Abstract
Background
The World Health Organization (WHO) estimates that the number of obese or overweight individuals worldwide will increase to 1.5 billion by 2015. Chronic diseases associated with overweight or obesity include diabetes, heart disease, hypertension and stroke.
Objectives
To assess the effects of interactive computer‐based interventions for weight loss or weight maintenance in overweight or obese people.
Search methods
We searched several electronic databases, including CENTRAL, MEDLINE, EMBASE, CINAHL, LILACS and PsycINFO, through 25 May 2011. We also searched clinical trials registries to identify studies. We scanned reference lists of included studies and relevant systematic reviews.
Selection criteria
Studies were included if they were randomized controlled trials or quasi‐randomized controlled trials that evaluated interactive computer‐based weight loss or weight maintenance programs in adults with overweight or obesity. We excluded trials if the duration of the intervention was less than four weeks or the loss to follow‐up was greater than 20% overall.
Data collection and analysis
Two authors independently extracted study data and assessed risk of bias. Where interventions, control conditions, outcomes and time frames were similar between studies, we combined study data using meta‐analysis.
Main results
We included 14 weight loss studies with a total of 2537 participants, and four weight maintenance studies with a total of 1603 participants. Treatment duration was between four weeks and 30 months. At six months, computer‐based interventions led to greater weight loss than minimal interventions (mean difference (MD) ‐1.5 kg; 95% confidence interval (CI) ‐2.1 to ‐0.9; two trials) but less weight loss than in‐person treatment (MD 2.1 kg; 95% CI 0.8 to 3.4; one trial). At six months, computer‐based interventions were superior to a minimal control intervention in limiting weight regain (MD ‐0.7 kg; 95% CI ‐1.2 to ‐0.2; two trials), but not superior to infrequent in‐person treatment (MD 0.5 kg; 95% ‐0.5 to 1.6; two trials). We did not observe consistent differences in dietary or physical activity behaviors between intervention and control groups in either weight loss or weight maintenance trials. Three weight loss studies estimated the costs of computer‐based interventions compared to usual care, however two of the studies were 11 and 28 years old, and recent advances in technology render these estimates unlikely to be applicable to current or future interventions, while the third study was conducted in active duty military personnel, and it is unclear whether the costs are relevant to other settings. One weight loss study reported the cost‐effectiveness ratio for a weekly in‐person weight loss intervention relative to a computer‐based intervention as USD 7177 (EUR 5678) per life year gained (80% CI USD 3055 to USD 60,291 (EUR 2417 to EUR 47,702)). It is unclear whether this could be extrapolated to other studies. No data were identified on adverse events, morbidity, complications or health‐related quality of life.
Authors' conclusions
Compared to no intervention or minimal interventions (pamphlets, usual care), interactive computer‐based interventions are an effective intervention for weight loss and weight maintenance. Compared to in‐person interventions, interactive computer‐based interventions result in smaller weight losses and lower levels of weight maintenance. The amount of additional weight loss, however, is relatively small and of brief duration, making the clinical significance of these differences unclear.
Keywords: Adult; Female; Humans; Male; Weight Loss; Obesity; Obesity/therapy; Overweight; Overweight/therapy; Randomized Controlled Trials as Topic; Therapy, Computer‐Assisted; Therapy, Computer‐Assisted/methods
Plain language summary
Interactive computer‐based interventions for weight loss or weight maintenance in overweight or obese people
Overweight and obesity are common health problems and increase the risk of developing several serious health conditions. The standard treatment for overweight and obesity is to help patients change their diet and exercise habits. Treatment programs in which patients interact with a computer may help people make these changes, and improve their ability to lose weight and keep it off. We looked for randomized or quasi‐randomized trials in which an interactive computer intervention was compared with no treatment, a limited treatment such as usual care or paper materials, or an in‐person treatment to help people lose weight or keep it off. We included 14 weight loss studies with a total of 2537 participants, and four weight maintenance studies with a total of 1603 participants. The length of treatment ranged from four weeks to 30 months. At six months, computer‐based interventions led to greater weight loss than minimal interventions (mean difference ‐1.5 kg; 95% confidence interval (CI) ‐2.1 to ‐0.9; two trials) but less than in‐person treatment (mean difference 2.1 kg; 95% CI 0.8 to 3.4; one trial). At six months, computer‐based interventions were superior to a minimal control intervention in limiting weight regain (mean difference ‐0.7 kg; 95% CI ‐1.2 to ‐0.2; two trials), but not superior to infrequent in‐person treatment (mean difference 0.5 kg; 95% ‐0.5 to 1.6; two trials).
Three weight loss studies estimated the costs of computer‐based interventions compared to usual care, however two of the studies were 11 and 28 years old, and these estimates are probably not relevant to interventions using current technology, while the third study was carried out in active duty military personnel, and it is unclear whether costs would be similar in other settings. One weight loss study reported the cost‐effectiveness ratio for a weekly in‐person weight loss intervention relative to a computer‐based intervention as USD 7177 (EUR 5678) per life year gained (80% CI USD 3055 to USD 60,291 (EUR 2417 to EUR 47,702)). It is unclear whether this is relevant to other studies. No studies had information on health‐related quality of life, morbidity, complications or adverse effects.
Compared to no intervention or minimal interventions (pamphlets, usual care), interactive computer‐based interventions are an effective intervention for weight loss and weight maintenance. Compared to in‐person interventions, interactive computer‐based interventions result in smaller weight losses and lower levels of weight maintenance. The amount of additional weight loss, however, is relatively small and of brief duration, making the clinical significance of these differences unclear.
Summary of findings
Summary of findings for the main comparison. Interactive computer intervention compared to usual care for weight loss or maintenance of weight loss in adults.
| Interactive computer intervention compared to usual care for weight loss or maintenance of weight loss in adults | ||||||
| Patient or population: adults with overweight or obesity Settings: community Intervention: interactive computer intervention Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual care | Interactive computer intervention | |||||
| Health‐related quality of life | See comment | See comment | Not estimable | See comment | See comment | Not investigated |
| Adverse effects | See comment | See comment | Not estimable | See comment | See comment | One weight maintenance study stated that no serious adverse events occurred. No other study investigated adverse events. |
|
Weight loss (change in kg weight) Follow‐up: 6 months |
The mean weight loss in the control groups ranged from 3.5 kg lost to 0.5 kg gained | The mean weight loss in the intervention groups was 1.5 kg (0.9 to 2.1) greater | 511 (2 studies) |
⊕⊕⊕⊝ moderate1 | ||
|
Weight regain (change in kg weight) Follow‐up: 12 months |
The mean weight regain in the control groups ranged from 0.6 kg to 3.0 kg | The mean weight regain in the intervention groups was 0.8 kg (0.2 to 1.4) lower | 1004 (3 studies) | ⊕⊕⊕⊝ moderate2 | ||
| Physical‐activity related outcomes | See comment | See comment | Not estimable | See comment | See comment | Few studies investigated these outcomes, and no individual studies or pooled analyses identified clinically or statistically significant physical‐activity effects |
| Cost‐effectiveness | See comment | See comment | Not estimable | See comment | See comment | Two weight loss studies estimated the costs of the intervention, however the studies were 11 and 28 years old. Recent advances in technology render these estimates unlikely to be applicable to current or future interventions. A companion publication to a third study estimated the costs of the intervention, but this study was conducted in active duty military personnel, and it is unclear whether costs could be extrapolated to other settings. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 One study stated that study staff could not be blinded. There was therefore a risk of bias in assessing outcome measurements. The same study was also unclear about allocation concealment. 2 Two studies were unclear about details of randomization, unclear about allocation concealment and unclear about blinding.
Summary of findings 2. Interactive computer intervention compared to in‐person interventions for weight loss or maintenance of weight loss in adults.
| Interactive computer intervention compared to in‐person intervention (monthly or less) for weight loss or maintenance of weight loss in adults | ||||||
| Patient or population: adults with overweight or obesity Settings: community Intervention: interactive computer intervention Comparison: in‐person intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| In‐person intervention | Interactive computer intervention | |||||
| Health‐related quality of life | See comment | See comment | Not estimable | See comment | See comment | Not investigated |
| Adverse effects | See comment | See comment | Not estimable | See comment | See comment | One weight maintenance study stated that no serious adverse events occurred. No other study investigated adverse events. |
|
Weight loss (change in kg weight) Follow‐up: 6 months |
The mean weight loss in the control group was 7.6 kg | The mean weight loss in the intervention group was 2.1 kg (0.8 to 3.4) smaller | 319 (1 study) |
⊕⊕⊕⊝ moderate1 | In‐person intervention was contact once per week | |
|
Weight regain (change in kg weight) Follow‐up: 12 months |
The mean weight regain in the control groups ranged from 4.0 kg to 0.6 kg | The mean weight regain in the intervention groups was 1.6 kg (0.1 lower to 3.2 higher) higher | 955 (3 studies) | ⊕⊕⊕⊝ moderate2 | In‐person intervention was contact monthly or less | |
|
Weight regain (change in kg weight) Follow‐up: 12 months |
The mean weight loss from start of weight loss to end of weight maintenance in the control group was 10.4 kg | The mean weight loss from start of weight loss to end of weight maintenance in the intervention group was 4.7 kg (1.7 to 7.7) lower | 62 (1 study) | ⊕⊕⊝⊝ low3 | In‐person intervention was contact every two weeks | |
| Physical‐activity related outcomes | See comment | See comment | Not estimable | See comment | See comment | Not investigated |
| Cost‐effectiveness | See comment | See comment | Not estimable | 62 (1 study) | See comment | The cost‐effectiveness ratio for the weekly in‐person weight loss intervention relative to the computer‐based intervention was reported in a companion publication as USD 7177 per life year gained (80% confidence interval USD 3055 to USD 60,291). It is unclear whether this could be extrapolated to other studies. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 The study was unclear about allocation concealment and blinding. 2 Two studies were unclear about details of randomization, unclear about allocation concealment and unclear about blinding.
3 The study was unclear about allocation concealment and blinding, and the total sample size for the comparison was very low.
Background
Description of the condition
Prevalence
Once considered a problem only in high‐income countries, overweight and obesity are now dramatically on the rise in low‐ and middle‐income countries, particularly in urban settings (World Health Organization 2011). The World Health Organization estimates that, without action, the number of overweight and obese individuals worldwide will increase from 1 billion in 2010 to 1.5 billion in 2015 (World Health Organization 2011). Overweight and obesity increase the risks for many chronic medical conditions, including diabetes, heart disease, hypertension and stroke (National Institutes of Health 2000), though modest reductions in weight can lead to important health benefits (Pi‐Sunyer 2007; Stevens 2001).
Aetiology
The fundamental cause of obesity and overweight is an energy imbalance between calories consumed and calories expended (World Health Organization 2004). Global increases in overweight and obesity are attributable to a number of factors including a global shift in diet towards increased intake of energy‐dense foods that are high in fat and sugars but low in vitamins, minerals and other micronutrients and a trend towards decreased physical activity due to the increasingly sedentary nature of many forms of work, changing modes of transportation and increasing urbanization (World Health Organization 2011).
Costs
Obesity accounts for 2% to 6% of total healthcare costs in several developed countries; some estimates put the figure as high as 7% (Withrow 2011). The true costs are undoubtedly much greater as not all obesity‐related conditions are included in the calculations. According to a study of national costs attributed to overweight and obesity, related medical expenditures accounted for 9.1 percent of the total U.S. medical costs in 1998 and may have reached as high as USD 78.5 billion (USD 92.6 billion in 2002 dollars) (Finkelstein 2003; see also http://www.cdc.gov/nccdphp/dnpa/obesity/economic_consequences.htm). Private employers alone are estimated to spend USD 45 billion per year paying for the direct and indirect costs of obesity (Finkelstein 2003).
A major issue is that overweight and obesity affects a great number of people, which means that any potential intervention needs to be highly cost‐effective. A quick calculation shows that, assuming that in‐person sessions cost USD 10 each and an individual attends 24 biweekly weight maintenance sessions per year, treatment of the 145 million U.S. adults who are overweight or obese would cost approximately USD 35 billion per year, an amount similar to the total annual budget of the U.S. National Institutes of Health (NIH) (Heinen 2009).
As computer and web‐based interventions have the potential to be cost‐effective or even free to the end‐user, supported by advertising, they have the potential for a significant public health impact (Mitchell 2008; Tate 2009). Due to this potentially great public health impact, understanding the impact of these interventions is critical in formulating a public health strategy for addressing the epidemic of overweight and obesity.
Diagnostic criteria
Body mass index (BMI) is an index of weight‐for‐height that is commonly used in classifying overweight and obesity in adult populations and individuals. It is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). The World Health Organization characterizes 'overweight' (a BMI greater than or equal to 25 kg/m2) and 'obesity' (a BMI greater than or equal to 30/m2) as “abnormal or excessive body weight that may impair health." (World Health Organization 2011).
Description of the intervention
The U.S. National Institutes of Health (NIH) recommend that weight loss programs include dietary therapy, physical activity and behavior therapy. The results of the National Weight Control Registry (Wing 2005) indicate four types of behavior common to the National Weight Control Registry participants:
eating a low‐fat, high‐carbohydrate diet;
eating breakfast almost every day;
frequent self monitoring of weight; and
participation in a high level of physical activity.
These behaviors may be supported by computer or Internet‐based programs. Today many people conduct their information‐seeking online, particularly information about health. Individuals who seek out that information are often motivated to learn about a health condition and many are particularly interested in self management of their health. Consequently, computer and/or Internet‐based interventions are associated with improved knowledge and/or behavioral outcomes (Wantland 2004).
Over the past decade, web‐based interventions have been developed and tested for a range of behaviors and chronic conditions, including weight control. Websites that attract enough users can be provided at no cost to those users and remain profitable when supported by advertising (Meenan 2009; Miller 2008; Mitchell 2008). In addition, web‐based programs overcome the time and travel barriers of face to‐face interventions, and increasingly include social features similar to the in‐person experience. If it were possible to create effective web‐based tools that were able to engage individuals for the long term, the reach of the Internet would give these interventions the ability to have a major public health impact (Glasgow 2007).
How the intervention might work
Behavioral weight control is the sum total of a great number of practices that each influence caloric intake, caloric expenditure, or both (Foster 2005). Traditional behavioral weight‐management programs typically include multiple components from multiple theoretical approaches (e.g. cognitive‐behavioral therapy, self regulation theory) (Brownell 2000; DPP Research Group 2002; Foster 2005). Participants are taught a number of recommended practices such as stimulus control, self monitoring (e.g. food records) and identification of high‐risk situations for relapse (Brownell 2000; DPP Research Group 2002; National Institutes of Health 2000). Weight loss maintenance interventions typically include a focus on the same set of weight control practices as in weight loss interventions (Rothman 2000), and reinforce the long‐term use of these practices by building problem‐solving skills (Perri 1992; Perri 2001; Perri 2008; Svetkey 2008).
As a result, interactive weight management interventions include features that mimic these components that would traditionally be provided in‐person, such as online goal‐setting as opposed to face‐to‐face goal setting. While face‐to‐face interventions often include diaries of caloric intake and exercise and a therapist compares these to the recommendations and goals for the patient, this feedback can be computerized and provided online without a therapist involved. Most of what is available, therefore, in interactive interventions has been a computerization of what is available face‐to‐face. This includes online chat sessions and message boards which are designed to replicate what might happen in a group counseling session.
Adverse effects of intervention
There are no known adverse effects of interactive computer‐based interventions for weight loss or weight maintenance.
Why it is important to do this review
As the prevalence of obesity continues to rise, the need for practical, easily disseminated and effective weight loss and weight maintenance programs has become increasingly important. Computer‐based interventions may serve as an efficient and cost‐effective method to meet this growing public health need (World Health Organization 2011).
For example, in 2001, Tate and colleagues published the results of a randomized trial that studied the impact of an interactive weight control website with the following features: 24 weekly lessons, weekly submission of self monitoring diaries, weekly recommendations from a therapist, and the opportunity for social support among group members (Tate 2001). The behavior therapy group lost a mean (standard deviation (SD)) of 4.0 (2.8) kg by three months and 4.1 (4.5) kg by six months. Since this first study, a large number of other studies have been published using a variety of interactive computer intervention features.
A Cochrane systematic review concluded that in people with chronic diseases, interactive health communication applications can help increase knowledge and social support and result in improved behavioral and clinical outcomes (Murray 2005). Two systematic reviews on computer‐based interventions to modify physical activity and dietary behaviors (Kroeze 2006; Wantland 2004) concluded that there is potential for the application of computer tailoring for promoting healthy diets. In addition, a recent review by Neve and colleagues excluded a number of studies that used interactive health communication methods that were not conducted over the Internet (Neve 2010). This distinction is important as most of the studies that have utilized the Internet could have been performed using computer‐tailored messages stored on the computer’s hard drive, rather than on a server at some distant location. For that reason, what was learned in studies that used interactive computer‐tailored messages stored locally is important for understanding what types of interactive interventions are effective. We have therefore included them in this review, rather than including only 'web‐based' interventions. This systematic review provides current evidence on all interactive computer‐based weight loss or weight maintenance interventions.
Objectives
To assess the effects of interactive computer‐based interventions for weight loss or weight maintenance in overweight or obese people.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) and quasi‐randomized controlled trials (quasi‐RCTs). We did not restrict by language or publication status (e.g. unpublished, abstract only or full journal publication).
Types of participants
We included studies with adult participants who were overweight or obese. Diagnostic criteria for overweight were usually based on the common body mass index (BMI) guidelines for adults, but we did not exclude studies that used other criteria (e.g. 10 pounds overweight). We excluded studies in which participants were not stated to be overweight or obese. We excluded studies including a mix of overweight and normal weight participants unless we were able to obtain data for the subgroup of overweight participants.
Types of interventions
We included trials evaluating computer‐based weight loss or weight maintenance programs that require the user to interact directly with the computer. We excluded trials in which the duration of the intervention was less than four weeks. We also excluded trials in which the loss to follow‐up was greater than 20% overall.
The control interventions were usual care, educational materials (either online or paper), telephone interventions and in‐person interventions.
We excluded studies using personal digital assistants (PDAs) or other communication media (e.g. interactive voice response) because computers allow by far the most rich set of possible interactions. At the time that this review was planned, PDAs and mobile telephones had lesser interactive potential due to their limited screen size and software functionality. However, we note that smartphones now have the capacity to function as fully mobile computers with interactive potential similar to that of laptops and desktops. We are not aware of any randomized trials of interactive weight loss programs on smartphones, but plan to search for and include trials of smartphones for the update of this review.
Types of outcome measures
Primary outcomes
Body weight (measured in kilograms or pounds) or body mass index (BMI). Body weight and BMI could be measured at endpoint, as absolute change from baseline, or as percentage change from baseline.
Waist circumference (measured in inches or centimeters). Waist circumference could be measured at endpoint, as absolute change from baseline, or as percentage change from baseline.
Health‐related quality of life, well‐being and patient satisfaction, as measured by any instrument.
Secondary outcomes
Physical activity‐related outcomes, such as steps per day, kilocalories per week, or any other measure of energy expenditure.
Diet‐related outcomes such as total fat intake, total calories, total fibre and number of servings of fruits/vegetables.
Cost‐effectiveness.
Adverse events.
Covariates, effect modifiers and confounders
Adherence.
Timing of outcome measurement
We assessed outcomes at short‐term (defined as four months or less), medium‐term (defined as greater than four months and less than 12 months) and long‐term (defined as 12 months or more) follow‐up. In studies with multiple short‐term times of outcome measurement, we chose to include the outcome measured at the time closest to the end of treatment. In studies where initiation of treatment was delayed substantially after randomization, we considered the starting point for follow‐up to be initiation of treatment rather than randomization.
Search methods for identification of studies
Electronic searches
We first searched the following databases from inception to April 2009, and then re‐ran the searches up to May 2011 for the identification of trials:
The Cochrane Library
Ovid MEDLINE(R)
Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations
Ovid EMBASE
EBSCOHost CINAHL
Web of Science
Dissertation Abstracts
Ovid PsycINFO
LILACS
Cochrane Behavioral Medicine Field Specialized Register
We searched databases on 14 and 15 April 2009 and on 25 May 2011. There were no language restrictions applied to any of the search strategies.
After the searches in these databases had been run, we set up for weekly alerts MEDLINE and PsycINFO and scanned the contents of key journals on a weekly basis up until September 2011 to check for any newly published studies.
Details of all search strategies are given in Appendix 1.
Searching other resources
To identify ongoing studies, we searched the CRISP database and Current Controlled Trials registries. We searched the reference lists of review articles and of all included studies in order to find other potentially eligible trials or ancillary publications.
We contacted several experts in this field (including authors of some of the included studies) to ensure that no other ongoing or unpublished studies had been missed.
Data collection and analysis
Selection of studies
To determine the studies to be assessed further, two authors (KJT and LF for the original search results, and LF and LSW for the updated search results) independently scanned the abstract, title or both sections of every record retrieved. We investigated all potentially relevant articles as full text. We measured interrater agreement for study selection using the kappa statistic (Cohen 1960). Where differences in opinion existed, they were resolved by a third party. If resolving disagreement was not possible, we added the article to those 'awaiting assessment' and contacted authors for clarification. An adapted PRISMA (preferred reporting items for systematic reviews and meta‐analyses) flow‐chart of study selection shown in Figure 1 (Liberati 2009).
1.
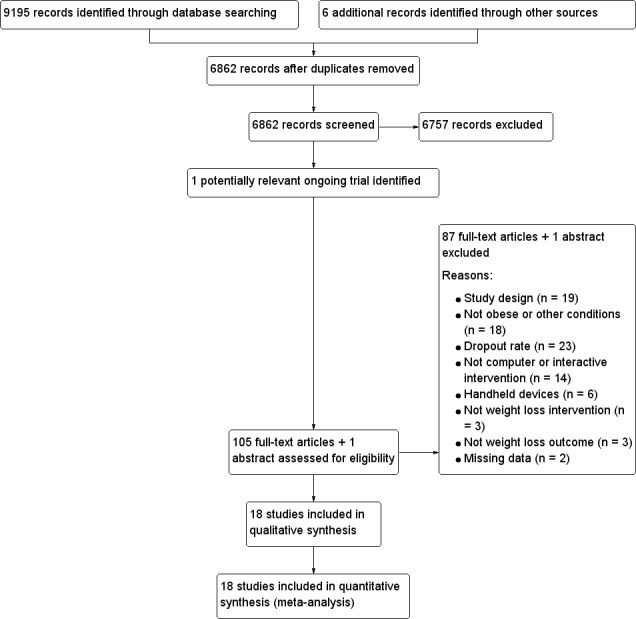
Study flow diagram.
Data extraction and management
Two review authors (LSW, SBF) independently abstracted relevant population and intervention characteristics using standard data extraction templates (for details see Characteristics of included studies; Table 3; Appendix 2; Appendix 3; Appendix 4; Appendix 5). We resolved all disagreements by discussion. Extracted data included year and country of study, study design, participant characteristics, inclusion and exclusion criteria, description of intervention and control conditions, duration of intervention, study outcomes and duration of follow‐up. We sought any missing information on key study characteristics or weight outcomes from the corresponding author of the article.
1. Overview of study populations.
|
Characteristic Study ID |
Intervention(s) and control(s) | [n] screened | [n] randomized | [n] safety | [n] ITT | [n] finishing study | [%] of randomized participants finishing study |
| Bennett 2010 | I: Internet‐based interactive weight loss approach; health coach support | Total: 390 | 51 | 51 | 51 | 43 | 84 |
| (weight loss study) | C: current standard of outpatient care and written materials | 50 | 50 | 50 | 42 | 82 | |
| total: | 101 | 101 | 101 | 85 | 84 | ||
| Cussler 2008 | I: Internet‐based program | Total: 300 | 66 | 66 | 66 | 52 | 79 |
| (weight maintenance study) | C: continue to practice principles during weight loss intervention | 69 | 69 | 69 | 59 | 86 | |
| total: | 135 | 135 | 135 | 111 | 82 | ||
| DeLucia 1988 | I1: Ferguson behavioral program and nutritional software 'The Eating Machine' | Not described | 10 | 10 | Not done | 9 | 90 |
| (weight loss study) | I2: Ferguson behavioral program and nutritional software 'EATS' | 10 | 10 | 9 | 90 | ||
| C: Ferguson program | 9 | 9 | 8 | 89 | |||
| total: | 29 | 29 | 26 | 90 | |||
| Gabriele 2011 | I1: Internet‐based program and directive e‐coach support | Total: 105 | 34 | 34 | 34 | 31 | 91 |
| (weight loss study) | I2: Internet‐based program and non‐directive e‐coach support | 35 | 35 | 35 | 33 | 94 | |
| C: Internet‐based program with minimal support | 35 | 35 | 35 | 32 | 91 | ||
| total: | 104 | 104 | 104 | 96 | 92 | ||
| Harvey‐Berino 2002 | I: Internet support | Not described | 40 | 40 | 40 | 30 | 75 |
| (weight maintenance study) | C1: continue to practice principles during weight loss intervention | 41 | 41 | 41 | 32 | 78 | |
| C2: minimal in‐person support | 41 | 41 | 41 | 28 | 68 | ||
| total: | 122 | 122 | 122 | 90 | 74 | ||
| Harvey‐Berino 2010 | I: online recording and chat sessions | Ineligible: 485 Consented: 658 Total: 1143 |
161 | 161 | 161 | 159 | 99 |
| (weight loss study) | C1: online recording and chat sessions and in‐person meetings | 162 | 162 | 162 | 153 | 94 | |
| C2: paper recording and in‐person chat sessions | 158 | 158 | 158 | 150 | 95 | ||
| total: | 481 | 481 | 481 | 462 | 96 | ||
| Hunter 2008b | I: behavioral Internet treatment | Total: 682 | 227 | 227 | 224 | 193 | 85 |
| (weight loss study) | C: usual care | 224 | 224 | 222 | 206 | 92 | |
| total: | 451 | 451 | 446 | 397 | 88 | ||
| Morgan 2009c | I: Internet weight loss program; information session and program booklet | Total: 136 | 34 | 34 | 34 | 28 | 82 |
| (weight loss study) | C: information session (modified) and program booklet | 31 | 31 | 31 | 26 | 84 | |
| total: | 65 | 65 | 65 | 54 | 83 | ||
| Morgan 2011 | I: Internet weight loss program; information session and program booklet; group‐based financial incentives | Total: 127 | 65 | 65 | 65 | 54 | 83 |
| (weight loss study) | C: wait list | 45 | 45 | 45 | 36 | 80 | |
| total: | 110 | 110 | 110 | 89 | 81 | ||
| Schroder 2010 | I1: computer‐assisted intervention and interactive software | Total: 94 | 30 | 30 | 30 | 24 | 80 |
| (weight loss study) | I2: computer‐assisted intervention and interactive software; in‐person self management group training | 31 | 31 | 31 | 26 | 84 | |
| C: wait list | 30 | 30 | 30 | 26 | 87 | ||
| total: | 91 | 91 | 91 | 76 | 84 | ||
| Svetkey 2008 | I1: in‐person support | 1685 in weight loss program 653 excluded from weight maintenance trial Total: 1685 |
342 | ‐ | 341 | 320 | 94 |
| (weight maintenance study) | C1: continue to practice principles during weight loss intervention | 348 | 347 | 323 | 93 | ||
| C2: printed life‐style guidelines; meeting with study interventionist | 342 | 341 | 321 | 94 | |||
| total: | 1032 | 1029 | 964 | 93 | |||
| Tate 2001d | I: Internet behavioral therapy | Total: 114 | 45 | 45 | 45 | 33 | 73 |
| (weight loss study) | C: Internet educational intervention | 46 | 46 | 46 | 32 | 70 | |
| total: | 91 | 91 | 91 | 65 | 71 | ||
| Tate 2003 | I: Internet weight loss program and weekly e‐mail behavioral counseling | 273 screened 92 ineligible 145 invited to orientation 37 did not attend 108 attended 16 excluded Total: 273 |
46 | 46 | 46 | 38 | 83 |
| (weight loss study) | C: Internet weight loss program | 46 | 46 | 46 | 39 | 85 | |
| total: | 92 | 92 | 92 | 77 | 84 | ||
| Tate 2006 | I1: Internet weight loss program and weekly e‐mail behavioral counseling | 553 screened 239 ineligible 314 invited to orientation 212 consented Total: 553 |
61 | 61 | 61 | 44 | 72 |
| (weight loss study) | I2: Internet weight loss program and weekly automated computer feedback | 64 | 64 | 64 | 52 | 81 | |
| C: Internet weight loss program | 67 | 67 | 67 | 59 | 88 | ||
| total: | 192 | 192 | 192 | 155 | 81 | ||
| Threlfall 1984 | I: weight loss manual plus computer‐based lessons | Total: 119 | 38 | 38 | not done | 31 | 82 |
| (weight loss study) | C: weight loss manual | 38 | 38 | 32 | 84 | ||
| total: | 76 | 76 | 63 | 83 | |||
| Webber 2008 | I: Internet weight loss program and online chat group sessions | 145 screened 52 ineligible 93 invited to orientation 25 did not attend 68 attended Total: 66 |
33 | 33 | 32 | 32 | 97 |
| (weight loss study) | C: Internet weight loss program | 33 | 33 | 32 | 32 | 97 | |
| total: | 66 | 66 | 64 | 64 | 97 | ||
| Wing 2006e | I1: Internet weight maintenance program | Total: 648 | 104 | 104 | 104 | 101 | 97 |
| (weight maintenance study) | C1: continue to practice principles during weight loss intervention | 105 | 105 | 105 | 92 | 88 | |
| C2: quarterly newsletters | 105 | 105 | 105 | 98 | 93 | ||
| total: | 314 | 314 | 314 | 291 | 93 | ||
| Wylie‐Rosett 2001 | I1: computerized weight loss intervention and workbook | Total: 1041 | 236 | 236 | not done | 183 | 78 |
| (weight loss study) | I2: computerized weight loss intervention, workbook and staff consultation | 236 | 236 | 194 | 82 | ||
| C: workbook | 116 | 116 | 97 | 84 | |||
| total: | 588 | 588 | 588 | 81 | |||
| Total | all interventions | 2452 | 2134 | 87 | |||
| all controls | 1688 | 1497 | 89 | ||||
| all interventions and controls | 4140 | 3631 | 88 | ||||
| all weight maintenance studies: intervention | 552 | ||||||
| all weight maintenance studies: controls | 1051 | ||||||
| all weight maintenance studies: total | 1603 | ||||||
a Percentage follow‐up is for those who completed both the weight loss treatment and the weight maintenance trial. Attrition after six months of weight loss treatment was 18% and 24% over 18 months of weight loss followed by weight maintenance. Therefore the attrition from the weight maintenance segment was less than 20%.
b Five participants were excluded from ITT analysis due to pregnancy after randomization.
c Participants were followed to 12 months (separate publication). Follow‐up at 12 months was 71% and therefore we did not include the 12‐month data in this review.
d Authors stated that 65/91 (71%) participants had objective follow‐up data at all assessments. 77/91 (85%) completed baseline and 3‐month follow‐up, therefore 3‐month data were included in the review. 71/91 (78%) completed baseline and 6‐month follow‐up, therefore 6‐month data were not eligible for inclusion in the review. Data for physical activity and diet at three and six months were only presented for 60/91 (66%) of participants and therefore were not included in the review.
e Follow‐up varied across time points. Follow‐up was 96% at six months, 92% at 12 months, and 93% at 18 months.
Abbreviations C: control; I: intervention; ITT: intention‐to‐treat
Dealing with duplicate publications
In the case of duplicate publications and companion papers of a primary study, we tried to maximize yield of information by simultaneous evaluation of all available data. In cases of doubt, the original publication (usually the oldest version) was given priority.
Assessment of risk of bias in included studies
Two authors (KJT, LF) assessed each trial independently. Disagreements were resolved by consensus, or by consultation with a third party. We calculated interrater agreement for key bias indicators (e.g. allocation concealment, incomplete outcome data) using the kappa statistic (Cohen 1960). In cases of disagreement, the rest of the group was consulted and a judgement was made based on consensus.
We assessed risk of bias using the Cochrane Collaboration’s tool (Higgins 2009), which includes the following items.
Was the allocation sequence adequately generated?
Was the allocation adequately concealed?
Was knowledge of the allocated intervention adequately prevented during the study?
Were incomplete outcome data adequately addressed?
Were reports of the study free of suggestion of selective outcome reporting?
Was the study apparently free of other problems that could put it at a high risk of bias?
We judged risk of bias criteria as 'low risk', 'high risk' or 'unclear risk' and evaluated individual bias items as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009).
Measures of treatment effect
Dichotomous data
We expressed dichotomous outcomes (e.g. weight loss yes/no) as odds ratios (OR) or risk ratios (RR) with 95% confidence intervals (CI), where deemed clinically relevant and appropriate.
Continuous data
For continuous outcomes (e.g. weight) on the same scale, we calculated the weighted mean difference (MD) and 95% confidence intervals. We calculated pooled continuous outcomes from different scales used to measure the same underlying concept (e.g. different measures of physical activity) using the standardized mean difference (SMD) and 95% confidence intervals. We extracted outcomes as change from baseline when possible, otherwise we extracted outcomes at endpoint. We combined change and endpoint outcomes in the calculation of weighted mean differences if necessary, however we did not mix endpoint and change outcomes in calculation of standardized mean differences. Studies that reported outcomes using Imperial measures (pounds rather than kilograms, and inches rather than centimeters) had their results converted to the metric standard (kilograms and centimeters) prior to performing all analyses.
Unit of analysis issues
For cluster‐randomized trials which did not adjust for clustering in reporting their results, we followed the guidance in chapter 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009). We used an estimate of the intra class correlation coefficient (ICC) to calculate a design effect for each cluster‐randomized trial. The design effect was used to divide the sample size in the experimental and control groups for analyses using continuous data, and to divide the standard error for analyses using generic inverse variance data.
Dealing with missing data
We contacted the corresponding author of the study report to obtain any relevant missing data for key study characteristics (e.g. sample size) or weight outcomes. In cases where study participants were lost to follow‐up, and intention‐to‐treat analyses were conducted using baseline observation carried forward (BOCF) or other methods were used to impute the missing values, we used the imputed data for our primary analysis, and conducted a sensitivity analysis using available case data. When an individual study report used multiple methods of imputation, we used the data created using the most conservative method (e.g. BOCF for a weight loss trial). When statistics such as standard deviations were not present in the study report, we used the methods outlined in chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009) to calculate the missing statistics. Whenever possible, we used the procedures outlined in chapters 7 and 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009) to calculate change outcomes from extracted baseline and endpoint outcomes. When standard deviations were present for the baseline and endpoint measurements, but not for the mean change from baseline, we followed the procedures described in chapter 16.1.3.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009). We calculated the correlation coefficient from a similar study reporting standard deviations for baseline, endpoint and change values of the same variable (e.g. weight, BMI), and used the calculated correlation coefficient to impute the missing standard deviation for the change from baseline.
Assessment of heterogeneity
In the event of substantial clinical or methodological heterogeneity we did not combine study results in a meta‐analysis. We identified statistical heterogeneity by visual inspection of the forest plots, by using a standard Chi2 test and a significance level of α = 0.1, in view of the low power of this test, and by using the I2 statistic (Higgins 2002), where I2 values of 50% and more indicate a substantial level of heterogeneity (Higgins 2003; Higgins 2009). When substantial statistical heterogeneity was found, we attempted to determine potential reasons for it by examining individual study and subgroup characteristics.
Assessment of reporting biases
For analyses including at least 10 trials, we used funnel plots to assess for the potential existence of small study bias. In light of the many possible explanations for funnel plot asymmetry, we were cautious in our interpretation of the results (Lau 2006; Sterne 2001).
Data synthesis
We combined data from individual studies when the trials were sufficiently similar in terms of the intervention goal (weight loss or weight maintenance), the treatment (e.g. computer‐based intervention as a sole intervention, computer‐based intervention as an adjunct to another intervention), the control intervention (e.g. minimal or no intervention, intensive in‐person intervention), outcome measures (e.g. weight, BMI, waist circumference) and timing of outcome assessment (short‐term, medium‐term or long‐term). For pooled data, we calculated summary test statistics using a random‐effects effect model to account for expected heterogeneity between studies. If the I2 statistic was greater than or equal to 50%, we interpreted the summary measures of effect with caution, and investigated heterogeneity between trials.
Subgroup analysis and investigation of heterogeneity
We planned to carry out subgroup analyses if one of the primary outcome parameters demonstrated statistically significant differences between intervention groups.
We planned to carry out subgroup analyses on the following subgroups if data were available:
overweight and obese participants;
gender;
younger and older persons.
Sensitivity analysis
When data were available, we performed sensitivity analyses to explore the influence of the following factors on effect size:
repeating the analysis excluding unpublished studies;
repeating the analysis taking account of risk of bias, as specified above;
repeating the analysis excluding any very long or large studies to establish how much they dominate the results;
repeating the analysis excluding studies using the following filters: diagnostic criteria, language of publication, source of funding (industry versus other), country.
We also tested the robustness of the results by repeating the analysis using different methods for obtaining outcome data (available case data, ITT analysis using imputed data) and different statistical models (fixed‐effect model and random‐effects model).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies; and Table 3.
Results of the search
The electronic search strategies, weekly updates and additional searching of resources yielded 9195 abstracts retrieved between 14 April 2009 and 25 May 2011. From the potentially eligible 376 titles, we excluded 184 and retrieved 105 in full text for further examination. A total of 18 studies met the inclusion criteria and were included in the review. See Figure 1. The kappa statistic for trial selection was 0.61 (95% confidence interval (CI) is 0.42 to 0.80). The details of these studies are described in Characteristics of included studies.
Included studies
We included 18 studies (Bennett 2010; Cussler 2008; DeLucia 1988; Gabriele 2011; Harvey‐Berino 2002; Harvey‐Berino 2010; Hunter 2008; Morgan 2009; Morgan 2011; Schroder 2010; Svetkey 2008; Tate 2001; Tate 2003; Tate 2006; Threlfall 1984; Webber 2008; Wing 2006; Wylie‐Rosett 2001), of which 14 focused on weight loss and four focused on weight maintenance. In these 18 trials, 2452 people were in the computer treatment groups and 1688 people in one of the comparison groups. The earliest study report was a PhD dissertation (Threlfall 1984) from 1984, and the most recent study reports were published in 2011 (Gabriele 2011; Morgan 2011). All reports were in English, and with the exception of the PhD dissertation, all studies were published in peer‐reviewed journals. Aside from two trials which were conducted in Australia (Morgan 2009; Morgan 2011), all trials were conducted in the USA. All interventions were carried out in outpatient or community settings. Two studies (Harvey‐Berino 2010; Svetkey 2008) were multi‐centre trials. Study sample sizes ranged from 29 participants (DeLucia 1988) to 1032 participants (Svetkey 2008). Seven trials included fewer than 100 participants (DeLucia 1988; Morgan 2009; Schroder 2010; Tate 2001; Tate 2003; Threlfall 1984; Webber 2008), six trials included between 100 and 150 participants (Bennett 2010; Cussler 2008; Gabriele 2011; Harvey‐Berino 2002; Morgan 2011; Tate 2006), four trials included between 200 and 600 participants (Harvey‐Berino 2010; Hunter 2008; Wing 2006; Wylie‐Rosett 2001) and one trial included over 1000 participants (Svetkey 2008). As required by our review inclusion criteria, all studies collected follow‐up data from at least 80% of participants.
Design
Seventeen studies were randomized controlled trials (RCTs) and one study (Schroder 2010) was a quasi‐randomized controlled trial (quasi‐RCT). All studies were parallel‐arm trials in which individuals were allocated to study arms, with the exception of Cussler 2008 and Morgan 2011, in which groups were cluster‐randomized to parallel study arms.
Participants
There were a total of 4140 participants in the 18 trials. All trials were conducted in adults.
Two trials (Cussler 2008; Webber 2008) included solely women and two trials (Morgan 2009; Morgan 2011) included solely men. The remaining 14 studies contained both men and women. Across all participants 27% were men and 73% were women. In the trials which included both men and women (3759 participants in total) the gender percentages were 26% men and 74% women.
Most inclusion criteria were based on body mass index (BMI). Participants in Wylie‐Rosett 2001 had a BMI of at least 25 kg/m2, or a BMI of at least 24 with at least one risk factor for cardiovascular disease, and Schroder 2010 included people with a BMI ≥ 27 kg/m2. Hunter 2008 included participants with a BMI of ≥ 25 for women and BMI ≥ 27.5 for men. BMI ranges for participants in the other studies were: 25 to 36 kg/m2 (Tate 2001), 25 to 37 kg/m2 (Morgan 2009), 25 to 40 kg/m2 (Gabriele 2011; Morgan 2011; Webber 2008), 25 to 50 kg/m2 (Harvey‐Berino 2010), 27 to 40 kg/m2 (Tate 2003; Tate 2006) and 30 to 40 kg/m2 (Bennett 2010). Study participants in the DeLucia 1988 trial were least 10 lb overweight. The Threlfall 1984 study included participants who had a body weight of at least 10% over the midpoint of the desired weight range on the Metropolitan Life Insurance Company table of recommended weights based on gender, height and body frame size.
In three of the four included weight maintenance trials, participants met BMI criteria at the beginning of the weight loss segment of the study. Participants in Cussler 2008 had a BMI of 25 to 38 kg/m2 and participants in Harvey‐Berino 2002 had a BMI of 25 kg/m2 or greater. Participants in Svetkey 2008 had BMIs of 25 to 40 kg/m2 at the beginning of weight loss and had lost at least 4 kg during the weight loss phase of the study. In the fourth weight maintenance trial (Wing 2006), participants had to have lost at least 10% of their body weight during the previous two years to qualify for study entry.
Interventions
We analyzed studies focusing on interventions for weight loss and studies focusing on interventions for weight maintenance separately. The rationale for this was that, although the practices that contribute to weight loss and weight loss maintenance are hypothesized to be the same (Rothman 2000; Rothman 2009), the rates of weight change are very different in weight loss versus weight loss maintenance studies, making them difficult to combine statistically. Rates of weight loss are rapid in the initial six months, after which point a significantly slower process of weight regain typically occurs (Franz 2007). Most studies that focus on weight loss maintenance enroll people after the period of most rapid weight regain (months six to 12), so that the rate of regain in those studies is, on average, even slower. For example, in Foster behavioral treatment produces weight loss of approximately 10 kg during the first six months of treatment (Foster 2005), yet a recent weight loss maintenance study by Perri and colleagues observed a weight regain of only 3.7 kg in the control group over 12 months (Perri 2008). This different rate of weight change suggests that weight loss and weight loss maintenance interventions need to be considered separately. Each study included in this review tested the effect of a computer‐based intervention for either weight loss or weight maintenance, with the exception of Hunter 2008, which began by focusing on weight‐gain prevention in overweight individuals but shifted, in response to participant motivations for participating in the trial, to a focus on weight loss. We classified Hunter 2008 as a weight‐loss trial in this review.
A total of 14 studies with 2537 participants assessed the effectiveness of interactive computer‐based interventions on achievement of weight loss (Bennett 2010; DeLucia 1988; Gabriele 2011; Harvey‐Berino 2010; Hunter 2008; Morgan 2009; Morgan 2011; Schroder 2010; Tate 2001; Tate 2003; Tate 2006; Threlfall 1984; Webber 2008; Wylie‐Rosett 2001). The duration of the intervention ranged from 10 weeks to 12 months (see Appendix 4).
Seven of the weight loss studies (Bennett 2010; Hunter 2008; Morgan 2009; Morgan 2011; Schroder 2010; Threlfall 1984; Wylie‐Rosett 2001) compared an interactive computer‐based intervention with a minimal or no treatment control condition. In two trials (Threlfall 1984; Wylie‐Rosett 2001) the control condition was a weight loss workbook or manual, in two trials (Bennett 2010; Morgan 2009) the control condition was a booklet or leaflet, in one trial (Hunter 2008) the control condition was usual care on a military base, and in two trials (Morgan 2011; Schroder 2010) the control condition was a wait list. Two of the studies comparing an interactive computer‐based intervention with a minimal or no treatment control condition (Schroder 2010; Wylie‐Rosett 2001) were three‐arm trials, in which a third treatment arm supplemented the computer‐based intervention with an in‐person treatment component. Both studies reported that there was not a significant difference between the two computer intervention arms. We therefore combined the two computer intervention arms for our main analyses, and conducted sensitivity analyses omitting the arms with the in‐person treatment component.
One weight loss study (Harvey‐Berino 2010) compared an interactive computer‐based intervention with an in‐person intervention. This study randomized participants to one of three treatment conditions: Internet‐based treatment with access to a website and weekly online chats, in‐person treatment with paper materials and a weekly in‐person group session, and a hybrid condition which was Internet‐based but in which in‐person group sessions supplanted some of the weekly online chats. We compared the Internet‐based treatment to each of the comparison treatments (in‐person and hybrid) separately.
Five of the weight loss studies (Gabriele 2011; Tate 2001; Tate 2003; Tate 2006; Webber 2008) evaluated the effect of an interactive computer‐based intervention as an adjunct or supplement to an Internet‐delivered weight‐loss intervention. In Gabriele 2011, all participants received an Internet‐based weight loss program with weekly lessons and feedback delivered by e‐mail. Participants were randomized to one of three groups: no individualized support, directive e‐mail coaching or non‐directive e‐mail coaching. We analyzed the directive and non‐directive e‐mail coaching separately because they were based upon different theoretical approaches to counseling and the trial found important differences in the efficacy of the two conditions. In Tate 2001, following an in‐person one‐hour behavioral weight loss session, participants were randomized to either online education or online behavior therapy. The online education group received online information about weight loss, and was also encouraged to use the online resources to track their diet and exercise. The interactive computer intervention group submitted individual weight, calorie and fat intake, exercise data and questions or comments online, and also had access to an electronic bulletin board. A behavioral therapist e‐mailed individualized feedback to the interactive group participants weekly. In Tate 2003, the control group submitted their weight and received weight loss information online, while an interactive intervention group submitted weight, calorie and fat intake, exercise information, and any comments or questions and received e‐mailed feedback from investigators. In Tate 2006, all intervention groups were instructed in the use of an interactive website. The control group received no further feedback. Two additional intervention groups received weekly feedback that was either 1) e‐mail counseling from a human weight loss counselor or 2) tailored feedback from an automated computer program. We analyzed the e‐mail counseling and automated feedback both combined and separately. In Webber 2008, both the intervention and control groups were assigned to 16 weeks of online self monitoring, but the intervention group participated in weekly online group chats in addition to the online self monitoring. We analyzed the e‐mail counseling trials (Gabriele 2011; Tate 2001; Tate 2003; Tate 2006) and the group chats trial (Webber 2008) separately.
One weight loss study (DeLucia 1988) evaluated the effect of an interactive computer‐based intervention as an adjunct to an in‐person weight loss intervention. All study participants received a standard in‐person behavioral intervention program (Ferguson 1975) from counselors. There were a total of three treatment conditions: the behavioral intervention alone, and the behavioral intervention plus one of two different nutritional software programs. The study reported that there was no difference between the effects of the two computer intervention arms, and we therefore combined these two intervention arms for our analyses.
Four studies (Cussler 2008; Harvey‐Berino 2002; Svetkey 2008; Wing 2006) with a total of 1603 participants assessed the effectiveness of interactive computer‐based interventions in maintenance of weight loss. The duration of the intervention ranged from 12 months to 30 months (see Appendix 4). Three of these studies (Cussler 2008; Harvey‐Berino 2002; Svetkey 2008) began with a weight loss intervention, randomly assigned participants to computer‐based or a control intervention for weight maintenance, and then followed the participants for at least 12 months to assess the amount of weight regain. The fourth study (Wing 2006) recruited participants who had lost at least 10% of their body weight during the last two years, randomly assigned the participants to computer‐based or control intervention groups, and followed them for 18 months.
Three of the weight maintenance studies (Cussler 2008; Svetkey 2008; Wing 2006) compared an interactive computer‐based intervention with a minimal or no treatment control condition, such as printed newsletters. In the Cussler 2008 study staff did not counsel the control group participants, although the participants could continue to meet in the groups they had formed during the preceding weight loss segment of the trial. In Svetkey 2008 and Wing 2006, control group participants were given printed guidelines or printed newsletters. The computer‐based interventions in these studies were an interactive website with occasional chat‐room sessions and e‐mail responses to questions (Cussler 2008), unlimited access to an interactive website and online bulletin board plus e‐mail or telephone reminders for participants who did not log on (Svetkey 2008), and access to an interactive website plus online group meetings and message boards (Wing 2006).
Three studies (Harvey‐Berino 2002; Svetkey 2008; Wing 2006) compared a computer‐based intervention to a face‐to‐face treatment control condition. The computer‐based interventions were biweekly Internet chat sessions with e‐mails from therapists on non‐chat weeks, combined with web‐based data entry (Harvey‐Berino 2002), an interactive website plus online bulletin board and e‐mail reminders (Svetkey 2008), and an interactive website plus online group meetings and message boards (Wing 2006). Each of the three studies in this group compared the computer‐based intervention to a minimal (defined as contact monthly or less often) face‐to‐face treatment intervention. One study (Harvey‐Berino 2002) also compared the computer‐based intervention to a frequent (defined as contact more often than monthly) face‐to‐face treatment intervention. The minimal face‐to‐face intervention in Wing 2006 was weekly meetings for the first month (only) of the trial, then monthly meetings until the end of follow‐up at 18 months. The minimal face‐to‐face intervention in Svetkey 2008 was monthly telephone support, with in‐person meetings substituted every four months. The minimal face‐to‐face intervention in Harvey‐Berino 2002 was monthly in‐person contact for the first six months of weight maintenance, followed by no contact from month seven to 12. The frequent face‐to‐face intervention in Harvey‐Berino 2002 was in‐person meetings every two weeks for the entire 12 months of weight maintenance, supplemented by phone calls from a therapist during non‐meeting weeks and regular submission of self monitoring data by postal mail.
Outcomes
All studies included weight outcomes in kilograms or pounds of body weight. The inclusion of other outcomes varied between studies, and there was no other outcome found in all studies. Weight, height (if assessed for purposes of calculating BMI) and waist circumference (if assessed) were measured by study personnel. When dietary intake was measured, it was always by means of dietary questionnaires completed by the participants. When physical activity was measured, it was by means of physical activity questionnaires completed by the participants, with the exception of Morgan 2009, in which physical activity was measured using pedometers, and Svetkey 2008, in which physical activity was measured by accelerometry.
Excluded studies
Nineteen studies were not randomized or quasi‐randomized controlled trials and so we excluded them on the grounds of study design (Burnett 1984; Cange 2008; Collinson 2011; Cousineau 2008; Faghri 2008; Haugen 2007; James 2001; Joo 2010; Liou 2006; McHugh 2008; McTigue 2009; Nieto 2010; Park 2009; Petersen 2008; Riva 2000; Thurston 1991; Touger‐Decker 2010; van der Mark 2009; Verheijden 2007).
There were 23 studies which we excluded due to the participant dropout rate being higher than specified in our inclusion criteria (Booth 2008; Brantley 2008; Burnett 1992; Carr 2008; Castelnuovo 2011; Gold 2007; Heetderks‐Cox 2001; Jones 1997; Kerr 2008; McConnon 2007; McDoniel 2010; Micco 2007; Mobley 2006; Pullen 2008; Rothert 2006; Ryan 2010; Sartor 1991; Shay 2009; Turnin 2001; van Wier 2009; Wing 2009; Womble 2004). Studies which we excluded for other reasons were either because none or not all participants were overweight or obese (16 in total: Anderson‐Bill 2011; Carr 2009; Cook 2007; De Bourdeaudhuij 2007; Dekkers 2011; Gow 2010; Herrick 2009; Kroeze 2008; Kroeze 2008a; Marcus 2007; Smeets 2007; Southard 2003; Vandelanotte 2005; Vandelanotte 2008; Werkman 2010; Winett 2007) and in one case because the focus was diabetes management (Kalten 2000), and in another because the focus was treatment of binge eating disorder (Carrard 2011).
Thirteen studies were excluded on the grounds that the interventions were not interactive or the interactive component of the intervention was not computer‐based (Adachi 2007; Campbell 2002; Christian 2011; Cook 2007; Foree‐Gavert 1980; Jacobs 2010; Kremers 2005; Kristal 2000; Lohof 2007; Polzien 2007; Sbrocco 1999; Tanaka 2010; Vandelanotte 2008). A further three were not computer‐based (Fitzgibbon 1995; Harvey‐Berino 1998; Weinstock 1998); five studies involved hand‐held or pocket computer‐based interventions (Agras 1990; Burke 2011; Sbrocco 2005; Taylor 1991; Yon 2007). Four studies had interventions which were designed to promote physical activity rather than specifically to increase weight loss (Bischoff 2010; Carr 2009; Smith 2009; Steele 2007) and one study compared two interactive computer‐based interventions (Webber 2010).
Finally one study had to be excluded because we were unable to contact the author to obtain the necessary information for data extraction (Harvey‐Berino 2002a). Another study by the same author was excluded from this review because the study did not meet the 80% follow‐up inclusion criterion at 12 months, there were no extractable data for earlier follow‐up points, and we were unable to contact the author to obtain data for the earlier follow‐up time points (Harvey‐Berino 2004).
Two potential studies were identified but are awaiting classification. One is an ongoing study (Harvey‐Berino NCT01232699) and one is a conference abstract which does not give sufficient information to determine eligibility and whose author could not yet be contacted for further information (Magnusdottir 2010).
Risk of bias in included studies
The methodological quality of included studies is described in Characteristics of included studies. Interrater agreement for risk of bias assessment was measured as 0.51 using the kappa statistic (Cohen 1960). This measure relates only to the 15 included studies retrieved from the original search results; the measure was not recalculated to incorporate the three studies from the updated search in 2011. See Figure 2 ('Risk of bias' graph) and Figure 3 ('Risk of bias' summary).
2.
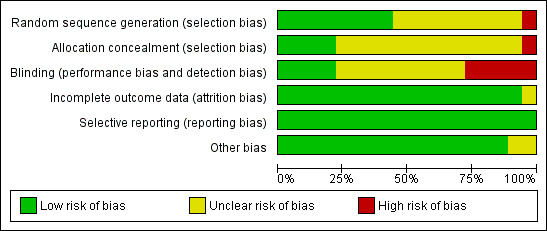
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
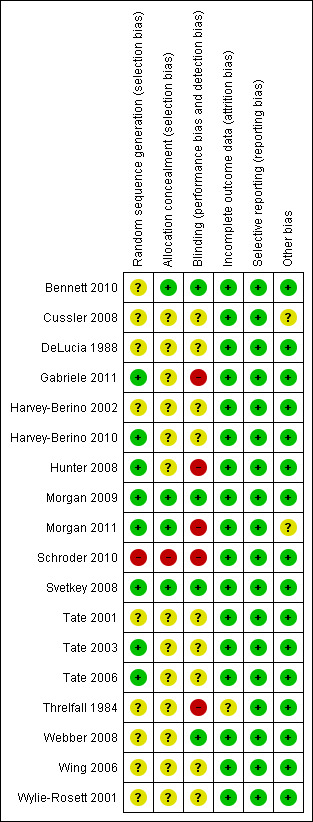
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Three trials (Morgan 2009; Morgan 2011; Svetkey 2008) clearly reported adequate methods of randomization and allocation concealment, and a further five trials (Gabriele 2011; Harvey‐Berino 2010; Hunter 2008; Tate 2003; Tate 2006) adequately randomized participants but were unclear about whether allocation was adequately concealed. One trial (Bennett 2010) did not describe the method of randomization, but did state that assignments were enclosed in nontransparent envelopes, and we therefore judged that allocation was adequately concealed. Methods of both randomization and allocation concealment were either not described or unclear in eight trials (Cussler 2008; DeLucia 1988; Harvey‐Berino 2002; Tate 2001; Threlfall 1984; Webber 2008; Wing 2006; Wylie‐Rosett 2001). One trial (Schroder 2010) was a quasi‐randomized controlled trial which assigned every third participant, hence investigators and participants could potentially have foreseen assignments and we judged that allocation was not adequately concealed.
Blinding
None of the following studies stated whether any of the parties were blinded to treatment allocation: Cussler 2008; DeLucia 1988; Harvey‐Berino 2010; Tate 2003; Threlfall 1984; Wing 2006; Wylie‐Rosett 2001.
Bennett 2010 stated that research staff collecting evaluation data were blinded to randomization status. In Gabriele 2011 participants were reported to be blinded to treatment condition. Hunter 2008 stated that the study could not be blinded. The Morgan 2009 trial reported that participants were blind to group allocation at baseline assessment and that assessors were blinded to treatment allocation at all points. Morgan 2011 stated that participants and assessors were blind to treatment allocation at baseline, but did not report whether they were still blinded at follow‐up. Research team members were blind to the type of intervention assignments in the Schroder 2010 study. In Svetkey 2008 and Webber 2008 outcome measurements were taken by staff members masked to treatment assignment. The Tate 2006 study reported that non‐intervention staff weighed participants at baseline and at three and six months, but there is no specific statement of whether or not they were blinded. Participants were aware of randomization assignment, but their knowledge of the other interventions is unclear. It was stated that human e‐counselors were blinded to the algorithms used to program the automated feedback counselor, but it is unclear whether they were aware of assignment of participants across all three groups.
Incomplete outcome data
All included studies had a loss to follow‐up of less than 20% as specified in the inclusion criteria for the review.
We assessed attrition rates, noted whether reasons for dropout were given, and whether methods of handling missing data were stated.
DeLucia 1988 and Threlfall 1984 presented data for completers only and did not use any methods to handle missing data.
All other studies used an intention‐to treat analysis. Bennett 2010; Cussler 2008; Gabriele 2011; Harvey‐Berino 2002; Harvey‐Berino 2010; Hunter 2008; Morgan 2011; Tate 2001; Tate 2003 and Tate 2006 all used a baseline observation carried forward approach (BOCF). Tate 2006 also used last observation carried forward, expectation maximization and regression to impute missing values, and stated that the pattern of statistical significance using observed data and imputed data was identical with all methods. Morgan 2009 used linear mixed models to assess the primary analysis of effects of losses to follow‐up. Schroder 2010 replaced missing data points with pre‐intervention scores. Svetkey 2008 used multiple imputation to replace missing end‐of‐study weights, missing interim weights and other measures (apart from weights missing due to participant death). Wing 2006 assumed all dropouts regained 2.3 kg or more for their analysis. Wylie‐Rosett 2001 reported that the study completers did not differ significantly from the dropouts with respect to baseline characteristics, but did not otherwise state how missing data were handled.
Selective reporting
Six of the included studies had protocols: Harvey‐Berino 2010; Morgan 2009; Morgan 2011; Svetkey 2008; Tate 2006; Wing 2006. The primary outcome in the protocol was the same as the primary outcome in the methods section for each of these studies. Based on the available information all the trials appear to be free of selective reporting.
Other potential sources of bias
We assessed studies for any additional potential sources of bias in studies. These included: discrepancies between pre‐specified questions/entries in study protocols and the published reports; treatment variation or additional treatment in the intervention group; differences in groups at baseline; conflicts of authors and funding sources. None of the included studies appeared to have any other potential sources of bias.
Effects of interventions
The primary outcomes of this review were changes in body weight, BMI, waist circumference and health‐related quality of life. Secondary outcomes were changes in physical activity or diet, relative cost‐effectiveness of interventions and adverse effects.
Weight loss studies
Computer‐based intervention versus minimal treatment control for weight loss
Seven studies (Bennett 2010; Hunter 2008; Morgan 2009; Morgan 2011; Schroder 2010; Threlfall 1984; Wylie‐Rosett 2001) with a combined total of 1367 participants included data on the effect of computer‐based interventions versus a minimal intervention or no treatment upon weight loss. Two of the trials (Schroder 2010; Wylie‐Rosett 2001) were three‐arm studies in which one of the computer‐based intervention arms was supplemented with an in‐person intervention. In all analyses incorporating these studies, we conducted main analyses by combining the two computer‐based intervention arms and then carried out subgroup analyses in which the study arm supplemented with in‐person contact was excluded.
Primary outcomes
Weight loss outcomes
After 10 to 14 weeks of treatment, the five individual trials with weight loss measurements at three months (Bennett 2010; Morgan 2009; Morgan 2011; Schroder 2010; Threlfall 1984) showed that participants in the computer‐based intervention groups lost more weight than participants in the minimal intervention control groups (mean difference (MD) ‐2.5 kg (95% confidence interval (CI) ‐3.4 to ‐1.6), P < 0.00001; 430 participants; five trials; Analysis 1.1: primary analysis 1.1.1. The heterogeneity in this analysis (I2 = 44%) was unsurprising given the heterogeneity of interventions and comparisons. When we omitted the sole quasi‐randomized trial (Schroder 2010), which was also the only trial that included an ongoing in‐support arm as one component of the computer intervention, results were again similar to the initial analysis (MD ‐2.8 kg (95% CI ‐3.7 to ‐1.9), P < 0.00001; 339 participants; four trials; Analysis 1.1: sensitivity analysis 1.1.2), although heterogeneity remained moderate (I2 = 31%). When we repeated the analysis omitting only the ongoing in‐person support arm from the quasi‐randomized trial, results were similar to the initial comparison (MD ‐2.5 kg (95% CI ‐3.4 to ‐1.6), P < 0.00001; 399 participants; five trials; Analysis 1.1: sensitivity analysis 1.1.3), and heterogeneity was intermediate (I2 = 39%). When we omitted the sole trial conducted in a workplace setting, which was also a cluster‐randomized trial, and one of the two trials conducted in men only (Morgan 2011), from the analysis, weight loss was slightly less (MD ‐2.2 kg) and heterogeneity was greatly decreased (I2 = 0%) (Analysis 1.1: sensitivity analysis 1.1.4).
1.1. Analysis.
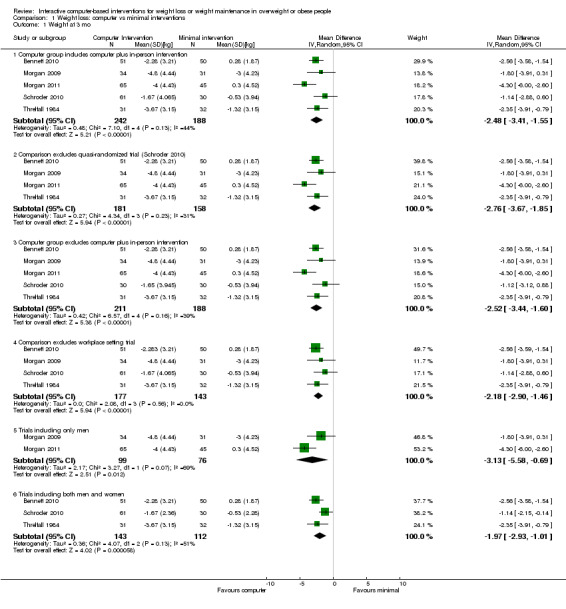
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 1 Weight at 3 mo.
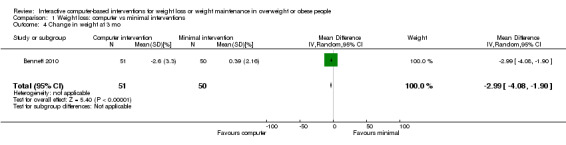
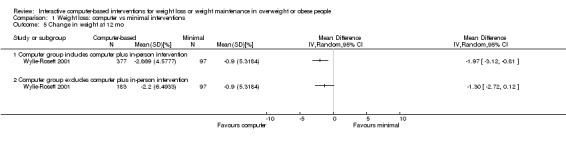
Two trials presented weight loss outcomes at six months (Hunter 2008; Morgan 2009). After six months of treatment, participants in the computer‐based intervention lost more weight than participants in the control intervention (MD ‐1.5 kg (95% CI ‐2.1 to ‐0.9); P < 0.00001; 511 participants; two trials; Analysis 1.2) (Figure 4).
1.2. Analysis.
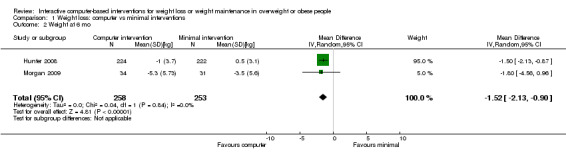
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 2 Weight at 6 mo.
4.
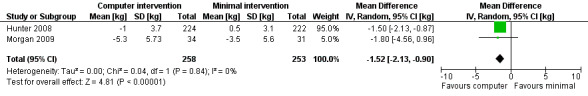
Forest plot of comparison: 1 Weight loss: computer vs minimal intervention, outcome: 1.2 Weight at 6 mo [kg].
Only one trial (Wylie‐Rosett 2001) examined weight loss outcomes at 12 months of follow‐up. After 12 months of treatment, participants in the computer‐based intervention lost more weight than participants in the control intervention (MD ‐1.8 kg (95% CI ‐3.1 to ‐0.5); P = 0.009; 474 participants; one trial; Analysis 1.3: primary analysis 1.3.1). This trial also contained an intervention arm with an in‐person component, and when that arm was excluded from the comparison, the effect was smaller and no longer statistically significant (MD ‐1.1 kg (95% CI ‐2.6 to 0.3); P = 0.12; 280 participants; one trial, Analysis 1.3: sensitivity analysis 1.3.2).
1.3. Analysis.
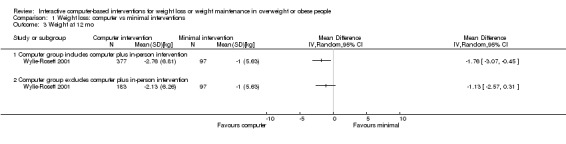
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 3 Weight at 12 mo.
Results were similar when percent weight lost and change in BMI rather than change in kilograms body weight were the weight‐related outcomes. In the one study reporting percent weight loss at three months (Bennett 2010), participants in the computer intervention lost 3% more body weight (or approximately 2.5 kg) compared to participants in the control group (MD ‐3.0% (95% CI ‐4.1 to ‐1.9); P < 0.00001; 101 participants, one trial, Analysis 1.4). In the single study reporting percent weight loss at 12 months (Wylie‐Rosett 2001), participants in the computer intervention lost a greater percentage of body weight than participants in the control group (MD ‐2.0% (95% CI ‐3.1 to ‐0.8); P = 0.0008; 474 participants; Analysis 1.5; primary analysis 1.5.1), although this effect was smaller and no longer statistically significant when participants receiving additional in‐person consultations were excluded from the analysis (MD ‐1.3% (95% CI ‐2.7 to 0.1); P = 0.07; 280 participants; Analysis 1.5: sensitivity analysis 1.5.2).
1.4. Analysis.
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 4 Change in weight at 3 mo.
1.5. Analysis.
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 5 Change in weight at 12 mo.
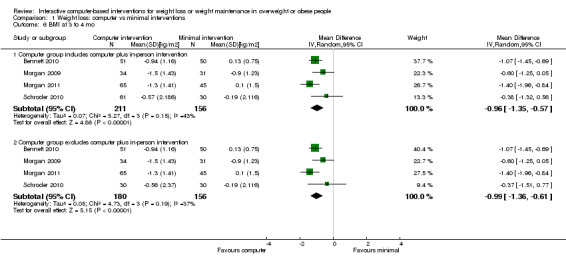
In the trials reporting BMI outcomes at three months, there was a larger decrease in BMI among participants in the computer intervention groups (MD ‐1.0 kg/m2 (95% CI ‐1.4 to ‐0.6), P < 0.00001; 367 participants; four trials; Analysis 1.6; primary analysis 1.6.1). When intervention participants receiving some in‐person contacts were excluded from the analysis, the mean difference in percentage weight lost remained similar (MD ‐1.0 kg/m2 (95% CI ‐1.4 to ‐0.6); P < 0.00001; 336 participants; four trials; Analysis 1.6; sensitivity analysis 1.6.2). At six months the mean difference in BMI was smaller (MD ‐0.7 kg/m2 (95% CI ‐0.9 to ‐0.5); P < 0.00001; 464 participants; two trials; Analysis 1.7). At 12 months the mean difference was similar to that at six months (MD ‐0.6 kg/m2 (95% CI ‐1.1 to ‐0.1); P = 0.01; 474 participants; one trial; Analysis 1.8; primary analysis 1.8.1), although the difference was smaller and not statistically significant when intervention participants receiving supplementary in‐person contact were excluded from the analysis (MD ‐0.4 kg/m2 (95% CI ‐0.9 to 0.1), P = 0.14; 280 participants; one trial; Analysis 1.8: sensitivity analysis 1.8.2).
1.6. Analysis.
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 6 BMI at 3 to 4 mo.
1.7. Analysis.
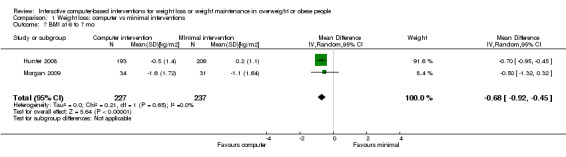
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 7 BMI at 6 to 7 mo.
1.8. Analysis.
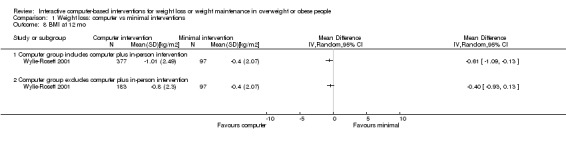
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 8 BMI at 12 mo.
Waist circumference outcomes
Five studies (Bennett 2010; Hunter 2008; Morgan 2009; Morgan 2011; Wylie‐Rosett 2001) with a combined total of 1200 participants included data on the effect of computer‐based interventions versus a minimal or no treatment intervention upon waist circumference. At three months, the pooled analysis favored the computer intervention group (MD ‐3.0 cm (95% CI ‐6.2 to 0.3); P = 0.07; 276 participants; three trials; Analysis 1.9; primary analysis 1.9.1). This analysis was extremely heterogenous (I2 = 86%), due to the inclusion of the Morgan 2011 trial, which displayed a mean difference in waist circumference that was almost three times greater than that seen in any of the other trials. When we removed the Morgan 2011 trial from the meta‐analysis, the pooled estimate of effect was smaller (MD ‐1.4 cm (95% CI ‐3.1 to 0.2); P = 0.08; 166 participants; two trials; Analysis 1.9: sensitivity analysis 1.9.2). At six months the computer intervention group had a greater decrease in waist measurement (MD ‐1.7 cm (95% CI ‐2.5 to ‐0.9); P < 0.00001; 464 participants; two trials; Analysis 1.10) but this difference decreased and was not statistically significant at 12 months (MD ‐0.9 cm (95% CI ‐2.2 to 0.5); P = 0.20; 474 participants; one trial; Analysis 1.11).
1.9. Analysis.
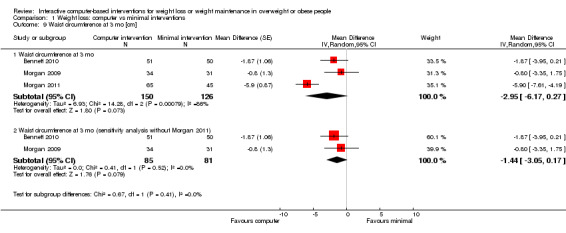
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 9 Waist circumference at 3 mo [cm].
1.10. Analysis.
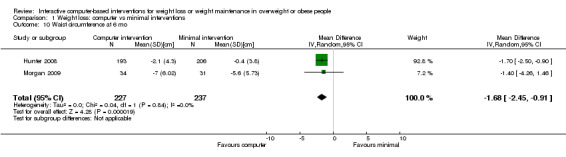
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 10 Waist circumference at 6 mo.
1.11. Analysis.
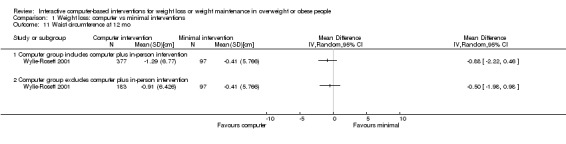
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 11 Waist circumference at 12 mo.
Health‐related quality of life outcomes
No study included data on health‐related quality of life outcomes.
Secondary outcomes
Dietary outcomes
Four studies (Hunter 2008; Morgan 2009; Morgan 2011; Wylie‐Rosett 2001) with a combined total of 1099 participants included data on the effect of computer‐based interventions versus a minimal or no treatment intervention upon diet‐related outcomes. Diet‐related outcomes were generally expressed as kilocalories (kcal) per day. There were no outcomes examined at the same time point in more than one study, therefore we performed no meta‐analyses.
In one study (Morgan 2009) participants in the computer intervention arm decreased their caloric intake more than participants in the control arm at the three‐month follow‐up (MD ‐269 kcal/day (95% CI ‐592 to 54); P = 0.1; 65 participants; Analysis 1.12) and this difference increased and became statistically significant at the six‐month follow‐up (MD ‐421 kcal/day (95% CI ‐799 to ‐42); P = 0.03; 65 participants; Analysis 1.13). A later study by the same investigators (Morgan 2011) observed that the computer intervention arm had a greater decrease in self reported intake of cola and other soda drinks than did the control group, but did not report data on overall energy intake. In a third study (Wylie‐Rosett 2001), which followed participants to 12 months, participants in the control arm decreased their caloric intake slightly more than participants in the computer intervention arm at 12 months follow‐up, although the difference was small and not significant at P < 0.05 for the analysis including all participants (MD 94 kcal/day (95% CI ‐29 to 217); P = 0.14; 474 participants; Analysis 1.14; primary analysis 1.14.1) or for the analysis excluding intervention participants receiving in‐person intervention components (MD 115 kcal/day (95% CI ‐21 to 250); P = 0.14; 280 participants; Analysis 1.14; sensitivity analysis 1.14.2).
1.12. Analysis.
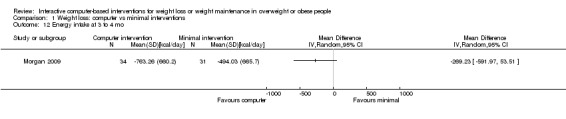
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 12 Energy intake at 3 to 4 mo.
1.13. Analysis.
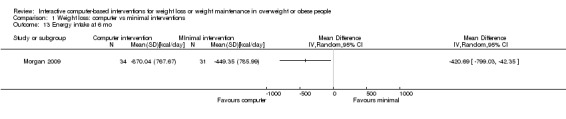
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 13 Energy intake at 6 mo.
1.14. Analysis.
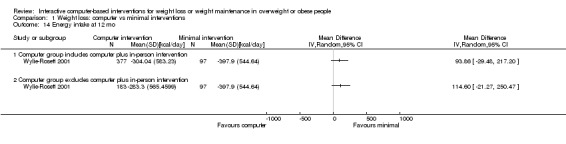
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 14 Energy intake at 12 mo.
The decrease in percent calories from fat at six months was slightly greater in the computer intervention arm than the control arm of one study (Hunter 2008) (MD ‐1.1% (95% CI ‐2.0 to ‐0.2); P = 0.02; 399 participants; Analysis 1.15). In a second study (Wylie‐Rosett 2001), the decrease in percent calories from fat at 12 months was not significantly different between intervention arms, whether all computer intervention participants were included in the analysis (MD 0.6% (95% CI ‐1.0 to 2.3); P = 0.45; 474 participants; Analysis 1.16; primary analysis 1.16.1) or those receiving in‐person treatment components were excluded from the analysis (MD 1.4% (95% CI ‐0.4 to 3.2); P = 0.12; 280 participants; one trial; Analysis 1.16; sensitivity analysis 1.16.1).
1.15. Analysis.
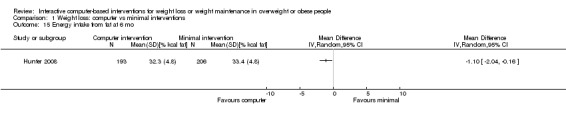
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 15 Energy intake from fat at 6 mo.
1.16. Analysis.
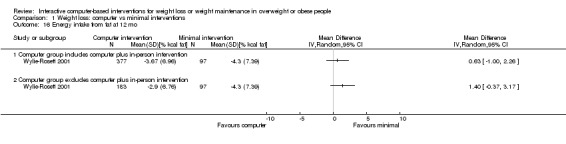
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 16 Energy intake from fat at 12 mo.
Dietary fibre intake was examined in a single study (Hunter 2008), which found that at six months participants in the computer intervention arm improved their fibre intake more than participants in the control arm, as measured by the dietary fibre score (Block 2000) (MD 1.3 (95% 0.5 to 2.1); P = 0.001; 399 participants; Analysis 1.17).
1.17. Analysis.
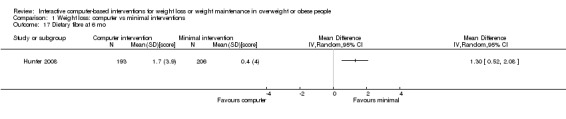
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 17 Dietary fibre at 6 mo.
Physical activity outcomes
Four studies (Hunter 2008; Morgan 2009; Morgan 2011; Wylie‐Rosett 2001) with a combined total of 1099 participants included data on the effect of computer‐based interventions versus a minimal or no treatment intervention upon physical activity‐related outcomes. Physical activity was measured as steps per day (Morgan 2009), total metabolic equivalent (MET) minutes (Hunter 2008), total log‐transformed MET minutes (Morgan 2011) and minutes walked continuously (Wylie‐Rosett 2001). At three months, the computer intervention group had greater mean log‐transformed MET minutes in one trial (MD 0.30 log‐transformed MET minutes (95% CI 0.0 to 0.6); P = 0.03; 71 participants; Analysis 1.18; analysis 1.18.1) but there was no difference in mean steps per day in a second trial (MD 208 mean steps/day (95% ‐1111 to 1527); P = 0.76; 65 participants; Analysis 1.18; analysis 1.18.1). There was no difference in physical activity change between intervention and control groups at six months (standardized mean difference (SMD) ‐0.0 mean steps/day (95% CI ‐0.2 to 0.1); P = 0.69; 464 participants; two trials; Analysis 1.19). There was also no difference in physical activity between computer and control groups at 12 months, whether all computer intervention participants were included (MD 0 minutes walked continuously (95% CI ‐3 to 3); P = 0.97; 474 participants; one trial; Analysis 1.20; primary analysis 1.20.1) or computer intervention participants with added in‐person contacts were excluded (MD 0 minutes walked continuously (95% CI ‐4 to 4); P = 1.00; 280 participants; one trial; Analysis 1.20; sensitivity analysis 1.20.2).
1.18. Analysis.
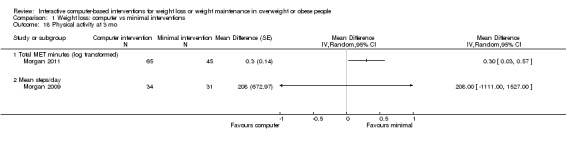
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 18 Physical activity at 3 mo.
1.19. Analysis.
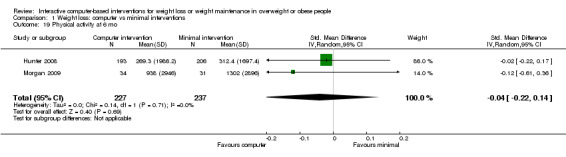
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 19 Physical activity at 6 mo.
1.20. Analysis.
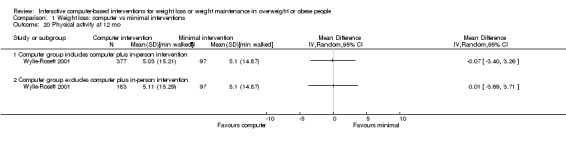
Comparison 1 Weight loss: computer vs minimal interventions, Outcome 20 Physical activity at 12 mo.
Cost‐effectiveness outcomes
Only two studies comparing computer‐based interventions to a minimal intervention addressed the cost‐effectiveness of the computer intervention (Threlfall 1984; Wylie‐Rosett 2001). The cost‐effectiveness of the intervention in the Hunter 2008 study was examined in a companion publication (Rasu 2010). Based on 2010 Euros, the intervention from Threlfall cost EUR 55.6 per participant and led to an average participant loss of 4.8% of body weight. The intervention from Wylie‐Rosett and colleagues cost EUR 38.6 per participant and led to an average participant loss of 4.0% of body weight. The intervention by Hunter and colleagues led to an increase in weight loss by approximately 2.1% for a cost of EUR 65.5 per participant.
Adverse effects outcomes
No study reported assessing adverse effects of the intervention.
Covariates
Adherence
Several trials (Bennett 2010; Hunter 2008; Morgan 2009; Morgan 2011; Wylie‐Rosett 2001) tested for and demonstrated statistically significant positive associations between amount of computer use, measured in a variety of ways, and amount of weight loss in the intervention group.
Computer‐based intervention versus in‐person treatment for weight loss
One study (Harvey‐Berino 2010) with a total of 481 participants assessed the effects of an interactive computer‐based intervention versus an in‐person intervention, versus an interactive computer‐based intervention with some in‐person contacts (hybrid intervention).
Primary outcomes
Weight loss outcomes
At the completion of the six‐month intervention, participants in the interactive computer‐based intervention group lost less weight than the participants in the in‐person intervention group (MD 2.1 kg (95% CI 95% CI 0.8 to 3.4) P = 0.002; 319 participants, one trial, Analysis 2.1; analysis 2.1.1). When the interactive computer‐based intervention group was compared to the hybrid intervention group, there was no statistically significant difference in weight loss (MD 0.2 kg (95% CI ‐1.0 to 1.4) P = 0.75; 323 participants; Analysis 2.1; analysis 2.1.2). Results were similar when percent weight change rather than kilograms change was the outcome (MD 2.2% (95% CI 0.9 to 3.5); P = 0.0007; 319 participants; Analysis 2.2; analysis 2.2.1) and (MD 0.3% (95% CI ‐0.9 to 1.5); P = 0.63; 323 participants; Analysis 2.2; analysis 2.2.2)).
2.1. Analysis.
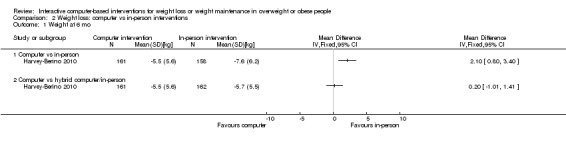
Comparison 2 Weight loss: computer vs in‐person interventions, Outcome 1 Weight at 6 mo.
2.2. Analysis.
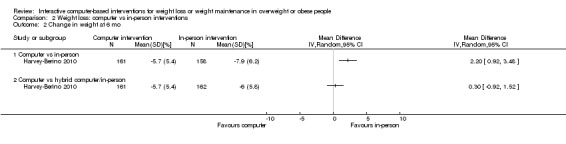
Comparison 2 Weight loss: computer vs in‐person interventions, Outcome 2 Change in weight at 6 mo.
Waist circumference outcomes
No waist circumference outcomes were reported.
Health‐related quality of life outcomes
No study included data on health‐related quality of life outcomes.
Secondary outcomes
Dietary and physical activity outcomes
Dietary and physical activity outcomes (kcal/day intake, kcal/day expenditure, % fat intake) were reported but we were unable to extract data from the trial report due to incomplete information on sample size for reported outcomes. The authors reported that there were no differences in dietary and physical activity effects between treatment conditions.
Cost‐effectiveness outcomes
Cost‐effectiveness for the Internet and in‐person arms of Harvey‐Berino 2010 was examined in a companion publication (Krukowski 2010). The Internet intervention cost EUR 288 per participant and led to a loss of 5.6% of body weight, while the in‐person intervention in the same trial cost EUR 549 to deliver and led to an average weight loss of 8.2% (Harvey‐Berino 2010; Krukowski 2010). Assuming a 50% weight regain at one year post‐treatment, Krukowski and colleagues calculated the cost per (discounted) year of life gained to be USD 2160 for the Internet intervention versus a hypothesized no treatment, no costs, no weight loss condition, and USD 7177 (80% CI USD 3055 to USD 60,291) per (discounted) year of life gained for the in‐person relative to the Internet intervention (Harvey‐Berino 2010; Krukowski 2010).
Adverse effects outcomes
No study reported assessing adverse effects of the intervention.
Covariates
Adherence
The proportion of online chats or in‐person groups attended was measured, as was the percent of weeks that participants submitted a journal (either online or paper, depending on the treatment group). There was not a statistically significant difference between intervention groups in attendance or journal submission, and the authors did not test for associations between attendance or compliance and weight loss within intervention groups.
Computer‐based intervention as adjunct to an Internet intervention
Five studies (Gabriele 2011; Tate 2001; Tate 2003; Tate 2006; Webber 2008) with a combined total of 441 participants assessed the effects of an interactive computer‐based intervention as an adjunct or supplement to an Internet intervention. Each study compared an Internet intervention with the same or similar intervention supplemented by a computer interaction. In Gabriele 2011; Tate 2001; Tate 2003 and Tate 2006, the interaction was individual e‐mail counseling, e‐coaching or automated computer feedback. In Webber 2008, the interaction was an online chat group. We analyzed the chat group trial separately from the trials using individualized e‐mail or automated feedback.
Gabriele 2011 compared both non‐directive e‐coaching and directive e‐coaching to minimal support. We initially combined the directive and non‐directive arms of the trial, compared the combined arms with the minimal support arm, and analyzed the Gabriele trial together with the Tate trials (Tate 2001; Tate 2006). All analyses incorporating the Gabriele trial showed high heterogeneity, however. Furthermore, the authors found more differences between the directive and non‐directive intervention arms than between either arm and the control intervention. We therefore redid the analyses combining the directive arm of the Gabriele trial with the Tate trials, as we believed that the counseling in the Tate trials was more similar to the directive intervention than to the non‐directive intervention.
Tate 2006 compared both e‐mail counseling and automated tailored computer feedback to an Internet program alone. In all analyses incorporating data from Tate 2006 we therefore conducted the main analysis by combining the two intervention arms of the trial (e‐mail counseling and automated feedback) and then conducted additional analyses for e‐mail counseling only and automated counseling only.
The intervention duration was 12 weeks in Gabriele 2011, 16 weeks in Webber 2008, six months in Tate 2001 and Tate 2006, and 12 months in Tate 2003. Because follow‐up in Tate 2001 was above 80% at three months follow‐up and less than 80% at six months follow‐up, only the data from the three‐month follow‐up were eligible for inclusion in this review.
Primary outcomes
Weight loss outcomes
Four trials (Gabriele 2011; Tate 2001; Tate 2006; Webber 2008) presented data on weight loss outcomes at three to four months, one trial (Tate 2006) presented data on weight loss at six months, and one trial (Tate 2003) presented data on weight loss at 12 months. At three months, participants receiving individualized feedback lost more weight than participants receiving no additional feedback (MD ‐2.1 kg (95% CI ‐2.9 to ‐1.4); P < 0.00001; 352 participants; three trials; Analysis 3.1; main comparison 3.1.1). The effect was slightly greater for e‐mail counseling (MD ‐2.3 kg (95% CI ‐3.1 to ‐1.5); P < 0.00001; 291 participants; three trials; Analysis 3.1; subgroup analysis 3.1.2) than for automated feedback (MD ‐1.8 kg (95% CI ‐3.2 to ‐0.5); P = 0.009; 128 participants; one trial; Analysis 3.1; subgroup analysis 3.1.3). Non‐directive e‐mail counseling did not appear effective (MD ‐0.3 kg (95% CI ‐2.2 to 1.7); P = 0.80; 69 participants; one trial; Analysis 3.1; secondary comparison 3.1.4).
3.1. Analysis.
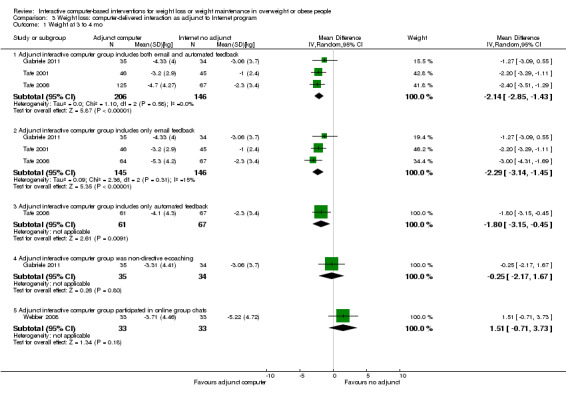
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 1 Weight at 3 to 4 mo.
In contrast to the effects seen with most forms of individualized counseling or feedback, participants receiving a group chat intervention in addition to online self monitoring (Webber 2008) lost less weight at four months than participants who did not receive the group chat intervention (MD 1.5 kg (95% CI ‐0.7 to 3.7); P = 0.18; 66 participants; one trial; Analysis 3.1; analysis 3.1.5). The group chat intervention was not followed past four months.
At six months, participants receiving individualized feedback lost more weight than participants not receiving such feedback (MD ‐2.4 kg (95% CI ‐4.1 to ‐0.8); P = 0.004; 192 participants; one trial; 192 participants; Analysis 3.2; main comparison 3.2.1), but this overall difference was composed of a large difference for e‐mail counseling (‐3.6 kg (95% CI ‐5.6 to ‐1.6); P = 0.0004; 131 participants; one trial; Analysis 3.2; subgroup analysis 3.2.2) and a smaller difference for automated feedback that was not statistically significant (MD ‐1.2 (95% CI ‐3.1 to 0.7); P = 0.21; 128 participants; one trial; Analysis 3.2; subgroup analysis 3.2.3). At 12 months, participants receiving individualized e‐mail feedback lost more weight than participants who did not (MD ‐2.4 kg (95% CI ‐4.8 kg to 0.0 kg); P = 0.05; 92 participants; one trial; Analysis 3.3).
3.2. Analysis.
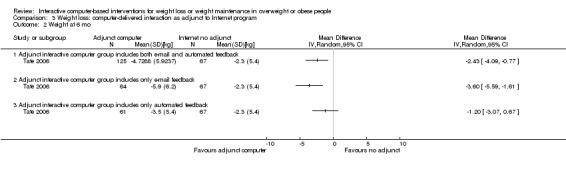
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 2 Weight at 6 mo.
3.3. Analysis.
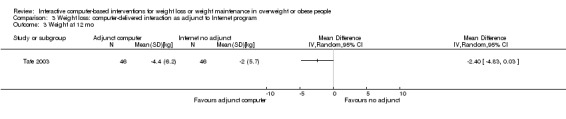
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 3 Weight at 12 mo.
Results were similar when percent weight lost and change in BMI rather than change in kilograms body weight were the weight‐related outcomes. At three months, participants receiving individualized feedback or support lost a greater percentage of their body weight (MD ‐2.5% (95% CI ‐4.1 to ‐0.9); P = 0.003; 227 participants; two trials; Analysis 3.4: main comparison 3.4.1). When types of feedback or support were examined separately, a similar percentage weight loss was observed for e‐mail feedback, including the directive e‐mail coaching in the Gabriele 2011 trial (MD ‐2.7% (95% CI ‐4.7 to ‐0.6); P = 0.01; 180 participants; two trials; Analysis 3.4: subgroup analysis 3.4.2), and automated feedback (MD ‐2.6% (95% ‐4.2 to ‐1.0); P = 0.001; 102 participants; one trial; Analysis 3.4: subgroup analysis 3.4.3). However, the analyses combining Gabriele 2011 and Tate 2006 showed moderate to high heterogeneity (I2 = 49% and I2 = 66%), as the Gabriele trial consistently showed a smaller effect size than the Tate trial. Meanwhile, non‐directive e‐mail coaching as conducted in the Gabriele 2011 trial did not result in greater weight loss (MD ‐0.2% (95% CI ‐2.3 to 2.0); P = 0.89; 69 participants; one trial; Analysis 3.4: secondary comparison 3.4.4).
3.4. Analysis.
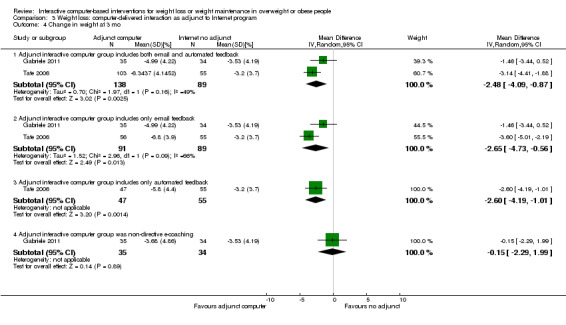
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 4 Change in weight at 3 mo.
In the studies reporting percent weight loss at six or 12 months, participants receiving individualized feedback lost a larger percentage of their body weight at six months (MD ‐4.0% (95% CI ‐6.0 to ‐2.0); P < 0.0001; 155 participants; one trial; Analysis 3.5: main comparison 3.5.1) and 12 months (MD ‐2.6% (95% CI ‐4.9 to ‐0.3); P = 0.03; 92 participants; one trial; Analysis 3.6). At six months, the effect was greater among participants receiving e‐mail feedback than among participants receiving automated feedback (Analysis 3.5; subgroup analyses 3.5.2 and 3.5.3).
3.5. Analysis.
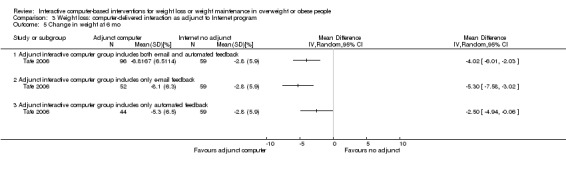
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 5 Change in weight at 6 mo.
3.6. Analysis.
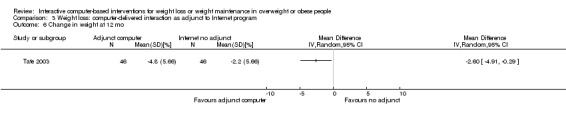
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 6 Change in weight at 12 mo.
In the single study reporting change in BMI (Tate 2003), the reduction in BMI at 12 months was not statistically significantly greater among participants in the e‐counseling group (MD ‐0.8 kg/m2 (95% CI ‐1.7 to 0.1); P = 0.07; 92 participants; one trial; Analysis 3.7).
3.7. Analysis.
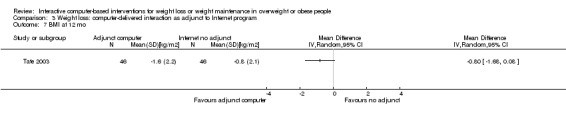
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 7 BMI at 12 mo.
Waist circumference outcomes
Gabriele 2011; Tate 2001 and Tate 2003 reported waist circumference outcomes. At three months, compared to the participants in the control group, participants in e‐counseling or directive e‐coaching had a greater reduction in mean waist circumference compared to participants in the control groups (MD ‐2.6 cm (95% CI ‐4.0 to ‐1.2); P = 0.0003; 160 participants; two trials; Analysis 3.8: main comparison 3.8.1), however non‐directive e‐coaching was not effective (MD ‐0.3 cm (95% CI ‐2.8 to 2.2); P = 0.80; 69 participants; one trial; Analysis 3.8: secondary comparison 3.8.2). At 12 months, participants in the e‐counseling group lost an average of 2.8 cm more from their waist (95% CI ‐5.5 to ‐0.1; P = 0.04; 92 participants; one trial; Analysis 3.9).
3.8. Analysis.
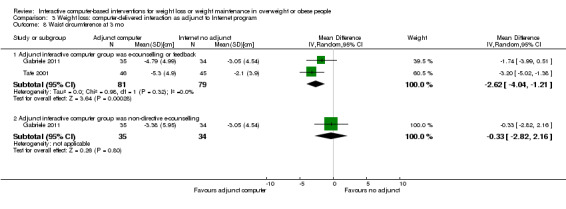
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 8 Waist circumference at 3 mo.
3.9. Analysis.
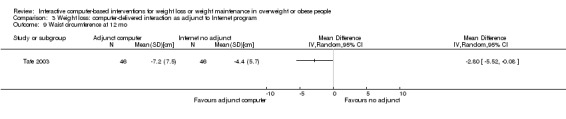
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 9 Waist circumference at 12 mo.
Health‐related quality of life outcomes
No study included data on health‐related quality of life outcomes.
Secondary outcomes
Dietary outcomes
Tate 2006 and Webber 2008 reported data on change in total kilocalories per day, and Tate 2003; Tate 2006 and Webber 2008 reported data on change in percent calories from fat.
Individualized computer‐based feedback was not associated with statistically significant decreases in caloric intake at three months (MD ‐115 calories/day (95% CI ‐308 to 78); P = 0.24; 155 participants; one trial; Analysis 3.10: main comparison 3.10.1) or six months (MD ‐117 kcal/day (95% CI ‐359 to 125); P = 0.34; 146 participants; one trial; Analysis 3.11: main comparison 3.11.1). Individualized feedback was associated with decreases in percent fat intake at three months (MD ‐2.9% (95% CI ‐5.0 to ‐0.8); P = 0.007; 155 participants; one trial; Analysis 3.12: main comparison 3.12.1) and six months (MD ‐3.8% (95% CI ‐5.9 to ‐1.7); P = 0.0004; 146 participants; one trial; Analysis 3.13: main comparison 3.13.1). At 12 months, the decrease in percentage dietary fat intake was three percent greater in the e‐counseling group than the control group (95% CI ‐6.1 to 0.1); P = 0.06; 92 participants; one trial; Analysis 3.14).
3.10. Analysis.
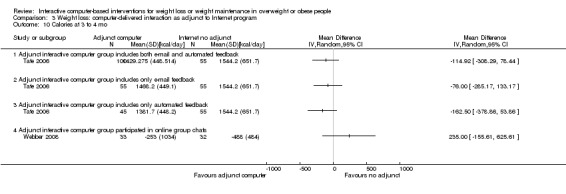
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 10 Calories at 3 to 4 mo.
3.11. Analysis.
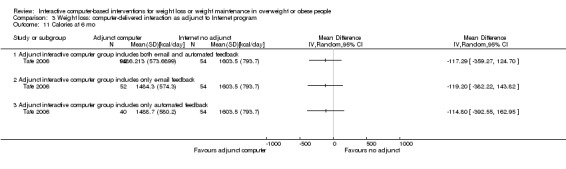
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 11 Calories at 6 mo.
3.12. Analysis.
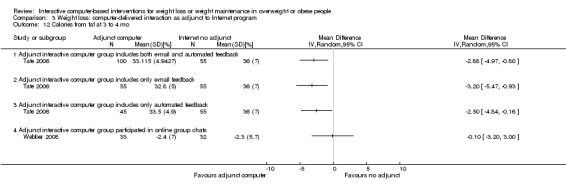
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 12 Calories from fat at 3 to 4 mo.
3.13. Analysis.
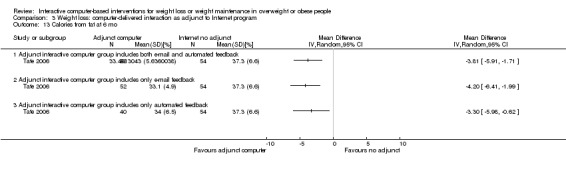
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 13 Calories from fat at 6 mo.
3.14. Analysis.
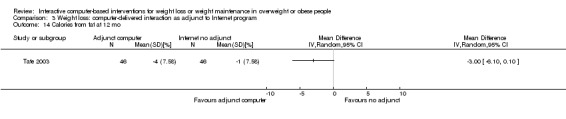
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 14 Calories from fat at 12 mo.
In contrast to individual support or feedback interventions, online group chats were associated with smaller (not greater) non‐significant decreases in caloric intake at four months (MD 235 kcal/day (95% ‐156 to 626); P = 0.24; 65 participants; one trial; Analysis 3.10: secondary comparison 3.10.4), and there was no difference between intervention and control group participants in percentage fat intake (MD ‐0.1% (95% CI ‐3.2 to 3.0); P = 0.95; 65 participants; one trial; Analysis 3.12: secondary comparison 3.12.4).
Physical activity outcomes
Tate 2003; Tate 2006 and Webber 2008 reported data on physical activity at three to four months, while Tate 2006 reported physical activity at six months and Tate 2003 reported physical activity at 12 months. At three months, participants receiving individualized feedback increased their energy expenditure more than did participants without such feedback (MD 347 kcal/week (95% CI 94 to 600); P = 0.0007; 250 participants; two trials; Analysis 3.15: main comparison 3.15.1). A similar effect was also observed when the analysis was restricted to trial arms with e‐mail feedback, but the difference was much smaller and not statistically significant when the intervention was restricted to automated feedback (Analysis 3.15: subgroup analysis 3.15.3). Participants receiving individualized feedback had statistically non‐significant greater increases in energy expenditure at six months (MD 294 kcal/week (95% CI ‐96 to 684); P = 0.14; 152 participants; one trial; Analysis 3.16: main comparison 3.16.1) and 12 months (MD 279 kcal/week (95% CI ‐165 to 723); P = 0.22; 92 participants; one trial; Analysis 3.17).
3.15. Analysis.
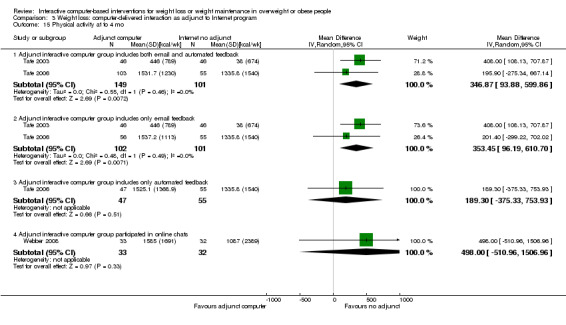
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 15 Physical activity at to 4 mo.
3.16. Analysis.
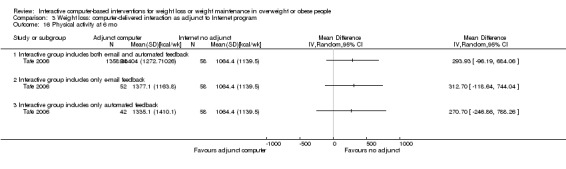
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 16 Physical activity at 6 mo.
3.17. Analysis.
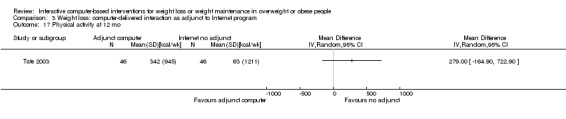
Comparison 3 Weight loss: computer‐delivered interaction as adjunct to Internet program, Outcome 17 Physical activity at 12 mo.
Online group chats were not associated with statistically significant increases in physical activity at four months (MD 498 kcal/week (95% CI ‐511 to 1507); P = 0.33; 65 participants; one trial; Analysis 3.15: secondary comparison 3.15.4).
Cost‐effectiveness outcomes
None of the studies collected information on costs.
Adverse effects outcomes
Tate 2006 reported that no serious adverse events had occurred. No other study reported assessing adverse effects of the intervention.
Covariates
Adherence
Gabriele 2011 collected information on the number of times participants submitted information via the online check‐in page to the e‐coach about weight, calorie intake or physical activity, but did not look within intervention groups to test whether adherence was associated with weight loss or any other outcomes. In the Webber 2008 trial, participants in the online chat intervention group who attended more online chats had greater weight loss. In Tate 2001, Tate 2003 and Tate 2006, login frequency was significantly correlated with weight change in all intervention groups. In both Tate 2001 and Tate 2003, participants in the feedback intervention groups logged in more frequently than participants in the control group. In Tate 2006, post hoc comparisons showed that the control and e‐mail feedback groups logged in significantly more often than the automated feedback group did.
Computer‐based intervention as adjunct to an in‐person intervention
One study (DeLucia 1988) with a total of 29 participants assessed the effects of an interactive computer‐based intervention as an adjunct to an in‐person behavioral weight loss intervention.
Primary outcomes
Weight loss outcomes
There was no statistically significant difference in weight loss between groups immediately after the completion of the 10‐week intervention (MD ‐0.4 kg (95% CI ‐4.1 to 3.3); P = 0.83; 26 participants; Analysis 4.1) or six months after the completion of the intervention (MD 0.1 kg (95% CI ‐3.6 to 3.7); P = 0.97; 26 participants; Analysis 4.2).
4.1. Analysis.
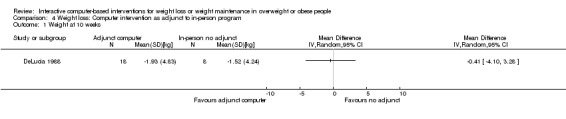
Comparison 4 Weight loss: Computer intervention as adjunct to in‐person program, Outcome 1 Weight at 10 weeks.
4.2. Analysis.
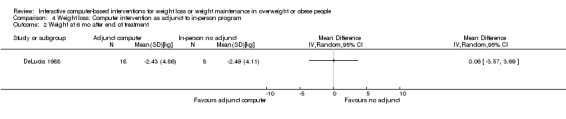
Comparison 4 Weight loss: Computer intervention as adjunct to in‐person program, Outcome 2 Weight at 6 mo after end of treatment.
Waist circumference outcomes and health‐related quality of life outcomes
DeLucia 1988 did not collect data on waist circumference or health‐related quality of life.
Secondary outcomes
Diet, physical activity, costs and adverse effects outcomes
DeLucia 1988 did not collect data on dietary intake, physical activity or costs. Assessment of adverse effects was not reported.
Covariates
Adherence
Treatment groups had equivalent adherence to the intervention, as measured by completion of homework assignments. There was not any exploration of within‐group relationships between adherence and outcomes.
Weight maintenance studies
Computer‐based intervention versus minimal or no treatment control for weight maintenance
Three studies (Cussler 2008; Svetkey 2008; Wing 2006) with a combined total of 1032 participants assessed the effects of an interactive computer‐based intervention compared to a minimal or no treatment control for maintenance of weight loss.
Primary outcomes
Weight change outcomes
Two trials (Svetkey 2008; Wing 2006) presented data on weight loss outcomes at six months, three trials (Cussler 2008; Svetkey 2008; Wing 2006) presented data on weight loss at 12 months, and two trials (Svetkey 2008; Wing 2006) contained information on weight loss at 18 months. Compared to participants in the minimal or no treatment conditions, participants in the computer interventions regained less weight at six months (MD ‐0.7 kg (95% CI ‐1.2 to ‐0.2); P = 0.004; 897 participants; two trials; Analysis 5.1) and 12 months (MD ‐0.8 kg (95% CI ‐1.4 to ‐0.2); P = 0.01; 1004 participants; three trials; Analysis 5.2) (Figure 5). Participants in the computer intervention continued to have regained less weight at 18 months (‐0.7 kg (95% CI ‐1.6 to 0.1); P = 0.10; 897 participants; two trials; Analysis 5.3), although the difference was not statistically significant. One study (Svetkey 2008) followed participants to 24 and 30 months; weight maintenance was statistically significantly better in the computer intervention group at 24 months (MD ‐0.9 kg (95% CI ‐1.8 to ‐0.0); P = 0.04; 688 participants; Analysis 5.4) but not at 30 months (MD ‐0.3 kg (95% CI ‐1.3 to 0.5); P = 0.48; 688 participants; Analysis 5.5). Svetkey 2008 also collected data on percent weight change at 30 months, and found that the percentage weight regained during maintenance was not significantly smaller in the intervention group (‐0.4% (95% CI ‐1.6 to 0.8); P = 0.50; 688 participants; Analysis 5.6).
5.1. Analysis.
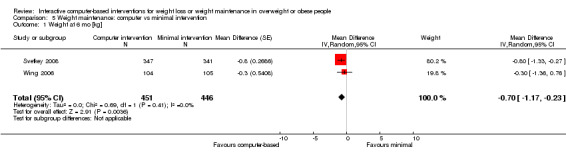
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 1 Weight at 6 mo [kg].
5.2. Analysis.
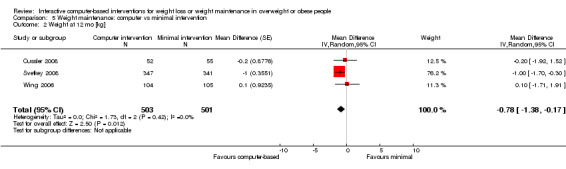
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 2 Weight at 12 mo [kg].
5.
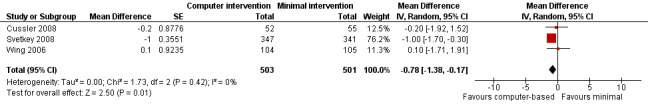
Forest plot of comparison: 5 Weight maintenance: computer vs minimal intervention, outcome: 5.2 Weight at 12 mo [kg].
5.3. Analysis.
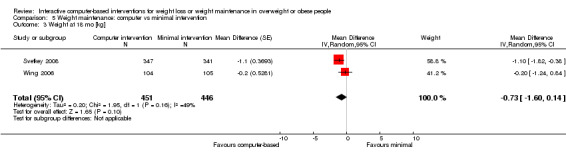
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 3 Weight at 18 mo [kg].
5.4. Analysis.
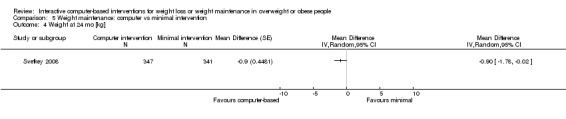
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 4 Weight at 24 mo [kg].
5.5. Analysis.
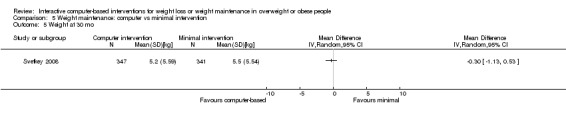
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 5 Weight at 30 mo.
5.6. Analysis.
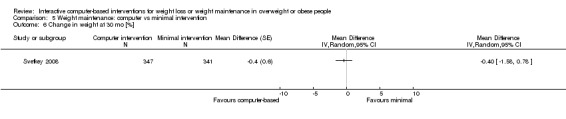
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 6 Change in weight at 30 mo [%].
One study (Cussler 2008) presented BMI outcome data. At 12 months of follow‐up, the difference between intervention groups was small and not statistically significant (MD ‐0.4 kg/m2 (95% CI ‐0.3 to 1.1); P = 0.26; 688 participants; Analysis 5.7).
5.7. Analysis.
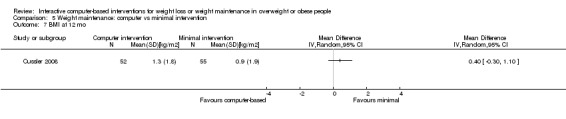
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 7 BMI at 12 mo.
Waist circumference outcomes
No study included data on change in waist circumference outcomes.
Health‐related quality of life outcomes
No study collected data on health‐related quality of life outcomes.
Secondary outcomes
Dietary outcomes
One study (Cussler 2008) reported data on energy intake at 12 months (MD ‐48 kcal/day (95% CI ‐198 to 102); P = 0.53; 107 participants; Analysis 5.8) and one study (Svetkey 2008) reported data on energy intake at 30 months (MD ‐72 kcal/day (95% CI ‐168 to 24); P = 0.14; 688 participants; Analysis 5.9). In both cases, the computer intervention group had a smaller increase in kcal/day intake but the difference was not statistically significant.
5.8. Analysis.
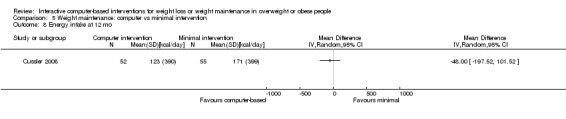
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 8 Energy intake at 12 mo.
5.9. Analysis.
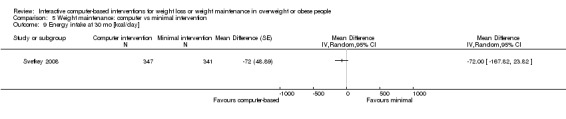
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 9 Energy intake at 30 mo [kcal/day].
Physical activity outcomes
One study (Cussler 2008) reported data on energy expenditure at 12 months; there was no statistically significant difference between intervention groups (MD ‐7 kcal/day (95% CI ‐117 to 103); P = 0.90; 107 participants; Analysis 5.10).
5.10. Analysis.
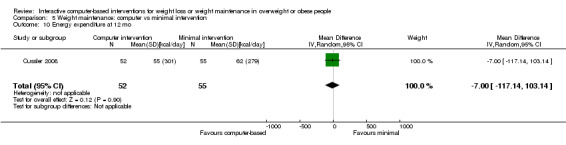
Comparison 5 Weight maintenance: computer vs minimal intervention, Outcome 10 Energy expenditure at 12 mo.
Cost‐effectiveness outcomes
No study included data on costs.
Adverse effects outcomes
Wing 2006 reported that there were no serious adverse events. No other study reported assessing for adverse effects of the intervention.
Covariates
Adherence
Cussler 2008 used several measures of engagement with the computer‐based intervention (e.g. submission of diet and weight logs, number of e‐mail contacts, number of articles posted) and found a wide range in adherence to intervention activities. For example, almost one‐third of the computer‐based group accessed the Internet only once per week during maintenance. Among participants who completed the study, there was a significant correlation between submission of diet logs and change in weight. No other measures of adherence were correlated with weight maintenance. Svetkey 2008 tracked website contacts, and found that participants in the computer‐based intervention logged in at least once per month for 77% of the months of the maintenance intervention. There was no examination in this study of relationships between Internet use and weight outcomes. Wing 2006 measured attendance at the chat‐room sessions and the percentage of participants who reported their weight each week, and both measures decreased significantly over time (P < 0.001). There was no assessment of relationships between either measure and weight maintenance.
Computer‐based intervention versus minimal in‐person control treatment for weight maintenance
Three studies (Harvey‐Berino 2002; Svetkey 2008; Wing 2006) with a combined total of 955 participants assessed the effects of an interactive computer‐based intervention compared to a minimal in‐person treatment control, defined as in‐person contact no more than once per month, for maintenance of weight loss.
Primary outcomes
Weight change outcomes
Two trials (Svetkey 2008; Wing 2006) presented data on weight loss outcomes at six months, three trials (Harvey‐Berino 2002; Svetkey 2008; Wing 2006) presented data on weight loss at 12 months, and two trials (Svetkey 2008; Wing 2006) contained information on weight loss at 18 months. At six months, the computer intervention group regained slightly more weight than the face‐to‐face group, although the difference was not statistically significant (MD 0.5 kg (95% CI ‐0.5 to 1.6); P = 0.32; 897 participants; two trials; Analysis 6.1). At 12 months, the computer group regained more weight than the face‐to‐face group, and the difference was near to statistical significance (MD 1.6 kg (95% ‐0.1 to 3.2); P = 0.07; 955 participants; three trials; Analysis 6.2) (Figure 6). This difference was also seen at 18 months (MD 1.1 kg (95% CI ‐0.2 to 2.5); P = 0.10; 897 participants; two trials; Analysis 6.3). Each of these meta‐analyses displayed moderate to high heterogeneity (I2 = 42% to I2 = 66%) due to differing interventions, controls and populations. However, the effects in individual trials, while small and varying in size and statistical significance, were consistently in favor of the face‐to‐face intervention. One study (Svetkey 2008) followed participants to 24 and 30 months and observed that participants in the computer‐based intervention group had gained approximately one kg more than participants in the in‐person intervention group at both time points, and this difference was statistically significant (at 24 months, MD 1.1 kg (95% CI 0.3 to 1.9); P = 0.01; 688 participants; Analysis 6.4) (at 30 months, MD 1.2 kg (95% CI 0.3 to 2.1); P = 0.009; 688 participants; Analysis 6.5). The same study reported data on percent weight change at 30 months, and found that the percentage weight gain during maintenance was 1.5% greater in the computer‐based intervention (95% CI 0.5 to 2.5; P = 0.003; 688 participants; Analysis 6.6).
6.1. Analysis.
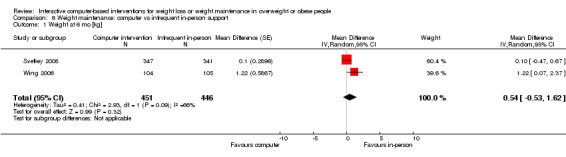
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 1 Weight at 6 mo [kg].
6.2. Analysis.
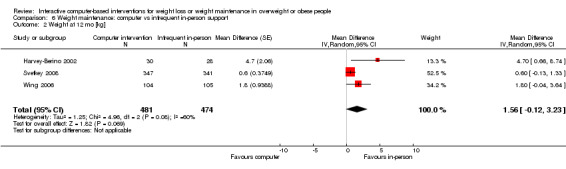
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 2 Weight at 12 mo [kg].
6.
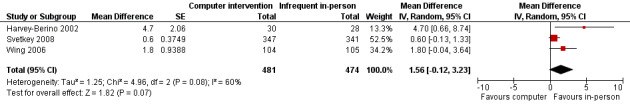
Forest plot of comparison: 6 Weight maintenance: computer vs infrequent in‐person support, outcome: 6.2 Weight at 12 mo [kg].
6.3. Analysis.
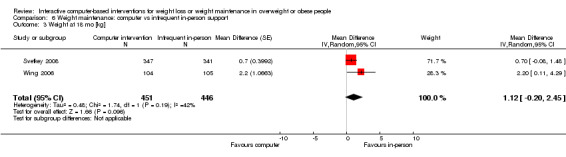
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 3 Weight at 18 mo [kg].
6.4. Analysis.
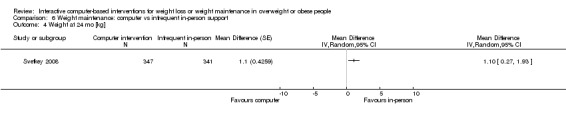
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 4 Weight at 24 mo [kg].
6.5. Analysis.
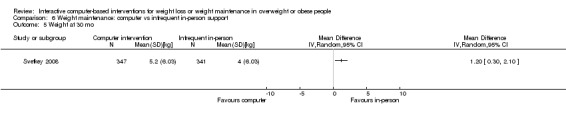
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 5 Weight at 30 mo.
6.6. Analysis.
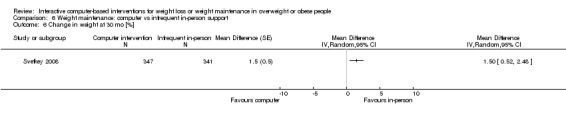
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 6 Change in weight at 30 mo [%].
Waist circumference outcomes
No study included data on change in waist circumference.
Health‐related quality of life outcomes
No study included data on health‐related quality of life.
Secondary outcomes
Dietary outcomes
One study (Svetkey 2008) reported data on energy intake at 30 months. At 30 months, the computer intervention group took in slightly more calories than the in‐person intervention group but this was not statistically significant (MD 39 kcal/day (95% CI ‐45 to 123); P = 0.36; 688 participants; Analysis 6.7).
6.7. Analysis.
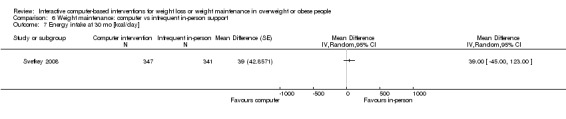
Comparison 6 Weight maintenance: computer vs infrequent in‐person support, Outcome 7 Energy intake at 30 mo [kcal/day].
Physical activity outcomes
No study included data on change in physical activity outcomes.
Cost‐effectiveness outcomes
Although the costs of the intervention in one trial (Svetkey 2008) were detailed in related publications (Meenan 2009; Meenan 2010) no data on cost‐effectiveness or relative costs of interventions and controls were presented.
Adverse effects outcomes
Wing 2006 reported that there were no serious adverse events. No other study reported assessing for adverse effects of the intervention.
Covariates
Adherence
Harvey‐Berino 2002 reported that, compared to participants in the computer‐based treatment group, participants in the infrequent in‐person treatment group attended a greater percentage of group sessions during the first six months of weight maintenance. However, the infrequent in‐person treatment group did not receive any study contacts at all during the second six months of weight maintenance. Svetkey 2008 stated that participants in the personal‐contact group completed an average of 91% of monthly intervention contacts, while participants in the computer‐based intervention logged onto the Internet at least once per month for 77% of the months of the maintenance intervention. Wing 2006 reported that while attendance at both the in‐person and the Internet chat‐room sessions decreased over time, the percentage of sessions attended was significantly higher in the in‐person group throughout the trial. Weekly reporting of weight also decreased over time, and was consistently higher among participants in the in‐person intervention, but the difference between the in‐person and computer‐based groups was not statistically significant. None of the three studies explored within‐group relationships between adherence or dose of the intervention, and weight outcomes.
Computer‐based intervention versus intensive in‐person control treatment for weight maintenance
Only one included study (Harvey‐Berino 2002) presented data on the effects of a computer‐based intervention versus an intensive in‐person intervention, defined as contact that is more frequent than once per month, for maintenance of weight loss. The in‐person contact in this study was once every two weeks throughout one year of follow‐up.
Primary outcomes
Weight change outcomes
Compared to participants in the in‐person group, participants in the Internet group regained more weight during the first six months of weight maintenance (MD 2.2 kg (95% CI 0.3 to 4.1); P = 0.03; 62 participants; Analysis 7.1). Overall, from the time of entry into the weight loss component of the trial to the end of the 12 months of weight maintenance, participants in the in‐person group lost more weight than did participants in the Internet group (MD 4.7 kg (95% CI 1.7 to 7.7); P = 0.002; 62 participants; Analysis 7.2).
7.1. Analysis.
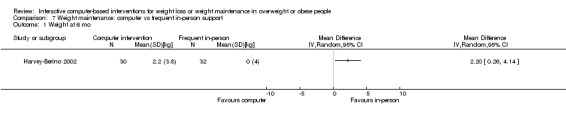
Comparison 7 Weight maintenance: computer vs frequent in‐person support, Outcome 1 Weight at 6 mo.
7.2. Analysis.
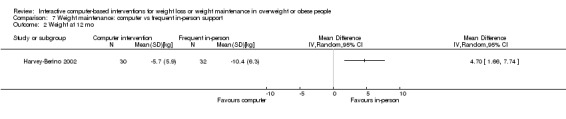
Comparison 7 Weight maintenance: computer vs frequent in‐person support, Outcome 2 Weight at 12 mo.
Waist circumference and health‐related quality of life outcomes
Harvey‐Berino 2002 did not present data on change in waist circumference or health‐related quality of life outcomes.
Secondary outcomes
Dietary, physical activity, cost‐effectiveness and adverse effects outcomes
Harvey‐Berino 2002 did not present data on dietary or physical activity outcomes. Information on costs was not collected. No assessment of adverse effects of the intervention was reported.
Covariates
Adherence
The authors reported that attendance at treatment sessions was greater for the intensive in‐person condition than the computer condition, and participants in the in‐person condition also reported more peer‐support contacts. However, there was no between‐group difference in the number of weeks for which self monitoring data were submitted. The authors did not investigate whether there were any within‐group relationships between dose of intervention and amount of weight lost.
Subgroup analyses
The number of trials available for analysis was small for all outcomes, and subgroup analyses by age group and overweight versus obesity could not be performed. When the two weight‐loss trials that included only men (Morgan 2009; Morgan 2011) were analyzed together, the mean weight loss was larger than that of trials conducted in mixed‐gender populations (3 kg versus 2 kg; Analysis 1.1; subgroup analyses 1.1.4 and 1.1.5) but there was substantial heterogeneity in the analysis of men only (I2 = 60%), as the mean difference between intervention groups in Morgan 2009 was less than half that observed in Morgan 2011. While the computer intervention group in Morgan 2009 lost more weight than the computer intervention group in Morgan 2011, the control group in Morgan 2009 also lost a substantial amount of weight, while the control group in Morgan 2011 did not lose any weight. In the case of these two trials, differences in response to the computer intervention may be related to differences in contextual factors. For example, the earlier trial was conducted at a university and the later trial was conducted in factory shift workers, raising issues such as possible differences in ease and comfort of computer use in the two populations. However, we were unable to explore this explanation further given the available data.
Sensitivity analyses
When we conducted sensitivity analyses omitting the sole quasi‐randomized trial (Schroder 2010) or the oldest randomized and the sole non‐published trial (Threlfall 1984), or both, heterogeneity decreased but the results were consistent with the original analyses. Likewise, omitting the one very large trial (Wing 2006) from weight maintenance analyses did not make large differences to the estimate of effect or the statistical significance of those analyses. When we omitted the cluster‐randomized studies (Cussler 2008; Morgan 2011) from analyses, there were not large differences in the estimate of effect or the statistical significance of those analyses, with two exceptions. In the analysis of change in waist circumference at six months, the omission of Morgan 2011 from the analysis (Analysis 1.9: sensitivity analysis 1.9.2) reduced the pooled effect size although the difference between intervention groups remained near statistical significance (P = 0.08 versus P = 0.07). This change in effect size was likely due to the extremely large change in waist circumference seen in Morgan 2011, which we cannot explain. In the analysis of change in weight maintenance at 12 months (Analysis 5.2), the omission of Cussler 2008 from the analysis did not change the pooled effect estimate of 0.8 kg, but altered the statistical significance from P = 0.01 to P = 0.08. Since the estimate of effect in Cussler 2008 was intermediate between that in the other two trials in the analysis, it is likely that the omission of the trial reduced the statistical significance of the effect estimate due to less information being present in the analysis. Because there were few trials available for all outcomes, we could not further examine the effects of components of risk of bias (e.g. allocation concealment) on outcomes. Also, while we had hoped to conduct sensitivity analyses on additional factors (e.g. language of publication), included studies possessed insufficient variability in those factors to allow performance of sensitivity analyses.
We would also have liked to conduct analyses based on adherence to interventions or associations between the intensity of the intervention and effects of interventions. Most studies collected some data on adherence, and the majority of these examined relationships between adherence or intervention dose and weight change outcomes (Bennett 2010; Cussler 2008; Hunter 2008; Morgan 2009; Morgan 2011; Tate 2001; Tate 2003; Tate 2006; Webber 2008; Wylie‐Rosett 2001). However, the different measures of adherence, and different analyses of relationships between adherence and outcomes, made combining data across studies impossible.
Publication and small study bias
Because there were five or fewer studies in all meta‐analyses, we did not construct funnel plots to examine for publication and small study bias. When there are fewer than 10 studies in a comparison, it is difficult to assess asymmetry by visual examination, and the power of the funnel plot test is too low to distinguish chance from real asymmetry (Higgins 2009, Chapter 10).
Discussion
Summary of main results
The findings of this review demonstrate that computer‐based interventions have a positive effect on short‐term weight loss and short‐term weight loss maintenance. The strongest conclusion, based on the greatest number of studies, supports the observation that a variety of interactive computer‐based interventions led to short‐term weight loss when compared to a minimal or no treatment condition. Computer‐based feedback also appeared to be effective as an adjunct to Internet interventions in promoting weight loss. Fewer trials tested computer‐based interventions for maintenance of weight loss, however computer‐based interventions consistently led to lower levels of weight regain when compared to a minimal or no treatment condition. Few interventions led to changes in caloric intake, physical activity or waist circumference, though these outcomes were not reported in all studies. Greater amounts of intervention use, particularly self monitoring, were typically associated with greater amounts of weight loss, though it was not clear what intervention elements would best encourage greater use or whether encouraging greater use would lead to larger effects. These results are similar to those of other recent reviews (Neve 2010; Reed 2012).
While interactive computer‐based interventions appear to be more effective than a minimal or no treatment control, they do not appear to be more effective than in‐person treatments, even in cases where the in‐person contacts are infrequent. This was true in the one study comparing in‐person and computer‐based interventions for weight loss, as well as the three studies comparing in‐person and computer‐based interventions for maintenance of weight loss. For maintenance of weight loss, both minimal (once per month or less) and intensive (more often than once per month) in‐person interventions outperformed computer‐based interventions. The amount of additional weight loss, however, is relatively small and of brief duration, making the clinical significance of these differences unclear.
Few studies included cost information, making conclusions about cost‐effectiveness difficult. This is similar to the observations of Tate and colleagues in a 2009 review of eight studies examining cost‐effectiveness of Internet interventions (Tate 2009). In the present review, however, the studies that examined cost‐effectiveness observed relatively high levels of cost effectiveness, and the single study comparing the cost‐effectiveness of an in‐person and a computer‐based intervention found that the computer‐based intervention was more cost‐effective.
Overall completeness and applicability of evidence
A challenge in interpreting these findings is the heterogeneity of the intervention goal (loss versus maintenance), timing of measures (three months, six months, 12 months, or longer) and control group (minimal, adjunct to Internet intervention, adjunct to minimal in‐person treatment). Given the small number of studies (18 total) and the many permutations of intervention goal, intervention components, control condition and timing, firm conclusions were hard to make and were typically based on a relatively small number of studies. The interventions, however, tended to be similar in that they typically included computer‐based education, self monitoring (of weight, intake and activity) using a computer interface, and some form of feedback based upon the self monitoring. With the exception of one study examining a computer‐based group chat intervention, and a non‐directive counseling arm in a second study, interactive computer‐based interventions were consistently more effective than minimal interventions and less effective than in‐person contacts for weight loss and weight maintenance.
A major advantage of computer‐based interventions is their ability to reach large numbers of people at a relatively low cost. However, the issue of costs and cost‐effectiveness in the area of computer‐based interventions is complex. Though cost‐analyses can be important tools to assist organizations in making decisions, it is increasingly complicated to understand their significance. Over the past decade, end‐users are being provided more and more services for free online and in mobile applications, their costs being offset by revenue from advertising (Miller 2008). In addition, while these analyses are often done from the perspective of the employer or the managed care organization, who pay for a large percentage of care in the U.S., such organizations pay very little for the direct care of overweight and obesity, other than for surgery (Wylie‐Rosett 2001). Comparisons with surgery, however, should optimally include a longer time‐horizon than is typically included in behavioral interventions. As overweight and obesity are increasingly considered chronic illnesses, interventions will need to examine the cost‐effectiveness over time, as the comparator will increasingly be surgery. Sjöström and colleagues, for example, have conducted a 15‐year follow‐up study of obese patients treated with different surgical approaches (Sjöström 2007). These durations of follow‐up are very challenging for behavioral interventions, given the difficulties in assuring long‐term fidelity. Furthermore, in 2011, the U.S. Food and Drug Administration (FDA) lowered the body mass index (BMI) threshold for use of laparoscopic band procedures for those with obesity‐related conditions, from a previous BMI of 35 kg/m2 to 30 kg/m2 (Corbett Dooren 2011), so the rates of surgical treatment of obesity can be expected to increase. Due to these complexities, conclusions from cost‐effectiveness studies in obesity treatment, even well‐done ones, can be challenging to make in the ever‐shifting landscape of the epidemiology and treatment options for obesity.
Finally, interactive technologies change quickly, so it is quite likely that what is reviewed here will be quite different from the trials reviewed 10 years from now. The increased use of smartphones and sophisticated mobile computing means that a growing number of individuals have a global positioning chip and accelerometer with them at all times. This means that applications such as location‐based coupons for healthy foods and real‐time step counter feedback are technically possible today and will certainly be incorporated into future interventions. The concurrent rise of social networking and the more than 500 million Facebook users worldwide will, for example, likely herald the rise of peer‐based weight control interventions (Madden 2006; Pew 2009). We would anticipate future reviews to include smartphone applications, given the rich interactive features of these devices which now often exceed (e.g. accelerometer) those of personal computers.
Quality of the evidence
We included one quasi‐randomized trial and 17 randomized trials. Most randomized trials did not give details about the methods of randomization, and we were uncertain about the concealment of allocation to treatment and the blinding of outcome assessors in many of the included trials. Incomplete outcome reporting was only considered to be a risk in one trial, and selective reporting and other sources of potential bias were not observed. However, only two trials were rated to have no perceived risk of bias.
Our inclusion criterion of 80% or greater follow‐up was intended to ensure that included trials were of good quality. We instituted this inclusion criterion because loss to follow‐up is a serious threat to the validity of a randomized trial (Guyatt 2001).
Due to the methodological quality of some trials and the heterogeneity of some analyses, the overall quality of the evidence on weight loss and weight maintenance according to the GRADE approach ranged between 'moderate' and 'low'.
Potential biases in the review process
We excluded several studies from this review because they did not meet the inclusion criterion of at least 80% follow‐up. As mentioned above, this was intended to ensure that the included trials were of high quality. The criterion of 80% follow‐up has been used as a quality criterion by some organizations assessing evidence from randomized controlled trials. The McMaster University McMaster Online Rating of Evidence (Health Information Research Unit) uses 80% follow‐up of a randomized controlled trial as a criterion for scientific merit (CITE) and the DynaMed Level of Evidence scheme uses 80% follow‐up of trial participants as a criterion for Level 1 (likely reliable) evidence (DynaMed). However, because it is common for behavioral intervention trials to experience large losses to follow‐up, the effect of this exclusion was to lower the number of trials in this review, reduce the total amount of information available for review outcomes, and decrease the power of reported meta‐analyses.
Agreements and disagreements with other studies or reviews
To date, two systematic reviews have been published that examine the impact of web‐based weight control programs among adults (Arem 2010; Neve 2010). In 2010 Arem and Irwin published a systematic review that included nine studies (Arem 2010). The authors observed a wide range of weight losses and made few conclusions, in part because the interventions differed so greatly and treatment adherence rates were low (Arem 2010). In 2010, Neve and colleagues published a review that included 20 studies (Neve 2010). Although this review compared a greater number of studies, the heterogeneity of the research questions posed and study designs, coupled with the small number of studies made conclusions difficult (Neve 2010). Neve and colleagues observed that login frequency was associated with impact, consistent with what has been observed in a number of the individual trials in this review (Cussler 2008; Harvey‐Berino 2004; Tate 2001; Tate 2003; Womble 2004).
Authors' conclusions
Implications for practice.
This review indicates that interactive computer‐based programs are effective weight loss interventions, and that e‐mailed or automated counseling increase the effectiveness of computer‐based interventions, although the value of online group chats is unclear. These computer‐based programs, however, do not result in weight losses that are equivalent to face‐to‐face treatments, which typically led to a loss of 7% to 10% of body weight over 26 weeks (Foster 2005). Providers, however, have few options to offer to their patients, so programs of less impact are still potentially important to consider as treatment options. In addition, a recent large study by Jebb and colleagues of 772 adults observed that those who were referred to and provided free access to Weight Watchers lost an additional 2.3 kg (95% confidence interval (CI) –3.0 to ‐1.6), which is quite similar to the losses of interactive computer‐based programs in this review (Jebb 2011). Similarly, while there is less available evidence on the effects of interactive computer‐based interventions for weight maintenance, this review suggests that here too, computer‐based interventions are more effective than no treatment but less effective than face‐to‐face interventions. The impact of computer‐based interventions appears relatively small when compared to standard of care face‐to‐face interventions published elsewhere. In‐person treatments tend to lead to a loss of 7% to 10% of body weight in the first six months (Foster 2005; Franz 2007). This is substantially more than the amount of weight lost at six months in the computer‐based intervention groups included in this review, which raises the question of what role these interventions may play in addressing the epidemic of overweight and obesity. Weight losses at this level are below the five percent threshold that the U.S. National Heart, Lung and Blood Institute guidelines suggest will lead to clinical improvement, though a meta‐analysis of 25 studies and 4874 participants observed blood pressure reductions of 1.1 mm Hg (95% CI 1.4 to 0.7) systolic and 0.9 mm Hg (95% CI 1.3 to 0.6) diastolic for each kilogram of weight lost (National Institutes of Health 2000; Neter 2003). It is likely, therefore, that the weight loss observed in the analyses comparing computer‐based interventions to minimal or no treatment controls is clinically significant on an individual and public health level, though weight regain will limit the impact of this benefit. All studies reviewed, however, are efficacy studies and not effectiveness studies, so it is not clear whether these interventions would have the same level of impact if integrated into routine primary care settings. Those studies would first need to be done before the interventions would be ready to be used routinely in clinical settings. In the studies examined, adherence decreased dramatically in the first few months. In Tate 2006, for example, the average number of logins decreased by approximately 50% over the first three months in the automated feedback treatment group. Without understanding what level of adherence was clinically significant over the long term, it will be difficult for clinicians to recommend and monitor the use of these interventions. Also, using a web‐based intervention is more complicated than taking a pill, so physicians would need to understand what compliance means to these interventions to be able to use them routinely. This question will become more relevant should interventions be shown, in the future, to lead to greater effect sizes or clinical improvements.
Implications for research.
There was not a sufficient number of studies to examine the longer‐term impacts of computer‐based interventions for weight loss. Only one study (Wylie‐Rosett 2001) examined 12‐month outcomes versus minimal treatment and only one study (Tate 2003) examined 12‐month outcomes as an adjunct to an Internet intervention. Both of these studies, however, showed positive results. All studies that examined utilization of interventions over time showed a drop‐off in use. For example, Tate and colleagues observed an average monthly login of greater than 20 in months one to three and fewer than 10 in months 10 to 12 (Tate 2003). This is similar to patterns observed in a later study by this group (Tate 2006). Finally, Wing and colleagues observed that 65.7% of web sessions attended were attended in months zero to six and 34.2% in months 13 to 18 (Wing 2006). As weight management is an ongoing health issue, both longer‐term weight‐loss studies and additional studies on weight maintenance are needed, as is additional research on adherence to interventions.
We observed heterogeneity across studies in how adherence to the intervention is expressed, allowing us to make general observations about patterns but making specific conclusions about intervention usage over time difficult. Cussler and colleagues expressed adherence as “percent using a feature at least once per week” (Cussler 2008), Svetkey and colleagues expressed adherence as “percent logging in at least once per month” (Stevens 2008) and Wing and colleagues expressed adherence as the overall “percentage of sessions attended” (Wing 2006). Other studies expressed adherence as mean logins per period of time (Bennett 2010), median logins per period of time (Tate 2006) or simply examined the relationship between quartiles of use and outcomes (Hunter 2008), making comparisons difficult. While beyond the scope of our results, the challenges in comparing adherence data lead to the conclusion that the field would move forward more quickly if standards could be created for expressing adherence rates, both in overall use and in the use of specific features. This is particularly important as all studies that reported the relationship between adherence to the intervention and weight control outcomes observed positive associations. Over time, standards have emerged for reporting weight loss in clinical trials, such as kilograms lost, percent of weight lost and percentage of participants losing five percent and 10 percent of body weight. Similar standards for measuring and reporting adherence may be helpful for advancing the field of computer‐based weight interventions, and behavioral interventions more generally.
Appendices
Appendix 1. Search strategies
| Databases and search terms |
| Unless otherwise stated, search terms are free‐text terms; MeSH = Medical subject heading (MEDLINE medical index term); exp = exploded MeSH; the dollar sign ($) stands for any character(s); the question mark (?) substitutes one or no characters; tw = text word; pt = publication type; sh = MeSH; adj = adjacent. |
| The Cochrane Library |
| #1 MeSH descriptor Obesity explode all trees
#2 obes*:ti,ab
#3 MeSH descriptor Overweight explode all trees
#4 overweight:ti,ab
#5 MeSH descriptor Body Weight explode all trees
#6 (body next (weight or mass)):ti,ab
#7 MeSH descriptor Body Mass Index explode all trees
#8 (body mass index or bmi):ti,ab
#9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8)
#10 MeSH descriptor Computer Systems explode all trees
#11 computer*:ti,ab
#12 (pc or pcs):ti,ab
#13 MeSH descriptor Software explode all trees
#14 MeSH descriptor Multimedia explode all trees #15 (multi‐media or multimedia):ti,ab #16 interactive:ti,ab #17 MeSH descriptor Computer‐Assisted Instruction explode all trees #18 MeSH descriptor Medical Informatics explode all trees #19 cd‐rom:ti,ab #20 (compact next (disc* or disk*)):ti,ab #21 internet:ti,ab #22 (world next wide next web):ti,ab #23 (web next based):ti,ab #24 (online or on‐line):ti,ab #25 (surf* near/2 (web or net)):ti,ab #26 e‐health:ti,ab #27 (consumer* next health next informatic*):ti,ab #28 (#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27) #29 (#9 AND #28) |
| MEDLINE (original search) |
| 1. exp Obesity/
2. obes$.tw.
3. exp Overweight/
4. overweight.tw.
5. exp Body Weight/
6. (body adj (weight or mass)).tw.
7. exp Body Mass Index/
8. (body mass index or bmi).tw.
9. or/1‐8
10. exp Computer systems/
11. computer$.tw.
12. (pc or pcs).tw.
13. exp software/
14. exp Multimedia/
15. (multi‐media or multimedia).tw.
16. interactive.tw.
17. computer‐assisted instruction/
18. exp medical informatics/
19. cd‐rom.tw.
20. (compact adj dis?$).tw.
21. internet.tw.
22. (world adj wide adj web).tw.
23. (web adj based).tw.
24. (online or on‐line).tw.
25. (surf$ adj2 (web or net)).tw. 26. e‐health.tw. 27. (consumer$ adj health adj informatic$).tw. 28. or/10‐27 29. 9 and 28 30. randomized controlled trial.pt. 31. controlled clinical trial.pt. 32. randomized.ab. 33. placebo.ab. 34. drug therapy.fs. 35. randomly.ab. 36. trial.ab. 37. groups.ab. 38. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 39. humans.sh. 40. 38 and 39 41. 29 and 40 |
| MEDLINE (updated search) |
| 1. exp Obesity/ 2. obes$.tw. 3. exp Overweight/ 4. overweight.tw. 5. exp Body Weight/ 6. (body adj (weight or mass)).tw. 7. exp Body Mass Index/ 8. (body mass index or bmi).tw. 9. or/1‐8 10. exp Computer systems/ 11. computer$.tw. 12. (pc or pcs).tw. 13. exp software/ 14. exp Multimedia/ 15. (multi‐media or multimedia).tw. 16. interactive.tw. 17. computer‐assisted instruction/ 18. exp medical informatics/ 19. cd‐rom.tw. 20. (compact adj dis?$).tw. 21. internet.tw. 22. (world adj wide adj web).tw. 23. (web adj based).tw. 24. (online or on‐line).tw. 25. (surf$ adj2 (web or net)).tw. 26. e‐health.tw. 27. (consumer$ adj health adj informatic$).tw. 28. or/10‐27 29. 9 and 28 30. randomized controlled trial.pt. 31. controlled clinical trial.pt. 32. randomized.ab. 33. placebo.ab. 34. drug therapy.fs. 35. randomly.ab. 36. trial.ab. 37. groups.ab. 38. or/30‐37 39. (animals not (humans and animals)).sh. 40. 38 not 39 41. 29 and 40 |
| EMBASE |
| 1 exp Obesity/ 2 obes$.tw. 3 overweight.tw. 4 exp body weight/ 5 (body adj (weight or mass)).tw. 6 body mass/ 7 (body mass index or bmi).tw. 8 or/1‐7 9 exp computer/ 10 computer$.tw. 11 (pc or pcs).tw. 12 exp computer program/ 13 multimedia/ 14 (multi‐media or multimedia).tw. 15 interactive.tw. 16 medical informatics/ 17 compact disk/ 18 cd‐rom.tw. 19 (compact adj dis?$).tw. 20 internet/ 21 (world adj wide adj web).tw. 22 (web adj based).tw. 23 (online or on‐line).tw. 24 (surf$ adj2 (web or net)).tw. 25 e‐health.tw. 26 (consumer$ adj health adj informatic$).tw. 27 or/9‐26 28 8 and 27 29 random$.ti,ab. 30 factorial$.ti,ab. 31 (crossover$ or cross over$ or cross‐over$).ti,ab. 32 placebo$.ti,ab. 33 (doubl$ adj blind$).ti,ab. 34 (singl$ adj blind$).ti,ab. 35 assign$.ti,ab. 36 allocat$.ti,ab. 37 volunteer$.ti,ab. 38 crossover procedure.sh. 39 double blind procedure.sh. 40 randomized controlled trial.sh. 41 single blind procedure.sh. 42 or/29‐41 43 exp animal/ or nonhuman/ or exp animal experiment/ 44 exp human/ 45 43 and 44 46 43 not 45 47 42 not 46 48 28 and 47 |
| LILACS |
| (Obes* OR Overweight ) AND (Computer* OR internet OR Web) (All indexes) |
| CINAHL |
| 1. exp Obesity/ 2. obes$.tw. 3. exp Overweight/ 4. overweight.tw. 5. exp Body Weight/ 6. (body adj (weight or mass)).tw. 7. exp Body Mass Index/ 8. (body mass index or bmi).tw. 9. or/1‐8 10. exp Computer systems/ 11. computer$.tw. 12. (pc or pcs).tw. 13. exp software/ 14. exp Multimedia/ 15. (multi‐media or multimedia).tw. 16. interactive.tw. 17. computer‐assisted instruction/ 18. exp medical informatics/ 19. cd‐rom.tw. 20. (compact adj dis?$).tw. 21. internet.tw. 22. (world adj wide adj web).tw. 23. (web adj based).tw. 24. (online or on‐line).tw. 25. (surf$ adj2 (web or net)).tw. 26. e‐health.tw. 27. (consumer$ adj health adj informatic$).tw. 28. or/10‐27 29. 9 and 28 |
| CINAHL (updated search) |
| S1 (MH "Obesity+") S2 ti obes* or ab obes* S3 ti overweight or ab overweight S4 (MH "Body Weight+") S5 (MH "Body Weight Changes+") S6 TI ( body weight or body mass ) or AB ( body weight or body mass ) S7 (MH "Body Mass Index") S8 ( ti body mass index or ab body mass index ) or ( ti bmi or ab bmi ) S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 S10 (MH "Computer Systems+") S11 ti computer* or ab computer* S12 ( ti pc or pcs ) or ( ab pc or pcs ) S13 (MH "Software+") S14 Multimedia S15 TI ( multi‐media or multimedia ) or AB ( multi‐media or multimedia ) S16 ti interactive or ab interactive S17 (MH "Computer Assisted Instruction") S18 (MH "Medical Informatics") S19 ti cd‐rom or ab cd‐rom S20 ti compact dis?* or ab compact dis?* S21 ti internet or ab internet S22 ti world wide web or ab world wide web S23 ti web‐based or ab web‐based S24 TI ( online or on‐line ) or AB ( online or on‐line ) S25 TI ( surf N2 web or surf N2 net ) or AB ( surf N2 web or surf N2 net ) S26 ti consumer health informatic* or ab consumer health informatic* S27 ti e‐health or ab e‐health S28 S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 S29 S9 and S28 S30 (MH "Clinical Trials+") S31 PT clinical trial S32 TI clinical* trial* or AB clinical* trial* S33 TI singl* blind* or TI singl* mask* or TI doub* blind* or TI doubl* mask* or TI trebl* blind* or TI trebl* mask* or TI tripl* blind* or TI tripl* mask* S34 AB singl* blind* or AB singl* mask* or AB doub* blind* or AB doubl* mask* or AB trebl* blind* or AB trebl* mask* or AB tripl* blind* or AB tripl* mask* S35 TI Randomi?ed control* trial* or AB Randomi?ed control* trial* S36 (MH "Random Assignment") S37 TI Random* allocat* or AB Random* allocat* S38 TI Placebo* or AB Placebo* S39 (MH "Placebos") S40 (MH "Quantitative Studies") S41 TI Allocat* random* or AB Allocat* random* S42 S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 S43 S29 and S42 |
| Web of Science |
| #1 (obes* or overwieght or body weight or body mass index or bmi) in Title #2 (computer* or pc or pcs or software or mutimedia or multi‐media or interactive or cd‐rom* or compact disk*or compact disc* or internet or web‐based or world wide web or online or on‐line or e‐health or consumer* health informatic*) in Topic #3 ((trial* or random* or placebo* or control* or double or treble or triple or blind* or mask* or allocat* or prospective* or volunteer*or comparative or evaluation or follow‐up or follow up)) in Topic #4 #1 and #2 and #3 |
| Dissertation Abstracts |
| obes* OR overwieght OR body weight OR body mass index OR bmi in Citation and Abstract AND computer* OR pc OR pcs OR software OR mutimedia OR multi‐media OR interactive OR cd‐rom* OR compact disk*OR compact disc* OR internet OR web‐based or world wide web OR online OR on‐line OR e‐health OR consumer* health informatic*) in Citation and Abstract |
| PsycINFO |
| 1. exp Obesity/
2. obes$.tw.
3. exp Overweight/
4. overweight.tw.
5. exp Body Weight/
6. (body adj (weight or mass)).tw.
7. exp Body Mass Index/
8. (body mass index or bmi).tw.
9. or/1‐8
10. exp computers/
11. exp computer software/
12. exp Computer Assisted Therapy/
13. computer$.tw.
14. (pc or pcs).tw.
15. (multi‐media or multimedia).tw.
16. interactive.tw.
17. exp Computer Assisted Instruction/
18. exp Information Technology/
19. cd‐rom.tw.
20. (compact adj dis?$).tw.
21. internet.tw.
22. (world adj wide adj web).tw.
23. (web adj based).tw.
24. (online or on‐line).tw. 25. (surf$ adj2 (web or net)).tw. 26. e‐health.tw. 27. (consumer$ adj health adj informatic$).tw. 28. or/10‐27 29. 9 and 28 |
| Cochrane Medicine Field Specialized Register |
| Obesity in Health Condition Computer‐based intervention OR web‐based intervention in Intervention |
| CRISP |
| Search 1: Obesity and computer Obesity and software Obesity and multimedia Obesity and internet Obesity and online Obesity and web Search 2: Overweight and computer Overweight and software Overweight and multimedia Overweight and internet Overweight and online Overweight and web |
Appendix 2. Descriptions of interventions
|
Characteristic Study ID |
Design | Intervention(s) | Control(s) |
| Bennett 2010 | Parallel RCT | Internet‐based interactive weight loss approach. Participants collaborated with health coach to select series of behavior change goals, and were encouraged to use website for regular self monitoring. Behavioral skills training and regular health coach support also provided. | Current standard of outpatient care plus a copy of the 'Aim for a Healthy Weight' written materials published by the National Heart, Lung and Blood Institute |
| Cussler 2008 | Cluster‐RCT | Internet‐based program with private mail, group mail, bulletin board, chat rooms, monitoring tools for weight, physical activity and diet, curriculum materials, dietary and physical activity information, and links to websites of interest | Continue to practice principles learned during weight loss intervention. No contact with study staff except for testing. |
| DeLucia 1988 | Parallel RCT | (1) Ferguson behavioral program plus The Eating Machine (Thorne 1982), a nutritional software intervention administered in weekly 90‐minute Applie IIe computer sessions. Computerized feedback of user dietary patterns. (2) Ferguson behavioral program plus EATS (Byrd‐Bredbenner 1981), a nutritional software intervention administered in weekly 90‐minute Apple IIe computer sessions. Computerized feedback of user dietary patterns. | Ferguson program only. No computerized intervention. |
| Gabriele 2011 | Parallel RCT | (1) Internet‐based program supplemented with directive e‐coach support (2) Internet‐based program supplemented with non‐directive e‐coach support | Internet‐based program with minimal support |
| Harvey‐Berino 2002 | Parallel RCT | Internet support. 52 weeks of bi‐weekly Internet chat sessions facilitated by a group therapist. E‐mail from group therapist in weeks when meetings not held. | (1) Frequent in‐person support. 52 weeks of bi‐weekly in‐person group therapist meetings. Phone calls from therapist in weeks when meetings not held. (2) Minimal in‐person support. Six months of monthly in‐person support group meetings. No contact between meetings. No contact for months 7 to 12. |
| Harvey‐Berino 2010 | Parallel RCT | Weight loss program with online recording of diet, physical activity and weight, and weekly online chat sessions | (1) Weight loss program with online recording of diet, physical activity and weight, and weekly online chat sessions, with the exception that once per month the meetings were in‐person (2) Weight loss program with paper recording of diet, physical activity and weight, and weekly in‐person chat sessions |
| Hunter 2008 | Parallel RCT | Behavioral Internet treatment. Submission of electronic food and exercise diaries at least 5 times a week, weekly counselor feedback and weekly website lessons and quizzes. | Usual care |
| Morgan 2009 | Parallel RCT | Internet weight loss program. Self monitoring of diet and activity with regular feedback based on participant online entries. Information session and program booklet. | Information session (modified) and program booklet |
| Morgan 2011 | Cluster RCT | Internet weight loss program with online eating, exercise and weight monitoring, and individualized e‐mail feedback. Information session, program booklet and group‐based financial incentives | Wait list control |
| Schroder 2010 | Parallel quasi‐RCT | (1) Computer‐assisted dieting intervention. Provision of interactive diet software. (2) Computer‐assisted dieting intervention plus in‐person intervention. Provision of interactive diet software plus 4 sessions of in‐person self management group training. | Wait list control |
| Svetkey 2008 | Parallel RCT | (1) In‐person support. 30 months of person‐to‐person guidance and support by telephone for 5 to 15 minutes each month except for every fourth month. Every fourth month included 45‐ to 60‐minute face‐to‐face contact. Self reported weight (or measured weight each fourth month), review of progress and action plans. (2) Interactive technology‐based intervention. Unlimited access to weight loss maintenance support website, weekly login encouraged. Self monitoring of physical activity and calorie intake, and reporting of current weight. E‐mail prompts and automated telephone calls if failure to make self scheduled logins | Self directed weight maintenance. Receipt of printed life‐style guidelines and meeting with study interventionist at randomizations and after 12‐month data collection visit. |
| Tate 2001 | Parallel RCT | Internet behavioral therapy. Internet education, plus weekly submission of electronic self monitoring diaries, together with any questions or comments, to a behavioral therapist. Weekly e‐mail received from therapist with behavioral weight loss lesson and individualized feedback as well as answers to questions. Access to electronic bulletin board for social support from other participants. | Internet educational intervention. Given access to study website with basic information related to weight loss and an organized directory of selected Internet resources. One‐hour lesson on behavioral weight control. Encouraged to use the self monitoring web resources to track diet and exercise. |
| Tate 2003 | Parallel RCT | Internet weight loss program plus weekly e‐mail behavioral counselling | Internet weight loss program only |
| Tate 2006 | Parallel RCT | (1) Internet weight loss program plus weekly e‐mail behavioral counselling (2) Internet weight loss program plus weekly automated computer feedback | Internet weight loss program only |
| Threlfall 1984 | Parallel RCT | Jeffrey and Katz weight loss manual plus computer‐based lessons written by the study author that included self regulatory activities and management and additional practice of Jeffrey and Katz learning | Jeffrey and Katz weight loss manual only |
| Webber 2008 | Parallel RCT | Internet weight loss program with study website, online self monitoring, and message boards, with addition of moderated online chat group sessions | Internet weight loss program with study website, online self monitoring and message boards |
| Wing 2006 | Parallel RCT | (1) Internet weight maintenance program incorporating self monitoring and feedback (2) In‐person weight maintenance program incorporating self monitoring and feedback | Quarterly newsletters |
| Wylie‐Rosett 2001 | Parallel RCT | (1) Computerized weight loss intervention. Workbook plus interactive computerized tailored behavioral goals based upon participant input. (2) Computerized weight loss intervention. Workbook plus interactive computerized tailored behavioral goals based upon participant input and staff consultation. |
Workbook |
Appendix 3. Baseline characteristics (I)
|
Characteristic Study ID |
Intervention(s) and control(s) | Participating populationa | Country | Setting | Sex [female%] | Age [mean years (SD)] |
| Bennett 2010 | I: Internet‐based interactive weight loss approach; health coach support C: current standard of outpatient care and written materials |
Obese and hypertensive patients who visited the internal medicine department of a large outpatient practice | USA | outpatient community |
T: 47.5 I: 41.2 C: 54.0 |
T: 54.4 (8.1) I: 54.4 (7.4) C: 54.5 (8.9) |
| Cussler 2008 | I: Internet‐based program C: continue to practice principles during weight loss intervention |
Women who had completed participation in a 4‐month behavioral weight‐loss program | USA | community | T: 100 I: 100 C: 100 |
T: 48.0 (4.4) I: 48.0 (4.6) C: 48.4 (4.3) |
| DeLucia 1988 | I1: Ferguson behavioral program and nutritional software 'The Eating Machine' I2: Ferguson behavioral program and nutritional software 'EATS' C: Ferguson program |
Participants recruited through a university faculty‐staff newsletter | USA | university community |
T: 90 I1: 90 I2: 90 C: 89 |
T: 40.6 I1: ‐ I2: ‐ C: ‐ |
| Gabriele 2011 | I1: Internet‐based program and directive e‐coach support I2: Internet‐based program and non‐directive e‐coach support C: Internet‐based program with minimal support |
C: Internet‐based program with minimal support | USA | academic | T: 84 I1: 80 I2: 86 C: 85 |
T: 45.4 (8.7) I1: 42.9 (7.5) I2: 46.6 (8.5) C: 46.8 (9.6) |
| Harvey‐Berino 2002 | I: Internet support C1: frequent in‐person support C2: minimal in‐person support |
Participants, recruited from newspaper advertisements, who completed a 24‐week weight loss program | USA | community | 85 I: 90 C1: 86 C2: 81 |
48.4 (9.6) I: 46.3 (11.1) C1: 49.8 (8.4) C2: 49.1 (9.1) |
| Harvey‐Berino 2010 | I: online recording and chat sessions C1: online recording and chat sessions and in‐person meetings C2: paper recording and in‐person chat sessions |
Participants recruited from 2 clinical centres | USA | outpatient clinical centres |
T: 93 I: 92 C1: 94 C2: 94 |
T: 46.6 (9.9) I: 46.2 (9.8) C1: 46.7 (9.6) C2: 46.7 (10.2) |
| Hunter 2008 | I: behavioral Internet treatment C: usual care |
Active duty military personnel recruited through e‐mail advertisements and flyers | USA | military medical research centre | T: 50 I: 50 C: 50 |
T: 33.9 (7.3) I: 33.5 (7.4) C: 34.4 (7.2) |
| Morgan 2009 | I: Internet weight loss program; information session and program booklet C: information session (modified) and program booklet |
Male university staff and students recruited from university notice boards and website | Australia | community university |
T: 0 I: 0 C: 0 |
T: 35.9 (11.1) I: 37.5 (10.4) C: 34.0 (11.6) |
| Morgan 2011 | I: Internet weight loss program; information session and program booklet; group‐based financial incentives C: wait list |
Male shift workers recruited from the workplace | Australia | workplace | T: 0 I: 0 C: 0 |
T: 44.4 (8.6) I: 44.8 (8.3) C: 43.7 (9.1) |
| Schroder 2010 | I1: computer‐assisted intervention and interactive software I2: computer‐assisted intervention and interactive software; in‐person self management group training C: wait list |
Participants recruited through announcements in local newspapers and radio stations | USA | outpatient community |
T: 85 I1: 87 I2: 84 C: 83 |
T: 42.6 (10.7) I1: ‐ I2: ‐ C: ‐ |
| Svetkey 2008 | I1: in‐person support I2: interactive technology‐based intervention; weight loss maintenance support website C: printed life‐style guidelines; meeting with study interventionist |
Participants taking hypertension or dyslipidemia medications, who completed a 6‐month weight loss program and lost at least 4 kg | USA | academic medical centres | 63 I1: 62 I2: 63 C: 65 |
55.6 (8.7) I1: 55.4 (9.1) I2: 55.7 (8.5) C: 55.8 (8.5) |
| Tate 2001 | I: Internet behavioral therapy C: Internet educational intervention |
Participants, employed by a large network of hospitals with access to e‐mail and the Internet, recruited through a series of 2 e‐mail messages and an advertisement posted to the work site's Intranet website | USA | academic medical centre | T: 89 I: 89 C: 89 |
T: 40.9 (10.6) I: 41.1 (11.6) C: 40.6 (9.7) |
| Tate 2003 | I: Internet weight loss program and weekly e‐mail behavioral counselling C: Internet weight loss program |
Participants, recruited from newspaper advertisements, who were overweight or obese, and had at least one additional risk factor for type 2 diabetes | USA | academic medical centre | T: 89 I: 91 C: 89 |
T: 48.5 (9.4) I: 49.8 (9.3) C: 47.3 (9.5) |
| Tate 2006 | I1: Internet weight loss program and weekly e‐mail behavioral counselling I2: Internet weight loss program and weekly automated computer feedback C: Internet weight loss program |
Participants, recruited from newspaper advertisements, who were overweight or obese, and were willing to use meal replacements as part of the dietary regimen | USA | academic medical centre | 84 I1: 84 I2: 87 C: 82 |
49.2 (9.9) I1: 47.9 (9.8) I2: 49.7 (11.4) C: 49.9 (8.3) |
| Threlfall 1984 | I: weight loss manual plus computer‐based lessons C: weight loss manual |
Participants recruited from posters, handouts and counselor contacts.The study was an independent‐study college course. | USA | university course | T: 91 I: ‐ C: ‐ |
‐ |
| Webber 2008 | I: Internet weight loss program and online chat group sessions C: Internet weight loss me |
Female participants recruited through newspaper advertisements | USA | academic medical centre | T: 100 I: 100 C: 100 |
T: 50.0 (9.9) I: 49.3 (10.6) C: 50.8 (9.3) |
| Wing 2006 | I1: Internet weight maintenance program I2: in‐person weight maintenance program C: quarterly newsletters |
Adults, recruited through newspaper advertisements, brochures, and contacts with commercial and research weight‐control programs, who had lost at least 10% of their body weight during the previous 2 years | USA | academic medical centre community |
T: 81 I1: 81 I2: 80 C: 83 |
T: 51.3 (10.1) I1: 50.9 (9.3) I2: 51.0 (10.3) C: 52.0 (10.8) |
| Wylie‐Rosett 2006 | I1: computerized weight loss intervention and workbook I2: computerized weight loss intervention, workbook and staff consultation C: workbook |
Participants recruited from HMO and surrounding community using a variety of techniques, who had a BMI greater than 25 or a BMI of 24 plus at least one cardiovascular risk factor | USA | health maintenance organization (HMO) | T: 81.5 I1: 83 I2: 82 C: 86 |
T: 52.6 (11.3) I1: 52.7 (11.27) I2: 51.6 (12.14) C: 52.5 (11.5) |
|
Footnotes "‐" denotes not reported a duration of obesity/overweight not stated in any study. Abbreviations: BMI: body mass index; C: control; HMO: health maintenance organization; I: intervention; T: total | ||||||
Appendix 4. Baseline characteristics (II)
|
Characteristic Study ID |
Intervention(s) and control(s) | BMI [mean kg/m2(SD)] | Weight [mean (SD) lb or kg] a | Ethnic groups [%] | Duration of intervention/follow‐up |
| Bennett 2010 | I: Internet‐based interactive weight loss approach; health coach support C: current standard of outpatient care and written materials |
T: 34.6 (3.2) I: 35.0 (3.5) C: 34.6 (3.2) |
T: 97.3 (10.9) kg I: 101.l0 (15.4) C: 97.3 (10.9) |
T: 50 White, 31 Black, 5 Hispanic, 15 other I: 45 White, 37 Black, 6 Hispanic, 12 other C: 54 White, 24 Black, 4 Hispanic, 18 other |
12 weeks |
| Cussler 2008 | I: Internet‐based program C: continue to practice principles during weight loss intervention |
T: 30.7 (3.6) I: 31.09 (3.9) C: 30.4 (3.3) |
T: 83.7 (11.8) kg I: 84.6 (12.9) kg C: 82.8 (10.7) kg |
Primarily white, numbers not stated | 12 months |
| DeLucia 1988 | I1: Ferguson behavioral program and nutritional software 'The Eating Machine' I2: Ferguson behavioral program and nutritional software 'EATS' C: Ferguson program |
‐ | T: 174.2 (39.1) lb I1: 173.3 (43.36) lb I2: 176.72 (40.52) lb C: 172.32 (36.92) lb |
‐ | 10 weeks |
| Gabriele 2011 | I1: Internet‐based program and directive e‐coach support I2: Internet‐based program and non‐directive e‐coach support C: Internet‐based program with minimal support |
T: 32.07 (4.3) I1: 32.60 (4.58) I2: 31.56 (4.61) C: 32.04 (3.81) |
T: 87.9 (13.8) kg I1: 90.88 (15.14) kg I2: 85.67 (13.33) kg C: 87.27 (12.52) kg |
T: 71 Caucasian I1: 77 Caucasian I2: 60 Caucasian C: 76 Caucasian |
12 weeks |
| Harvey‐Berino 2002 | I: Internet support C: frequent in‐person support C2: minimal in‐person support |
T: 32.2 (4.5)b I: 32.2 (4.0) C1: 31.5 (4.8) C2: 32.8 (4.6) |
T: 88.7 (13.3) kgb I: 89.3 (15.3) C1: 86.5 (10.1) C2: 9.2 (13.9) |
T: 98 White I: 97 White C1: 100 White C2: 97 White |
52 weeks |
| Harvey‐Berino 2010 | I: online recording and chat sessions C1: online recording and chat sessions and in‐person meetings C2: paper recording and in‐person chat sessions |
T: 35.7 (5.6) I: 35.6 (5.7) C1: 35.6 (5.5) C2: 36.0 (5.7) |
T: 97.0 (17.7) kg I: 97.2 (18.7) C1: 96.5 (16) C2: 97.4 (18.5) |
T: 28 African‐American I: 30 African‐American C1: 26 African‐American C2: 29 African‐American |
6 months |
| Hunter 2008 | I: behavioral Internet treatment C: usual care |
T: 29.3 (3.0) I: 29.4 (3.0) C: 29.3 (3.0) |
T: 87.0 (15.1) kg I: 87.4 (15.6) kg C: 86.6 (14.7) kg |
T: 56 White I: 58 White C: 53 White |
6 months |
| Morgan 2009 | I: Internet weight loss program; information session and program booklet C: information session (modified) and program booklet |
T: 30.6 (2.8) I: 30.6 (2.7) C: 30.5 (3.0) |
T: 99.1 (12.8) kg I: 99.1 (12.2) C: 99.2 (13.7) |
‐ | 3 months |
| Morgan 2011 | I: Internet weight loss program; information session and program booklet; group‐based financial incentives C: wait list |
T: 30.5 (3.6) I: 30.7 (3.6) C: 30.2 (3.5) |
T: 94.9 (13.4) kg I: 96.3 (12.9) kg C: 92.9 (14.1) kg |
‐ | 3 months |
| Schroder 2010 | I1: computer‐assisted intervention and interactive software I2: computer‐assisted intervention and interactive software; in‐person self management group training C: wait list |
T: 34.6 (5.4) I1: 34.8 (5.96) I2: 34.48 (5.03) C: 34.54 (5.28) |
T: 217.4 (36.2) lb I1: 215.22 (35.74) lb I2: 219.75 (38.35) lb C: 217.28 (35.43) lb |
T: 95 Caucasian I1: ‐ I2: ‐ C: ‐ |
3 monthsc |
| Svetkey 2008 | I1: in‐person support I2: interactive technology‐based intervention; weight loss maintenance support website C: printed life‐style guidelines; meeting with study interventionist |
T: 34.1 (4.8)b I1: 34.2 (4.8) I2: 34.2 (4.9) C: 34.0 (4.8) |
T: 88.2 (15.8) kg I1: 88.7 (16.9) kg I2: 88.6 (15.4) kg C: 87.4 (15.3) kg |
T: 38 African‐American, 62 non‐African American I1: 39 African‐American, 61 non‐African American I2: 38 African‐American, 62 non‐African American C: 37 African‐American, 63 non‐African American |
30 months |
| Tate 2001 | I: Internet behavioral therapy C: Internet educational intervention |
T: 29.0 (3.0) I: 29.1 (3.0) C: 28.9 (3.1) |
T: 78.1 (10.5) kg I: 77.4 (9.4) kg C: 78.8 (11.6) kg |
T: 84 White I: 89 White C: 78 White |
6 months |
| Tate 2003 | I: Internet weight loss program and weekly e‐mail behavioral counselling C: Internet weight loss program |
T: 33.1 (3.8) I: 32.5 (3.8) C: 33.7 (3.7) |
T: 87.8 (13.5) kg I: 86.2 (14.3) kg C: 89.4 (12.6) kg |
T: 89 White I: 89 White C: 89 White |
12 months |
| Tate 2006 | I1: Internet weight loss program and weekly e‐mail behavioral counselling I2: Internet weight loss program and weekly automated computer feedback C: Internet weight loss program |
32.6 (3.5) I1: 32.8 (3.4) I2: 32.7 (3.5) C: 32.3 (3.7) |
T: 88.8 (13.3) kg I1: 89.0 (13.0) kg I2: 89.0 (13.2) kg C: 88.3 (13.9) kg |
T: 10 minority ethnicity I1: 13 minority ethnicity I2: 10 minority ethnicity C: 9 minority ethnicity |
6 months |
| Threlfall 1984 | I: weight loss manual plus computer‐based lessons C: weight loss manual |
‐ | T: 176.3 (26.4) lb I: 181.5(31.3) lb C: 171.4(21.9) lb |
‐ | 10 weeks |
| Webber 2008 | I: Internet weight loss program and online chat group sessions C: Internet weight loss program |
T: 31.1 (3.7) I: 30.8 (4.0) C: 31.4 (3.3) |
T: 82.3 (11.21) kg I: 82.1 (13.6) kg C: 82.5 (8.4) kg |
T: 86 White I: 88 White C: 85 White |
16 weeks |
| Wing 2006 | I1: Internet weight maintenance program I2: in‐person weight maintenance program C: quarterly newsletters |
T: 28.6 (4.8) I1: 28.1 (4.6) I2: 28.7 (4.7) C: 29.1 (5.0) |
T: 77.8 (16.1) kg I1: 76.0 (16.4) kg I2: 78.6 (17.1) kg C: 78.8 (14.8) kg |
‐ | 18 months |
| Wylie‐Rosett 2006 | I1: computerized weight loss intervention and workbook I2: computerized weight loss intervention, workbook and staff consultation C: workbook |
T: 36 (6.5) I1: 35.7(6.7) I2:35.16 (6.5) C: 36.5(6.0) |
T: 214.2 (44.1) lb I1: 213.3 (44.0) lb I2: 211.8 (43.4) lb C: 220.8 (45.6) lb |
T: 84 White I1: 83 White I2: 82 White C: 86 White |
12 months |
|
Footnotes "‐" denotes not reported a conversion factor between pounds and kilograms used in this review is 1 lb = 0.4536 kg. b at start of weight‐loss intervention. c control group patients were distributed between intervention groups, and intervention continued for additional three months. Abbreviations: BMI: body mass index; C: control; I: intervention; T: total | |||||
Appendix 5. Matrix of study endpoints
|
Characteristic Study ID |
Primary endpoint(s) | Secondary endpoint(s) | Other endpoint(s) |
| Bennett 2010 | Change in body weight (absolute weight change in kg ‐ at least 5 kg) | Change in BMI, blood pressure control and waist circumference | |
| Cussler 2008 | Change in body weight (absolute weight change in kg and percentage total weight) | ‐ | Change in BMI, change in body composition (percent fat, total body fat and fat‐free mass), and change in calorie intake |
| DeLucia 1988 | Change in body weight (absolute weight change in lb) | Percentage excess weight lost (lb lost/lb overweight) | |
| Gabriele 2011 | Change in body weight and waist circumference | Change in physical activity, dietary behavior, and program engagement with the intervention | |
| Harvey‐Berino 2002 | Change in body weight | Energy intake and energy expended in physical activity | |
| Harvey‐Berino 2010 | Change in body weight | ‐ | Change in BMI, change in dietary energy intake and percent fat intake, energy expended in physical activity |
| Hunter 2008 | Change in body weight (absolute weight change in kg and percentage change from baseline), change in percent body fat, change in waist circumference | ‐ | Changes in dietary intake of fat, fruit, vegetables and fibre, and changes in physical activity |
| Morgan 2009 | Change in body weight (absolute weight change in kg and percentage change from baseline) | BMI, waist circumference, blood pressure, physical activity, dietary intake | |
| Morgan 2011 | Change in body weight | Waist circumference, BMI, blood pressure, resting heart rate | |
| Schroder 2010 | Change in body weight (absolute change in lb) and change in BMI | Lipid panel results, including total blood cholesterol, HDL, LDL, ratio of total cholesterol to HDS and triglycerides | |
| Svetkey 2008 | Weight change (absolute weight change in kg) from the end of the initial weight loss program to the end of the 30‐month weight maintenance intervention period | ‐ | Change in weight from entry into weight loss program to end of study, dichotomous measures of weight change (maintenance of 4 kg weight loss or more, no net weight gain from entry, 5% or more weight loss from entry, 3% or less weight gain from randomization). Changes in total energy intake (kcal/d) and MVPA (min/wk) |
| Tate 2001 | Change in body weight (absolute change in kg) measured at 6 and 12 months | ‐ | Waist circumference, Paffenbarger activity questionnaire, Block Food Frequency questionnaire, Centers for Epidemiological Studies Depression Scale |
| Tate 2003 | Weight change at 12 months | ‐ | Waist circumference, venous blood glucose, Paffenbarger activity questionnaire, Block Food Frequency questionnaire, Centres for Epidemiological Studies Depression Scale |
| Tate 2006 | Weight change at 6 months | Dietary intake (total calories and percent calories from fat), energy expenditure (kcal/week) | |
| Threlfall 1984 | ‐ | ‐ | Change in weight (pounds), percent reduction in excess body weight and costs |
| Webber 2008 | Weight change at 16 weeks | ‐ | Dietary intake (calories, percent fat), physical activity (kcal/week) |
| Wing 2006 | Weight change at 18 months | Percentage of participants gaining 2.3 kg or more, changes in diet, changes in physical activity, use of behavioral strategies | |
| Wylie‐Rosett 2001 | ‐ a | ‐ | Body weight, body composition, waist and hip circumference, lipid measurements, blood pressure, physical activity and dietary intake |
|
Footnotes "‐" denotes not reported Primary or secondary endpoint(s) refer to verbatim statements in the publication, other endpoints relate to outcomes which were not specified as 'primary' or 'secondary' outcomes in the publication. a change in body weight was not specified as a primary outcome, but was used to calculate sample size. Abbreviations: BMI: body mass index; C: control; I: intervention; HDL: high‐density lipoprotein; LDL: low‐density lipoprotein; MVPA: moderate to vigorous physical activity | |||
Appendix 6. Adverse events
|
Characteristic Study ID |
Intervention(s) and control(s) | Deaths [n] | Adverse events [n] a | Serious adverse events (n) | Dropouts due to adverse events [n] | Hospitalisation [n] | Outpatient treatment [n] | Symptoms [n] |
| Bennett 2010 | I: Internet‐based interactive weight loss approach; health coach support C: current standard of outpatient care and written materials |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Cussler 2008 | I: Internet‐based program C: continue to practice principles during weight loss intervention |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| DeLucia 1988 | I1: Ferguson behavioral program and nutritional software 'The Eating Machine' I2: Ferguson behavioral program and nutritional software 'EATS' C: Ferguson program |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Gabriele 2011 | I1: Internet‐based program and directive e‐coach support I2: Internet‐based program and non‐directive e‐coach support C: Internet‐based program with minimal support |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Harvey‐Berino 2002 | I: Internet support C: frequent in‐person support C2: minimal in‐person support |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Harvey Berino 2010 | I: online recording and chat sessions C1: online recording and chat sessions and in‐person meetings C2: paper recording and in‐person chat sessions |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Hunter 2008 | I: behavioral Internet treatment C: usual care |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Morgan 2009 | I: Internet weight loss program; information session and program booklet C: information session (modified) and program booklet |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Morgan 2011 | I: Internet weight loss program; information session and program booklet; group‐based financial incentives C: wait list |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Schroder 2010 | I1: computer‐assisted intervention and interactive software I2: computer‐assisted intervention and interactive software; in‐person self management group training C: wait list |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Svetkey 2008 | I1: in‐person support I2: interactive technology‐based intervention; weight loss maintenance support website C: printed life‐style guidelines; meeting with study interventionist |
I1: 1/342 I2: 1/348 C1: 1/342 T: 3/1032 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Tate 2001 | I: Internet behavioral therapy C: Internet educational intervention |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Tate 2003 | I: Internet weight loss program and weekly e‐mail behavioral counselling C: Internet weight loss program |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Tate 2006 | I1: Internet weight loss program and weekly e‐mail behavioral counselling I2: Internet weight loss program and weekly automated computer feedback C: Internet weight loss program |
T: 0 | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Threlfall 1984 | I: weight loss manual plus computer‐based lessons C: weight loss manual |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Webber 2008 | I: Internet weight loss program and online chat group sessions C: Internet weight loss program |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Wing 2006 | I1: Internet weight maintenance program I2: in‐person weight maintenance program C: quarterly newsletters |
T: 0 | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
| Wylie‐Rosett 2001 | I1: computerized weight loss intervention and workbook I2: computerized weight loss intervention, workbook and staff consultation C: workbook |
T: 0 | T: ‐ | T: 0 | T: 0 | T: 0 | T: 0 | T: 0 |
|
Footnotes "‐" denotes not reported a No study made any mention of adverse effects with the exception of Wing 2006, which reported that there were no serious adverse events and Tate 2006, which reported that there were no significant adverse events. Abbreviations: C: control; I: intervention; T: total | ||||||||
Data and analyses
Comparison 1. Weight loss: computer vs minimal interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 3 mo | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Computer group includes computer plus in‐person intervention | 5 | 430 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.41, ‐1.55] |
| 1.2 Comparison excludes quasi‐randomized trial (Schroder 2010) | 4 | 339 | Mean Difference (IV, Random, 95% CI) | ‐2.76 [‐3.67, ‐1.85] |
| 1.3 Computer group excludes computer plus in‐person intervention | 5 | 399 | Mean Difference (IV, Random, 95% CI) | ‐2.52 [‐3.44, ‐1.60] |
| 1.4 Comparison excludes workplace setting trial | 4 | 320 | Mean Difference (IV, Random, 95% CI) | ‐2.18 [‐2.90, ‐1.46] |
| 1.5 Trials including only men | 2 | 175 | Mean Difference (IV, Random, 95% CI) | ‐3.13 [‐5.58, ‐0.69] |
| 1.6 Trials including both men and women | 3 | 255 | Mean Difference (IV, Random, 95% CI) | ‐1.97 [‐2.93, ‐1.01] |
| 2 Weight at 6 mo | 2 | 511 | Mean Difference (IV, Random, 95% CI) | ‐1.52 [‐2.13, ‐0.90] |
| 3 Weight at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Change in weight at 3 mo | 1 | 101 | Mean Difference (IV, Random, 95% CI) | ‐2.99 [‐4.08, ‐1.90] |
| 5 Change in weight at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 BMI at 3 to 4 mo | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Computer group includes computer plus in‐person intervention | 4 | 367 | Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.35, ‐0.57] |
| 6.2 Computer group excludes computer plus in‐person intervention | 4 | 336 | Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐1.36, ‐0.61] |
| 7 BMI at 6 to 7 mo | 2 | 464 | Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐0.92, ‐0.45] |
| 8 BMI at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Waist circumference at 3 mo [cm] | 3 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 9.1 Waist circumference at 3 mo | 3 | 276 | Mean Difference (Random, 95% CI) | ‐2.95 [‐6.17, 0.27] |
| 9.2 Waist circumference at 3 mo (sensitivity analysis without Morgan 2011) | 2 | 166 | Mean Difference (Random, 95% CI) | ‐1.44 [‐3.05, 0.17] |
| 10 Waist circumference at 6 mo | 2 | 464 | Mean Difference (IV, Random, 95% CI) | ‐1.68 [‐2.45, ‐0.91] |
| 11 Waist circumference at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Energy intake at 3 to 4 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13 Energy intake at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14 Energy intake at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Energy intake from fat at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16 Energy intake from fat at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Dietary fibre at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18 Physical activity at 3 mo | 2 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 18.1 Total MET minutes (log transformed) | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Mean steps/day | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Physical activity at 6 mo | 2 | 464 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.22, 0.14] |
| 20 Physical activity at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Computer group includes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Computer group excludes computer plus in‐person intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Weight loss: computer vs in‐person interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 6 mo | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Computer vs in‐person | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Computer vs hybrid computer/in‐person | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Change in weight at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Computer vs in‐person | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Computer vs hybrid computer/in‐person | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Weight loss: computer‐delivered interaction as adjunct to Internet program.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 3 to 4 mo | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 3 | 352 | Mean Difference (IV, Random, 95% CI) | ‐2.14 [‐2.85, ‐1.43] |
| 1.2 Adjunct interactive computer group includes only e‐mail feedback | 3 | 291 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.14, ‐1.45] |
| 1.3 Adjunct interactive computer group includes only automated feedback | 1 | 128 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐3.15, ‐0.45] |
| 1.4 Adjunct interactive computer group was non‐directive e‐coaching | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐2.17, 1.67] |
| 1.5 Adjunct interactive computer group participated in online group chats | 1 | 66 | Mean Difference (IV, Random, 95% CI) | 1.51 [‐0.71, 3.73] |
| 2 Weight at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Weight at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Change in weight at 3 mo | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 2 | 227 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐4.09, ‐0.87] |
| 4.2 Adjunct interactive computer group includes only e‐mail feedback | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.65 [‐4.73, ‐0.56] |
| 4.3 Adjunct interactive computer group includes only automated feedback | 1 | 102 | Mean Difference (IV, Random, 95% CI) | ‐2.60 [‐4.19, ‐1.01] |
| 4.4 Adjunct interactive computer group was non‐directive e‐coaching | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐2.29, 1.99] |
| 5 Change in weight at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Change in weight at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 BMI at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Waist circumference at 3 mo | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Adjunct interactive computer group was e‐counselling or feedback | 2 | 160 | Mean Difference (IV, Random, 95% CI) | ‐2.62 [‐4.04, ‐1.21] |
| 8.2 Adjunct interactive computer group was non‐directive e‐counselling | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐2.82, 2.16] |
| 9 Waist circumference at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10 Calories at 3 to 4 mo | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Adjunct interactive computer group participated in online group chats | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Calories at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Calories from fat at 3 to 4 mo | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.4 Adjunct interactive computer group participated in online group chats | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Calories from fat at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Adjunct interactive computer group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Adjunct interactive computer group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Calories from fat at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15 Physical activity at to 4 mo | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Adjunct interactive computer group includes both e‐mail and automated feedback | 2 | 250 | Mean Difference (IV, Random, 95% CI) | 346.87 [93.88, 599.86] |
| 15.2 Adjunct interactive computer group includes only e‐mail feedback | 2 | 203 | Mean Difference (IV, Random, 95% CI) | 353.45 [96.19, 610.70] |
| 15.3 Adjunct interactive computer group includes only automated feedback | 1 | 102 | Mean Difference (IV, Random, 95% CI) | 189.30 [‐375.33, 753.93] |
| 15.4 Adjunct interactive computer group participated in online chats | 1 | 65 | Mean Difference (IV, Random, 95% CI) | 498.0 [‐510.96, 1506.96] |
| 16 Physical activity at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Interactive group includes both e‐mail and automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Interactive group includes only e‐mail feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Interactive group includes only automated feedback | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Physical activity at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. Weight loss: Computer intervention as adjunct to in‐person program.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 10 weeks | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Weight at 6 mo after end of treatment | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 5. Weight maintenance: computer vs minimal intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 6 mo [kg] | 2 | 897 | Mean Difference (Random, 95% CI) | ‐0.70 [‐1.17, ‐0.23] |
| 2 Weight at 12 mo [kg] | 3 | 1004 | Mean Difference (Random, 95% CI) | ‐0.78 [‐1.38, ‐0.17] |
| 3 Weight at 18 mo [kg] | 2 | 897 | Mean Difference (Random, 95% CI) | ‐0.73 [‐1.60, 0.14] |
| 4 Weight at 24 mo [kg] | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 5 Weight at 30 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Change in weight at 30 mo [%] | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 7 BMI at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Energy intake at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Energy intake at 30 mo [kcal/day] | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 10 Energy expenditure at 12 mo | 1 | 107 | Mean Difference (IV, Random, 95% CI) | ‐7.00 [‐117.14, 103.14] |
Comparison 6. Weight maintenance: computer vs infrequent in‐person support.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 6 mo [kg] | 2 | 897 | Mean Difference (Random, 95% CI) | 0.54 [‐0.53, 1.62] |
| 2 Weight at 12 mo [kg] | 3 | 955 | Mean Difference (Random, 95% CI) | 1.56 [‐0.12, 3.23] |
| 3 Weight at 18 mo [kg] | 2 | 897 | Mean Difference (Random, 95% CI) | 1.12 [‐0.20, 2.45] |
| 4 Weight at 24 mo [kg] | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 5 Weight at 30 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Change in weight at 30 mo [%] | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 7 Energy intake at 30 mo [kcal/day] | 1 | Mean Difference (Random, 95% CI) | Totals not selected |
Comparison 7. Weight maintenance: computer vs frequent in‐person support.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight at 6 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Weight at 12 mo | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bennett 2010.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Age 25 to 65 years, diagnosed hypertension and use of hypertension medication, non‐smoker for at least 6 months prior to recruitment, fluency in English, and home or work access to a computer with Internet access EXCLUSION CRITERIA: current pregnancy, history of a medical illness that would prohibit exercise, such as known dementia, cancer or stroke DIAGNOSTIC CRITERIA: BMI 30.0 to 40.0 kg/m2 CO‐MORBIDITIES: all participants had been diagnosed with hypertension and were taking hypertension medication CONCOMITANT TREATMENTS: none |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: outpatient/community TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL FUNDING: Sanofi Aventis NON‐COMMERCIAL FUNDING: authors supported by NCI grants PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "We aimed to create a moderate‐intensity weight loss intervention that, in contrast to traditional approaches ... would have minimal barriers to participant uptake, be well suited for web‐based implementation, and be sustainable in a wide range of practice settings. " | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized, but method not stated |
| Allocation concealment (selection bias) | Low risk | Randomization assignments enclosed in nontransparent envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | All research staff collecting evaluation data blinded to randomization status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 43 out of 51 participants randomized to the Intervention group completed the study 42 out of 50 participants randomized to the usual care group completed the study Reason for loss of follow‐up in both groups was inability to contact or discontinued intervention For intention‐to‐treat analysis, authors used a baseline carried forward imputation approach |
| Selective reporting (reporting bias) | Low risk | All of the outcomes listed in the methods section were reported as results |
| Other bias | Low risk | |
Cussler 2008.
| Methods | PARALLEL CLUSTER‐RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight maintenance component of weight loss intervention trial. Age 40 to 55 years, non‐smoker and access to a computer that could run an Internet browser and Java scripts EXCLUSION CRITERIA: major medical illnesses, participation in any other weight loss program DIAGNOSTIC CRITERIA: BMI 25.0 to 38.0 kg/m2 at start of weight loss intervention CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: both groups attended weekly support group meetings |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: community TREATMENT BEFORE STUDY: weight maintenance was preceded by a 4‐month behavioral weight loss intervention |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: NIH grant PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "We hypothesized that ... women assigned to an Internet weight loss maintenance program would regain less weight than women assigned to a self‐directed, maintenance program. " | |
| Notes | This trial was cluster‐randomized, however the investigators had calculated an effective sample size. "Because of group randomization, a weeknight group intra class correlation was calculated using the between‐group variance divided by the sum of the between‐group variance plus the within‐group variance. For change in weight from baseline to 4 months, the intra class correlation was 0.02, producing an effective sample size of 107" (P. 1055). We used the effective sample size to adjust the sample size in the control and intervention groups proportionally for all analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 52 out of 66 participants randomized to the Internet group completed the study 59 out of 69 participants randomized to the self directed group completed the study Reasons for loss to follow‐up not stated Baseline observation carried forward method used for the final body weight of 24 participants who did not complete the weight maintenance period. Missing values for all other measured variables handled similarly. |
| Selective reporting (reporting bias) | Low risk | All of the outcomes listed in the methods section were reported as results |
| Other bias | Unclear risk | Risks of bias specific to cluster‐randomized trials were assessed as follows: Recruitment bias: report stated that groups were randomized but details of methods or procedure were not given, therefore prior knowledge of cluster assignment cannot be absolutely ruled out Baseline differences: no statistically significant differences between randomized groups Missing clusters: not present Incorrect statistical analysis: not present; the analysis took clustering into account Comparability with individually randomized trials: similar effects were seen in this trial and in the trials using individual randomization |
DeLucia 1988.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Willing to place USD 50 deposit refundable upon completing behavioral program EXCLUSION CRITERIA: student status, participating in another weight‐loss program, taking medication which might affect weight loss DIAGNOSTIC CRITERIA: at least 10 lb overweight CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: both treatment groups received Ferguson's (Ferguson 1975) behavioral intervention for weight loss, composed of stimulus control, environmental support and homework assignments including keeping of food diaries |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: university/community TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL/NON‐COMMERCIAL FUNDING: funding not stated PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The present study was designed to provide a "consumer product evaluation" of two computer‐based nutrition programs as adjuncts to the behavioral treatment of obesity. .... Should the computer programs prove to be incrementally effective on indices of nutritional knowledge, eating behavior, and/or weight loss, behavioral health specialists might rely on them to provide the necessary nutritional aspects of treatment. " | |
| Notes | We contacted the author to obtain the sample size for each intervention group and received a reply with this information on 2 April 2010 For weight outcomes, we calculated the change from baseline following procedures in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009). We calculated the correlation coefficient from a weight loss study in this review (Hunter 2008) reporting standard deviations for baseline, endpoint and change values of weight, and used the calculated correlation coefficient to impute the missing standard deviation for the change from baseline. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States participants were stratified on sex and weight and randomly assigned, but details of method of randomization not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant in each of the 3 treatment groups due to reported work or scheduling conflicts |
| Selective reporting (reporting bias) | Low risk | All of the outcomes listed in the methods section were reported as results |
| Other bias | Low risk | |
Gabriele 2011.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial for adults. Inclusion criteria were: age 30 to 60 years, access to e‐mail and BMI of 25 to 40 kg/m2 EXCLUSION CRITERIA: BMI greater than 40 kg/m2. History of myocardial infarction, stroke or cancer in the last 5 years; joint problems that would prohibit exercise, pregnancy, psychiatric hospitalization in the previous year, weight loss of more than 10 pounds during the previous 6 months, use of weight loss medications during the previous 6 months, current use of medication for which substantial weight gain is a potential side effect, and inability to read and write English fluently. DIAGNOSTIC CRITERIA: participants had to have a BMI between 25 and 40 kg/m2 CO‐MORBIDITIES: not stated CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: academic setting TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: National Heart, Lung, Blood Institute and Washington University Dissertation Fellowship PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "We hypothesized that participants in the nondirective and directive support conditions would have greater weight loss, improvements in dietary behavior and physical activity, and engagement than participants in the minimal support condition. In addition ... we expected that participants in the nondirective support condition would show greater changes in these outcomes relative to participants in the directive support condition." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned by drawing a number. For every 9 patients enrolled, 3 were randomized to each condition. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants were blinded to treatment condition, but it is not stated that assessors were also blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 31 out of 34 participants randomized to the Minimal Support Group completed the study at 12 weeks 33 out of 35 randomized to the Non‐directive Support Group completed the study at 12 weeks 32 out of 35 randomized to the Directive Support Group completed the study at 12 weeks Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All of the outcomes listed in the methods section were reported as results |
| Other bias | Low risk | |
Harvey‐Berino 2002.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight maintenance intervention trial. At least 18 years old, possess a computer with at least 16 megabytes of RAM and Windows 95 or 98 as a computer operating system, and access to a 28.8 kbps Internet connection EXCLUSION CRITERIA: history of major medical or psychiatric problems, a plan to become pregnant within the next 18 months, or inability to participate in an exercise program DIAGNOSTIC CRITERIA: BMI ≥ 25 kg/m2 at start of weight loss intervention CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: community TREATMENT BEFORE STUDY: all participants participated in a 24‐week behavioral weight control program before they were told what weight maintenance condition they had been randomized to |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: USDA Hatch Act Funds (HA 593) PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "[T]he purpose of this study was to test a novel approach to sustaining long‐term contact with individuals following participation in a structured behavioral weight loss program. We hypothesized that individuals in the Internet condition would maintain more weight loss than those in the comparable in‐person condition." | |
| Notes | In August 2010 we e‐mailed the author for information on weight maintenance outcomes at 12 months of maintenance. We were unable to obtain any response and therefore extracted data for overall change between the start of the 6‐month weight loss segment of the trial and the end of the 12‐month weight loss segment of the trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100 out of 122 participants completed the study at 6 months 92 out of 122 participants completed the study at 18 months 90 out of 122 participants had complete data for all measures Data were examined using both an intention‐to‐treat analysis and with those having complete data for all measures (90) |
| Selective reporting (reporting bias) | Low risk | All of the outcomes listed in the methods section were reported as results |
| Other bias | Low risk | |
Harvey‐Berino 2010.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Adults with a BMI between 25 and 50 kg/m2 and access to a computer with an Internet connection. EXCLUSION CRITERIA: history of major medical or psychiatric problems, a planned or recent pregnancy, medical conditions that would prohibit exercise, or a schedule that would prohibit or restrict attendance at a designated time for weekly group meetings DIAGNOSTIC CRITERIA: BMI between 25 and 50 kg/m2 CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 2 COUNTRY/LOCATION: USA SETTING: outpatient clinical centres TREATMENT BEFORE STUDY: none |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): "Primary Outcome Measures: Body Mass Index or body weight change." (ClinicalTrials.gov Identifier NCT00265954) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "[T]he purpose of this study was to directly evaluate the comparative efficacy of a comprehensive behavioral weight loss treatment program delivered online with the same program delivered in‐person and with an innovative combined in‐person and online approach." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized using a biased coin approach |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 150 out of 158 participants randomized to the In‐Person group completed the study at 6 months 153 out of 162 participants randomized to the Hybrid group completed the study at 6 months 159 out of 161 participants randomized to the Internet group completed the study at 6 months |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Hunter 2008.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Age between 18 and 65, availability of a personal computer with Internet access, and plans to remain in the local area for 1 year. EXCLUSION CRITERIA: loss of more than 10 pounds in the previous 3 months, use of prescription or over‐the‐counter weight‐loss medications in the previous 6 months, any physical activity restrictions, history of myocardial infarction, stroke or cancer in the last year, reported diabetes, angina or thyroid difficulties, or had orthopedic or joint problems that would prohibit exercise. Women were excluded if they were pregnant or breast‐feeding, or planned to become pregnant within the next year. DIAGNOSTIC CRITERIA: weight 5 pounds or more above the maximum allowable weight for the US Air Force. Maximum allowable weight corresponds to BMI = 25 in women and BMI = 27.5 in men for most heights. CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: military medical research centre TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: US Department of Defense PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "It was hypothesized that those in the Internet‐based program would, as a group, demonstrate the prevention of weight gain or small‐to‐moderate weight losses. It was further hypothesized that participants in the usual‐care condition would not show any weight loss and would, in fact, gain weight over the 6‐month period from baseline to reassessment." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was conducted using a random‐numbers table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | States study could not be blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 206 of the 224 participants randomized to usual care completed the study 193 of the 227 participants randomized to the behavioral Internet‐based program completed the study In both cases reasons given were: leaving the local area, medical reasons and the wish to withdraw Intention‐to‐treat analysis used using the baseline observation carried forward approach |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Morgan 2009.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Adult men who are overweight or obese and have access to a computer with e‐mail and Internet facilities. EXCLUSION CRITERIA: history of major medical problems such as heart disease in the past 5 years, diabetes, orthopedic or joint problems that would be a barrier to physical activity; recent weight loss of 4.5 kg or more; or taking medications that might affect body weight DIAGNOSTIC CRITERIA: BMI between 25 and 37 kg/m2 CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: Australia SETTING: community/university TREATMENT BEFORE STUDY: none |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): change in body weight (kg) (Australian New Zealand Clinical Trials Registry No: ANZCTRN12607000481471) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: University of Newcastle strategic pilot grant PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The primary aim of our assessor‐blinded randomized controlled trial was to evaluate the feasibility and efficacy of an Internet‐based weight‐loss program for overweight men." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was generated by computer‐based random number‐producing algorithm |
| Allocation concealment (selection bias) | Low risk | Reported that allocation sequence was concealed |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blind to group allocation at baseline assessment Assessors blinded to treatment allocation at all time points |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 28 out of the 34 participants assigned to Internet group completed the study 26 out of the 31 participants assigned to Information and Self Help group completed the study Reasons for loss to follow‐up were: personal reasons, no contact, unavailable, death and moved interstate Intention‐to‐treat analysis included all randomized participants. Authors used linear mixed models to assess analysis of effects of losses to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Morgan 2011.
| Methods | PARALLEL CLUSTER‐RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Adult men aged 18 to 65 years with a BMI between 25 and 40 kg/m2. Completion of a pre‐exercise risk assessment screening questionnaire was required. EXCLUSION CRITERIA: history of major medical problems such as heart disease in the last 5 years, diabetes, orthopedic or joint problems that would be a barrier to physical activity, recent weight loss of >=4.5 kg, or taking medications that might affect body weight DIAGNOSTIC CRITERIA: BMI between 25 and 40 kg/m2 CO‐MORBIDITIES: none specified CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: Australia SETTING: workplace (Tomago Aluminium) TREATMENT BEFORE STUDY: none |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): change in body weight (kg) (Australian New Zealand Clinical Trials Registry No: ANZCTRN12609001003268) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL FUNDING: Tomago Aluminium and Hunter Medical Research Institute PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The primary aim of this study was to evaluate the feasibility and efficacy of a workplace‐based weight loss program that targeted overweight and obese male shift workers. We hypothesized that weight and health‐related outcomes and behaviors of men would improve in the intervention group when compared to a wait‐list control group." | |
| Notes | We e‐mailed the author for information about the confidence interval for weight loss in the control group of the trial, and received a reply with the requested information (95% CI ‐1.017 to 1.7) on 25 August 2011 This trial is cluster‐randomized. We contacted the author to confirm that data presented in the publication were adjusted for clustering. On 4 September 2011 we received an e‐mail stating that "[T]he means in Table 5 are adjusted for clustering." We therefore used the statistics and sample sizes in Table 5 for our analyses without further adjustment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were cluster‐randomized based on timing and rotation of work shifts. Random allocation sequence generated by a computer‐based random number‐producing algorithm. |
| Allocation concealment (selection bias) | Low risk | Randomization and participant study arm assignment completed by a researcher not involved in participant assessment, and allocation sequence concealed when enrolling participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | States that participants and assessors were blind to group allocation at baseline assessment, but it is not stated that assessors were still blind at 14‐week follow‐up |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 54 out of 65 participants randomized to the intervention group completed the study at 14 weeks 36 out of 45 participants randomized to the control group completed the study at 14 weeks Intention‐to‐treat analysis used |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Unclear risk | Risks of bias specific to cluster‐randomized trials were assessed as follows: Recruitment bias: report did not provide details of the cluster‐randomization procedure, therefore prior knowledge of cluster assignment cannot be absolutely ruled out Baseline differences: no statistically significant differences between randomized groups Missing clusters: not present Incorrect statistical analysis: not present; the analysis took clustering into account Comparability with individually randomized trials: similar effects were seen in this trial and in the trials using individual randomization, with the exception of a larger effect size for decrease in waist measurement. Since all other effects of the intervention were comparable to the individually randomized trials, it is not likely that the difference in waist measurement is due to cluster‐randomization. |
Schroder 2010.
| Methods | PARALLEL QUASI‐RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Age 25 to 65 years, a BMI of 27 kg/m2 or more, fluency in English and daily access to a computer with a Windows operating system, Internet access and a valid e‐mail account EXCLUSION CRITERIA: diagnosis of diabetes, hypercholesterolemia or a mental disorder, enrolment in an alternative weight loss program, or having a friend or relative already enrolled in the study DIAGNOSTIC CRITERIA: BMI 27.0 kg/m2 or greater CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: none |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: outpatient/community TREATMENT BEFORE STUDY: None |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: grant from Utah State University PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The following hypotheses were tested: (1) A brief CAD intervention will support initial weight loss relative to a no‐treatment wait list control condition. (2) Compared to a CAD‐only condition, CAD augmented with a self‐management group (CAD+G) intervention will further enhance its effectiveness and improve the maintenance of weight loss over a longer period of time." | |
| Notes | We calculated the change from baseline following procedures in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009). We calculated the correlation coefficient from a weight loss study in this review (Hunter 2008) reporting standard deviations for baseline, endpoint and change values of weight, and used the calculated correlation coefficient to impute the missing standard deviation for the change from baseline. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | First author randomly assigned participants, separately by gender, in the order of their entry into the study, with every third participant being assigned to CAD, CAD+G and control groups |
| Allocation concealment (selection bias) | High risk | No randomization sequence generated to conceal |
| Blinding (performance bias and detection bias) All outcomes | High risk | First author was aware of assignations, participants were informed about their group assignment, but research team members were blind to the type of intervention assignments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 24 out of 30 assigned to the CAD group completed the 3‐month follow‐up 26 out of 31 assigned to the CAD+G group completed 3‐month follow‐up 26 out of 30 assigned to the wait list control group completed 3 month‐follow‐up No details given for patient dropout Intention‐to‐treat analysis used. Missing data points replaced with pre‐intervention scores. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Svetkey 2008.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight maintenance intervention trial for adults who had completed a 6‐month weight loss program. Inclusion criteria for the weight loss program were: taking medication for hypertension, dyslipidemia, or both; having access to a telephone and the Internet; and keeping a food diary for 5 days during the screening period. EXCLUSION CRITERIA: exclusion criteria for the weight loss program were: active cardiovascular disease or a recent cardiovascular event; medication‐treated diabetes mellitus, or any other medical or psychiatric condition that would preclude full participation in the study; weight loss of more than 9 kg in the previous 3 months; recent use of weight loss medications; and prior weight loss surgery DIAGNOSTIC CRITERIA: at the beginning of the weight loss intervention, participants had to have a BMI between 25 and 45. In order to be randomized to the weight maintenance trial, participants had to have lost at least 4 kg during the weight loss program. CO‐MORBIDITIES: all participants were taking medication for hypertension or dyslipidemia CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 4 COUNTRY/LOCATION: USA SETTING: academic medical centres TREATMENT BEFORE STUDY: all participants had participated in a 6‐month behavioral weight control program before randomization to weight maintenance conditions |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): "The primary outcome will be weight change from the end of the initial weight loss program to the end of the 30‐month weight maintenance intervention period." (ClinicalTrials.gov Identifier NCT00054925) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: National Heart, Lung, Blood Institute of the NIH PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "To compare two weight loss maintenance interventions [monthly personal contact or unlimited access to an interactive technology‐based intervention] with a self‐directed control group." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization assignments were stratified by clinic, race and amount of weight loss during phase 1 and were allocated in blocks. Allocation was generated using a password‐restricted, web‐based application. |
| Allocation concealment (selection bias) | Low risk | The allocation assignments were accessible only to authorized unblinded personnel |
| Blinding (performance bias and detection bias) All outcomes | Low risk | States that measurements were taken by staff members masked to treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 320 out of 342 randomized to the self directed weight loss maintenance arm completed the study at 30‐month follow‐up 323 out of 348 randomized to the interactive technology arm completed the study at 30‐month follow‐up 321 out of 342 randomized to the personal‐contact arm completed the study at 30‐month follow‐up Reasons given for loss to follow‐up were missed visits or death in all cases Multiple imputation used to replace missing end‐of‐study weights, missing interim weights and other measures (apart from weights missing due to participant death). All randomized surviving participants included in primary outcome analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Tate 2001.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial for adults. Inclusion criteria were: age 18 to 60 years and BMI of 25 to 36. EXCLUSION CRITERIA: history of myocardial infarction, stroke or cancer in the last 5 years; diabetes, angina, or orthopedic or joint problems that would prohibit exercise; major psychiatric disease; or current, planned or previous pregnancy within 6 months. If prospective participants endorsed any item on the Physical Activity Readiness Questionnaire, physician consent was required before the individual could be included. DIAGNOSTIC CRITERIA: participants had to have a BMI between 25 and 36 CO‐MORBIDITIES: not stated CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: academic medical centre TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL FUNDING: Weight Risk Investigators Study Council, a research division of Knoll Pharmaceutical PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "We hypothesized that better weight loss might be produced by using the Internet to deliver a structured behavioral weight loss program.... To test this hypothesis we conducted a randomized controlled trial to test the feasibility and initial efficacy of a structured Internet behavioral weight loss program compared with an educational Web site that was representative of weight loss resources widely available on the Internet." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 32 out of 45 participants randomized to the Internet Education group completed baseline, 3 and 6‐month follow‐up 35 out of 45 participants randomized to the Internet Education group completed baseline and 6‐month follow‐up 33 out of 46 participants randomized to the Internet Behavior Therapy group completed baseline,3 and 6‐month follow‐up 36 out of 46 participants randomized to the Internet Behavior Therapy group completed baseline and 6‐month follow‐up An intention‐to‐treat analysis was performed |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Tate 2003.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial for adults at risk for type 2 diabetes. Inclusion criteria were: BMI of 27 to 40 and one or more other risk factor for type 2 diabetes. EXCLUSION CRITERIA: major health or psychiatric disease, pregnancy or recent weight loss of 4.5 kg or more. If prospective participants endorsed any item on the Physical Activity Readiness Questionnaire or were taking medication that might be affected by weight loss, physician consent was required before the individual could be included. DIAGNOSTIC CRITERIA: participants had to have a BMI between 27 and 40 CO‐MORBIDITIES: all participants had at least one risk factor for type 2 diabetes (age > 45, family history of diabetes, high cholesterol or blood pressure, impaired glucose tolerance, history of gestational diabetes, being delivered of a neonate weighing 4 kg or more, or belonging to a minority group) in addition to overweight. 69% of participants had 3 or more risk factors. CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: academic medical centre TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: Clinical Research Award, American Diabetes Association PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "[T]he efficacy of Internet‐based weight loss programs and specifically e‐mail counseling has not been used in a population at risk of diabetes nor evaluated for a year‐long weight loss intervention." | |
| Notes | We e‐mailed the author in August 2010 and October 2010 to enquire whether it would be possible to obtain outcome data for 3 and 6 months of follow‐up. We received a reply but no additional data, therefore we used only the 12 months data that were included in the publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized using a computerized random numbers sequence |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 39 out of 46 randomized to the Basic Internet group completed the study 38 out of 46 randomized to the Basic Internet Plus Counselling group completed the study Reasons for loss of follow‐up were medical reasons, unknown or lack of interest Intention‐to‐treat analysis used including all randomized participants and assuming no change from baseline for those with missing data |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Tate 2006.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL. | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Inclusion criteria were: age 20 to 65 years, BMI of 27 to 40, willingness to use meal replacements as part of the dietary regimen, and availability of a computer with Internet access EXCLUSION CRITERIA: history of heart attack, stroke or cancer in the past 5 years; diabetes, angina or orthopedic or joint problems that would prohibit exercise; a major psychiatric disorder involving hospitalization during the past year; current or planned pregnancy or less than 6 months postpartum DIAGNOSTIC CRITERIA: participants had to have a BMI between 27 and 40 CO‐MORBIDITIES: not mentioned CONCOMITANT TREATMENTS: all participants were recommended to consume 2 liquid meal replacements per day (Slim‐Fast) |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: Academic medical centre TREATMENT BEFORE STUDY: none |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): weight loss at 6 months (ClinicalTrials.gov Identifier NCT00200304) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL FUNDING: Slim‐Fast Nutrition Institute PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The goal of this study was to determine the short‐term efficacy of a self‐directed Internet weight loss program compared with the same program supplemented with behavioral counseling from either a computer‐automated tailored system or from a human counselor." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized random numbers were used to assign participants to 1 of 3 groups |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Non‐intervention staff weighed participants at baseline and at 3 and 6 months, but no statement of whether or not they were blinded. Participants were aware of randomization assignment, but knowledge of other interventions is unclear. Stated that human e‐counselors blinded to algorithms used to program automated feedback counselor, but unclear whether they were aware of assignment of participants across all 3 groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 55 out of 67 randomized to the Website + No Counselling group completed the study at 3 months and 59 completed at 6 months 47 out of 61 randomized to the Website + Automated Feedback group completed the study at 3 months and 44 completed at 6 months 56 out of 64 randomized to the Website + Human Counselling group completed the study at 3 months and 52 completed at 6 months All participants were included in the intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Threlfall 1984.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial for adults. Inclusion criteria were body weight at least 10% over the desirable midpoint on the Metropolitan Life Insurance Company tables but less than 70% overweight by this same criterion EXCLUSION CRITERIA: planning pregnancy during the course of the intervention DIAGNOSTIC CRITERIA: participants had to have a body weight at least 10% over the desirable midpoint on the Metropolitan Life Insurance Company tables but less than 70% overweight by this same criterion CO‐MORBIDITIES: no CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: University course TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL/NON‐COMMERCIAL FUNDING: funding source, if any, not stated PUBLICATION STATUS: dissertation |
|
| Stated aim of study | Quote: "The current study was designed to test the following hypotheses: During 10 weeks of treatment, participants randomly assigned to a computer‐administered treatment supplement to the Jeffrey and Katz (1977) weight control manual will show a greater mean loss of pounds than will participants assigned to use the manual only." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | At baseline participants were measured by a student nurse, but there is no report of whether the nurse was blinded to the treatment assignment The investigator had no contact with either group but offered counseling during the trial to the intervention group. The investigator carried out the analyses. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reasons for attrition were not explored, with exception of one participant who became pregnant. It is unclear whether the reasons for attrition could be related to outcome. |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in the research hypotheses were reported |
| Other bias | Low risk | |
Webber 2008.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Adult women ages 25 to 40 with a BMI of 25 to 40 and home access to a computer with Internet service. EXCLUSION CRITERIA: diagnosis with a major psychiatric disorder or hospitalization for a psychiatric disorder within the last year, cancer diagnosis within 5 years with the exception of skin cancer, medical diagnosis of HIV, being pregnant, nursing or being less than 9 months post‐partum, planning to become pregnant within the study period, history of anorexia or bulimia nervosa, or recent weight loss of 10 pounds or more. A medical diagnosis of orthopedic or joint problems that might prohibit regular exercise. Endorsement of any of the first 3 items on the Physical Activity Readiness Questionnaire (PAR‐Q), or endorsement of any of the other items on the PAR‐AQ without a physician's consent to participate in the trial. Participants were also excluded if they admitted to knowing another potential study participant. DIAGNOSTIC CRITERIA: participants had to have a BMI between 25 and 40 CO‐MORBIDITIES: none specified CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: academic medical centre TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL/NON‐COMMERCIAL FUNDING: no funding statement PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The goal of the current study was to investigate the efficacy of the addition of weekly motivationally enhanced chats to a standard behavioral Internet weight loss program. We hypothesized that an intervention which incorporated a motivationally enhanced face‐to‐face session, an Internet behavioral weight loss program, and weekly online chats led using motivational techniques would produce greater weight loss than a similar intervention which did not include weekly online chats." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Trained research assistants who were blinded to group assignment took participant measurements |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 33 participants randomized to the Enhanced Intervention group completed the final weight measurement and questionnaires 32 of the 33 participants randomized to the Minimal Intervention completed the final measurement and questionnaires |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Wing 2006.
| Methods | PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL | |
| Participants |
INCLUSION CRITERIA: weight maintenance intervention trial. Adults who had lost at least 10% of their body weight during the previous 2 years. All participants had to have a friend, physician or weight loss counselor complete and sign a form verifying the amount and timing of their weight loss. EXCLUSION CRITERIA: serious physical or psychological disorders, pregnancy or a planned move. Persons with medical conditions that might affect their ability to safely complete the intervention or their ability to exercise were required to obtain written permission to participate from a physician. DIAGNOSTIC CRITERIA: participants had to have lost at least 10% of their body weight during the previous 2 years CO‐MORBIDITIES: none specified CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: academic medical centre/community TREATMENT BEFORE STUDY: none |
|
| Outcomes |
OUTCOME(S) (as stated in the protocol/registered trial documents): "The primary outcome measure is weight regain from baseline to 18 months." (ClinicalTrials.gov Identifier NCT00067145) |
|
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English COMMERCIAL FUNDING: no NON‐COMMERCIAL FUNDING: National Institute of Diabetes and Digestive and Kidney Diseases PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "We hypothesized that the interventions, delivered face to face or over the Internet, would decrease average weight regain and reduce the proportion of participants who regained 2.3 kg or more during a period of 18 months." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 98 out of the 105 participants randomized to the Control group completed 18‐month follow‐up 101 out of the 104 participants randomized to the Internet group completed 18‐month follow‐up 92 out of the 105 participants randomized to the Face‐to‐face group completed 18‐month follow‐up Reasons for loss to follow‐up were death, declined and had cancer Authors assumed all dropouts regained 2.3 kg or more |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Wylie‐Rosett 2001.
| Methods |
PARALLEL RANDOMIZED CONTROLLED CLINICAL TRIAL RANDOMIZATION RATIO: 1:2:2 |
|
| Participants |
INCLUSION CRITERIA: weight loss intervention trial. Adults who had a BMI greater than 25, or a BMI of at least 24 plus at least one cardiovascular risk factor. Participants had to be willing to follow the study protocol and pay a refundable USD 100 deposit. EXCLUSION CRITERIA: intention to move beyond commuting distance within the next 12 months, medical conditions that would interfere with study participation, and unwillingness to follow the study protocol DIAGNOSTIC CRITERIA: participants had to have a BMI greater than 25, or a BMI of at least 24 plus at least one cardiovascular risk factor CO‐MORBIDITIES: none specified CONCOMITANT TREATMENTS: no |
|
| Interventions |
NUMBER OF STUDY CENTRES: 1 COUNTRY/LOCATION: USA SETTING: Health Maintenance Organisation (HMO) TREATMENT BEFORE STUDY: none |
|
| Outcomes | OUTCOME(S) (as stated in the protocol/registered trial documents): no protocol/registered trial documents | |
| Study details |
RUN‐IN PERIOD: no STUDY TERMINATED BEFORE REGULAR END: no |
|
| Publication details |
LANGUAGE OF PUBLICATION: English NON‐COMMERCIAL FUNDING: National Heart, Lung and Blood Institute and the Diabetes Research and Training Center PUBLICATION STATUS: peer‐reviewed journal |
|
| Stated aim of study | Quote: "The goals of our study were to evaluate weight‐loss outcomes and the effect on CVD risk factors, and the resources required (from the perspective of a managed care organization) of the self‐help, non clinical, and clinical approaches to weight control." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized, but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 97 out of the 116 participants randomized to the Workbook only intervention group completed the study 183 out of the 236 participants randomized to the Workbook + computer intervention group completed the study 194 out of the 236 participants randomized to the Workbook + computer + staff intervention group completed the study Reasons for loss to follow‐up were not stated. It was reported that the study completers did not differ significantly from the dropouts with respect to baseline characteristics, but method of handling missing data not stated. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported as results |
| Other bias | Low risk | |
Abbreviations: BMI: body mass index; CAD: computer‐assisted dieting; CAD + G: computer‐assisted dieting plus group intervention; CI: confidence interval; NCI National Cancer Institute:
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adachi 2007 | Computer messages were generated from participant data but participants did not interact with computer program |
| Agras 1990 | Intervention ‐ handheld device |
| Anderson‐Bill 2011 | Patients ‐ not all obese |
| Bischoff 2010 | Intervention ‐ physical activity intervention rather than specifically aimed at weight loss |
| Booth 2008 | Patients ‐ dropout rate |
| Brantley 2008 | Patients ‐ dropout rate |
| Burke 2011 | Intervention ‐ handheld device |
| Burnett 1984 | Study design ‐ not RCT or quasi‐RCT |
| Burnett 1992 | Patients ‐ dropout rate |
| Campbell 2002 | Intervention ‐ not interactive; computer messages were generated from survey data but participants did not interact with computer program |
| Cange 2008 | Study design ‐ not RCT or quasi‐RCT |
| Carr 2008 | Patients ‐ dropout rate |
| Carr 2009 | Patients ‐ not all obese Intervention ‐ physical activity intervention rather than specifically aimed at weight loss |
| Carrard 2011 | Patients ‐ aimed specifically at people with eating disorders |
| Castelnuovo 2011 | Patients ‐ dropout rate |
| Christian 2011 | Intervention ‐ not interactive |
| Collinson 2011 | Study design ‐ not RCT or quasi‐RCT |
| Cook 2007 | Patients ‐ not obese Intervention ‐ not interactive; intervention was a multi‐media program but participants did not interact with it |
| Cousineau 2008 | Study design ‐ not RCT or quasi‐RCT |
| De Bourdeaudhuij 2007 | Patients ‐ not all obese |
| Dekkers 2011 | Patients ‐ dropout rate |
| Faghri 2008 | Study design ‐ not RCT or quasi‐RCT |
| Fitzgibbon 1995 | Intervention ‐ not computer‐based |
| Foree‐Gavert 1980 | Intervention ‐ not interactive; computer‐generated feedback was given, but participants did not interact with computer program |
| Gold 2007 | Patients ‐ dropout rate |
| Gow 2010 | Patients ‐ not all obese |
| Harvey‐Berino 1998 | Intervention ‐ not computer or web‐based |
| Harvey‐Berino 2002a | Unable to extract data or contact author |
| Harvey‐Berino 2004 | Follow‐up in weight maintenance trial was 84% at 6 months and 76% at 12 months. Six months data were not presented in the study report and we were unable to contact the author for information. Twelve months data were excluded due to follow‐up less than 80%. |
| Haugen 2007 | Study design ‐ not RCT or quasi‐RCT |
| Heetderks‐Cox 2001 | Patients ‐ dropout rate |
| Herrick 2009 | Patients ‐ not all obese |
| Jacobs 2010 | Intervention ‐ not interactive |
| James 2001 | Study design ‐ not RCT or quasi‐RCT |
| Jones 1997 | Patients ‐ dropout rate |
| Joo 2010 | Study design ‐ not RCT or quasi‐RCT |
| Kalten 2000 | Patients ‐ diabetic |
| Kerr 2008 | Patients ‐ dropout rate |
| Kremers 2005 | Intervention ‐ not interactive |
| Kristal 2000 | Intervention ‐ not interactive |
| Kroeze 2008 | Patients ‐ not obese |
| Kroeze 2008a | Patients ‐ not obese |
| Liou 2006 | Study design ‐ not RCT or quasi‐RCT |
| Lohof 2007 | Intervention ‐ not interactive; participants recorded activities on a website but no feedback was given. Primary outcome was increase in participants' self efficacy and physical activity levels. |
| Magnusdottir 2010 | Insufficient information to determine eligibility; author could not be contacted for further information |
| Marcus 2007 | Patients ‐ not obese Outcomes ‐ primary outcome was change in physical activity and secondary outcome was exercise performance |
| McConnon 2007 | Patients ‐ dropout rate |
| McDoniel 2010 | Patients ‐ dropout rate |
| McHugh 2008 | Study design ‐ not RCT or quasi‐RCT |
| McTigue 2009 | Study design ‐ not RCT or quasi‐RCT |
| Micco 2007 | Patients ‐ dropout rate |
| Mobley 2006 | Patients ‐ dropout rate |
| Nieto 2010 | Study design ‐ not RCT or quasi‐RCT |
| Park 2009 | Study design ‐ not RCT or quasi‐RCT |
| Patrick 2011 | Patients ‐ dropout rate |
| Petersen 2008 | Study design ‐ not RCT or quasi‐RCT |
| Polzien 2007 | Intervention ‐ not interactive |
| Pullen 2008 | Patients ‐ dropout rate |
| Riva 2000 | Study design ‐ not RCT or quasi‐RCT |
| Rothert 2006 | Patients ‐ dropout rate |
| Ryan 2010 | Patients ‐ dropout rate |
| Sartor 1991 | Patients ‐ dropout rate |
| Sbrocco 1999 | Intervention ‐ not interactive |
| Sbrocco 2005 | Intervention ‐ handheld device |
| Shay 2009 | Patients ‐ dropout rate |
| Smeets 2007 | Patients ‐ not obese |
| Smith 2009 | Outcome ‐ primary outcome was change in physical activity levels |
| Southard 2003 | Patients ‐ not all obese or overweight |
| Steele 2007 | Intervention ‐ physical activity intervention rather than specifically aimed at weight loss |
| Tanaka 2010 | Intervention ‐ computer messages were generated from participant data but participants did not interact with computer program |
| Taylor 1991 | Intervention ‐ handheld device |
| Thurston 1991 | Study design ‐ not RCT or quasi‐RCT |
| Touger‐Decker 2010 | Study design ‐ not RCT or quasi‐RCT |
| Turnin 2001 | Patients ‐ dropout rate |
| van der Mark 2009 | Study design ‐ not RCT or quasi‐RCT |
| van Wier 2009 | Patients ‐ dropout rate |
| Vandelanotte 2005 | Patients ‐ not obese |
| Vandelanotte 2008 | Patients ‐ not obese Intervention ‐ not interactive |
| Verheijden 2007 | Study design ‐ not RCT or quasi‐RCT |
| Webber 2008a | Patients ‐ dropout rate |
| Webber 2010 | Intervention: motivational interviewing and not specifically computer‐based weight loss |
| Weinstock 1998 | Intervention ‐ not computer‐based |
| Werkman 2010 | Patient ‐ not all obese |
| Winett 2007 | Patients ‐ not all obese |
| Wing 2009 | Patients ‐ dropout rate |
| Womble 2004 | Patients ‐ dropout rate |
| Yon 2007 | Intervention ‐ handheld device |
Abbreviations: RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
Harvey‐Berino NCT01232699.
| Trial name or title | Internet obesity treatment enhanced with motivational interviewing |
| Methods |
Trial design: randomized controlled trial Duration of intervention: 6‐month weight loss program followed by 12 months of weight maintenance Country: United States of America |
| Participants | Inclusion criteria: 18 years and older; male and female; BMI between 18 and 50; must be able to walk for exercise |
| Interventions |
Internet Obesity Treatment: active comparator Internet Obesity Treatment with Motivational Interviewing: experimental |
| Outcomes |
Primary outcome: change in body weight at 6 months Secondary outcomes: adherence to treatment components at 6, 12 and 18 months Motivation measures at 6, 12 and 18 months |
| Starting date | December 2010 |
| Contact information | Doris E Ogden, M.S. +1‐802‐656‐1960 doris.ogden@uvm.edu |
| Notes |
ClinicalTrials.gov Identifier: NCT01232699 Other Study ID Numbers:10‐124 |
Abbreviations: BMI: body mass index
Differences between protocol and review
TITLE: changed from "Computer‐based interventions for weight loss or weight maintenance in overweight or obese people" to "Interactive computer‐based interventions for weight loss or weight maintenance in overweight or obese people".
OBJECTIVES: changed to "To assess the effects of interactive computer‐based interventions for weight loss or weight maintenance in overweight or obese people".
TYPES OF STUDIES: quasi‐randomized controlled trials (quasi‐RCTs) added.
ELECTRONIC SEARCHES: CRISP deleted from list of databases searched.
SELECTION OF STUDIES: LSW added for selection of studies.
DATA EXTRACTION AND MANAGEMENT: LF replaced by LSW for data extraction.
RISK OF BIAS IN INCLUDED STUDIES: CS added for risk of bias assessment.
Contributions of authors
L. Susan Wieland: trial selection, data extraction, data analysis, data interpretation, draft manuscript, review final draft.
Louise Falzon: protocol draft, search strategy development, trial selection, data extraction, 'Risk of bias' assessment, draft manuscript, review final draft.
Chris N. Sciamanna: protocol draft, 'Risk of bias' assessment, draft manuscript, review final draft.
Kimberlee J. Trudeau: protocol draft, study selection, 'Risk of bias' assessment, review final draft.
Suzanne Brodney: protocol draft, data extraction, review final draft.
Joseph E Schwartz: data analysis, review final draft.
Karina W Davidson: protocol draft, review final draft.
Declarations of interest
L. Susan Wieland: none known.
Louise Falzon: none known.
Chris N. Sciamanna is developing and testing a web‐based weight loss program. It is a university‐based, grant‐funded project.
Kimberlee J. Trudeau: none known.
Suzanne Brodney: none known.
Joseph E. Schwartz: none known.
Karina W. Davidson: none known.
New
References
References to studies included in this review
Bennett 2010 {published data only}
- Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web‐based weight loss in primary care: a randomized controlled trial. Obesity (Silver Spring, Md.) 2010;18(2):308‐13. [PUBMED: 19696764] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cussler 2008 {published data only}
- Cussler EC, Teixeira PJ, Going SB, Houtkooper LB, Metcalfe LL, Blew RM, et al. Maintenance of weight loss in overweight middle‐aged women through the Internet. Obesity (Silver Spring, Md.) 2008;16(5):1052‐60. [PUBMED: 18309301] [DOI] [PubMed] [Google Scholar]
DeLucia 1988 {published and unpublished data}
- DeLucia JL, Kalodner CR, Horan JJ. The effect of two nutritional software programs used as adjuncts to the behavioral treatment of obesity. Journal of Substance Abuse 1988;1(2):203‐8. [PUBMED: 2980870] [DOI] [PubMed] [Google Scholar]
Gabriele 2011 {published data only}
- Gabriele JM, Carpenter BD, Tate DF, Fisher EB. Directive and nondirective e‐coach support for weight loss in overweight adults. Annals of Behavioral Medicine 2011;41(2):252‐63. [PUBMED: 21108032] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harvey‐Berino 2002 {published data only}
- Harvey‐Berino J, Pintauro S, Buzzell P, DiGiulio M, Gold BC, Moldovan C, et al. Does using the Internet facilitate the maintenance of weight loss?. International Journal of Obesity and Related Metabolic Disorders 2002;26(9):1254‐60. [DOI] [PubMed] [Google Scholar]
Harvey‐Berino 2010 {published data only}
- Harvey‐Berino J, West D, Krukowski R, Prewitt E, VanBiervliet A, Ashikaga T, et al. Internet delivered behavioral obesity treatment. Preventive Medicine 2010;51(2):123‐8. [PUBMED: 20478333] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krukowski RA, Tilford JM, Harvey‐Berino J, West DS. Comparative cost‐effectiveness for in‐person versus online behavioral weight loss programs. Obesity Reviews 2010;11 Suppl 1:249. [PUBMED: 17316318] 17316318 [Google Scholar]
- Krukowski RA, Tilford JM, Harvey‐Berino J, West DS. Comparing behavioral weight loss modalities: incremental cost‐effectiveness of an internet‐based versus an in‐person condition. Obesity (Silver Spring, Md.) 2011;19(8):1629‐35. [PUBMED: 21253001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunter 2008 {published data only}
- Hunter CM, Peterson AL, Alvarez LM, Poston WC, Brundige AR, Haddock CK, et al. Weight management using the internet a randomized controlled trial. American Journal of Preventive Medicine 2008;34(2):119‐26. [PUBMED: 18201641] [DOI] [PubMed] [Google Scholar]
- Rasu RS, Hunter CM, Peterson AL, Maruska HM, Foreyt JP. Economic evaluation of an Internet‐based weight management program. American Journal of Managed Care 2010;16(4):e98‐104. [PUBMED: 20370312] [PubMed] [Google Scholar]
- Rasu RS, Hunter CM, Peterson AL, Maruska HM, Foreyt JP. Economic evaluation of an Internet‐based weight management program. American Journal of Managed Care 2010;16(4):e98‐e104. [PubMed] [Google Scholar]
Morgan 2009 {published data only}
- Collins CE, Morgan PJ, Warren JM, Lubans DR, Callister R. Men participating in a weight‐loss intervention are able to implement key dietary messages, but not those relating to vegetables or alcohol: the Self‐Help, Exercise and Diet using Internet Technology (SHED‐IT) study. Public Health Nutrition 2011;14(1):168‐75. [PUBMED: 20602869] [DOI] [PubMed] [Google Scholar]
- Lubans DR, Morgan PJ, Collins CE, Warren JM, Callister R. Exploring the mechanisms of weight loss in the SHED‐IT intervention for overweight men: a mediation analysis. International Journal of Behavioral Nutrition and Physical Activity 2009;6:76. [PUBMED: 19922613] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. 12‐month outcomes and process evaluation of the SHED‐IT RCT: an internet‐based weight loss program targeting men. Obesity (Silver Spring, Md.) 2011;19(1):142‐51. [PUBMED: 20523304] [DOI] [PubMed] [Google Scholar]
- Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. The SHED‐IT randomized controlled trial: evaluation of an Internet‐based weight‐loss program for men. Obesity (Silver Spring, Md.) 2009;17(11):2025‐32. [PUBMED: 19343018] [DOI] [PubMed] [Google Scholar]
Morgan 2011 {published and unpublished data}
- Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. Efficacy of a workplace‐based weight loss program for overweight male shift workers: the Workplace POWER (Preventing Obesity Without Eating like a Rabbit) randomized controlled trial. Preventive Medicine 2011;52(5):317‐25. [PUBMED: 21300083] [DOI] [PubMed] [Google Scholar]
Schroder 2010 {published data only}
- Schroder KE. Computer‐assisted dieting: effects of a randomised controlled intervention. Psychology and Health 2010;25(5):519‐34. [PUBMED: 20204974] [DOI] [PubMed] [Google Scholar]
Svetkey 2008 {published data only}
- Brantley P, Appel L, Hollis J, Stevens V, Ard J, Champagne C, et al. Design considerations and rationale of a multi‐center trial to sustain weight loss: the Weight Loss Maintenance Trial. Clinical Trials (London, England) 2008;5(5):546‐56. [PUBMED: 18827047] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk KL, Stevens VJ, Appel LJ, Bauck A, Brantley PJ, Champagne CM, et al. Associations of internet website use with weight change in a long‐term weight loss maintenance program. Journal of Medical Internet Research 2010; Vol. 12, issue 3:e29. [DOI] [PMC free article] [PubMed]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the weight‐loss. American Journal of Preventive Medicine 2008;35(2):118‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meenan RT, Stevens VJ, Funk K, Bauck A, Jerome GJ, Lien LF, et al. Development and implementation cost analysis of telephone‐ and Internet‐based interventions for the maintenance of weight loss. International Journal of Technology Assessment in Health Care 2009;25(3):400‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meenan RT, Stevens VJ, Funk, K, Bauck A, Jerome GJ, Stevens VJ, et al. PS2‐34: Implementation cost analysis of telephone and internet‐based interventions for the maintenance of weight loss. Clinical Medicine and Research 2010;8(1):52‐b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens VJ, Funk KL, Brantley PJ, Erlinger TP, Myers VH, Champagne CM, et al. Design and implementation of an interactive website to support long‐term maintenance of weight loss. Journal of Medical Internet Research 2008;10(1):e1. [PUBMED: 18244892] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008;299(10):1139‐48. [PUBMED: 18334689] [DOI] [PubMed] [Google Scholar]
Tate 2001 {published data only}
- Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA 2001;285(9):1172‐7. [DOI] [PubMed] [Google Scholar]
Tate 2003 {published data only}
- Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003;289(14):1833‐6. [PUBMED: 12684363] [DOI] [PubMed] [Google Scholar]
Tate 2006 {published data only}
- Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e‐mail counseling, computer‐automated tailored counseling, and no counseling in an Internet weight loss program. Archives of Internal Medicine 2006;166(15):1620‐5. [DOI] [PubMed] [Google Scholar]
Threlfall 1984 {published data only}
- Threlfall WE. Computer‐assisted bibliotherapy for weight control. Dissertation Abstracts International 1984;45(6‐A):1697‐8. [Google Scholar]
Webber 2008 {published data only}
- Webber KH, Tate DF, Michael Bowling J. A randomized comparison of two motivationally enhanced Internet behavioral weight loss programs. Behaviour Research and Therapy 2008;46(9):1090‐5. [PUBMED: 18675402] [DOI] [PubMed] [Google Scholar]
- Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self‐monitoring and weight loss in a 16‐week Internet behavioral weight loss intervention. Journal of Nutrition Education and Behavior 2010;42(3):161‐7. [DOI] [PubMed] [Google Scholar]
Wing 2006 {published data only}
- Marinilli Pinto A, Gorin AA, Raynor HA, Tate DF, Fava JL, Wing RR. Successful weight‐loss maintenance in relation to method of weight loss. Obesity (Silver Spring, Md.) 2008;16(11):2456‐61. [PUBMED: 18719680] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self‐regulation program for maintenance of weight loss. New England Journal of Medicine 2006;355(15):1563‐71. [PUBMED: 17035649] [DOI] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: are there negative effects of daily weighing? [erratum appears in Journal of Consulting & Clinical Psychology 2007 Oct;75(5):715]. Journal of Consulting & Clinical Psychology 2007;75(4):652‐6. [DOI] [PubMed] [Google Scholar]
Wylie‐Rosett 2001 {published data only}
- Wylie‐Rosett J, Swencionis C, Ginsberg M, Cimino C, Wassertheil‐Smoller S, Caban A, et al. Computerized weight loss intervention optimizes staff time: the clinical and cost results of a controlled clinical trial conducted in a managed care setting. Journal of the American Dietetic Association 2001;101(10):1155‐62; quiz 1163‐4. [PUBMED: 11678486] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adachi 2007 {published data only}
- Adachi Y, Sato C, Yamatsu K, Ito S, Adachi K, Yamagami T. A randomized controlled trial on the long‐term effects of a 1‐month behavioral weight control program assisted by computer tailored advice. Behaviour Research and Therapy 2007;45(3):459‐70. [PUBMED: 16713991] [DOI] [PubMed] [Google Scholar]
Agras 1990 {published data only}
- Agras WS, Barr TC, Feldman DE, Losch M, Burnett KF. Developing computer‐assisted therapy for the treatment of obesity. Behavior Therapy 1990, issue 1:99‐109.
Anderson‐Bill 2011 {published data only}
- Anderson‐Bill ES, Winett RA, Wojcik JR, Winett SG. Web‐based guide to health: relationship of theoretical variables to change in physical activity, nutrition and weight at 16‐months. Journal of Medical Internet Research 2011;13(1):e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bischoff 2010 {published data only}
- Bischoff SA. The effects of goal setting on increasing physical activity behavior through a 16‐week internet‐delivered intervention. ProQuest Dissertation Dissertations. United States ‐‐ Wyoming: Kinesiology & Health, 2010; Vol. Kinesiology & Health.
Booth 2008 {published data only}
- Booth AO, Nowson CA, Matters H, Booth AO, Nowson CA, Matters H. Evaluation of an interactive, Internet‐based weight loss program: a pilot study. Health Education Research 2008;23(3):371‐81. [DOI] [PubMed] [Google Scholar]
Brantley 2008 {published data only}
- Brantley P, Appel L, Hollis J, Stevens V, Ard J, Champagne C, et al. Design considerations and rationale of a multi‐center trial to sustain weight loss: the Weight Loss Maintenance Trial. Clinical Trials 2008;5(5):546‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burke 2011 {published data only}
- Burke LE, Conroy MB, Sereika SM, Elci OU, Styn MA, Acharya SD, et al. The effect of electronic self‐monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity 2011;19(2):338‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burnett 1984 {published data only}
- Burnett KF. Ambulatory computer‐assisted therapy in the behavioral treatment of obesity [Dissertation]. Stanford University, 1984. [Google Scholar]
Burnett 1992 {published data only}
- Burnett KF, Taylor C, Agras W. Ambulatory computer‐assisted behavior therapy for obesity: an empirical model for examining behavioral correlates of treatment outcome. Computers in Human Behavior 1992;8(2‐3):239‐48. [Google Scholar]
Campbell 2002 {published data only}
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue‐collar workers: Health Works for Women. Preventive Medicine 2002;34(3):313‐23. [DOI] [PubMed] [Google Scholar]
Cange 2008 {published data only}
- Cange A, Bickmore T, Harris K, Neylon D, Kvedar J, Brown J, et al. Improving adherence to an exercise program: a personalized virtual coach. Telemedicine and e‐Health 2008;14(Suppl 1):39. [Google Scholar]
Carr 2008 {published data only}
- Carr LJ, Bartee RT, Dorozynski C, Broomfield JF, Smith ML, Smith DT, et al. Internet‐delivered behavior change program increases physical activity and improves cardiometabolic disease risk factors in sedentary adults: results of a randomized controlled trial. Preventive Medicine 2008;46(5):431‐8. [DOI] [PubMed] [Google Scholar]
Carr 2009 {published data only}
- Carr, LJ. Short and long‐term efficacy of an internet‐delivered physical activity behavior change program on physical activity and cardiometabolic disease risk factors in sedentary, overweight adults. Dissertation Abstracts International: Section B: The Sciences and Engineering 2009;69(12‐B):7454. [Google Scholar]
Carrard 2011 {published data only}
- Carrard I, Crepin C, Rouget P, Lam T, Linden M, Golay A. Acceptance and efficacy of a guided internet self‐help treatment program for obese patients with binge eating disorder. Clinical Practice and Epidemiology in Mental Health 2011;7:8‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castelnuovo 2011 {published data only}
- Castelnuovo G, Manzoni GM, Cuzziol P, Cesa GL, Corti S, Tuzzi C, et al. TECNOB Study: ad interim results of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type‐2 diabetes. Clinical Practice and Epidemiology in Mental Health 2011;7:44‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Christian 2011 {published data only}
- Christian JG, Byers TE, Christian KK, Goldstein MG, Bock BC, Prioreschi B, et al. A computer support program that helps clinicians provide patients with metabolic syndrome tailored counseling to promote weight loss. Journal of the American Dietetic Association 2011;111(1):75‐83. [DOI] [PubMed] [Google Scholar]
Collinson 2011 {published data only}
- Collinson A, Lindley R, Campbell A, Waters I, Lindley T, Wallace A. An evaluation of an internet‐based approach to weight loss with low glycaemic load principles. Journal of Human Nutrition and Dietetics 2011;24(2):192‐5. [DOI] [PubMed] [Google Scholar]
Cook 2007 {published data only}
- Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A, Cook Royer F, et al. A field test of a web‐based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. Journal of Medical Internet Research 2007;9(2):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cousineau 2008 {published data only}
- Cousineau T, Houle B, Bromberg J, Fernandez KC, Kling WC. A pilot study of an online workplace nutrition program: the value of participant input in program development. Journal of Nutrition Education and Behavior 2008;40(3):160‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Bourdeaudhuij 2007 {published data only}
- Bourdeaudhuij I, Stevens V, Vandelanotte C, Brug J. Evaluation of an interactive computer‐tailored nutrition intervention in a real‐life setting. Annals of Behavioral Medicine 2007;33(1):39‐48. [DOI] [PubMed] [Google Scholar]
Dekkers 2011 {published data only}
- Dekkers JC, Wier MF, Ariens GA, Hendriksen IJ, Pronk NP, Smid T, et al. Comparative effectiveness of lifestyle interventions on cardiovascular risk factors among a Dutch overweight working population: a randomized controlled trial. BMC Public Health 2011;11(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faghri 2008 {published data only}
- Faghri PD, Omokaro C, Parker C, Nichols E, Gustavesen S, Blozie E. E‐technology and pedometer walking program to increase physical activity at work. Journal of Primary Prevention 2008;29(1):73‐91. [DOI] [PubMed] [Google Scholar]
Fitzgibbon 1995 {published data only}
- Fitzgibbon ML, Stolley MR, Kirschenbaum DS. An obesity prevention pilot program for African‐American mothers and daughters. Journal of Nutrition Education 1995;27(2):93‐9. [Google Scholar]
Foree‐Gavert 1980 {published data only}
- Foree‐Gavert S, Gavert L. Obesity: behavior therapy with computer‐feedback versus traditional starvation treatment. Scandinavian Journal of Behaviour Therapy 1980;9(1):1‐14. [Google Scholar]
Gold 2007 {published data only}
- Gold BC, Burke S, Pintauro S, Buzzell P, Harvey‐Berino J, Gold BC, et al. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity 2007;15(1):155‐64. [DOI] [PubMed] [Google Scholar]
Gow 2010 {published data only}
- Gow RW, Trace SE, Mazzeo SE. Preventing weight gain in first year college students: an online intervention to prevent the "freshman fifteen". Eating Behaviors 2010;11(1):33‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harvey‐Berino 1998 {published data only}
- Harvey‐Berino J. Changing health behavior via telecommunications technology: using interactive television to treat obesity. Behavior Therapy 1998, issue 3:505‐19.
Harvey‐Berino 2002a {published data only}
- Harvey‐Berino J, Pintauro SJ, Gold EC. The feasibility of using Internet support for the maintenance of weight loss. Behavior Modification 2002;26(1):103‐16. [PUBMED: 11799651] [DOI] [PubMed] [Google Scholar]
Harvey‐Berino 2004 {published data only}
- Harvey‐Berino J, Pintauro S, Buzzell P, Gold EC. Effect of internet support on the long‐term maintenance of weight loss. Obesity Research 2004;12(2):320‐9. [PUBMED: 14981225] [DOI] [PubMed] [Google Scholar]
Haugen 2007 {published data only}
- Haugen HA, Tran ZV, Wyatt HR, Barry MJ, Hill JO. Using telehealth to increase participation in weight maintenance programs. Obesity (Silver Spring, Md.) 2007;15(12):3067‐77. [PUBMED: 18198316] [DOI] [PubMed] [Google Scholar]
Heetderks‐Cox 2001 {published data only}
- Heetderks‐Cox MJ, Alford BB, Bednar CM, Heiss CJ, Tauai LA, Edgren KK. CD‐ROM nutrient analysis database assists self‐monitoring behavior of active duty Air Force personnel receiving nutrition counseling for weight loss. Journal of the American Dietetic Association 2001, issue 9:1041‐6. [DOI] [PubMed]
Herrick 2009 {published data only}
- Herrick M. Characterization of time and order of internet lessons in Project WebHealth [Dissertation]. South Dakota: United States: South Dakota State University, 2009. [Google Scholar]
Jacobs 2010 {published data only}
- Jacobs N, Clays E, Bacquer D, Backer G, Dendale P, Thijs H, et al. Effect of a tailored behaviour change programme on a composite lifestyle change score: a randomised controlled trial. European Journal of Cardiovascular Prevention and Rehabilitation 2010;17:S106. [Google Scholar]
James 2001 {published data only}
- James LC, Folen RA, Earles J. Behavioral telehealth applications in the treatment of obese soldiers: a feasibility project and a report on preliminary findings. Military Psychology 2001;13(3):177‐86. [Google Scholar]
Jones 1997 {published data only}
- Jones KS. A comparison of instructional methods for weight loss and curriculum comprehension in women [Dissertation]. Arizona: United States: Arizona State University, 1997. [Google Scholar]
Joo 2010 {published data only}
- Joo NS, Park YW, Park KH, Kim CW, Kim BT. Cost‐effectiveness of a community‐based obesity control programme (Provisional abstract). Journal of Telemedicine and Telecare 2010;16(2):63‐7. [DOI] [PubMed] [Google Scholar]
Kalten 2000 {published data only}
Kerr 2008 {published data only}
- Kerr J, Patrick K, Norman G, Stein MB, Calfas K, Zabinski M, et al. Randomized control trial of a behavioral intervention for overweight women: impact on depressive symptoms. Depression and Anxiety 2008;25(7):555‐8. [DOI] [PubMed] [Google Scholar]
Kremers 2005 {published data only}
- Kremers SPJ, Visscher TLS, Brug J, Chin A, Paw MJM, Schouten EG, et al. Netherlands research programme weight gain prevention (NHF‐NRG): rationale, objectives and strategies. European Journal of Clinical Nutrition 2005;59(4):498‐507. [DOI] [PubMed] [Google Scholar]
Kristal 2000 {published data only}
Kroeze 2008 {published data only}
- Kroeze W, Oenema A, Campbell M, Brug J. The efficacy of web‐based and print‐delivered computer‐tailored interventions to reduce fat intake: results of a randomized, controlled trial. Journal of Nutrition Education and Behavior 2008;40(4):226‐36. [DOI] [PubMed] [Google Scholar]
Kroeze 2008a {published data only}
- Kroeze W, Oenema A, Dagnelie PC, Brug J. Examining the minimal required elements of a computer‐tailored intervention aimed at dietary fat reduction: results of a randomized controlled dismantling study. Health Education Research 2008;23(5):880‐91. [DOI] [PubMed] [Google Scholar]
Liou 2006 {published data only}
- Liou T‐H, Chen C‐H, Hsu C‐Y, Chou P, Chiu H‐W. A pilot study of videoconferencing for an Internet‐based weight loss programme for obese adults in Taiwan. Journal of Telemedicine and Telecare 2006;12(7):370‐3. [DOI] [PubMed] [Google Scholar]
Lohof 2007 {published data only}
- Lohof Christy H. Self‐efficacy and physical activity: the effect of a theory‐driven, Internet‐based intervention [Dissertation]. Wyoming: United States: University of Wyoming, 2007. [Google Scholar]
Magnusdottir 2010 {published data only}
- Magnusdottir OK, Ramel A, Thorsdottir I. One year weight reduction in young overweight adults: two months controlled modest energy restriction and/or 12 months program with internet based education and visits to the clinic. Obesity Reviews 2010;11:247‐8. [Google Scholar]
Marcus 2007 {published data only}
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht AE, et al. Examination of print and telephone channels for physical activity promotion: rationale, design, and baseline data from Project STRIDE. Contemporary Clinical Trials 2007;28(1):90‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
McConnon 2007 {published data only}
- McConnon A, Kirk SF, Cockroft JE, Harvey EL, Greenwood DC, Thomas JD, et al. The Internet for weight control in an obese sample: results of a randomised controlled trial. BMC Health Services Research 2007;7:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
McDoniel 2010 {published data only}
- McDoniel SO, Wolskee P, Shen J. Treating obesity with a novel hand‐held device, computer software program, and Internet technology in primary care: the SMART motivational trial. Patient Education and Counseling 2010;79(2):185‐91. [DOI] [PubMed] [Google Scholar]
McHugh 2008 {published data only}
- McHugh JE. The effectiveness of web‐based tailored messaging on employee health [Dissertation]. Florida: United States: Nova Southeastern University, 2008. [Google Scholar]
McTigue 2009 {published data only}
- McTigue KM, Conroy MB, Hess R, Bryce CL, Fiorillo AB, Fischer GS, et al. Using the Internet to translate an evidence‐based lifestyle intervention into practice. Telemedicine Journal and e‐health 2009;15(9):851‐8. [DOI] [PubMed] [Google Scholar]
Micco 2007 {published data only}
- Micco N, Gold B, Buzzell P, Leonard H, Pintauro S, Harvey‐Berino J, et al. Minimal in‐person support as an adjunct to internet obesity treatment. Annals of Behavioral Medicine 2007;33(1):49‐56. [DOI] [PubMed] [Google Scholar]
Mobley 2006 {published data only}
- Mobley AR. Evaluation of behavioral theory and integrated Internet/telephone technologies to support military obesity and weight management programs [Dissertation]. Maryland: United States: University of Maryland, College Park, 2006. [Google Scholar]
Nieto 2010 {published data only}
- Nieto L. A comparison of weight loss outcome across three distinct weight‐loss program delivery venues [Dissertation]. Vol. TUI University, California: United States: TUI University, 2010. [Google Scholar]
Park 2009 {published data only}
- Park M‐J, Kim H‐S, Kim K‐S. Cellular phone and Internet‐based individual intervention on blood pressure and obesity in obese patients with hypertension. International Journal of Medical Informatics 2009;78(10):704‐10. [DOI] [PubMed] [Google Scholar]
Patrick 2011 {published data only}
Petersen 2008 {published data only}
- Petersen R, Sill S, Lu C, Young J, Edington DW. Effectiveness of employee Internet‐based weight management program. Journal of Occupational and Environmental Medicine 2008;50(2):163‐71. [DOI] [PubMed] [Google Scholar]
Polzien 2007 {published data only}
- Polzien KM, Jakicic JM, Tate DF. The efficacy of a technology‐based system in a short‐term behavioral weight loss intervention. Obesity 2007;15(4):825–30. [DOI] [PubMed] [Google Scholar]
Pullen 2008 {published data only}
- Pullen CH, Hageman PA, Boeckner L, Walker SN, Oberdorfer MK. Feasibility of internet‐delivered weight loss interventions among rural women ages 50‐69. Journal of Geriatric Physical Therapy 2008;31(3):105‐12. [DOI] [PubMed] [Google Scholar]
Riva 2000 {published data only}
- Riva G, Bacchetta M, Baruffi M, Rinaldi S, Vincelli F, Molinari E. Virtual reality‐based experiential cognitive treatment of obesity and binge‐eating disorders. Clinical Psychology and Psychotherapy 2000;7(3):209‐19. [Google Scholar]
Rothert 2006 {published data only}
- Rothert K, Strecher VJ, Doyle LA, Caplan WM, Joyce JS, Jimison HB, et al. Web‐based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity 2006;14(2):266‐72. [DOI] [PubMed] [Google Scholar]
Ryan 2010 {published data only}
- Ryan DH, Johnson WD, Myers VH, Prather TL, McGlone MM, Rood J, et al. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Archives of Internal Medicine 2010;170(2):146‐54. [DOI] [PubMed] [Google Scholar]
Sartor 1991 {published data only}
- Sartor MR. The use of computer technology in teaching weight loss. Dissertation Abstracts International. University of Mississippi, US, 1991; Vol. 52, issue 2‐A:446.
Sbrocco 1999 {published data only}
- Sbrocco T, Nedegaard RC, Stone JM, Lewis EL. Behavioral choice treatment promotes continuing weight loss: preliminary results of a cognitive‐behavioral decision‐based treatment for obesity. Journal of Consulting and Clinical Psychology 1999;67(2):260‐6. [DOI] [PubMed] [Google Scholar]
Sbrocco 2005 {published data only}
- Sbrocco T, Carter MM, Lewis EL, Vaughn NA, Kalupa KL, King S, et al. Church‐based obesity treatment for African‐American women improves adherence. Ethnicity and Disease 2005;15(2):246‐55. [PMC free article] [PubMed] [Google Scholar]
Shay 2009 {published data only}
- Shay LE, Seibert D, Watts D, Sbrocco T, Pagliara C. Adherence and weight loss outcomes associated with food‐exercise diary preference in a military weight management program. Eating Behaviors 2009;10(4):220‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smeets 2007 {published data only}
- Smeets T, Kremers SP, Brug J, Vries H, Kremers SPJ. Effects of tailored feedback on multiple health behaviors. [erratum appears in Annals of Behavioral Medicine 2007 Jul‐Aug;34(1):104]. Annals of Behavioral Medicine 2007;33(2):117‐23. [DOI] [PubMed] [Google Scholar]
Smith 2009 {published data only}
- Smith DT, Carr LJ, Dorozynski C, Gomashe C, Smith DT, Carr LJ, et al. Internet‐delivered lifestyle physical activity intervention: limited inflammation and antioxidant capacity efficacy in overweight adults. Journal of Applied Physiology 2009;106(1):49‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Southard 2003 {published data only}
- Southard BH, Southard DR, Nuckolls J. Clinical trial of an Internet‐based case management system for secondary prevention of heart disease. Journal of Cardiopulmonary Rehabilitation 2003;23(5):341‐8. [DOI] [PubMed] [Google Scholar]
Steele 2007 {published data only}
- Steele RM, Mummery WK, Dwyer T. Examination of program exposure across intervention delivery modes: face‐to‐face versus internet. International Journal of Behavioral Nutrition and Physical Activity 2007;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanaka 2010 {published data only}
- Tanaka M, Adachi Y, Adachi K, Sato C. Effects of a non‐face‐to‐face behavioral weight‐control program among Japanese overweight males: a randomized controlled trial. International Journal of Behavioral Medicine 2010;17(1):17‐24. [PUBMED: 19685190] [DOI] [PubMed] [Google Scholar]
Taylor 1991 {published data only}
- Taylor CB, Agras WS, Losch M, Plante TG, Burnett K. Improving the effectiveness of computer‐assisted weight loss. Behavior Therapy 1991, issue 2:229‐36.
Thurston 1991 {published data only}
- Thurston WE. Development and formative evaluation of a decision‐management health promotion program on healthy weights for women [Dissertation]. Canada: University of Calgary (Canada), 1991. [Google Scholar]
Touger‐Decker 2010 {published data only}
- Touger‐Decker R, Denmark R, Bruno M, O'Sullivan‐Maillet J, Lasser N. Workplace weight loss program; comparing live and internet methods. Journal of Occupational and Environmental Medicine 2010;52(11):1112‐8. [DOI] [PubMed] [Google Scholar]
Turnin 2001 {published data only}
- Turnin MC, Bourgeois O, Cathelineau G, Leguerrier AM, Halimi S, Sandre‐Banon D, et al. Multicenter randomized evaluation of a nutritional education software in obese patients. Diabetes and Metabolism 2001;27(2 Pt 1):139‐47. [PubMed] [Google Scholar]
van der Mark 2009 {published data only}
- Mark M, Jonasson J, Svensson M, Linne Y, Rossner S, Lagerros YT. Older members perform better in an internet‐based behavioral weight loss program compared to younger members. Obesity Facts 2009;2(2):74‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Wier 2009 {published data only}
- Wier MF, Ariens GA, Dekkers JC, Hendriksen IJ, Smid T, Mechelen W. Phone and e‐mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health 2009;9(1):6. [DOI: 10.1186/1471-2458-9-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vandelanotte 2005 {published data only}
- Vandelanotte C, Bourdeaudhuij I, Sallis JF, Spittaels H, Brug J. Efficacy of sequential or simultaneous interactive computer‐tailored interventions for increasing physical activity and decreasing fat intake. Annals of Behavioral Medicine 2005;29(2):138‐46. [DOI] [PubMed] [Google Scholar]
Vandelanotte 2008 {published data only}
- Vandelanotte C, Reeves MM, Brug J, Bourdeaudhuij I, Vandelanotte C, Reeves MM, et al. A randomized trial of sequential and simultaneous multiple behavior change interventions for physical activity and fat intake. Preventive Medicine 2008;46(3):232‐7. [DOI] [PubMed] [Google Scholar]
Verheijden 2007 {published data only}
- Verheijden MW, Jans MP, Hildebrandt VH, Hopman‐Rock M. Rates and determinants of repeated participation in web‐based behavior change program for healthy body weight and healthy lifestyle. Journal of Medical Internet Research 2007;9(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Webber 2008a {published data only}
- Webber KH, Tate DF, Quintiliani LM, Webber KH, Tate DF, Quintiliani LM. Motivational interviewing in internet groups: a pilot study for weight loss. Journal of the American Dietetic Association 2008;108(6):1029‐32. [DOI] [PubMed] [Google Scholar]
Webber 2010 {published data only}
- Webber KH, Gabriele JM, Tate DF, Dignan MB. The effect of a motivational intervention on weight loss is moderated by level of baseline controlled motivation. International Journal of Behavioral Nutrition and Physical Activity 2010;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weinstock 1998 {published data only}
- Weinstock RS, Dai H, Wadden TA. Diet and exercise in the treatment of obesity: effects of 3 interventions in insulin resistance. Archives of Internal Medicine 1998;158(22):2477‐83. [DOI] [PubMed] [Google Scholar]
Werkman 2010 {published data only}
- Werkman A, Hulshof PJ, Stafleu A, Kremers SP, Kok FJ, Schouten EG, et al. Effect of an individually tailored one‐year energy balance programme on body weight, body composition and lifestyle in recent retirees: a cluster randomised controlled trial. BMC Public Health 2010;10:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winett 2007 {published data only}
- Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T, Winett Richard A, et al. Guide to health: nutrition and physical activity outcomes of a group‐randomized trial of an Internet‐based intervention in churches. Annals of Behavioral Medicine 2007;33(3):251‐61. [DOI] [PubMed] [Google Scholar]
Wing 2009 {published data only}
- Wing RR, Pinto AM, Crane MM, Kumar R, Weinberg BM, Gorin AA. A statewide intervention reduces BMI in adults: Shape Up Rhode Island Results. Obesity 2009;17(5):991‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Womble 2004 {published data only}
- Womble LG, Wadden TA, McGuckin BG, Sargent SL, Rothman RA, Krauthamer‐Ewing ES. A randomized controlled trial of a commercial internet weight loss program. Obesity Research 2004;12(6):1011‐8. [DOI] [PubMed] [Google Scholar]
Yon 2007 {published data only}
- Yon BA, Johnson RK, Harvey‐Berino J, Gold BC, Howard AB, Yon BA, et al. Personal digital assistants are comparable to traditional diaries for dietary self‐monitoring during a weight loss program. Journal of Behavioral Medicine 2007;30(2):165‐75. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Harvey‐Berino NCT01232699 {published data only}
- Harvey‐Berino JR. Internet obesity treatment enhanced with motivational interviewing. Clinicaltrials.gov.
Additional references
Arem 2010
- Arem H, Irwin M. A review of web‐based weight loss interventions in adults. Obesity Reviews 2011;12(5):e236‐43. [PUBMED: 20804523] [DOI] [PMC free article] [PubMed] [Google Scholar]
Block 2000
- Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. American Journal of Preventive Medicine 2000;18(4):284‐8. [PUBMED: 10788730] [DOI] [PubMed] [Google Scholar]
Brownell 2000
- Brownell KD. The Learn Program for Weight Management 2000. Euless, TX: American Health Pub Co, 2000. [Google Scholar]
Cohen 1960
- Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement 1960;20:37‐46. [Google Scholar]
Corbett Dooren 2011
- Corbett Dooren J. FDA approves wider use of Allergan's lap band for obesity. The Wall Street Journal. Washington, DC: Dow Jones & Company, Inc., 2011; Vol. February 16.
DPP Research Group 2002
- Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25(12):2165‐71. [PUBMED: 12453955] [DOI] [PMC free article] [PubMed] [Google Scholar]
DynaMed
- DynaMed. Levels of evidence. http://dynamed.ebscohost.com/content/LOE.. DynaMed, Accessed February 22, 2012.
Ferguson 1975
- Ferguson JM. Learning to Eat: Behavior Modification for Weight Control. Palo Alto, CA: Bull Publishing Co., 1975. [Google Scholar]
Finkelstein 2003
- Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying?. Health Affairs (Project Hope) 2003;Suppl Web Exclusives:W3‐219‐26. [DOI] [PubMed] [Google Scholar]
Foster 2005
- Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. American Journal of Clinical Nutrition 2005;82(1 Suppl):230S‐5S. [PUBMED: 16002827] [DOI] [PubMed] [Google Scholar]
Franz 2007
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight‐loss outcomes: a systematic review and meta‐analysis of weight‐loss clinical trials with a minimum 1‐year follow‐up. Journal of the American Dietetic Association 2007;107(10):1755‐67. [PUBMED: 17904936] [DOI] [PubMed] [Google Scholar]
Glasgow 2007
- Glasgow RE, Nelson CC, Kearney KA, Reid R, Ritzwoller DP, Strecher VJ, et al. Reach, engagement, and retention in an Internet‐based weight loss program in a multi‐site randomized controlled trial. Journal of Medical Internet Research 2007;9(2):e11. [PUBMED: 17513282] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2001
- Guyatt G, Cook C, Devereaux PJ, Meade M, Straus S. Therapy. Users' Guides to the Medical Literature: a Manual for Evidence Based Practice. AMA Press, 2001. [Google Scholar]
Health Information Research Unit
- Health Information Research Unit McMaster University. McMaster Online Rating of Evidence (MORE). http://hiru.mcmaster.ca/more_new/.. Hamilton, Ontario: McMaster University, Accessed February 22, 2012.
Heinen 2009
- Heinen L, Darling H. Addressing obesity in the workplace: the role of employers. Milbank Quarterly 2009;87(1):101‐22. [PUBMED: 19298417] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analysis. BMJ 2003;327:557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2009
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.
Jebb 2011
- Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011; Vol. Sep 7 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
Kroeze 2006
- Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer‐tailored education on physical activity and dietary behaviors. Annals of Behavioral Medicine 2006;31(3):205‐23. [PUBMED: 16700634] [DOI] [PubMed] [Google Scholar]
Krukowski 2010
- Krukowski RA, Tilford JM, Harvey‐Berino J, West DS. Comparative cost‐effectiveness for in‐person versus online behavioral weight loss programs. Obesity Reviews 2010;11 Suppl 1:249. [PUBMED: 17316318] 17316318 [Google Scholar]
Lau 2006
- Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ 2006;333:597‐600. [PUBMED: 16974018] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic and meta‐analyses of studies that evaluate interventions: explanation and elaboration. PLoS Medicine 1999;6(7):1‐28. [DOI: 10.1371/journal.pmed.1000100; PUBMED: 19621070] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madden 2006
- Madden M, Fox S. Riding the waves of “Web 2.0”: more than a buzzword, but still not easily defined. http://pewresearch.org/pubs/71/riding‐the‐waves‐of‐web‐20. Washington, DC: Pew Research Center for the People & the Press, 2006:6.
Meenan 2009
- Meenan RT, Stevens VJ, Funk K, Bauck A, Jerome GJ, Lien LF, et al. Development and implementation cost analysis of telephone‐ and Internet‐based interventions for the maintenance of weight loss. International Journal of Technology Assessment in Health Care 2009;25(3):400‐10. [PUBMED: 19619360] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meenan 2010
- Meenan RT, Stevens VJ, Funk K, et al. PS2‐34: Implementation cost analysis of telephone and Internet‐based interventions for the maintenance of weight loss. Clinical Medicine and Research 2010;8(1):52‐b. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2008
- Miller Claire Cain. Woman to Woman, Online. The New York Times. New York: The New York Times, 14 August 2008:1‐C.
Mitchell 2008
- Mitchell D. A small empire built on cuddly and fuzzy branches out from the web. The New York Times. New York: The New York Times, 20 August 2008:4‐C.
Murray 2005
- Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD004274.pub4] [DOI] [PubMed] [Google Scholar]
National Institutes of Health 2000
- National Institutes of Health. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.htm. Bethesda, Maryland: National Institutes of Health, 2000:94.
Neter 2003
- Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta‐analysis of randomized controlled trials. Hypertension 2003;42(5):878‐84. [PUBMED: 12975389] [DOI] [PubMed] [Google Scholar]
Neve 2010
- Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web‐based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta‐analysis. Obesity Reviews 2010;11(4):306‐21. [PUBMED: 19754633] [DOI] [PubMed] [Google Scholar]
Perri 1992
- Perri MG, Nezu AM, Viegener BJ. Improving the Long‐term Management of Obesity: Theory, Research, and Clinical Guidelines. New York, NY: Wiley, 1992. [Google Scholar]
Perri 2001
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem‐solving therapy in the long‐term management of obesity. Journal of Consulting and Clinical Psychology 2001;69(4):722‐6. [PUBMED: 11550740] [PubMed] [Google Scholar]
Perri 2008
- Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, et al. Extended‐care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Archives of Internal Medicine 2008;168(21):2347‐54. [PUBMED: 19029500] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pew 2009
- Pew Research Center for the People & the Press. Internet, Cell Phones Are Changes for the Better. http://pewresearch.org/. Washington, DC: Pew Research Center for the People & the Press, 2009:22.
Pi‐Sunyer 2007
- Pi‐Sunyer FX. How effective are lifestyle changes in the prevention of type 2 diabetes mellitus?. Nutrition Reviews 2007;65(3):101‐10. [PUBMED: 17425061] [DOI] [PubMed] [Google Scholar]
Rasu 2010
- Rasu RS, Hunter CM, Peterson AL, Maruska HM, Foreyt JP. Economic evaluation of an Internet‐based weight management program. American Journal of Managed Care 2010;16(4):e98‐104. [PUBMED: 20370312] [PubMed] [Google Scholar]
Reed 2012
- Reed VA, Schifferdecker KE, Rezaee ME, O'Connor S, Larson RJ. The effect of computers for weight loss: a systematic review and meta‐analysis of randomized trials. Journal of General Internal Medicine 2012;27(1):99‐108. [PUBMED: 21805218] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothman 2000
- Rothman AJ. Toward a theory‐based analysis of behavioral maintenance. Health Psychology 2000;19(1 Suppl):64‐9. [PUBMED: 10709949] [DOI] [PubMed] [Google Scholar]
Rothman 2009
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine 2009;38 Suppl 1:S4‐17. [PUBMED: 19787308] [DOI] [PubMed] [Google Scholar]
Sjöström 2007
Sterne 2001
- Sterne JAC, Egger M, Davey Smith G. Investigating and dealing with publication and other biases. In: Egger M, Davey Smith G, Altman DG editor(s). Systematic Reviews in Health Care; Meta‐analysis in Context. London: BMJ Publishing Group, 2001:189‐208. [Google Scholar]
Stevens 2001
- Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long‐term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Annals of Internal Medicine 2001;134(1):1‐11. [PUBMED: 11187414] [DOI] [PubMed] [Google Scholar]
Stevens 2008
- Stevens VJ, Funk KL, Brantley PJ, Erlinger TP, Myers VH, Champagne CM, et al. Design and implementation of an interactive website to support long‐term maintenance of weight loss. Journal of Medical Internet Research 2008;10(1):e1. [PUBMED: 18244892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tate 2009
- Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of internet interventions: review and recommendations. Annals of Behavioral Medicine 2009;38(1):40‐5. [PUBMED: 19834778] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wantland 2004
- Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web‐based vs. non‐web‐based interventions: a meta‐analysis of behavioral change outcomes. Journal of Medical Internet Research 2004;6(4):e40. [PUBMED: 15631964] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wing 2005
- Wing RR, Phelan S. Long‐term weight loss maintenance. American Journal of Clinical Nutrition 2005;82(1 Suppl):222S‐5S. [PUBMED: 16002825] [DOI] [PubMed] [Google Scholar]
Withrow 2011
- Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obesity Reviews 2011;12(2):131‐41. [PUBMED: 20122135] [DOI] [PubMed] [Google Scholar]
World Health Organization 2004
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. http://www.who.int/dietphysicalactivity/strategy/en/. Geneva: World Health Organization, 2004:21.
World Health Organization 2011
- World Health Organization. Obesity and overweight. WHO Fact Sheet. Geneva: World Health Organization, 2011; Vol. 311.


