Abstract
Lung cancer is the leading cause of cancer death in women, accompanied by greater psychological distress than other cancers. There is minimal but increasing awareness of the impact of lung cancer stigma (LCS) on patient outcomes. LCS is associated with increased symptom burden and decreased quality of life. The purpose of this study was to explore the experience of female long term lung cancer survivors in the context of LCS and examine how participants discursively adhere to or reject stigmatizing beliefs. Findings situated within Cataldo et al.’s theoretical model include: 1) addiction and tobacco marketing as possible precursors for LCS, 2) the possible role of expert providers as LCS enhancers, 3) response of overlapping complicated identity shifts, 4) simultaneous rejection and assumption of LCS, and 5) information control via advocacy activities as a LCS mitigation response. These findings expand the current understanding of LCS, and call for future conceptual exploration and theoretical revision, particularly with respect to the possibility of interaction between relevant related stigma(s) and LCS. As the number of women living with lung cancer increases, with longer survival times, the effect of LCS and other experiences of discrimination on patient outcomes could be substantial.
Keywords: oncology, marginalization, lung cancer, stigma, women’s health, patient outcomes, long-term lung cancer, survivors
Introduction
Lung cancer is the leading cause of cancer death in both men and women and is associated with greater levels of psychological distress than any other cancer (Zabora et al. 2001; Else-Quest et al. 2009; Lynch et al. 2010). There is a growing body of evidence that lung cancer stigma (LCS) is a co-occurring factor in the psychological and physical health of lung cancer patients (Chapple, Ziebland and McPherson 2004; Cataldo, Jahan and Pongquan 2012). Stigma in lung cancer is based on the belief that one caused their own cancer (i.e., by smoking). With the increase in the social unacceptability of smoking there has been a significant decrease in tobacco use with a subsequent experience of stigma by about half of all smokers (Stuber, Galea and Link 2009). Smoker stigmatization, although effective as an anti-smoking policy, seems to be transferred to patients with tobacco related diseases (e.g., lung cancer) and results in poor health outcomes.
This year, over 226,000 new cases of lung and bronchus cancer will be diagnosed in the U.S. (American Cancer Society 2012). Lung cancer is thought of as a disease of old men who smoked: two out of three newly diagnosed patients are older than 65, historically the prevalence has been greater for men, and currently 80 to 90% of all lung cancer cases are still smoking-related (American Cancer Society 2012). In January 2012, there were 223,150 female lung cancer survivors in the United States, and more women are currently living with lung cancer than men (American Cancer Society 2012). Because women as a population began smoking cigarettes later than men in the 20th century, lung cancer incidence in women has not yet begun to decrease (Siegel, Naishadham and Jemal 2012). For 2012, lung cancer is expected to account for 14% of new cases of cancer and will be the leading cause of cancer death in both men and women (Siegel et al. 2012). There is some evidence that women may be more susceptible to lung cancer than men (Henschke and Miettinen 2004), and some evidence to the contrary (Brennan, Hainaut and Boffetta 2011); this difference may be attributable to a greater proportion of andenocarcinoma (the most common type of non-small cell lung cancer) in women which has been linked with genetic susceptibility (Truong et al. 2010). Lung cancer prevalence for women is lower but the mortality rate is higher (Fogarty 2012). In 2007, in the U.S., lung cancer killed 70,354 women and more women die yearly from lung cancer than breast cancer and cervical cancer combined (U.S. Cancer Statistics Working Group 2012).
Overall survival in lung cancer remains low; however, changes in demographics and treatment have brought about an increase in long term lung cancer (LTLC) survivors. Population growth and aging are expected to contribute to the increase of LTLC survivors (Sugimura and Yang 2006), and a study examining cancer survival trends in a number of higher income countries found that relative survival improved from 1995-2007, increasing from a range of 6.9-16.6% for 5-year survival in the 1995-99 interval to 8.7-20.1% in the 2005-07 interval (Coleman et al. 2011). Decreasing death rates coupled with incidence stabilization translate to an expected increase in LTLC survivors (Siegel et al. 2012). Prognosis and mortality rates differ, dependent on exact diagnosis, disease stage, and gender. Based on data from 1975-2008, across all stages of lung cancer, an estimated 16 out of 100 patients live longer than 5 years (Howlader et al. 2011).
Treatment changes affect the longevity of female lung cancer patients (Fogarty 2012). Standard of care shifted in 2005 to include adjuvant chemotherapy after surgery when studies found survival increased by 15 percentage points (Winton et al. 2005). Currently, a variety of tumor inhibiting drugs are being used or tested with promising results, particularly for women (Malin et al. 2011; Fogarty 2012; Wakelee et al. 2012).
Lung cancer, in addition to being associated with the highest level of psychological distress for long term survivors (Zabora et al. 2001; Sugimura and Yang 2006; Else-Quest et al. 2009; Lynch et al. 2010), is also associated with diminished quality of life (QOL). These poor outcomes may be due in part to long-term exposure to LCS. Health issues for LTLC survivors include: sleep disturbance (Gooneratne et al. 2007); reduced QOL (Sarna et al. 2002); risk behaviors (i.e., smoking, second hand smoke, alcohol use)(Evangelista et al. 2003); inadequate physical activity (Clark et al. 2008); and overall symptom burden (Yang et al. 2012). The only qualitative analysis of LTLC experience reported that current distress results in more negative talk about related experiences (Maliski et al. 2003). The issues of central importance to survivors included: existential questions, health and self-care, physical ability, adjustment, and social support (Maliski et al. 2003). There are no studies with a focus on female LTLC survivors.
Research on LCS is limited. Chapple reported in 2004 that stigmatization had “far reaching consequences” for lung cancer patients (Chapple et al. 2004) and three studies reported a high prevalence of LCS and strong positive associations with depression, symptom burden, and diminished QOL (Gonzalez and Jacobsen 2010); Cataldo et al. 2011; Cataldo et al. 2012). As an instantiation of health related stigma, LCS is a significant barrier to effective patient/provider communication (Holland, Kelly and Weinberger 2010; Nelson et al. 2011). The increased stress and decreased provider support that accompanies LCS have very real costs. In addition, as a result of LCS, patients are less likely to be referred to oncologists from their general practitioners than other cancer patients (Wassenaar et al. 2007).
The purpose of this exploratory study was to begin to elucidate the experience of female LTLC survivors in the context of LCS, based on discourse analysis from one-on-one and group interviews. The secondary aim of this study was to begin to examine how women discursively adhere to or reject stigmatizing beliefs about their disease.
Theoretical Framework
Stigma, first defined by Goffman in relation to mental illness in the 1960s, addresses the “spoiled identity” of an individual as it is linked to attributes that are perceived negatively by society (Goffman 1974). Stigma can consist of experiences of discrimination (enacted stigma) (Van Brakel 2006), the anticipation or fear of discrimination (perceived or felt stigma), or the application of negative stereotypes to oneself (self-stigma) (Corrigan 1998).
Health-related stigma (HRS) is a specific type of stigma that includes a personal experience characterized by exclusion, rejection, blame, and/or devaluation related to a health problem or condition (Weiss and Ramakrishna 2006; Thornicroft et al. 2009). Higher levels of HRS are associated with depression (Cataldo et al. 2012), limited social support (Berger, Ferrans and Lashley 2001), and decreased treatment adherence (Fung, Tsang and Corrigan 2008). HRS ascribed to controllable factors (e.g., drug abuse) elicits a greater negative reaction than stigma ascribed to uncontrollable factors (e.g., genetics) (Weiner, Perry and Magnusson 1988; Lebel and Devins 2008).
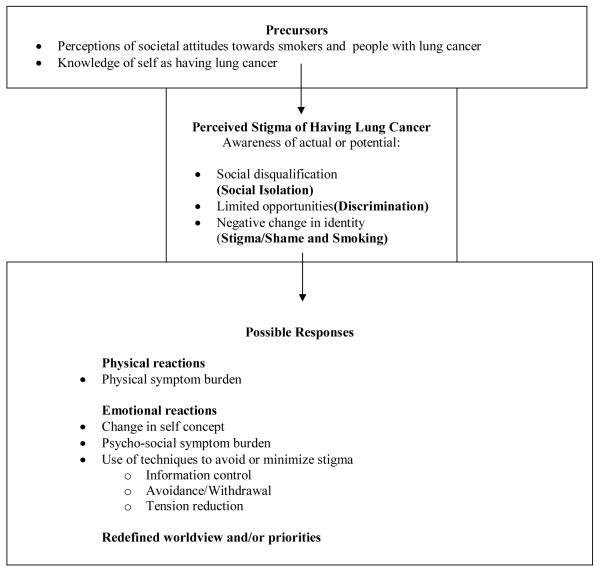
Lung cancer is often associated with smoking cigarettes, and because smoking is a proven cause of lung cancer, smoking is perceived to be a controllable factor (Weiner et al. 1988). In fact, lung cancer stigma has been conceptualized by some as a ’stacked stigma’ wherein co-occurring stigmas originate from a “primary stigma event” (Conlon et al. 2010). As a stacked stigma, it is proposed that LCS and smoking stigma feed and amplify one another, for a total stigmatized experience that is more detrimental than either stigma individually. Thus, the stacked stigma of lung cancer includes stigma related not just to smoking and lung cancer but to specific aspects of experience including cigarette use, nihilism, ageism, health disparities, and lack of advocacy support (Conlon et al. 2010). A model of LCS adapted to guide the development of the Cataldo Lung Cancer Stigma Scale (Cataldo et al. 2012) draws on the work of Goffman (1974) and previous AIDS/HIV stigma research (Berger et al. 2001). In this model, the perceived stigma of lung cancer occurs in the context of two factors: personal knowledge of having lung cancer and a perception of societal attitudes toward lung cancer. In this model, perceived stigma relates to awareness of social disqualification, limited opportunities, and negative change in societal identity (Figure 1). Stigma research has shown that perceived stigma can lead to several negative outcomes that include: increased levels of psycho-social symptoms (e.g. anxiety and depression), diminished QOL, and increased physical symptom occurrence, severity and distress (Cataldo et al. 2012).
Figure 1.
Model of Health Related Stigma in people with lung cancer (adapted from Cataldo et al. 2012)
Methods
Participants were recruited from Northern California lung cancer support groups to discuss LCS in one-on-one and group interviews. Each interview took 30 to 90 minutes and occurred between April and July, 2011. Total word count for transcriptions was 28,791. General interview structure included questions about: 1) diagnosis, 2) experience with health care providers since diagnosis, 3) experience of other peoples’ attitudes towards lung cancer, 4) changes in social network as a result of diagnosis, 5) experience with stigma, and 6) methods to cope with stigma.
Analytic Framework
The qualitative analytic framework for this study draws from Gee’s discourse analysis methodology (Gee 2011) and Fairclough’s Critical Discourse theory (Fairclough 2003), and integrates thematic analysis (i.e., examination of relevant text for themes), linguistic analysis (i.e., examination of language for recurrent linguistic patterns), discourse analysis and Critical Discourse Analysis (CDA).This framework was used to allow for a more open-ended inquiry into lung cancer stigma that originates from the viewpoint of women living with lung cancer. Previous nursing research has used similar analytic frameworks: an analysis of aging women’s stories examined how women are shaped and reshaped by discourse (Feldman 1999).
Gee asserts that people use language not just to communicate information, but to build real things (e.g., relationships, identities, expectations). Situations, histories and cultures are built via language. Accordingly, Gee presents seven building tasks of language, five of which were used to understand and analyze the discursive dynamics in this study’s transcripts: activities (i.e., what activities are enacted in the text?), identities (i.e., what identities are referenced, created or reinforced?), relationships (i.e., what relationship are created?), social norms (i.e., what is presented as right or normal in the discourse?), and connections (i.e., what things are connected in the text and what might be expected to be connected that is not?).
Discourse analysis situates the discourse in a local context and begins to establish how the discourse might be situated in broader societal power dynamics (Gee 2011). The explicit aims of CDA are to expose relations of power and control in discourse (van Dijk 1993). CDA is well suited to an analysis of LCS with the current theoretical model that includes information control as a possible response (Figure 1). A focus of CDA is to study complex social phenomena that requires a multi-disciplinary and multi-methodological approach (Wodak and Meyer 2009). In this study, particular attention was paid to unvoiced perspectives – those assumed, excluded or forgotten “voices” that impact the discourse even when they are not explicitly stated and that may interact with Cataldo et al.’s model by changing self concept or worldview. An eight-step integrated method of analysis that includes thematic, linguistic and discourse analysis as well as CDA of the data was used (Figure 2).
Figure 2.
Integrating discourse analysis and Critical Discourse Analysis methodology
Lastly, we assume a social constructionist epistemology, along the lines of Vygotsky’s Social Development Theory, which incorporates the role of community into experience for the creation of individual meaning and interpretation of experiences (Vygotsky 1978). We acknowledge that our findings are based on the “truth” as experienced and shared by participants in this study. This truth has been constructed in a social context, one that in the instance of these individuals seems to have been influenced by social interactions and perceptions laden with the shame, blame and discrimination of stigma.
Data
Eight female long term lung cancer survivors (estimated average number of years since diagnosis is 6.5), both ex-smokers and never smokers, participated in recorded interviews. Table 1 provides additional information about participants, as well as their pseudonyms.
Table 1.
Participant demographics
| Pseudonym | Smoking Status | Years Since Diagnosis |
Treatment |
|---|---|---|---|
| Andrea | Never smoker | unknown | unknown |
| Brooke | Never smoker | 7 years | unknown |
| Caroline | Ex-smoker, 38 years ago | 11 years | surgery |
| Danielle | Ex-smoker, 20 years ago | 7 years | surgery |
| Ella | Ex-smoker, 15 years ago | 2 years | surgery, radiation, chemo |
| Faith | Never smoker | unknown | surgery |
| Gabriella | Ex-smoker | 6 years | surgery, chemo |
| Hailey | Ex-smoker | 6 years | surgery, radiation, chemo |
Results
Unvoiced Precursors –Tobacco Industry and Addiction Influence
Though addiction and industry marketing are significant factors for smoking initiation and continuation and thus contribute to lung cancer and LCS, both were missing from this study’s discourse. Using CDA, we are able to connect text-external influences to the text, if only to comment that expected external influences such as two critical tobacco-related factors, addiction and the tobacco industry, were not emphasized.
There is substantial proof that smoking tobacco is addictive. Considering the impact of addiction on smokers, and by extension many lung cancer patients, it is notable that addiction only appeared once in the discussion: “Even though I had quit smoking, a number of years ago, it is still disturbing to me to be around smokers, because the addiction is so strong, and I still wouldn’t mind having one. In fact, I still have dreams where I smoke.” Similarly, references to the tobacco industry were few. Only one tangential reference to the tobacco industry surfaced, a reference to the “Marlboro man:”
Yeah, and it is very – people don’t come out and say it. It’s just a subtle attitude like, “You know you asked for it.” Or “You shouldn’t have smoked.” You know, I grew up in the days of the Marlboro man. It was hip to smoke when I was a teenager. We didn’t know the things we do know. Do I excuse myself? No. It was a stupid thing to do. I don’t know that I should be penalized for it now.
One participant eloquently outlined the links between smoking, lung cancer and LCS, notably excluding the issues of addiction and tobacco industry influence:
Yes I do believe there is stigma. I believe that the ninety percent of the world or could be the United States – 95% – believe that smoking always comes from – I mean, lung cancer always comes from smoking. Then there is an unspoken, inherent next thought which is, therefore it is your own fault.
Perception of LCS – Diagnosis and Interaction with Healthcare Providers
The women in this study experienced LCS in interactions with their health care providers, and they voiced awareness of the connections between smoking stigma and LCS. All participants reported experiences with providers that did not meet their expectations for interpersonal interactions or treatment-related care, to such a degree that the moderator reacted with surprise when Hailey replied that she’d had no negative provider experiences. However, when Hailey’s “positive” experience is more closely examined, it is revealed that out of all of her doctors, only her oncologist actually said the word cancer. By way of explanation for how all her providers could have had that much trouble communicating with her about her diagnosis, Hailey explains:
I think they – (laughs) well, you know if you have lung cancer you’re pretty much dead. It’s like how do you tell somebody they’re dying. My general practitioner is my age. She and I have kids the same age. We went through menopause together. We have the same experiences in our lives at the same time.
Experience with individual doctors was mixed; oncology doctors and staff, and particular providers and clinics were singled out as being positive support for these women. One participant differentiated between lab/hospital and oncology staff, pointing out that oncology staff did not make negative comments about smoking: “Oncology people I don’t hear that [negative comments] from. They are top notch people.” By negative contrast, negative and negated linguistic constructions (e.g., no, don’t, didn’t, not) focused the participants’ stories of diagnosis on negative experiences with clinicians. For example, one participant reported:
I thought I’d get referred to a cancer center, but I didn’t. I didn’t get to see an oncologist or anything. I kept getting referred back to the lung surgeon that I saw at the county hospital and I didn’t want him to do my surgery because he didn’t – he kind of treated me in a condescending manner. [bolding added for emphasis]
In addition to being characterized by negative phrases, patients invoked a modal phrase, the “epistemic must”, in stories about interactions with providers. The epistemic must construction is “must” plus be verb and expresses conviction or rightness. Andrea, a younger patient who had a hard time getting diagnosed, reports that her doctors would say, “Oh, your immune system must be messed up…” or “You must be allergic to the trees on campus” [bolding added for emphasis] when she reported that her frequent respiratory infections worried her. Andrea’s case was complicated by lapsed health insurance, but despite repeated bouts of pneumonia, she was only referred to an ear, nose and throat specialist who helped locate her tumor after “one morning [when] I coughed up a whole cup full of blood.”
Perception of Stigma – Shifting Identities
The identities discussed and taken on within this data are varied. The link between the physical disease (lung cancer) and identity is manifested in a wide variety of labels, both self-assumed and applied to patients by providers, family friends and acquaintances. Included in Table 2 is a typology of all discussed and created participant identities that might be influenced by or result from perceptions of stigma.
Table 2.
Participant identities
| Context | Identity |
|---|---|
| Within the medical establishment |
“Lung cancer patient”, “clinical trial candidate” |
| With respect to cigarette smoking |
“smoker”, “non-smoker”, “former smoker”, “never-smoker” |
| With respect to stigma | “victim”, “perpetrator” |
| Job/career assignments | “waitress” (this had been assumed of one participant), “employer,” “co-worker,” “associate”, “PhD in chemistry”, “retiree of the University of California” |
| Age | “older”, “of a different generation”, “67-year-old woman”, “60-year-old woman” |
| Familial/ group | wife (“my husband and I”), parent (“my son”), family-member (“my family”), friend (“my friends”), “spouse,” support group attendee |
| Empowerment-related | teacher/educator (“I try to educate now…”), “volunteer”, expert (on lung cancer – quoting statistics to uninformed people) |
| Disempowering | “honey” (address from a clinician) |
| Within the context of other lung cancer patients/victims |
“lucky”, “cancer-free”, “survivor,” “the face of lung cancer” |
In particular, the identities that surround smoking are extremely important to the interaction of stigma and lung cancer. Regardless of smoking status, lung cancer patients reported that they are largely assumed to be smokers. All participants agreed that the very first thing people said as a reaction to a lung cancer diagnosis was “have you ever smoked?”; “Always… without fail,” ratified Caroline. Ella concurred that “the first question always is, Did you smoke?” Participants also complain that their identity as lung cancer patients engenders less sympathy than other cancer patients. Even non-smokers experience this: “We’re actually the perpetrators because we smoked, even though we never did.”
Identity is also involved with lung cancer advocacy. In reference to the choice of recent advocacy efforts to build a new “face of lung cancer” around atypical patients (i.e., younger, non-smoker) (Bonnie J. Addario Lung Cancer Foundation 2009-2012), participants had strong reactions. Gabriella, who is closer to the average age and smoking status of patients generally, reported feeling left out and potentially even more stigmatized by this shift:
The Foundation is trying to capitalize on the fact, to the general public, that you don’t have to be an old smoker to get lung cancer. But, frankly, the rest of us survivors who were at the run/walk last year, felt a little belittled, because we are, too. That’s the fact. You know, as a sixty-year-old ex-smoker, I, too, am the face of lung cancer.
In this quote, Gabriella identified herself as “survivor,” “sixty-year-old ex-smoker” and “the face of lung cancer.”
Participants reiterated that it is the connection to smoking that creates LCS: “Everyone thinks that if you get lung cancer, you have it because you smoked and if you were that dumb you deserve to die… Everybody wants you to suffer” [bolding added for emphasis]. Smoking was stigmatized as something you do only “if you were that dumb.” The steps between smoking on one hand and “deserving to die” were highly negatively valenced (e.g., “if you were that dumb”). The negative connotative connection between smoking and lung cancer was a precursor to patients not being eligible for sympathy: “Everybody wants you to suffer.”
Responses to Stigma - Information Control, Advocacy
A young survivor (< 60 years old) reported isolation as her response to LCS: “What the cancer did to me economically? … killed my career, and so, I just became isolated from everybody… It’s frustrating that you know I can’t continue with the career that I loved.” This experience of loss due to lung cancer contrasts with other survivors like Danielle, who responded to illness and LCS by controlling information and redefining her worldview. Danielle’s response allowed her to characterize cancer as instrumental in creating positive effects such as helping to find “a mission in my life” to educate people and support other lung cancer patients.
By focusing on deictic terms – terms that change meaning depending upon who is saying them and in what context (e.g., pronouns such as I and we, and temporal terms such as now and later) – there is evidence that participants had a difficult time letting go of the need for a reason for their lung cancer. In the following phrase about looking for a reason for the disease, the externalized generalization “people” became the first person “we” later in the phrase, and thus shifted the need to look for a reason from others (people) to inclusive group (we). This indicates that this is the instinct not just for others, but for patients themselves: “People always look for some reason for something, you know? It’s just, if… there’s no explanation we can’t let it go that we don’t know, you know?” [bolding added for emphasis]. This need for explanation activates lung cancer stigma for participants, some of whom trace their actions to their disease. Danielle, for example, takes responsibility for her disease: “I’d done the damage…and someday I was going to have it [lung cancer].”
Conflicting Responses to Stigma - Simultaneous Rejection and Assumption of Stigma
Examining the way participants talk about their experiences from a CDA perspective, it is evident that at least some participants simultaneously reported rejecting stigma overtly while revealing through their choice of words an assumption of stereotypes. One conversation participant reported rejecting stigma by sharing her diagnosis, “I like to tell [people my diagnosis] to make them aware.” But her further comments demonstrated internalized LCS, “I think sharing is important to make people aware that normal people who weren’t smokers…do get lung cancer” [bolding added for emphasis]. In labeling non-smokers as “normal people” she implicitly labeled smokers abnormal.
Discussion
Although this is an exploratory study with a small sample size, this is the first study to focus on female LTLC survivors and LCS. This study adds to preliminary evidence in the extant literature that regardless of smoking status, lung cancer patients experience LCS from multiple origination points (Chapple et al. 2004): health care providers (Nelson et al. 2011), the public (Cataldo et al. 2012), and themselves (Else-Quest et al. 2009). The connection between smoking, lung cancer and personal responsibility is implicated in the foundation of LCS for patients, even if they never smoked. Other potential stigma-producing aspects interacted with lung cancer stigma but were not omnipresent, including age (both youth and older age), perceived social status (i.e., lack of health insurance), and a host of factors surrounding death including prognosis, fear of death and nihilism in the face of a lung cancer diagnosis. These factors warrant further exploration.
Precursors - Addiction and Tobacco Industry
Social norms about lung cancer revealed themselves in the discourse explicitly in some cases, but in many cases they were only apparent as underlying assumptions that informed the discourse through smoking stigma’s influence on LCS but remained unvoiced (i.e., addiction and tobacco industry influence). This connection between unvoiced elements and smoking could indicate one of two things: a clearer demarcation than is currently reported between smoking stigma and lung cancer stigma, or total assumption of the normal-ness of addiction and industry influence in the backdrop of LCS.
Perception - Provider/Patient Experience
This study adds to the literature that LCS interferes with an ideal patient/provider experience (Nelson et al. 2011). Furthermore, there is an open question as to whether clinicians play a role in the creation of LCS by shutting down open communication and dismissing patient knowledge of their disease experience, particularly for younger, female, or non-typical patients. Nelson et al. had found a deficit in physician communication to lung cancer patients about emotional symptoms, practical needs, spiritual concerns, living will preparation, life support preferences and hospice (Nelson et al. 2011).
Previous discursive studies of provider-patient communication have demonstrated that the poorest communication outcomes occur when patients’ accounts are ignored while doctors use the “voice of medicine,” (Barry et al. 2001). Mishler (1984) described the “voice of medicine” as technologically focused, and used in the service of maintaining control and power imbalance (Mishler 1984). In our current study, a perception of the “voice of medicine” is reflected in the participant stories of provider-patient interactions. One linguistic mechanism by which physicians may shut down conversation is the epistemic must, which, as reported by the participant Andrea, undervalues expertise of patients while increasing provider self-importance. However, to avoid a narrow interpretation on this point, it is worthwhile to revisit our social construction epistemology and recall that Andrea’s account of these interactions may be communicating not simply her verbatim interaction with providers, but her overall experience of them as dismissive due in part to preconceptions about her age (too young for lung cancer) or her socio-economic status (uninsured).
Imperfect patient-provider interaction is not the sole purview of lung cancer patients, but may in fact be an overarching artifact of the construction of medical expertise. Considering our guiding framework (Fig 1), however, this type of patient-provider interaction serves to strengthen and reinforce patient perceptions on all three key aspects of LCS: it disqualifies patient opinion, limits patient opportunities (e.g., to provide input, or for referral, etc.), and reinforces a negative (i.e., less knowledgeable) change in identity.
Perception - Identities
Participants in this study categorically reported others assuming that they were current or former smokers. The experience of stigma for smokers is not categorical (Stuber et al. 2009); however, in this context, the assumption of smoking status represents a negative change in identity for patients. The LTLC survivors in this study were not content being labeled as smokers and resisted by informing people that not all lung cancer patients were smokers and that there are many causes of lung cancer. Framing this within Cataldo et al.’s model, for these women, the identity of smoker coincided with a negative change in social identity compared to alternative non-smoking selves. Similarly, assumption of the identity of lung cancer patient coincided with a negative change in social identity compared to other cancer patients.
Echoing findings from qualitative research on lung cancer stigma conducted with oncology social workers, in their identities as “lung cancer patients,” participants experienced perceived LCS in the form of a lack of sympathy from others (Conlon et al. 2010). Some perceived that other similar patient groups (i.e., breast cancer patients) experienced support from the community in general and garnered interpersonal sympathy, while lung cancer patients did not.
The centrality of identity as smoker necessitates the addition of a smoking-specific precursor to the current theoretical model. Currently, knowledge of diagnosis in addition to perceptions and attitudes towards lung cancer constitute the sole precursors to perception of lung cancer stigma (Figure1). Given the change in attitudes towards smoking and smokers over the past fifty years, perhaps an expansion of this model should include a third precursor, perception of societal attitudes towards smokers and smoking cigarettes.
Responses – Self-stigma
This study suggests that women LTLC survivors have a complicated understanding of the cause of their disease, both rejecting and assuming beliefs that they are responsible. Participants co-created their LCS implicitly through linguistic choices (i.e., using words and structures that implicitly reinforced stigmatizing thoughts) even as they overtly expressed their rejection of stigma. This fluidity of locus for stigma, originating from strangers, friends, family, and providers, and in “friendly fire” situations like lung cancer support and research communities and self-stigma, seems to complicate the roles a patient may take. In essence, because stigma is at least reinforced by, if not emergent from, internalized beliefs about responsibility and what is “normal,” single relationships and individuals can enact more than one role simultaneously. Additionally, the model’s predicted possible response of “change in self concept” might arguably be expected to occur with complicated identity interactions, since it includes an identity or self concept in flux.
This preliminary evidence of simultaneous overlapping identities points to a layered and more dynamic model of LCS, where multiple pathways exist concurrently through precursors, perception and responses. The current model does not specifically delineate this possibility, but does not exclude a layered account of LCS. Participants were observed rejecting and creating LCS within the same utterance. One explanation for this close proximity of rejection and creation is that different precursors have simultaneously produced different and distinct pathways of perceived LCS through experience and responses.
Responding to Stigma – the Role of Advocacy
The women in this study built support networks based on both in-person and online support groups. These networks represent possible stigma minimizing responses to LCS through information control, avoidance/withdrawal, and tension reduction. One participant resisted LCS in the context of social media, using Facebook exclusively to raise awareness about lung cancer and LCS. Online patient support group participation has been demonstrated to increase empowerment for patients with breast cancer, fibromyalgia, arthritis and other diagnoses in a population that was skewed highly female (94%) (van Uden-Kraan et al. 2009). Online networking and advocacy show promise as methods to cope with LCS.
Additionally, there is preliminary evidence in this data that some women lung cancer patients have addressed their experience of stigma by becoming advocates and educators. Within other areas of health- and situation-related stigma, advocacy has been proposed as a tool to challenge and discredit stigma and shame. For example, Bergart (2004) suggests advocacy as the next step beyond the positive participation in support groups with her study of stigma and patients experiencing infertility or who have been victims of incest (Bergart 2004), and a review of the global literature on disability in higher education has shown that advocacy (along with agency and achievement) opens up the possibility for positive patient transformation (Morley and Croft 2011).
In at least one case, women in particular have successfully used advocacy as a tool to challenge and discredit stigma and shame. A cohort of highly stigmatized HIV positive African American women used a variety of strategies over two years to combat stigma, including sharing the diagnosis strategically, reframing stigma as ignorance, thus casting themselves simultaneously as experts, and becoming advocates (Buseh and Stevens 2007). Advocacy, then, seems to be a consistent possible response within the Cataldo et al. model and could either be construed as an instantiation of redefined worldview and priorities.
Future Research
This exploratory study suggests the need for further exploration of the context and experience of women who are LTLC survivors in relation to LCS and to examine how LCS affects women and their cancer experience, and conceptual expansion and further testing of the current LCS model. An expanded model could better accommodate diverse responses to stigma (i.e., concurrent stigmatized/non-stigmatized identity, and information control manifested through advocacy). Additionally, theoretical expansion would provide a framework by which to explore the emergent themes of perception of LCS in the receipt of the diagnosis and in interactions with health care providers, and shifting identities in the context of a sense of responsibility, both of which are in need of further exploration.
Conclusion
This study represents the beginning of an important focus for inquiry: female LTLC survivors and their experience of stigma. As their numbers increase, they stand to experience more prolonged exposure to LCS and thus LCS needs to be conceptualized and the relationships with health outcomes identified.
Given the increasing number of survivors, the extent of the impact of LCS on patient outcomes, the dearth of information on women survivors, and the important role of nursing in the care of lung cancer patients from prevention through remission and survivorship, the elucidation of women lung cancer patient experiences is essential for informed care and potential self-management focused interventions.
Acknowledgements
This research was supported in part by National Cancer Institute Grant CA-113710.
Contributor Information
Cati Brown, Research Fellow, Center for Tobacco Control Research and Education University of California San Francisco 530 Parnassus Avenue, Ste. 366 San Francisco, CA 94143 706-296-7767 cati.brown-johnson@ucsf.edu.
Janine Cataldo, 2 Koret Way, Room N611Q Box 0610 San Francisco, CA 94143 Phone Number: 415-476-4721 janine.cataldo@nursing.ucsf.edu.
References
- American Cancer Society [accessed 5 May 2012];Lung cancer (non-small cell) 2012 http://www.cancer.org/Cancer/LungCancer-Non-SmallCell/DetailedGuide/index.
- Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor-patient communication in general practice. Social Science & Medicine. 2001;53:487–505. doi: 10.1016/s0277-9536(00)00351-8. [DOI] [PubMed] [Google Scholar]
- Bergart AM. Group work as an antidote to the isolation of bearing an invisible stigma. Social Work with Groups. 2004;26:33–43. [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bonnie J. Addario Lung Cancer Foundation [accessed 11 Nov 2012];Anyone can get lung cancer - yes, anyone! 2009-2012 http://www.lungcancerfoundation.org/2010/04/07/this-is-the-face-of-lung-cancer/
- Brennan P, Hainaut P, Boffetta P. Genetics of lung-cancer susceptibility. Lancet Oncology. 2011;12:399–408. doi: 10.1016/S1470-2045(10)70126-1. [DOI] [PubMed] [Google Scholar]
- Buseh AG, Stevens PE. Constrained but not determined by stigma: Resistance by African American women living with HIV. Women & Health. 2007;44:1–18. doi: 10.1300/J013v44n03_01. [DOI] [PubMed] [Google Scholar]
- Cataldo JK, Jahan TM, Pongquan VL. Lung cancer stigma, depression, and quality of life among ever and never smokers. European Journal of Oncology Nursing. 2012;16:264–269. doi: 10.1016/j.ejon.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. British Medical Journal. 2004;328:1470–1473. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MM, Novotny PJ, Patten CA, Rausch SM, Garces YI, Jatoi A, Yang P. Motivational readiness for physical activity and quality of life in long-term lung cancer survivors. Lung Cancer. 2008;61:117–122. doi: 10.1016/j.lungcan.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman MP, Forman D, Bryant H, Butler J, Rachet B, Maringe C, Richards MA. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995-2007 (the international cancer benchmarking partnership): An analysis of population-based cancer registry data. Lancet. 2011;377:127–138. doi: 10.1016/S0140-6736(10)62231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlon A, Gilbert D, Jones B, Aldredge P. Stacked stigma: Oncology social workers’ perceptions of the lung cancer experience. Journal of Psychosocial Oncology. 2010;28:98–115. doi: 10.1080/07347330903438982. [DOI] [PubMed] [Google Scholar]
- Corrigan PW. The impact of stigma on severe mental illness. Cognitive and Behavioral Practice. 1998;5:201–222. [Google Scholar]
- Else-Quest NM, LoConte NK, Schiller JH, Hyde JS. Perceived stigma, self-blame, and adjustment among lung, breast and prostate cancer patients. Psychology & Health. 2009;24:949–964. doi: 10.1080/08870440802074664. [DOI] [PubMed] [Google Scholar]
- Evangelista LS, Sarna L, Brecht ML, Padilla G, Chen J. Health perceptions and risk behaviors of lung cancer survivors. Heart Lung. 2003;32:131–139. doi: 10.1067/mhl.2003.12. [DOI] [PubMed] [Google Scholar]
- Fairclough N. Analysing discourse : Textual analysis for social research. Routledge; London ; New York: 2003. [Google Scholar]
- Feldman S. Please don’t call me ’dear’: Older women’s narratives of health care. Nursing Inquiry. 1999;6:269–276. doi: 10.1046/j.1440-1800.1999.00041.x. [DOI] [PubMed] [Google Scholar]
- Fogarty M. [accessed 21 March 2012];The face of lung cancer changes, but new drugs show promise. Patient Care News. 2012 http://cancer.stanford.edu/features/patient_care_news/lungcancer.html.
- Fung KM, Tsang HW, Corrigan PW. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatric Rehabilitation Journal. 2008;32:95–104. doi: 10.2975/32.2.2008.95.104. [DOI] [PubMed] [Google Scholar]
- Gee JP. An introduction to discourse analysis : Theory and method. 3rd edn Routledge; Milton Park, Abingdon ; New York: 2011. [Google Scholar]
- Goffman E. Stigma : Notes on the management of spoiled identity. J. Aronson; New York: 1974. [Google Scholar]
- Gonzalez BD, Jacobsen PB. Depression in lung cancer patients: The role of perceived stigma. Psycho-Oncology. 2010;21:239–246. doi: 10.1002/pon.1882. [DOI] [PubMed] [Google Scholar]
- Gooneratne NS, Dean GE, Rogers AE, Nkwuo JE, Coyne JC, Kaiser LR. Sleep and quality of life in long-term lung cancer survivors. Lung Cancer. 2007;58:403–410. doi: 10.1016/j.lungcan.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henschke CI, Miettinen OS. Women’s susceptibility to tobacco carcinogens. Lung Cancer. 2004;43:1–5. doi: 10.1016/j.lungcan.2003.08.024. [DOI] [PubMed] [Google Scholar]
- Holland JC, Kelly BJ, Weinberger MI. Why psychosocial care is difficult to integrate into routine cancer care: Stigma is the elephant in the room. Journal of the National Comprehensive Cancer Network. 2010;8:362–366. doi: 10.6004/jnccn.2010.0028. [DOI] [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Edwards BKe. SEER cancer statistics review, 1975-2008. National Cancer Institute; Bethesda, MD: 2011. [Google Scholar]
- Lebel S, Devins GM. Stigma in cancer patients whose behavior may have contributed to their disease. Future Oncology. 2008;4:717–733. doi: 10.2217/14796694.4.5.717. [DOI] [PubMed] [Google Scholar]
- Lynch J, Goodhart F, Saunders Y, O’Connor SJ. Screening for psychological distress in patients with lung cancer: Results of a clinical audit evaluating the use of the patient distress thermometer. Support Care Cancer. 2010;19:193–202. doi: 10.1007/s00520-009-0799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malin D, Chen F, Schiller C, Koblinski J, Cryns VL. Enhanced metastasis suppression by targeting trail receptor 2 in a murine model of triple-negative breast cancer. Clinical Cancer Research. 2011;17:5005–5015. doi: 10.1158/1078-0432.CCR-11-0099. [DOI] [PubMed] [Google Scholar]
- Maliski SL, Sarna L, Evangelista L, Padilla G. The aftermath of lung cancer: Balancing the good and bad. Cancer Nursing. 2003;26:237–244. doi: 10.1097/00002820-200306000-00011. [DOI] [PubMed] [Google Scholar]
- Mishler EG. The discourse of medicine : Dialectics of medical interviews. Ablex Publishing Corporation; Norwood, N.J.: 1984. [Google Scholar]
- Morley L, Croft A. Agency and advocacy: Disabled students in higher education in Ghana and Tanzania. Research in Comparative and International Education. 2011;6:383–389. [Google Scholar]
- Nelson JE, Gay EB, Berman AR, Powell CA, Salazar-Schicchi J, Wisnivesky JP. Patients rate physician communication about lung cancer. Cancer. 2011;117:5212–5220. doi: 10.1002/cncr.26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarna L, Padilla G, Holmes C, Tashkin D, Brecht ML, Evangelista L. Quality of life of long-term survivors of non-small-cell lung cancer. Journal of Clinical Oncology. 2002;20:2920–2929. doi: 10.1200/JCO.2002.09.045. [DOI] [PubMed] [Google Scholar]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- Stuber J, Galea S, Link BG. Stigma and smoking: The consequences of our good intentions. Social Service Review. 2009;83:585–609. [Google Scholar]
- Sugimura H, Yang P. Long-term survivorship in lung cancer: A review. Chest. 2006;129:1088–1097. doi: 10.1378/chest.129.4.1088. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: A cross-sectional survey. Lancet. 2009;373:408–415. doi: 10.1016/S0140-6736(08)61817-6. [DOI] [PubMed] [Google Scholar]
- Truong T, Hung RJ, Amos CI, Wu XF, Bickeboller H, Rosenberger A, Spitz MR. Replication of lung cancer susceptibility loci at chromosomes 15q25, 5p15, and 6p21: A pooled analysis from the international lung cancer consortium. Journal of the National Cancer Institute. 2010;102:959–971. doi: 10.1093/jnci/djq178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group . United States cancer statistics: 1999-2008 incidence and mortality web-based report. Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2012. access at http://www.cdc.gov/uscs. [Google Scholar]
- Van Brakel WH. Measuring health-related stigma - a literature review. Psychology, Health and Medicine. 2006;11:307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- van Dijk TA. Principles of critical discourse analysis. Discourse & Society. 1993;4:249–283. [Google Scholar]
- van Uden-Kraan CF, Drossaert CH, Taal E, Seydel ER, van de Laar MA. Participation in online patient support groups endorses patients’ empowerment. Patient Education and Counseling. 2009;74:61–69. doi: 10.1016/j.pec.2008.07.044. [DOI] [PubMed] [Google Scholar]
- Vygotsky LS. Mind in society: The development of higher psychological processes. 1978 edn Harvard University Press; Boston: 1978. [Google Scholar]
- Wakelee HA, Dahlberg SE, Brahmer JR, Schiller JH, Perry MC, Langer CJ, Johnson DH. Differential effect of age on survival in advanced NSCLC in women versus men: Analysis of recent eastern cooperative oncology group (ECOG) studies, with and without bevacizumab. Lung Cancer. 2012;76:410–415. doi: 10.1016/j.lungcan.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassenaar TR, Eickhoff JC, Jarzemsky DR, Smith SS, Larson ML, Schiller JH. Differences in primary care clinicians’ approach to non-small cell lung cancer patients compared with breast cancer. Journal of Thoracic Oncology. 2007;2:722–728. doi: 10.1097/JTO.0b013e3180cc2599. [DOI] [PubMed] [Google Scholar]
- Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1988;55:738–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Ramakrishna J. Stigma interventions and research for international health. Lancet. 2006;367:536–538. doi: 10.1016/S0140-6736(06)68189-0. [DOI] [PubMed] [Google Scholar]
- Winton T, Livingston R, Johnson D, Rigas J, Johnston M, Butts C, Shepherd F. Vinorelbine plus cisplatin vs. Observation in resected non-small-cell lung cancer. New England Journal of Medicine. 2005;352:2589–2597. doi: 10.1056/NEJMoa043623. [DOI] [PubMed] [Google Scholar]
- Wodak R, Meyer M. Methods of Critical Discourse Analysis. 2nd edn Sage; London; Thousand Oaks California: 2009. [Google Scholar]
- Yang P, Cheville AL, Wampfler JA, Garces YI, Jatoi A, Clark MM, Sloan JA. Quality of life and symptom burden among long-term lung cancer survivors. Journal of Thoracic Oncology. 2012;7:64–70. doi: 10.1097/JTO.0b013e3182397b3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]