Abstract
Purpose
Total hip arthroplasty (THA) has been efficacious for treating hip fractures in healthy older patients. However, in those patients with fractures a widely variable prevalence of dislocation has been reported, partly because of varying durations of follow up for this specific end-point. The purpose of the present study was to determine the cumulative risk of dislocation in these patients with fractures and to investigate if retentive cups decrease the risk of dislocation.
Methods
Between 2000 and 2005, 325 patients with neck fracture underwent primary THA using a retentive (325 hips) cup. The results of these 325 acetabular cups were compared to 180 THA without retentive cups performed for neck fractures in the same hospital between 1995 and 2000 by the same surgical team. The mean age of the 505 patients was 75 years (range 65–85). All patients were followed for a minimum of five years for radiographic evidence of implant failure. The patients were followed at routine intervals and were specifically queried about dislocation. The cumulative risk of dislocation and recurrent dislocation was calculated with use of the Kaplan–Meier method.
Results
For patients without retentive cups, the cumulative risk of a first-time dislocation was 5 % at one month and 12 % at one year and then rose at a constant rate of approximately 1 % every year to 16 % at five years. For patients with retentive cups, the cumulative risk of a first-time dislocation was 1 % at one month, 2 % at one year and then did not changed at five years. There were no differences in the mortality rates or in loosening rates among the treatment groups. The rate of secondary surgery was highest in the group without retentive (10 % for recurrent dislocation) compared with 1 % in the group treated with retentive cups. In absence of retentive cups, multivariate analysis revealed that the relative risk of dislocation for female patients (as compared with male patients) was 2.1 and that the relative risk for patients who were 80 years old or more (as compared with those who were less than 80 years old) was 1.5. Two underlying diagnoses occurring during follow up—cognitively impaired patients or neurologic disease—were also associated with a significantly greater risk of dislocation in absence of retentive cup. For these patients the risk was also decreased with a retentive cup.
Conclusion
With standard cups the incidence of dislocation is highest in the first year after arthroplasty and then continues at a relatively constant rate for the life of the arthroplasty. Patients at highest risk are old female patients and those with a diagnosis of neurologic disease. Retentive cups in these patients are an effective technique to prevent post-operative hip dislocation.
Introduction
The usual indications for the use of retentive or constrained components [1] are recurrent dislocations, patients with high risk of dislocation (multiple revisions), and patients with central nervous system disorders. Thus, constrained devices are usually reserved for procedures in which the likelihood of dislocation would be unacceptably high for other operative treatment. With the increased use of constrained devices, however there has also been an increased level of caution expressed regarding long-term survival of these devices, and particularly loosening. The indication of the retentive cup to prevent dislocation in total hip arthroplasty (THA) for patients with a femoral neck fracture has never been reported to our knowledge. Total hip arthroplasty when performed optimally provides the most functional outcome for elderly patients after displaced femoral neck fractures [2–4]. Total hip arthroplasty conferred superior short-term clinical results and fewer complications when compared with hemiarthroplasty in a prospectively randomized study [2] of mobile, independent patients who had sustained a displaced fracture of the femoral neck. However, in these patients with fractures a widely variable prevalence of dislocation [3, 5–7] has been reported after THA, partly because of varying durations of follow up for this specific end point. Thus, the success in achieving better clinical results with THA may be balanced by increased risk of dislocation [8].
Therefore, we compared patients with THA for femoral neck fracture treated with standard cups and with retentive cups to determine whether (1) the incidence of first-time dislocation as a function of time differed between the two groups, (2) the various types of cups (standard or retentive cups) influenced the cumulative long-term risk of dislocation, and (3) the various types of cups influenced revision.
Methods
The study design analysed the incidence of dislocation in patients with femoral neck fractures treated with arthroplasties. These elderly patients with displaced femoral neck fractures treated with arthroplasty were active, mentally competent, and independent patients. After 2000 in our hospital, these patients with neck fracture underwent primary THA using a cemented polyethylene (PE) acetabular cup and cemented femoral stem (Ceraver Osteal, Roissy, France). We compared 180 of these patients receiving THA with a standard cup (un-retentive cup) from 1995 to the end of 2000 with the 325 patients operated on immediately after this date (from 2001 to 2005) who received THA using a retentive cup (Groupe lépine, Genay, France).
The key patient demographics of the cohort study for the group with THA with un-retentive cups consisted of 180 patients (79 men, 101 women) with an average age of 77 years (range 65–85). The diagnosis was neck fracture. All patients received a cemented arthroplasty (both cup and stem) performed between 1995 and 2000 in the same hospital. The 90-day mortality in these patients undergoing retentive cup for hip fracture was 2.6 %. Twenty patients died before five years follow up. In addition, 30 of the 180 patients were lost to follow up after two years. This left 130 of the 180 patients with a follow up of five years for study, and 72 with a follow up of ten years. We examined their records at the time of their most recent follow up or before their death. The average follow up, as reported in medical records, was ten years (range, one–15 years). Surgery was performed with a posterolateral approach and general anaesthesia. The conventional acetabular component was a standard PE cemented cup. The alumina head was 32 mm in diameter and anchored through a Morse taper. The stems and cups were always the same, manufactured by Ceraver Osteal (Roissy, France), and were made of anodized titanium alloy (TiAl6V4), smooth, and always cemented. Femoral components were fixed with cement (Palacos® G; Heraeus Medical GmbH, Hanau, Germany) containing antibiotics (gentamicin).
The 325 patients in the THA group operated on immediately after this date (from 2001 to 2005) who received THA using a retentive cup consisted of 154 men and 171 women with an average age of 79 years (range, 64–90 years). All patients were operated in the same hospital. The 90-day mortality in these patients undergoing THA for hip fracture was 2.8 %. Sixty patients died before five-years follow up, and 12 of the 325 patients were lost to follow up after two years. This left 253 of the 325 patients with a minimum follow up of five years for study, and 73 with a follow up of eight years. The average follow up (as reported in medical records) was seven years (range, one–10 years). Surgery was also performed with a posterolateral approach and general anaesthesia. The cemented UHMWPE retentive cup (Groupe lépine, Genay, France) is a design incorporating a mobile ring in a more enveloping cup than the hemispheric model. The flange in the equatorial plane permits insertion of a split PE ring reinforced by a stainless steel hoop. This ring plays the role of a retentive clip (Fig. 1). On crossing the equator of the cup, the head opens the ring, which then closes through simple elasticity (Fig. 2). The alumina head was 28 mm in diameter and anchored through a Morse taper. The cups were manufactured by Ceraver Osteal (Roissy, France) and by Groupe lépine (Genay, France).
Fig. 1.
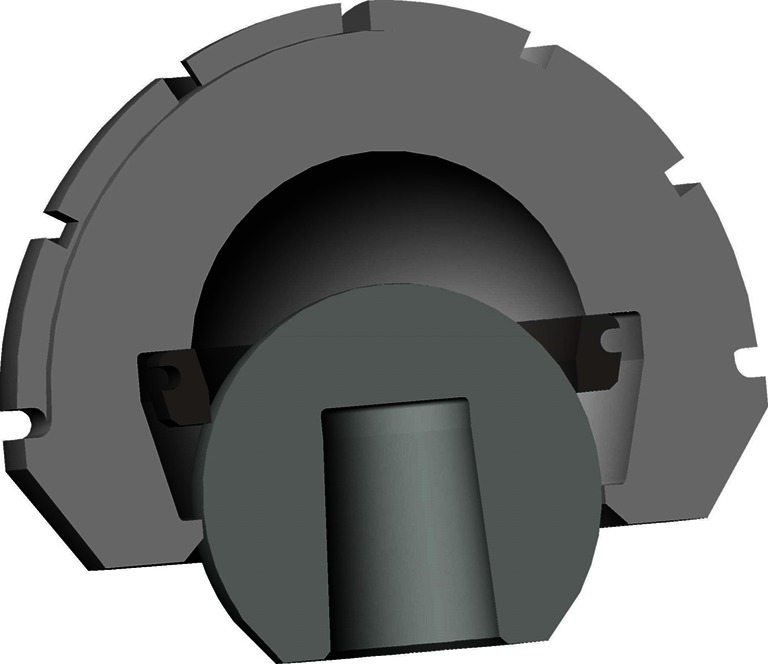
Photograph illustrating the retentive cup (Groupe lépine, Genay, France). The principle of retentiveness is obtained with a more enveloping cup than the hemispheric model. The flange in the equatorial plane permits insertion of a split PE ring reinforced by a stainless steel hoop
Fig. 2.
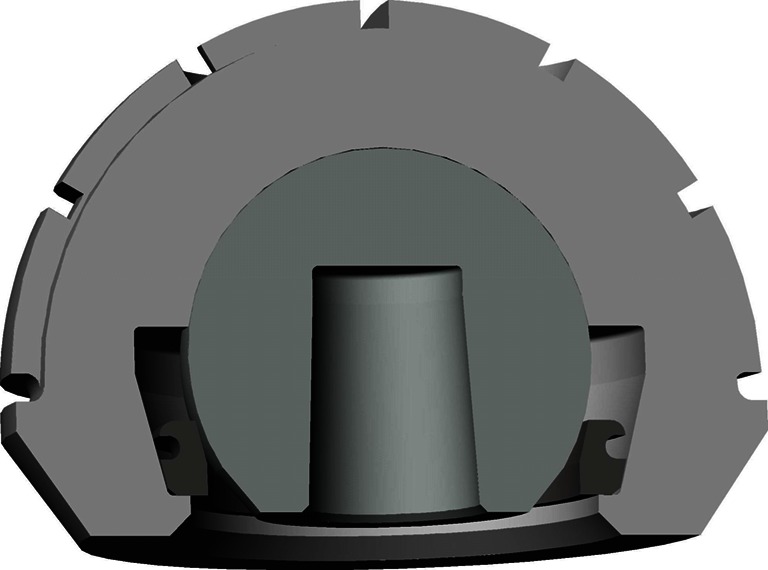
Once the head has crossed the ring, it falls below the equatorial plane. Therefore, in most situations, the cup is not really a retentive liner. Only in movements at risk for dislocation, the ring is constrained
In the postoperative rehabilitation, no patient was placed into a hip spica cast to minimize the possibility of hip dislocation. The patients were encouraged to be upright with weight bearing after surgery. Range of motion of the hip and knees was begun immediately and ambulation progressed as tolerated according to the ability of each patient (usually after 48 hours). The physiotherapy was supervised by a medical doctor for three weeks and continued for 45 days.
The follow-up routine time was at three, six, and 12 months, then annually thereafter. At each visit, patients had clinical and radiological evaluation. The usual hip rating scores do not reflect the function of THA in patients with hip fractures well because the age or medical status may affect the functional variables. The pre- and postoperative walking status of patients was graded as unable to walk, able to walk indoors only, able to walk about the community, and able to walk an unlimited distance. All patients, except eight with hip infection, subjectively exhibited improved ambulation (they were able to walk about the community, or able to walk an unlimited distance) after surgery. We took plain radiographs (AP and lateral view) every year until the most recent follow up. From the charts, we determined whether or not there were any dislocations (posterior or anterior) or revisions for recurrent dislocation, or loosening. We routinely evaluated patients, in person or by means of a standardized letter or telephone questionnaire, at two to three months postoperatively, at one, two and five years, and then at each subsequent five-year interval until revision or death. At each time point, we specifically asked patients about whether they had had dislocation of the hip. We did not consider a sensation of subluxation of the hip to be sufficiently specific to represent an episode of hip instability, and only considered a complete hip dislocation requiring reduction to be a dislocation event.
Plain radiographs (AP and lateral view) were taken to assess loosening of the cup for THA every year until the most recent follow up. We had all postoperative radiographs immediately available. We determined loosening on all films. Absence of loosening of the socket was defined as no cup migration exceeding 5 mm, no angular rotation exceeding 5°, and no continuous radiolucent line wider than 2 mm [9] when comparing the immediate postoperative films to those at last follow up.
Qualitative data (i.e., gender) were expressed as counts and percentages within groups and quantitative data by mean ± standard deviation or range. Qualitative data between the two groups were compared with use of the chi-square test or Fisher’s exact test, and quantitative data (postoperative acetabular abduction angle) with the Mann–Whitney test. Kaplan–Meier survivorship analysis [10], with 95 % confidence intervals, was used to estimate the cumulative probability of not having a dislocation in the whole series. Differences in survival were determined using the log-rank test. The cumulative risk of dislocation as reported by Berry et al. [11] was estimated using the Kaplan–Meier method [10]. Kaplan–Meier survivorship analysis was performed with revision due to recurrent dislocation, or loosening as the end point.
Results
The incidence of first-time dislocation was lower in the group with a retentive (325 hips) cup and occurred in a shorter period after surgery. Seven (2 %) of the 325 hips treated with retentive cup were known to have had at least one dislocation. Four dislocations occurred within 30 days after total hip arthroplasty, two occurred 67 to 180 days after arthroplasty, and none occurred more than one year after arthroplasty. When treated with THA without retentive cups, 20 (12 %) of the 180 hips were known to have had at least one dislocation. Seven first-time (4 %) dislocations occurred within 60 days after arthroplasty, six occurred two months to 12 months after arthroplasty, four occurred one to three years after arthroplasty, and three occurred more than four years after arthroplasty.
Recurrent hip dislocation and the cumulative risk of dislocation were higher with THA without retentive cup. Six patients (six hips) treated with THA without retentive cup had recurrent hip dislocation: five patients had two recurrent hip dislocations, one patient had three, and one had four recurrent dislocations. Therefore the cumulative number of dislocations (both first time and recurrent dislocation) for patients treated with 180 THAs was 30 (16 %) at the most recent follow up. For these patients without retentive cups, the cumulative risk of a first-time dislocation was 5 % at one month and 12 % at one year and then rose at a constant rate of approximately 1 % every year to 16 % at five years. In the group of patients with a retentive cup, at five-year follow up the incidence of recurrent dislocation was lower (one patient with recurrent dislocations two times among 325 hips) than in the patients with a THA. For patients with retentive cups, the cumulative risk of a first-time dislocation was 1 % at one month, 2 % at one year and then did not change at five years.
The rate of secondary surgery was highest in the group without retentive (10 % for recurrent dislocation) compared with 1 % in the group treated with retentive cups. In absence of retentive cup, multivariate analysis revealed that the relative risk of dislocation for female patients (as compared with male patients) was 2.1 and that the relative risk for patients who were 80 years old or more (as compared with those who were less than 80 years old) was 1.5. Two underlying diagnoses occurring during follow up—cognitively impaired patients or neurologic disease—were also associated with a significantly greater risk of dislocation in patients without retentive cups.
The incidence of loosening was not increased with the retentive cup. In the group of patients without retentive cup (standard cup, Ceraver) for hips had revision for loosening of the cup. In the group with retentive cup (Groupe lépine), only two loosenings were observed and had revision at seven years’ follow up. At the most recent follow up, there was no progressive radiolucent line or osteolytic lesions observed that could be determined radiographically about the acetabular component or proximal femur. The survival rate was 100 % at five years and 99 % at seven years with revision due to loosening of the retentive cup as the end point, compared with 95 % at five years and 91 % at seven years in the un-retentive group.
Discussion
Total hip replacement has not been a popular treatment choice for displaced intracapsular hip fractures in the past. Many patients who sustain this injury are not natural choices for THA, e.g. most are elderly, with limited mobility and many have some degree of cognitive impairment. In addition to these considerations, the initial experience with THA for intracapsular fractures was not very encouraging; high rates of dislocation were features in some early reports. However, there is now an accumulating body of evidence that supports the use of THA in suitable patients, and some recent trials have indicated that the functional outcome may be more favourable than other procedures, particularly hemiarthroplasty or osteosynthesis. Despite a general suggestion that there is a higher rate of dislocation and recurrent dislocation in patients treated with THA [11–14] as compared with hemiarthroplasty, there is very little literature about the frequency of this problem and about the long-term risk of dislocation after primary THA. Although it has become clear that there is markedly decreased dislocation when retentive cups for the treatment of recurrent dislocation in THA as compared with other solutions [15], to our knowledge no analysis has been conducted using retentive cup to prevent dislocation in total hip arthroplasty for patients with a femoral neck fracture. We therefore evaluated if the risk of dislocation was decreased when a retentive cup was used for these patients.
Several limitations must be considered when interpreting the presented data. First, ours was a retrospective study of a nonrandomized patient population. Second, the two different procedures were performed at two different periods of time, although the surgeons were the same and attempted to keep the same approaches and same perioperative treatments. Third, some patients were lost to follow up during this study; others died. At least the head size used in the different groups was different—hemiarthroplasties with large femoral heads or 32-mm diameter heads in the unconstrained group, and 28-mm diameter heads in the group with retentive cups; however, this difference is not really a problem since the 28-mm diameter heads are perhaps a little more prone to dislocation. It is also possible that some patients had unknown dislocation treated in another hospital and not related this because of the status of cognitively impaired patients [16] when they became older.
The present study demonstrates that after total hip arthroplasty there is a higher initial level risk of first-time dislocation that increases infinitively with time, and that after retentive cup this risk of first-time dislocation is lower and decreases after six months; thus, the longer patients are followed, the greater the cumulative risk for THA as compared with retentive cup in the treatment of fractures. Our cumulative risk of dislocation for patients with THAs is higher than expected. This may be explained by the fact that most studies of THA for femoral neck fracture have relatively short follow-up periods, often for only two years. Hip dislocation rates in two recent randomized studies [3, 12] were 2 and 4 %, but with only two- and four-years follow up. Follow up duration is important as the risk of dislocation is not constant but cumulative. A multivariate analysis reporting the effects of demographics on the long-term risk of dislocation as a function of time for the Charnley hip replacement [11] reported a cumulative risk much greater than the early short-term reports, with a 1 % risk at one month postoperatively, 1.9 % at one year postoperatively, a constant 1 % increase every five years, and a 7 % increase at 25 years. The prevalence of redislocation after nonoperative management is another variable, with 33 % a commonly reported figure [17]. Our data are consistent with this observation.
Our findings (decreased risk for dislocation) are supported by those of other large series for other indications [1]. From review of the literature, there is evidence that the retentive cup is successful in providing stability in patients. These findings have consequences concerning the treatment of hip fractures with arthroplasties. The type of arthroplasty should be different according to the age and the activity of the patient treated for hip fracture. Cognitive dysfunctions from confusion, dementia and psychosis are reported as risk factors for hip instability. Neuromuscular dysfunction has a positive association with dislocation. Therefore when hip fracture occurs these patients should be treated with a retentive cup.
Our finding of nearly an absence of loosening (only two cases) for the retentive cup is lower than that reported in other studies [1] with retentive cups. However, comparisons of loosening rates between different retentive (cementless or cemented) components should be made cautiously, since patient populations may not be similar. Our low rate of loosening may also be related to the designs of the implant. Since once the head has crossed the ring it falls below the equatorial plane and the clip is no longer retentive, and then the cup works conventionally except in extreme movements. This retentive cup prevents dislocation as reported by dual mobility implants [18, 19].
References
- 1.Williams JT, Jr, Ragland PS, Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop. 2007;31:273–277. doi: 10.1007/s00264-006-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker RP, Squires B, Gargan MF, Bannister GD. Total hip arthroplasty and retentive liner or in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a randomized controlled trial. J Bone Joint Surg Am. 2006;88A:2583–2589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 3.Blumfeldt R, Tornkvist H, Ponzer S, et al. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures: randomized controlled trial performed at four years. J Bone Joint Surg Am. 2005;87A:1680–1688. doi: 10.2106/JBJS.D.02655. [DOI] [PubMed] [Google Scholar]
- 4.Macaulay W, Pagnotto MR, Iorio R, et al. Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:287–293. doi: 10.5435/00124635-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Lee BP, Berry DJ, Harmsen WS, et al. Total hip arthroplasty for the treatment of an acute fracture of the femoral neck: long-term results. J Bone Joint Surg Am. 1998;80:70–75. doi: 10.1302/0301-620X.80B1.7268. [DOI] [PubMed] [Google Scholar]
- 6.Mabry TM, Prpa B, Haidukewych GJ, et al. Long-term results of total hip arthroplasty for femoral neck fracture nonunion. J Bone Joint Surg Am. 2004;86:2263–2267. doi: 10.2106/00004623-200410000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Tarasevicius S, Jermolajevas V, Tarasevicius R, et al. Total hip replacement for the treatment of femoral neck fractures. Long-term results. Medicina (Kaunas) 2005;41:465–469. [PubMed] [Google Scholar]
- 8.Parvizi J, Morrey BF. Bipolar hip arthroplasty as a salvage treatment for instability of the hip. J Bone Joint Surg Am. 2000;82:1132–1139. doi: 10.2106/00004623-200008000-00010. [DOI] [PubMed] [Google Scholar]
- 9.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;121:20–32. [PubMed] [Google Scholar]
- 10.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 11.Berry DJ, Von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Keating JF, Grant A, Masson M, et al. Randomized comparison of reduction and fixation, bipolar retentive liner or dual mobility, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 13.Tidermark J, Ponzer S, Svensson O, et al. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly: a randomized controlled trial. J Bone Joint Surg. 2003;85B:380–388. doi: 10.1302/0301-620X.85B3.13609. [DOI] [PubMed] [Google Scholar]
- 14.van Vugt AB, Oosterwijk WM, Goris RJ. Osteosynthesis versus endoprosthesis in the treatment of unstable intracapsular hip fractures in the elderly. A randomised clinical trial. Arch Orthop Trauma Surg. 1993;113:39–45. doi: 10.1007/BF00440593. [DOI] [PubMed] [Google Scholar]
- 15.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed] [Google Scholar]
- 16.Hernigou P, Filippini P, Flouzat-Lachaniette CH, Batista SU, Poignard A. Constrained liner in neurologic or cognitively impaired patients undergoing primary THA. Clin Orthop Relat Res. 2010;468(12):3255–3262. doi: 10.1007/s11999-010-1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meek RMD, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 18.Bosker BH, Ettema HB, Verheyen CC, Castelein RM. Acetabular augmentation ring for recurrent dislocation of total hip arthroplasty: 60 % stability rate after an average follow-up of 74 months. Int Orthop. 2009;33(1):49–52. doi: 10.1007/s00264-007-0456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33(4):927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


