Abstract
Objective
To evaluate the diagnostic performance of chest x-ray (CXR) compared to computed tomography (CT) for detection of pulmonary opacities in adult emergency department (ED) patients.
Methods
We conducted an observational cross sectional study of adult patients presenting to 12 EDs in the United States from July 1, 2003 through November 30, 2006 who underwent both CXR and chest CT for routine clinical care. CXRs and CT scans performed on the same patient were matched. CXRs and CT scans were interpreted by attending radiologists and classified as containing pulmonary opacities if the final radiologist report noted opacity, infiltrate, consolidation, pneumonia, or bronchopneumonia. Using CT as a criterion standard, the diagnostic test characteristics of CXR to detect pulmonary opacities were calculated.
Results
The study cohort included 3,423 patients. Shortness of breath, chest pain and cough were the most common complaints, with 96.1% of subjects reporting at least one of these symptoms. Pulmonary opacities were visualized on 309 (9.0%) CXRs and 191 (5.6 %) CT scans. CXR test characteristics for detection of pulmonary opacities included: sensitivity 43.5% (95% CI: 36.4%–50.8%); specificity 93.0% (95% CI: 92.1%–93.9%); positive predictive value 26.9% (95% CI: 22.1%–32.2%); and negative predictive value 96.5% (95% CI: 95.8%–97.1%).
Conclusion
In this multicenter cohort of adult ED patients with acute cardiopulmonary symptoms, CXR demonstrated poor sensitivity and positive predictive value for detecting pulmonary opacities. Reliance on CXR to identify pneumonia may lead to significant rates of misdiagnosis.
Keywords: chest x-ray, computed tomography, pneumonia, emergency department, diagnostic testing
1. Introduction
A chest x-ray (CXR) is completed during approximately 18.5% of all emergency department (ED) visits in the United States (US), with an estimated 20.4 million ED CXRs performed annually.1 When evaluating patients with chest symptoms, such as shortness of breath, chest pain and cough, emergency clinicians must decide if CXR findings are consistent with pneumonia. Failure to promptly recognize and treat bacterial pneumonia may lead to significant morbidity and mortality.2, 3 Meanwhile, inappropriate use of antibiotics for respiratory symptoms not caused by bacterial infection is likely a major contributor to the development of antibiotic resistance.4–6 Furthermore, attributing a patient’s symptoms to pneumonia based on CXR results when, in fact, pneumonia is not present may lead to diagnostic anchoring and failure to recognize the patient’s true illness.7
Pulmonary opacitiesareas of increased attenuation visualized within the lung fields on chest imaging,8–9 are commonly used as criteria to support a diagnosis of pneumonia.3, 10 Despite CXR being used as the primary radiographic test to evaluate for pneumonia, the test characteristics of CXR for detecting pneumonia are not well understood. Computed tomography (CT) is a more precise technique for imaging the chest, but has not supplanted CXR as the primary imaging test for pneumonia due to increased time, cost, and radiation exposure associated with CT.11–13 However, comparing CXR to CT offers an opportunity to evaluate the accuracy of CXR for demonstrating radiographic findings consistent with pneumonia and to help inform clinicians how to use CXR results when considering a diagnosis of pneumonia. The purpose of this study was to evaluate the diagnostic test characteristics of CXR for detection of pulmonary opacities compared to a chest CT criterion standard in adult ED patients.
2. Methods
We conducted an observational, multicenter, cross-sectional study of adult ED patients who underwent both a CXR and chest CT as part of their evaluation. The diagnostic test characteristics of CXR for detection of pulmonary opacities were calculated using a concurrent chest CT as a criterion standard. The Institutional Review Board at all participating sites approved this study.
2.1 Patients
The study consisted of a secondary analysis of a prospective cohort recruited in 12 US EDs from July 1, 2003 through November 30, 2006. The cohort was initially recruited to study the diagnostic evaluation of pulmonary embolism (PE) and has been previously described.14, 15 Briefly, patients presenting to a study ED with acute symptoms were enrolled if a treating clinician ordered a diagnostic test for PE, including a chest CT, D-dimer assay, or ventilation/perfusion scan. Subjects were managed by emergency clinicians independent of the study protocol. Enrolled subjects underwent a structured interview and medical records review to obtain demographic and clinical data. For the current study, we included subjects who underwent both a CXR and chest CT as part of their ED evaluation.
2.2 Radiographic studies
All CXRs and chest CT scans were ordered by treating clinicians and interpreted by attending radiologists as part of routine clinical care. For each subject, the first CXR completed during his/her ED visit was matched to the first chest CT scan. Both single view (anterior-posterior) and two-view (posterior-anterior/lateral) CXRs were included. All CT scans included intravenous administration of iodinated contrast. Radiologists interpreted these studies as routine CXRs and CT scans completed at their institutions and were able to review the medical record and previous radiographic studies as part of standard clinical care. Radiologists entered their final interpretation for each CXR and CT scan into the medical record. Trained research assistants read the radiologist’s final interpretation and classified CXRs and CT scans as having a pulmonary opacity if the interpretation indicated the presence of any of the following: pulmonary opacity, pulmonary infiltrate, pulmonary consolidation, pneumonia, or bronchopneumonia.
2.3 Statistical Analysis
Descriptive statistics were used to summarize demographic and clinical characteristics of the study population. Using CT scan as a criterion standard, we calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and corresponding binomial 95% confidence intervals (CIs) of CXR for detection of pulmonary opacities. Additionally, Cohen’s kappa and standard error were calculated to describe the level of agreement between CXR and CT scan for detection of opacities. Statistical analyses were performed with Stata 11.1 (Stata Corp, College Station, TX).
3. Results
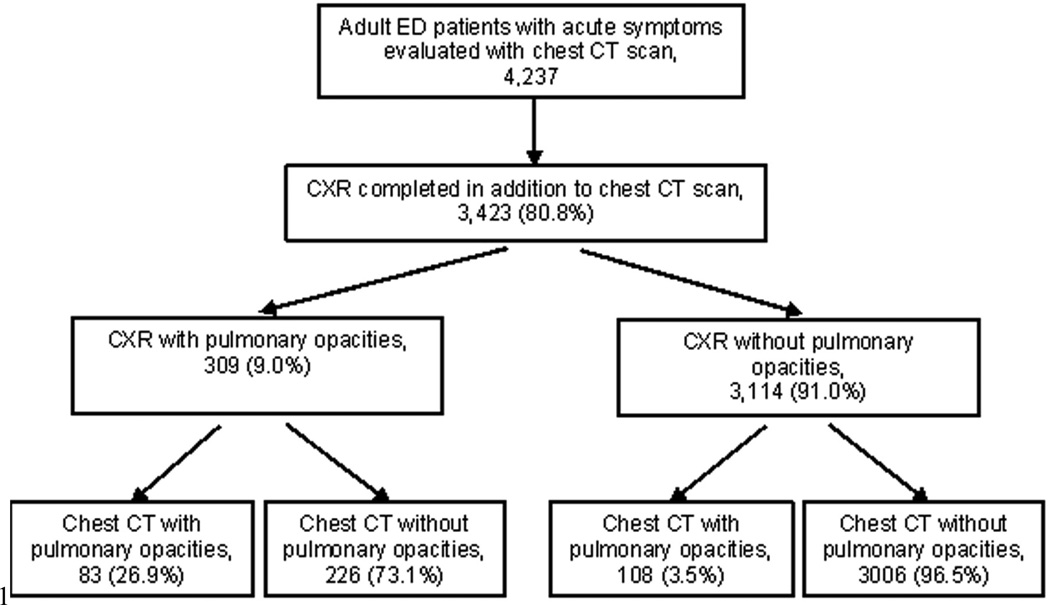
During the study period, 4,237 subjects underwent a chest CT scan; 3,423 (80.8%) of these subjects also had a CXR completed and were included in the final analyses (Fig 1). Demographic and clinical characteristics of these subjects are summarized in Table 1. Shortness of breath, chest pain and cough were the most common presenting complaints, with 96.1% of subjects reporting at least one of these symptoms.
Figure 1.
Flow diagram of patient enrollment and classification according to chest x-ray (CXR) and chest computed tomography (CT) findings. ED: emergency department; CT: computed tomography; CXR: chest x-ray.
Table 1.
Demographic and clinical characteristics of study participants.
| Characteristic | Subjects with pulmonary opacities on CT scan (n = 191) |
Subjects without pulmonary opacities on CT scan (n = 3232) |
|---|---|---|
| Demographics | ||
| Median age, years (IQR) | 54 (41 – 66) | 52 (39–65) |
| Females, no (%) | 112 (58.6%) | 2172 (67.2%) |
| Race | ||
| White, no (%) | 116 (60.7%) | 1894 (58.6%) |
| Black, percent (%) | 59 (30.9%) | 1100 (34.0%) |
| Other, percent (%) | 16 (8.4%) | 238 (7.4%) |
| Chronic medical conditions | ||
| Coronary artery disease, no (%) | 25 (13.1%) | 390 (12.1%) |
| Heart Failure, no (%) | 21 (11.0%) | 279 (8.6%) |
| Hypertension, no (%) | 72 (37.7%) | 1330 (41.2%) |
| Asthma, no (%) | 30 (15.7%) | 384 (11.9%) |
| COPD, no (%) | 32 (16.8%) | 289 (8.9%) |
| Diabetes mellitus, no (%) | 32 (16.8%) | 459 (14.2%) |
| Renal disease on dialysis, no (%) | 7 (3.7%) | 48 (1.5%) |
| Prior stroke, no (%) | 11 (5.8%) | 142 (4.4%) |
| Active malignancy, no (%) | 13 (6.8%) | 295 (9.1%) |
| Current smoker, no (%) | 51 (26.7%) | 680 (21.0%) |
| BMI > 30, no (%) | 62 (32.5%) | 1182 (36.6%) |
| Symptoms | ||
| Shortness of breath, no (%) | 155 (81.2%) | 2437 (75.4%) |
| Chest pain, no (%) | 118 (61.8%) | 2255 (69.8%) |
| Cough, no (%) | 106 (55.5%) | 1053 (32.6%) |
| Vital sign abnormalities* | ||
| Temperature > 100.4°F, no (%) | 21 (11.0%) | 152 (4.7%) |
| Heart Rate > 100 / min, no (%) | 101 (52.9%) | 1137 (35.2%) |
| Oxygen saturation < 95%, no (%) | 86 (45.0%) | 809 (25.0%) |
| Respiratory rate > 24/min, no (%) | 77 (40.3%) | 817 (25.3%) |
| Disposition from ED | ||
| Discharge, no (%) | 58 (30.4%) | 1276 (39.5%) |
| Admit obs or general ward, no (%) | 120 (62.8%) | 1839 (56.9%) |
| Admit ICU, no (%) | 11 (5.8%) | 93 (2.9%) |
Vital sign abnormalities represent the most extreme values recorded during a subject’s emergency department course.
IQR: interquartile range; no: number; COPD: chronic obstructive pulmonary disease; BMI: body mass index; ED: emergency department; obs: observation; ICU: intensive care unit.
Pulmonary opacities were visualized on 309 (9.0%) CXRs and 191 (5.6 %) CT scans. The diagnostic test characteristics of CXR for detection of pulmonary opacities using CT as a criterion standard are displayed in Table 2. In this population with a 5.6% prevalence of opacities on CT, the PPV of CXR—the probability of opacities visualized on CXR also being seen on CT—was only 26.9% (95% CI: 22.1% – 32.2%). The sensitivity of CXR—the probability of opacities detected on CT also being seen on CXR—was 43.5% (95% CI: 36.4% – 50.8%) Overall, agreement between CXR and CT was 90.2% (95% CI: 89.2 – 91.2%), with 6.6% (95% CI: 5.8–7.5%) of all patients having an opacity noted on CXR but not CT, and 3.2% (95% CI: 2.6–3.8%) of all patients having an opacity detected on CT but not CXR. Cohen’s kappa comparing CXR and CT for detection of pulmonary opacities was 0.28 (standard error: 0.017).
Table 2.
Test characteristics of chest x-ray (CXR) for detection of pulmonary opacities compared to a chest computed tomography (CT) criterion standard among 3,423 symptomatic adult emergency department patients.
| Point estimate (%) | 95% CI (%) | |
|---|---|---|
| Prevalence of pulmonary opacities on CT | 5.6 | 4.8 – 6.4 |
| CXR sensitivity | 43.5 | 36.4 – 50.8 |
| CXR specificity | 93.0 | 92.1 – 93.9 |
| CXR positive predictive value | 26.9 | 22.1 – 32.2 |
| CXR negative predictive value | 96.5 | 95.8 – 97.1 |
CI: confidence interval; CT: computed tomography; CXR: chest x-ray.
4. Discussion
From the standpoint of maximizing diagnostic accuracy, an optimal strategy for diagnosing pneumonia would involve culturing specimens obtained from the lower respiratory tract. However, due to the invasive nature of collecting these specimens and the time lapse needed for cultures to grow, this strategy is not practical. Therefore, the standard for diagnosing pneumonia that has developed over the past several decades involves recognition of a syndrome of clinical, laboratory and radiographic features compatible with pulmonary infection.3, 10
Currently, CXR is the standard radiographic test used to evaluate for pneumonia.3 CT is a more precise technique for imaging the chest, but is not routinely used to evaluate for pneumonia due to greater cost, increased time required to obtain images, and higher radiation exposure.11–13 The goal of this investigation was to evaluate the accuracy of CXR compared to a concurrent CT for demonstrating pulmonary opacities in order to help clinicians interpret the significance of CXR findings when considering a diagnosis of pneumonia. We found substantial discordance with respect to detection of pulmonary opacities between CXR and chest CT as interpreted by radiologists viewing the studies for routine clinical care. Only 43.5% of patients with opacities on CT had opacities noted on CXR. Furthermore, CXR findings interpreted as pulmonary opacities were frequently not reproduced on concurrent CT; only 26.9% of patients with a CXR interpreted as having pulmonary opacities had opacities recognized on CT.
These findings suggest CXR results cannot independently rule-in or rule-out pneumonia. Patients with a presentation highly suspicious for bacterial pneumonia but without pulmonary opacities visualized on CXR may benefit from further diagnostic testing, close observation, or empiric antibiotic therapy to prevent patient harm from unrecognized pneumonia. Similarly, patients with nonspecific CXR opacities but without clinical features suggestive of pulmonary infection should not be reflexively diagnosed with pneumonia and treated with antibiotics. In this study of adult ED patients presenting with acute cardiopulmonary symptoms, 6.6% of patients had pulmonary opacities interpreted on CXR that were not reproduced on CT. Considering the 12.4 million ED visits annually in the US due to shortness of breath, chest pain or cough,16 an “opacity equals antibiotics” reflexive management strategy is likely to lead to frequent overuse of antibiotics and unnecessary pressure for the development of antibiotic resistance. Moreover, misattributing clinical signs and symptoms, such as hypoxia or chest pain, to pneumonia based solely on CXR appearance may result in failure to identify the true cause of these signs and symptoms.
Similar to our results, previous small studies in other populations have found CT to be more sensitive than CXR for radiographic findings of pneumonia. In a prospective study of 58 hospitalized, bedridden patients, Esayaget al17 found CXR to be 65% sensitive for findings of pneumonia compared to concurrent CT. Syrjala et al13 prospectively studied 47 patients with clinical features of respiratory infection and found radiographic evidence of pneumonia in 38% of patients on CXR compared to 55% on concurrent CT. Hayden and Wrenn18retrospectively reviewed 97 ED patients diagnosed with pneumonia who underwent both CXR and CT; 27% of these patients had opacities visualized on CT but not CXR. Heusselet al19 prospectively studied the use of CT to evaluate for pneumonia in 188 patients with neutropenic fever and a normal CXR; 60% of these patients had CT findings of pneumonia.
Higher sensitivity of CT compared to CXR is likely attributable to enhanced visualization of chest cavity regions not well imaged with CXR, such as the lung bases and lingula, as well as thin, three-dimensional CT images detecting opacities too small to appreciate on CXR.11, 13 The phenomenon of CXR findings interpreted as pulmonary opacities not being reproduced on concurrent CT has not been well characterized. Transient atelectasis, shallow inspiration or poor patient positioning during CXR imaging may contribute to CXRs falsely appearing to contain pulmonary opacities, but further study is needed to understand the prevalence and etiology of this phenomenon.
Due to the limitations of CXR for demonstrating signs of pulmonary infection, future research is needed to investigate alternative and supplemental strategies to diagnose pneumonia. Chest CT provides detailed radiographic images of the lungs and appears to have higher sensitivity and specificity compared to CXR for pulmonary changes caused by pneumonia. Although CT is not currently an appropriate test to routinely assess for pneumonia, the risk-to-benefit ratio may favor using CT to evaluate for pneumonia in selected clinical scenarios, such as in the management of critically ill patients or to delineate between alternative diagnoses that can produce similar abnormalities on CXR. Given the limitations of CXR and our current strategy to diagnose pneumonia in the ED, development of biomarkers and clinical decision rules has the potential to greatly improve diagnostic algorithms for pneumonia.
4.1. Limitations
The study was nested within a larger study investigating risk factors for pulmonary embolism. This nested design was chosen for practical considerations—the pulmonary embolism study cohort provided a large, multicenter sample of ED patients with acute cardiopulmonary symptoms who underwent both CXR and chest CT. Due to overlap in signs and symptoms of pneumonia and pulmonary embolism, we believe this was a relevant population to study for a preliminary comparison of CXR and CT for the detection of opacities. However, prevalence of opacities in this study was relatively low and the operating characteristics for CXR detection of opacities may be different in other populations with higher prevalence. We analyzed CXR and CT interpretations from radiologists working in real-world, clinical environments. This maximized applicability of study results to ED clinicians, but also introduced limitations from a study design perspective. Radiologists were not blinded to prior radiographic studies; when interpreting a CT scan, radiologists were able to review CXRs completed earlier in the patient’s ED course. This lack of blinding may have been a source of bias toward concordance between CXR and CT. Furthermore, each radiographic study was interpreted by only one radiologist, and the inter-rater reliability among different radiologists in the study was not measured.
5. Conclusion
In this multicenter cohort of adult ED patients with acute cardiopulmonary symptoms evaluated with both CXR and chest CT, 9.8% of patients had discordant findings on CXR and CT with respect to the presence of pulmonary opacities as interpreted by radiologists. Using chest CT as a criterion standard for pulmonary opacities, CXR demonstrated poor sensitivity and positive predictive value. Reliance on CXR to identify pneumonia may lead to significant rates of misdiagnosis. Further research is indicated to investigate alternative and supplemental strategies to diagnose pneumonia in the ED setting.
Acknowledgments
Support:
Supported by the National Institutes of Health (R41HL074415, R42HL074415, K23HL077404 and R01HL074384).
Supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars Program with resources and the use of facilities at VA Tennessee Valley Healthcare System, Nashville, TN.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2002 emergency department summary. Adv Data. 2004;340:1–34. [PubMed] [Google Scholar]
- 2.Garnacho-Montero J, García-Cabrera E, Diaz-Martín A, et al. Determinants of outcome in patients with bacteraemic pneumococcal pneumonia: Importance of early adequate treatment. Scand J Infect Dis. 2010;42:185–192. doi: 10.3109/00365540903418522. [DOI] [PubMed] [Google Scholar]
- 3.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen DK, McGeer A, De Azavedo JC, Low DE. The Canadian Bacterial Surveillance Network. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada. N Engl J Med. 1999;341:233–239. doi: 10.1056/NEJM199907223410403. [DOI] [PubMed] [Google Scholar]
- 5.Lipsitch M, Samore MH. Antimicrobial use and antimicrobial resistance: Apopulation perspective. Emerg Infect Dis. 2002;8:347–354. doi: 10.3201/eid0804.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214–219. [PubMed] [Google Scholar]
- 7.Sibinga EMS, Wu AW. Clinical mindfulness and patient safety. JAMA. 2010;304:2532–2533. doi: 10.1001/jama.2010.1817. [DOI] [PubMed] [Google Scholar]
- 8.Tuddenham WJ. Glossary of terms for thoracic radiology: recommendations of the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol. 1984;143:509–517. doi: 10.2214/ajr.143.3.509. [DOI] [PubMed] [Google Scholar]
- 9.Austin JH, Muller NL, Friedman PJ, et al. Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology. 1996;200:327–331. doi: 10.1148/radiology.200.2.8685321. [DOI] [PubMed] [Google Scholar]
- 10.Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440–1445. [PubMed] [Google Scholar]
- 11.Wheeler JH, Fishman EK. Computed tomography in the management of chest infections: current status. Clin Infect Dis. 1996;23:232–240. doi: 10.1093/clinids/23.2.232. [DOI] [PubMed] [Google Scholar]
- 12.Mayo JR, Aldrich J, Muller NL. Radiation exposure at Chest CT: A statement of the Fleischner Society. Radiology. 2003;228:15–21. doi: 10.1148/radiol.2281020874. [DOI] [PubMed] [Google Scholar]
- 13.Syrjala H, Broas M, Suramo I, et al. High resolution computed tomography for the diagnosis of community-acquired pneumonia. Clin Infect Dis. 1998;27:358–363. doi: 10.1086/514675. [DOI] [PubMed] [Google Scholar]
- 14.Courtney DM, Kline JA, Kabrhel C, et al. Clinical features from the history and physical examination that predict the presence or absence of pulmonary embolism in symptomatic emergency department patients: results of a prospective, multicenter study. Ann Emerg Med. 2010;55:307–315. doi: 10.1016/j.annemergmed.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of pulmonary embolism rule-out criteria. J ThrombHaemost. 2008;6:772–780. doi: 10.1111/j.1538-7836.2008.02944.x. [DOI] [PubMed] [Google Scholar]
- 16.Pitts SR, Niska RW, XU J, Burt CW. National Hospital Ambulatory Medical Care Survey; 2006 emergency department survey. Natl Health Stat Report. 2008;7:1–38. [PubMed] [Google Scholar]
- 17.Esayag Y, Nikitin I, Bar-Ziv J, et al. Diagnostic value of chest radiographs in bedridden patients suspected of having pneumonia. Am J Med. 2012;123:88.e1–88.e6. doi: 10.1016/j.amjmed.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Hayden GE, Wrenn KW. Chest radiograph vs computed tomography scan in the evaluation for pneumonia. J Emerg Med. 2009;36:266–270. doi: 10.1016/j.jemermed.2007.11.042. [DOI] [PubMed] [Google Scholar]
- 19.Heussel CP, Kauczor HU, Heussel GE, et al. Pneumonia in febrile neutropenic patients and in bone marrow and blood stem-cell transplant recipients: use of high-resolution computed tomography. J ClinOncol. 1999;17:796–805. doi: 10.1200/JCO.1999.17.3.796. [DOI] [PubMed] [Google Scholar]