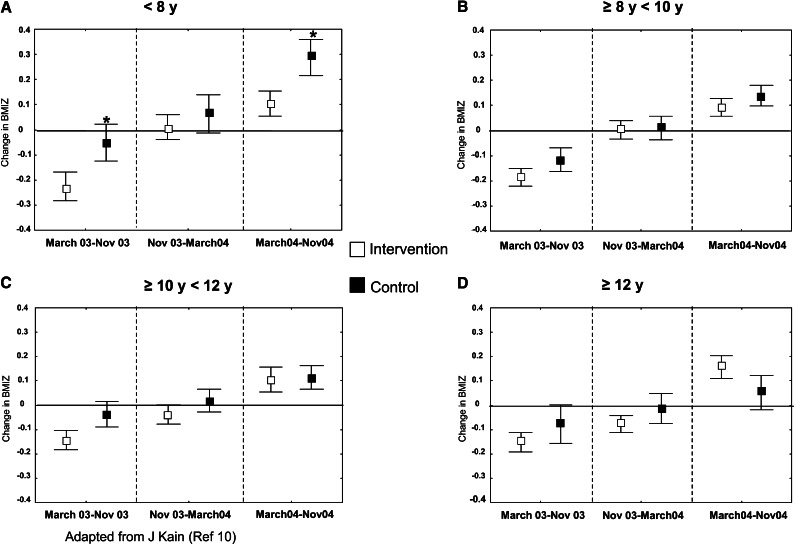
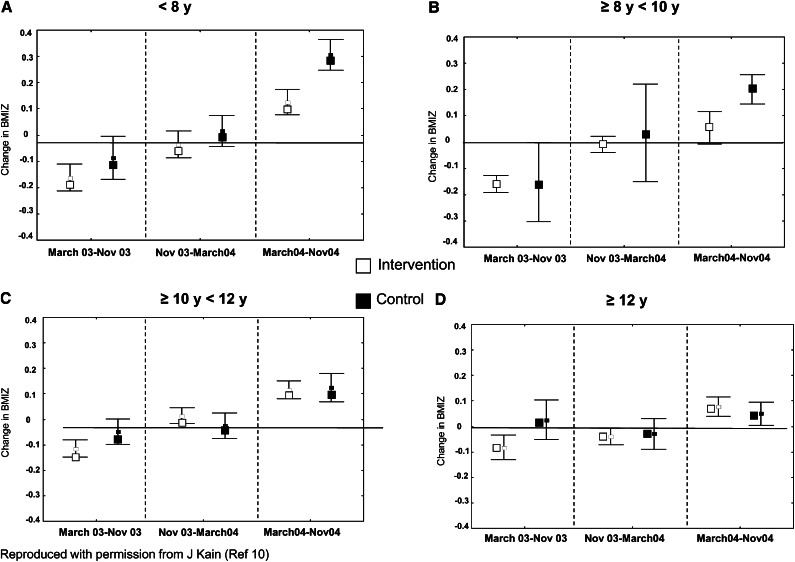
Figure 1 shows that the BMI Z-score decreased in all age categories for boys in intervention schools during period 1; however, the decline was significant only in the youngest (P = 0.03). No differences were observed in controls during that period. During the summer recess, there was practically no change in the BMI Z-score. During period 3, the BMI Z-score increased in both intervention and control groups; however, this increase was only significant among controls in the youngest category (P = 0.032). In girls (Fig. 2), the BMI Z-score followed a similar trend as in boys, but none of the changes were significant (P > 0.07).
Figure 1.
Change in mean BMI Z-score in boys (95% CI) relative to baseline in intervention and control schools according to age and period of study. Period 1 (March 03–Nov 03), period 2 (Nov 03–March 04), period 3 (March 04–Nov 04). Proc Mixed and Tukey test to compare intervention and control groups and time effects. There was a significant difference between intervention and control. *P < 0.05. Adapted from Reference 10 with permission.
Figure 2.
Change in mean BMI Z-score in girls (95% CI) relative to baseline in intervention and control schools according to age and period of study. Period 1 (March 03–Nov 03), Period 2 (Nov 03–March 04), Period 3 (March 04–Nov 04). Proc Mixed and Tukey test to compare intervention and control groups and time effects. Adapted from Reference 10 with permission.
Pilot test of a wellness program for teachers attending 7 public schools located in Macul, a district of Santiago, to prevent obesity in 4- to 9-y-old students (2006)
In this study, we hypothesized that a healthy lifestyle intervention for the improvement of teachers’ health status might enhance the effect of the educational and physical activity interventions on the children by serving as role models. Because the results of the Casablanca intervention showed greatest impact on the younger children, we decided to focus this study on preschool and schoolchildren (4–9 y old). A total of 522 children in that age category were included in a 5-mo intervention; additionally in 4 of the schools, a nutritionist applied a monthly wellness program for teachers of the same grade as the participating children. In this pilot study, we determined how best to implement the wellness program with the cooperation of the teachers. We also held 2 meetings with parents to request their support for the program at home; we were able obtain ∼30% participation in 2 regular school meetings.
Regarding physical activity, we determined the amount of time that children were in PE class and the proportion of time students engaged in moderate/vigorous activity. On average, the proportion of time that children engaged in moderate/vigorous activity during PE classes was only 19%. Nutritional status and physical fitness were evaluated in the 522 schoolchildren. Results showed a nonsignificant downward trend in the BMI Z-score in the 4- to 7-y-old children (P = 0.15), whereas in the 8- and 9-y-old children, the BMI Z-score increased nonsignificantly (P = 0.22). The prevalence of obesity remained unchanged, whereas there was a slight improvement in fitness (11).
Two-year intervention of a wellness program for teachers attending 7 public schools located in Macul to prevent obesity in 4- to 9–y-old students (2007–2008)
As a follow-up to the pilot program in Macul, we implemented the same wellness intervention for 2 y. The nutrition education component included a nutritionist who reinforced the training and supervised the implementation of the educational program over the entire period. Teachers were also trained on how to increase the time that children engage in moderate/vigorous activity in PE class. This initiative was conducted in 3 practical sessions each year. The impact was assessed by changes in the prevalence of obesity and BMI Z-score observed in the children (by sex) and by comparing students of participating teachers with controls (Table 2). We also measured the impact on the teachers by changes in anthropometry (Table 3) and blood measures (obtained only in the intervention teachers) (Table 4).
Table 2.
Changes in BMI Z-score and prevalence of obesity in the total sample by group and sex: Macul 2007–2008
| Total sample |
Students of intervention teachers |
Students of control teachers |
|||||||
| Total (n = 714) | Boys (n = 390) | Girls (n = 351) | Total (n = 412) | Boys (n = 209) | Girls (n = 203) | Total (n = 237) | Boys (n = 135) | Girls (n = 102) | |
| BMI Z-score at baseline1 | 1.03 (1.1) | 1.07 (1.2) | 0.98 (1.1) | 1.03 (1.1) | 1.1 (1.2) | 0.96 (1.0) | 1.03 (1.1) | 1.03 (1.1) | 1.04 (1.1) |
| BMI Z-score at follow-up1 | 0.92 (1) | 0.94 (1.1) | 0.90 (1.0) | 0.94 (1.0) | 1.0 (1.1) | 0.87 (1.0) | 0.9 (1.0) | 0.81 (0.94)* | 0.98 (1.0) |
| % Obesity at baseline | 20.2 | 21.5 | 18.8 | 20.0 | 21.9 | 18.1 | 20.7 | 20.7 | 20.6 |
| % Obesity at follow-up | 18.32 | 21.0 | 15.43 | 19.2 | 22.7 | 15.73 | 16.52 | 17.8 | 14.73 |
Students of intervention teachers compared with students of control teachers. Values are mean (SD). Adapted from Reference 12 with permission.
Significant difference between baseline and follow-up of students of intervention teachers and those of control teachers
Significant difference between baseline and follow-up of students of intervention teachers and those of control teachers by sex.
Table 3.
Comparison of changes in the nutritional status of intervention and control teachers: Macul 2007–2008
| Intervention teachers (n = 28) |
Control teachers (n = 19) |
|||
| Mar 07 | Nov 08 | Mar 07 | Nov 08 | |
| BMI1 | 27.1 (3.7) | 26.8 (3.7) | 27.2 (3.9) | 26.8 (3.9) |
| Waist circumference, cm1 | 84.7 (10.4) | 84.9 (7.9) | 84.3 (10.5) | 86.7 (10.9) |
| % Obesity | 25.0 | 22.4 | 21.4 | 24.6 |
Values are means ± SD unless specified otherwise. Reproduced from Reference 13 with permission.
TABLE 4.
Changes in blood measures in intervened teachers: Macul 2007–20081
| March 2007 | November 2008 | |
| Glucose, mg/dL | 93.3 (7.6) | 88.0 (6.2)2 |
| Total cholesterol, mg/dL | 201.8 (42.5) | 201.2 (40.4) |
| HDL cholesterol, mg/dL | 48.1 (9.9) | 57.4 (11.6)2 |
| LDL cholesterol, mg/dL | 129.9 (33.2) | 118.3 (39.2) |
| Triglycerides, mg/dL | 118.6 (65.0) | 107.2 (53.9) |
Values are means ± SD. Reproduced from Reference 12 with permission.
Significant difference between baseline and follow-up.
Table 2 shows that the overall prevalence of obesity decreased significantly at follow-up, from 20.2% to 18.3%, due exclusively to a decrease in girls; obesity in boys remained unchanged. On the other hand, the BMI Z-score decreased significantly for both sexes. The comparison in obesity prevalence and BMI Z-score between children whose teachers participated in the wellness program (intervened) and those who did not (controls) showed that there was a significant decrease in obesity prevalence only among the children of control teachers. The analysis by sex revealed obesity prevalence decreased significantly in girls; however, the decrease was greater among girls of control teachers. Results for the total sample in terms of the BMI Z-score showed a significant decrease from 1.03 to 0.92; however, this was mainly due to changes in boys of control teachers whose mean BMI Z-score decreased from 1.03 to 0.81.
Table 3 shows the comparison of changes in anthropometry and some blood measures among teachers who received the wellness program with those who did not. The prevalence of obesity of the wellness group decreased nonsignificantly from 25% to 22.4%, whereas the control group increased nonsignificantly from 21.4% to 24.6%. Blood measures (determined only for the wellness group) improved; significant changes were observed in serum glucose and total cholesterol (12). The proportion of time that children engaged in moderate/vigorous activity increased significantly from 19% to 29% (no difference was observed between the 2 groups of children).
Since 2009, we have also progressively implemented, “healthy kiosks” in the 7 schools of Macul following a predefined approach that includes training the person in charge on healthy foods and gradually increasing the offer of healthy inexpensive foods (13).
With the experience gained by our group in school-based obesity prevention programs over the years, we are able to recognize some pitfalls in the overall process involving design, implementation, and evaluation of these interventions and also acknowledge the lessons learned.
Recognition of pitfalls
Interventions need to be fully resourced (human and material resources need to be in place and fully trained at the outset) because changes in the strength of the interventions detract from being able to measure the impact.
Teachers’ apathy and failure to comply with requested participation cannot be overcome with persuasion alone. The authorization to work in the school and even the expressed interest of the school directives are clearly not enough to secure genuine participation. Incentives, monetary or otherwise, are necessary to produce changes, but, at least in Chile, they are unlikely to succeed as a form of pressure.
School kiosks are commonly at odds with obesity prevention. Incentives to sell unhealthy choices need to be removed before attempting to change products sold.
Lessons learned
Experimental designs using random allocation of schools to 1 or more interventions are nearly impossible to implement within an educational system that is not accustomed to controlled evaluations and local school administration that sees no actual value or consequences of the results of an evaluation process. At best, we were able to implement interventions in schools where there was a higher obesity prevalence in children, thus making them less likely participate in the program.
There is a need for an enabling environment and actively sensitizing multiple stakeholders to have the potential for success. Intervention in the school setting without modifying home or social environment will hardly ever succeed.
Clearly defined processes, targets, and measures of success are needed. Ideally, consequences of success and failure for the school administrators, teachers, and other parties involved should be in place before starting the intervention.
Contribution of parents in the process of change is grossly underestimated and may be in fact a key factor for success or failure. In the setting of urban transitional countries, it is very difficult to engage parents in an obesity prevention program for their children. Possible explanations for this are that they do not acknowledge obesity as problem, they do not have time to participate, grandmothers or other adults are directly caring for the children, and the perception that cost of healthy foods makes them beyond their means.
Increasing physical activity at school is difficult because the academic curriculum is inflexible and uses most of the potential free time for additional Spanish and math classes, subjects included in the annual evaluation of schools. In addition, teachers report being heavily burdened by the need to implement various programs during the school year, and extra work is not welcome. Unless initiatives are integrated into the school curricula, they are not sustainable and unlikely to have an impact. Although extracurricular physical activity is a possibility, it is not sustainable unless parents and communities are fully committed to it.
Other potential contributory factors are a poorly suited school infrastructure and the possibility of training teachers to address obesity is very limited because they are committed to multiple tasks of which this aspect is not a priority. In brief, the culture of change for better is weak at best.
Finally, obesity prevention must begin much earlier. Data collected from a cohort of children followed from birth to 8 y of age show that the increase in obesity takes place very early in life. In fact, 30% of the obese children at school entry were already obese at 12 mo (14).
Acknowledgments
All authors have read and approved the final manuscript.
Footnotes
Published in a supplement to Advances in Nutrition. Presented at the conference “2nd Forum on Child Obesity Interventions” held in Mexico City, Mexico, August 22–24, 2011. The conference was organized and cosponsored by Fundación Mexicana para la Salud A.C. (FUNSALUD). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of FUNSALUD. The supplement coordinator for this supplement was Frania Pfeffer, FUNSALUD. Supplement Coordinator disclosures: Frania Pfeffer is employed by FUNSALUD, which received a research donation from Coca Cola, PEPSICO, and Peña Fiel, 3 major beverage companies in Mexico, to support the program of childhood obesity research and communication. The supplement is the responsibility of the Guest Editor to whom the Editor of Advances in Nutrition has delegated supervision of both technical conformity to the published regulations of Advances in Nutrition and general oversight of the scientific merit of each article. The Guest Editor for this supplement was Nanette Stroebele, University of Colorado, Denver. Guest Editor disclosure: Nanette Stroebele had no conflicts to disclose. Publication costs for this supplement were defrayed in part by the payment of page charges. This publication must therefore be hereby marked “advertisement” in accordance with 18 USC section 1734 solely to indicate this fact. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
Funding for the intervention studies described in this article was provided by the Chilean company Tresmontes Lucchetti.
Author disclosures: J. Kain, R. Uauy, F. Concha, B. Leyton, N. Bustos, G. Salazar, L. Lobos, F. Vio, no conflicts of interest.
Literature Cited
- 1.National School Association for Scholarships (JUNAEB) Available from: www.junaeb.cl. Accessed May 2011.
- 2.Ministry of Planning (Mideplan) Casen Survey 2009. Available from: www.mideplan.gob.cl /casen2009/Resultados. Accessed June 2011
- 3.Vio F, Albala C, Kain J. Nutrition transition in Chile revisited: mid-term evaluation of obesity goals for the period 2000–2010. Public Health Nutr. 2008;11:405–12 [DOI] [PubMed] [Google Scholar]
- 4.Ministry of HealthQuality of Life Survey 2006. Available from: www.minsal.cl/epi/htm/sdesalud/ calidad de vida 2006/Informe. Accessed June 2011
- 5.Ministry of HealthFinal Evaluation of Healthy Goals for the Decade 2000–2010. Available from: www.minsal.gob.cl/portal/url/item/94c 89f 56c 4e 270boe 04C. Accessed June 2011
- 6.Salinas J, Cancino A, Pezoa S, Salamanca F, Soto M. Vida Chile 1998–2006: resultados y deafíos de la política de promoción de la salud en Chile. Rev Panam Salud Publica. 2007;21:136–44 [DOI] [PubMed] [Google Scholar]
- 7.Ministry of HealthGlobal Strategy against Obesity. Available from: www.ego-chile.cl. Accessed on November 2010
- 8.Faculty of Medicine, University of Chile Evaluación externa de las acciones realizadas en las EGO-escuelas para el Ministerio de Salud. Santiago, Enero 2010. Available from: http:/www.redsalud.gov.cl/portal/ur/item/8781 c832880544e9e04001011e015e3b.pdf Accessed on November 2010
- 9.Kain J, Uauy R, Albala C, Vio F, Cerda R, Leyton B. School-based obesity prevention in Chilean school children: methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord. 2004;28:483–93 [DOI] [PubMed] [Google Scholar]
- 10.Kain J, Leyton B, Cerda R, Vio F, Uauy R. Two-year controlled effectiveness trial of a school-based intervention to prevent obesity in Chilean children. Public Health Nutr. 2009;12:1451–61 [DOI] [PubMed] [Google Scholar]
- 11.Kain J, Concha F, Salazar G, Leyton B, Rodríguez MP, Zeballos X, Vio F. Obesity prevention in preschool and schoolchildren attending public schools located in a district of Santiago, Chile: pilot study 2006. Arch Latinoam Nutr. 2009;59:139–46 [PubMed] [Google Scholar]
- 12.Kain J, Leyton B, Concha F, Salazar G, Lobos L, Vio F. Estrategia de prevención de obesidad en escolares: Efecto de un programa aplicado a sus profesores (2007–2008). Rev Med Chil. 2010;138:181–7 [PubMed] [Google Scholar]
- 13.Bustos N, Kain J, Vio F. Guía para el Diseño e Implementación de un Espacio y Punto de Venta Saludable en Escuelas Básicas de Chile, INTA, 2009.
- 14.Kain J, Corvalán C, Lera L, Galván M, Uauy R. Accelerated growth in early life and obesity in preschool chilean children. Obesity (Silver Spring). 2009;17:1603–8 [DOI] [PubMed] [Google Scholar]