Abstract
Nanotechnology based Pharma has emerged significantly and has influenced the Pharma industry up to a considerable extent. Nanoparticles technology holds a good share of the nanotech Pharma and is significant in comparison with the other domains. Electrospraying technology answers the potential needs of nanoparticle production such as scalability, reproducibility, effective encapsulation etc. Many drugs have been electrosprayed with and without polymer carriers. Drug release characteristics are improved with the incorporation of biodegradable polymer carriers which sustain the release of encapsulated drug. Electrospraying is acknowledged as an important technique for the preparation of nanoparticles with respect to pharmaceutical applications. Herein we attempted to consolidate the reports pertaining to electrospraying and their corresponding therapeutic application area.
Keywords: electrospray, nanoparticle, nanomedicine, drug delivery, sustained release
Introduction
Nanotechnology in healthcare
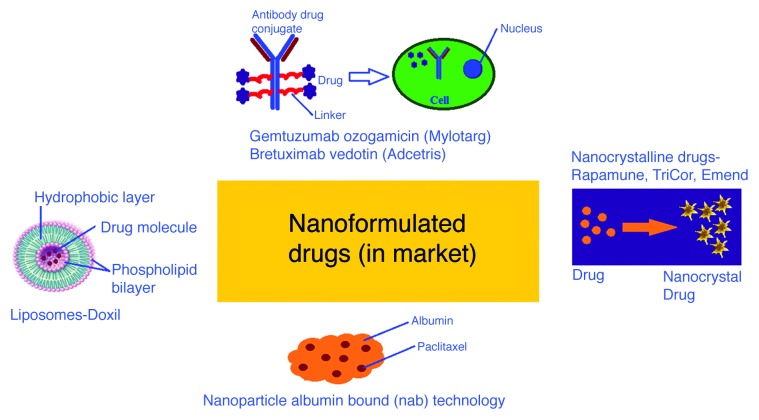
Nanotechnology not only in academic research but has emerged as a wonderful tool in product perspective in all the industry sectors. Nanotechnology mediated drug delivery research has attracted Pharma, biotech and healthcare industries during the recent decades.1 The projected timelines “from invention to market” (Fig. 1) was shortened from 30 y to ten or 15 y regarding the nanoparticulate drug formulations. And the research has gained momentum to see more FDA approvals in near future. But the expected commercial tissue engineering scaffolds or artificial organs or nano robots is getting delayed. Therapeutic benefits of nano-formulated drugs, drug eluting stents, drug coatings and devices involve improved efficacy, targeted drug delivery, reduced active drug ingredient and reduced drug side effects. Nanopharma technologists attempt for the nanoformulation that delivers the drug selectively, effectively and in a sustained manner at the site of requirement. Nanopharma drug delivery entered the healthcare industry as a result of many generic blockbuster drug patent expiry, excess cost of drug discovery and development and nanotechnology mediated drug formulation. The nano-therapeutics can enhance the efficacy and sustained release of drugs and also add to the commercial value of the healthcare products. The polymer carrier carters the drug to target, reduces the metabolic drug degradation, accounts for sustained release, increases the activity of the active pharmaceutical ingredient and reduces the side effects of the drug. The total market for nanotechnology-enabled drug delivery2 was estimated to be $26 billion by 2012 and further projected to the sky rocket $220 billion by 2015 with an average annual increase of 37%. The current trend in Nanomedicine3 drug formulations (Fig. 2) works with the nanoformulation of existing generic drug and hence reducing the cost of drug development into many folds. The main aim of the nano-formulations is to fine-tune the normal metabolic profile of proven established drug molecules by significantly improving the drug efficacy, sustained release and reduced side effects. Abraxane® is a marketed product4 of Abraxis and is a similar nanoformulation that has brought in up to 70% increase of Paclitaxel delivery against solvent based Paclitaxel delivery for breast cancer and non-small-cell lung cancer. Abraxis Bio Sciences has invented this first-in-class nanoformulation with blockbuster Paclitaxel (Taxol) drug from Bristol-Meyers-Squibb Company. Nanotechnology based drug delivery systems include nanoemulsions, lipid or polymeric nanoparticles, liposomes and nanofibers. Polymeric nanoparticular drug delivery systems have the advantages of cheaper cost, scalability, targeted delivery, biodegradability, biocompatibility, sustainability in release of encapsulated drug and improved efficacy. The biopolymers of carbohydrate origin such as Chitosan, Alginate and proteinous origin such as albumin, gelatin and silk proteins have added advantage over the synthetic polymers when there can be a compromise for long lasting stability. At the same time there are many synthetic polymers that are biocompatible and comparatively less biodegradable in comparison with natural polymers, which include polylactides (PLA), polyglycolides (PGA), poly(lactide-co-glycolides) (PLGA), polyorthoesters and polyanhydrides. These nanoparticulate drug delivery systems modify the normal pharmacokinetic profile of encapsulated therapeutic drug and help in targeted and sustained release of drug. Thus they overcome the barrier of systemic delivery which is the only way of administration for a wide range of active pharmaceutical ingredients. Nanotechnology based drug delivery systems can be classified under three major categories which can be further subdivided as tabulated (Table 1). Of these various drug delivery technologies some of which are marketed and a few in clinical trials (Table 2),5 our main interest is the nanoparticulate drug delivery which in general falls in to the following categories based on their synthesis method.6-8
Figure 1. Projected timelines for Nanopharma “from research to market”.
Figure 2. Existing Nanomedicine in clinical usage.
Table 1. Nanotechnology based drug delivery systems classification.
| Delivery Method/Routes of administration | Therapeutics | Technology |
|---|---|---|
| Oral administration |
Cancer therapy |
Nanoparticulate encapsulation |
| Transdermal delivery |
Vaccines |
Dendrimer-based targeted therapeutics technology |
| Injectable delivery |
Antibody |
Liposomes nanotechnology |
| Topical delivery |
DNA-based therapy |
Nanotube technologies |
| Nasal/pulmonary delivery |
|
Nanoparticles coating technology |
| Implantable delivery |
|
Silica-chitosan nanocomposite |
| |
|
Nanosome technology |
| |
|
Nanosuspension technology |
| |
|
Nanocrystal technology |
| |
|
Nanoshell technology |
| Polymer therapeutics |
Table 2. Nanotechnology products approved for market/in clinical trials.
| Nanocrystalline drug products | Technology of /Licensed to (Year of approval) | Indication |
|---|---|---|
| Rapamune (Sirolimus), oral |
Elan/Wyeth (2000) |
Immunosuppressant |
| Emend (Aprepitant), oral |
Elan/Merck (2003) |
Antiemetic |
| Tricor (Fenofibrate), oral |
Elan/Abbott (2004) |
Treatment of high cholesterol and high triglycerides |
| Invega Sustena (Paliperidone Palmitate), IV |
Elan/Johnson and Johnson (2009) |
Treatment of schizophrenia |
| |
|
|
| Liposomal drug products |
|
|
| Ambisome (Amphotericin B), IV |
Gilead (1990) |
Severe fungal infections |
| Abelcet (Amphotericin B), IV |
Cephalon (1995) |
Severe fungal infections |
| Depacyt (Cytarabine), Epidural |
Napp (2002) |
Neoplastic meningitis and lymphomatous meningitis |
| DepoDur (Morphine sulfate), Spinal |
Flynn Pharma Limited (2004) |
Pain Management |
| |
|
|
| Polymeric micelles |
|
|
| NK-911 (Doxorubicin), IV |
Nippon Kayaku Co (Phase II) |
Cancer targeting |
| NK-6004 (Cisplatin), IV |
Nanocarrier Co (Phase II) |
Cancer targeting |
| SP-1049C (Doxorubicin), IV | Anti-multidrug resistance (Phase II) | Supratek Pharma Inc. |
Lipid-Based Delivery Systems
Submicron lipid-drug nanocapsules constitute oily lipid core encapsulated by a solid or semisolid shell. These DDSs have the dual characterof colloidal stability of solid particle suspensions in biological fluids and the solubilizing properties of liquids.9,10 Because of the solubilizable matrix, it can incorporate the active pharmaceutical ingredient from metabolism11 and ensure sustained release of the drug component.12
Micelles (Polymer Nanoparticles) in Drug Delivery
The nanoparticle polymeric micelles have the merits of solubilizing hydrophobic drug molecules, smaller particle size formation, in vivo thermodynamic stability, sustained release of various drugs and sustaining the drug against the reticulo-endothelial system.13 These polymeric micelles can deliver the lipophilic drug in oral route. Target specific drug delivery through drug encapsulated polymeric micelles followed ultrasound mediated increased intracellular drug uptake in tumor cells was reported by Gao etal as a new technology.14
Polymer-Based Nanoparticulate Drug-Delivery Systems
A variety of non-lipid nanoparticulate systems are available as ideal carriers of drug encapsulation and sustained release, out of which hydrogels, dendrimers, chitosan based saccharide nanoparticles, protein based gelatin or albumin nanoparticles and lactide based biodegradable polymer nanoparticles are very common. In this review we focus only on the polymer nanoparticle drug carriers synthesized by electrospraying method and their worthiness as drug delivery systems. Various synthetic methods are available for the synthesis of the polymer nanoparticles mainly classified in to top-down and bottom up processes (Table 3). The electrosprayed nanoparticle synthesis falls under the top-down category where the larger particle is broken down into a smaller nanoparticle with the application of potential charge difference.
Table 3. Comparison of Nanoparticle synthesis methods.
| Type | Method | Mechanism | Merits | Demerits | Application Domain |
||
|---|---|---|---|---|---|---|---|
|
Bottom – Up Synthesis |
Gas (Vapor) phase fabrication-Pyrolysis |
Precursor vaporization, nucleation, growth |
Simple, low cost, continuous operation, high yield |
More chances of polymer, drug or biomaterial degradation |
Calcium phosphate microspheres and Au nanoparticles for drug delivery |
||
| Liquid Phase Fabrication- Sol-Gel or solvothermal synthesis |
Precursor solution (involves catalyst), nucleation, growth |
Simple, low cost, continuous operation, high yield |
Needs removal of catalyst components, May involve excess solvent usage for scale ups |
Highly explored technology for drug delivery and biomedical applications |
|||
| | |||||||
| Top-Down Synthesis | Lithography, Etching, Milling or Machining |
Braking down of large piece of material |
offers reliability and device complexity |
Higher energy spent and more waste produced |
Electronic device Industry |
||
| Electrospraying | Driven by difference in electric potential and surface viscosity | Increased drug encapsulation efficiency, simplicity, low cost, continuous operation, high yield. | Chances of shear or thermal stress in some biomaterial nanoparticle synthesis | Has good prospects in drug delivery and pharma based industry | |||
Electrosprayed Nanoparticulate Drug Delivery Systems
Electrospray technique (Fig. 3) is one of the most efficient techniques for the preparation of Nano particles/Nanospheres. The experimental set up has a syringe pump with polymer solution connected to the high voltage power supply that constitutes the functional electrode. A metal foil collector placed opposite functions as the ground electrode. The flow rate and the applied voltage were optimized depend on the type of the solution used for electro spraying. The liquid emerging from the nozzle into the electric field forms tailor cone because of the surface tension.15 By increasing the electric field the Taylor cone breaks into highly charged droplets, selecting the suitable conditions leads those droplets close to micro or nano size level. Solid particles can be produced by solvent evaporation. Needle gauge diameter, applied voltage, flow rate and working distance differ for the respective drug delivery systems. The principle of electro spraying is to apply a high voltage to a polymeric solution to force the polymer to come out from the syringe in the form of nanoparticles. Electrospraying has emerged as a similar technique as the electrospinning which uses the analogous technology for the production of nanostructures. The nanoparticles can be useful for numerous biological, medicinal or pharmaceutical applications because of its zero dimensional nature, whereas the nanofibers can be only useful for their two dimensional applications. Even then the research work done on electrosprayed nanoparticles quantified in terms of journal publications is quite less in comparison with that of the electrospun nanofibers. The advantages of the electrospraying include increased scalable synthesis, reproducibility and high encapsulation efficiency. This method is not only convenient for the synthesis of synthetic polymer nanoparticles but also for natural polymer nanoparticles either protein or carbohydrate and was found to produce stable nanoparticles without any loss of their bioactivity of either the drug or encapsulating biomolecules. These nanoparticles have broad spectrum applicability from soft tissue to hard tissue regeneration. When the PLGA nanoparticles are used for soft tissue applications, coatings of calcium phosphate nanoparticles find application on titanium implants16 and for developing bioceramics scaffolds of zirconia.17 Electrospray nebulizers were used for producing micro particles of size range 2–5 microns and the particles serve the purpose of inhaling medicines through lungs. These “breathable size range particles” are designed to deliver the medicine in to the lower airways without loss of drug activity of the encapsulated medicine.18-23 Electrosprayed nanoparticles can encapsulate drugs and can be specific drug carriers because of their active surface absorption, binding or complexation with drug.24 In the other hand the nano particle size plays an important role in the therapeutic treatment, the particle size is one of the factors to decide the drug carrier velocity, specificity towards binding or adhesion and reactivity.25 Thus the electrosprayed nanoparticle technology opens a new domain for drug delivery applications and therapeutic use (Table 4).

Figure 3. Illustration for electro spraying technique.
Table 4. Therapeutic area and conditions for the synthesis of electrosprayed drug loaded micro/nanoparticles.
| No | Polymer carrier | Drug encapsulated | Particle size (nm) | Therapeutic area | Condition |
|---|---|---|---|---|---|
| 1 |
Polycapolactone36 |
Budesonide |
116.1 ± 19 |
Asthma |
0.5 to 6% PCL, 120 μg/ml of drug, 0.001% (v/v) surfactant flow rate 1ml/h, Applied voltage 5–15 kV. |
|
2 |
PLGA37 |
Celecoxib |
1 to 4 µm |
Anti-inflammatory |
Total concentration at 5% PLGA+ drug, Flow rate 1.2 ml/h, Applied voltage 11–13 kV. |
|
3 |
- |
Carbamazepine38 |
320 to 1000 |
Anticonvulsant |
Up to 3 wt % solution, Flow rate up to 1.2 ml/h, Applied voltage 20 kV |
|
4 |
Lactose39 |
Bovine Serum albumin (BSA) |
700 |
Formulations as dry powder inhalers |
2% BSA with respect to solvent ethanol/acetic acid (96/4), Flow rate up to 0.3 ml/h, Applied voltage 5 kV |
|
5 |
Stearic acid and Ethyl cellulose41 |
Tamoxifen |
922 ± 52 nm |
Lipid nanoparticles (for Breast cancer treatment) |
Polymer carrier/drug ratio was 10/1. Flow rate up to 0.6 ml/h, Applied voltage 30 kV. |
| 6 | Polyvinylpyrrolidone (PVP) and Tristearin (GTS)42 | Naproxen | 720 ± 700 nm | Self-assembled solid lipid nanoparticles. (anti-inflammatory) | PVP/GTS/Naproxen ratio was 20/5/1. Flow rate up to 1 ml/h, Applied voltage 6–12 kV. |
Advantages of electro spraying technique:
Can produce lowest and uniform particle size as possible.
Easy to control the operation parameters.
Fast preparation and one step technique.
This involves simple ideology
This technique can be able to extend for bulk production.26
Disadvantages of electro spraying technique:
This technique may induce some macromolecule degradation due to the stress involved in the operation parameters (ex: Thermal stress in drying, shear stress in the nozzle).27,28
Cancer Drug Delivery
Gulfam et al.,29 electrosprayed nanoparticles of natural gliadin polymer for controlled release of cyclophosphamide anticancer drug. Cyclophosphamide is a cyclic phosphamide ester of mechlorethamine used to treat retinoblastoma, neuroblastoma, lung cancer and breast cancer by cross-linking with DNA and prevent cell division. Over 72.02 ± 5.6% of drug loading was achieved with the 7% gliadin based nanoparticles. At 7% gliadin, the particles were homogeneous and had an average size 218.66 ± 5.1 nm and have a narrow distribution. The particle size of gliadin or gliadin-gelatin composite nanoparticles were found increase with increase in gelatin concentration as observed by dynamic light scattering and X-ray diffractometry experiments. The drug loading of 64.23 ± 8.9% with the particle size of 398 ± 4.2 nm and 52.77 ± 12.6% with the particle size of 450.10 ± 9.7 nm were obtained with the 7% gliadin/4% gelatin and 7% gliadin/8% gelatin respectively. Also the gliadin-gelatin composite nanoparticles released cyclophosphamide rapidly whereas gradual release was noted with gliadin nanoparticles for 48 h. By culturing breast cancer cells with cyclophosphamide-loaded 7% gliadin nanoparticles for 24 h, downregulation of Bcl-2 protein was observed with western blot analysis which confirmed the apoptotic effect of the nanoparticle formulation. Even though the preparation of gliadin and gliadin-gelatin composite nanoparticles carried the same active drug component, gliadin based nanoparticle had the advantage over gliadin-gelatin composite nanoparticle because of its smaller size and slow drug release. Electrosprayed chitosan nano/micro particles were attempted for drug delivery with chitosan as a natural biodegradable and biocompatible polymer.30 Kim etal.,31 observed 3D chitosan nanofibrous networks by freeze-drying the electrosprayed chitosan nanoparticles. Doxorubicin (DOX) is the well-known anticancer drug has its own side effects such as cytotoxicity to normal tissues, induction of multidrug resistance and acute cardio toxicity. In order to reduce these effects and to improve the therapeutic efficiency of DOX, DOX-loaded chitosan stabilized with Tripolyphosphate nanoparticles tried for its feasibility using an optimized electro spray ionization technique. Doxorubicin loaded chitosan nanoparticles were electrosprayed with Tripolyphosphate stabilization32 and achieved high encapsulation efficiency (EE) up to 67.9%. The controlled release of the drug from the biopolymer nanoparticle was up to 70% over the period of 72 h. The variation of the parameters such as applied voltage, working distance, needle gauze and flow rate were manipulated so as to obtain nanoparticles of the drug loaded chitosan-Tripolyphosphate nanoparticle system. Titanium dioxide (TiO2) nanoparticles loaded with Paclitaxel (TiO2 electrosprayed core-shell microspheres for Paclitaxel delivery) was electrosprayed as core shell nanoparticles by Jing etal. The particle size was observed in 600 nm to 6 µm with the Titania protecting the initial burst release of the drug. The drug release was triggered with ultrasonic stimulation of the nanoformulation. Yun Wu et al.33 produced oligodeoxynucleotide (ODN) encapsulated lipoplex nanoparticles by coaxial electrodynamic spraying for intravenous injection and for pulmonary delivery. Lipoplex had its own advantage that it has phospholipids bilayers that can encapsulate and carry drug or gene within the hydrophobic bilayers or in the hydrophilic core. ODN is a potential therapeutic agent against viral infection, cardiovascular inflammation, other pulmonary diseases and cancer. G3139 type ODN /lipoplex nanoparticles were successfully generated by coaxial electro spray technique. Lipoplex nano particles of size 190 ± 39 nm showed Zeta potential of +4.5 ± 0.4 mV were produced. The G3139 encapsulation efficiency up to 90 ± 6% was achieved with the above conditions. Transferrin was well conjugated with the lipoplex nanoparticles formed and provided the ability for the leukemia cellular uptake.G3139 in both non targeted and Tf-targeted lipoplex nanoparticles was efficiently delivered to K562 cells by 34 ± 6% and downregulated the bcl-2 protein expression by 57 ± 3%.
Cardiac Applications of Nanoparticular Formulations
Injectable nanoparticles have been widely studied for cardiomyoplasty both by means of acellular and cellular approach. In general the injectable nanoparticulate materials form a hydrogel or occupies the intrices of the infarcted myocardium, renders temporary mechanical support, assist in cardiomyocyte regeneration and thereby cardiac restoration. Electrosprayed PLGA porous beads were cellularized with human amniotic fluid stem cells (hAFSCs) and tested as injectables.34 The microporous, cellularised microparticles improved regional contractile capacity together with neovascularization and myocardial regeneration. Li etal35 attempted hydrogen peroxide releasing electrosprayed core-shell microparticle together with cardiosphere-derived cells (CDCs) and thermosensitive hydrogel, from hydroxyethyl methacrylate-oligo hydroxybutyrate) (HEMA-oHB) as cardiac regeneration. The oxygen releasing scaffold improved survival and assisted in cardiac differentiation of CDCs. Further the combination hydrogel system matched the stiffness of a cardiac tissue, supported cardiomyocytes formation and sustained the release of oxygen up to two weeks.
Nanoparticles as Antibacterial Agents
Hazeri et al. electro sprayed nanopowder of Sericin, an antibacterial agent used in food, cosmetics and drug delivery. Basically Sericin is a porteinous substrate available in Bombyx mori (silk worm). Electro spraying solution was prepared by dissolving the Sericin sponge in Dimethyl Sulfoxide and achieved 25nm particle size which consists of small crystallites and high moisture absorbance.36 Roine et al. discussed about the feasibility of preparing the mesoporous silicon (PSi) nanoparticles which can be used as a drug carrier in drug delivery system.37
Ag nanoparticles play an important role as antibacterial agent and this property of Ag+ ion extends its use biomedicine. So far Ag nanoparticles used in cosmetics, pigments and antibacterial agents. Zhijun et al.38 investigated the synthesis of Ag nano particles. In order to prevent coagulation or oxidation Ag nano particles, it has to be stored in stabilizer matrix so that it can act as an antibacterial agent without degradation for long time. SiO2 is highly recommended by many users as a stabilizer because of its chemical stability and biocompatibility. These silica stabilized silver nanoparticles can be made by coating the synthesized Ag nanoparticles with a thin layer of SiO2. These nano particles are quite stable with notable surface properties that of SiO2. But the antibacterial efficiency of Ag nanoparticles toward microorganism gets reduced. The other method for the synthesis of silica stabilized Ag nano particles involves incorporation of Ag nanoparticles into the porous silica surface by coupling or chemical adsorption. In this case the Ag nanoparticles can be directly contact with microorganism and can establish its activity as an antibacterial agent. But the interaction between Ag nano particles and SiO2 is weak or unstable and thereby it loses its antibacterial activity within the required period of time. The practical biomedical applications demand the long lasting antibacterial activity in order to avoid further infections after any treatment or implantations. In order to achieve the long lasting anti-infective property, Zhijun et al. attempted the new efficient Ag NPs- SiO2 microspheres by electro spraying. In this method, the Ag nanoparticles were doped inside SiO2 and were also embedded on the surface of the SiO2. The resultant nanoparticles were proved to be very efficient and more stable. The silica precursor was made by adding 4.5mL HNO3 in to 30 ml of tetra ethoxysilane in 30 ml of ethanol solvent and finally hydrolyzing the mixture at 80°C for almost 3 h. In parallel, Ag solution was prepared by dissolving required amount of AgNO3 in 2:1 ethanol/acetonitrile and was added to silica precursor. The resultant solution was electrosprayed, dried at room temperature for 24 h, annealed at 400°C and reduced with 5% H2, 95% N2. The bactericidal efficiency was calculated with the E. coli count and was shown that maximum bactericidal efficiency was achieved at 500 ppm. Further it was also shown (Fig. 4) that the Ag-NPs-SiO2 microspheres were biocompatible with a cytotoxicity study using human Bone marrow derived mesenchymal stem cell (BMSC) as a model cell. The shelf life was investigated for Ag-NPs-SiO2 microspheres and was shown to be very good antibacterial efficiency even after two months of storage.

Figure 4. Antimicrobial efficacy and bactericidal efficiency as a measure of silver/silica nanoparticle sample concentration.
Nano Particles in Inflammatory Drug Delivery
Midhun et al.39 synthesized Budesonide loaded polycaprolactone nanobeads by using electro spray technique. Budesonide is a glucocorticoid steroid used for treatment of asthma, non- infectious rhinitis or allergies, nasal polyposis and inflammatory bowel disease. Polycaprolactone as a biodegradable polyester was used as a drug carrier and 116.1 ± 19 nm size particles were synthesized from optimal operating conditions of 1.5 wt% polymer concentration, 0.001% (v/v) surfactant concentration, flow rate 1ml/h, tip-target distance 10 cm and with the applied DC voltage ~8 kV. The drug encapsulation efficiency was found to be 75 ± 2.4% and the drug release profile observed at pH 7.4 and 5.6 in vitro showed the sustainable result @37°C. The analytical methods dynamic laser light Scattering (DLS) used for particle size conformation, laser Doppler anemometry for stability of colloidal suspension and SEM for surface morphology. The drug entrapment in the PCL matrix was confirmed using Fourier Transform Infrared spectrometry (FT-IR). Celecoxib, a sulfo non-steroidal drug for inflammatory disease nano beads were prepared with PLGA by electro hydrodynamic spraying. The particle size can be produced in the range of 1 to 4 µm by this method.40
Nanoparticles in Neurology
Mao Wang et al.41 produced nano crystals with anticonvulsant drug called carbamazepine. It is a poor water soluble drug and continually used for pharmaceutical manufacturing process. They developed the electro sprayed carbamazepine crystals of 320 nm particle size. The crystallization was accelerated by annealing @90°C for 5 min and the resultant T50of the formed carbamazepine = 3 ± 3mins.This shows that its solubility increased by 26.4%. It is confirmed by XRD and surface morphology by SEM.
Protein Based Nanoparticles in Drug Delivery
Tavares et al.42 successfully developed a protein based nano particle of size 700 nm by electrohydrodynamic atomization (EHDA). They used Bovine Serum albumin (BSA) as a model protein and lactose as a biological carrier (Fig. 5). This new approach opens a door for the production of new formulation for dry powders for drug delivery system. Christopher et al.43 developed a ferritin based nano particle. Ferritin is an intracellular protein molecule that stores the iron in a soluble and non-toxic form and releases it in a controlled fashion. The ferritin dissolved in 10 mM Ammonium acetate taken in the syringe and sprayed along with CO2 gas flow 0.51/min. The applied voltage was controlled at 2-3 kV and the ferritin-aerosol complexes were introduced into the furnace at the flow rate of 1.01/min. The furnace temperature varied from 25°C to 800°C.The particles thus produced were sent to the radioactive source kr-85 to produce reduced and steady charged particles. The Scanning Mobility Particle spectra supports the size distribution and showed the result that the ferritin particle size is about 13.1 nm and apoferritin particle size is about 11.8 nm. Ferritin and apoferritin are clearly distinguishable and separated out with different degrees of compression.
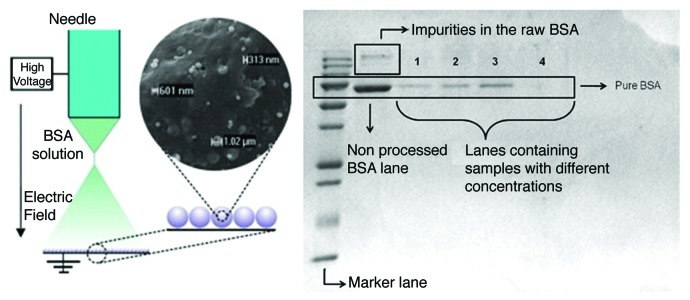
Figure 5. SEM image of the composite lactose plus BSA obtained by EHDA and SDS-PAGE of the BSA not processed and of 4 different samples of the composite lactose–BSA. Lanes 1, 2 and 4, lactose exposed to the jet for 1200s. Lane 3, lactose exposed to the jet for 3600s.
Lipid-Based Nanoparticles in Drug Delivery
Biodegradable polymers can be used as drug carriers and they are very effective in terms or reducing the drug side effects. Lipids are the novel drug carriers and many researches have been done on lipid based drug delivery systems. It is evident that they can also be prepared as nanoparticles for effective and controlled drug release. Trotta et al.44 tried a new method to prepare Lipid based nanoparticles by electro spraying. They prepared Tamoxifen –lipid nanoparticles. A known weight of drug was dissolved in Stearic acid and Ethyl cellulose mixture (4.5:0.5 w/w) and the solution was taken in a syringe. Then it was electrosprayed under high voltage and the nano particles were collected on the 150 mm distant aluminum tray kept as ground opposite to the syringe. The particle size of the nano particles formed was less than 1 µm with 76% drug encapsulation efficiency and the in vitro Tamoxifen drug release from lipid nanoparticles was observe by shaker experiment. The experiments showed 96% drug release from the encapsulated lipid nanoparticle in solution and followed slow kinetics through the through dialysis membrane. It was observed that there was an initial burst release of 30% and constant release up to 50% till 24 h through dialysis membrane. Deng et al.45 developed a self-assembled lipid based nanoparticles for the drug Naproxen (NAP). NAP is a drug widely used for inflammatory bowel disease. By the electro spraying method they achieved 376 ± 20nm particle size. The carrier chosen for the preparation of lipid based nanoparticle polyvinyl pyrrolidone K25, glyceryl tristearate (GTS) with NAP in the ratio of 20%:5%:1% at 50°C. The voltage applied was 6–12 kV, at the flow rate of 1 ml/h, the working distance kept at 25 cm and 50 degrees elevated-temperature was achieved by auxiliary apparatus. As a result of electrospraying micro-particles were obtained and drug encapsulation efficiency was found to be 86.2%. The in vitro cumulative drug release was calculated as 85.6% after 24 h and was explained with the release mechanism which was via micro-particle aggregation route. In the first step, the micro-particles absorb water, swell and finally collapse to liberate GTS and NAP molecules in to the buffer. In the second step there occurs strong interaction between the GTS and NAP molecules which results nanoparticle aggregates. This occurs when the PVP molecules dissolve completely, entirely collapse and thereby GTS and NAP self-assemble as nanoparticle and freed into the dissolution medium. This solid liquid nanoparticles (SLN) could find wide range of applications in cosmetics and drug delivery pharmaceutical fields.
Miscellaneous Electrosprayed Nanoparticles for Drug Delivery/Biomedical Applications
Andres et al.46 formed α-eicosene wax nanoparticles of size range from 0.5–5 µm by electro spraying. The wax was preheated above its melting point, 26°C and introduced into the metallic syringe for electrospraying. The working distance is 7 cm with the applied voltage 2.6 to 2.9 kV and flow rate up to 3.0 ml/h. The particles thus formed washed with ethanol and dried. The Dynamic light scattering supports to analyze the particle size distribution (Fig. 6). The α-eicosene nanoparticles were produced owing to their prospective cosmetics preparations. Luis B et al.47 tried to prepare TiO2 agglomerates with ethanol by electro spraying method which is used to develop the nano structured film deposition. The film thus produced has précised nano structures and larger surface area when compared with the other printing methods. Lahann48 developed an interesting compartmentalized nano particle by electro spray method. He tried electro spraying with different polymers using water and organic solvents. His idea of compartmentalization was a hint to achieve a targeted drug release from the drug delivery systems. Zhang et al.49 fabricated the chitosan nanoparticles by one step electro spray deposition method. They obtained the smallest average particle size of 124 nm. Yiquan et al.50 suggested an electro spraying technique that is flexible and effective method for generating stimuli –responsive drug particles. They fabricated the elastin-like polypeptide (ELPs) based nanoparticles of size 300–400 nm. Novel, quantum dots (QDs) encoded microspheres (Fig. 7) were electrosprayed for the detection of bio molecules by Lei sun et al.51 They prepared polystyrene based microspheres with CdSe-ZnS QDs by electro spraying method. Polystyrene solution was prepared by dissolving in DMF at room temperature with vigorous stirring for 24 h. QD solution was prepared by dissolving 0.15 g in Chloroform. Then the two solutions were mixed, electrosprayed to yield microspheres and the particles were separated by ultrasound. The in vitro release of the quantum dots was examined by the incubation of the Hela cells with QD encoded microspheres at varying concentrations for 24 h and viability was measured with MTT assay.

Figure 6. Monodisperse wax emulsions produced with a collection solution of 80 wt% ethanol, 20 wt% water, 0.005 wt% of Tergitol 15-S-9 and 20 mM SDS. The flow rate is 4 ml/h and the voltage is 2.8 kV. (A) Micrograph of the hexagonal lattices of emulsion droplets confirms size uniformity. (B) Droplet size distribution measured by dynamic light scattering. The diameter of the droplets is 1.02 ± 0.03 μm, and the polydispersity is 2.7 ± 0.1%.
Figure 7. Quantum dot encoded microspheres synthesized by electrospraying.
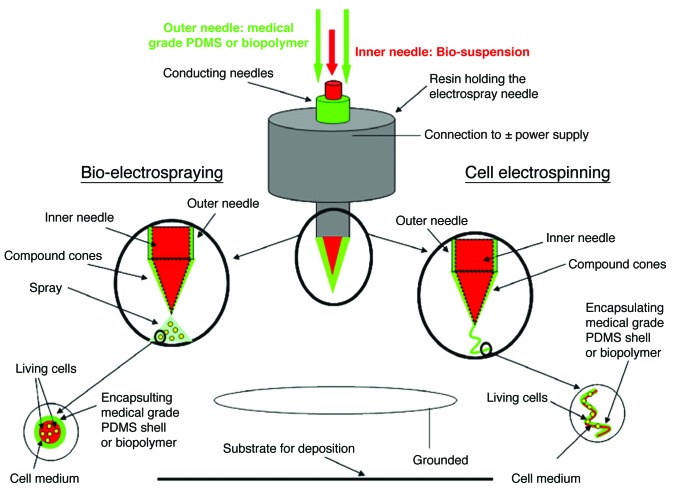
Bio-Electrospraying
Bio-electrospraying is the technique which involves spraying of cells with the application of electrical potential difference. Jayasinghe et al., have electrosprayed human bood52 (Fig. 8) and jurkat cells,53 assessed for their viability by way of trypan blue staining. This methodology of bio-electrospraying provides a wide range of applications54-57 spanning bio-analytics, diagnostics which has potential to form of synthetic or artificial tissues. Further it can be applied for repairing and replacing damaged/aging tissues, to the targeted and controlled delivery of personalised medicine through experimental and/or medical cells and/or genes.
Figure 8. Schematic representation of a coaxial needle arrangement for controlled generation of either cell-bearing droplets or threads.
Conclusions
This review dealt with the applications of electrosprayed nanoparticles mainly in the drug delivery and pharmaceutical domain where the technology is yet to reach its maximum utility. When both the nanofibers and nanoparticles have the accessibility by means of similar technique which involves the application of electrical potential difference, it was noted that the research in the area of electrospun nanofibers has resulted in more number of publications when compared with the numbers from electrosprayed nanoparticles (Fig. 9). In terms of pharmaceutical applications, nanoparticles have wider applicability than the nanofibers. This implies that electrosprayed nanoparticles though have huge potential applications in various domains still remains unexplored as compared with the electrospun nanofibers. Though there may be issues with stability of biomolecules or thermal stress or shear stress, they can be overcome with suitable carrier molecules and appropriate electrospraying conditions which can set a breakthrough in Nanopharma industry.
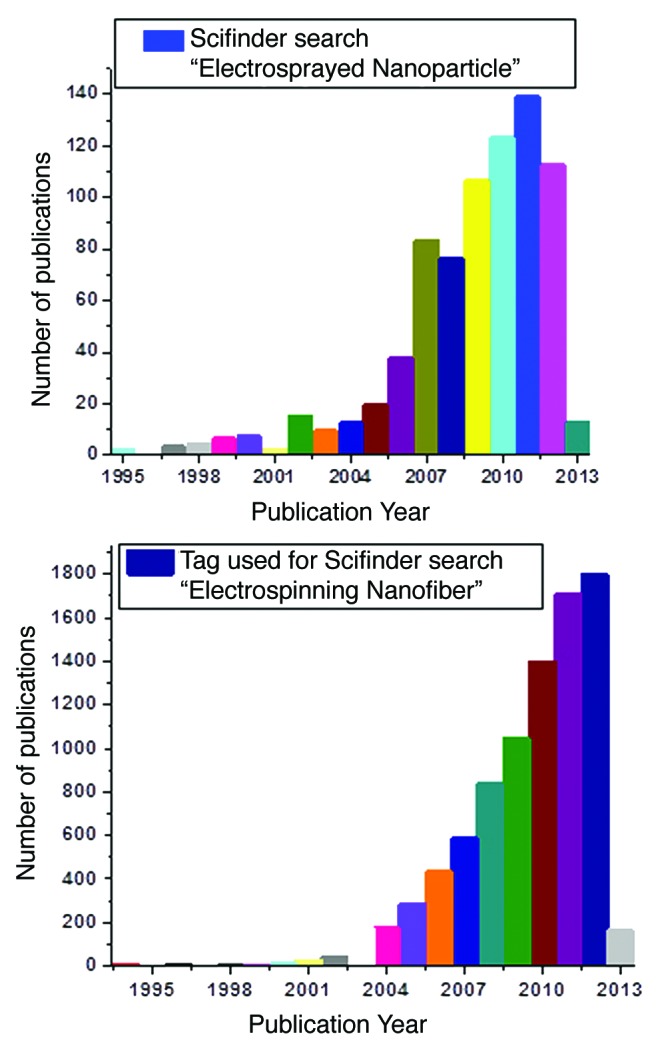
Figure 9. Comparison of publications of electrosprayed nanoparticles and electrospun nanofibers (based on Scifinder search).
Acknowledgments
This study was supported by the Ministry of Education (R-265–000–318–112), NRF-Technion (R-398–001–065–592), A*STAR-BEP (R-265–000–437–305) and NUSNNI, National University of Singapore, Singapore.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/biomatter/article/24281
References
- 1. http://nextbigfuture.com/2008/01/silicon-electronics-providing-early.html
- 2. http://www.cientifica.com/WhitePapers/054_Drug%20Delivery%20White%20Paper.pdf
- 3.Raj Bawa. Nanoparticle-based Therapeutics in Humans: A Survey. www.rpitechnology.com/files/NANOPA4.pdf
- 4. http://www.fd.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation /EnforcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalCompanies/UCM289191.pdf
- 5. http://www.americanpharmaceuticalreview.com/Featured-Articles/126889-Implementing-Nanotechnology-and-Novel-Drug-Delivery-Systems-to-Improve-Dissolution-and-Solubilization
- 6.Gulsun T., Gursoy RN, Levent O. Nanocrystal Technology for Oral Delivery of Poorly Water soluble Drugs. FARAD Journal of Pharmaceutical Sciences. 2009;34:55–65. [Google Scholar]
- 7.Chang HI, Yeh MK. Clinical development of liposome-based drugs: formulation, characterization, and therapeutic efficacy. Int J Nanomedicine. 2012;7:49–60. doi: 10.2147/IJN.S26766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yokoyama M. Polymeric micelles as a new drug carrier system and their required considerations for clinical trials. Expert Opin Drug Deliv. 2010;7:145–58. doi: 10.1517/17425240903436479. [DOI] [PubMed] [Google Scholar]
- 9.Heurtault B, Saulnier P, Benoit JP, Proust JE, Pech B, Richard J. Lipid nanocapsules, preparation, method and use as a medicine. Patent No. W001/64328, 2000.
- 10.Heurtault B, Saulnier P, Pech B, Benoit JP, Proust JE. Interfacial stability of lipid nanocapsules. Colloids Surf B Biointerfaces. 2003;30:225. doi: 10.1016/S0927-7765(03)00096-1. [DOI] [Google Scholar]
- 11.Jenning V, Schäfer-Korting M, Gohla S. Vitamin A-loaded solid lipid nanoparticles for topical use: drug release properties. J Control Release. 2000;66:115–26. doi: 10.1016/S0168-3659(99)00223-0. [DOI] [PubMed] [Google Scholar]
- 12.zur Mühlen A, Schwarz C, Mehnert W. Solid lipid nanoparticles (SLN) for controlled drug delivery--drug release and release mechanism. Eur J Pharm Biopharm. 1998;45:149–55. doi: 10.1016/S0939-6411(97)00150-1. [DOI] [PubMed] [Google Scholar]
- 13.Kabanov AV, Batrakova EV, Alakhov VY. Pluronic block copolymers as novel polymer therapeutics for drug and gene delivery. J Control Release. 2002;82:189–212. doi: 10.1016/S0168-3659(02)00009-3. [DOI] [PubMed] [Google Scholar]
- 14.Gao ZG, Fain HD, Rapoport N. Controlled and targeted tumor chemotherapy by micellar-encapsulated drug and ultrasound. J Control Release. 2005;102:203–22. doi: 10.1016/j.jconrel.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 15.Bock N, Woodruff MA, Hutmacher DW, Dargaville TR. Electrospraying, a Reproducible Method for Production of Polymeric Microspheres for Biomedical Applications. Polymers. 2011;3:131–49. doi: 10.3390/polym3010131. [DOI] [Google Scholar]
- 16.Siebers MC, Walboomers XF, Leeuwenburgh SCG, Wolke JGC, Jansen JA. Electrostatic spray deposition (ESD) of calcium phosphate coatings, an in vitro study with osteoblast-like cells. Biomaterials. 2004;25:2019–27. doi: 10.1016/j.biomaterials.2003.08.050. [DOI] [PubMed] [Google Scholar]
- 17.Dorozhkin SV. Review: Calcium Orthophosphates as Bioceramics: State of the Art. J. Funct. Biomater. 2010;1:22–107. doi: 10.3390/jfb1010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez A, Bingham D, de Juan L, Tang K. Production of protein nanoparticles by electrospray drying. J Aerosol Sci. 1998;29:561–74. doi: 10.1016/S0021-8502(97)10031-3. [DOI] [Google Scholar]
- 19.Kaerger JS, Price R. Processing of spherical crystalline particles via a novel solution atomization and crystallization by sonication (SAXS) technique. Pharm Res. 2004;21:372–81. doi: 10.1023/B:PHAM.0000016252.97296.f1. [DOI] [PubMed] [Google Scholar]
- 20.Gomez A. The electrospray and its application to targeted drug inhalation. Respir Care. 2002;47:1419–31, discussion 1431-3. [PubMed] [Google Scholar]
- 21.Huikko K, Kostiainen R, Kotiaho T. Introduction to micro-analytical systems: bioanalytical and pharmaceutical applications. Eur J Pharm Sci. 2003;20:149–71. doi: 10.1016/S0928-0987(03)00147-7. [DOI] [PubMed] [Google Scholar]
- 22.Ijsebaert JC, Geerse KB, Marijnissen JCM, Scarlett B. Electrohydrodynamic spraying of inhalation medicine. J Aerosol Sci. 1999;30:825–6. doi: 10.1016/S0021-8502(99)80423-6. [DOI] [Google Scholar]
- 23.Ijsebaert JC, Geerse KB, Marijnissen JCM, Lammers JWJ, Zanen P. Electro-hydrodynamic atomization of drug solutions for inhalation purposes. J Appl Physiol. 2001;91:2735–41. doi: 10.1152/jappl.2001.91.6.2735. [DOI] [PubMed] [Google Scholar]
- 24.De Jong WH, Borm PJA. Drug delivery and nanoparticles: applications and hazards. Int J Nanomedicine. 2008;3:133–49. doi: 10.2147/IJN.S596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Champion JA, Katare YK, Mitragotri S. Particle shape: a new design parameter for micro- and nanoscale drug delivery carriers. J Control Release. 2007;121:3–9. doi: 10.1016/j.jconrel.2007.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaworek A. Micro –and nanoparticle production by electrospraying. Powder Technol. 2007;176:18–35. doi: 10.1016/j.powtec.2007.01.035. [DOI] [Google Scholar]
- 27.Yurteri CU, Hartman RPA, Marijnissen JCM. Producing Pharmaceutical particles via Electrospraying with an Emphasis on Nano and Nano Structured Particles - A Review. KONA Powder and Particle Journal 2010; 28. [Google Scholar]
- 28.Zhikai T. Mechanisms involved in the electrospray of biological macromolecules. Submitted for the degree of Doctor of Philosophy, Department of Engineering, Queen Mary, University of London. [Google Scholar]
- 29.Gulfam M, Kim JE, Lee JM, Ku B, Chung BH, Chung BG. Anticancer drug-loaded gliadin nanoparticles induce apoptosis in breast cancer cells. Langmuir. 2012;28:8216–23. doi: 10.1021/la300691n. [DOI] [PubMed] [Google Scholar]
- 30.Zhang S, Kawakami K. One-step preparation of chitosan solid nanoparticles by electrospray deposition. Int J Pharm. 2010;397:211–7. doi: 10.1016/j.ijpharm.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 31.Kim MY, Lee J. Chitosan fibrous 3D networks prepared by freeze drying. Carbohydr Polym. 2011;84:1329–36. doi: 10.1016/j.carbpol.2011.01.029. [DOI] [Google Scholar]
- 32.Songsurang K, Praphairaksit N, Siraleartmukul K, Muangsin N. Electrospray fabrication of doxorubicin-chitosan-tripolyphosphate nanoparticles for delivery of doxorubicin. Arch Pharm Res. 2011;34:583–92. doi: 10.1007/s12272-011-0408-5. [DOI] [PubMed] [Google Scholar]
- 33.Wu Y, Yu B, Jackson A, Zha W, Lee LJ, Wyslouzil BE. Coaxial electrohydrodynamic spraying: a novel one-step technique to prepare oligodeoxynucleotide encapsulated lipoplex nanoparticles. Mol Pharm. 2009;6:1371–9. doi: 10.1021/mp9000348. [DOI] [PubMed] [Google Scholar]
- 34.Huang CC, Wei HJ, Yeh YC, Wang JJ, Lin WW, Lee TY, et al. Injectable PLGA porous beads cellularized by hAFSCs for cellular cardiomyoplasty. Biomaterials. 2012;33:4069–77. doi: 10.1016/j.biomaterials.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 35.Li Z, Guo X, Guan J. An oxygen release system to augment cardiac progenitor cell survival and differentiation under hypoxic condition. Biomaterials. 2012;33:5914–23. doi: 10.1016/j.biomaterials.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Najmeh H, Hossein T, Ali Reza M. Production and properties of electro sprayed sericin nanopowder. Science and Technology of Advanced Materials. 2012;13:1–7. doi: 10.1088/1468-6996/13/3/035010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jorma R, Matti M, Markko M, Jarno S. Dual-capillary electroencapsulation of mesoporous silicon drug carrier particles for controlled oral drug delivery. J Electrost. 2012;70:428–37. doi: 10.1016/j.elstat.2012.06.003. [DOI] [Google Scholar]
- 38.Ma Z, Ji H, Tan D, Dong G, Teng Y, Zhou J, et al. Large-scale preparation of strawberry-like, AgNP-doped SiO2 microspheres using the electrospraying method. Nanotechnology. 2011;22:305307. doi: 10.1088/0957-4484/22/30/305307. [DOI] [PubMed] [Google Scholar]
- 39.Midhun BT, Shalumon KT, Manzoor K, Jayakumar R, Nair SV, Deepthy M. Preparation of budesonide-loaded polycaprolactone nanobeads by electrospraying for controlled drug release. J Biomat Sci Polymer Edn 2011; 22:2431-44. [DOI] [PubMed] [Google Scholar]
- 40.Wu Y. Anthony Duong, L. James Lee, and Barbara E. Wyslouzil. Electrospray Production of Nanoparticles for Drug/Nucleic Acid Delivery. Book chapter from The Delivery of Nanoparticles. Edited by Abbass A. Hashim, ISBN 978-953-51-0615-9 (InTech publishers). [Google Scholar]
- 41.Wang M, Rutledge GC, Myerson AS, Trout BL. Production and characterization of carbamazepine nanocrystals by electrospraying for continuous pharmaceutical manufacturing. J Pharm Sci. 2012;101:1178–88. doi: 10.1002/jps.23024. [DOI] [PubMed] [Google Scholar]
- 42.Tavares Cardoso MA, Talebi M, Soares PAMH, Yurteri CU, van Ommen JR. Functionalization of lactose as a biological carrier for bovine serum albumin by electrospraying. Int J Pharm. 2011;414:1–5. doi: 10.1016/j.ijpharm.2011.04.045. [DOI] [PubMed] [Google Scholar]
- 43.Christopher JH, Pratim B. Narrow size distribution nanoparticles production by electro spray processing of ferritin. Aerosol science. 2008;39:432–40. [Google Scholar]
- 44.Trotta M, Cavalli R, Trotta C, Bussano R, Costa L. Electrospray technique for solid lipid-based particle production. Drug Dev Ind Pharm. 2010;36:431–8. doi: 10.3109/03639040903241817. [DOI] [PubMed] [Google Scholar]
- 45.Yu DG, Williams GR, Yang JH, Wang X, Yang JM, Li XY. Solid lipid nanoparticles self-assembled from electro sprayed polymer based macro particles. J Mater Chem. 2011;21:15957. doi: 10.1039/c1jm12720a. [DOI] [Google Scholar]
- 46.Meija AF, He P, Luo D, Marquez M, Cheng Z. Uniform discotic wax particles via electro spray emulsification. J coll and interface Sci. 2009;334:22–8. doi: 10.1016/j.jcis.2009.02.044. [DOI] [PubMed] [Google Scholar]
- 47.Modesto-Lopez LB, Biswas P. Role of the effective electrical conductivity of nano suspensions in the generation of TiO2 agglomerates with elctro spray. J Aerosol Sci. 2010;41:790–804. doi: 10.1016/j.jaerosci.2010.04.010. [DOI] [Google Scholar]
- 48.Lahann J. Recent progress in nano-biotechnology: compartmentalized micro- and nanoparticles via electrohydrodynamic co-jetting. Small. 2011;7:1149–56. doi: 10.1002/smll.201002002. [DOI] [PubMed] [Google Scholar]
- 49.Zhang S, Kawakami K. One-step preparation of chitosan solid nanoparticles by electrospray deposition. Int J Pharm. 2010;397:211–7. doi: 10.1016/j.ijpharm.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 50.Wu Y, MacKay JA, McDaniel JR, Chilkoti A, Clark RL. Fabrication of elastin-like polypeptide nanoparticles for drug delivery by electrospraying. Biomacromolecules. 2009;10:19–24. doi: 10.1021/bm801033f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun L, Yu X, Sun M, Wang H, Xu S, Dixon JD, et al. Preparation of quantum dots encoded microspheres by electrospray for the detection of biomolecules. J Colloid Interface Sci. 2011;358:73–80. doi: 10.1016/j.jcis.2011.02.047. [DOI] [PubMed] [Google Scholar]
- 52.Mongkoldhumrongkul N, Best S, Aarons E, Jayasinghe SN. Bio-electrospraying whole human blood: analysing cellular viability at a molecular level. J Tissue Eng Regen Med. 2009;3:562–6. doi: 10.1002/term.185. [DOI] [PubMed] [Google Scholar]
- 53.Jayasinghe SN, Eagles PAM, Qureshi AN. Electric field driven jetting: an emerging approach for processing living cells. Biotechnol J. 2006;1:86–94. doi: 10.1002/biot.200500025. [DOI] [PubMed] [Google Scholar]
- 54.Eagles PAM, Qureshi AN, Jayasinghe SN. Electrohydrodynamic jetting of mouse neuronal cells. Biochem J. 2006;394:375–8. doi: 10.1042/BJ20051838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jayasinghe SN. Bio-electrosprays: from bio-analytics to a generic tool for the health sciences. Analyst. 2011;136:878–90. doi: 10.1039/c0an00830c. [DOI] [PubMed] [Google Scholar]
- 56.Andreu N, Thomas D, Saraiva L, Ward N, Gustafsson K, Jayasinghe SN, et al. In vitro and in vivo interrogation of bio-sprayed cells. Small. 2012;8:2495–500. doi: 10.1002/smll.201200138. [DOI] [PubMed] [Google Scholar]
- 57.Sahoo S, Lee WC, Goh JC, Toh SL. Bio-electrospraying: A potentially safe technique for delivering progenitor cells. Biotechnol Bioeng. 2010;106:690–8. doi: 10.1002/bit.22734. [DOI] [PubMed] [Google Scholar]