Abstract
Neuraminidase (NA) mutations conferring resistance to NA inhibitors (NAIs) generally compromise the fitness of influenza viruses. The only NAI-resistant virus that widely spread in the population, the A/Brisbane/59/2007 (H1N1) strain, contained permissive mutations that restored the detrimental effect caused by the H275Y change. Computational analysis predicted other permissive NA mutations for A(H1N1)pdm09 viruses. Here, we investigated the effect of T289M and N369K mutations on the viral fitness of the A(H1N1)pdm09 H275Y variant. Recombinant wild-type (WT) A(H1N1)pdm09 and the H275Y, H275Y/T289M, H275Y/N369K, and H275Y/V241I/N369K (a natural variant) NA mutants were generated by reverse genetics. Replication kinetics were performed by using ST6GalI-MDCK cells. Virulence was assessed in C57BL/6 mice, and contact transmission was evaluated in ferrets. The H275Y mutation significantly reduced viral titers during the first 12 to 36 h postinfection (p.i.) in vitro. Nevertheless, the WT and H275Y viruses induced comparable mortality rates, weight loss, and lung titers in mice. The T289M mutation eliminated the detrimental effect caused by the H275Y change in vitro while causing greater weight loss and mortality in mice, with significantly higher lung viral titers on days 3 and 6 p.i. than with the H275Y mutant. In index ferrets, the WT, H275Y, H275Y/T289M, and H275Y/V241I/N369K recombinants induced comparable fever, weight loss, and nasal wash viral titers. All tested viruses were transmitted at comparable rates in contact ferrets, with the H275Y/V241I/N369K recombinant demonstrating higher nasal wash viral titers than the H275Y mutant. Permissive mutations may enhance the fitness of A(H1N1)pdm09 H275Y viruses in vitro and in vivo. The emergence of such variants should be carefully monitored.
INTRODUCTION
Influenza viruses are responsible for respiratory tract infections of significant public health importance. Influenza A viruses of the H1N1 subtype have been associated with seasonal influenza epidemics, from the 1918-1919 pandemic (1) until 1957, with a resurgence in 1977. Those seasonal A/H1N1 viruses then consistently circulated until 2009, at which time they were replaced by the triple-reassortant influenza A/H1N1 pandemic virus [A(H1N1)pdm09] of swine origin (2). As the M gene of this pandemic virus contained the S31N mutation, conferring resistance to adamantanes (amantadine and rimantadine), only neuraminidase inhibitors (NAIs) (i.e., oral oseltamivir, inhaled zanamivir, and, to a lesser extent, intravenous peramivir) were considered for the pharmacological control of A(H1N1)pdm09 infections (3). During the 2009-2010 pandemic and thereafter, approximately 0.4 to 1.5% of all tested A(H1N1)pdm09 viruses were found to be highly resistant to oseltamivir (4, 5), and these strains were initially identified mainly in immunocompromised patients who had received prolonged treatment or as a result of antiviral prophylaxis (6, 7). As was the case for human A/H1N1 viruses that circulated before the 2009 pandemic, the majority of drug-resistant A(H1N1)pdm09 viruses harbored the H275Y (N1 numbering) NA mutation. Since its introduction in humans in April 2009, the transmission of the A(H1N1)pdm09 H275Y variant in the community has remained limited (8). Such a low level of drug resistance contrasts with the situation observed with the seasonal influenza virus A/Brisbane/59/2007 (H1N1) H275Y variant, which began to circulate in Europe and the United States in 2007 to 2008 before spreading worldwide during the subsequent season (9). The efficient fitness and transmissibility of oseltamivir-resistant A/Brisbane/59/2007 H275Y viruses were attributed to additional “permissive” NA mutations (R222Q, V234M, and D334N), which counteracted the detrimental impact of the H275Y substitution on enzymatic function and replicative properties (10, 11). A possible permissive role for T82K, K141E, and R189K mutations within the hemagglutinin (HA) gene was also proposed (12). However, no HA changes were involved in the enhanced transmissibility observed for an oseltamivir-resistant A/Brisbane/59/07-like isolate compared to a closely related drug-susceptible (275H) isolate when investigated in the guinea pig model (13). Using the same computational analysis that previously led to the successful identification of permissive mutations in the A/Brisbane/59/2007 (H1N1) background, Bloom and colleagues recently proposed a set of potential permissive NA mutations, including T289M and N369K, for influenza A(H1N1)pdm09 H275Y viruses (14). The latter mutations have been shown to enhance surface expression of an oseltamivir-resistant influenza virus NA protein, but their role in replicative capacity and virulence has not been demonstrated. Interestingly, the compensatory role of the N369K mutation and that of another NA mutation (V241I) were also recently suggested in the context of large community outbreaks of oseltamivir-resistant influenza A(H1N1)pdm09 viruses implicating transmission events reported in Australia (15) and Spain (16).
In this study, we generated several recombinant influenza A(H1N1)pdm09 H275Y variants in order to assess the impact of N369K, T289M, and V241I permissive mutations on in vitro replicative capacity as well as on virulence and transmissibility in animals.
MATERIALS AND METHODS
Generation of recombinant A(H1N1)pdm09 viruses.
Recombinant wild-type (WT) influenza A/Quebec/144147/09 virus, an A/California/07/2009-like A(H1N1)pdm09 virus, was generated by using bidirectional pLLBA/G plasmids as previously described (17). The pLLBA plasmid containing the NA gene was used for the introduction of single (H275Y, N369K, and T289M), double (H275Y/N369K and H275Y/T289M), and triple (H275Y/V241I/N369K) mutations (N1 numbering), using appropriate primers and the QuikChange site-directed mutagenesis kit (Stratagene, La Jolla, CA). The resulting plasmids, pLLB-NAWT, pLLB-NA275Y, pLLB-NA289M, pLLB-NA369K, pLLB-NA275Y/289M, pLLB-NA275Y/369K, and pLLB-NA275Y/241I/369K, were sequenced to ensure the absence of undesired mutations. pLLB-NA plasmids and the remaining 7 plasmids (pLLB-HA, -M, -NS, -NP, -PA, -PB1, and -PB2) from A/Quebec/1441417/09 were cotransfected into 293T human embryonic kidney cells by using Lipofectamine 2000 reagent (Invitrogen, Carlsbad, CA) according to the manufacturer's instructions. Supernatants were collected at 72 h posttransfection and used to inoculate Madin-Darby canine kidney cells overexpressing the α2,6 sialic acid receptors (ST6GalI-MDCK cells), kindly provided by Y. Kawaoka from the University of Wisconsin, Madison, WI. The resulting recombinant WT and NA mutant viruses were subsequently sequenced and titrated by plaque assays in ST6GalI-MDCK cells.
NA enzyme kinetics assays.
A fluorometric-based assay using MUNANA (methylumbelliferyl-N-acetylneuraminic acid) (Sigma, St. Louis, MO) as the substrate was performed to determine NA enzymatic parameters. Briefly, recombinant viruses were standardized to an equivalent dose of 106 PFU/ml and incubated at 37°C in 50-μl reaction mixtures with different concentrations of MUNANA in a buffer containing 23 mM N-morpholino-ethanesulfonic acid (pH 6.5) and 3 mM CaCl2 (18). The final concentration of the substrate ranged from 0 to 3,000 μM. Fluorescence was monitored every 90 s for 53 min (35 measurements). The Michaelis-Menten constant (Km) and the maximum velocity (Vmax) normalized to PFU were calculated with Prism software (version 5; GraphPad), by fitting the data to the Michaelis-Menten equation using nonlinear regression.
Cell surface NA activity.
Recombinant NA plasmids and plasmids pCAGGS-PA, -PB1, -PB2, and -NP (1 μg each) were used to cotransfect 106 293T cells in order to express recombinant NA enzymes (19). At 24 h posttransfection, cells were briefly treated with trypsin-EDTA and neutralized by the addition of serum before collection of the cells by centrifugation at 3,000 rpm for 5 min. After two washes with phosphate-buffered saline (PBS), the cells were resuspended in a nonlysing buffer (15 mM morpholinepropanesulfonic acid [MOPS], 145 mM sodium chloride, 2.7 mM potassium chloride, and 4 mM calcium chloride, adjusted to pH 7.4) and used in an NA assay using MUNANA as the substrate (11).
In vitro replication kinetics experiments.
Replicative capacities of the recombinant viruses were evaluated by infecting ST6GalI-MDCK cells at a multiplicity of infection (MOI) of 0.001 PFU/cell. Supernatants were collected every 12 h until 72 h p.i. and titrated by plaque assays using ST6GalI-MDCK cells.
Mouse studies.
Groups of 16 6- to 8-week-old female C57BL/6 mice (Charles River, ON, Canada) were infected by intranasal inoculation of 105 PFU of recombinant WT or NA mutant A(H1N1)pdm09 viruses. Animals were weighed daily for 12 days and monitored for clinical signs. Four mice per group were sacrificed on days 3 and 6 p.i., and lungs were removed aseptically. For determination of viral titers, harvested lung tissues were homogenized in Dulbecco's modified Eagle medium (Life Technologies Corporation, Grand Island, NY) with antibiotics by using a bead mill homogenizer (Tissue Lyser; Qiagen). Cells were pelleted by centrifugation (2,000 × g for 5 min), and supernatants were titrated by plaque assays in ST6GalI-MDCK cells.
Ferret studies.
Groups of 4 seronegative (800- to 1,200-g) male ferrets (Marshall BioResources, North Rose, NY) housed in individual cages were lightly anesthetized by isoflurane and received an intranasal instillation of 5 × 104 PFU of recombinant WT A(H1N1)pdm09 or one of the three selected NA mutants (H275Y, H275Y/T289M, and H275Y/V241I/N369K). Ferrets were weighed daily, and body temperature was measured by rectal thermometers every day until day 10 p.i. Nasal wash samples were collected from animals on a daily basis until day 8 p.i., and viral titers were determined every other day by plaque assays in ST6GalI-MDCK cells. Serum samples were collected from each ferret before intranasal infection (day 0) and on day 14 p.i. to evaluate specific antibody levels against the A/California/07/2009 A(H1N1)pdm09 and A/Wisconsin/15/2009 (H3N2) viral strains by using standard hemagglutination inhibition (HAI) assays with 0.7% turkey red blood cells. To evaluate contact transmissibility, inoculated-contact animal pairs were established by placing a naive ferret into each cage 24 h after inoculation of the donor ferret. Contact animals were monitored for clinical signs, and nasal wash and serum samples were collected as described above for determination of viral titers and serological status, respectively. All animal procedures were approved by the Institutional Animal Care Committee of Laval University according to the guidelines of the Canadian Council on Animal Care.
Sequencing.
NA genes of viruses recovered from in vitro replication assays, mouse lung homogenates, and ferret nasal wash samples were amplified and sequenced by using the ABI 3730 DNA analyzer (Applied Biosystems, Carlsbad, CA) to confirm both the presence of the desired mutations and the absence of additional mutations.
Statistical analyses.
All data were expressed as the means of 3 replicates. NA kinetic parameters, surface NA activity, viral titers, and body weight loss were compared by one-way analysis of variance (ANOVA) with Tukey's multiple-comparison posttest. Areas under the curve of temperature values over 10 days were compared by unpaired two-tailed t tests with GraphPad, version 5.
RESULTS
Characterization of permissive NA mutations in vitro.
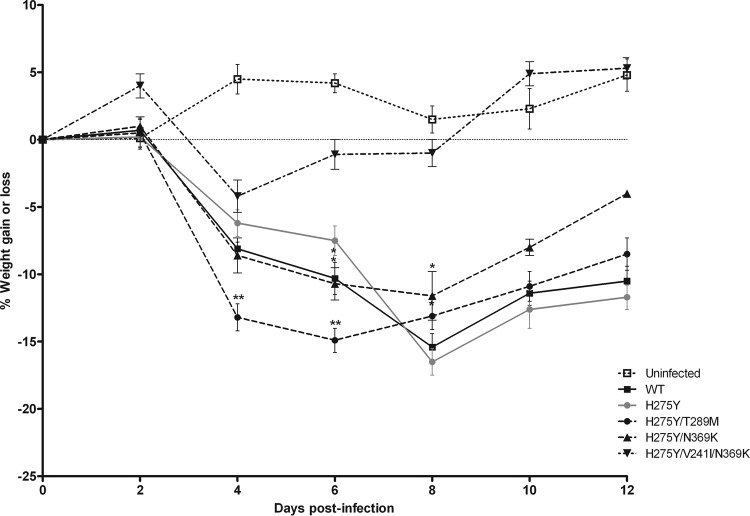
The effects of the different mutations selected for this study on NA enzyme kinetics parameters for viruses normalized to 106 PFU are summarized in Table 1. Compared to the affinity of the single H275Y mutant (Km of 80.84 ± 7.93 μM), an increase in NA affinity was observed for the WT and the T289M, N369K, H275Y/T289M, and H275Y/I241V/N369K variants, supported by significantly lower Km values. Of note, the Km values of the H275Y/T289M (36.02 ± 3.38 μM) and the WT (26.21 ± 1.74 μM) viruses were not significantly different. The WT and the T289M variant were the only two NA proteins that also exhibited significant differences in Vmax compared to the H275Y variant (11.39 ± 0.39 and 14.87 ± 0.68 versus 2.21 ± 0.09 U/s, respectively; P < 0.01). The Vmax ratio of the H275Y/T289M variant was 3.5-fold higher than that of the H275Y variant (0.74 versus 0.19). Moreover, using recombinant NA proteins expressed in 293T cells, the H275Y mutation was shown to be associated with a significant reduction in NA activity at the cell surface compared to the WT protein, with a relative total surface activity of 19.73% (P < 0.001) (Fig. 1). In all cases, the addition of the potentially permissive mutations to the H275Y variant partially compensated for the loss of NA activity, with relative total surface activities of 43.63% (P < 0.001), 27.45% (P < 0.05), and 74.49% (P < 0.001) for the H275Y/T289M, H275Y/N369K, and H275Y/V241I/N369K mutants, respectively. Of interest, the cell surface activity of the H275Y/V241I/N369K triple mutant was significantly higher than that of the double mutant (H275Y/N369K) (P < 0.001).
TABLE 1.
Enzyme kinetics parameters of recombinant A(H1N1)pdm09 viruses harboring several neuraminidase mutationsa
| Recombinant influenza A(H1N1)pdm09 virus | Mean Km (μM) ± SD | Relative Vmax (U/s) ± SD | Vmax ratio |
|---|---|---|---|
| Wild type | 26.21 ± 1.74*** | 11.39 ± 0.39 | 1** |
| H275Y | 80.84 ± 7.93 | 2.21 ± 0.09 | 0.19 |
| N369K | 46.14 ± 3.42*** | 4.07 ± 0.6 | 0.36 |
| T289M | 60.76 ± 6.44** | 14.87 ± 0.68 | 1.3** |
| H275Y/N369K | 94.20 ± 3.57* | 3.34 ± 0.17 | 0.36 |
| H275Y/T289M | 36.02 ± 3.38*** | 8.41 ± 0.64 | 0.74 |
| H275Y/V241I/N369K | 54.81 ± 3.58*** | 5.76 ± 0.21 | 0.51 |
Numbers indicate mean Km and relative NA activity (Vmax) values of a representative experiment performed in triplicate, using recombinant viruses standardized to 106 PFU/ml. *, P < 0.05; **, P < 0.01; ***, P < 0.001 (compared to the recombinant H275Y virus).
FIG 1.
Surface activity of recombinant A(H1N1)pdm09 NA proteins. 293T cells were transfected with plasmids expressing the WT or mutant A(H1N1)pdm09-like NAs. At 24 h posttransfection, cells were treated with a nonlysing buffer, and surface NA activity was measured by using a fluorogenic substrate (MUNANA). Percent surface NA activities are shown compared to the WT from triplicate experiments ± standard deviations. *, P < 0.05; ***, P < 0.001 (compared to the recombinant H275Y virus).
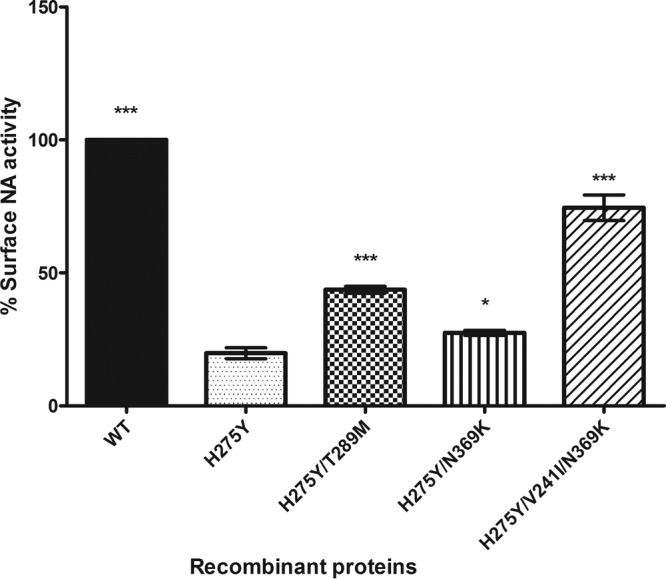
The impact of NA mutations on viral fitness of recombinant viruses was assessed in ST6GalI-MDCK cells (Fig. 2). The H275Y mutant showed significantly reduced viral titers compared to the rest of the recombinant viruses in the first 12 h p.i. and also compared to the WT and the H275Y/T289M mutant at 24 h and 36 h p.i. The H275Y/T289M double mutant still displayed viral titers significantly higher than those of the H275Y mutant at 48 h p.i. (2.9 × 108 ± 0.9 × 108 versus 7.6 × 107 ± 1.8 × 107 PFU/ml; P < 0.001). The growth curves of the remaining mutant viruses were not significantly different from that of the H275Y virus beyond 12 h p.i. Sequence analysis of viral samples from infected cell culture supernatants did not show mutations other than the expected ones in viruses recovered at 72 h p.i.
FIG 2.
In vitro replicative capacities of recombinant wild-type (WT) and NA mutant influenza A(H1N1)pdm09 viruses. Viral titers were determined at the indicated time points from supernatants of MDCK-α2,6 cells infected at a multiplicity of infection (MOI) of 0.001. Mean viral titers ± standard deviations from triplicate experiments were determined by using standard plaque assays. *, P < 0.05; **, P < 0.01; ***, P < 0.001 (compared to the recombinant H275Y virus).
Effect of permissive NA mutations in mice.
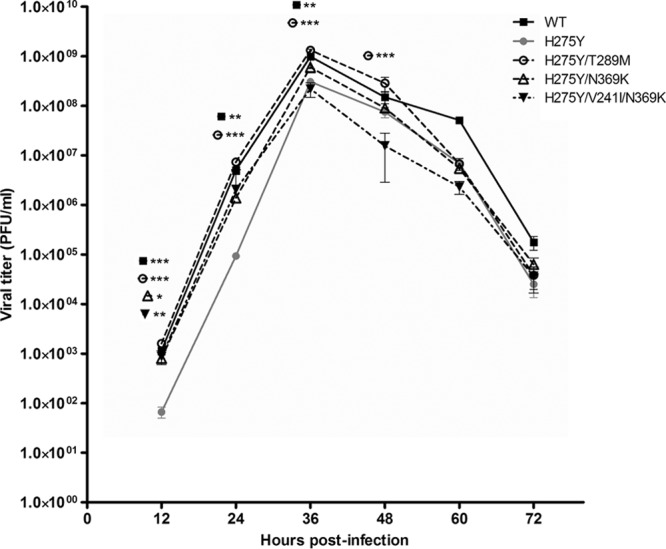
As shown in Table 2, intranasal inoculation of mice with 105 PFU of the recombinant viruses resulted in mortality rates of 50% for the WT and H275Y/T289M, 37.5% for the H275Y, 12.5% for the H275Y/N369K, and 0% for the H275Y/V241I/N369K groups. Interestingly, the H275Y/T289M group showed significantly higher mean weight loss than the H275Y group on day 4 p.i. (13.2% ± 1.5% versus 6.2% ± 1.8%; P < 0.01) (Fig. 3) as well as a shorter mean number of days to death (4.75 versus 6.33 days; P < 0.05) (Table 2). In line with the above-described observations, lung viral titers (LVTs) were significantly higher for the H275Y/T289M group than for the H275Y group on both day 3 p.i. (7.8 × 106 ± 0.3 × 106 versus 3.9 × 106 ± 0.1 × 106 PFU/ml; P < 0.05) and day 6 p.i. (3.5 × 106 ± 0.3 × 106 versus 0.7 × 106 ± 0.1 × 106 PFU/ml; P < 0.05). Conversely, no significant differences in weight loss, mean number of days to death, or LVT were observed between any of the other 3 groups (WT, H275Y/N369K, and H275Y/V241I/N369K) and the H275Y group (Table 2). The LVTs of the H275Y/T289M group were significantly higher than those of the WT group on day 3 p.i. (7.8 × 106 ± 0.3 × 106 versus 1.8 × 106 ± 0.2 × 106 PFU/ml; P < 0.05). Sequence analysis of the NA gene from lung samples of mice confirmed the presence of the desired mutations and no other mutations or mixed viral populations.
TABLE 2.
Virulence of recombinant influenza A(H1N1)pdm09 viruses harboring several neuraminidase mutations in C57BL/6 micea
| Recombinant influenza A(H1N1)pdm09 virus | Mean % wt change on day 4 p.i. ± SD (n = 12) | % mortality (day 14 p.i.) (n = 8) | Mean no. of days to death | Mean LVT (PFU/ml) on day 3 p.i. ± SD (n = 4) | Mean LVT (PFU/ml) on day 6 p.i. ± SD (n = 4) |
|---|---|---|---|---|---|
| WT | 8.1 ± 1.4 | 50 | 7.75 | 1.8 × 106 ± 0.17 × 106 | 1.5 × 106 ± 0.66 × 106 |
| H275Y | 6.2 ± 1.8 | 37.5 | 6.33 | 3.9 × 106 ± 0.13 × 106 | 0.65 × 106 ± 0.1 × 106 |
| H275Y/N369K | 8.6 ± 1.3 | 12.5 | 7 | 3.1 × 106 ± 0.47 × 106 | 1.8 × 106 ± 0.71 × 106 |
| H275Y/V241I/N369K | 4.2 ± 1.2 | 0 | NA | 4.8 × 105 ± 0.27 × 105 | 0.15 × 106 ± 0.05 × 106 |
| H275Y/T289M | 13.2 ± 1.5** | 50 | 4.75* | 7.75 × 106 ± 0.32 × 106* | 3.5 × 106 ± 0.27 × 106* |
| Uninfected | −4.5 ± 0.2 | 0 | NA |
LVT, lung viral titers in PFU/ml; NA, not applicable. *, P < 0.05, **, P < 0.01 (compared to the recombinant H275Y virus).
FIG 3.
Mean body weight loss of mice infected intranasally with 105 PFU of recombinant WT or NA mutant influenza A(H1N1)pdm09 viruses. Percent body weight losses were determined daily up to day 12 postinoculation. *, P < 0.05; **, P < 0.01 (compared to the recombinant H275Y virus).
Effect of permissive NA mutations in ferrets.
Intranasal inoculation of ferrets with 5 × 104 PFU of the recombinant WT, H275Y, H275Y/T289M, or H275Y/V241I/N369K viruses yielded mild clinical signs, with febrile responses that peaked on days 2 and 4 p.i. for the donor and contact animals, respectively, in all groups (data not shown). Although the WT and H275Y/T289M groups exhibited the highest peak temperature values, no significant differences in the area under the curve (AUC) of temperatures from days 0 to 10 p.i. were observed among any of the four groups. Also, there were no significant differences in body weight loss (maximum of 3.6%) at any time points among groups (data not shown).
Mean viral titers in nasal wash samples collected from donor animals on days 2 and 4 p.i. were comparable among the four groups, ranging from 2.0 × 103 ± 0.6 × 103 to 1.4 × 104 ± 0.9 × 104 PFU/ml and from 4.5 × 102 ± 0.2 × 102 to 1.9 × 103 ± 1.4 × 103 PFU/ml, respectively (Fig. 4A). Nasal wash viral titers were undetectable on day 6 p.i., except for one ferret in each of the H275Y/T289M and H275Y/V241I/N369K groups. All contact animals seroconverted for A/California/07/2009 (H1N1), with reciprocal geometric mean HAI titers of between 180 and >1,280 on day 14 p.i., compared to <10 on day 0. For A/Wisconsin/15/2009 (H3N2), reciprocal geometric mean HAI titers were <10 on both days 0 and 14 p.i. As shown in Fig. 4B, mean viral titers in nasal wash samples obtained from contact ferrets of the H275Y/V241I/N369K group were significantly higher than those of the H275Y group on day 3 p.i. (1.2 × 104 ± 0.8 × 104 versus 1.9 × 102 ± 0.5 × 102 PFU/ml; P < 0.05) and day 5 p.i. (2.7 × 104 ± 1.3 × 104 versus 5.9 × 103± 3.2 × 103; P < 0.05) but not on day 7 p.i. (1.4 × 103 ± 0.7 × 103 versus 8.9 × 102 ± 5.7 × 102 PFU/ml). Mean nasal wash viral titers of contact ferrets of the WT group were also significantly higher than those of the H275Y group on day 5 p.i. (1.9 × 104 ± 0.9 × 104 versus 5.9 × 103 ± 3.2 × 103 PFU/ml, respectively; P < 0.05). On the other hand, mean viral titers were comparable for contact ferrets of the H275Y/T289M and H275Y groups at all 3 time points. Sequence analysis of the NA gene in nasal wash samples of ferrets confirmed the presence of the desired mutations in each of the four animals of the respective donor and contact groups, with no other mutations or mixed viral populations being detected.
FIG 4.
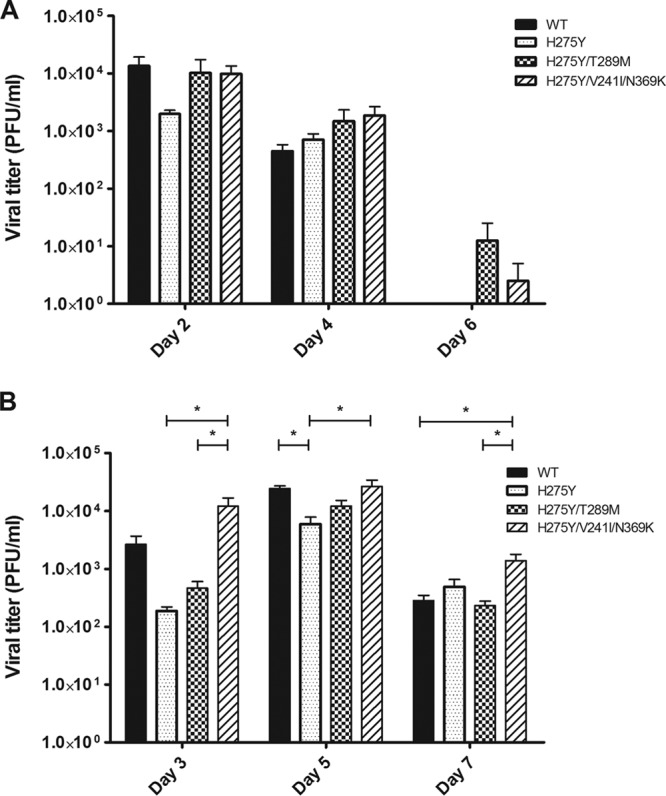
Mean viral titers ± standard deviations in nasal wash specimens of index ferrets infected with 5 × 104 PFU of recombinant WT and NA mutant A(H1N1)pdm09 viruses (A) and in samples of their direct-contact animals (B). Viral titers were determined at the indicated days postinoculation by using standard plaque assays. *, P < 0.05 compared to the recombinant H275Y virus.
DISCUSSION
In this study, we found that the T289M NA mutation in particular as well as the N369K substitution partially restore the replicative capacity and virulence of the H275Y A(H1N1)pdm09 variant in vitro and in mice. Moreover, direct-contact transmission experiments in ferrets have shown that all tested viruses were successfully transmitted at comparable rates, with the H275Y/V241I/N369K recombinant demonstrating higher nasal wash viral titers than the H275Y mutant in contact animals.
Given widespread adamantane resistance, NAIs constitute the most clinically relevant class of anti-influenza virus agents that have been used in many countries as therapeutic and prophylactic modalities for seasonal or pandemic influenza virus infections. Since their introduction in the late 1990s, some concerns have been raised with regard to the emergence and spread of NAI-resistant variants, which may compromise the clinical utility of these antiviral agents. Previous reports have shown that NAI-resistant influenza viruses may emerge under NAI pressure in vitro or in the clinic as a result of NA mutations which occur in a subtype- and drug-specific manner (20, 21). In the N1 subtype, the phenotype of resistance to oseltamivir is usually mediated by the framework H275Y NA mutation (22). As NAIs target the active site of a key viral enzyme, resistance mutations occurring within the NA gene were expected to compromise the viral fitness of these variants. In fact, when present in older A/H1N1 strains, including A/WSN/33 (19), A/Texas/36/91 (23), A/New Caledonia/20/99 (24), and A/Mississippi/3/01 (25), the H275Y NA mutation was found to be deleterious both in vitro and in animal models. However, more recent seasonal A/H1N1 mutant strains, such as A/Brisbane/59/2007-like isolates, were fully virulent and transmissible (9). Bloom and colleagues demonstrated that the H275Y mutation was associated with a significant decrease in the amount of the NA enzyme that is expressed on the cell surface (11). Those authors suggested that, as the H275Y mutation apparently altered NA protein folding, additional (so-called “permissive”) NA mutations occurring at distant sites in the three-dimensional (3D) structure could restore adequate NA folding (11). Using a computational approach based on potentially important phylogenetic sites (PIPS), the R194G NA mutation was predicted to correct the deficiency caused by the H275Y mutation in the A/WSN/33 background, and as expected, the R194G/H275Y double mutation restored the viral fitness of this strain in vitro (11). This method was also successfully used to predict the ability of R222Q and V234M mutations to correct the deficiency caused by the H275Y change in the A/Texas/36/91 virus (11). Our group further demonstrated the compensatory nature of these mutations in recombinant viruses by reverting the latter two substitutions (i.e., Q222R and M234V) in NA of the oseltamivir-resistant A/Brisbane/59/2007 (H1N1) H275Y variant (10). As predicted, these substitutions significantly altered the in vitro viral fitness and contact transmissibility of the drug-resistant virus in ferrets.
A similar computational approach was recently performed by Bloom and colleagues (14) to predict permissive NA mutations in the A(H1N1)pdm09 virus background harboring the oseltamivir-resistant H275Y mutation. A rationale exists for using this approach, since, as was observed in older seasonal A/H1N1 viruses (11), the H275Y mutation also induced significant decreases in the levels of total NA protein and cell surface enzymatic activity in the 2009 pandemic virus. Of note, the compromising impact of the H275Y substitution in the context of the A(H1N1)pdm09 background has been controversial. While some studies reported a statistically significant impairment in viral growth in vitro (17, 26), other groups did not detect significant differences in terms of replicative capacity between the A(H1N1)pdm09 WT virus and its H275Y variant (27, 28). In studies based on the ferret model, the A(H1N1)pdm09 H275Y variant demonstrated comparable contact transmission efficiency compared to the WT (29, 30), whereas the mutant appeared to compromise airborne transmission (which is probably more biologically relevant) in some but not all investigations (26, 27, 31, 32). Nevertheless, the fact that the oseltamivir-resistant A(H1N1)pdm09 virus has not replaced the WT counterpart indicates some fitness alteration due to the H275Y mutation. It is thus worthwhile to assess the future impact of potential permissive NA mutations on the viral fitness of drug-resistant influenza A(H1N1)pdm09 viruses, as these strains have been circulating worldwide since 2009. Recent outbreaks implicating transmission of oseltamivir-resistant A(H1N1)pdm09 strains in the absence of antiviral treatment also justify this investigation. In those cases, a set of permissive NA mutations (such as N369K and V241I) may have facilitated the emergence of the H275Y resistance mutation and improved virus transmissibility (15, 16). Of importance, during the 2010-2011 influenza season in the United States, up to 74% of oseltamivir resistance cases were not associated with drug exposure (33).
As part of our study, we generated recombinant viruses and proteins in order to characterize the two best candidates from a list of 12 potentially permissive NA mutations proposed for A(H1N1)pdm09 viruses (14), namely, the T289M and N369K substitutions. In addition, we investigated the N369K mutation in conjunction with the V241I substitution since variants with the three (H275Y/V241I/N369K) NA mutations were recently identified among clinical A(H1N1)pdm09 Australian (15) and Spanish (16) isolates. Moreover, NA sequences containing the V241I/N369K changes, without the H275Y mutation, have been deposited in the GISAID public sequence database (15). On the other hand, the T289M change has not yet been reported in A(H1N1)pdm09 viruses.
Our experiments demonstrated the ability of T289M and N369K mutations to partially restore the NA cell surface expression defect associated with the H275Y mutation. This compensation could be explained by a greater number of NA molecules that reach the cell surface, an increased activity of the enzyme, or a combination of both effects (11, 14). Our results are in agreement with a previous NA protein expression analysis (14). Interestingly, the impact of adding the permissive V241I/N369K double mutation to the H275Y mutation in restoring NA cell surface expression was greater than that of the single N369K change (P < 0.001) and may account for the better replication and/or earlier contact transmission of the triple mutant in ferrets as well as its presence in community outbreak isolates.
Our results show that, as predicted, the addition of the potentially permissive NA mutations can enhance the fitness and virulence of A(H1N1)pdm09 viruses containing the H275Y mutation both in vitro and in vivo. It should be noted, however, that the efficiency of the PIPS approach to successfully identify permissive NA mutations is not perfect, as the V241I change, which seems to possess a potential permissive role, was not predicted, whereas the T289M mutation, which was predicted with a high score, has not yet been described in clinical samples. In particular, the T289M substitution seems to have the most significant compensatory effect by improving NA kinetic parameters, with a 2.2-fold increase in affinity and a 3.8-fold increase in Vmax activity compared to the H275Y mutant (Table 1). This mutation also significantly improved the replicative capacity of the H275Y A(H1N1)pdm09 virus in ST6GalI-MDCK cells (Fig. 2) as well as its virulence in C57BL/6 mice to levels comparable to or even higher than those of the WT virus (Table 2 and Fig. 3). However, no significant differences were observed between the H275Y and H275Y/T289M groups with respect to the nasal wash viral titers of both index and contact ferrets. In our study, the triple (H275Y/V241I/N369K) NA mutation resulted in a significant increase in nasal wash viral titers compared to the H275Y group in contact ferrets, although this genotype was not associated with increased virulence in mice. This discrepancy could be attributed to differences in receptor binding cells, which are a major determinant for efficient transmission of influenza viruses (34), between mice (predominantly α2,3 sialic acid receptors) and ferrets (predominantly α2,6 sialic acid receptors). Thus, the triple (H275Y/V241I/N369K) NA mutant enzyme may cleave the α2,6 sialic acid linkage with a better efficiency than the α2,3 sialic acid one. This may result in better airborne transmission, which was not evaluated in our study. Of interest, A(H1N1)pdm09 viruses containing the V241I/N369K double mutation that demonstrated the potential to counteract the detrimental effect of the H275Y mutation already exist (15). Thus, exposure of individuals infected with A(H1N1)pdm09 V241I/N369K viruses to oseltamivir during prophylaxis or treatment courses may rapidly select for the H275Y mutation, which could constitute a serious public health threat. Moreover, exposure to NAIs is not necessary to select for the H275Y mutation if permissive mutations are already present in the NA gene, as exemplified by the emergence and global dissemination of oseltamivir-resistant A/Brisbane/59/2007-like variants (9, 35).
In conclusion, our study confirmed that, as was the case for recent seasonal A/H1N1 viruses containing permissive NA mutations that facilitated the replacement of the susceptible virus by the H275Y oseltamivir-resistant variant, permissive mutations that may enhance the fitness of A(H1N1)pdm09 H275Y viruses do exist. Consequently, the potential emergence and dissemination of such variants should be carefully monitored.
ACKNOWLEDGMENTS
This study was supported by the Canadian Institutes of Health Research and GlaxoSmithKline Canada (grants 230187 and 229733 to G.B.).
We are grateful to Jesse Bloom for helpful discussions and critical review of the manuscript.
Footnotes
Published ahead of print 20 November 2013
REFERENCES
- 1.Reid AH, Janczewski TA, Lourens RM, Elliot AJ, Daniels RS, Berry CL, Oxford JS, Taubenberger JK. 2003. 1918 influenza pandemic caused by highly conserved viruses with two receptor-binding variants. Emerg. Infect. Dis. 9:1249–1253. 10.3201/eid0910.020789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, Ma SK, Cheung CL, Raghwani J, Bhatt S, Peiris JS, Guan Y, Rambaut A. 2009. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459:1122–1125. 10.1038/nature08182 [DOI] [PubMed] [Google Scholar]
- 3.Committee on Infectious Diseases of the American Academy of Pediatrics 2012. Recommendations for prevention and control of influenza in children, 2012-2013. Pediatrics 130:780–792. 10.1542/peds.2012-2308 [DOI] [PubMed] [Google Scholar]
- 4.WHO 2012. Review of the 2011-2012 winter influenza season, northern hemisphere. Wkly. Epidemiol. Rec. 87:233–240 http://www.who.int/wer/2012/wer8724.pdf [PubMed] [Google Scholar]
- 5.CDC 2013. Influenza activity—United States, 2012-13 season and composition of the 2013-14 influenza vaccine. MMWR Morb. Mortal. Wkly. Rep. 62:473–479 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6223a5.htm [PMC free article] [PubMed] [Google Scholar]
- 6.Graitcer SB, Gubareva L, Kamimoto L, Doshi S, Vandermeer M, Louie J, Waters C, Moore Z, Sleeman K, Okomo-Adhiambo M, Marshall SA, St George K, Pan CY, LaPlante JM, Klimov A, Fry AM. 2011. Characteristics of patients with oseltamivir-resistant pandemic (H1N1) 2009, United States. Emerg. Infect. Dis. 17:255–257. 10.3201/eid1702.101724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baz M, Abed Y, Papenburg J, Bouhy X, Hamelin ME, Boivin G. 2009. Emergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxis. N. Engl. J. Med. 361:2296–2297. 10.1056/NEJMc0910060 [DOI] [PubMed] [Google Scholar]
- 8.Hurt AC, Chotpitayasunondh T, Cox NJ, Daniels R, Fry AM, Gubareva LV, Hayden FG, Hui DS, Hungnes O, Lackenby A, Lim W, Meijer A, Penn C, Tashiro M, Uyeki TM, Zambon M. 2012. Antiviral resistance during the 2009 influenza A H1N1 pandemic: public health, laboratory, and clinical perspectives. Lancet Infect. Dis. 12:240–248. 10.1016/S1473-3099(11)70318-8 [DOI] [PubMed] [Google Scholar]
- 9.Dharan NJ, Gubareva LV, Meyer JJ, Okomo-Adhiambo M, McClinton RC, Marshall SA, St George K, Epperson S, Brammer L, Klimov AI, Bresee JS, Fry AM. 2009. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA 301:1034–1041. 10.1001/jama.2009.294 [DOI] [PubMed] [Google Scholar]
- 10.Abed Y, Pizzorno A, Bouhy X, Boivin G. 2011. Role of permissive neuraminidase mutations in influenza A/Brisbane/59/2007-like (H1N1) viruses. PLoS Pathog. 7:e1002431. 10.1371/journal.ppat.1002431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275. 10.1126/science.1187816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ginting TE, Shinya K, Kyan Y, Makino A, Matsumoto N, Kaneda S, Kawaoka Y. 2012. Amino acid changes in hemagglutinin contribute to the replication of oseltamivir-resistant H1N1 influenza viruses. J. Virol. 86:121–127. 10.1128/JVI.06085-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouvier NM, Rahmat S, Pica N. 2012. Enhanced mammalian transmissibility of seasonal influenza A/H1N1 viruses encoding an oseltamivir-resistant neuraminidase. J. Virol. 86:7268–7279. 10.1128/JVI.07242-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bloom JD, Nayak JS, Baltimore D. 2011. A computational-experimental approach identifies mutations that enhance surface expression of an oseltamivir-resistant influenza neuraminidase. PLoS One 6:e22201. 10.1371/journal.pone.0022201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurt AC, Hardie K, Wilson NJ, Deng YM, Osbourn M, Leang SK, Lee RT, Iannello P, Gehrig N, Shaw R, Wark P, Caldwell N, Givney RC, Xue L, Maurer-Stroh S, Dwyer DE, Wang B, Smith DW, Levy A, Booy R, Dixit R, Merritt T, Kelso A, Dalton C, Durrheim D, Barr IG. 2012. Characteristics of a widespread community cluster of H275Y oseltamivir-resistant A(H1N1)pdm09 influenza in Australia. J. Infect. Dis. 206:148–157. 10.1093/infdis/jis337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meijer A, Jonges M, van Beek P, Swaan CM, Osterhaus AD, Daniels RS, Hurt AC, Koopmans MP. 2012. Oseltamivir-resistant influenza A(H1N1)pdm09 virus in Dutch travellers returning from Spain, August 2012. Euro Surveill. 17(36):pii=20266 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20266 [PubMed] [Google Scholar]
- 17.Pizzorno A, Bouhy X, Abed Y, Boivin G. 2011. Generation and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitors. J. Infect. Dis. 203:25–31. 10.1093/infdis/jiq010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yen HL, Ilyushina NA, Salomon R, Hoffmann E, Webster RG, Govorkova EA. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418–12426. 10.1128/JVI.01067-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abed Y, Goyette N, Boivin G. 2004. A reverse genetics study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antivir. Ther. 9:577–581 http://www.intmedpress.com/serveFile.cfm?sUID=6e16aa7b-7705-44ba-897a-2c80c1cc076f [PubMed] [Google Scholar]
- 20.Gubareva LV. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199–203. 10.1016/j.virusres.2004.02.034 [DOI] [PubMed] [Google Scholar]
- 21.Aoki FY, Boivin G, Roberts N. 2007. Influenza virus susceptibility and resistance to oseltamivir. Antivir. Ther. 12:603–616 http://www.intmedpress.com/serveFile.cfm?sUID=f23174a4-603e-477e-a576-004bf982bf3b [PubMed] [Google Scholar]
- 22.Pizzorno A, Abed Y, Boivin G. 2011. Influenza drug resistance. Semin. Respir. Crit. Care Med. 32:409–422. 10.1055/s-0031-1283281 [DOI] [PubMed] [Google Scholar]
- 23.Ives JA, Carr JA, Mendel DB, Tai CY, Lambkin R, Kelly L, Oxford JS, Hayden FG, Roberts NA. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307–317. 10.1016/S0166-3542(02)00053-0 [DOI] [PubMed] [Google Scholar]
- 24.Herlocher ML, Truscon R, Elias S, Yen HL, Roberts NA, Ohmit SE, Monto AS. 2004. Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J. Infect. Dis. 190:1627–1630. 10.1086/424572 [DOI] [PubMed] [Google Scholar]
- 25.Baz M, Abed Y, Simon P, Hamelin ME, Boivin G. 2010. Effect of the neuraminidase mutation H274Y conferring resistance to oseltamivir on the replicative capacity and virulence of old and recent human influenza A(H1N1) viruses. J. Infect. Dis. 201:740–745. 10.1086/650464 [DOI] [PubMed] [Google Scholar]
- 26.Duan S, Boltz DA, Seiler P, Li J, Bragstad K, Nielsen LP, Webby RJ, Webster RG, Govorkova EA. 2010. Oseltamivir-resistant pandemic H1N1/2009 influenza virus possesses lower transmissibility and fitness in ferrets. PLoS Pathog. 6:e1001022. 10.1371/journal.ppat.1001022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seibert CW, Kaminski M, Philipp J, Rubbenstroth D, Albrecht RA, Schwalm F, Stertz S, Medina RA, Kochs G, Garcia-Sastre A, Staeheli P, Palese P. 2010. Oseltamivir-resistant variants of the 2009 pandemic H1N1 influenza A virus are not attenuated in the guinea pig and ferret transmission models. J. Virol. 84:11219–11226. 10.1128/JVI.01424-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong DD, Choy KT, Chan RW, Sia SF, Chiu HP, Cheung PP, Chan MC, Peiris JS, Yen HL. 2012. Comparable fitness and transmissibility between oseltamivir-resistant pandemic 2009 and seasonal H1N1 influenza viruses with the H275Y neuraminidase mutation. J. Virol. 86:10558–10570. 10.1128/JVI.00985-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamelin ME, Baz M, Abed Y, Couture C, Joubert P, Beaulieu E, Bellerose N, Plante M, Mallett C, Schumer G, Kobinger GP, Boivin G. 2010. Oseltamivir-resistant pandemic A/H1N1 virus is as virulent as its wild-type counterpart in mice and ferrets. PLoS Pathog. 6:e1001015. 10.1371/journal.ppat.1001015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Memoli MJ, Davis AS, Proudfoot K, Chertow DS, Hrabal RJ, Bristol T, Taubenberger JK. 2011. Multidrug-resistant 2009 pandemic influenza A(H1N1) viruses maintain fitness and transmissibility in ferrets. J. Infect. Dis. 203:348–357. 10.1093/infdis/jiq067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kiso M, Shinya K, Shimojima M, Takano R, Takahashi K, Katsura H, Kakugawa S, Le MT, Yamashita M, Furuta Y, Ozawa M, Kawaoka Y. 2010. Characterization of oseltamivir-resistant 2009 H1N1 pandemic influenza A viruses. PLoS Pathog. 6:e1001079. 10.1371/journal.ppat.1001079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamelin ME, Baz M, Bouhy X, Beaulieu E, Dube K, Mallett C, Boivin G. 2011. Reduced airborne transmission of oseltamivir-resistant pandemic A/H1N1 virus in ferrets. Antivir. Ther. 16:775–779. 10.3851/IMP1794 [DOI] [PubMed] [Google Scholar]
- 33.Storms AD, Gubareva LV, Su S, Wheeling JT, Okomo-Adhiambo M, Pan CY, Reisdorf E, St George K, Myers R, Wotton JT, Robinson S, Leader B, Thompson M, Shannon M, Klimov A, Fry AM. 2012. Oseltamivir-resistant pandemic (H1N1) 2009 virus infections, United States, 2010-11. Emerg. Infect. Dis. 18:308–311. 10.3201/eid1802.111466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659. 10.1126/science.1136212 [DOI] [PubMed] [Google Scholar]
- 35.Meijer A, Lackenby A, Hungnes O, Lina B, van-der-Werf S, Schweiger B, Opp M, Paget J, van-de-Kassteele J, Hay A, Zambon M. 2009. Oseltamivir-resistant influenza virus A (H1N1), Europe 2007-08 season. Emerg. Infect. Dis. 15:552–560. 10.3201/eid1504.181280 [DOI] [PMC free article] [PubMed] [Google Scholar]