Abstract
Meniscus root tear leads to circumferential hoop tension loss and increases femorotibial contact force, which causes irreversible cartilage degeneration. Biomechanical studies have shown that meniscus root repair provides better femorotibial contact force than meniscectomy. Many techniques for meniscus root repair have been published in recent years. The soft suture anchor is widely used in the glenoid labral repair. It is a small low-profile soft anchor. This article presents a new and simple technique of lateral meniscus root repair using the small soft anchor, which results in an anatomic and more vertical anchor position. It avoids instrument-related complications, such as cartilage delamination, material reaction, metal retention, and hard suture anchor pullout.
The attachment of the posterior horn of the meniscus is essential to maintain meniscal function by circumferential hoop tension and to prevent extrusion of the meniscus. If a complete transection of the circumferential fibers occurs in the case of the meniscus root tear, the biomechanical function of the meniscus is lost. The femorotibial contact pressure in the knee with meniscectomy is higher than that in the knee with meniscus root repair, which then results in degenerative changes of the knee. Anatomic meniscus root repair is one of the important factors that affects femorotibial force pressure.1 Many meniscus root repair techniques have been published over the years, such as the pullout suture repair and suture anchor repair.2-7 The JuggerKnot 1.4 anchor (Biomet Sports Medicine, Warsaw, IN) is a small low profile soft anchor commonly used in labral repairs of the shoulder. We created a new technique for lateral meniscus root repair with the soft anchor.
Surgical Technique
We prefer placing the patient supine on the operating table. The lateral post controls the hip rotation, and the foot rests against a distal support that maintains the knee at 90° of flexion. (Fig 1). A tourniquet is usually used if not clinically contraindicated. General arthroscopic examination is routinely carried out through the standard anterolateral and anteromedial portals.
Fig 1.

The right knee, set in the position of 90° of flexion on the operating table, is maintained with the distal foot support and lateral post. The standard anteromedial (AM) portal, high accessory anteromedial (AAM) portal, and standard anterolateral (AL) portal are marked.
If a posterior root tear of the lateral meniscus is found, we create a high accessory anteromedial portal. The knee is placed in the fully flexed position on the operating table. In this position the distal femur is glided posteriorly by the rollback mechanism, allowing a clear approach for the anatomic footprint of the posterior root of the lateral meniscus (Fig 2, Video 1). The curved guide sleeve (Biomet Sports Medicine, Warsaw, IN) is passed through the high accessory anteromedial portal (Fig 3). The tip of the guide sleeve is placed on the anatomic footprint. A 1.4-mm-diameter flexible drill bit (Biomet Sports Medicine, Warsaw, IN) is used to create a pilot hole through the curved guide sleeve. A JuggerKnot 1.4 anchor is inserted through the guide and into the hole. The surgeon performs light tapping with a mallet to fully seat the anchor into the bone. The surgeon releases the suture from the handle and pulls on both sutures to set the anchor.
Fig 2.
The rollback mechanism occurs when the knee is placed in the fully flexed position. This position makes the tibia shift anteriorly and allows for a clear approach to the anatomic footprint for the posterior root of the lateral meniscus.
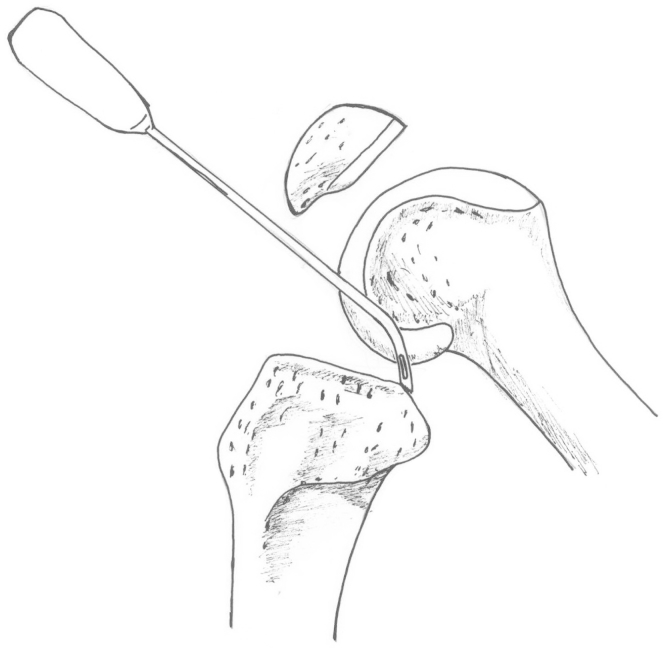
Fig 3.

Curved drill guide sleeve and flexible drill bit, which are used to place the more vertical soft anchor through the high anteromedial portal.
The knee position is changed to the figure-of-4 position, which opens up the lateral compartment. The 90° curved suture hook (SutureLasso; Arthrex, Naples, FL) is passed through the standard anteromedial portal. The peripheral one-third of the torn meniscus is hooked from the femoral side to the tibial side (Fig 4A). The malleable passing wire, which is already loaded into the suture hook, is advanced. The tibial side of the passing wire is retrieved through the high accessory anteromedial portal with a suture retriever. The strand of the anchor suture, which is passed into the loop end of the passing wire, is pulled through the meniscus with the shuttle relay technique (Fig 4B). The other strand of the anchor is passed through the central one-third of the meniscus with the same technique. A knot is pushed down under adequate reduction and tension (Fig 5). After the meniscus repair is finished, the ACL is reconstructed with soft-tissue graft if ACL deficiency is found. A compression dressing is applied. Advantages, tips and pearls, and limitations of the procedure are further described in Table 1.
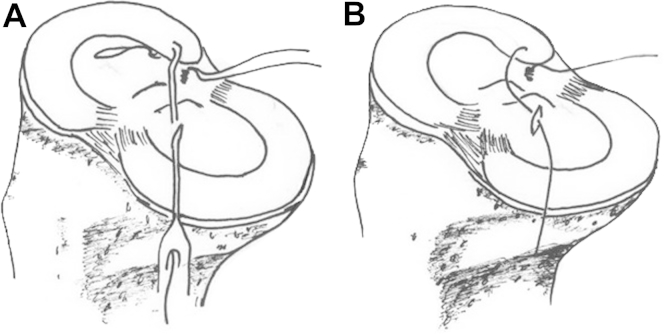
Fig 4.
(A) After the soft anchor is seated into the bone, the suture hook, which is loaded with the malleable wire loop, is placed through the standard anteromedial portal. The meniscus is hooked in the vertical direction. The surgeon then retrieves the loop end of the malleable passing wire and one strand of the anchor suture through the high accessory anteromedial portal. (B) The strand of the anchor suture, which is passed into the loop end of the passing wire, is pulled through the meniscus with the shuttle relay technique.
Fig 5.
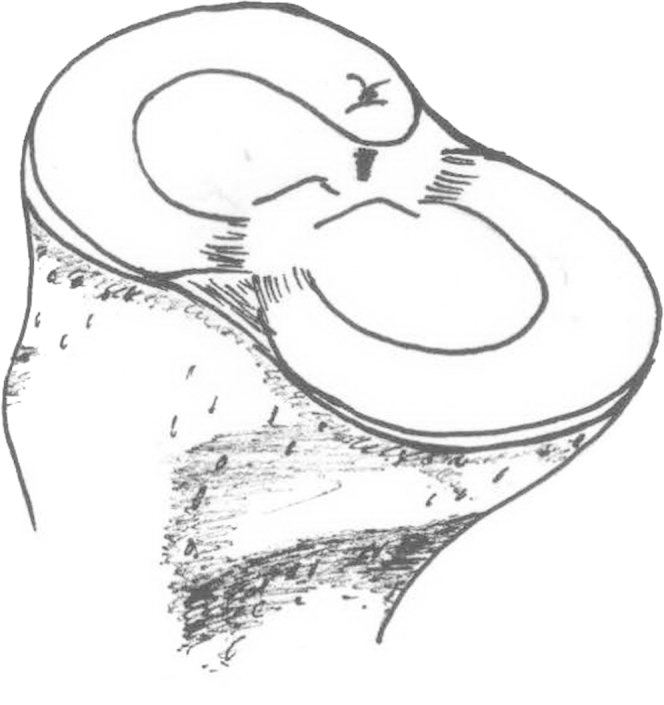
The suture is tied, closing the gap between the meniscus and its footprint.
Table 1.
Advantages, Tips and Pearls, and Limitations
| Advantages |
| Familiar approach from anterior portals to repair posterior root tear of lateral meniscus into anatomic footprint |
| More vertical placement of soft anchor |
| Less risk of chondral damage with low-profile soft suture anchor |
| Tips and pearls |
| The fully flexed knee position allows for a clear approach to the anatomic footprint of the lateral meniscus. |
| Decorticate the footprint to increase the healing rate. |
| Use the malleable drill bit and curved guide sleeve through the high accessory anteromedial portal to achieve a more vertical soft anchor position. |
| To open up the lateral compartment, turn the knee position to the figure-of-4 position. |
| The anteromedial portal should be created as low as possible to easily pass the suture hook to the posterior root of the lateral meniscus. |
| Limitations |
| In the knee with a normal ACL, this technique may be more difficult because of narrowing of the working space. |
Postoperative Protocol
The patient should be encouraged to perform active quadriceps exercises on the first postoperative day. Passive knee flexion to no more than 60° is allowed in a hinged knee brace. The patient increases to 90° of knee flexion after 2 weeks. Non–weight-bearing ambulation is restricted, and then partial to full weight-bearing ambulation is allowed after 6 to 8 weeks. Full flexion, squatting, and return to sports are allowed after 6 months.
Discussion
The functions of the meniscus are joint load distribution, force absorption, and circumferential hoop tension. A posterior root tear of the meniscus causes a loss of biomechanical function, which then results in degenerative changes of the knee. Femorotibial contact pressure after a meniscectomy is higher than the contact pressure after a meniscus root repair, which still does not restore the biomechanical function back to the normal level. Achieving an anatomic meniscus root repair is one of the important factors affecting femorotibial force pressure. The study of Starke et al.1 has shown an increase in the conversion of femorotibial loads into circumferential tension in the non–anatomically repaired meniscus. Many techniques for meniscus root repair have been developed in recent years.
Lee et al.3 published 2-year follow-up results on the repair of posterior root tears in the medial meniscus. They used the arthroscopic pullout suture repair technique. All patients were able to return to their normal or nearly normal preinjured activity level. At second-look arthroscopy, all of the repaired menisci had healed completely without additional chondral lesions. Kim et al.7 reported on arthroscopic suture anchor repair of posterior root tears of the medial meniscus compared with pullout suture repair. For the suture anchor technique, they passed the suture anchor through the high posteromedial portal for anchor placement in a more vertical position. The International Knee Documentation Committee, Lysholm, and Hospital for Special Surgery scores showed statistically significant postoperative improvements in pain, locking, and giving way. However, there were no statistically significant differences between the preoperative and postoperative groups on radiographic evaluation and in cartilage degeneration.
The JuggerKnot 1.4 anchor is a low-profile soft anchor that is usually used in the case of glenoid labral repair. The highest mean tension (60.1 ± 20.2 N) of the repaired medial meniscus root is generated with internal rotation, a 500-N load, and 90° of flexion.8 A biomechanical study measuring the tensile force for vertical repair of a longitudinal tear of the lateral meniscus has shown that the combined mean force generated by flexion and rotation is between 0.5 and 4.1 N on the repaired site.9 A biomechanical study has also shown that the mean pullout force of the JuggerKnot anchor is 239.1 ± 30.2 N,10 which is at least 3 times stronger than the highest mean tension of the medial meniscus root repair and is rigid enough for a longitudinal tear of the lateral meniscus.
Our technique for posterior root repair of the lateral meniscus uses the high accessory anteromedial portal, curved drill guide sleeve, and flexible drill bit to place a more vertical soft anchor at the anatomic footprint for the posterior root of the lateral meniscus. The approach through the anterior side portals is easy to perform. The knee should be fully flexed to achieve the rollback mechanism for a clear view of the footprint. In the case of an ACL tear, which usually occurs with a meniscus tear, there is more available space to repair the meniscus root tear. The anatomic root attachment recreates nearly normal circumferential tension of the meniscus, which avoids irreversible cartilage degeneration sequentially.
A posterior root tear of the lateral meniscus is one of the more challenging meniscus injuries to treat. Anatomic meniscus root repair keeps the function of the circumferential hoop tension and avoids irreversible cartilage degeneration. The soft anchor repair is a new option for the treatment of the meniscus root tear. This technique creates an anatomic and rigid repair using simple arthroscopic techniques.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical procedure using soft suture anchor technique in posterior root tear of lateral meniscus.
References
- 1.Starke C., Kopf S., Grobel K.H., Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: A biomechanical study. Arthroscopy. 2010;26:358–365. doi: 10.1016/j.arthro.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 2.Nicholas S.J., Golant A., Schachter A.K., Lee S.J. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee. 2009;17:1433–1436. doi: 10.1007/s00167-009-0874-1. [DOI] [PubMed] [Google Scholar]
- 3.Lee J.H., Lim Y.J., Kim K.B., Kim K.H., Song J.H. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: Radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Jung Y.H., Choi N.H., Oh J.S., Victoroff B.N. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40:1406–1411. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 5.Choi N.H., Son K.M., Victoroff B.N. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: A technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16:891–893. doi: 10.1007/s00167-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 6.Jung W.H., Kim D.H., Chun C.W., Lee J.H., Ha J.H., Jeong J.H. Arthroscopic, suture anchor repair through a novel medial quadriceptal portal for medial meniscal root tear. Knee Surg Sports Traumatol Arthrosc. 2012;20:2391–2394. doi: 10.1007/s00167-012-1895-8. [DOI] [PubMed] [Google Scholar]
- 7.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 8.Starke C., Kopf S., Lippisch R., Lohmann C.H., Becker R. Tensile forces on repaired medial meniscus root tear. Arthroscopy. 2013;29:205–212. doi: 10.1016/j.arthro.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Staerke C., Brettschneider O., Grobel K.H., Becker R. Tensile forces on sutures in the human lateral knee meniscus. Knee Surg Sports Traumatol Arthrosc. 2009;17:1354–1359. doi: 10.1007/s00167-009-0875-0. [DOI] [PubMed] [Google Scholar]
- 10.Barber F.A., Herbert M.A., Hapa O. Biomechanical analysis of the pullout strength of rotator cuff and glenoid anchors: 2011 update. Arthroscopy. 2011;27:895–905. doi: 10.1016/j.arthro.2011.02.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical procedure using soft suture anchor technique in posterior root tear of lateral meniscus.