Abstract
Importance
Chronic periodontitis, a destructive inflammatory disorder of the supporting structures of the teeth, is prevalent in patients with diabetes. Limited evidence suggests that periodontal therapy may improve glycemic control.
Objective
To determine if non-surgical periodontal treatment reduces hemoglobin A1c (HbA1c) in persons with type 2 diabetes (DM) and moderate to advanced chronic periodontitis.
Design, Setting and Participants
The Diabetes and Periodontal Therapy Trial (DPTT) is a 6-month, single-masked, randomized, multi-center clinical trial. Participants had DM, were taking stable doses of medications, had HbA1c ≥7% and <9%, and untreated periodontitis. Five hundred fourteen participants were enrolled between November 2009 and March 2012 from diabetes and dental clinics and communities affiliated with five academic medical centers.
Intervention
The treatment group (n=257) received scaling and root planing plus chlorhexidine oral rinse at baseline, and supportive periodontal therapy at three and six months. The control group (n=257) received no treatment for six months.
Main Outcome Measure
Difference in HbA1c change from baseline between groups at six months. Secondary outcomes included changes in probing pocket depths, clinical attachment loss, bleeding on probing, gingival index, fasting glucose, and the Homeostasis Model Assessment (HOMA2).
Results
Enrollment was stopped early due to futility. At 6 months, the periodontal therapy group increased HbA1c 0.17% (1.0) (mean (SD)) compared to 0.11% (1.0) in the control group, with no significant difference between groups based on a linear regression model adjusting for clinical site (mean difference = -0.05%; 95% Confidence Interval (CI): -0.23%, 0.12%; p=0.55). Probing depth, clinical attachment loss, bleeding on probing and gingival index measures improved in the treatment group compared to the control group at six months with adjusted between-group differences of 0.33mm (95% CI: 0.26, 0.39), 0.31mm (95% CI: 0.23, 0.39), 16.5% (95% CI: 12.9, 20.0) and 0.28 (95% CI: 0.21, 0.35), respectively; all p values <0.0001).
Conclusions and Relevance
Non-surgical periodontal therapy did not improve glycemic control in patients with DM and moderate to advanced chronic periodontitis. These findings do not support the use of nonsurgical periodontal treatment in patients with diabetes for the purpose of lowering HbA1c.
Keywords: Diabetes, Diabetes Mellitus, Type 2, Periodontal Disease, Periodontitis, Glycated Hemoglobin, HbA1c
Introduction
Emerging evidence implicates inflammation in the pathogenesis of type 2 diabetes (DM). 1,2 Chronic periodontitis, a destructive inflammatory disorder of the soft and hard tissues supporting the teeth,3 is a major cause of tooth loss in adults.4 Nearly half of the U.S. population over the age of 30 is estimated to have chronic periodontitis, with 38% having moderate or advanced disease. 5 Individuals with DM are at greater risk for incident and prevalent chronic periodontitis and have more severe chronic periodontitis than individuals without diabetes. 6-10 Well-controlled diabetes is associated with less severe chronic periodontitis and a lower risk for periodontitis progression, 8,11,12 suggesting that level of glycemia is an important mediator of the relationship between diabetes and chronic periodontitis risk. Evidence that chronic periodontitis is in the causal pathway of DM, however, is observational, limited, and inconsistent.
Several small interventional studies have suggested that chronic periodontitis treatment may improve metabolic control of patients with DM. A meta-analysis of these clinical trials 13 found a non-significant weighted average decrease of HbA1c three months following periodontal therapy of 0.38% (95% CI -1.5-0.7). A subsequent trial by Jones et al 14 involving 165 participants resulted in a mean non-significant reduction in HbA1c of 0.65% four months after periodontal therapy, but that study was underpowered. Therefore, the Diabetes and Periodontal Therapy Trial (DPTT) was designed to determine whether non-surgical periodontal therapy (scaling and root planing and supportive periodontal therapy), compared to no therapy, reduces HbA1c at 6 months in persons with DM and moderate to advanced chronic periodontitis.
Methods
Trial design and setting
The Diabetes and Periodontal Therapy Trial (DPTT) was a multicenter, randomized, single-masked, clinical trial that enrolled participants from outpatient medical and dental clinics and communities of five academic medical centers in the United States. A more detailed description of the methods and rationale for the DPTT has been published elsewhere. 15 The study protocol was approved by institutional review boards at each participating center, and all participants provided written informed consent. An independent Data and Safety Monitoring Board (DSMB) reviewed the safety data throughout the trial.
Participants
Participants were recruited between November 2009 and March 2012. Men and women ages 35 years and older were eligible if they had physician-diagnosed DM of more than three months duration, an HbA1c value >7.0% and <9.0% at screening, reported no changes in diabetes medications within the last 3 months, were under the care of a physician for their diabetes, agreed to not change diabetes medications during the trial unless medically indicated, and agreed to avoid pregnancy while in the trial. Participants required a diagnosis of moderate to advanced chronic periodontitis defined as clinical attachment loss and probing depth of at least > 5mm in 2 or more quadrants of the mouth,16 a minimum of 16 natural teeth, and no periodontal treatment in the prior 6 months. Radiographs were used to confirm a diagnosis of chronic periodontitis. Participants needing treatment of extensive tooth decay, tooth abscesses, or other oral infection such as teeth needing root canal therapy, were excluded. Additional exclusion criteria included limited life expectancy, diabetes-related emergency within 30 days, use of non-steroidal anti-inflammatory (NSAID) medications other than daily low dose aspirin (75-325mg), use of immunosuppressive medications, antibiotic use (>7 days within 30 days of enrollment), dialysis, risk of bleeding complications, or heavy alcohol consumption (>3 drinks/day for men and >2/day for women).
Data Collection
Data were collected by trained and certified study personnel; periodontal examiners were also calibrated before examining participants and annually thereafter.17 Study personnel recorded medical history, medication use, demographics, and life-style information. Ethnicity was self-reported using multiple choice questions according to NIH-specified categories. Participants were allowed to provide options not included in the administered questions. Height, weight, and blood pressure were measured in duplicate. The oral examination included probing depth, clinical attachment loss, and bleeding on probing from six locations around each tooth, and plaque index and gingival index18 from six index teeth.
Study Procedures
Recruitment occurred during diabetes or dental care visits, or referral from community medical practices or local advertisements. Potential participants were screened for periodontitis and HbA1c level. Eligible individuals were randomized using a permuted-block randomization scheme, stratified by clinical site, with block sizes of 2, 4 or 6.
Laboratory measures
Fasting venous blood samples were collected prior to periodontal measures or therapy. Fresh whole blood samples were refrigerated and sent on ice within four days to the study's core laboratory (University of Minnesota) for analysis of HbA1c by high performance liquid chromatography (Tosoh HPLC G7 Glycohemoglobin Analyzer, Tosoh Medics, Inc, San Francisco, CA). Serum and plasma aliquots were snap frozen and shipped on dry ice for analysis of lipids, creatinine and fasting glucose by enzymatic methods on a Roche Chemistry Analyzer (Roche Diagnostics Corporation, Indianapolis, IN), and insulin by sandwich immunoassay on a Roche Elecsys 2010 Analyzer (Roche Diagnostics Corporation). HOMA2 scores were calculated from fasting glucose and insulin values of non-insulin users using the HOMA2 Calculator version 2.2 (http://www.dtu.ox.ac.uk/index.php?maindoc=/homa/).
Study Intervention
Initial treatment consisted of at least 160 minutes of scaling and root planing using curettes and ultrasonic instruments with local anesthetic during two or more sessions completed within 42 days of the baseline visit.15 Completeness of therapy was assessed by the study therapist and confirmed by a study periodontist. Following treatment, the therapist provided oral hygiene instructions and dispensed chlorhexidine gluconate 0.12% oral rinse (twice daily for two weeks), toothbrush, toothpaste and dental floss. Three and 6 months following the baseline visit, treatment group participants received scaling and root planing for approximately one hour during a single session, and oral hygiene instructions. Control group participants received only oral hygiene instructions at the baseline and 3- and 6-month visits. Following their 6-month visit, control group participants were offered scaling and root planing.
Outcome Assessment
The primary study outcome was the change in HbA1c from baseline to 6 months. Secondary outcomes included 3-month change in HbA1c, and change in 3- and 6-month fasting glucose, HOMA2 and clinical measures of chronic periodontitis. Change in diabetes medications at 3 and 6 months and the need for periodontal rescue therapy and diabetes rescue therapy were evaluated as safety outcomes. A change in medication was defined as more than two-fold change in dosage for a hyperglycemic drug, or more than 10% for insulin, or by addition or subtraction of an oral hyperglycemic agent or insulin.
Adverse events and Safety Monitoring
Oral symptoms were recorded two weeks following treatment (treatment group) or baseline for the control group. Rescue therapy was performed on any participant who experienced progressive periodontitis.15 After the trial, participants were referred for follow-up periodontal care or additional treatment as needed.
Masking
Periodontal examiners and laboratory personnel who performed the HbA1c analyses were masked to treatment group assignment.
Statistical Analyses
The trial's sample size was estimated assuming a 6-month reduction from baseline in HbA1c of 0.6% (SD 2%)19 or greater in the treatment than control group. Based on a two-tailed, two-sample t-test and 0.05 type I error, a sample size of 468 participants was required to achieve 90% power. Assuming an attrition rate of 20%, the planned sample size was 600 participants (300 in each treatment group).
Baseline characteristics were summarized for continuous variables by means (SD) and/or medians (interquartile ranges) and for categorical variables by frequencies (percentages). Mean periodontal measures (and changes) were computed as a per-person average, and averaged across participants within each treatment group. Between-group baseline comparisons were based on two-sample t-tests or Wilcoxon Mann-Whitney tests for continuous, and χ2 tests for categorical variables. The primary outcome, change in HbA1c, was analyzed using the intention-to-treat principle using linear extrapolation with multiple imputation to impute missing 6-month HbA1c values. A sensitivity analysis using different approaches including no imputation, last observation carried forward, and multiple imputation showed similar results for the primary outcome and the treatment effect. The primary efficacy analysis was performed using linear regression models to evaluate 6-month HbA1c change (follow-up - baseline) as the dependent variable, with treatment group as the independent factor and clinical site as a covariate. Homogeneity of clinical site was evaluated using the F-test based on linear regression model. The secondary efficacy analysis used linear regression models that included selected baseline variables as covariates, e.g. HbA1c, gender, age, ethnicity, smoking status, body mass index, diabetes medication usage and duration of diabetes, to evaluate main effects of covariates; interactions with treatment group were tested using F-tests. A “per protocol” analysis based on data available both at baseline and the 6-month visit, was also performed without imputation. Subgroup analyses were pre-planned for gender and ethnicity. Additional post-hoc subgroup analyses were also conducted. Between-group comparisons in changes of 3- month HbA1C and additional secondary outcomes (periodontal measurements (probing depth, clinical attachment loss, bleeding on probing, gingival index and plaque index), fasting glucose, fasting insulin, HOMA2 insulin resistance and HOMA2 β-cell function), weight and blood pressure at the 3- and 6-month visits also used linear regression models. P values < 0.05 were adjusted for multiple comparisons using Bonferroni's correction. All statistical analyses were performed using SAS v.9.3 (SAS Institute, Cary, NC).
One futility analysis was planned after the first 300 participants completed their 6-month visit. Stopping guidelines were based on a two-sided, independent t-test and predetermined conditional power threshhold.20
Results
Participants
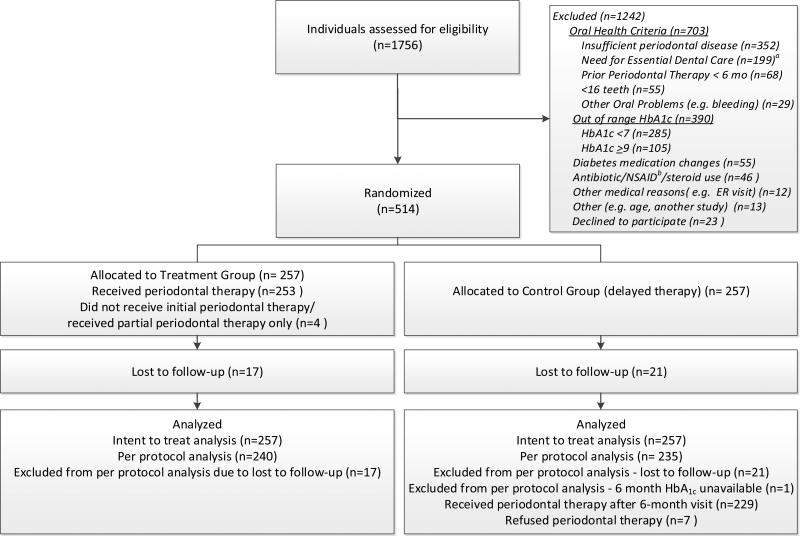
1,756 individuals were screened and 514 were randomized from November 2009 and March 2012 (Figure 1), at which time enrollment was stopped because of futility. The guidelines for terminating DPTT for futility were based on a primary conditional power threshold of 40% and required an observed interim test statistic less than -0.12. Since the futility analysis t-test statistic for the primary outcome was -0.37, the DSMB recommended cessation of recruitment and continued follow up of enrolled participants.
Figure 1.
DPTT Participant Flow Chart
a Essential Dental Care – defined as participants needing treatment of extensive tooth decay, tooth abscesses, or other oral infections: b Non-steroidal anti - inflammatory drug
Ninety-three percent of randomized participants completed the study with similar retention in the treatment (240/257) and control groups (236/257).
Baseline characteristics were similar between groups and were reflective of individuals with DM and periodontitis (Table 1). Forty-seven percent (224/514) of participants used oral hypoglycemic agents alone, 16% (80/514) insulin alone, and 35% (179/514) both. Only 2% (11/514) were not taking diabetes medications.
Table 1.
General Baseline Characteristics of DPTT Participants by Study Group
| Characteristics | Treatment Group (N=257) | Control Group (N=257) |
|---|---|---|
| Age, mean (sd), years | 56.7 (10.5) | 57.9 (9.6) |
| Female, No. (%) | 114 (44.4) | 123 (47.9) |
| Race, No. (%) | ||
| African American/ Black | 76 (29.6) | 70 (27.2) |
| White | 140 (54.5) | 140 (54.5) |
| Other(e.g., Native American, Asian) | 41 (16.0) | 47 (18.3) |
| Hispanic, No. (%) | 81 (31.5) | 85 (33.1) |
| Smoking history, No. (%) | ||
| Never smoked | 129 (50.2) | 144 (56.0) |
| Former | 89 (34.6) | 86 (33.5) |
| Current | 39 (15.2) | 27 (10.5) |
| Diabetes factors, mean (SD) | ||
| HbA1c, % | 7.8 (0.65) | 7.8 (0.60) |
| HbA1c, No. (%) | ||
| <7.0 | 12 (4.7) | 10 (3.9) |
| >7.0 to <8.0 | 143 (55.6) | 154 (59.9) |
| >8.0 to <9.0 | 93 (36.2) | 86 (33.5) |
| >9.0 to <10 | 9 (3.5) | 7 (2.7) |
| Fasting glucose, mg/dL , median | 150 | 147 |
| IQR | (125 – 174) | (122 – 172) |
| Duration of diabetes, years | 12.3 (8.2) | 11.3 (8.4) |
| Fasting insulin, (pmol/L), excluding insulin usea | ||
| median | 95 | 88 |
| IQR | (61 – 138) | (61 – 133) |
| HOMA2 insulin sensitivity (%S), excluding insulin usea,b | ||
| median | 50.1 | 53.9 |
| IQR | (34.1 – 77.0) | (38.0 – 79.0) |
| HOMA2 β-cell function (%β), excluding insulin use a,b | ||
| median | 55.5 | 52.0 |
| IQR | (34.1 – 76.2) | (36.7 – 76.0) |
| Hypoglycemic medications, No. (%) | ||
| No diabetes medications | 7 (3) | 4 (2) |
| Oral agents only | 117 (46) | 127 (49) |
| Insulin only | 40 (16) | 40 (16) |
| Combination of medications | 93 (37) | 86 (33) |
| Anthropometrics, mean (SD) | ||
| Weight, kg | 99.5 (24.3) | 97.5 (21.7) |
| BMI, kg/m2 | 34.7 (7.5) | 34.2 (6.7) |
| Blood pressurec, mean(sd), mm Hg | ||
| Systolic | 133.1 (20.7) | 135.1 (20.4) |
| Diastolic | 78.8 (12.3) | 78.8 (10.9) |
| Cardiovascular disease factors, mg/dL, median IQR | ||
| Cholesterol, median, IQR, excluding statin used | ||
| Cholesterol | 189 | 185 |
| IQR | (162 – 211) | (161 – 212) |
| Low-density lipoprotein | 113 | 108 |
| IQR | (92 – 135) | (94 – 130) |
| High density lipoprotein | 46 | 41 |
| IQR | (38 – 53) | (37 – 48) |
| Triglycerides, median, excluding statin used | 117 | 126 |
| IQR | (89 – 169) | (93 – 231) |
| Creatinine, median | 0.81 | 0.81 |
| IQR | (0.68 – 1.0) | (0.67 – 0.98) |
| Periodontal measurementse, mean (SD) | ||
| Number of teeth (count/person) | 25.4 (3.7) | 24.7 (3.6) |
| Probing depth (PD) (mm, mean sites/person) | 3.3 (0.6) | 3.3 (0.7) |
| # sites | ||
| ≥4mm | 51.3 (27.3) | 49.2 (27.5) |
| ≥5mm | 28.9 (21.6) | 28.0 (22.3) |
| ≥7mm | 3.5 (6.3) | 3.5 (8.2) |
| % sites | ||
| ≥4mm | 33.8 (17.6) | 33.6 (18.7) |
| ≥5mm | 19.0 (14.2) | 19.3 (15.6) |
| ≥7mm | 2.3 (4.2) | 2.5 (6.1) |
| Clinical Attachment loss (CAL) (mm, mean sites/person) | 3.5 (0.8) | 3.5 (0.9) |
| # sites | ||
| ≥4mm | 60.1 (30.7) | 57.5 (30.7) |
| ≥5mm | 35.9 (25.9) | 33.6 (26.0) |
| ≥7mm | 6.6 (9.7) | 6.9 (11.9) |
| % sites | ||
| ≥4mm | 40.3 (21.1) | 39.5 (21.3) |
| ≥5mm | 24.3 (18.2) | 23.4 (18.6) |
| ≥7mm | 4.7 (7.3) | 5.0 (9.2) |
| Bleeding on probing (BOP) (% sites/person) | 61.2 (24.1) | 59.6 (26.0) |
| Gingival Index (GI) (mean sites/person) | 1.4 (0.4) | 1.4 (0.4) |
| Plaque Index (PLA) (% sites/person) | 86.7 (17.9) | 84.5 (20.8) |
| Self-reported overall health, No. (%) | ||
| Excellent – very good | 50 (19.5) | 59 (23.0) |
| Good | 123 (47.9) | 138 (53.7) |
| Fair – poor | 84 (32.6) | 60 (23.3) |
| Other medical history, No. (%) | ||
| Angina | 21 (8.2) | 11 (4.3) |
| Myocardial infarction | 22 (8.6) | 21 (8.2) |
| Stroke | 12 (4.7) | 12 (4.7) |
| Hypertension | 180 (70.0) | 184 (71.6) |
| Kidney disease | 14 (5.4) | 12 (4.7) |
| Other medication use, No. (%) | ||
| Blood pressure | 202 (78.6) | 210 (81.7) |
| Cholesterol | 172 (66.9) | 170 (66.1) |
Limited to non-insulin users: n=133 treatment group; 488 n=138 control group
HOMA2 - calculated using the HOMA2 calculator version 2.2 (http://www.dtu.ox.ac.uk/homacalculator/index.php).
Includes blood pressure measurements for all participants independent of reported blood pressure medication use.
Non-statin users: n=85 Treatment Group; n=87 Control Group
Each periodontal measurement was evaluated on 6 sites of each tooth. A participant-based summary measurement was determined by first calculating an average of the six sites per tooth and then calculating an average for all teeth measured for that participant.
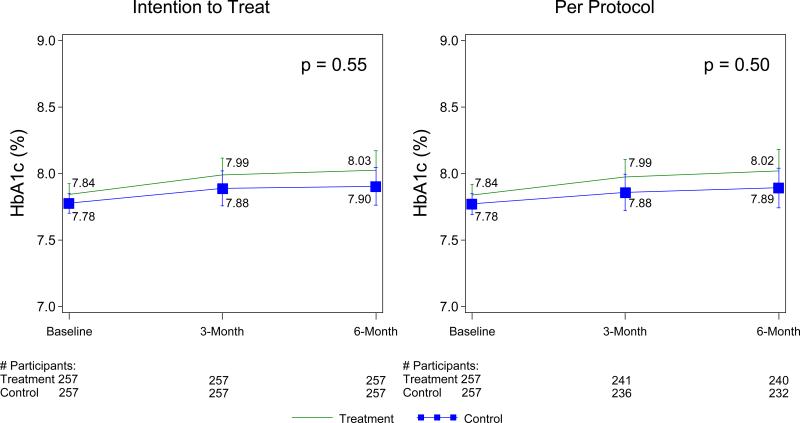
Primary outcome
HbA1c did not change significantly between baseline and the 3-month or 6-month visits in either the treatment or control group (Figure 2 and Table 2) and the target six-month reduction of HbA1c of 0.6% or greater was not achieved. In the intention-to -treat analysis of the primary outcome based on a linear regression model including clinical site as a covariate, 6-month HbA1c change did not differ significantly between the treatment and control groups (adjusted 6-month treatment effect (95% CI) = -0.05% (-0.23%, 0.12%); p=0.55). Three-month results were similar. No significant differences in Hba1c results across centers were found (p= 0.44 (intention to treat); p=0.59 (per protocol) based on F-test for homogeneity from the linear regression model).
Figure 2.
Hemoglobin A1c Levels at Baseline and Follow-up Mean values and standard errors are presented at each visit.
P-values comparing 6-month change in Hb A1c between the two treatment groups were based on t-tests from linear regression models with 6-month HbA1c change as a dependent variable, treatment group and Clinical Site as covariates.
Table 2.
3-month and 6-month Change in HbAlc by Treatment Group
| Baseline | 3- month Change (Δ=3-month - Baseline) | 6- month Change (A=6-month - Baseline) | ||||||
|---|---|---|---|---|---|---|---|---|
| Treatment | Control | Treatment | Control | Treatment | Control | |||
| Study Outcome | mean (SD) | mean (SD) | meana 95% C.I.) | meana (95% C.I.) | p voluea | meana (95% C.I.) | meana (95% C.I.) | p voluea |
| Intent to Treat | N=257 | N=257 | N=257 | N=257 | N=257 | N=257 | ||
| HbA1c(%) | 7.84 (0.65) | 7.78 (0.60) | 0.l4 (0.02, 0.27) | 0.ll (−0.02, 0.24) | 0.64 | 0.l5 (−0.01, 0.30) | 0.09 (−0.06, 0.25) | 0.55 |
| Per protocolb | N=240 | N=235 | N=233 | N=228 | N=240 | N=235 | ||
| HbA1c(%) | 7.84 (0.65) | 7.77 (0.60) | 0.l3 (−0.01, 0.26) | 0.08 (−0.05, 0.22) | 0.57 | 0.l5 (−0.02, 0.32) | 0.09 (−0.09, 0.26) | 0.50 |
Mean changes and 95% CI's were determined from linear regression models with 3-month and 6-month change in HbAjC included as dependent variables, treatment group as an independent factor and the Clinical Site as a covariate; p-values were based on t-tests comparing mean changes between the two groups.
Per protocol: Analyses were based on all participants with HbAlc data at the 6-month visit (n=240 in the Treatment group, n=235 in the Control Group). 6 participants in the Treatment Group and 7 in the Control Group missed their 3 month visit. HbAlc data were not available for one additional Treatment Group participant at 3 months.
Secondary outcomes
A per protocol linear regression analysis evaluating change in HbA1c did not reveal HbA1c differences between groups at either time point (adjusted treatment effect (95% CI) =-0.07% (-0.26%, 0.13%); p= 0.50) (Table 2).
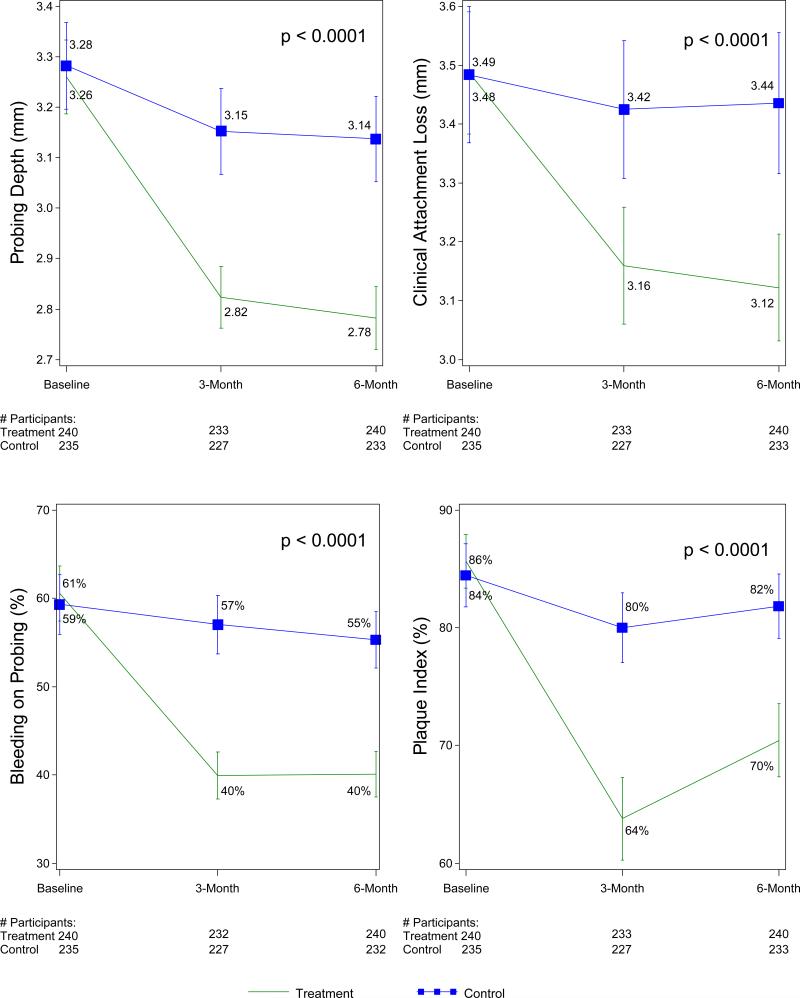
Using linear regression models, all periodontal clinical parameters improved significantly at 3 months and were sustained at 6 months in the treatment but not the control group. (Figure 3 and e-Table 2). At 6 months, mean (95% CI) probing depth improved by 0.42 mm (0.36, 0.48) in the treatment group compared to 0.14mm (0.08, 0.21) in the control group (adjusted treatment effect (95% CI) of 0.33mm (0.26, 0.39); p (Bonferroni's correction) <.0001). In the treatment group, bleeding on probing decreased by 19.0% (15.7, 22.4) (mean (95% CI)) compared with 5.9% (2.3, 9.6) for the control group (adjusted difference (95% CI): 16.5% (12.9, 20.0); p (Bonferroni's correction) <.0001). Clinical attachment loss and gingival index measures also improved more in the treatment group compared to the control group (adjusted between-group differences were 0.31mm (95% CI: 0.23, 0.39) and 0.28 (95% CI: 0.21, 0.35), respectively; both p values <0.0001). A post-hoc subgroup comparison of treatment groups by response tertiles likewise revealed no significant differences between groups at any time point (eTable 1). Changes in blood pressure, weight, fasting glucose, fasting insulin and HOMA2 sensitivity (%s) and HOMA2 β-cell function (%β) are summarized in eTable 3. All these measurements remained stable during follow-up, with no significant differences between groups. Of the 462 participants with medication data available at all study visits, 55% (128/233) in the treatment group and 60% (137/229) in the control group had no protocol-defined changes in diabetes medications during the study.
Figure 3.
Periodontal Measurements at Baseline and Follow-up (Per Protocol)
Mean values and standard errors are presented at each visit.
P-values comparing 6-month changes in periodontal outcomes between the two treatment groups were based on t-tests from linear regression models with 6-month periodontal change as a dependent variable, treatment group and Clinical Site as covariates.
Safety
The DPTT was a low risk study and no study related serious adverse events occurred. Two weeks after completion of treatment or baseline, the treatment group experienced more soreness/tenderness/pain than the controls (40.2% (102/254) and 28.1% (72/257) respectively; p <0.01(based on chi-square test), and thermal sensitivity (31.9% (81/254) vs. 18.3% (47/257), respectively (p <0.01(based on chi-square test)). These symptoms are commonly reported following scaling and root planing.14 Few participants, (4/241 in the treatment group and 5/236 in the control group) required generalized periodontal rescue therapy during the study.
Discussion
The DPTT is to our knowledge the largest multi-center, randomized, clinical trial to investigate the effect of periodontal therapy on measures of glycemic control in patients with DM and chronic periodontitis. Despite its effectiveness in improving clinical measures of periodontitis, periodontal therapy did not significantly change HbA1c after 3 or 6 months in the treatment group, and no differences in HbA1c change were observed between the treatment and control groups. Findings were similar in the intent-to-treat and the per-protocol analysis. Likewise, periodontal therapy had no significant effect on fasting glucose or the HOMA2 score. Current treatment guidelines 21,22 do not include periodontal therapy as a means of achieving glycemic control, and the results of our study support those treatment guidelines. However, though not specifically evaluated in our study, periodontal therapy may be considered in patients with DM for reasons other than glycemic control, such as for benefits to tooth retention and masticatory function.
These results are in contrast to recently published meta-analyses that showed a modest (0.36% CI 0.54- 0.19) but significant reduction in HbA1c following periodontal therapy.23 A number of features of the present study may account for these differences. First, all previous trials were small, while DPTT had greater than 90% power to detect a clinically meaningful difference between groups in HbA1c change from baseline of 0.6%, even with early cessation of trial enrollment. Secondly, our trial enrolled participants who were under the care of a physician for their diabetes and who were within a range of HbA1c values that would be less likely to trigger a change in medications during the study period. The DPTT enrollment criteria excluded individuals who had experienced a recent change in hypoglycemic medications, and we monitored changes of hypoglycemic medication and insulin during the study period. Changes in diabetes medications during the DPTT were similar between treatment groups and may in part account for absence of differences in HbA1c outcome. This aspect of the DPTT study design was critical since medications may have profound short-term influence on HbA1c levels and have not been adequately documented in previous studies. Also, meta-analyses of small trials have been reported to be subject to high false positive rates. 24-26 Finally, it is possible that periodontal inflammation and infection in fact do not influence glycemic control. Indeed, the results of this trial indicate that glycemic control worsened, although not significantly, six months following study therapy.
The largest previous trial of periodontal treatment and glycemic control (n=157) reported a non-statistically significant HbA1c reduction of 0.36% in the treatment compared with the control group after three months. 27 Another study of 132 male Veterans Administration participants14 failed to demonstrate a positive effect on glycemic control. The results of the DPTT are consistent with the latter study.
Possible limitations to the present study should be considered. Our periodontal treatment did not include systemic or topical antibiotics nor was any participant treated surgically due to the difficulties of standardizing a surgical protocol. Systemic antibiotics were not used so as not to confound the effects of the study intervention. However, a recent study that administered systemic antibiotics in addition to scaling and root planing in patients with metabolic syndrome likewise did not achieve a reduction in glycemic control.28 While probing depths and clinical attachment levels were significantly improved in the treatment group, dental plaque and bleeding score improvements were only modest and indicate that changing oral hygiene habits remains a challenge. A subgroup comparison by tertiles of response, however, did not reveal HbA1c differences even among those with the largest improvements in periodontal parameters. Since DPTT participants were enrolled with HbA1c > 7% and <9%, we cannot rule out the possibility that individuals with values outside of this range might experience HbA1c reduction following periodontal treatment.
The DPTT had a number of strengths. The sample size was sufficient to ensure adequate statistical power to detect a meaningful clinical difference in HbA1c. The study population was geographically and ethnically diverse, increasing generalizability of the results. A thorough screening and enrollment process ensured that participants met eligibility criteria and retention was high, with 93% of participants completing the trial. Diabetes medication changes were monitored during follow up. Periodontal treatment was conducted under supervision, averaging 190 minutes of treatment per individual, and resulted in a positive effect on clinical measures of periodontitis among participants in the treatment group. The magnitude of clinical change achieved was consistent with results of other multi-center trials of non-surgical therapy in non-diabetic populations. 29,30 The DPTT core laboratory responsible for the centralized analysis of blood samples is a reference laboratory for the analysis of HbA1c in North America.31
Conclusions
In conclusion, this multi-centered randomized clinical trial of non-surgical periodontal treatment for participants with DM and chronic periodontitis did not demonstrate a benefit to measures of glycemic control. Although periodontal treatment improved clinical measures of chronic periodontitis in patients with DM, the findings do not support the use of nonsurgical periodontal treatment for the purpose of lowering HbA1c.
DPTT Study Group
DPTT Study Group
Study Chair (Stony Brook University): Steven Engebretson, DMD, MS, MS(Study Chair); Marie Gelato, MD, (Diabetes Consultant); Baljit Moonga, PhD, (Assistant to Study Chair) (7/08-3/10); Ruth Tenzler, RN,BSN, CCRC (Assistant to Study Chair), (4/10-present).
Coordinating Center (Stony Brook University Medical Center: Leslie Hyman, PhD(PI); Elinor Schoenfeld, PhD (Co-PI); Li Ming Dong, PhD, (Lead Biostatistician), (7/09-6/10); Melissa Fazzari, PhD (Lead Biostatistician) (5/11-5/12); Wei Hou, PhD (Lead Biostatistician) (11/12-present); Gail Lerner, MS (Data Analyst) (1/10-1/13); Hao Chen, (PhD Candidate) Student Data Analysis (1/12-present); Soyoun Lee (PhD Candidate), Student Data Analysis (11/12-present); Colette Knuth, PhD (Study Coordinator) (3/09-8/10); Jayme Mendelsohn, MA, (Data Entry),(9/09-12/10); Gabriel Pietrzak, MPH (Study Coordinator) (12/10-11/11); Catherine Hytner, BA (Assistant Study Coordinator) (5/11-1/13); Lisa Snelling, BA (Assistant Study Coordinator) (8/11-5/13); Sakeena Ahmed (Data Entry) (1/09-8/10); Maria Rodriguez; (Data Entry), (7/08-12/12); Michael Merin (9/10-4/11); Joanna Merin (Data Entry) (3/11-6/12); Leanne Merill, MA (Data Entry) (11/11-6/13); Lydia Seib, AAS (Administrative Assistant) (8/08-present).
Clinical Centers
University of Alabama at Birmingham: Michael Reddy, DMD, DMSc (PI) ; Cora Lewis, MD, MSPH, FACP, FAHA, (Diabetologist); Nicolaas Geurs, DDS, MS (Masked Periodontal Examiner); Phillip Vassilopoulos, DDS (Back-up Masked Examiner); Adrian Abrahams, DMD, (Study Therapist) (8/09-6/11); Jennifer Doobrow, DMD,(Study Therapist) (8/09-7/10); Maria Geisinger, DDS, MS (Study Therapist and Phlebotmist); Simha Kukunooru, (Study Therapist) (8/09-7/10); Curry Leavitt, DMD, (Study Therapist), (8/09-7/10); Juan Pardo, DDS, (Study Therapist), (8/09-6/11); Ramzi Abou Arraj, DDS, (Study Therapist); Anothy Reganato, (Study Therapist) (8/09-7/10); Kristi Simmons, DMD (Study Therapist) (8/09-6/11); Erik Unger, DDS, (Study Therapist), (8/09-6/11); Jennifer Bain, DMD (Study Therapist); Kathleen Beaudry, DMD, (Study Therapist), (10/09-8/12); Michael Nguyen, DDS, (Study Therapist) (2/10-6/12); Ruben Sauceda, DDS, (Study Therapist) (11/10-6/12); Jared Bauerle, DMD, (Study Therapist), (3/11-present); Michael Madigan, DMD, (Study Therapist), (3/11-6/13); Thanos Ntounis , DDS, (Periodontal Resident),(3/11-6/13); Maninder Kaur, BDS, MS, (Clinical Research Assistant) (5/11-6/13); Alvin Stevens, DMD (Study Therapist) (7/11-present); Susanna Goggin, DMD, (Study Therapist) (10/11-present); Lillie Pitman, DMD, (Study Therapist), (10/11-present); Kyle Trammel, DMD (Study Therapist), (10/11-6/13); C Peterson (1/12-present); Sandra Haigh, BS, MS, (Study Coordinator); Javetta Jackson, (Study/Clinic Coordinator) (8/09-4/11); Erin Finch, BSN, (Study Coordinator/Administrator), (10/11-4/12); Sheila Akers, (Asst. Clinical Coordinator); Vivian Stoyanova Grant (Study/Clinic Coordinator) (3/11-5/12); Sushma Acharya, BDS, (Asst. Clinical Coordinator), (4/11-8/11); Stephanie McLean, MS (Study Coordinator) (10/11-present); Janet Turman, BS (Recruiter); Jackie Roche, (Recruiter) (2/10-3/12); Charlotte Bragg, BA, MS, RD (Recruiter) (8/09-10/10); Rupa Rajanna, BDS, (Assistant Clinic Coordinator) (8/09-8/10; Elizabeth Bolton (Administrative Assistant). University of Minnesota/Hennepen County Medical Center (HCMC): Bryan Michalowicz, DDS (PI); Anthony DiAngelis, DMD, MPH, (PI-HCMC); Elizabeth Seaquist, MD, (Diabetologist PI); Judy Danielson, RDH, (Masked Periodontal Examiner); Pat Lenton, RDH, BS, MA (Recruiter/Retention Back-up Study Therapist); Larry Wolff, DSS, PhD (Backup Examiner) (2/10-present); Pamela Thibado, RDH, (Treatment/Recruiter) (2/10-9/12); Satya Molletti, (Dentist/Therapist) (4/10-11/12); Leslie Long-Simpson, (Study Coordinator); Yolanda Okorocha, LPN, (Study Recruiter/Clinic Coordinator/Blood Draw); Brian Hadfield, (Assistant Clinical Coordinator/Blood Draw/Processing); Lindsay Bartels, (Recruiter) (5/10-5/12); Carol Dunn, (Dental Assistant); Kelly Meyer, RDH, (Treatment/Recruitment) (10/09-6/10); Kristina Reibel, RDH (Recruiter) (10/09-5/10); Andi Jordan, RDH (Recruiter) (5/10-12/10); R Hedge (6/10-5/11); Ophelia Herrera, (Interpreter/Interviewer), (8/10-2/11); E Romero (2/11-3/11); Suban Mohamed, (Recruiter) (7/11-11/12); Cyndee Stull, BS (Recruiter) (10/11-12/11).
University of Texas Health Science Center at San Antonio: Thomas Oates, DMD, PhD, (PI); Devjit Tripathy, MD, (Diabetologist); Peggy Alexander, DDS, (Masked Examiner); David Lasho; DDSM MSD, (Masked Periodontal Examiner), H Gregory (10/10-12/10); Guy Huynh-Ba, DMD, (Therapist), (9/10-4/13); Jo Ann Jordan, RDH, (Study Coordinator); Sandra Pena (3/10-4/13); Cassandra Pacheco-Vera, DA, (Research Asst.) (8/11-4/13); Ashley Munoz, (Dental Asst, Blood Processing and Shipping) (1/10-5/11).
Stony Brook University (site became active 09/2010): David Paquette, DMD, MPH, DMSc, (PI) 10/11-present); Steven Engebretson, DMD, MS, MS, (PI) 9/10-10/11); Marie Gelato, MD, (Diabetes Consultant); Chindanout (Tok) Sayasith, RDH, BSDH, (Masked Periodontal Examiner); Ying Gu, DDS, (Back-up Masked Examiner), (2/11-12/12); Anita Roth, RDH, BSDH (Study Therapist/Recruiter); Alice Urbankova, DDS, MUDr, (Study Therapist); Maria Ryan, DDS, PhD, (Study Therapist/Recruiter), (10/11-12/12); Janet Tuthill, RDH, MA, (Study Therapist)(12/11-12/12); Jill Hughes, DC, BS (Study Coordinator); Suman Grewal, PhD, (Blood Processing and Measurement/Data Recording) ; RuthTenzler, RN, BSN, CCRC, (Back-up Study/Clinical Coordinator/Study Phlebotomist; Bahar Houshmand, DDS, MS (Blood Processing and Measurement/Data Recording) (10/11-6/12); Vincent Iacono, DMD, (Periodontal Consultant) (4/11-12/12).
University of Texas Health Science Center at Houston(site became active 08/2011): James Katancik, DDS, PhD, (PI) 8/11-6/12); Bing-Yan Wang, DDS, MS, PhD (PI) 8/12-4/13); Phillip Orlander, MD (Diabetes Investigator); Sridhar Eswaran, BDS,MS (Masked Periodontal Examiner); Kavitha Parthasarathy, BDS, MS (Masked Periodontal Examiner); Robin Weltman, DDS,MS (Masked Examiner); Meggan Wehmeyer, DDS, (Study Therapist); Ali Arastu, DMD,(3/12-4/13); Rosemary Thomas, DMD (3/12-4/13); Janelle Headley, RN, (Study/Clinic Coordinator); Adriana Cavender, BA/Registered Dental Asst,(Study/Clinic Coordinator); Nathaniel J Harrison, BSN,(Recruiter); T Dancsak (12/11-4/13); Matt Galpin, (Medical Asst. thru the military)(4/12-4/13); Monika Ruscheinksy, MS, CPhT (Study/Clinic Coordinator) (4/12-4/13).
University of Minnesota Core Laboratory: Michael Tsai, PhD (PI); Naomi Hanson, MS, CLS,(NCA), MT (ASCP), (Lab Coordinator/Technical Supervisor; Maren Nowicki, CLS,(Technical Supervisor); Van H. Le., CLS, (Clinical Laboratory Scientist). Executive Committee: Steven Engebretson, DMD, MS, MS (Chair); Leslie Hyman, PhD; MarieGelato, MD; Bryan Michalowicz, DDS ; Holli Hamilton, MD, MPH (ex-officio); Jane Atkinson, DDS (ex officio).
Steering Committee: Steven Engebretson, DMD (Chair); Leslie Hyman, PhD; Marie Gelato, MD; Bryan Michalowicz, DDS; Holli Hamilton, MD (ex officio); Jane Atkinson, DDS (ex officio); Elinor Schoenfeld, PhD; Li Ming Dong, PhD; Melissa Fazzari, PhD; Wei Hou, PhD; Elizabeth Seaquist, MD; Michael Reddy, DMD, DMSc; Cora Lewis, ; Thomas Oates, ; Devjit Tripathy; MD, James Katancik; DDS, PhD, Bing-Yan Wang, DDS, MS, PhD; Phillip Orlander, MD.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the contributions of the following individuals to the DPTT study: The Data and Safety Monitoring Board: John C. Gunsolley, D.D.S., M.S. Virginia Commonwealth University School of Dentistry(Chair); Vivian A. Fonseca M.D., F.R.C.P., Tulane University Health Sciences Center; Judith A. Jones, D.D.S., M.P.H., D.Sc.D., Boston University Henry M. Goldman School of Dental Medicine; Daniel F. Heitjan, Ph.D, University of Pennsylvania, Perelman School Of Medicine ; James B. Meigs, M.D., M.P.H, Harvard Medical School; Jane C. Atkinson, D.D.S., National Institute of Dental and Craniofacial Research (Ex Officio) ) and Holli Hamilton, M.D., M.P.H., Senior Medical Officer, National Institute of Dental and Craniofacial Research/NIH (Ex Officio). Members of the Data and Safety Monitoring Board except Ex-Officio members were compensated for participation.
Drs. Engebretson and Hyman had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding/Support: The DPTT study was funded through cooperative agreements Grants UO1 DE018902 (SE), and U01 DE018886 (LH) from the National Institute of Dental and Craniofacial Research.
Role of the Sponsor: The National Institutes of Health did not contribute to the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Grant Support: Supported by NIH/NIDCR Grant UO1 DE018902 (SE), and U01 DE018886 (LH).
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Dr. Paquette disclosed Board membership, and speaker honorarium with the Colgate-Palmolive company, and paid consultancy with MIS Implant Technologies. No other disclosures were reported.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.