Abstract
Airway management is a challenge to anesthesiologists particularly in maxillofacial surgeries. The oral tracheal tube is unsuitable because it interferes with the surgical field and prevents dental occlusion. Nasotracheal intubation may not always be possible due to structural deformity or trauma to the nasal bones. Tracheostomy and submental intubation have their drawbacks. To overcome these shortcomings we used Percutaneous Dilatational Tracheostomy Kit (PDTK) to modify the technique of submental intubation. Serial dilatations were performed over the guide wire before passing the tracheal tube by submental route, using the PDT kit in four patients. Submental intubation could be achieved in all the four cases with this technique and there were no associated complications. Seldinger's technique is a simple and easy technique with minimal bleeding, imperceptible scar, and more importantly anesthesiologists feel more comfortable because of their familiarity with the Seldinger technique.
Keywords: Maxillofacial surgeries, percutaneous dilatational tracheostomy kit, seldinger's technique
INTRODUCTION
Submental intubation allows unhindered access to the airway and facilitates reduction and fixation of complex maxillofacial fractures for which simultaneous access to nasal pyramid fractures and/or dental occlusion are required. Submental intubation was first described by Altemir.[1] Current techniques of submental intubation involve blunt dissection in the floor of the mouth (with its potential for injury to the vessels, nerves, and glands) to create a submental passage through which the proximal end of a reinforced tracheal tube is pulled out after initial orotracheal intubation. The Seldinger technique using a Percutaneous Dilatational Tracheostomy© Kit (PDTK) (Cook Critical Care, Europe) offers an interesting alternative to the classical blunt dissection technique. We describe here our experience with this technique in four of our patients.
CASE REPORT
Four patients with maxillofacial trauma posted for surgery during the period from August 2012 to January 2013 were planned to be subjected to submental intubation. Institutional Ethical Committee approval and informed and written patient consent was obtained.Thorough preanaesthetic evaluation was followed by usual preparation for anaesthesia.
Airway accessories and equipments were kept ready for a difficult airway. A 7 mm ID reinforced endotracheal tube was selected to be used in the procedure. Its connector was removed and then reconnected to ensure that these steps would easily be carried out subsequently during the procedure. Following general anaesthesia and neuromuscular blockade, oral endotracheal intubation was performed in the standard way using the preselected tube referred to earlier and controlled ventilation was commenced following connection to the breathing system. A throat pack was inserted. Under aseptic conditions, PDTK was opened [Figure 1]. We passed the Seldinger needle either (1) in the mid submental region (submental approach) just inferior to the lower border of the mandible or (2) in the paramedian submental region, directly adjacent to the medial aspect of the lower border of the mandible (transmylohyoid approach)[2] depending on the surgical need as shown in Figure 2a. We then passed the guide wire through the needle so that it emerged into the oral cavity where it was grasped firmly by an assistant. The needle was then removed. Over the guide wire, we passed successively large serial dilators starting with the white introducer through the skin into the oral cavity as shown in the Figures 2b and 3a. Over the white introducer, the lubricated blue tracheal dilators were passed to emerge into the oral cavity with a twisting motion thereby gradually dilating the path to accommodate the preselected reinforced tracheal tube. Then, the tracheal tube was disconnected from the breathing system and the connector that was pretested for easy removal was removed. The pilot balloon after deflation was grasped with an artery forceps and pulled from within the mouth to the exterior. While stabilizing the tracheal end of tube with one hand, the proximal end of the tube was brought out through the oral cavity as shown in Figure 3b. The connector was then reattached to the tracheal tube and the breathing system was reconnected. The patients were ventilated with 100% oxygen for about 3 min during the period of interruptions to ventilation when the tube was made to emerge externally through the tract created. After ensuring bilaterally equal air entry, the tracheal tube was secured with stay sutures and connected to the breathing system.
Figure 1.

Percutaneous tracheostomy set (cook critical care)
Figure 2.
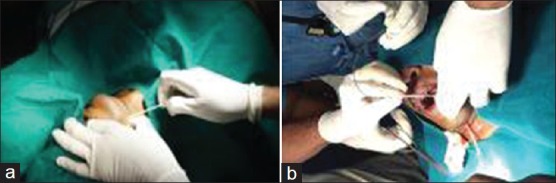
(a) Insertion of needle with cannula. (b) Passing guide wire and sheath through cannula
Figure 3.

(a) Insertion of needle with cannula. (b) Endotracheal tube brought out
At the end of the procedure, the deflated pilot balloon and the tracheal tube were pulled in reverse order into the oral cavity and the breathing system was reattached. Following extubation, the skin wound was closed and no attempt was made to close the intraoral opening.
DISCUSSION
The dilatational technique for submental intubation was performed in 4 cases on a pilot basis and the procedure could be completed in less than 10 min. The four patients in the present series could be intubated by submental approach successfully. No complications such as haemorrhage, injury to the sublingual glands, Wharton's duct, lingual nerve or any fistula were encountered. Ventilation interruption lasted approximately 2 min and there was no significant desaturation in any patient. The intraoral wound healed spontaneously without sutures and the cutaneous wound with a reasonably acceptable scar. No patient developed a keloid/hypertrophic scar. Complex maxillofacial injuries demand special anaesthetic considerations as far as the route for securing the airway is concerned. Anaesthesia for these procedures requires securing the airway either by orotracheal or nasotracheal intubation or via a tracheostomy. Oral intubation may hinder surgical access in most of the procedures. Nasal bone fractures or skull-base fractures may preclude nasotracheal intubation.[3,4] When neither nasotracheal nor orotracheal intubation is suitable, tracheostomy is a traditional method favoured by some surgeons and anaesthesiologists. Tracheostomy is also a major procedure and has its own unique complications such as haemorrhage, subcutaneous emphysema, pneumomediastinum, blockage of tracheostomy cannula, cellulitis, tracheoesophageal fistula, late tracheal stenosis, and problems with decannulation.[5,6,7,8] Submental intubation has been suggested as an alternative technique that offers a secure airway to the anaesthesiologists, an optimal operating field and an opportunity to check dental occlusion for the surgeon and with limited morbidity for the patient. The submental technique of endotracheal intubation is an accepted technique of airway management in patients with panfacial trauma undergoing corrective surgical procedures.[9,10] The existing techniques require the following steps (1) Blunt dissection of the soft tissues in the submental area to create the submental passage (with its potential for injury to the vessels, nerves, and glands in that area). (2) Forcible manipulation of tissue to create a passage with the potential risk of greater tissue damage. Other possible complications include keloid formation, and occasionally mucocoele.
In order to overcome these shortcomings, we used Percutaneous Dilatational Tracheostomy Kit to modify the technique of submental intubation in four of our patients. We found that this modification had the following potential advantages over the classical blunt dissection technique. (1) Minimal bleeding because of the use of dilators.[11] (2) Minimal scar formation due to less tissue dissection.[11] (3) Minimal effort to pull the tracheal tube from inside the oral cavity to the outside. (4) Finally, the anesthesiologists would be more comfortable with this modification because of familiarity with the Seldinger technique that is regularly used for central venous cannulations.
CONCLUSION
Percutaneous Dilatational Tracheostomy Kit© can be used to facilitate submental intubation in maxillofacial surgeries as it causes less tissue trauma, less scarring and gentler manipulations with minimal complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hernández Altemir F. The Submental route for endotracheal intubation. J Maxillofac Surg. 1986;14:64–5. doi: 10.1016/s0301-0503(86)80261-2. [DOI] [PubMed] [Google Scholar]
- 2.Gadre KS, Kushte D. Transmylohyoid oroendotracheal intubation: A novel method. J Craniofac Surg. 1992;3:39–40. doi: 10.1097/00001665-199207000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Muzzi DA, Losasso TJ, Cucchiara RF. Complication from a nasopharyngeal airway in a patient with a basilar skull fracture. Anesthesiology. 1991;74:366–8. doi: 10.1097/00000542-199102000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Marlow TJ, Goltra DD, Jr, Schabel SI. Intracranial placement of a nasotracheal tube after facial fracture: A rare complication. J Emer Med. 1997;5:187–91. doi: 10.1016/s0736-4679(96)00356-3. [DOI] [PubMed] [Google Scholar]
- 5.Chew JY, Cantrell RW. Tracheostomy. Complications and their management. Arch Otolaryngol. 1972;96:538–45. doi: 10.1001/archotol.1972.00770090816008. [DOI] [PubMed] [Google Scholar]
- 6.Walker DG. Complications of trachesotomy: Their prevention and treatment. J Oral Surg. 1973;31:480–2. [PubMed] [Google Scholar]
- 7.Stauffer JL, Olson DF, Petty TL. Complications and consequences of endotracheal intubation and tracheostomy. A prospective study of 150 critically ill adult patient. Am J Med. 1981;70:65–76. doi: 10.1016/0002-9343(81)90413-7. [DOI] [PubMed] [Google Scholar]
- 8.Wood DE. Tracheostomy. Chest Surg Clin N Am. 1996;6:749–64. [PubMed] [Google Scholar]
- 9.Amin M, Dill-Russell P, Manisali M, Lee R, Sinton I. Facial fractures and submental tracheal intubation. Anaesthesia. 2002;57:1195–9. doi: 10.1046/j.1365-2044.2002.02624_1.x. [DOI] [PubMed] [Google Scholar]
- 10.Caron G, Paquin R, Lessard MR, Trepanier CA, Landry PE. Submental endotracheal intubation: An alternative to tracheostomy in patients with midfacial and panfacial fractures. J Trauma. 2000;48:235–40. doi: 10.1097/00005373-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Biswas BK, Joshi S, Bhattacharyya P, Gupta PK, Baniwal S. Percutaneous dilatational tracheostomy kit: An Aid to Submental intubation. Anesth Analg. 2006;103:1055. doi: 10.1213/01.ane.0000239041.31044.c9. [DOI] [PubMed] [Google Scholar]


