Introduction
Operating rooms can be dangerous places as harm to both patients and operators can occur in many different ways. Although most people understand that patients in operating rooms undergo risky, highly complex, and potentially life-threatening procedures, they seem much less aware that operating rooms have many potentially harmful energy devices used by anesthesiologists, surgeons, and nurses. Malfunction or misapplication of these devices can endanger the well-being of both the patient and the operator.
Anesthesiologists and nurses have been aware of this possibility for many decades. In 1979 Chambers and Saha reported a cardiac arrest due to electrocution in a young patient undergoing laparotomy (1). The patient died because of a faulty electrical switch in the operating table. An EKG monitor with a direct earth ground created an electrical circuit that included the patient and resulted in the electrocution. Although this design has been abandoned in favor of isolated electrical systems, and every electrical device in the operating room must comply with numerous safety requirements, injuries from electrical devices continue to occur. As recently as 2010 Wills et al. reported a case of electroshock injury to a nurse in a modern operating room.(2) These few publications helped create awareness and have led to safer standards and technologies for the typical electrical systems used in operating rooms, including EKG machines, anesthesia monitors, operating room tables, electrical outlets and switches. These publications also appear to be have been largely ignored by surgeons who relied on their anesthesia colleagues and allied health personnel to address them. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has developed the “Fundamental Use of Surgical Energy™” (FUSE) program to address this knowledge gap and contribute to a safer operating room environment.
The “Fundamental Use of Surgical Energy” Program – FUSE
Historical perspective and creation of the concept:
Devices that apply energy to tissue therapeutically have been in use for millennia. Cautery, the direct application of heat to tissue, has been in use since 3000 BC to destroy tumors and achieve hemostasis (3). At the beginning of the 20th century William T Bovie invented an instrument in which high-frequency alternating current (radiofrequency electrosurgery) was used to achieve effects similar to a knife, but in addition could coagulate tissue while cutting through it. (4) It was introduced into surgical practice by Harvey W Cushing and remains the most widely used energy-based device today with very little modification of its basic principles. In the 1940’s, bipolar devices were introduced, with innovations such as the incorporation of cutting blades and real-time impedance measurement into bipolar instruments appearing over the next few decades.
After this relatively slow pace of innovation, the last two decades have seen an explosion in the type and availability of energy devices used by physicians of all specialties. Fueled by the minimally invasive “revolution” which required new devices for tissue dissection and efficient control of larger vessels without suturing, there is now a vast array of devices that apply energy to tissues in clinical use throughout the world across all surgical specialties and operative approaches - open, laparoscopic, robotic and endoscopic. These devices use a variety of energy sources: electric current at radiofrequency wave-length, mechanical energy at ultrasonic wave-length and microwave energy. Without question these technical innovations have enabled the advances in minimally invasive surgery, endoscopic interventional techniques and percutaneous approaches to diseases that have greatly enhanced our ability to treat patients. However, this technological boon has also created a dizzying multitude of energy device platforms, configurations, generators, cost points and vendors, and this complexity has increased the potential for injury.
Today’s surgeon encounters complex energy systems to be used after a short introduction by a specific vendor without any incentive or need to understand the fundamental principles of function and safety of the device. Clearly, there is a need for an educational program to address this gap. With the rapid increase in number, types, and forms of energy applications to tissue, the wide variety of indications and devices and the complex environment in which they are used, the risk for complications and harm to both to patients and operators has become part of daily practice.
Injury and harm from electrosurgical devices in laparoscopic surgery is estimated to occur at a rate of 1-2 per 1000 patients. (5) These complications include unrecognized bowel injuries and major vascular injuries.(6,7) Although vascular injuries declare themselves through the presence of unexpected bleeding, unrecognized thermal injuries to the intestine during laparoscopic surgery are difficult to detect and therefore particularly dangerous, with a significant associated mortality.(8,9)
Over 600 operating fires occur each year in the United States with 2-3 mortalities each year.(11) These injuries are potentially preventable and most of them are associated with the use of surgical energy devices. In over 90% the reported ignition source is an electrosurgical device. As a proportion of all surgical claims, those related to fires have increased from less than 1% of all surgical claims during 1985-1989 to 4.4% between the 2000 and 2009, representing a greater then 5-fold increase.(10) The scope of harm from fires and thermal injuries is comparable to more publicized safety issues like retained foreign objects (0.7-1 per 1000 abdominal operations) and wrong-site surgery (1 in 9000 cases) (12,13)
In response to this safety issue, individual surgeons, health care professionals and surgical societies both nationally and internationally have tried to increase our understanding of the fundamental properties of electrosurgical instruments. (14,15,16,17,18) These pioneers raised awareness of the specific complications associated with electrosurgical devices and the risks involved in their use, particularly in laparoscopy. This early work included a survey sponsored by the American College of Surgeons to assess the complication rate associated with the use of electrosurgical devices, showing that the majority of respondents reported inappropriately high power settings when using electrosurgical instruments (19). In 1998, the Society of Laparoendoscopic Surgery publicized the need for better education of surgeons on the safe use of laparoscopic monopolar electrosurgical devices. (20) Similarly, the Association of periOperative Registered Nurses (AORN) has published recommendations on the safe use of energy devices in electrosurgery, but without a comprehensive review of all devices and without an assessment component. (21)
Despite these early attempts to make surgeons aware of the potential threat from energy devices used every day in the operating room, the general understanding among surgeons about the correct use and inherent dangers of energy devices has remained very poor. Compared to anesthesia and nursing textbooks, standard surgical textbooks provide little relevant information. Training on new energy devices is not standardized, with almost all training on a particular device delivered by a sales representative or an industry sponsored course. In preparation for a postgraduate course addressing surgical energy devices given at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) in 2011, a pretest consisting of 11 multiple-choice questions was given to 48 society leaders. The pretest included items addressing fundamental principles of electrosurgery as well as safety issues with a variety of energy-based devices. On initial administration of the test the median number of correct answers was 6.5 or 59%. The range of correct answers was 3 to 11. Thirty-one percent of the participants did not know how to handle an operating room fire involving a patient; 31% could not identify the energy device least likely to interfere with a pacemaker; 13 % did not know about thermal spread of bipolar instruments; and 10% would have cut a dispersive electrode (return pad) to fit a child. (22) Only 35% knew the correct nomenclature for electrosurgical device function and only 20% were able to describe the generator output. When surveyed, few surgeons consider themselves “expert” on the energy-based devices they use every day, and the most common source of knowledge about these devices (42%) came from industry sales representatives or an industry-sponsored course. (23) These results suggest that surgeons in practice may have a relatively poor understanding of the potential safety issues of commonly used surgical energy devices and that training has been provided mostly by industry.
In summary, multiple factors have coalesced in the field of energy-based surgical devices, including the laparoscopic revolution, the rapid expansion of surgical energy technologies and the identification of operating room fires as an important safety issue. Where will the training to master these devices come from? Who will create a curriculum covering their functioning and safety profiles? How should we offer appropriate training and certification? What is the standard procedure when a surgeon or a nurse is suddenly faced with unfamiliar equipment? How will we mandate and pay for fire safety training? Should there be a standard approach for how energy devices get introduced into the hands of surgeons? Who will create these standards? A nationwide, non-industry, multidisciplinary educational program with validated assessment in surgical energy–based devices could address this knowledge and certifications gap and potentially contribute to a safer operating room environment. (24)
The FUSE educational curriculum and certification
In October 2010, SAGES created the FUSE (Fundamental Use of Surgical Energy) program to address this gap (Figure 1). Working in partnership with AORN, AAGL (American Association of Gynecologic Laparoscopists), and the AUA (American Urologic Association), the FUSE task force includes general surgeons with a variety of subspecialty practices, nurses, anesthesiologists, engineers, and gynecologists. As with the two other SAGES “Fundamentals” programs (FLS, or Fundamentals of Laparoscopic Surgery™, and FES, or Fundamentals of Endoscopic Surgery™), FUSE includes two components: a standardized curriculum for surgeons and allied health care professionals of all specialties, and a certification test that meets high psychometric and accreditation standards. Success on the test will result in FUSE certification, documenting the basic knowledge that underlies the safe use of energy-based devices in the operating room.
Figure 1.
Fundamental Use of Surgical Energy – FUSE Program Logo (copyright with SAGES)
The FUSE curriculum content was first delivered as a postgraduate course at the SAGES meeting in 2011 and 2012. The material was expanded into a textbook on surgical energy and safety (The FUSE manual), published in 2012 (25) and an online multimedia curriculum completed in late 2012.
The curriculum includes 10 sections:
Fundamentals of electrosurgery
Mechanisms and prevention of adverse events with electrosurgery
Monopolar devices
Bipolar devices
Radiofrequency for soft tissue ablation
Endoscopic devices
Ultrasonic energy systems
Microwave energy systems
Energy-based devices in pediatric surgery
Integration of energy systems with other medical devices
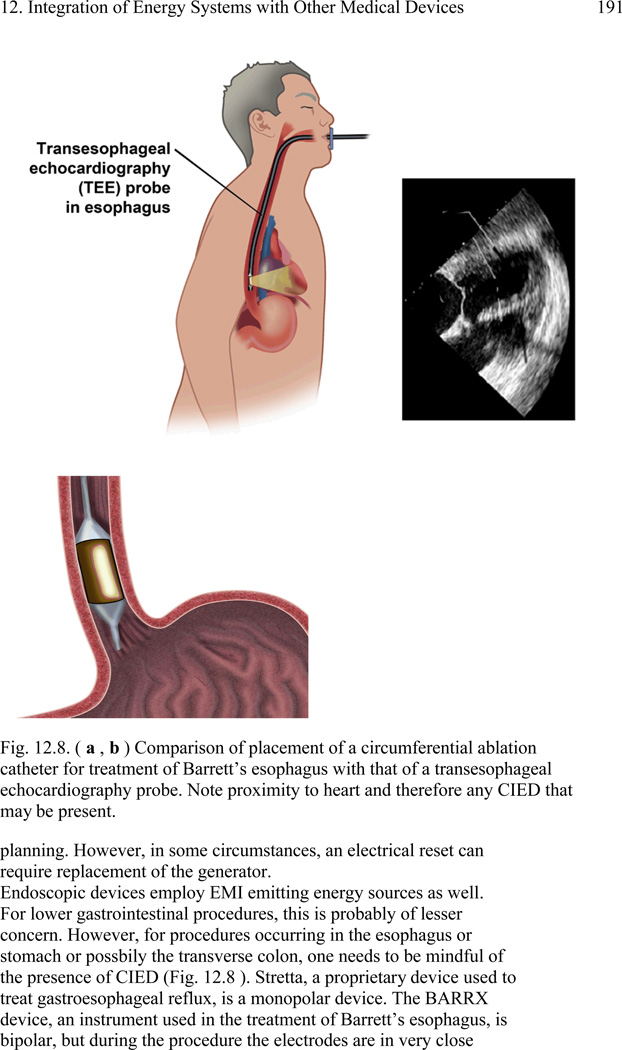
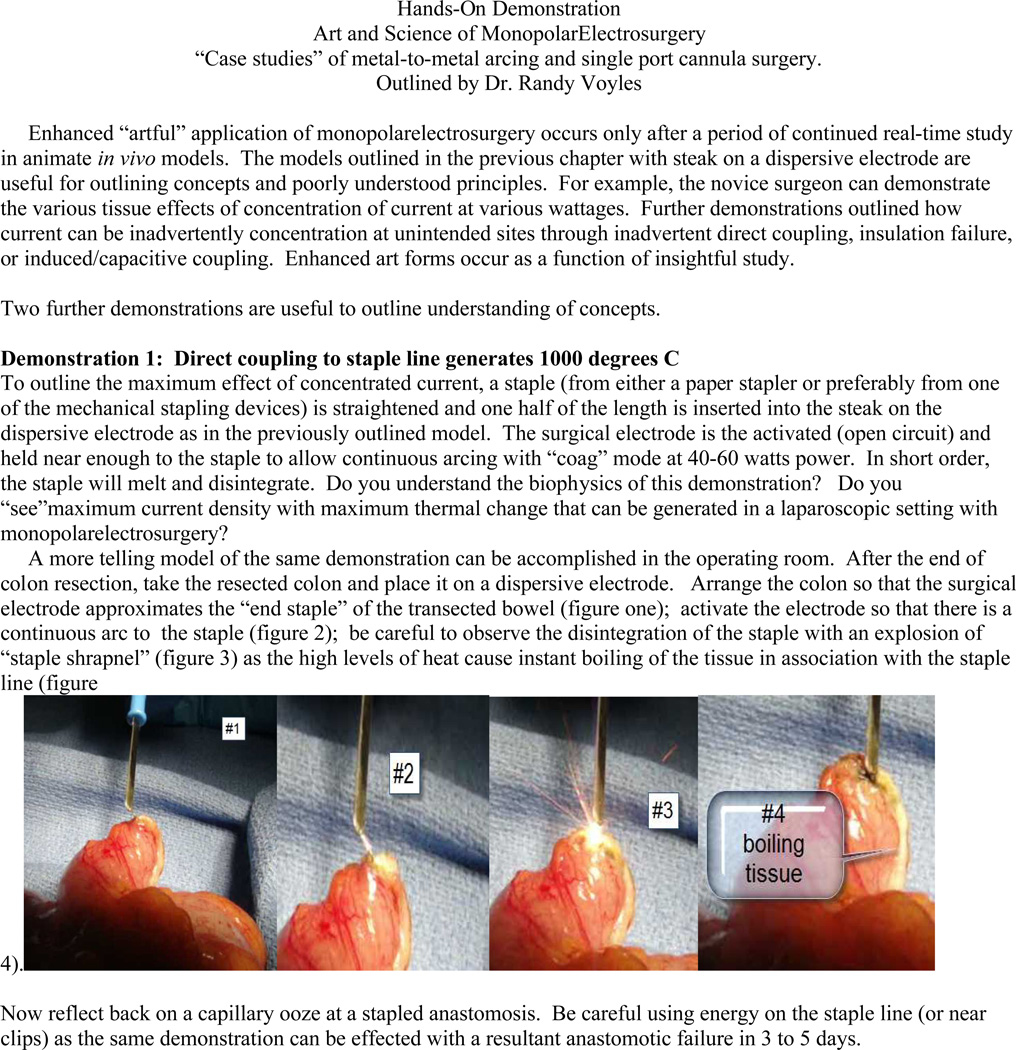
The content focuses on the fundamental principles required for safe and effective use of devices. For example, section 1, Fundamentals of Electrosurgery, includes the types of currents used, correct nomenclature, explanation of physics such as Ohm’s law as it is applied to electrosurgery, electrosurgical generators, differences in “coag” and “cut” waveforms, monopolar versus bipolar systems, isolated versus ground-referenced systems, active and dispersive electrodes, physical effects of temperature and alternating current on cells and tissue, resistive heating, and the different tissue effects (desiccation versus coagulation versus fulguration). Section two focuses on the safe use of electrosurgical devices, including direct and capacitive coupling, insulation failure, and prevention and response to operating room fires. A similar emphasis on fundamental principles and safe application is used in the sections on specific devices, including monopolar, bipolar, radiofrequency ablation, microwave and endoscopic devices. Additional sections deal with the special considerations for use of energy devices in pediatric patients and when used in patients carrying other medical devices such as pacemakers. For illustration, Figure 2 shows a page of the “Integration of energy systems with other medical devices” chapter of the FUSE Manual. The manual contains supplemental “Hands-On” chapters describing how to set up “live” stations for demonstration and teaching surgical energy principles and safe practice. Figure 3 shows an example of a FUSE manual hands-on chapter. The online curriculum includes the essential content of the FUSE Manual in an electronic multimedia self-assessment format with multiple choice test questions eligible for CME and CEU. An example of a “page” from the online curriculum is shown in Figure 4.
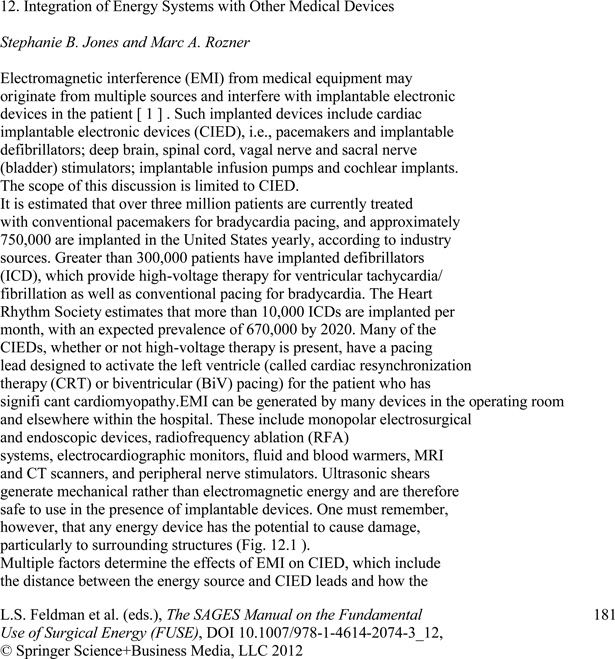
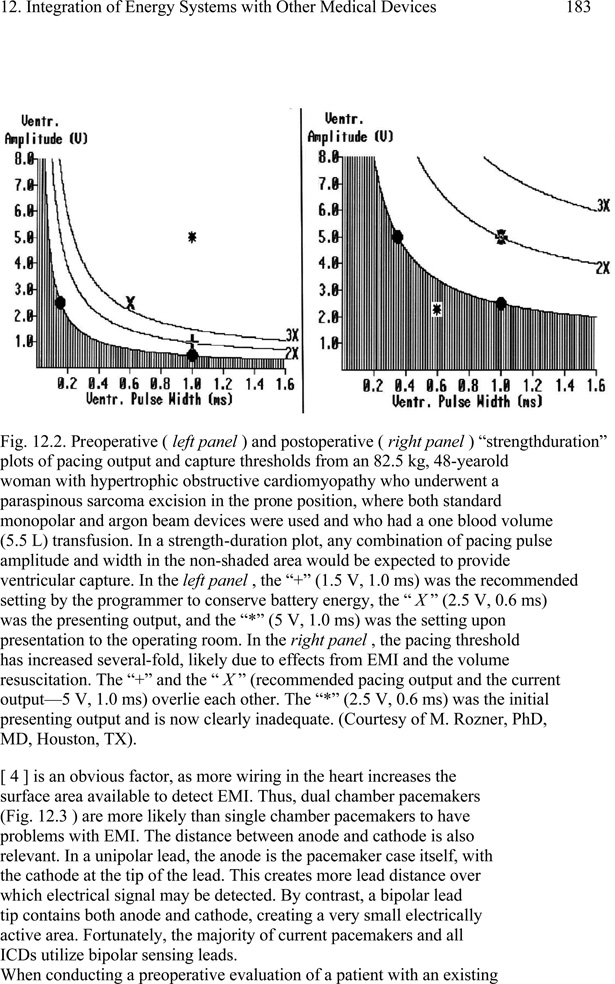
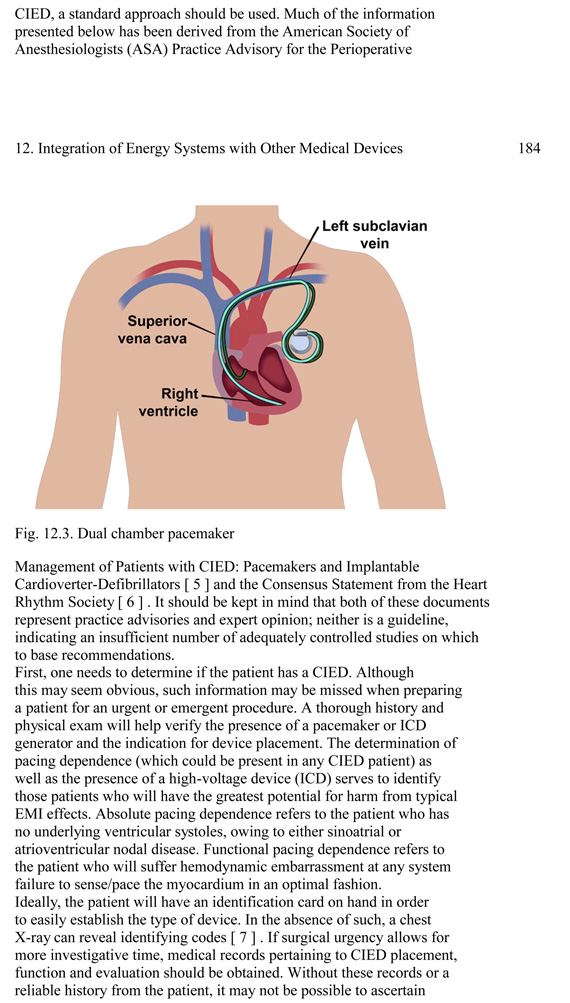
Figure 2.
Page examples of the FUSE manual, chapter “Integration of Energy Systems With Other Medical Devices” (24)
Figure 3.
Examples of the FUSE manual Hands-On Demonstration chapter (24)
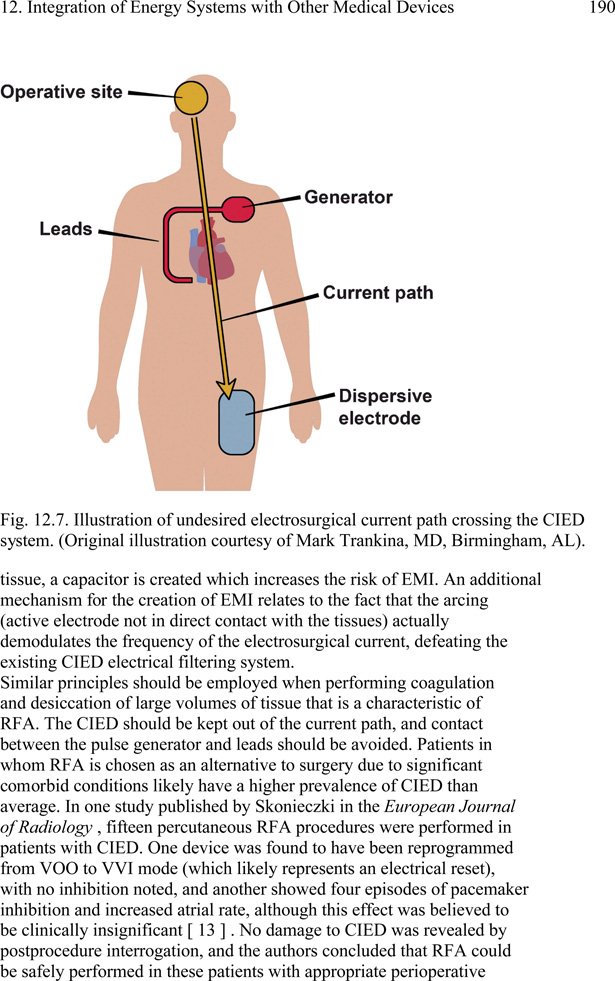
Figure 4.
Screenshot of the FUSE online program
Successful completion of the FUSE program, including assessment, will lead to certification. SAGES is following a test development process that complies with the legal and technical requirements for professional certification. This included a “job task analysis” where psychometricians lead 15 FUSE content experts in a systematic process to define the competencies required to use energy devices safely. The results describe the breadth and depth of knowledge and skills that must be covered by the certification exam in order for it to be deemed valid, reliable, and legally defensible. This was used to create test objectives for the exam. For each section of the curriculum, between 2 and 20 objectives were identified, for a total of 63 objectives. For example, for Section 1, “Fundamentals of Electrosurgery”, objectives include “Identify the function (input and output) of an electrosurgical (RF) generator“ and “Identify how radiofrequency electrical energy causes effects in cells and tissue”. For section 2 “Mechanisms and Prevention of Adverse Events with Electrosurgery”, objectives include “Identify circumstances, mechanisms, and prevention of dispersive electrodes-related injury” and “Identify circumstances which promote OR fires and identify prevention strategies”. Test objectives help ensure that the knowledge measured by the exam is the same knowledge that is required for safe practice in the operating room. SAGES leaders, along with selected members of AORN and AAGL, participated in development of the test blueprint by ranking each objective and by determining the number of test items to be written. Competencies that emphasize the fundamental principles of energy devices, their electrosurgical safety and the integration of energy systems with other devices were viewed as most important for the FUSE assessment. Beta testing of the program and assessment are underway and will serve as the basis for any revisions of the certification exam and to determine the passing score range. The final program including the online curriculum and certification is expected to be launched in late 2013.
Summary
The Fundamental Use of Surgical Energy program by SAGES has multiple components: a comprehensive educational curriculum on the principles and safety of surgical and endoscopic energy devices available as a postgraduate course, a comprehensive manual and an online multimedia CME approved program; and a psychometrically sound high-stakes examination for physicians that can be used for maintenance of certification. Future developments of the FUSE program will include specific modules tailored to individual energy devices. These modules will be developed in collaboration with industry to provide standardized education for the safe and appropriate use of current and new energy devices. This will ensure that FUSE continues on its mission to fill the unmet curricular, regulatory, safety and competency assessment needs that exist for the use of energy devices in patients by surgeons, endoscopists, anesthesiologists and nurses.
Table 1.
Example of educational objectives used to develop online curriculum and certification exam
| FUSE Blueprint | |
| Final - September 1, 2011 | |
| 1 | Fundamentals of Electrosurgery |
| 1.1 | Define proper electrosurgery terms. |
| 1.2 | Given a clinical situation, identify the application of Ohms law, power equation, and energy. |
| 1.3 | Identify the function (input and output) of an electrosurgical (RF) generator. |
| 1.4 | Identify the characteristics of monopolar and bipolar instruments and the differences between them. |
| 1.5 | Identify the characteristics of the RF electromagnetic spectrum and why it is used for surgical applications. |
| 1.6 | Identify how RF electrical energy causes effects in cells and tissue. |
| 1.7 | Identify the different effects of ranges of temperature on cells and tissue. |
| 2 | Mechanisms and Prevention of Adverse Events with Electrosurgery |
| 2.1 | Identify general patient protection measures for setup and settings for the electrosurgical unit. |
| 2.2 | Identify various mechanisms whereby electrosurgical injuries may occur. |
| 2.3 | Identify circumstances, mechanisms, and prevention of dispersive electrodes-related injury. |
Acknowledgements
The authors would like to thank Jessica Mischna, Sallie Matthews, Brenda Castaneda, Carla Bryant from the SAGES headquarters for their invaluable support of the FUSE project and the members of the FUSE task force Sharon L Bachman MD, L. Michael Brunt MD, James Choi MD, Suvranu De Sc.D., Brian J Dunkin MD, Warren Grundfest MD, Charlotte Gugliemi RN, Jeffrey W Hazey MD, Scott Helton MD, Daniel M Herron MD, David Iannitti MD, Gretchen Purcell Jackson MD, Jarrod Kaufman MD, Leena Khaitan MD, Dean J Mikami MD, William S Richardson MD, Thomas N Robinson MD, Daniel J Scott MD, Victoria J Steelman PhD, Thadeus L Trus MD, C Randy Voyles MD and Eelco Wassenaar MD.
The FUSE project is funded by unrestricted educational grants to SAGES. The authors derive no financial benefit from this project. All Authors are members of the FUSE Task Force within SAGES.
Contributor Information
Pascal Fuchshuber, Hepatobiliary and Oncologic Surgery, The Permanente Medical Group, Inc., Walnut Creek , CA , USA.
Stephanie Jones, Department of Anesthesia, Critical Care and Pain Medicine, Beth Israel Deaconess Medical Center, Boston , MA , USA.
Daniel Jones, Harvard Medical School Beth Israel Deaconess Medical Center, Boston, MA, USA.
Liane S Feldman, McGill University Health Centre, Montreal, QC, Canada.
Steven Schwaitzberg, Department of Surgery, Cambridge Health Alliance, Harvard Medical School, Cambridge , MA , USA.
Mark Rozner, Department of Anesthesiology and Perioperative Medicine, Department of Cardiology, The University of Texas MD Anderson Cancer Center, Houston , TX , USA.
REFERENCES
- 1.Chambers JJ, Saha AK. Electrocution during anesthesia. Anesthesia. 1979 Feb;34(2):173–175. doi: 10.1111/j.1365-2044.1979.tb06273.x. [DOI] [PubMed] [Google Scholar]
- 2.Wills John H, FANZCA Jan Ehrenwerth, MD, Rogers Dan., MD Electrical Injury to a Nurse Due to Conductive Fluid in an Operating Room Designated as a Dry Location. Anesth Analg. 2010;110:1647–1649. doi: 10.1213/ane.0b013e3181a89627. [DOI] [PubMed] [Google Scholar]
- 3.Schwaitzberg SD. Evolution and revolutions in surgical energy. In: Feldman LS, Fuchshuber P, Jones DB, editors. The fundamental use of surgical energy (FUSE) manual. New York: Springer; p. 3. [Google Scholar]
- 4.O’Connor JL, Bloom DA, William T. Bovie and electrosurgery. Surgery. 1996;119(4):390–396. doi: 10.1016/s0039-6060(96)80137-1. [DOI] [PubMed] [Google Scholar]
- 5.Schwaitzberg SD. Evolution and revolutions in surgical energy. In: Feldman LS, Fuchshuber P, Jones DB, editors. The fundamental use of surgical energy (FUSE) manual. New York: Springer; p. 3. [Google Scholar]
- 6.Nduka CC, Super PA, Monson JR, Darzi AW. Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg. 1994 Aug;179(2):161–170. [PubMed] [Google Scholar]
- 7.Cormier B, Nezhat F, Sternchos J, Sonoda Y, Leitao MM., Jr Electrocautery-associated vascular injury during robotic-assisted surgery. Obstet Gynecol. 2012 Aug;120(2 Pt 2):491–493. doi: 10.1097/AOG.0b013e31825a6f60. [DOI] [PubMed] [Google Scholar]
- 8.LeBlanc KA, Elieson MJ, Corder JM., 3rd Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. JSLS. 2007 Oct-Dec;11(4):408–414. [PMC free article] [PubMed] [Google Scholar]
- 9.Bishoff JT, Allaf ME, Kirkels W, Moore RG, Kavoussi LR, Schroder F. Laparoscopic bowel injury: incidence and clinical presentation. J Urol. 1999;161(3):887. doi: 10.1016/s0022-5347(01)61797-x. [DOI] [PubMed] [Google Scholar]
- 10.Mehta SP, Bhananker SM, Posner KL, Domino KB. Operating room fires: a closed claims analysis. Anesthesiology. 2013 May;118(5):1133–1139. doi: 10.1097/ALN.0b013e31828afa7b. [DOI] [PubMed] [Google Scholar]
- 11. [Accessed 5/17/13];Preventing Fires in the Operating Room FDA Patient Safety News: Show #105. 2010 Dec; http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/printercfm?id=1460.
- 12.Hyslop JW, Maull KI. Natural history of the retained surgical sponge. South Med J. 1982;75:657–660. doi: 10.1097/00007611-198206000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Kwaan MR, Studdert DM, et al. Incidence, patterns, and prevention of wrong-site surgery. Arch Surg. 2006;141:353–358. doi: 10.1001/archsurg.141.4.353. [DOI] [PubMed] [Google Scholar]
- 14.Voyles CR, Tucker RD. Education and engineering solutions for potential problems with laparoscopic monopolar electrosurgery. Am J Surg. 1992 Jul;164(1):57–62. doi: 10.1016/s0002-9610(05)80648-8. [DOI] [PubMed] [Google Scholar]
- 15.Tucker RD, Voyles CR. Laparoscopic electrosurgical complications and their prevention. AORN J. 1995 Jul;62(1):51–53. 55. doi: 10.1016/s0001-2092(06)63683-1. 58-9 passim; quiz 74-7. [DOI] [PubMed] [Google Scholar]
- 16.Harrell GJ, Kopps DR. Minimizing patient risk during laparoscopic electrosurgery. AORN J. 1998 Jun;67(6):1194–1196. 1199–1205. doi: 10.1016/s0001-2092(06)62606-9. quiz 1206-10. [DOI] [PubMed] [Google Scholar]
- 17.Wu MP, Ou CS, Chen SL, Yen EY, Rowbotham R. Complications and recommended practices for electrosurgery in laparoscopy. Am J Surg. 2000 Jan;179(1):67–73. doi: 10.1016/s0002-9610(99)00267-6. [DOI] [PubMed] [Google Scholar]
- 18.Alkatout I, Schollmeyer T, Hawaldar NA, Sharma N, Mettler L. Principles and safety measures of electrosurgery in laparoscopy. JSLS. 2012 Jan-Mar;16(1):130–139. doi: 10.4293/108680812X13291597716348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tucker RD. Laparoscopic electrosurgical injuries: survey results and their implications. Surg Laparosc Endosc. 1995 Aug;5(4):311–317. [PubMed] [Google Scholar]
- 20.Brill AI, Feste JR, Hamilton TL, Tsarouhas AP, Berglund SR, Petelin JB, Perantinides PG, et al. Patient safety during laparoscopic monopolar electrosurgery--principles and guidelines. Consortium on electrosurgical safety during laparoscopy. Journal of Society of Laparoscopic Surgeons. 1998;2(3):221–225. [PMC free article] [PubMed] [Google Scholar]
- 21.Recommended practices for electrosurgery. AORN Journal. 2005;81(3):616–618. 621–626, 629–632. doi: 10.1016/s0001-2092(06)60447-x. [DOI] [PubMed] [Google Scholar]
- 22.Schwaitzberg SD, Jones DB. Don't get burned from lack of knowledge. Ann Surg. 2012 Aug;256(2):219–212. doi: 10.1097/SLA.0b013e318260260c. [DOI] [PubMed] [Google Scholar]
- 23.Feldman LS, Fuchshuber P, Jones DB, Mischna J, Munro MG. Society of American Gastrointestinal and Endoscopic Surgeons (Oral presentation) Baltimore, MD: 2013. Apr, Schwaitzberg S for the FUSE (Fundamental Use of Surgical Energy™) Task Force. Rationale for the fundamental use of surgical energy™ (FUSE) educational program. [Google Scholar]
- 24.Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD. FUSE (Fundamental Use of Surgical Energy™) Task Force. Surgeons don't know what they don't know about the safe use of energy in surgery. Surg Endosc. 2012 Oct;26(10):2735–2739. doi: 10.1007/s00464-012-2263-y. Epub 2012 Apr 27. [DOI] [PubMed] [Google Scholar]
- 25.Feldman Liane, Fuchshuber Pascal, Jones Daniel B., editors. The SAGES Manual on the Fundamental Use of Surgical Energy (FUSE) NY: Springer Verlag NY; 2012. [Google Scholar]