Abstract
Botulinum neurotoxins (BoNTs) are listed among the most potent biothreat agents. Simultaneously, two out of seven known serotypes of these toxins are used in medicine and cosmetics. This situation calls for development of detailed epitope maps of these toxins. Such maps will help to develop new ways for decreasing damage caused by these toxins if they were to be used as weapons while retaining the therapeutic effect of these toxins used as medicine. Here, we used a library of random fragments of DNA encoding the catalytic domain of botulinum neurotoxin serotype A to identify short epitope-forming sequences. We demonstrated that knowledge of such sequences in a BoNT of one serotype can be used for identification of epitope-forming sequences in other serotypes of BoNTs. We also demonstrated a serodiagnostic value of identified sequences and their ability to retain epitope-specific structures and trigger production of corresponding antibodies, even when they are transferred into a background of a completely alien carrier protein.
Keywords: botulinum, neurotoxin, epitope, chimers, antibody
1. Introduction
Botulinum neurotoxins (BoNT/A, /B, /C, /D, /E, /F, /G) produced by C. botulinum, C. argentiensis, C. baratii, are the most potent toxins known to mankind (Schantz and Johnson, 1992). Currently, seven different serotypes of these toxins are known: A, B, C, D, E, F and G (BoNT/A, /B, /C, /D, /E, /F and /G, respectively). The diversity becomes even more dramatic when the existence of different subtypes of the same serotype are taken into account (Kalb et al., 2012; Smith et al., 2007). All these homologous toxins specifically target neurons and act through interruption of the process of neurotransmission. This interruption results in muscle paralysis, which, in severe cases of intoxication, leads to death from asphyxiation of humans and animals.
Botulinum neurotoxins are produced by host bacterial cells in the form of single polypeptide chains, which are about 1500 amino acid residues in length (Mr~150 kDa) (Binz et al., 1990; East et al., 1992; Hauser et al., 1990; Poulet et al., 1992; Thompson et al., 1993). A single molecule of each toxin possesses three functional domains: receptor-recognizing, transport and catalytic. Catalytic domains of these toxins are Zn2+ metallo-proteases that recognize and selectively cleave proteins involved in targeting of presynaptic vesicles and their fusion with the neuronal plasma membrane (Schiavo et al., 1992a; Schiavo et al., 1992b; Schiavo et al., 1993a; Schiavo et al., 1993b). In this way, neurotoxins block neurotransmitter release into the synaptic cleft. Although there is a certain degree of homology between different clostridial neurotoxins, their catalytic domains recognize different substrates: BoNT/B, /D, /F and /G cleave synaptobrevin 2, BoNT/A, /C and /E – synaptosomal-associated protein of 25 kDa and BoNT/C – syntaxin (Schiavo et al., 1994). Catalytic domains of clostridial neurotoxins are inactive while connected to the rest of the polypeptide chain by a peptide bond and a disulfide bond (Schiavo et al., 1994). Nevertheless, as a result of limited proteolysis conducted in the presence of reducing agents, a single polypeptide chain of each neurotoxin can be converted into two chains: light (Mr~50 kDa) and heavy (Mr~100 kDa). The light chain corresponds to the catalytic domain while heavy chains of these neurotoxins contain the receptor-recognizing and transport domains, and are responsible for transport of corresponding light chains into the cytosol of neuronal cells.
Botulinum neurotoxins (BoNTs) are listed among the most potent biological warfare agents. At the same time, BoNTs of serotypes A and B are extensively used as drugs for the treatment of multiple neurological conditions (Scott, 1980; Scott et al., 1985) and as rejuvenation agents (Carruthers et al., 1996). The dual nature of applications of these toxins created a need to protect the population from the destructive potential of these toxins if they were to be used as biowarfare agents, while preserving the ability of the population to benefit from using these toxins as drugs. This need has fueled an interest in the detailed epitope structure of these toxins.
In recent years, a number of researchers have been involved in assembling epitope maps of BoNTs. For example, Marks and coauthors used phage or cell displays of BoNT/A fragments and focused on mapping epitopes recognized by isolated monoclonal or single-chain antibodies (Amersdorfer et al., 1997; Amersdorfer et al., 2002; Chen et al., 1997; Levy et al., 2007; Marks, 2004; Mullaney et al., 2001; Nowakowski et al., 2002). Several other groups have published reports on attempts to identify epitopes recognized by antibodies that can neutralize BoNTs (Baldwin et al., 2005; Bavari et al., 1998; Brown et al., 1997; Pless et al., 2001; Wu et al., 2001; Yang et al., 2004). Atassi and coauthors used yet another approach. This group used whole sera from immunized individuals to probe assembled sets of synthetic peptides that encompass the entire length of the chosen BoNT fragment (Atassi, 2004; Atassi et al., 1996; Atassi et al., 2005; Atassi et al., 2012a; Atassi and Oshima, 1999; Dolimbek et al., 2007; Oshima et al., 1998; Rosenberg et al., 1997). These studies revealed that antibodies developed both in humans and mice recognize only a few peptides out of the whole collection of overlapping synthetic peptides. For a long time, the epitope mapping efforts were mostly focused on the heavy chains of botulinum neurotoxins, as those chains were considered to be the most important for development of protective immunity against these toxins (Baldwin et al., 2008; Dux et al., 2011; Smith and Rusnak, 2007; Yu et al., 2009). Only recently were results of the first attempts to analyze the epitope composition of light chains published (Atassi et al., 2011; Atassi et al., 2012a; Atassi et al., 2012b).
Herein, we describe the use of an expression library of short, randomly generated fragments of BoNT/A light chain (BoNT/A-L) for identification of corresponding epitopes. Our results demonstrate that in rabbits, only a limited number of BoNT/A-L regions trigger an immune response. We have demonstrated that simple alignment of BoNTs sequences of different serotypes and projection of identified sequences of BoNT/A-L epitopes onto other BoNT sequences allows identification of epitopes of other BoNTs serotypes. We also demonstrated that epitope-forming peptides may be incorporated into the backbones of BoNT-unrelated carrier proteins, resulting in hybrids carrying epitopes of BoNTs. Such proteins can be used as affinity ligands for purification of corresponding anti-BoNT antibodies, as well as new standards in BoNT detection and identification assays and prototypes of future multivalent “mosaic” vaccines.
2. Materials and methods
2.1. Cell and Plasmids
Escherichia coli DH5αF′ cells were used as a host in the course of all genetic engineering efforts. The same strain was used for expression of assembled hybrid sequences controlled by arabinose promoter. E. coli strain BL21(λDE3) was used for expression of assembled hybrid sequences controlled by bacteriophage T7 promoter. (Studier and Moffatt, 1986). Plasmid pUCentryBoNT/A-L1 which contains the sequence encoding the light chain of BoNT/A, flanked from one side by unique KpnI and XbaI sites and from the other side by unique SalI and SacI sites -- was priorly constructed in our laboratory. This plasmid was used in the process of generation of random fragments of BoNT/A-L. Plasmids pParaBAD-bioGST7, pParaBAD-T7HisbioBirA1, pParaBAD-T7HisbioThio5, and pParaBAD-T7HisbioRAP2 were constructed earlier in our laboratory and were used for expression of fragments of BoNT/A. All of these plasmids have the same backbone and encode derivatives of glutathione S-transferase (GST), biotin ligase from E. coli (BirA), thioredoxin (Thio) and Receptor Associated Protein (RAP), respectively, which were used as carriers for BoNT/A fragments. pParaBAD-bioGST7 encodes GST derivative (bioGST), which at the N-terminus contains a peptide that is specifically biotinylated by BirA both in vivo and in vitro. In this plasmid, the bioGST-encoding sequence is under control of arabinose promoter. Plasmids pParaBAD-T7HisbioBirA1, pParaBAD-T7HisbioThio5, and pParaBAD-T7HisbioRAP2 encode BirA, thioredoxin and RAP derivatives (HisbioBirA, HisbioThio and HisbioRAP, respectively) that, in addition to the target for BirA, contain His-tag at the N-termini. In all three plasmids, expression of hybrid proteins is under control of arabinose and bacteriophage T7 promoters. Unlike plasmid pParaBAD-bioGST7 that carries a gene for ampicillin resistance, these plasmids encode resistance to kanamycin. Also, these plasmids possess unique sites for endonucleases XhoI and SfiI immediately downstream of sequences encoding BirA, thioredoxin and RAP. These features were used to transfer BoNT/AL-encoding fragments from GST-encoding plasmids into plasmids pParaBAD-T7HisbioBirA1, pParaBAD-T7HisbioThio5, and pParaBAD-T7HisbioRAP2. Specifically, DNAs of BoNT/A-L –encoding derivatives of pParaBAD-bioGST7 were consecutively treated with EcoRI, DNA polymerase T4 and XhoI. Resulting fragments were separated by electrophoresis and BoNT/A-L-encoding fragments were isolated from the gel. These fragments were combined with fragments of either pParaBAD-T7HisbioBirA1, pParaBAD-T7HisbioThio5 or pParaBAD-T7HisbioRAP2, similarly generated as a result of consecutive treatment of DNAs of corresponding plasmids with SfiI, DNA polymerase T4 and XhoI, gel electrophoresis and isolation of corresponding large fragments from the gel. After ligation, DNAs were used for transformation of DH5αF′ cells and plasmids of interest were isolated from kanamycin-resistant clones.
Plasmid pETαtoxABglII1 was previously constructed in our lab. This plasmid possesses a sequence encoding a modified α-toxin of Clostridium perfringens and controlled by the promoter of bacteriophage T7.
All vectors used in these studies were constructed to carry similar polylinkers downstream from the sequence encoding the corresponding carrier protein. This feature allowed simple transfer of BoNT epitope-encoding sequences from one plasmid into another.
2.2. DNA modifying enzymes
All restriction endonucleases, as well as T4 DNA-polymerase, S1 nuclease and rapid DNA ligation kit, were supplied by Fermentas Life Sciences.
2.3. Oligonucleotides
Oligonucleotides used for assembling DNA encoding epitope-forming peptides are listed in Table 2. All of these oligonucleotides were synthesized at GenScript Corporation. Oligonucleotides for epitope-forming peptides Fep1s and Bep1s are made to form a sequence recognized by restriction endonuclease SalI. This sequence is located downstream from the sequence encoding the epitope-forming peptide itself. Cohesive ends generated by the endonuclease SalI are compatible with cohesive ends generated by restriction endonuclease XhoI, whose sites are present in polylinkers of all our vectors and upstream of sequences encoding epitope-forming peptides. This feature was used for fast combination of different epitope-forming sequences into the same plasmid. Indeed, the epitope-encoding fragment, generated by treatment with NdeI (site present in all vectors upstream from the XhoI site) and SalI, of a plasmid encoding the epitope of one type can be incorporated in the NdeI and XhoI sites of a plasmid encoding the epitope of another type. The resulting plasmid carries a sequence encoding both epitopes joined by a short peptide linker.
Table 2.
Oligonucleotides used for assembly of sequences encoding epitopes of BoNTs light chains.
| Name | Sequence | Used for |
|---|---|---|
| Ep1-5′ | 5′-gtacctggatccgttccggttagctattatgatagcacgtatttaagcacctaagcctgca | DNA fragment formed by these oligonucleotides was inserted into Acc65I-SdaI sites of pParaBAD-T7HisbioRAP2 to create plasmid encoding HisbioRAP-ep1s |
| Ep1-3′ | 5′-ggcttaggtgcttaaatacgtgctatcataatagctaaccggaacggatccag | |
| Ep4-5′ | 5′-gtacctggatcctttaatggtcaaaataccgaaattaataatatgaattttaccaaataagcctgca | DNA fragment formed by these oligonucleotides was inserted into Acc65I-SdaI sites of pParaBAD-T7HisbioRAP2 to create plasmid encoding HisbioRAP-ep4s |
| Ep4-3′ | 5′-ggcttatttggtaaaattcatattattaatttcggtattttgaccattaaaggatccag | |
| A-Zn5′ | 5′-ctggatcccatgaactgattcatgcgggccatcgcctgtatggcattgtcgactaaagcctgca | DNA fragment formed by these oligonucleotides was inserted into KpnI-SdaI sites of pParaBAD-T7HisbioRAP2 to create plasmid encoding HisbioRAP-A-Zn |
| A-Zn3′ | 5′-ggctttagtcgacaatgccatacaggcgatggcccgcatgaatcagttcatgggatccaggtac | |
| Fep1-5′ | 5′-ctggatccggcagcagcgcgtattatgatccgaactatctgaccaccgtcgactaagcctgca | DNA fragment formed by these oligonucleotides was inserted into KpnI-SdaI sites of pParaBAD-T7HisbioRAP2 to create plasmid encoding HisbioRAP-Fep1s |
| Fep1-3′ | 5′-ggcttagtcgacggtggtcagatagttcggatcataatacgcgctgctgccggatccaggtac | |
| Bep1-5′ | 5′-ctggatccgatgtgtgcgaatattatgatccggattatctgaacaccgtcgactaagcctgca | DNA fragment formed by these oligonucleotides was inserted into KpnI-SdaI sites of pParaBAD-T7HisbioRAP2 to create plasmid encoding HisbioRAP-Bep1s |
| Bep1-3′ | 5′-ggcttagtcgacggtgttcagataatccggatcataatattcgcacacatcggatccaggtac |
2.4. Antibodies
Rabbit sera raised against BoNT/A, /B and /F were kindly provided by Dr. Vertiev (Moscow, Russia). Also, to verify that identified epitopes and observed phenomena are not related to some unique properties of one specific serum, we used purified rabbit antibodies raised to the same serotypes of BoNT and purchased from Metabiologics Inc (Madison, USA).
2.5. Screening of library of hybrids carrying random BoNT/A-L fragments
The library was grown on LB-agar plates supplemented with ampicillin in the form of separate colonies. A replica of each plate was made by covering the plate with a sterile nitrocellulose filter and transferring each filter with the attached colonies onto a fresh LB-agar plate supplemented with ampicillin and arabinose. After 5 hours of incubation at 37°C, each filter was transferred for 5 min onto filter paper soaked with 0.1 M NaOH. Then, it was dried for 5 minutes at room temperature and transferred onto filter paper soaked with 1 M TrisHCl, pH 8.0. After colony debris was gently lifted and removed from each filter in PBS buffer containing 0.01% Tween20 (PBST), filters were incubated for 1 hour at 37°C in PBST supplemented with 2% BSA to block nonspecific canters of adsorption. After that, each filter was incubated with anti-BoNT/A, followed by incubation with anti-rabbit antibodies conjugated with horse radish peroxidase. Visualization of colonies producing BoNT/A epitopes was achieved with Metal Enhanced DAB Substrate Kit (Pierce, Inc).
2.6. Expression and Purification of Recombinant Proteins
All cultures were grown at 37°C until they reached an absorbency of 0.5–0.6 (600 nm). Protein expression was induced by addition of isopropyl-β-D thiogalactoside. Cultures (except for that possessing a derivative of plasmid pETαtoxABglII1) were transferred to 24°C and 16 hours later cells were harvested by centrifugation. After lysis of collected cells by sonication, proteins of interest were purified from a soluble cell fraction by affinity chromatography on Ni-NTA Superflow (Qiagen). The culture with the derivative of plasmid pETαtoxABglII1 was incubated at 37°C for 90 minutes and then culture media was separated from cells by centrifugation. The α-Tox-FBAep1s protein was purified from this culture media by ultrafiltration on PREP/SCALE-TFF Cartridge 30K (Millipore) and ion-exchange chromatography on HiTrap™ Q FF (GE Healthcare).
2.7. Immunization
Six- to eight-week-old female BALB/c mice were purchased from Harlan Laboratories, Inc. All mice were allowed a 1-week period of acclimatization prior to initiation of experiments. Mice were vaccinated 50% intraperitoneally and 50% subcutaneously with formaldehyde-treated α-Tox-FBAep1s in the presence of Freund’s Complete and Freund’s Incomplete as adjuvants. Three rounds of immunization were performed two weeks apart with increasing doses of α-Tox-FBAep1s (10, 20 and 40 μg, respectively). 300 μl of blood were obtained after 28 and 42 days of each immunization from the tail vain and sera were separated from blood cells by centrifugation.
2.8. ELISA
100 μl aliquots of diluted mouse sera were incubated in wells of an ELISA plate, precoated with α-Tox-FBAep1s or HisbioRAP-FBAep1s at 37°C for 60 min. After washing, the plate was incubated with goat anti-mice IgG (horseradish peroxidase conjugated; Accurate Chemical) for 45 min at 37°C. Following a final wash, 200 μl of tetramethyl benzidine substrate was added to each well for 20 min. The reaction was terminated by addition of 1 N H2SO4 (final concentration of 0.2 N) and read at 450 nm (Molecular Dynamics).
Western – after separation by 4–20% SDS PAGE, proteins were transferred onto an Immobilon Psq membrane. Centers for unspecific sorption were blocked by incubation of membranes in PBS containing 0.1% Tween 20 and 2% BSA. Then, membranes were incubated with appropriate anti-BoNT antibodies followed by incubation with either anti-rabbit or anti-mouse antibodies conjugated with horseradish peroxidase. Visualization of horseradish peroxidase was achieved with ImmunoPure® Metal Enhanced DAB Substrate Kit from Pierce (Rockford, IL).
3. Results
3.1. Construction and screening of library of random fragments of BoNT/A light chain
The library of short random fragments of BoNT/A-L required for the search of epitope-forming sequences was constructed in three stages. During the first two stages, progressively extending sequences were removed from each side of DNA encoding BoNT/A-L. For this, the DNA of plasmid pUCentryBoNT/A-L1 was first cut with restriction endonucleases KpnI and XbaI whose sites are located upstream from the sequence encoding BoNT/A-L with the XbaI site located between the KpnI site and BoNT/A-L- encoding sequence. Restriction endonuclease XbaI generates 5′-protruding ends that can be used by Exonuclease III as a substrate while endonuclease KpnI generates 3′-protruding ends that are resistant to degradation by Exonuclease III. Treatment of pUCentryBoNT/A-L1 linearized with endonucleases XbaI and KpnI for different periods of time with Exonuclease III, followed by treatment with nuclease S1 and DNA ligase, resulted in the library of plasmids with deletions of different length that all start at the same point, located upstream of the BoNT/A-L-encoding sequence, and extend into this sequence. Similarly, we used treatment of the resulting library of plasmids with endonucleases SalI and SacI, followed by treatment with Exonuclease III, nuclease S1 and DNA ligase, to further modify the resulting library of plasmids via introduction of unidirectional deletions of varying length into 3′-end regions of BoNT/A-L-encoding sequences. The third stage of library construction involved 1) treatment of the collection of created plasmids with endonuclease EcoRI and DNA polymerase T4 followed by treatment with endonuclease XhoI, 2) isolation of 100–150 b.p.-long products from the agarose gel, and 4) cloning of resulting DNA fragments into expression vector pParaBAD-bioGST7, treated with endonucleases Ecl136II and XhoI.
With the exclusion of linker regions, the average length of BoNT/A-encoding sequences in DNA fragments purified from the gel and incorporated into each plasmid should be ~75 b.p. The resulting library was composed of 3×104 independent clones. This size should be sufficient to represent all random 85 b.p.-long fragments of BoNT/A-L-encoding sequences, even considering that in only one out of three clones does the reading frame of the BoNT/A-L-encoding fragment coincide with the reading frame of the carrier protein.
Screening of the resulting library was conducted using rabbit anti-BoNT/A antibodies as described in Materials and Methods. This screening revealed a number of positive clones. BoNT/A-L-related sequences of some of them are presented in Fig. 1. Alignment of these sequences with the primary structure of BoNT/A-L revealed that they were clustered around four areas designated ep1, 2, 3 and 4. The corresponding fragments of BoNT/A-L were designated Aep1, 2, 3 and 4, followed by the additional number (Aep1-1, Aep1-2, for example).
Figure 1. Relative location of epitope-forming peptides on the primary structure of light chain of botulinum neurotoxin serotype A.
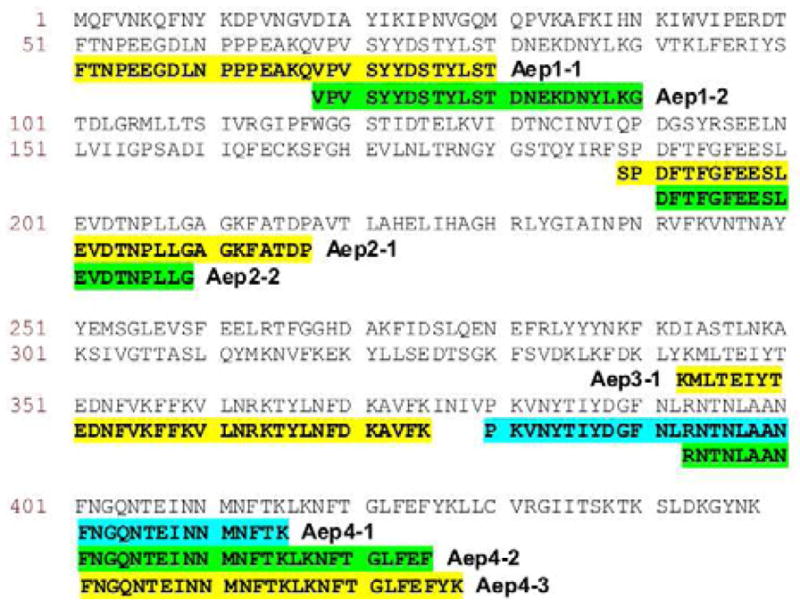
Identified sequences of peptides are highlighted and their names are marked by the bold text. Sequence of light chain of botulinum neurotoxin serotype A is in plain text.
Although all identified clones were carrying plasmids that, with the exception of a very short BoNT/A-L-encoding region, were identical to each other, further analysis revealed a lack of consistency in accumulation of corresponding hybrid proteins by host cells. Specifically, some plasmids directed production of hybrid proteins that were present in the cell predominantly in the soluble form, while others directed production of proteins that were accumulated in the form of inclusion bodies. In an attempt to consistently produce BoNT/A-L fragment-carrying proteins in soluble form, we tested three additional plasmids (pParaBAD-T7HisbioBirA1, pParaBAD-T7HisbioThio5, and pParaBAD-T7HisbioRAP2) as hosts for BoNT/A-L-encoding fragments. These plasmids are similar to each other, but encode BirA, thioredoxin, or RAP derivatives, respectively. Out of three tested plasmids, only pParaBAD-T7HisbioRAP2 assured consistent accumulation of BoNT/A-L fragment-carrying hybrids in the soluble form. Due to the His-tag present at their N-termini, RAP-BoNT/A-L hybrids are easy to purify (Fig. 2). Western blot of purified proteins confirmed that these proteins (see HisbioRAP-Aep1-1 and HisbioRAP-Aep2-1 on Fig. 2) are recognized by anti-BoNT/A antibodies and most likely encode linear epitopes. The only exception was a hybrid protein carrying fragment Aep3. After heat treatment and SDS exposure preceding Western blot, the RAP derivative carrying this fragment lost the ability to be recognized by rabbit anti-BoNT/A. This suggests that Aep3 fragment may form a structural epitope.
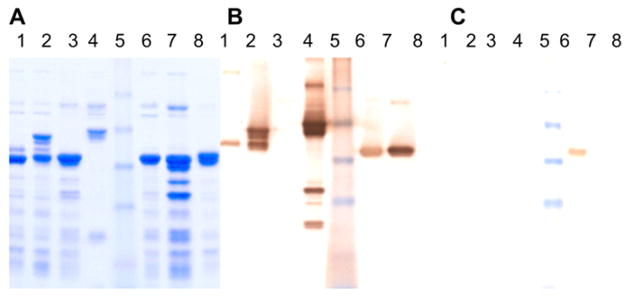
Figure 2. Purification and antigenic properties of RAP-containing hybrid proteins.
After purification on Ni-Sepharose, HisbioRAP derivatives were subjected to SDS PAGE and were visualized by staining with Coomassie (A), or were transferred onto a nitrocellulose membrane and treated with either rabbit anti-BoNT/A serum (B) or fraction of rabbit anti-BoNT/A serum, affinity purified on resin containing HisbioRAP-ep4s (C), and followed by treatment with anti-rabbit-horse radish peroxidase conjugate and diamine benzidine.
Line 1 contains HisbioRAP-Aep2, 2 - HisbioRAP-Aep1-1, 3 - HisbioRAP, 4 – BoNT/AB-L (a derivative of BoNT/A-L whose C-terminal ep4-containing region is substituted with the corresponding region of BoNT/B-L), 5 - pre-stained molecular weight markers from Invitrogen, Inc., 6 – HisbioRAP-Aep4s, 7 - HisbioRAP-Aep1s, and 8 - HisbioRAP-random peptide.
3.2. Further localization of epitope-forming sequences
BoNT/A-L fragments isolated from the expression library and listed in Fig. 1 are relatively long and may form more than one BoNT/A epitope. In an attempt to identify sequences forming single epitopes, we used overlapping peptides (such as Aep1-1 and Aep1-2, as well as peptides Aep4-1, Aep4-2 and Aep4-3). Synthetic DNA fragments corresponding to common areas in these overlaps, designated Aep1s and Aep4s, accordingly, were incorporated into the backbone of vector pParaBAD-T7HisbioRAP2. The resulting hybrid proteins (HisbioRAP-ep1s and HisbioRAP–ep4s, accordingly) were tested for the ability to be recognized by anti-BoNT/A. As a control, we used hybrid protein HisbioRAP-A-Zn, which carries a BoNT/A-L peptide from the most conservative region among all BoNT light chains (Fig. 3). Figs. 2 and 4 depict that both HisbioRAP-ep1s and HisbioRAP–ep4s were tested epitope-positive with rabbit antibodies raised to BoNT/A. At the same time, protein HisbioRAP-A-Zn was not recognized by these antibodies, suggesting that not every part of the BoNT/A-L molecule is used by the immune system of a mammalian organism to mount an immunologic response. To further confirm the specificity of structures formed by peptides Aep1s and Aep4s, we used the presence of a biotinylatable peptide in the structures of hybrid proteins HisbioRAP-ep1s and HisbioRAP–ep4s. This peptide is recognized by biotin ligase of E. coli, which modifies this peptide and, consequently, the whole hybrid protein, by attachment of a single biotin residue. Because of this residue, corresponding proteins can be immobilized on streptavidin-agarose beads and in this form can be used for purification of corresponding mono epitope-specific antibodies. Analysis revealed that antibodies isolated in this manner were able to recognize BoNT/A-L (data not presented) and proteins carrying the corresponding epitope (Fig. 2). At the same time, these antibodies were not able to recognize hybrids carrying other BoNT/A-L epitopes or BoNT/A-L derivatives in which the corresponding epitope-forming sequence was substituted with a sequence from the light chain of BoNT/B-L (see BoNT/AB-L on Figs. 2 and 4).
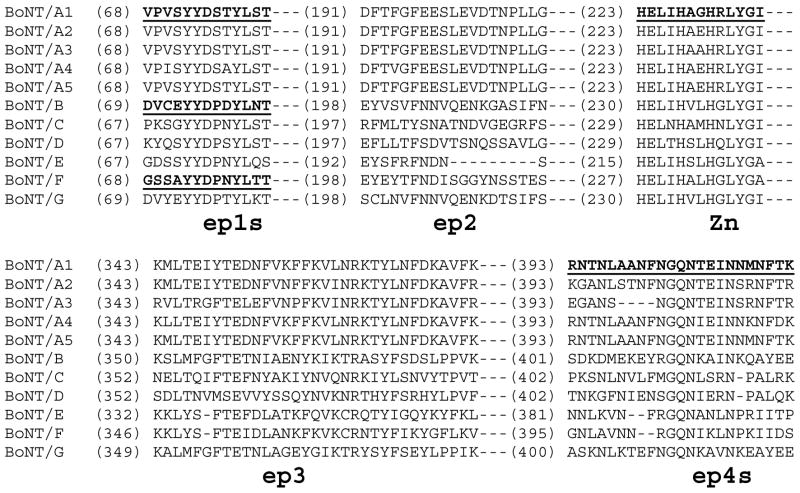
Figure 3. Relative location of BoNTs sequences used for construction of RAP derivatives on the alignment of sequences of BoNT/A subtypes and BoNT serotypes.
Sequences of BoNTs incorporated into RAP derivatives are marked by grey shadow and designated ep1s, ep4s and Zn. Yellow, green and blue colors are used to mark homologous residues, and the dashed lines represent not shown sequences located between two depicted blocks.
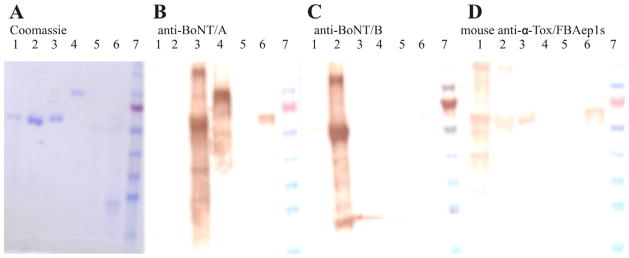
Figure 4. Recognition of RAP derivatives containing epitope-forming peptides by antibodies raised to different serotypes of BoNTs.
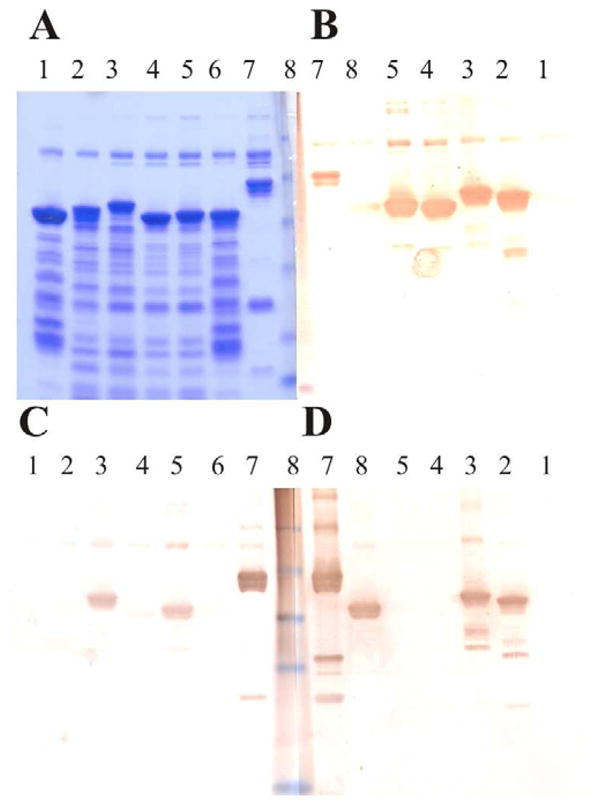
After purification on Ni-Sepharose, HisbioRAP derivatives were subjected to SDS PAGE and were visualized either by staining with Coomassie (A), or were transferred onto a nitrocellulose membrane and treated with rabbit anti-BoNT/F (B), anti-BoNT/B (C), or anti-BoNT/A (D), followed by treatment with anti-rabbit-horse radish peroxidase conjugate and diamine benzidine.
Line 1 contains HisbioRAP-A-Zn, 2 - HisbioRAP-FAep1s, 3 - HisbioRAP-BAep1s, 4 - HisbioRAP-Fep1s, 5 - HisbioRAP-Bep1s, 6 - HisbioRAP-Aep1s, 7 –BoNT/AB-L (a BoNT/A-L derivative whose C-terminal region is substituted with the corresponding region of BoNT/B-L), 8 - pre-stained molecular weight markers from Invitrogen, Inc.
3.3. Identification of epitope-forming sequences in BoNT-Ls other than serotype A and their combination into one hybrid protein
Due to the existing homology between botulinum neurotoxins it was reasonable to suggest that localization of epitopes in the molecule of one serotype will be similar to localization of those in other serotypes. If so, knowledge about epitope-forming sequences in a BoNT of one serotype can be used to identify corresponding epitopes of other serotypes. To test this hypothesis, we constructed proteins HisbioRAP-Bep1s and HsibioRAP-Fep1s that, instead of peptide Aep1s, possess homologous sequences from BoNTs serotypes B and F, respectively (see Fig. 3). The reason for choosing the ep1 region is related to our desire to see not only whether homologous regions from different serotypes of BoNT will trigger an immune response, but also whether corresponding antibodies will have a sero-diagnostic value. For this reason, we decided to use sequences that have the smallest degree of differences. As shown in Fig. 3, the ep1 region is the most conservative among four regions we have identified.
Analysis of the antigenic composition of proteins HisbioRAP-Bep1s and HsibioRAP-Fep1s revealed that each of these proteins was recognized by rabbit sera raised to the corresponding serotype of BoNT (Fig. 4). Among three different serotype-specific antibodies, only antibodies raised against BoNT serotype F were able to recognize the protein carrying heterologous peptide Bep1s. At the same time, these antibodies did not recognize the protein carrying peptide Aep1s. Nor did antibodies raised to BoNTs of serotypes A and B recognize hybrids carrying peptides from BoNTs of different serotypes. All of this data suggests the serodiagnostic value of ep1s peptides, as well as that structures of corresponding epitopes are quite stable and can be transposed into very different protein backgrounds.
To further test the robustness of these structures, we incorporated ep1s peptides, originating from two different serotypes of BoNTs, into the same carrier protein. Specifically, we assembled protein HisbioRAP-BAep1s, which carries peptides from BoNTs of serotypes B and A, and protein HisbioRAP-FAep1s, which carries peptides from BoNTs of serotypes F and A. Fig. 4 demonstrates that both proteins were detected as epitope positive by both types of corresponding serotype-specific antibodies: HisbioRAP-BAep1s was recognized by anti-BoNT/A and /B while HisbioRAP-FAep1s was recognized by anti-BoNT/F and /A. The inability of antibodies raised against BoNT/B to recognize HisbioRAP-FAep1s confirms the serotype-specific mode of interaction between hybrid proteins and anti-BoNTs. Antibodies raised to BoNT serotype F demonstrated the ability to recognize protein HisbioRAP-BAep1s, which, similarly to previously described protein HisbioRAP-Bep1s, did not carry an epitope originating from BoNT/F. This fact, however, does not suggest that HisbioRAP-BAep1s has gained a new affinity to antibodies that is not related to BoNT epitopes. Rather, it suggests that the preparation of anti-BoNT/F also had an affinity to BoNT/B. The ability of these antibodies to recognize BoNT/AB-L (which carries Bep4 instead of Aep4), but not BoNT/A-L, seems to support this hypothesis. The previously reported abilities of some C. botulinum strains to produce a mixture of predominantly one serotype of neurotoxin with a small amount of toxin of another serotype may explain the observed phenomenon. Interestingly, we tested anti-BoNT/Fs originating from two independent sources and observed their ability to recognize epitopes of serotype B in both cases.
3.4. Analysis of immunogenic properties of identified BoNT/Ls epitope-forming sequences
To determine whether identified epitope-forming sequences and hybrid proteins carrying them can be used as immunogens for triggering anti-BoNT responses or not, we assembled a combination of all three above-listed ep1s peptides (Aep1s, Bep1s and Fep1s) on the backbone of a new carrier protein – a derivative of Clostridium perfringens α-toxin. Earlier, we found that this carrier protein is capable of transporting itself along with polypeptides fused to it from E. coli cells into the culture media. As expected, the resulting α-Tox-FBAep1s hybrid was the only high-molecular weight polypeptide present in E. coli culture media in significant quantities. This feature has substantially simplified purification of the hybrid. Upon ultrafiltration followed by ion-exchange chromatography, this protein was co-incubated with formaldehyde to inhibit residual toxic activity of α-toxin and in this form was used for immunization of mice. The efficiency of immunization was monitored by comparison of anti-target antigen affinities present in sera of pre- and post-vaccination bleeds. Antibodies were analyzed by ELISA using α-Tox-FBAep1s and HisbioRAP-FBAep1s as specific targets. The second protein was created by joining a portion of α-Tox-FBAep1s that possesses all three BoNT epitope-forming peptides with the above-mentioned carrier protein, HisbioRAP. This portion is the only sequence shared by proteins α-Tox-FBAep1s and HisbioRAP-FBAep1s. Data of ELISA presented in Table 1 demonstrated that immunization triggered production of antibodies recognizing this common region of both proteins. Further analysis revealed that vaccination with α-Tox-FBAep1s triggered production of antibodies that recognized not only HisbioRAP-FBAep1s, but also light chains of BoNT/A, /B, /F and even tetanus toxin (Fig. 5) and BoNT/G (data not presented). At the same time, post-vaccination sera recognized neither HisbioRAP, carrying a sequence of BoNT/A-L other than peptide Aep1s (protein HisbioRAP-A-Zn), nor protein gfp-BoNT/A-CH, composed of Green Fluorescent Protein and the receptor-recognizing domain of BoNT/A.
Table 1.
Accumulation of antigen-specific antibodies in sera of immunized mice.
| Animal Antigen | A | B | ||
|---|---|---|---|---|
| α–Tox-FBAep1s | HisbioRAP-FBAep1s | α–Tox-FBAep1s | HisbioRAP-FBAep1s | |
| Bleed 1 | 9.5X1 | 3.9X | 4.9X | 1.3X |
| Bleed 2 | 18.8X | 2.8X | 9.0X | 1.3X |
| Bleed 3 | 33.7X | 15X | 30X | 4.1X |
Results are presented as an amount over background i.e. 30X means the test bleed sera produced an OD450 30 times higher than the pre-immune bleed sera in a direct ELISA.
Fig. 5. Specificities of antibodies raised to the hybrid protein carrying three different epitope-forming peptides.
Purified proteins were subjected to SDS PAGE and were visualized either by staining with Coomassie (A), or were transferred onto a nitrocellulose membrane and treated with rabbit anti-BoNT/A (B), anti-BoNT/B (C), or sera of mice immunized with α–Tox/FBAep1s (D), followed by the treatment with either donkey anti-rabbit-horse radish peroxidase conjugate (B and C) or goat anti-mice-horse radish peroxidase conjugate (D). Antibodies trapped on the filter were visualized with Metal Enhanced DAB Substrate Kit (Pierce, Inc).
Line 1 contains light chain of tetanus toxin, 2 – BoNT/B-L, 3 – BoNT/A-L, 4 – gfp-BoNT/ACH, 5 –HisbioRAP-A-Zn, 6 - HisbioRAP-FBAep1s and 7 - pre-stained molecular weight markers from Fermentas
4. Discussion
Using the light chain of BoNT/A as a model, we demonstrated that libraries of random fragments of the specific protein may be used as a reliable and inexpensive tool for revealing epitope-forming sequences of this protein. Using this tool, we confirmed an earlier observation by Atassi and coauthors that antibodies developed in a mammalian organism target only a limited number of BoNT regions in response to BoNT immunization. Specifically, we determined that only four discrete regions (Aep1, Aep2, Aep3 and Aep4) within BoNT/A-L sequence are recognized by rabbit anti-BoNT/A serum. Three (Aep2, Aep3 and Aep4) out of these four regions were reported earlier as those targeted by the immune response in cervical dystonia patients who developed a resistance to BoNT/A (Dolimbek et al., 2011). Taken together, these data suggest that identified epitopes are not randomly chosen by the immune system of the specific animal or specie, but rather reveal some important structures in the BoNT/A molecule and are universally targeted by different species. The importance of identified regions is supported by the finding that regions of BoNTs serotypes B and F (Bep1 and Fep1), homologous to the Aep1, are similarly targeted by the rabbit immune response. Presented data demonstrate that antibodies recognizing these regions may have sero-diagnostic value. Also, taking into account results of alignment presented in Fig. 3 and experimental data obtained with ep1, it is possible to predict that antibodies to at least some of these regions may be instrumental for distinguishing different neurotoxin subtypes. Interestingly, the Aep1 region was not revealed in studies of Atassi and coauthors as triggering an immune response in cervical dystonia patients (Dolimbek et al., 2011).
At the same time, the same group reported that the peptide overlapping with the Bep1 region is recognized by antibodies from cervical dystonia patients (Atassi et al., 2012a). On one hand, the inability of Atassi et al. to identify the Aep1 region may reflect differences between immune responses of different species to BoNTs. Alternatively, it may reflect limitations of the library of artificially chosen peptides as an epitope-detecting tool. Indeed, in the library Atassi et al. used to map BoNT/A-L epitopes, the Aep1 region was not present on a single peptide, but instead was split between two different peptides.
Here we demonstrated the abilities of identified epitopes to retain toxin-specific structure and trigger production of toxin-specific antibodies, even when corresponding epitope-forming sequences were incorporated in the backbone of a completely alien protein. These results suggest the possibility of assembling a new generation of vaccines – “mosaic” vaccines. These vaccines will utilize hybrid proteins carrying a collection of several different epitopes originating from the same pathogen or even from different pathogens. Unlike native pathogens or their components, these proteins will be safe, and easier to produce and formulate into a stable vaccine. Existing data suggest that, at least in the case of bacterial toxins, combination of just two-three pathogen-specific monoclonal antibodies may be able to neutralize the corresponding pathogen even better than corresponding hyperimmune sera. Consequently, a single hybrid protein carrying just two-three well chosen epitopes per individual pathogen may be able to trigger protective immunity against several pathogens simultaneously. Data presented here demonstrate that peptides as short as 13 amino acid residues can be used as epitope-forming components of the mosaic vaccine. This leads to the expectation that a single carrier protein (such as α-Tox used in this study) can easily be adapted to carry protective combinations of epitopes from three-four different pathogens without becoming too big to raise stability and production issues. The ability of the α-Tox-derivatives to accumulate in E. coli culture media creates the possibility for development of extremely simple and cost-effective production of future mosaic vaccines.
Finally, the phenomenon observed in the current study, of generating affinities against epitopes of light chains of BoNT/G and tetanus toxin, even though epitopes for these proteins were not present in the α-Tox derivative used for immunization, deserves special attention. There are two possible explanations for this phenomenon. First, the combination of epitope ep1-encoding peptides resulted in formation of new epitopes that are not related to ep1 epitopes. Alternatively, it is possible that ep1 epitopes present in the hybrid protein trigger production of antibodies that recognize additional modifications of the same ep1 epitope motif. If the first hypothesis is correct, proteins carrying a collection of pathogens’ epitopes will be unsuitable as vaccine components, because they may be able to trigger unpredicted immune responses targeting even host proteins. This subject requires further detailed examination. However, because of the demonstrated inability of sera from mice vaccinated with α-Tox-FBAep1s to recognize proteins related to BoNTs and yet not carrying ep1 epitopes, we suspect that the second hypothesis is closer to reality. If so, mosaic vaccines may have an additional advantage over traditional vaccines by triggering immunity to a broader spectrum of mutants of corresponding pathogens.
5. Conclusions
There is a limited number of regions in the botulinum neurotoxin molecule that are targeted by immune systems of mammalian organisms.
Knowledge of epitopes of one serotype of botulinum neurotoxin can be used to determine the location of epitopes in other serotypes.
Short epitope-forming peptides of botulinum neurotoxins retain their structure even if incorporated into the structure of completely foreign carrier proteins.
α-toxin of Clostridium perfringens can be used as a carrier for foreign polypeptides and has the ability to transport these polypeptides outside of E. coli cells.
Highlights.
Random fragments of BoNT/A light chain ware screened with rabbit anti-BoNT/A serum.
Four separate epitope-forming regions were determined.
Epitopes in other serotypes were determined by alignment of sequences.
Epitopes retain their structure even when incorporated into other proteins
α-toxin of C. perfringens can carry foreign polypeptides outside of the E. coli cell.
Acknowledgments
We thank Dr. Vertiev (Russia) for providing rabbit sera raised against botulinum neurotoxins serotypes A, B and F.
This work was supported by Public Health Service grant 1R43AI056852 from the National Institute of Allergy and Infectious Diseases.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amersdorfer P, Wong C, Chen S, Smith T, Deshpande S, Sheridan R, Finnern R, Marks JD. Molecular characterization of murine humoral immune response to botulinum neurotoxin type A binding domain as assessed by using phage antibody libraries. Infect Immun. 1997;65:3743–3752. doi: 10.1128/iai.65.9.3743-3752.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amersdorfer P, Wong C, Smith T, Chen S, Deshpande S, Sheridan R, Marks JD. Genetic and immunological comparison of anti-botulinum type A antibodies from immune and non-immune human phage libraries. Vaccine. 2002;20:1640–1648. doi: 10.1016/s0264-410x(01)00482-0. [DOI] [PubMed] [Google Scholar]
- Atassi MZ. Basic immunological aspects of botulinum toxin therapy. Mov Disord. 2004;19(Suppl 8):S68–84. doi: 10.1002/mds.20020. [DOI] [PubMed] [Google Scholar]
- Atassi MZ, Dolimbek BZ, Hayakari M, Middlebrook JL, Whitney B, Oshima M. Mapping of the antibody-binding regions on botulinum neurotoxin H-chain domain 855–1296 with antitoxin antibodies from three host species. J Protein Chem. 1996;15:691–700. doi: 10.1007/BF01886751. [DOI] [PubMed] [Google Scholar]
- Atassi MZ, Dolimbek BZ, Jankovic J, Steward LE, Aoki KR. Regions of botulinum neurotoxin A light chain recognized by human anti-toxin antibodies from cervical dystonia patients immunoresistant to toxin treatment. The antigenic structure of the active toxin recognized by human antibodies. Immunobiology. 2011;216:782–792. doi: 10.1016/j.imbio.2010.12.009. [DOI] [PubMed] [Google Scholar]
- Atassi MZ, Dolimbek GS, Deitiker PR, Aoki KR, Dolimbek BZ. Submolecular recognition profiles in two mouse strains of non-protective and protective antibodies against botulinum neurotoxin A. Mol Immunol. 2005;42:1509–1520. doi: 10.1016/j.molimm.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Atassi MZ, Jankovic J, Steward LE, Aoki KR, Dolimbek BZ. Molecular immune recognition of botulinum neurotoxin B. The light chain regions that bind human blocking antibodies from toxin-treated cervical dystonia patients. Antigenic structure of the entire BoNT/B molecule. Immunobiology. 2012a;217:17–27. doi: 10.1016/j.imbio.2011.08.009. [DOI] [PubMed] [Google Scholar]
- Atassi MZ, Oshima M. Structure, activity, and immune (T and B cell) recognition of botulinum neurotoxins. Crit Rev Immunol. 1999;19:219–260. [PubMed] [Google Scholar]
- Atassi MZ, Oshima M, Dolimbek BZ, Aoki KR. Antibody and T cell recognition of the light chain of botulinum neurotoxin A in two high-responder mouse strains. Immunobiology. 2012b;217:1–7. doi: 10.1016/j.imbio.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Baldwin MR, Tepp WH, Pier CL, Bradshaw M, Ho M, Wilson BA, Fritz RB, Johnson EA, Barbieri JT. Characterization of the antibody response to the receptor binding domain of botulinum neurotoxin serotypes A and E. Infect Immun. 2005;73:6998–7005. doi: 10.1128/IAI.73.10.6998-7005.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin MR, Tepp WH, Przedpelski A, Pier CL, Bradshaw M, Johnson EA, Barbieri JT. Subunit vaccine against the seven serotypes of botulism. Infect Immun. 2008;76:1314–1318. doi: 10.1128/IAI.01025-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bavari S, Pless DD, Torres ER, Lebeda FJ, Olson MA. Identifying the principal protective antigenic determinants of type A botulinum neurotoxin. Vaccine. 1998;16:1850–1856. doi: 10.1016/s0264-410x(98)00175-3. [DOI] [PubMed] [Google Scholar]
- Binz T, Kurazono H, Wille M, Frevert J, Wernars K, Niemann H. The complete sequence of botulinum neurotoxin type A and comparison with other clostridial neurotoxins. J Biol Chem. 1990;265:9153–9158. [PubMed] [Google Scholar]
- Brown DR, Lloyd JP, Schmidt JJ. Identification and characterization of a neutralizing monoclonal antibody against botulinum neurotoxin serotype F, following vaccination with active toxin. Hybridoma. 1997;16:447–456. doi: 10.1089/hyb.1997.16.447. [DOI] [PubMed] [Google Scholar]
- Carruthers A, Kiene K, Carruthers J. Botulinum A exotoxin use in clinical dermatology. J Am Acad Dermatol. 1996;34:788–797. doi: 10.1016/s0190-9622(96)90016-x. [DOI] [PubMed] [Google Scholar]
- Chen F, Kuziemko GM, Amersdorfer P, Wong C, Marks JD, Stevens RC. Antibody mapping to domains of botulinum neurotoxin serotype A in the complexed and uncomplexed forms. Infect Immun. 1997;65:1626–1630. doi: 10.1128/iai.65.5.1626-1630.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolimbek BZ, Aoki KR, Steward LE, Jankovic J, Atassi MZ. Mapping of the regions on the heavy chain of botulinum neurotoxin A (BoNT/A) recognized by antibodies of cervical dystonia patients with immunoresistance to BoNT/A. Mol Immunol. 2007;44:1029–1041. doi: 10.1016/j.molimm.2006.03.011. [DOI] [PubMed] [Google Scholar]
- Dolimbek BZ, Steward LE, Aoki KR, Atassi MZ. Regions of recognition by blocking antibodies on the light chain of botulinum neurotoxin A: antigenic structure of the entire toxin. Immunobiology. 2011;216:698–706. doi: 10.1016/j.imbio.2010.10.010. [DOI] [PubMed] [Google Scholar]
- Dux MP, Huang J, Barent R, Inan M, Swanson ST, Sinha J, Ross JT, Smith LA, Smith TJ, Henderson I, Meagher MM. Purification of a recombinant heavy chain fragment C vaccine candidate against botulinum serotype C neurotoxin [rBoNTC(H(c))] expressed in Pichia pastoris. Protein Expr Purif. 2011;75:177–185. doi: 10.1016/j.pep.2010.09.016. [DOI] [PubMed] [Google Scholar]
- East AK, Richardson PT, Allaway D, Collins MD, Roberts TA, Thompson DE. Sequence of the gene encoding type F neurotoxin of Clostridium botulinum. FEMS Microbiol Lett. 1992;75:225–230. doi: 10.1016/0378-1097(92)90408-g. [DOI] [PubMed] [Google Scholar]
- Hauser D, Eklund MW, Kurazono H, Binz T, Niemann H, Gill DM, Boquet P, Popoff MR. Nucleotide sequence of Clostridium botulinum C1 neurotoxin. Nucleic Acids Res. 1990;18:4924. doi: 10.1093/nar/18.16.4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalb SR, Baudis J, Rees JC, Smith TJ, Smith LA, Helma CH, Hill K, Kull S, Kirchner S, Dorner MB, Dorner BG, Pirkle JL, Barr JR. De novo subtype and strain identification of botulinum neurotoxin type B through toxin proteomics. Anal Bioanal Chem. 2012;403:215–226. doi: 10.1007/s00216-012-5767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy R, Forsyth CM, LaPorte SL, Geren IN, Smith LA, Marks JD. Fine and domain-level epitope mapping of botulinum neurotoxin type A neutralizing antibodies by yeast surface display. J Mol Biol. 2007;365:196–210. doi: 10.1016/j.jmb.2006.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks JD. Deciphering antibody properties that lead to potent botulinum neurotoxin neutralization. Mov Disord. 2004;19(Suppl 8):S101–108. doi: 10.1002/mds.20023. [DOI] [PubMed] [Google Scholar]
- Mullaney BP, Pallavicini MG, Marks JD. Epitope mapping of neutralizing botulinum neurotoxin A antibodies by phage display. Infect Immun. 2001;69:6511–6514. doi: 10.1128/IAI.69.10.6511-6514.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowski A, Wang C, Powers DB, Amersdorfer P, Smith TJ, Montgomery VA, Sheridan R, Blake R, Smith LA, Marks JD. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc Natl Acad Sci U S A. 2002;99:11346–11350. doi: 10.1073/pnas.172229899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshima M, Middlebrook JL, Atassi MZ. Antibodies and T cells against synthetic peptides of the C-terminal domain (Hc) of botulinum neurotoxin type A and their cross-reaction with Hc. Immunol Lett. 1998;60:7–12. doi: 10.1016/s0165-2478(97)00124-7. [DOI] [PubMed] [Google Scholar]
- Pless DD, Torres ER, Reinke EK, Bavari S. High-affinity, protective antibodies to the binding domain of botulinum neurotoxin type A. Infect Immun. 2001;69:570–574. doi: 10.1128/IAI.69.1.570-574.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulet S, Hauser D, Quanz M, Niemann H, Popoff MR. Sequences of the botulinal neurotoxin E derived from Clostridium botulinum type E (strain Beluga) and Clostridium butyricum (strains ATCC 43181 and ATCC 43755) Biochem Biophys Res Commun. 1992;183:107–113. doi: 10.1016/0006-291x(92)91615-w. [DOI] [PubMed] [Google Scholar]
- Rosenberg JS, Middlebrook JL, Atassi MZ. Localization of the regions on the C-terminal domain of the heavy chain of botulinum A recognized by T lymphocytes and by antibodies after immunization of mice with pentavalent toxoid. Immunol Invest. 1997;26:491–504. doi: 10.3109/08820139709022704. [DOI] [PubMed] [Google Scholar]
- Schantz EJ, Johnson EA. Properties and use of botulinum toxin and other microbial neurotoxins in medicine. Microbiol Rev. 1992;56:80–99. doi: 10.1128/mr.56.1.80-99.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavo G, Benfenati F, Poulain B, Rossetto O, Polverino de Laureto P, DasGupta BR, Montecucco C. Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin. Nature. 1992a;359:832–835. doi: 10.1038/359832a0. [DOI] [PubMed] [Google Scholar]
- Schiavo G, Rossetto O, Benfenati F, Poulain B, Montecucco C. Tetanus and botulinum neurotoxins are zinc proteases specific for components of the neuroexocytosis apparatus. Ann N Y Acad Sci. 1994;710:65–75. doi: 10.1111/j.1749-6632.1994.tb26614.x. [DOI] [PubMed] [Google Scholar]
- Schiavo G, Rossetto O, Santucci A, DasGupta BR, Montecucco C. Botulinum neurotoxins are zinc proteins. J Biol Chem. 1992b;267:23479–23483. [PubMed] [Google Scholar]
- Schiavo G, Santucci A, Dasgupta BR, Mehta PP, Jontes J, Benfenati F, Wilson MC, Montecucco C. Botulinum neurotoxins serotypes A and E cleave SNAP-25 at distinct COOH-terminal peptide bonds. FEBS Lett. 1993a;335:99–103. doi: 10.1016/0014-5793(93)80448-4. [DOI] [PubMed] [Google Scholar]
- Schiavo G, Shone CC, Rossetto O, Alexander FC, Montecucco C. Botulinum neurotoxin serotype F is a zinc endopeptidase specific for VAMP/synaptobrevin. J Biol Chem. 1993b;268:11516–11519. [PubMed] [Google Scholar]
- Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology. 1980;87:1044–1049. doi: 10.1016/s0161-6420(80)35127-0. [DOI] [PubMed] [Google Scholar]
- Scott AB, Kennedy RA, Stubbs HA. Botulinum A toxin injection as a treatment for blepharospasm. Arch Ophthalmol. 1985;103:347–350. doi: 10.1001/archopht.1985.01050030043017. [DOI] [PubMed] [Google Scholar]
- Smith LA, Rusnak JM. Botulinum neurotoxin vaccines: past, present, and future. Crit Rev Immunol. 2007;27:303–318. doi: 10.1615/critrevimmunol.v27.i4.20. [DOI] [PubMed] [Google Scholar]
- Smith TJ, Hill K, Foley BT, Detter JC, Munk AC, Bruce DC, Doggett NA, Smith LA, Marks JD, Xie G, Brettin TS. Analysis of the Neurotoxin Complex Genes in Clostridium botulinum A1–A4 and B1 Strains: BoNT/A3, /Ba4 and /B1 Clusters are Located within Plasmids. PlLoS ONE. 2007;2:e1271. doi: 10.1371/journal.pone.0001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studier FW, Moffatt BA. Use of bacteriophage T7 RNA polymerase to direct selective high-level expression of cloned genes. J Mol Biol. 1986;189:113–130. doi: 10.1016/0022-2836(86)90385-2. [DOI] [PubMed] [Google Scholar]
- Thompson DE, Hutson RA, East AK, Allaway D, Collins MD, Richardson PT. Nucleotide sequence of the gene coding for Clostridium barati type F neurotoxin: comparison with other clostridial neurotoxins. FEMS Microbiol Lett. 1993;108:175–182. doi: 10.1111/j.1574-6968.1993.tb06095.x. [DOI] [PubMed] [Google Scholar]
- Wu HC, Yeh CT, Huang YL, Tarn LJ, Lung CC. Characterization of neutralizing antibodies and identification of neutralizing epitope mimics on the Clostridium botulinum neurotoxin type A. Appl Environ Microbiol. 2001;67:3201–3207. doi: 10.1128/AEM.67.7.3201-3207.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang GH, Kim KS, Kim HW, Jeong ST, Huh GH, Kim JC, Jung HH. Isolation and characterization of a neutralizing antibody specific to internalization domain of Clostridium botulinum neurotoxin type B. Toxicon. 2004;44:19–25. doi: 10.1016/j.toxicon.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Yu YZ, Li N, Zhu HQ, Wang RL, Du Y, Wang S, Yu WY, Sun ZW. The recombinant Hc subunit of Clostridium botulinum neurotoxin serotype A is an effective botulism vaccine candidate. Vaccine. 2009;27:2816–2822. doi: 10.1016/j.vaccine.2009.02.091. [DOI] [PubMed] [Google Scholar]