Abstract
Background:
This study performed to assess the safety of cataract extraction with phacoemulsification and intraocular lens (IOL) implantation in patients with high axial length compared with patients with normal axial length.
Materials and Methods:
A total of 866 eyes were enrolled in this study; all subjects underwent phacoemulsification and IOL implantation for treatment of cataract. Seven hundred and nine eyes fell in the normal group with axial lengths ranging between 21 and 24.5 mm, and 157 eyes were considered myopic with axial length equal or greater than 26 mm. The two groups were compared regarding intraoperative surgical complications, such as vitreous loss, posterior capsular rupture, nucleolus drop, and undesirable implantation of IOL in the anterior chamber.
Results:
Age was a risk factor in both groups, with each year increase of age, the chance of incidence of intraoperative complications increased 1.04-folds (P = 0.03). And with 1 mm increase in axial length, the incidence of complications raised 1.22-folds (P = 0.007). There was no significant correlation between axial length and incidence of vitreous loss, although the incidence of posterior capsular rupture and nucleus fragment drops increased with increment in the axial length. Sex of the patients and side of the left or right eye were not found to be significant risk factors.
Conclusions:
As the results illustrate, in this survey, age and high axial length were statistically significant risk factors for incidence of intraoperative complications of cataract surgery with phacoemulsification technique. Anticipation of these complications and also preparation and prophylactic measures may decrease incidence of these complications.
Keywords: Age, axial length, cataract, myopia, phacoemulsification
INTRODUCTION
Cataract is the leading cause of blindness and low vision.[1–4] As the world population ages, cataract-induced visual dysfunction and blindness will be on the rise.[5] The expectations of cataract patients have risen with introduction of innovative tools and technical improvement in surgical methods. Most surgeries end with excellent results, and patients as well as the surgeon are intolerant of occasional complications. Surgical management of cataract in patients with high myopia is associated with special difficulties,[6,7] provision for the potential complications may improve the outcome.
Cataract surgery and implantation of an intraocular lens (IOL) is an especially efficient refractive procedure in high myopia. With adequate expertise and proper implantation of IOL with correct power patients will enjoy an improved vision. This is not achievable in the majority of patients by most of the other refractive modalities, such as glasses, contact lenses, and corneal refractive procedures. Some intraoperative complications may raze this benefit; it may be impossible or very difficult to implant a posterior chamber IOL into the bag in a problematic surgery. Implantation of IOL out of capsular bag will also produce additional potential for a problematic course. Erroneously implanted IOLs will not provide the anticipated result.
Introduction of Kelman phacoemulsification technique revolutionized cataract surgery.[8–11] Despite difficulty of learning, a new method and complexity of the procedure, having a small incision sutureless surgery using a foldable IOL, is fascinating enough to turn it into the prevailing technique of cataract extraction. Decreased surgically induced astigmatism, quicker postoperative recovery, reduced postoperative followup visits, and less inflammation after surgery are among the advantages of this technique.[12–16] However, there are some drawbacks for the procedure that dramatically change the outcome: Management of vitreous loss and dropped nucleus during phacoemulsification need a well-rehearsed plan.[17,18] Surgeon's experience, early recognition of potential complications, and optimal handling of events lead to better outcomes.[19,20]
In this work, we designed a comparative study to evaluate the intraoperative complications of phacoemulsification with intraocular lens implantation in eyes with high and normal axial length.
MATERIALS AND METHODS
In this study, a retrospective review was performed on 866 consecutive eyes that had undergone cataract surgery in a university hospital. We used patients’ records to collect data. Subjects had undergone biometry, including axial length measurement for intraocular lens calculation. Axial length measurement had been accomplished with the ultrasound contact biometry (Nidek Echoscan US-1800, Nidek Inc); the automatic phakic mode was used with ultrasound speed of 1532 m/s for the anterior chamber and vitreous and 1641 m/s for the lens. A Javal-style manual Keratometer (HAAG-STREIT, USA) was used to obtain corneal keratometry, and IOL powers were calculated by the SRK/T formula.
All subjects underwent cataract extraction using phacoemulsification method; a 3.2-mm clear corneal incision was made by means of disposable blades just anterior to the vascular arcades for entrance of the phaco tip. Routinely hydroxypropylmethylcellulose (HPMC) viscoelastic, Coatel, were used before a circular capsulorrhexis. The phacoemulsification surgery was finished with ventury-type Phacoemulsification machine (Bausch and Lomb Storz Phaco machine). Subsequently a foldable IOL was implanted with injector through the 3.2-mm incision. We generally did not use any sutures for wound closure.
Patients were divided into 2 groups according to their ocular axial length measured in preoperative biometry. The normal axial length group presumed to be patients with axial length ranged between 21 and 24.5 mm, and those that had axial length ≥26 mm were considered to be the myopic group. In this study, 709 eyes fell in the normal group and 157 eyes in the high axial length group. The 2 groups were compared regarding intraoperative surgical complications. The evaluated complications were vitreous loss, posterior capsular rupture, nucleolus drop, and displacement of IOL into the anterior chamber. In the case of tear in posterior capsule without vitreous prolapse “posterior capsular rupture” event was recorded, and for posterior capsular tear with vitreous prolapse in anterior chamber the event was named “vitreous loss.”
RESULTS
Mean axial length in the normal group was 22.95 ± 0.83 mm (mean ± standard deviation) and mean age was 68.45 ± 9.75 years. In the high axial length group mean axial length was 27.83 ±1.82 mm and mean age was 64.33 ± 9.35 years.
Eighteen cases in the normal axial group (2.5%) had posterior capsular rupture compared with 9 cases (5.7%) in the high axial length group. Sixteen cases (2.3%) in the normal group had vitreous loss versus 7 cases (4.5%) in the high axial length group.
In this study, 4 cases in the normal group (0.6%) had displacement of the intraocular lens into the anterior chamber after surgery (Iris-captured IOL, or displacement of at least 1 haptic to anterior chamber), versus 3 cases (1.9%) in the high axial length group. There were 2 (0.3%) nucleus drop cases in the normal group and we had no such complication in the high axial length group [Table 1].
Table 1.
Comparison between interaoperative complications of phacoemulcification cataract surgery in two groups with normal and high axial length

Age was a risk factor for incidence of intraoperative complications in either normal or high axial length groups. Every 1 year increase in the age of patients increased incidence of intraoperative complications by 1.04-folds (P = 0.03). Figure 1 demonstrates the rate of intraoperative complications in different age groups.
Figure 1.
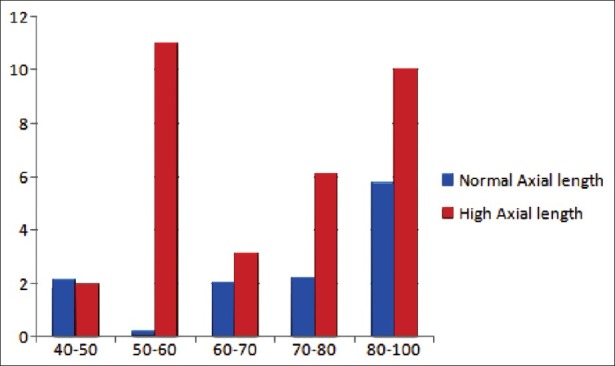
Intraoperative complication rate (%) in different age groups
Another risk factor for overall intraoperative complications in our study was the axial length itself. With 1 mm increase in axial length the incidence of intraoperative complications raised 1.22-folds (P = 0.007) [Figure 2].
Figure 2.

Posterior capsular tear (%) with different axial lengths
CONCLUSION
There was no significant correlation between axial length and incidence of vitreous loss, although incidence of posterior capsular rupture and nucleus fragment drops increased with increment in axial length. Sex of the patients and side of the left or right eye were not significant risk factors.
DISCUSSION
According to the results, the treatment of cataract in high-myopic patients using the phacoemulsification technique is safe in most patients, although there are additional difficulties in the management of the surgery to a safe endpoint due to special conditions of ocular response during the surgical process in high axial length eyes.
As illustrated, in this survey, we found 2 significant risk factors contributing to the intraoperative complications. Age of the patient significantly correlated to the occurrence of complications during phacoemulsification in normal or high-myopic eyes. Higher axial length of the eye is another predicting factor for intraoperative complications of cataract surgery with phacoemulsification technique.
We speculate that age-related changes in vitreous structure may be responsible for more motility of posterior capsule during phacoemulsification surgery that puts older patients in danger of capsular rupture. Higher axial length also alters the physical properties of vitreous body, and enhanced movement of capsule.
In conclusion, provisional measures should be taken more seriously in the patients with risk factors for complications in the cataract surgery, that is, patients with older age and higher axial length. Providing further preparation and prophylactic measures may decrease the rate of complications.
CONCLUSION
In conclusion, provisional measures should be taken more seriously in the patients with risk factors for complications in the cataract surgery, that is, patients with older age and higher axial length. Providing further preparation and prophylactic measures may decrease the rate of complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Abraham AG, Condon NG, West Gower E. The new epidemiology of cataract. Ophthalmol Clin North Am. 2006;19:415–25. doi: 10.1016/j.ohc.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Maberley DA, Hollands H, Chuo J, Tam G, Konkal J, Roesch M, et al. The prevalence of low vision and blindness in Canada. Eye. 2006;20:341–6. doi: 10.1038/sj.eye.6701879. [DOI] [PubMed] [Google Scholar]
- 3.Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290:2057–60. doi: 10.1001/jama.290.15.2057. [DOI] [PubMed] [Google Scholar]
- 4.Javitt JC, Wang F, West SK. Blindness due to cataract: Epidemiology and prevention. Annu Rev Public Health. 1996;17:159–77. doi: 10.1146/annurev.pu.17.050196.001111. [DOI] [PubMed] [Google Scholar]
- 5.Brian G, Taylor H. Cataract blindness-challenges for the 21st century. Bull World Health Organ. 2001;79:249–56. [PMC free article] [PubMed] [Google Scholar]
- 6.Iusef IuN, Iusef Siu, Reznikova EV, Vvedenskiĭ AS. Cataract surgery in patients with high myopia. Vestn Oftalmol. 2005;121:47–9. [PubMed] [Google Scholar]
- 7.Seward H, Packard R, Allen D. Management of cataract surgery in a high myope. Br J Ophthalmol. 2001;85:1372–8. doi: 10.1136/bjo.85.11.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelman CD. Symposium: Phacoemulsification. History of emulsification and aspiration of senile cataracts. Trans Am Acad Ophthalmol Otolaryngol. 1974;78:OP5–13. [PubMed] [Google Scholar]
- 9.Kelman CD. Symposium: Phacoemulsification. Summary of personal experience. Trans Am Acad Ophthalmol Otolaryngol. 1974;78:35–8. [PubMed] [Google Scholar]
- 10.Cotlier E, Rose M. Cataract extraction by the intracapsular methods and by phacoemulsification: The results of surgeons in training. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976;81:163–82. [PubMed] [Google Scholar]
- 11.Girard LJ, Hawkins RS. Cataract extraction by ultrasonic aspiration vitrectomy by ultrasonic aspiration. Trans Am Acad Ophthalmol Otolaryngol. 1974;78:50–9. [PubMed] [Google Scholar]
- 12.Chee SP, Ti SE, Sivakumar M, Tan DT. Postoperative inflammation: Extracapsular cataract extraction versus phacoemulsification. J Cataract Refract Surg. 1999;25:1280–5. doi: 10.1016/s0886-3350(99)00161-3. [DOI] [PubMed] [Google Scholar]
- 13.Dowler JG, Hykin PG, Hamilton AM. Phacoemulsification versus extracapsular cataract extraction in patients with diabetes. Ophthalmology. 2000;107:457–62. doi: 10.1016/s0161-6420(99)00136-0. [DOI] [PubMed] [Google Scholar]
- 14.Katsimpris JM, Petropoulos IK, Apostolakis K, Feretis D. Comparing phacoemulsification and extracapsular cataract extraction in eyes with pseudoexfoliation syndrome, small pupil, and phacodonesis. Klin Monbl Augenheilkd. 2004;221:328–33. doi: 10.1055/s-2004-812863. [DOI] [PubMed] [Google Scholar]
- 15.Cheng JW, Wei RL, Li Y. Effect of phacoemulsification versus extracapsular extraction on visual acuity: A meta-analysis. Zhonghua Yan Ke Za Zhi. 2004;40:474–7. [PubMed] [Google Scholar]
- 16.Tous HM, Nevárez J. Comparison of outcomes following combined ECCE-trabeculectomy versus phacoemulsification-trabeculectomy. P R Health Sci J. 2006;25:319–23. [PubMed] [Google Scholar]
- 17.Arbisser LB, Charles S, Howcroft M, Werner L. Management of vitreous loss and dropped nucleus during cataract surgery. Ophthalmol Clin North Am. 2006;19:495–506. doi: 10.1016/j.ohc.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Dickinson PJ, Greven CM. Avoiding and managing the dislocated crystalline lens. Compr Ophthalmol Update. 2006;7:113–27. [PubMed] [Google Scholar]
- 19.Arbisser LB. Managing intraoperative complications in cataract surgery. Curr Opin Ophthalmol. 2004;15:33–9. doi: 10.1097/00055735-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kim IK, Miller JW. Management of dislocated lens material. Semin Ophthalmol. 2002;17:162–6. doi: 10.1076/soph.17.3.162.14779. [DOI] [PubMed] [Google Scholar]


