Abstract
Background:
The pressure-flow study (PFS) is considered the gold standard for the detection of bladder outlet obstruction (BOO) in men. However, several studies have raised the possibility that transurethral catheterization might have an obstructive effect on PFS while others did not.
Objectives:
To evaluate the effect of a 6 Fr transurethral catheter on the pressure-flow study and to evaluate its clinical implication in men.
Materials and Methods:
A retrospective chart review study of 515 men referred for an evaluation of lower urinary tract symptoms and who underwent an urodynamic study (UDS). Of those, 133 met our inclusion/exclusion criteria. Non invasive free-flow studies (NIFFS) were performed before every UDS. Cystometrogram and PFS were performed through a 6 Fr transurethral catheter.
Results:
The maximal flow rate (Qmax) was significantly higher (P < 0.001) in the NIFFS (15.0 mL/s (range 9.0-23.0)) than in the PFS (11.0 mL/s (range 7.0-18.5)). This difference became greater (18.5 mL/s (range 10.0-30.3) vs. 13.0 mL/s (range 6.0-25.0), in favor of the NIFFS) when we analyzed only the patients (n = 34) who voided a similar volume. According to the International Continence Society (ICS) nomogram, the use of the PFS alone would have resulted in the upstaging of 14% of cases (10/71) in the overall population and 24% (4/17) in the sub-analyzed group.
Conclusion:
A 6 Fr transurethral catheter significantly lowers the maximal flow rate by 4 mL/s. Its presence resulted in an upstaging on the ICS nomogram. However, further studies will be necessary to confirm this upstaging.
Keywords: Benign prostatic hyperplasia, bladder outlet obstruction, maximum flow rate, pressure-flow study
INTRODUCTION
Bladder outlet obstruction (BOO) is an affliction causing lower urinary tract symptoms (LUTS) in a high number of aging men.[1] The non invasive free flow studies (NIFFS) and post void residual (PVR) are non-invasive tests which may indicate or lower the suspicion of BOO.[2] However, the pressure-flow studies (PFS) have long been regarded as the gold standard for the diagnostic of such an affliction.[2] In order to measure the bladder pressure, a small transurethral catheter is usually introduced in the bladder. Based on the information gathered, men are classified as being either obstructed, equivocal or unobstructed using the International Continence Society (ICS) nomogram. This nomogram established in 1997 by Griffith et al.[3] quantifies the bladder outlet resistance using the maximal flow rate (Qmax) and the detrusor pressure at maximal flow rate (Pdet Qmax). Both criteria are important to determine BOO as 25-30% of men with a decreased maximal flow rate are not obstructed.[4] In order to differentiate these two entities, it is thus also important to measure the Pdet Qmax.[5,6]
Several studies both in men and women have raised multiple questions about the potential obstructive nature of the transurethral catheterization during the PFS. A recent study[7] has confirmed its obstructive nature in women while others[8,9,10,11,12] have also found similar results in men. However, both in men and women, other authors have failed to show such results.[13,14]
Thus, the objectives of this study were to evaluate whether the use of a 6 Fr transurethral catheter affects the maximal flow rate and to assess whether its potential obstructive nature changes the classification of men on the ICS nomogram.
MATERIALS AND METHODS
This is a retrospective study in which we reviewed the charts of 515 men who underwent an urodynamic study (UDS) for the evaluation of LUTS in our institution between January 2005 and August 2010.
Patients were included in the study if NIFFS was performed before the UDS. Multichannel UDS were performed according to the recommendation of the ICS.[15] Cystometrogram (CMG) were performed through a 6 Fr double lumen transurethral catheter through which a normal saline solution was infused at a rate a 20 mL/min while monitoring rectal pressure. Filling was stopped and then reduced if uninhibited bladder contractions were encountered. The bladder was filled until maximal cystometric capacity after which the PFS was performed. NIFFS and PFS were deemed adequate if more than 150 mL of urine were voided. The PVR was measured at the end of each study.
Further analyses were performed in the sub-group of men who voided a similar volume and who also had similar initial bladder volume between the two studies (both varying by less than 20%). This analysis was performed because of the known correlation between the initial urine volume in bladder, the flow rate and the voided volume.[16]
Symptoms were evaluated using standardized questionnaires according the reason of consultation. Interstitial Cystitis Symptom Index (ICSI) and Interstitial Cystitis Problem Index (ICPI) were used for painful bladder syndrome/Interstitial cystitis patients. The presence of obstructive voiding symptoms was evaluated using the International Prostate Symptom Score.
SPSS version 17.0 statistical analysis software (©SPSS Inc., Chicago, Illinois) was used to analyze and compare the different data. Results were analyzed using either the student paired T test or the Wilcoxon signed-rank test for continuous variables according to the distribution. A P value of less than 0.05 was considered statistically significant. Data are presented as the mean plus or minus standard deviation, as percentage or as the median plus or minus 25% to 75% range according to the variables and distribution.
RESULTS
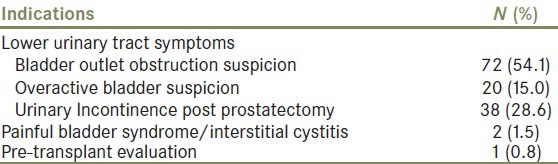
Of the 515 men whose charts were reviewed, 133 met the inclusion/exclusion criteria. Three hundred and eighty-one men were excluded either because they were not able to void during PFS or NIFFS (96 and 132 men, respectively) or because of inadequate voided volume (154 men). Of the 133 men included, 34 voided a volume varying by less than 20% between the NIFFS and PFS while having a similar volume of urine in the bladder before initiation of the micturition (sub-analyzed group). The Pdet Qmax was available in 71 patients in the overall population and in 17 patients in the sub-analyzed group. The given reasons for the missing data were technical difficulty or expulsion of the catheter during the voiding attempt which prevented the bladder pressure measurement. The presumptive diagnosis for the urodynamic studies are summarized in Table 1.
Table 1.
Indications for urodynamic study (n=133)
The mean age of the population was 63 ± 14 years old. The Qmax obtained during PFS was significantly lower than the one obtained during the NIFFS (11.0 mL/s (range 7.0-18.5) vs. 15.0 mL/s (range 9.0-23.0); P < 0.001). The difference between both Qmax was 3.0 mL/s (range 0-7.0). The median voided volume during the NIFFS was lower than during the PFS (P < 0.001; Table 2). The difference between the Qmax of both studies was greater when only the 34 men who voided similar volume were compared (18.5 mL/s (range 10.0-30.3) vs. 13.0 mL/s (range 6.0-25.0), median difference of 4.0 mL/s (range 0-9.3), in favour of the NIFFS; Table 3). The mean Pdet Qmax in the overall study population was 44.0 cm H2 O (range 30.0-65.0) while it was 40.0 cm H2 O (range 27.5-54.0) in the sub-analyzed group. Although not statistically significant, the PVR were higher after the NIFFS than after the PFS in both the study population and the sub-analysed group. However, this was probably explained by the delay found in our centre due to the UDS room set up between the end of the NIFFS and the calculation of the PVR. Such delay did not exist after the PFS.
Table 2.
Comparison of the voiding studies of the study population (n=133)

Table 3.
Comparison of the voiding studies for the sub-analysed group of patients with similar voiding volume (n=34)

Assuming the Pdet Qmax was at least the same in both studies, the bladder outlet obstruction index (BOOI) was significantly higher when the Qmax from the PFS was used (26.0 (range 6.0-43.0) vs. 17.0 (range 0-41.0), P < 0.001). When patients were separated according their classification on the ICS nomogram, we found that the resulting obstructive effect from the transurethral catheter did not correlate with severity of BOOI [Table 4]. Furthermore, according to the ICS nomogram, 32 men were classified as being unobstructed, 14 as being equivocal and 25 as being obstructed when findings of the PFS were used while similar results can be found in respectively 37, 14 and 20 men based on the findings of the NIFFS. If we analyzed only the patients in the sub-analyzed group according to the ICS nomogram, 12 were classified as being unobstructed, 1 as being equivocal and 4 as being obstructed when findings of the PFS were used while the same can be said of respectively 13, 1 and 3 men based on the findings of the NIFFS. Thus, the use of the PFS alone would have resulted in the upstaging of 14% (10/71) of cases in the study population and of 24% (4/17) in the sub-analyzed group. Paradoxically, only 1 patient would have been down staged in both groups if only the NIFFS were used.
Table 4.
Correlation between maximal flow rate (Qmax) of the non-invasive free-flow and pressure-flow studies in accordance to the classification of bladder outlet obstruction (n=74)

DISCUSSION
Urodynamic studies and especially the pressure-flow studies have been determined as being the most important tools to diagnose BOO in men.[2] Several studies have raised the possibility of the transurethral catheter used during the PFS as being itself obstructed with mixed results. It is generally accepted that transurethral catheters over 8 Fr should not be used because of their obstructive effects.[9,10,11] However, variable results exist in the literature in regard to the obstructive effect of smaller catheters.
Trumbeckas et al.[17] studied the effect of 7 Fr catheters used during the PFS in 111 men suffering from benign prostatic hyperplasia (BPH) and concluded that it lowered the Qmax by approximately 1 mL/s in patients with a mild obstruction but that it had no effect in patients classified as being unobstructed or equivocal using the BOOI. Zhang et al.[18] confirmed the mild obstructive effect of 7 Fr catheters which resulted in a lowering of the Qmax by 2.2 mL/s in comparison to NIFFS. Hermieu and colleagues[19] evaluated 260 men suffering from BPH and found that 6 Fr transurethral catheters resulted in the lowering of the maximal flow rate by 1.5 mL/s. Finally, Zhao et al.[12] examined the effect of 8 Fr transurethral catheters in 39 men who voided similar volumes between both studies and concluded that they resulted in a significant decrease of the Qmax (1.3 mL/s) which correlated with the grade of obstruction.
To the contrary, Reynard et al.[13] found no difference between the Qmax of PFS and NIFFS when an 8 Fr catheter was used in 59 men, they showed that the presence of the catheter resulted a significantly higher detrusor pressure than the presence of an intravesically placed 16 gauge epidural line. Anikwe[14] studied the effect of 6 Fr catheters in 43 men and concluded that they did not result in lower Qmax both in unobstructed men and in those with variable degree of obstruction.
Our study confirms that 6 Fr transurethral catheters do create an obstructive effect on the uroflowmetry of the PFS by lowering the maximal flow rate by 4 mL/s. This reduction of Qmax is higher than what was initially believed and did not correlate with the degree of obstruction based on the ICS nomogram.
Furthermore, according to the ICS nomogram while assuming that the Pdet Qmax was at least the same in both studies, we showed that the presence of a catheter resulted in the upstaging of 14% of men in the whole study population and up to 24% in the sub-analyzed group, although only 17 patients were included in the latter. The change of absolute BOOI calculation mainly upstaged the classification of those patients who already had a borderline index and this upstaging was never by more than one class in all of them. However, this study was not design to demonstrate the effect of a transurethral catheter on the Pdet Qmax and thus, further studies will be necessary in order to confirm these findings. Moreover, a few studies have demonstrated, that the Pdet Qmax was also falsely elevated as result of the obstruction caused by the transurethral catheter,[10,13] and not only the same as we assumed for the purpose of this study. In fact, two studies[20,21] compared the effect of transurethral catheterization to suprapubic catheterization in men suffering from benign prostatic hyperplasia. Both studies found that transurethral catheterization lowered the Qmax and resulted in a higher Pdet Qmax in comparison to a suprapubic one. Based on these studies, it is probable, but not definitive, that the upstaging is even greater that we estimated.
We believe that NIFFS may be helpful in order to lower this potential over diagnosis. In addition of being non invasive, easily performed and non expensive, it provides information on flow pattern and Qmax untainted by the obstructive effect of the transurethral catheter and thus may be more representative of the ‘normal’ voiding pattern. It is also useful in cases where patients are unable to void during PFS. Several authors have reported other non invasive methods of determining BOO in men, however, to this date, none has surpassed the PFS as the gold standard.[22]
Limitation of this study resided in its retrospective nature as well as the fact that the bladder was filled to the maximal cystographic capacity during the UDS which could have resulted in a lower Qmax due to overfilling. However, this bias was corrected in the sub-analysis group. Moreover, although filling rate was lowered in order to lower this potential limitation the bladder is under physiologic filling during the NIFFS while the filling is artificially induced in the PFS. Its low number of patients who voided similar volume and its relatively high number of patients in which the Pdet Qmax was unavailable are also limitations. Finally, this study lacks a comparison arm where a suprapubic catheter would have been used and this renders us incapable of definitely concluding on the effect of transurethral catheters on the Pdet Qmax. Nonetheless, the primary objective of this study was to evaluate the effect of transurethral catheters used during PFS on the maximal flow rate in men and to our knowledge it is one of the largest studies to show such a difference between the Qmax of both studies.
CONCLUSION
The presence of a transurethral catheter during PFS negatively affects the maximal flow rate. Furthermore, using the ICS nomogram and assuming the Pdet Qmax was the same in both studies, the presence of the catheter resulted in an upstaging of the BOO grading in up to 24% of cases. However, further studies will be necessary in order to confirm this latter finding. NIFFS in concomitance with PFS may be helpful in order to properly assess the degree of bladder outlet obstruction.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Roehrborn CG. Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH) Med Clin North Am. 2011;95:87–100. doi: 10.1016/j.mcna.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 2.Nitti VW. Pressure flow urodynamic studies: The gold standard for diagnosing bladder outlet obstruction. Rev Urol. 2005;7:S14–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths D, Höfner K, van Mastrigt R, Rollema HJ, Spångberg A, Gleason D. Standardization of terminology of lower urinary tract function: Pressure-flow studies of voiding, urethral resistance, and urethral obstruction. International Continence Society Subcommittee on Standardization of Terminology of Pressure-Flow Studies. Neurourol Urodyn. 1997;16:1–18. doi: 10.1002/(sici)1520-6777(1997)16:1<1::aid-nau1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Bruskewitz R, De La Rosette J, Griffiths D, Koyanagi T, Nordling J, et al. The diagnosis of bladder outlet obstruction: Urodynamics. In: Cockett AT, Khoury S, Aso Y, Chatelain C, Denis L, Griffiths K, et al., editors. Monaco: Proceedings of the 3rd International Consultation on BPH. 26-28 June 1995, SCI; 1996. pp. 299–367. [Google Scholar]
- 5.Chancellor MB, Blaivas JG, Kaplan SA, Axelrod S. Bladder outlet obstruction versus impaired detrusor contractility: The role of uroflow. J Urol. 1991;145:810–2. doi: 10.1016/s0022-5347(17)38458-6. [DOI] [PubMed] [Google Scholar]
- 6.Gerstenberg TC, Andersen JT, Klarskov P, Ramirez D, Hald T. High flow infravesical obstruction in men: Symptomatology, urodynamics and the results of surgery. J Urol. 1982;127:943–5. doi: 10.1016/s0022-5347(17)54140-3. [DOI] [PubMed] [Google Scholar]
- 7.Richard P, Icaza Ordonez N, Tu LM. The effect of a 6Fr catheter on pressure-flow studies in women: Are they really obstructed. Eur Urol Suppl. 2011;10:286–7. [Google Scholar]
- 8.Ryall RL, Marshall VR. The effect of a urethral catheter on the measurement of maximum urinary flow rate. J Urol. 1982;128:429–32. doi: 10.1016/s0022-5347(17)52953-5. [DOI] [PubMed] [Google Scholar]
- 9.Klingler HC, Madersbacher S, Schmidbauer CP. Impact of different sized catheters on pressure-flow studies in patients with benign prostatic hyperplasia. Neurourol Urodyn. 1996;15:473–8. doi: 10.1002/(SICI)1520-6777(1996)15:5<473::AID-NAU4>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 10.Klausner AP, Galea J, Vapnek JM. Effect of catheter size on urodynamic assessment of bladder outlet obstruction. Urology. 2002;60:875–80. doi: 10.1016/s0090-4295(02)01873-3. [DOI] [PubMed] [Google Scholar]
- 11.Lose G, Thunedborg P, Colstrup H, Jørgensen L. Spontaneous versus intubated flow in male patients. Urology. 1988;32:553–6. doi: 10.1016/s0090-4295(98)90044-9. [DOI] [PubMed] [Google Scholar]
- 12.Zhao SC, Zheng SB, Tan WL, Mao XM, Zhang P, Huang ZM, et al. [Effects of transurethral catheterization on uroflow rate in the pressure-flow study of patients with benign prostatic hyperplasia] Zhonghua Nan Ke Xue. 2007;13:710–2. [PubMed] [Google Scholar]
- 13.Reynard JM, Lim C, Swami S, Abrams P. The obstructive effect of a urethral catheter. J Urol. 1996;155:901–3. [PubMed] [Google Scholar]
- 14.Anikwe RM. The effect of a 6FG urethral catheter on urinary flow in benign prostatic hypertrophy. Int Surg. 1976;61:417–8. [PubMed] [Google Scholar]
- 15.Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: Uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21:261–74. doi: 10.1002/nau.10066. [DOI] [PubMed] [Google Scholar]
- 16.Drach GW, Layton TN, Binard WJ. Male peak urinary flow rate: Relationships to volume voided and age. J Urol. 1979;122:210–4. doi: 10.1016/s0022-5347(17)56333-8. [DOI] [PubMed] [Google Scholar]
- 17.Trumbeckas D, Milonas D, Jievaltas M, Danilevicius M, Matjosaitis AJ. Influence of catheter on urinary flow during urodynamic pressure-flow study in men with symptomatic benign prostatic hyperplasia. Medicina (Kaunas) 2006;42:15–21. [PubMed] [Google Scholar]
- 18.Zhang P, Wu ZJ, Gao JZ. Impact of catheter on uroflow rate in pressure-flow study. Chin Med J (Engl) 2004;117:1732–4. [PubMed] [Google Scholar]
- 19.Hermieu JF, Ravery V, Le Coent R, Delmas V, Boccon-Gibod L. Effects of a 6F urethral catheter on uroflowmetry in men with benign prostatic hypertrophy. Prog Urol. 1998;8:1035–8. [PubMed] [Google Scholar]
- 20.Walker RM, Di Pasquale B, Hubregtse M, St Clair Carter S. Pressure-flow studies in the diagnosis of bladder outlet obstruction: A study comparing suprapubic and transurethral techniques. Br J Urol. 1997;79:693–7. doi: 10.1046/j.1464-410x.1997.00143.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhao SC, Zhang P, Huang ZM, Zuo Y, Mao XM, Zheng SB. Suprapubic puncture: Preferable to transurethral catheterization for pressure-flow determination in BPH patients. Zhonghua Nan Ke Xue. 2008;14:973–6. [PubMed] [Google Scholar]
- 22.Belal M, Abrams P. Non-invasive methods of diagnosing bladder outlet obstruction in men. Part 2: Non-invasive urodynamics and combination of measures. J Urol. 2006;176:29–35. doi: 10.1016/S0022-5347(06)00570-2. [DOI] [PubMed] [Google Scholar]


