Case
Mrs. SC, 30-years old in her third pregnancy, had two previous pregnancies 7 and 2 years ago which ended in uncomplicated term vaginal deliveries. She was booked for antenatal care at about 13 weeks. The mother’s blood group was A Rhesus positive. She had triple test for trisomy 21 and neural tube defects at 16 weeks gestation and was found to be low risk for both. At 30 weeks gestation she reported reduced fetal movements. The Cardiotocography (CTG) (Fig. 1) showed diminished variability with a few shallow decelerations suggesting fetal hypoxia. Considering the suboptimal CTG an ultrasound scan was performed which showed significant ventriculomegaly (Fig. 2), pericardial effusion, ascites, splenomegaly and oligohydramnios. The couple was counselled regarding significant risk of handicap. Since the underlying cause was uncertain at that point, she had further investigations for hydrops including maternal serology for viral screening and fetal cordocentesis which subsequently confirmed maternal and fetal Cytomegalovirus (CMV) infection (Table 1). She did not want any active intervention. A couple of days later the mother reported no fetal movements and an ultrasound scan confirmed intrauterine fetal death. A stillborn female baby (Fig. 3) weighing 1,455 g was delivered 2 days later following induction of labour. In the post-mortem report, it was commented that the lung showed numerous enlarged cells with nuclear and cytoplasmic inclusions characteristic of active CMV infection. The macroscopic feature of hepatosplenomegaly was consistent with this finding and that no other internal anatomical abnormalities were found.
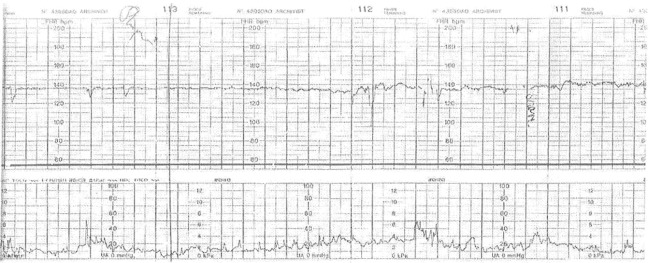
Fig. 1.
CTG showing reduced variability and intermittent shallow declarations signifying fetal hypoxia
Fig. 2.
Ultrasonography showing significant ventriculomegaly
Table 1.
Maternal and fetal serology confirming maternal and fetal CMV infection
| Maternal serolosv | Booking blood | 30 weeks |
|---|---|---|
| Cytomegalovirus IgG | Detected | Detected |
| Cytomegalovirus IgM | Detected | Not detected |
| CMV IgG avidity test | Low | Equivocal |
| Cordocentesis |
Cytomegalovirus IgM Detected
CMV infection in both mother and fetus confirmed
Fig. 3.

Shows still born female baby
Discussion
Cytomegalovirus (CMV) is the most common viral infection in pregnancy. 40–50 % of women are susceptible to the infection.
Primary infection occurs in 2 % of women during pregnancy [1]. 40 % of the babies are infected after a primary infection. 10 % of these will have symptoms at birth and another 10 % will develop long term sequelae (sensorineural deafness, mental retardation). This information helps in counselling.
Routine screening for CMV infection in pregnancy is not done as there is no established preventive vaccine or therapeutic antiviral agent avaiable [2]. Previous infection does not confer immunity but may modify the course of the disease and its consequences to the fetus [3].
Since CMV is a DNA virus and a member of the herpes virus family, they can establish latency. It can be excreted in the bodily fluids (e.g. saliva, urine) in adults after acute infections and children after congenital infections for a protracted period of time [4]. Hence women working in child care planning pregnancy should be counselled to wash their hands carefully after changing diapers and after any contact with children’s secretions (saliva etc.) [5].
Maternal infection is acquired by close contact, kissing and sexual intercourse. Clinical features are nonspecific and self-limiting and may include persistent fever, pharyngitis, cervical and generalised lymphadenopathy, fatigue, myalgia, headache, nausea and diarrhoea but may be minimally symptomatic or asymptomatic and therefore pass unnoticed.
Vertical transmission is mainly by haematogenous route by transplacental transfer but also by exposure to the virus from the cervix during birth and from breast milk after delivery [6].
Congenital CMV is a disseminated disease affecting the CNS (sensorineural deafness, hepatosplenomegaly, mental retardation, microcephaly, hydrocephalus, chorioretinitis, cerebral calcification), neonatal petechiae from thrombocytopenia, jaundice, pneumonia.
Severity of fetal affection is not influenced by the gestational age unlike rubella infection.
Maternal infection may be suspected if fetus shows soft markers e.g. echogenic bowel [7] and other signs of hydrops at routine anomaly scan at around 20 weeks or later. However majority of the CMV infections in pregnancy remain undiagnosed. Confirmation of maternal CMV infection is done by culturing the virus from body fluids or by PCR and serologically by demonstrating a rising IgG titre on paired sample from recent and stored booking bloods or raised CMV specific IgM titre in the recent blood.
The CMV IgG avidity test on paired sample (from stored booking and recent blood samples) helps to differentiate between a primary infection and a relapse. Low and equivocal result signifies primary infection whereas high avidity means past infection [8]. Expert microbiologist’s help should be taken in this respect as this information helps in counselling.
In the antenatal period whether the baby is infected or not is known either by amniocentesis after 20 weeks to culture the virus or by PCR or fetal blood sampling by cordocentesis which has the added advantage of estimating the fetal CMV antibody levels [9].
In cases where the baby is minimally affected, serial USS every 2 weeks for IUGR and any developing significant fetal abnormality e.g. hydrops, microcephaly, hydrocephalus, intracerebral calcification, hepatosplenomegaly should be done. Neonatologist should be involved in the antenatal period to counsel on the consequences on the baby. Detailed counselling helps the patients cope with their problems better.
Timing and mode of delivery will be influenced by gestational age, severity of the infection. Paediatrician should be present at the time of delivery.
In severely affected foetuses, termination of pregnancy should be considered in early gestations.
In future more studies are needed regarding CMV vaccines [10] for prevention and effective antiviral drugs for treatment.
References
- 1.Yow MD, Williamson DW, Leeds LJ, et al. Epidemiologic characteristics of cytomegalovirus infections in mothers and their infants. Am J Obst Gynaecol. 1988;158:1189–1195. doi: 10.1016/0002-9378(88)90252-9. [DOI] [PubMed] [Google Scholar]
- 2.Centres for Disease Control. Sexually transmitted Disease Treatment Guidelines. Mortality and morbidity weekly report. 1989;38(no S-8):39.
- 3.Kumar ML, Nankervis GA. Cytomegalovirus infections. South Med J. 1979;72(854–6):1. doi: 10.1097/00007611-197907000-00027. [DOI] [PubMed] [Google Scholar]
- 4.MacDonald H, Tobin JO. Congenital cytomegalovirus infection: a collaborative study on epidemiological, clinical and laboratory findings. Dev Med Child Neurol. 1978;20:471–482. doi: 10.1111/j.1469-8749.1978.tb15248.x. [DOI] [PubMed] [Google Scholar]
- 5.Alders SP. Cytome gal o virus and child day care. Evidence for an increased infection rate among day-care workers. N Eng J Med. 1989;321:1290–1296. doi: 10.1056/NEJM198911093211903. [DOI] [PubMed] [Google Scholar]
- 6.Stagno S, Reynolds DW, Pass RF, et al. Breast milk and the risk of Cytomegalovirus infection. N Eng J Med. 1980;302:1073–1076. doi: 10.1056/NEJM198005083021908. [DOI] [PubMed] [Google Scholar]
- 7.Peters MT, Lowe TW, Carpenter A, et al. Prenatal diagnosis of congenital cytomegalovirus infection with abnormal triple screen results and hyperechoic fetal bowel. Am J Obstet Gynecol. 1995;173:953–954. doi: 10.1016/0002-9378(95)90375-5. [DOI] [PubMed] [Google Scholar]
- 8.Bodeus M, Ranst M, Bernard P, et al. Anticytomegalovirus IgG avidity in pregnancy: a 2 year prospective study. Fetal Diagn Ther. 2002;17:362–366. doi: 10.1159/000065386. [DOI] [PubMed] [Google Scholar]
- 9.Azam AZ, Vial Y, Fawer CL, et al. Prenatal diagnosis of congenital cytomegalovirus infection. Obstet Gynecol. 2001;97:443–448. doi: 10.1016/S0029-7844(00)01140-6. [DOI] [PubMed] [Google Scholar]
- 10.Plotkin SA. Is there a formula for effective CMV vaccine? J Clin Virol. 2002;25:S13–S21. doi: 10.1016/S1386-6532(02)00093-8. [DOI] [PubMed] [Google Scholar]