Summary
Background and objectives
Living donors represented 43% of United States kidney donors in 2012. Although research suggests minimal long-term consequences of donation, few comprehensive longitudinal studies for this population have been performed. The primary aims of this study were to examine the incidence, risk factors, and causes of rehospitalization following donation.
Design, setting, participants, & measurements
State Inpatient Databases (SID) compiled by the Agency for Healthcare Research and Quality were used to identify living donors in four different states between 2005 and 2010 (n=4524). Multivariable survival models were used to examine risks for rehospitalization, and patient characteristics were compared with data from the Scientific Registry of Transplant Recipients (SRTR). Outcomes among patients undergoing appendectomy (n=200,274), cholecystectomy (n=255,231), and nephrectomy for nonmetastatic carcinoma (n=1314) were contrasted.
Results
The study population was similar to United States donors (for SRTR and SID, respectively: mean age, 41 and 41 years; African Americans, 12% and 10%; women, 60% and 61%). The 3-year incidence of rehospitalization following donation was 11% for all causes and 9% excluding pregnancy-related hospitalizations. After censoring of models for pregnancy-related rehospitalizations, older age (adjusted hazard ratio [AHR], 1.02 per year; 95% confidence interval [95% CI], 1.01 to 1.03), African American race (AHR, 2.16; 95% CI, 1.54 to 3.03), depression (AHR, 1.88; 95% CI, 1.12 to 3.14), hypothyroidism (AHR, 1.63; 95% CI, 1.06 to 2.49), and longer initial length of stay were related to higher rehospitalization rates among donors. Compared with living donors, adjusted risks for rehospitalizations were greater among patients undergoing appendectomy (AHR, 1.58; 95% CI, 1.42 to 1.75), cholecystectomy (AHR, 2.25; 95% CI, 2.03 to 2.50), and nephrectomy for nonmetastatic carcinoma (AHR, 2.95; 95% CI, 2.58 to 3.37). Risks for rehospitalizations were higher among African Americans than whites in each of the surgical groups.
Conclusions
The SID is a valuable source for evaluating characteristics and outcomes of living kidney donors that are not available in traditional transplant databases. Rehospitalizations following donor nephrectomy are less than seen with other comparable surgical procedures but are relatively higher among donors who are older, are African American, and have select comorbid conditions. The increased risks for rehospitalizations among African Americans are not unique to living donation.
Introduction
Living kidney donors have constituted 45% of all donors in the United States since 1988 (1). Living-donor transplantation is associated with a significant survival benefit compared with maintenance dialysis for patients with ESRD (2). However, living-donor kidney transplantation has declined in the United States since 2004 despite evidence that donors with a greater prevalence of risk factors are being accepted than in past decades (3,4). Mortality rates are not elevated among living donors compared with the general population, even after exclusion of individuals with documented contraindications to donation; however, African Americans, Hispanics, men, and donors with hypertension have relatively increased perioperative mortality (5). Among living donors with private health insurance, African Americans and Hispanics have an increased risk of hypertension and diabetes and an incidence of ESRD of 0.13% at a median 7.7 years of follow-up after donation (6). The rate of selected comorbid conditions, including cancers, cardiovascular disease, depression, and fractures, following living donation is also generally similar to that among individuals characterized as the “healthiest” portion of the general population and among age- and sex-matched controls with commercial insurance (7–10).
Comprehensive follow-up information of living donors’ health is unfortunately limited. Recommendations from the 2010 Living Kidney Donor Follow-Up Conference Writing Group included the need to capture information from sources beyond the Organ Procurement and Transplant Network (OPTN) and to improve surveillance of comorbid conditions (11). To address this need, we undertook a study using data that compiled hospitalizations in the United States from the Agency for Healthcare Research and Quality (AHRQ). These data include information on every hospitalization within participating states and, as opposed to standard transplant forms, include diagnoses and procedure codes that occur within a hospitalization. Rehospitalizations following hospital admission can be a proxy for subsequent morbidity of patients, are indicators of quality of life, and are used to evaluate quality of care by health care providers (12–14). In the United States, approximately 20% of Medicare patients are rehospitalized within 30 days after initial discharge (12,15). These rehospitalization rates vary by patient condition, demographic factors, region of the country, and individual facilities (16–18). Only 10% of early rehospitalizations are considered planned, and the most common principal diagnosis class of rehospitalizations are maternal (related to childbirth and postpartum conditions) (12,15).
The aims of this study were to evaluate (1) the external validity of samples derived from hospitalization files for the United States living-donor population; (2) the incidence, causes, and risk factors of rehospitalizations following living donor nephrectomy; and (3) the relative risk of rehospitalizations among living donors compared with other abdominal surgical interventions.
Materials and Methods
Two data sources were used for this study. The primary data set was the State Inpatient Databases (SID), compiled by AHRQ, which contains data for the full census of hospitalizations within the respective states (19). We used data from 2007 to 2009 for North Carolina, New York, and Florida and from 2005 to 2010 for California. These particular data were selected because more recent years contain identifiers with subsequent hospitalizations and these states were relatively large, representing diverse populations. The Scientific Registry of Transplant Recipients (SRTR) was used to compare and externally validate the composition of the sample with regard to donor characteristics in the United States over the study period. The SRTR data system includes data on all donors, wait-listed candidates, and transplant recipients in the United States, submitted by the members of OPTN, and has been described elsewhere (20). The Health Resources and Services Administration, US Department of Health and Human Services, provides oversight to the activities of the OPTN and SRTR contractors.
Three criteria were used to identify living donors in the SID. First, patients had an International Classification of Diseases, Ninth Revision (ICD-9), diagnosis code as kidney donors (V59.4). Second, patients received an ICD-9 procedure code for nephroureterectomy (55.51). Finally, only elective admissions were included. We used SID severity files to extract information on comorbid conditions of patients. Codes for these conditions have been established by AHRQ, and algorithms are available online (21). Comorbid conditions that were rare (<2% of the sample) or were not considered to be commonly present on admission were ignored for the purpose of this study. For comparison purposes, we also identified patients who underwent appendectomy, cholecystectomy, or nephrectomy for nonmetastatic carcinoma over the study period. We selected these conditions because they are abdominal surgeries requiring organ extraction. The codes for identifying these patients were based on prior studies using AHRQ data (22–24). Nephrectomy for nonmetastatic carcinoma was based on a primary ICD-9 diagnosis code of 189.1 or 189.2, excluding secondary diagnoses indicating metastases of 197.0, 197.7 and 198.×, and an ICD-9 procedure code of 55.51. Appendectomies were identified on the basis of ICD-9 primary procedure codes of 47.09 or 47.01 and a primary diagnosis code of 541.×, 542.×, 540.0, 540.1, or 540.9. Cholecystectomies were identified by ICD-9 diagnoses codes of 574.×, 575.×, or 576.× and a primary ICD-9 diagnosis code of 51.22 or 51.23.
To evaluate rehospitalization rates, we used the linking variable (visit link) provided in the SID. A limitation of these data is an inability to track patients across different states. As such, we limited the study population to patients who donated in the same state as their primary residence to minimize likelihood of hospitalizations not captured in other states. Kaplan-Meier plots and cumulative incidence curves were generated for time to rehospitalization following initial discharge. We used Cox proportional hazard models to evaluate independent risk factors for time to rehospitalization. Rehospitalizations were considered “all-cause”; however, we also generated models censoring follow-up at hospitalizations for pregnancy-related complications because the latter association was not related to morbidity. The inception time for survival models was the month of the index hospitalization (because exact dates are not provided), and models were censored in December of the last year of data available. We used an adjustment (robust sandwich estimator) for clustering of patients within hospitals in all Cox models. The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul, as outlined in the “Declaration of Istanbul on Organ Trafficking and Transplant Tourism.” The study was approved by the Cleveland Clinic Institutional Review Board. All analyses were conducted using SAS software, version9.2 (SAS Institute, Inc., Cary, NC).
Results
Study Population
The number of living donors initially identified in the SID was 5601. Four percent of individuals received a diagnosis of living donation but did not have an applicable procedure code or the procedure was not labeled as elective. In addition, 1077 patients were excluded because of residence in a state other than that for the hospital where the transplant was performed. Donors from out of state compared with those in the same state were slightly older (43 versus 41 years; P<0.001), more often white (76% versus 62%; P<0.001), and more likely to be male (43% versus 39%; P=0.01). Demographic characteristics of the remaining study population (n=4524) were relatively similar to those of all living donors between 2005 and 2010 in the SRTR (n=39,364) (Table 1). The principal exception was a higher prevalence of donors classified as Hispanic (21.2%) in the SID than in the SRTR (13.4%).
Table 1.
Comparison of study population characteristics with National Scientific Registry of Transplant Recipients Data
| Characteristic | SRTR Dataa (n=39,364) | State Inpatient Sampleb (n=4524) |
|---|---|---|
| Mean age ± SD (yr) | 40.8±11.3 | 41.1±11.5 |
| Age ≥50 yr, n/n (%) | 9526/39,364 (24) | 1062/4524 (24) |
| Ethnicity/race, n/n (%) | ||
| White | 27,555/39,364 (70) | 2146/3395 (63) |
| African American | 4724/39,364 (12) | 338/3395 (10) |
| Hispanic | 5275/39,364 (13) | 721/3395 (21) |
| Women, n/n (%) | 23,500/39,364 (60) | 2365/3861 (61) |
SRTR, Scientific Registry of Transplant Recipients.
Based on living donors in the United States from the SRTR database between 2005 and 2010.
Limited to nonmissing values; sample includes New York, Florida, and North Carolina from 2007 to 2009 and California from 2005 to 2010
Rehospitalizations among Living Donors
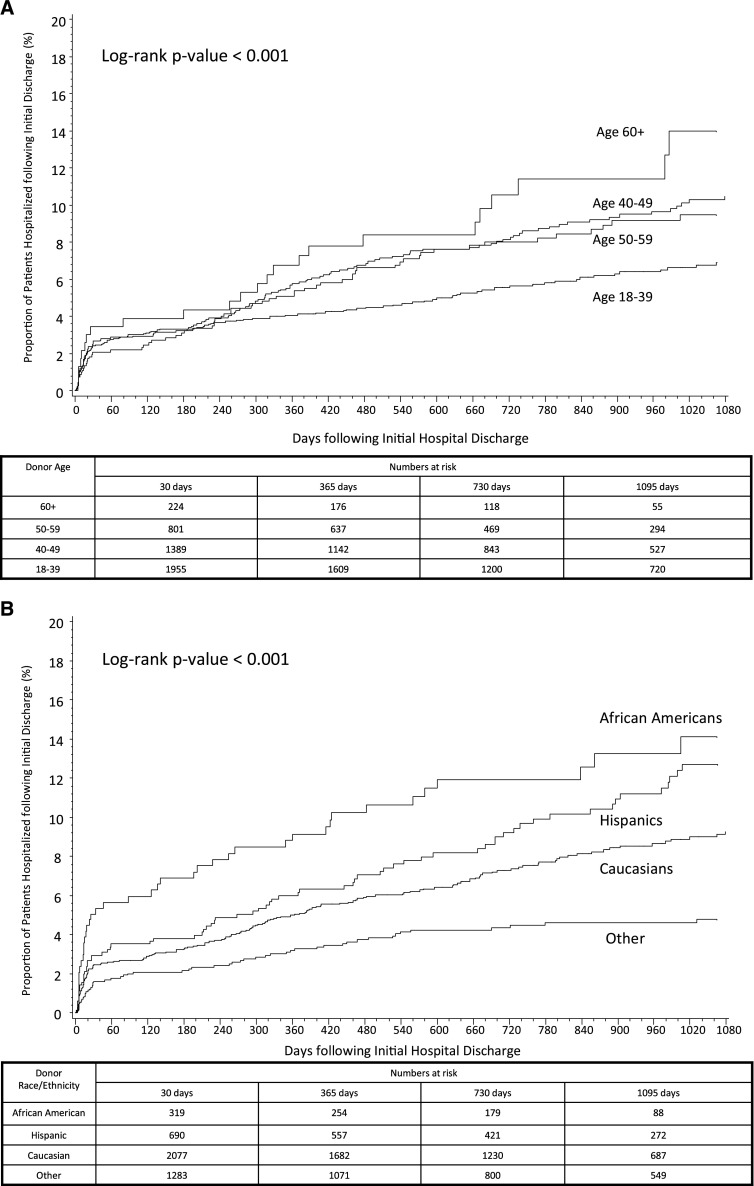
The cumulative 1- and 3-year incidences of all-cause rehospitalizations among living donors were 5% and 11%, respectively; for non–pregnancy-related hospitalizations, the rates were 5% and 9%. The incidence of rehospitalization was higher among women (only for all-cause rehospitalizations), African Americans and Hispanics, patients with diagnoses of depression and hypothyroidism, variation by insurance status and state of residence, and patients who had a longer length of stay during their initial hospitalization (Table 2). Time to rehospitalization (censored at rehospitalization for pregnancy-related diagnoses) are displayed in Figure 1, A–D, by age, race, depression, and hypothyroidism, which were all associated with significant differences. On the basis of the multivariable model, older age, hypothyroidism, African Americans, length of stay >4 days, and depression were all independently associated with higher risks for rehospitalization (Table 3).
Table 2.
Incidence of rehospitalization following living donor nephrectomy by patient characteristics
| Donor Characteristic | Incidence of All-Cause Rehospitalizations following Initial Discharge | Incidence of Non–Pregnancy-Related Rehospitalizations following Initial Discharge | ||||
|---|---|---|---|---|---|---|
| 1 Year (%) | 3 Years (%) | P Value | 1 Year (%) | 3 Years (%) | P Value | |
| Age | 0.14 | <0.001 | ||||
| 18–39 yr | 5 | 13 | 4 | 7 | ||
| 40–49 yr | 6 | 10 | 6 | 10 | ||
| 50–59 yr | 5 | 9 | 5 | 9 | ||
| ≥60 yr | 7 | 14 | 7 | 14 | ||
| Sex | <0.001 | 0.09 | ||||
| Female | 6 | 13 | 6 | 10 | ||
| Male | 4 | 7 | 4 | 7 | ||
| Race/ethnicity | <0.001 | <0.001 | ||||
| White | 5 | 11 | 5 | 9 | ||
| African American | 10 | 18 | 9 | 14 | ||
| Hispanic | 7 | 19 | 6 | 13 | ||
| Other | 3 | 6 | 3 | 5 | ||
| Primary payer | 0.04 | 0.10 | ||||
| Private | 5 | 11 | 4 | 9 | ||
| Medicare | 5 | 10 | 5 | 8 | ||
| Medicaid | 5 | 11 | 4 | 6 | ||
| Other | 7 | 13 | 6 | 10 | ||
| Depression diagnosis | 0.04 | 0.01 | ||||
| No | 5 | 11 | 5 | 9 | ||
| Yes | 11 | 17 | 10 | 16 | ||
| Obesity diagnosis | 0.54 | 0.57 | ||||
| No | 5 | 11 | 5 | 9 | ||
| Yes | 5 | 21 | 4 | 17 | ||
| Hypertension diagnosis | 0.29 | 0.24 | ||||
| No | 5 | 11 | 5 | 9 | ||
| Yes | 8 | 12 | 8 | 11 | ||
| Hypothyroidism diagnosis | 0.04 | 0.001 | ||||
| No | 5 | 11 | 5 | 9 | ||
| Yes | 10 | 16 | 10 | 16 | ||
| Chronic pulmonary disorder diagnosis | 0.99 | 0.67 | ||||
| No | 5 | 12 | 5 | 9 | ||
| Yes | 7 | 10 | 7 | 9 | ||
| State of residence | 0.004 | 0.02 | ||||
| New York | 5 | 8 | 4 | 6 | ||
| North Carolina | 6 | 8 | 6 | 8 | ||
| California | 6 | 13 | 6 | 10 | ||
| Florida | 6 | 12 | 6 | 10 | ||
| Initial length of stay | 0.03 | 0.02 | ||||
| <3 d | 5 | 11 | 4 | 7 | ||
| 3–4 d | 6 | 12 | 6 | 10 | ||
| >4 d | 7 | 15 | 7 | 12 | ||
Figure 1.
Cumulative incidence of non–pregnancy-related rehospitalizations among living donors by age (A), race/ethnicity (B), diagnosis of depression (C), and diagnosis of hypothyroidism (D).
Table 3.
Multivariable Cox proportional hazard model for factors associated with rehospitalization following living-donor nephrectomy
| Parameter (Reference Group) | Adjusted Hazard Ratio for All-Cause Rehospitalizations following Initial Discharge (95% CI) | Adjusted Hazard Ratio for Non–Pregnancy-Related Rehospitalizations following Initial Discharge (95% CI) |
|---|---|---|
| Age at living donation (per year) | 0.99 (0.99 to 1.00) | 1.02 (1.01 to 1.03) |
| State of residence (California) | ||
| New York | 0.54 (0.42 to 0.71) | 0.56 (0.42 to 0.75) |
| Florida | 0.71 (0.49 to 1.02) | 0.74 (0.50 to 1.09) |
| North Carolina | 0.80 (0.43 to 1.50) | 0.97 (0.52 to 1.81) |
| Race/ethnicity (white) | ||
| African American | 1.77 (1.32 to 2.38) | 2.16 (1.56 to 3.01) |
| Hispanic | 1.28 (1.02 to 1.61) | 1.29 (0.97 to 1.70) |
| Other/missing | 0.22 (0.14 to 0.34) | 0.29 (0.18 to 0.49) |
| Sex (male) | ||
| Female | 1.72 (1.35 to 2.20) | 1.17 (0.91 to 1.50) |
| Missing | 4.79 (3.25 to 7.04) | 2.59 (1.58 to 4.27) |
| Primary payer (Medicare) | ||
| Private | 1.22 (0.95 to 1.57) | 1.19 (0.89 to 1.59) |
| Medicaid | 1.51 (0.88 to 2.58) | 1.43 (0.73 to 2.80) |
| Other/missing | 1.48 (1.14 to 1.93) | 1.48 (1.09 to 2.00) |
| Hypertension (no) | ||
| Yes | 1.59 (0.92 to 2.75) | 1.26 (0.71 to 2.24) |
| Obesity (no) | ||
| Yes | 1.09 (0.62 to 1.92) | 1.11 (0.57 to 2.16) |
| Hypothyroidism (no) | ||
| Yes | 1.43 (0.94 to 2.17) | 1.63 (1.06 to 2.49) |
| Depression (no) | ||
| Yes | 1.79 (1.08 to 2.97) | 1.88 (1.12 to 3.17) |
| Chronic pulmonary disease (no) | ||
| Yes | 0.84 (0.52 to 1.38) | 0.97 (0.57 to 1.67) |
| Length of stay from initial donation (<3 d) | ||
| 3–4 d | 1.16 (0.96 to 1.41) | 1.37 (1.09 to 1.72) |
| ≥5 d | 1.47 (1.01 to 2.13) | 1.62 (1.07 to 2.45) |
| Hospitalization within 1 year before surgery (no) | ||
| Yes | 0.99 (0.72 to 1.36) | 0.94 (0.62 to 1.45) |
Based on State Inpatient Databases data from California, New York, North Carolina, and Florida (n=4524). 95% CI, confidence interval.
Primary Diagnoses at Rehospitalization among Living Donors
A total of 456 living donors required rehospitalization. The most common class of diagnoses codes was pregnancy-related causes (21%). Other diagnosis classes in descending order were diseases of the digestive system (14%), injuries and poisoning (13%), diseases of the genitourinary system (8%), mental disorders (6%), diseases of the musculoskeletal system (5%), neoplasms (5%), and diseases of the circulatory system (4%). Other than pregnancy-related causes, primary diagnoses did not differ by sex. Pregnancy-related diagnoses were most common among Hispanics (34%; P=0.002), and mental disorders most common among whites (8%; P=0.001). Older donors (age>59 years) were more likely to be rehospitalized with diseases of the musculoskeletal system (12%; P=0.001) and neoplasms (15%; P<0.001) compared with younger donors. Only 0.2% of rehospitalizations were classified as caused by complications related to pregnancy, including pre-eclampsia.
Rehospitalization Rates between Different Surgical Interventions
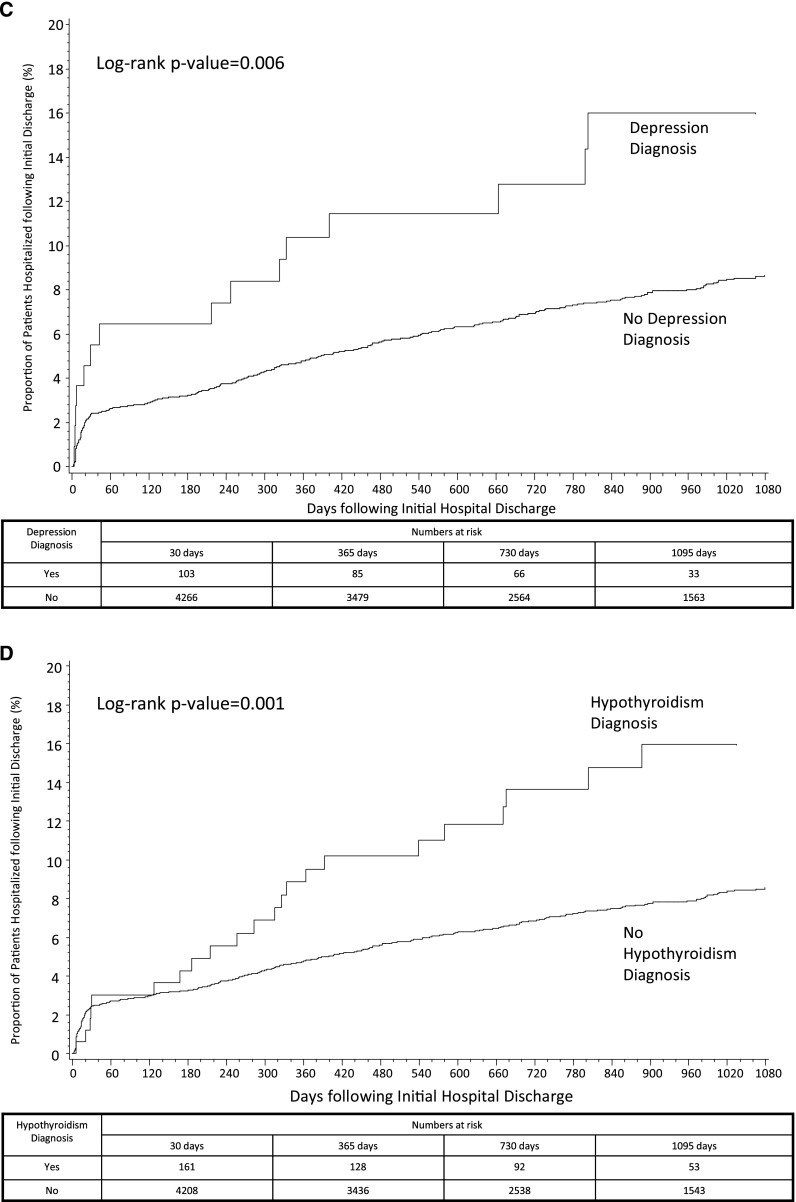
Characteristics of living donors compared with those of patients undergoing other abdominal surgical interventions are displayed in Table 4. Living donors more often were female and white and had Medicare as the primary payer than patients undergoing appendectomy or cholecystectomy. Patients undergoing nephrectomy for nonmetastatic carcinoma were generally older, male, and white. Diagnoses of depression, obesity, hypertension, hypothyroidism, and chronic pulmonary disorder were generally lower among living donors than among other groups. Overall, 21% of the study population had a rehospitalization over the study period, with median follow-up of 731 days (25th percentile, 365 days; 75th percentile, 1126 days) and maximum follow-up of 2160 days (5.9 years). The median (25th percentile, 75th percentile) lengths of stay during rehospitalization were 2 (1,4) days for living donors, 3 (2,6) days for nephrectomy for carcinoma, 3 (2,5) days for appendectomy, and 3 (2,6) days for cholecystectomy. The overall rates of all rehospitalizations (including multiple events for individuals) were as follows: living donor nephrectomy, 1.43/10,000 patient-years; nephrectomy for carcinoma, 15.15/10,000 patient-years; appendectomy, 3.00/10,000 patient-years; and cholecystectomy, 8.41/10,000 patient-years. Compared with other surgery groups, with censoring of pregnancy-related hospitalizations, living donors had a significantly longer time to initial rehospitalization (Figure 2). Differences were consistent in the multivariable model adjusting for patient characteristics at the time of initial hospitalization. Compared with living donors, adjusted risks for rehospitalizations were greater among patients undergoing appendectomy (adjusted hazard ratio [AHR], 1.58; 95% confidence interval [95% CI], 1.42 to 1.75), cholecystectomy (AHR, 2.25; 95% CI, 2.03 to 2.50), and nephrectomy for nonmetastatic carcinoma (AHR, 2.95; 95% CI, 2.58 to 3.37).
Table 4.
Distribution of patient characteristics between surgery groups
| Characteristicsa | Surgery Group | |||
|---|---|---|---|---|
| Living Donor Nephrectomy (n=4524) | Appendectomy (n=200,274) | Cholecystectomy (n=255,231) | Nephrectomy for Nonmetastatic Carcinoma (n=1314) | |
| Age, n (%) | ||||
| 18–39 yr | 2021 (45) | 109,734 (55) | 94,642 (37) | 25 (2) |
| 40–49 yr | 1441 (32) | 42,604 (21) | 57,319 (22) | 125 (10) |
| 50–59 yr | 827 (18) | 30,047 (15) | 54,969 (22) | 349 (27) |
| 60–70 yr | 235 (5) | 17,889 (9) | 48,301 (19) | 815 (62) |
| Sex, n/n (%) | ||||
| Female | 2365/3861 (61) | 88,460/186,790 (47) | 174,551/249,348 (70) | 471/1299 (36) |
| Male | 1496/3861 (39) | 174,551/249,348 (53) | 74,797/249,348 (30) | 828/1299 (64) |
| Race/ethnicity, n/n (%) | ||||
| White | 2146/3395 (63) | 100,430/160,440 (63) | 123861/222,237 (56) | 965/1201 (80) |
| African American | 338/3395 (10) | 9977/160,440 (6) | 19631/222,237 (9) | 54/1201 (5) |
| Hispanic | 721/3395 (21) | 40840/160,440 (25) | 69347/222,237 (31) | 134/1201 (11) |
| Other | 190/3395 (6) | 9193/160,440 (6) | 9398/222,237 (4) | 48/1201 (4) |
| Primary payer, n (%) | ||||
| Private | 2176 (48) | 128,865 (64) | 134,665 (53) | 2176 (54) |
| Medicare | 833 (18) | 10,273 (5) | 35,054 (14) | 462 (35) |
| Medicaid | 127 (3) | 26,293 (13) | 49,468 (19) | 71 (5) |
| Other | 1388 (30) | 34,778 (17) | 35,938 (14) | 75 (6) |
| Diagnosis at initial hospitalization, n (%) | ||||
| Depression | 112 (2) | 6452 (3) | 15170 (6) | 72 (5) |
| Obesity | 107 (2) | 14,290 (7) | 44,471 (17) | 128 (10) |
| Hypertension | 126 (3) | 29,917 (15) | 75,681 (30) | 639 (49) |
| Hypothyroidism | 168 (4) | 6275 (3) | 15,100 (6) | 66 (5) |
| Chronic pulmonary disorder | 177 (4) | 11,903 (6) | 26,103 (10) | 252 (19) |
| Initial length of stay, n (%) | ||||
| <3 d | 2199 (49) | 142,349 (71) | 122,155 (48) | 166 (13) |
| 3–4 d | 2037 (45) | 35,514 (18) | 74,826 (29) | 559 (43) |
| >4 d | 288 (6) | 22,411 (11) | 58,249 (23) | 589 (45) |
| Proportion of patients with hospitalizations in the year before surgery, n (%) | 205 (5) | 11,679 (6) | 21,194 (8) | 91 (7) |
Percentages are calculated out of all known levels (excluding missing values); data presented as n (%) or n/N (%) in cases in with missing levels; all comparisons between surgery groups statistically significant (P<0.05).
Figure 2.
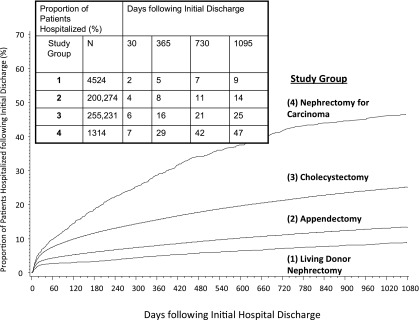
Time to non–pregnancy-related rehospitalization following initial discharge between different surgical interventions.
Risk factors for rehospitalization were relatively similar between surgical groups. The relative risk for rehospitalizations was higher for African Americans than whites in each surgical group. However, the relative odds were numerically lower in the comparison groups: appendectomy (AOR, 1.38; 95% CI, 1.31 to 1.45), cholecystectomy (AOR, 1.16; 95% CI, 1.13 to 1.19), and nephrectomy for nonmetastatic carcinoma (AOR, 1.36; 95% CI, 0.91 to 1.36). Older age and diagnosis of depression were consistent risk factors in each surgical group, while hypothyroidism had a numerically higher risk among living donors. Among women aged 18–40 years, the proportions of rehospitalizations due to pregnancy-related causes were 50% among living donors, 51% among patients having appendectomy, 41% among patients having cholecystectomy, and <1% among patients having nephrectomy for carcinoma. Rehospitalizations related to pregnancy-related complications among women aged 18–40 were slightly higher among patients initially hospitalized for appendectomy (0.4%) and cholecystectomy (0.5%) than among living donors (0.2%).
Discussion
The primary findings of the study were that (1) the SID provides a valuable source for analysis of outcomes and characteristics of living donors in the United States and, on the basis of these data, (2) the 3-year rehospitalization rate among living donors is 11%, (3) non–pregnancy-related rehospitalizations among living donors are higher for African Americans, older patients, patients with longer initial length of stay, and patients with documented diagnoses of depression and hypothyroidism, (4) rehospitalizations among living donors are significantly lower than among patients undergoing appendectomy, cholecystectomy, and nephrectomy for nonmetastatic carcinoma, and (5) certain risk factors for rehospitalizations, including African American race and depression, are not unique to living donation and are consistently higher in each of the surgical groups evaluated in this study. Cumulatively, these data confirm that long-term morbidity associated with living donation is relatively modest but significantly varies within the donor population.
Comprehensive long-term assessment of living-donor health has been challenging in the United States, partially because of incomplete documentation of donor status on standard follow-up forms (25,26). The AHRQ files used in this study provide a unique opportunity to evaluate living-donor outcomes for several reasons. These data have specific information about patients and processes of care, including all diagnosis and procedure codes that occur during hospitalization. This information is distinct from United Network for Organ Sharing forms, which do not assess a variety of comorbid conditions, and is also distinct from single-payer data (e.g., Medicare) because patients with different payer status may have unique conditions and outcomes. As presented in this study, these data also are not limited to transplant events and as such can be compared with other conditions necessitating hospitalizations. Importantly, the data appeared to have high external validity for identifying living donors given the similarity with national registry data over the contemporaneous period.
One of the aims of the study was to evaluate the incidence of rehospitalizations compared with other surgical conditions. Other studies have documented differences between living-donor outcomes and the general population; these studies include important findings but have certain limitations (5–7). Given that donors are carefully screened for physical and mental conditions and likely have intrinsic differences from the general population, including voluntary acceptance of a major surgical intervention, living donors might be expected to have more favorable outcomes. However, it is equally important to appreciate that living donors are also likely to be systematically different from the comparison groups used in this study. Despite the similarity of abdominal surgery that includes organ extraction, the more emergent nature of the conditions used for comparison in this study may also represent greater acuity among these patients and subsequent likelihood for rehospitalization. Given that an ideal control group (such as patients who were evaluated and considered viable for donation but did not ultimately donate) is difficult to identify in large numbers, it is important to place all research concerning the health of living donors in perspective and consider the relative strengths and weaknesses of each approach.
An interesting finding of the study was that risk factors for rehospitalization among living donors, including African American race and depression, were also evident in other surgical groups. This may suggest that patients with these characteristics are more likely to require hospitalization in general, irrespective of patients’ initial requirement for hospitalization, and as such may not be unique to living donation. In other words, for these characteristics, we might expect to observe higher rehospitalization rates independent of a patient undergoing donor nephrectomy (and thus these rates are not a direct consequence of the procedure). However, it also should be noted that numerically the relative risks for rehospitalizations for African Americans and patients with hypothyroidism were highest among living donors compared with other surgical groups.
A primary focus of this study was to evaluate the relative risks for rehospitalizations within the living-donor population. Ibrahim et al. previously reported that women were relatively more likely to have reduced renal function but less likely to have albuminuria following living donation (27). In the current study, women had increased rehospitalization rates; however, the increase was largely explained by pregnancy-related hospitalizations and as such does not appear to indicate excess morbidity. Also of note, among women of child-bearing age, the rate of pregnancy-related rehospitalizations among donors was similar to that among patients undergoing appendectomy and cholecystectomy, and among donors there was a very low rate of pregnancy-related complications necessitating hospitalization. As another comparator, among a cohort of all nonelderly Medicaid patients in 2007, pregnancy-related causes were also the most frequent class of primary diagnosis, representing 22% of first rehospitalizations (28).
Although the overall rate of rehospitalizations among donors is low, the relatively increased rates among African Americans are still noteworthy. Differences in short- and long-term outcomes among these groups relative to those in whites have been documented in other studies and merit continued surveillance (5,6). The primary diagnoses at rehospitalization were not markedly different by race/ethnicity except for higher rates for pregnancy-related hospitalizations among Hispanics and higher rates of hospitalizations for mental disorders among whites. As such, there does not appear to be a specific notable cause for this increased rate among African-Americans, but it should also be placed in context with the prior discussion that these elevated risks are not unique to living donors. Another notable outcome of the study was an 80% elevated adjusted risk of rehospitalization among donors with diagnoses of depression. Although only 2% of donors had documented diagnoses of depression, findings suggest that baseline and ongoing monitoring for depression are particularly important in this population. Lentine et al. reported that the incidence of depression among privately insured living donors was 11% at 5 years, reaffirming that this is a common and potential severe condition leading to hospitalization (9). Perhaps not surprisingly, donors with longer length of initial stay had increased risk of rehospitalization. This may indicate more complicated surgeries or perioperative complications that are more likely to manifest following initial discharge and may indicate that these donors require more vigilant follow-up care.
As described previously, using AHRQ data for research in the living-donor population has several advantages. However, there are also limitations that are important to consider. Because these data are used for administrative purposes, documentation of certain diagnoses and outcomes may not be complete, particularly for diagnoses not used for billing purposes. For example, obesity was diagnosed infrequently (2%) relative to the known proportion of actual obese living donors; as such, some caution with extrapolating certain results of this study is warranted (29). These data also do not include deaths that occur outside of hospitalizations, such that the estimated incidence of rehospitalizations is likely higher than reported based on some patient deaths rendering them no longer at risk for rehospitalization over time. In addition, rehospitalizations were limited to those within the same state, which likely resulted in an undercount of rehospitalizations. It is possible this may have affected some of the relative comparisons.
In summary, this study has several principal findings. First, the rehospitalization rate 3 years following living donation is approximately 11%. The incidence of rehospitalization is substantially less than that in patients undergoing other common abdominal surgeries. Excluding pregnancy-related hospitalizations, there is a relative increased risk for rehospitalization among African Americans, older donors, and patients diagnosed with depression and hypothyroidism. Further efforts to critically evaluate the long-term health of the living- donor population from all available data sources are needed.
Disclosures
The authors report no conflicts of interest related to this study. However, the authors have received consulting and speaking fees, research grants, and honoraria unrelated to the content of this study from Sanofi and Guidry and East (J.S.), Roche (J.R.), Astellas (D.G., E.P.), and Harvard Risk Management Foundation (D.M.) within the last 12 months.
Acknowledgments
The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the SRTR. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the SRTR or the US Government.
The study examined outcomes for living kidney donors using discharge data from California, Florida, New York, and North Carolina SIDs, Healthcare Cost and Utilization Project, AHRQ.
This research is supported, in part, by award number R01DK085185 (J.R., D.M., J.S.). The content is solely the responsibility of the authors and does not represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Rehospitalization after Living Kidney Donation,” on pages 227–228.
References
- 1.Organ Procurement and Transplantation Network. Donors recovered in the U.S. by donor type. Available at: http://optn.transplant.hrsa.gov/data/ August 14, 2013.
- 2.Gill JS, Schaeffner E, Chadban S, Dong J, Rose C, Johnston O, Gill J: Quantification of the early risk of death in elderly kidney transplant recipients. Am J Transplant 13: 427–432, 2013 [DOI] [PubMed] [Google Scholar]
- 3.Rodrigue JR, Schold JD, Mandelbrot DA: The decline in living kidney donation in the United States: random variation or cause for concern? [Published online ahead of print June 11, 2013] Transplantation 10.1097/TP.0b013e318298fa61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taler SJ, Messersmith EE, Leichtman AB, Gillespie BW, Kew CE, Stegall MD, Merion RM, Matas AJ, Ibrahim HN, RELIVE Study Group : Demographic, metabolic, and blood pressure characteristics of living kidney donors spanning five decades. Am J Transplant 13: 390–398, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segev DL, Muzaale AD, Caffo BS, Mehta SH, Singer AL, Taranto SE, McBride MA, Montgomery RA: Perioperative mortality and long-term survival following live kidney donation. JAMA 303: 959–966, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Lentine KL, Schnitzler MA, Xiao H, Saab G, Salvalaggio PR, Axelrod D, Davis CL, Abbott KC, Brennan DC: Racial variation in medical outcomes among living kidney donors. N Engl J Med 363: 724–732, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg AX, Prasad GV, Thiessen-Philbrook HR, Ping L, Melo M, Gibney EM, Knoll G, Karpinski M, Parikh CR, Gill J, Storsley L, Vlasschaert M, Mamdani M, Donor Nephrectomy Outcomes Research (DONOR) Network : Cardiovascular disease and hypertension risk in living kidney donors: an analysis of health administrative data in Ontario, Canada. Transplantation 86: 399–406, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Garg AX, Pouget J, Young A, Huang A, Boudville N, Hodsman A, Adachi JD, Leslie WD, Cadarette SM, Lok CE, Monroy-Cuadros M, Prasad GV, Thomas SM, Naylor K, Treleavan D, Donor Nephrectomy Outcomes Research (DONOR) Network : Fracture risk in living kidney donors: A matched cohort study. Am J Kidney Dis 59: 770–776, 2012 [DOI] [PubMed] [Google Scholar]
- 9.Lentine KL, Schnitzler MA, Xiao H, Axelrod D, Davis CL, McCabe M, Brennan DC, Leander S, Garg AX, Waterman AD: Depression diagnoses after living kidney donation: Linking U.S. registry data and administrative claims. Transplantation 94: 77–83, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lentine KL, Vijayan A, Xiao H, Schnitzler MA, Davis CL, Garg AX, Axelrod D, Abbott KC, Brennan DC: Cancer diagnoses after living kidney donation: Linking U.S. registry data and administrative claims. Transplantation 94: 139–144, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leichtman A, Abecassis M, Barr M, Charlton M, Cohen D, Confer D, Cooper M, Danovitch G, Davis C, Delmonico F, Dew MA, Garvey C, Gaston R, Gill J, Gillespie B, Ibrahim H, Jacobs C, Kahn J, Kasiske B, Kim J, Lentine K, Manyalich M, Medina-Pestana J, Merion R, Moxey-Mims M, Odim J, Opelz G, Orlowski J, Rizvi A, Roberts J, Segev D, Sledge T, Steiner R, Taler S, Textor S, Thiel G, Waterman A, Williams E, Wolfe R, Wynn J, Matas AJ, Living Kidney Donor Follow-Up Conference Writing Group : Living kidney donor follow-up: State-of-the-art and future directions, conference summary and recommendations. Am J Transplant 11: 2561–2568, 2011 [DOI] [PubMed] [Google Scholar]
- 12.Jencks SF, Williams MV, Coleman EA: Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360: 1418–1428, 2009 [DOI] [PubMed] [Google Scholar]
- 13.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P: Depressive sympto ms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, sympto m burden, functional status, and quality of life. Arch Intern Med 167: 60–67, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Stukel TA, Fisher ES, Alter DA, Guttmann A, Ko DT, Fung K, Wodchis WP, Baxter NN, Earle CC, Lee DS: Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. JAMA 307: 1037–1045, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wier LM, Barrett M, Steiner C, Jiang HJ: All-cause readmissions by payer and age; Healthcare Cost and Utilization Project (HCUP) Statistical Briefs, Rockville, MD, Agency for Health Care Policy and Research (US), 2006–2011 [Google Scholar]
- 16.Epstein AM, Jha AK, Orav EJ: The relationship between hospital admission rates and rehospitalizations. N Engl J Med 365: 2287–2295, 2011 [DOI] [PubMed] [Google Scholar]
- 17.Joynt KE, Jha AK: Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes 4: 53–59, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joynt KE, Orav EJ, Jha AK: Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 305: 675–681, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality: HCUP State Inpatient Databases (SID). Healthcare Cost and Utilization Project (HCUP). 2005-2009. Available at: www.hcup-us.ahrq.gov/sidoverview.jsp Accessed August 16, 2012.
- 20.Levine GN, McCullough KP, Rodgers AM, Dickinson DM, Ashby VB, Schaubel DE: Analytical methods and database design: Implications for transplant researchers, 2005. Am J Transplant 6: 1228–1242, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Agency for Healthcare Research and Quality: HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). 2006-2009. Available at: www.hcup-us.ahrq.gov/to olssoftware/ccs/ccs.jsp Accessed July 11, 2005.
- 22.Hanna N, Sun M, Trinh QD, Hansen J, Bianchi M, Montorsi F, Shariat SF, Graefen M, Perrotte P, Karakiewicz PI: Propensity-score-matched comparison of perioperative outcomes between open and laparoscopic nephroureterectomy: A national series. Eur Urol 61: 715–721, 2012 [DOI] [PubMed] [Google Scholar]
- 23.Livingston EH, Miller JA, Coan B, Rege RV: Costs and utilization of intraoperative cholangiography. J Gastrointest Surg 11: 1162–1167, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, Stamos MJ: Comparison of outcomes of laparoscopic versus open appendectomy in adults: Data from the Nationwide Inpatient Sample (NIS), 2006-2008. J Gastrointest Surg 15: 2226–2231, 2011 [DOI] [PubMed] [Google Scholar]
- 25.Mandelbrot DA, Pavlakis M, Danovitch GM, Johnson SR, Karp SJ, Khwaja K, Hanto DW, Rodrigue JR: The medical evaluation of living kidney donors: A survey of US transplant centers. Am J Transplant 7: 2333–2343, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Mandelbrot DA, Pavlakis M, Karp SJ, Johnson SR, Hanto DW, Rodrigue JR: Practices and barriers in long-term living kidney donor follow-up: A survey of U.S. transplant centers. Transplantation 88: 855–860, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, Guo H, Gross CR, Matas AJ: Long-term consequences of kidney donation. N Engl J Med 360: 459–469, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang HJ, Wier LM. All-cause hospital readmissions among non-elderly Medicaid patients; Healthcare Cost and Utilization Project (HCUP) Statistical Briefs, Rockville, MD, Agency for Health Care Policy and Research (US), 2006–2010 [PubMed] [Google Scholar]
- 29.Reese PP, Feldman HI, McBride MA, Anderson K, Asch DA, Bloom RD: Substantial variation in the acceptance of medically complex live kidney donors across US renal transplant centers. Am J Transplant 8: 2062–2070, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]