Abstract
Introduction:
Homeless adults are more likely to smoke tobacco and are less likely to successfully quit smoking than smokers in the general population, despite comparable numbers of cessation attempts and desire to quit. To date, studies that have examined smoking cessation in homeless samples have used traditional lab/clinic-based assessment methodologies. Real-time assessment of key variables may provide new insights into the process of quitting among homeless smokers.
Methods:
The purpose of the current study was to identify predictors of a quit attempt using real-time assessment methodology during the 6 days prior to a scheduled quit attempt among homeless adults seeking care at a shelter-based smoking cessation clinic. Parameters for multiple variables (i.e., motivation for quitting, smoking expectancies, quit self-efficacy, smoking urges, negative affect, positive affect, restlessness, hostility, and stress) were calculated and were used as predictors of biochemically verified quit date abstinence (i.e., ≥13hr abstinent) using logistic regression analyses.
Results:
Participants (n = 57) were predominantly male (59.6%), non-White (68.4%), and smoked an average of 18 cigarettes per day. A total of 1,132 ecological momentary assessments (83% completion rate) were collected at random times (i.e., up to 4 assessments/day) during the 6 days prior to a scheduled quit attempt. Results indicated that declining (negative slope) negative affect, restlessness, and stress predicted quit date abstinence. Additionally, increasing positive coping expectancies across the prequit week predicted quit date abstinence.
Conclusions:
Study findings highlight multiple variables that may be targeted during the precessation period to increase smoking cessation attempts in this difficult to treat population of smokers.
INTRODUCTION
Few populations experience greater health disparities than homeless adults, and an estimated 6% of all adults in the United States will be homeless at some point in their lifetime (Toro et al., 2007). Homeless individuals have higher rates of disease, shorter life expectancies, and disproportionately high health care costs compared to housed individuals (Barrow, Herman, Cordova, & Struening, 1999; Hwang, Wilkins, Tjepkema, O’Campo, & Dunn, 2009; Weinreb, Goldberg, & Perloff, 1998). A significant contributor to the health disparities experienced by homeless adults is their alarmingly high smoking prevalence (Arnsten, Reid, Bierer, & Rigotti, 2004; Butler et al., 2002; Hwang & Henderson, 2010). Over the past five decades, the prevalence of smoking has declined to 18.1% among U.S. adults yet over 70% of homeless individuals continue to smoke (Baggett & Rigotti, 2010; Centers for Disease Control and Prevention, 2014; Lee et al., 2005; Sachs-Ericsson, Wise, Debrody, & Paniucki, 1999). Approximately 75% of homeless smokers report a desire to quit smoking (Butler et al., 2002; Okuyemi et al., 2006), and they undertake comparable numbers of cessation attempts compared to nonhomeless smokers (Businelle, Cuate, Kesh, Poonawalla, & Kendzor, 2013; Butler et al., 2002). However, homeless smokers have considerable difficulty quitting smoking and maintaining long-term abstinence following a quit attempt (Bonevski, Baker, Twyman, Paul, & Bryant, 2012; Businelle et al., 2014; Okuyemi et al., 2013; Shelley et al., 2010; Spector, Alpert, & Karam-Hage, 2007). For example, in the largest clinical trial conducted among homeless smokers to date, Okuyemi et al. (2013) reported low abstinence rates one week after the scheduled quit date in both standard care (i.e., nicotine replacement therapy [NRT] plus advice to quit; 9% abstinent) and in the enhanced care group (i.e., Motivational Interviewing plus NRT; 10% abstinent). Another recent study reported that 76% of homeless smokers who enrolled in smoking cessation treatment failed to initiate their scheduled quit attempt (Businelle et al., 2014). In contrast, multiple studies have indicated that 20%–35% of domiciled smokers fail to quit on their scheduled quit date (Bailey, Bryson, & Killen, 2011; Kendzor et al., in press; Shiffman et al., 2006; Yeh, McCarthy, & Baker, 2012).
Few studies have examined the barriers to cessation or factors that influence the ability to quit in homeless smokers. One recent study shed light on this issue through the examination of similarities and differences between homeless smokers and low income domiciled smokers seeking cessation treatment (Businelle, Cuate, et al., 2013). Findings indicated similar smoking characteristics across the two samples (e.g., smoking rates, levels of nicotine dependence); however, homeless smokers were exposed to far more smokers, reported lower motivation to quit, lower self-efficacy for quitting, more days with mental health problems, and greater exposure to numerous stressors than domiciled socioeconomically disadvantaged smokers (Businelle, Cuate, et al., 2013). Thus, even when compared to very low income domiciled smokers, homeless smokers must overcome substantial hurdles in order to achieve smoking cessation. These hurdles likely contribute to the high smoking prevalence and abysmal cessation rates among homeless people, even when empirically supported cessation interventions are provided.
To date, the few studies that have examined smoking and smoking cessation in homeless smokers have used focus groups or traditional lab/clinic based assessment methodology which may result in biased and/or inaccurate estimates due to recall biases and errors in memory (Shiffman et al., 1997; Stone et al., 1998). Such biases and errors may be particularly relevant in the moments/days leading up to a quit attempt, when potentially important momentary changes in key variables may be missed or misrepresented. Ecological momentary assessment (EMA), in which handheld devices (e.g., smart phones) are used to capture moment to moment experience, may provide a more accurate and nuanced picture of the factors that influence smoking cessation. EMAs are often used to assess individuals at multiple time points throughout a day. Thus, trajectories of variables of interest can be characterized by a linear slope representing the direction and rate of symptom change (e.g., worsening symptoms over time) and volatility capturing range/scatter of that symptom over time.
Initial research with EMA has begun to provide insights into the role of postquit symptom trajectories in lapse and relapse among domiciled smokers. For example, Piasecki et al. (2002) showed that positive slopes and greater volatility in postcessation withdrawal predicted smoking relapse. Cofta-Woerpel et al. (2011) found that greater volatility in postcessation smoking urge predicted smoking relapse in women. Finally, Shiffman and Waters (2004) found that increases in EMA-measured negative affect (i.e., positive slope) prospectively predicted smoking lapse hours before the lapse occurred. Likewise, studies have shown that prequit parameters of key variables are related to quit attempt initiation and smoking relapse. For instance, studies have indicated that rising negative affect during the week prior to the scheduled quit date can predict relapse months after the quit date (Blalock, Robinson, Wetter, Schreindorfer, & Cinciripini, 2008; McCarthy, Piasecki, Fiore, & Baker, 2006). One recent EMA study of a sample of domiciled smokers found that rising negative affect in the 4 days prior to the quit date was related to a greater likelihood of abstinence on the quit date (Yeh et al., 2012).
EMA research may facilitate a better understanding of the mechanisms involved in cessation/relapse milestones, including the initiation of a cessation attempt, smoking lapses, and the transition from lapse to relapse. However, the mechanisms predicting each milestone may be unique (Shiffman et al., 2006). For example, positive expectancies about one’s ability to cope with withdrawal symptoms and/or motivation for smoking cessation may be particularly important during the period leading up to a cessation attempt, but may be less predictive of lapse after the onset of the cessation attempt. Likewise, prequit symptoms of nicotine withdrawal may not predict quit attempt initiation, but may predict smoking lapse/relapse (Cofta-Woerpel et al., 2011; Piasecki et al., 2002). Although multiple studies have focused on predicting smoking lapse or relapse, few studies have examined EMA-based predictors of quit attempt initiation. However, for difficult to treat populations of smokers, identification of prospective predictors of nonabstinence on the quit date may allow us to identify individuals who are in need of additional intervention prior to their quit date. To date, no studies have used EMA to collect data in homeless smokers.
Gaining a better understanding of the factors that influence smoking cessation among homeless smokers may facilitate the development of more effective interventions in this vulnerable and understudied population. Thus, the purpose of the current study was to examine parameters (i.e., trajectory and volatility) of prequit variables that may be linked to smoking abstinence on the quit date among a sample of homeless smokers undergoing an aided quit attempt. Based on conceptual models describing the links between socioeconomic disadvantage and health (e.g., Businelle et al., 2010; Businelle, Kendzor, et al., 2013; Kendzor et al., 2009; Matthews & Gallo, 2011) as well as prior EMA research among domiciled smokers (e.g., Piasecki et al., 2002; Shiffman & Waters, 2004; Wetter et al., 2011), it was hypothesized that EMA measures of motivation for quitting, positive coping expectancies, positive smoking expectancies, quit self-efficacy, smoking urges, negative affect, positive affect, restlessness, hostility, and stress in the week prior to the quit date would influence quit date abstinence.
METHODS
Parent Study
Data for the current study were from a project that compared standard care at a homeless shelter-based smoking cessation clinic to standard care plus financial incentives for smoking abstinence. Details about sample recruitment and methodology have been published previously (Businelle et al., 2014). In brief, most of the study participants enrolled in standard care (n = 58) which offered six support group sessions and free pharmacological treatment prescribed by the clinic physician. The final 10 study participants were enrolled in standard care plus contingent payments for biochemically verified self-reported smoking abstinence at each postbaseline visit. All participants were asked to carry a smart phone to complete EMAs for 2 weeks (1 week prequit through 1 week postquit) and to smoke as usual during the prequit week.
Participants
Participants in the current study were homeless individuals recruited from a smoking cessation clinic located at a Texas based homeless shelter between January 2012 and November 2012. Of the 68 participants who were recruited into the parent study, 8 did not return the study phone, 1 deleted the EMA application from the study phone, and 2 did not complete any prequit random EMAs. These individuals were allowed to remain in the study, but only the 57 participants who provided prequit EMA data were included in the current study analyses. In order to participate in this study, participants were required to: (a) be residents of the transitional shelter, (b) have an English reading level above the 6th grade, (c) smoke at least five cigarettes per day (CPD), (d) have an expired carbon monoxide level ≥8 parts per million (ppm), and (e) be willing and able to attend six consecutive weekly assessment visits (i.e., baseline [1 week precessation], quit date, 1, 2, 3, and 4 weeks postcessation).
Procedure
The Institutional Review Board at The University of Texas School of Public Health approved this study. A brief description of the parent study was provided at the beginning of each tobacco clinic group session. Informed consent was obtained from interested individuals and those who met study inclusion criteria were enrolled in the study. Participants completed baseline measures using study computers via Questionnaire Development System (QDS) software (NOVA Research, Bethesda, MD). Each question appeared on the computer screen while the program read the item to the participant, thus reducing reading time for low literacy participants.
At the end of the baseline visit, all participants were instructed on how to use the study provided LG Optimus smart phone to complete three types of EMAs: daily diary, random sampling, and event sampling (i.e., precessation smoking, urge, postcessation lapse). The current study focuses on data that were collected during the prequit random assessments. Random sampling EMAs were initiated by the phone. Each day of assessment was split into four equal epochs based on each participant’s reported waking hours. One random assessment was pushed during each epoch. The phone used audible (ringing) and tactile (vibration) cues to alert participants that it was time to complete EMAs. If the participant did not respond, the assessment was recorded as missed. Participants could opt to initiate a 5-min delay, up to three times, for each assessment. Participants were allowed to make personal calls and send/receive text messages on the study phone in order to increase the likelihood that the phone would be carried at all times over the 2-week assessment period. Participants were encouraged to use the study phone to contact study staff if they had problems with the phone or EMA software. Participants were paid based on the number of assessments completed (random and daily diary) when they returned the study phone at the 1 week postquit follow-up visit. Specifically, participants received a $25 gift card if they completed 50%–74% of all EMAs, a $50 gift card if they completed 75%–89% of all EMAs, and an $80 gift card if they completed 90% or more of the EMAs. Participants did not receive any payment if they completed less than 50% of the EMAs.
Measures
At the baseline visit (1 week prequit), participants completed computerized measures that assessed demographics (e.g., sex, race/ethnicity, education), smoking characteristics, smoking urges (Brief Questionnaire of Smoking Urges; QSU) (Cox, Tiffany, & Christen, 2001), positive and negative affect (Positive and Negative Affect Schedule; PANAS) (Watson, Clark, & Tellegen, 1988), motivation for smoking cessation (Texas Smoking Abstinence Motivation Scale; TSAMS) (Castro et al., unpublished manuscript), and perceived stress (Perceived Stress Scale; PSS) (Cohen, Kamarck, & Mermelstein, 1983).
Four random EMAs, which included the same 26 items, were pushed on each day of assessment. Random EMAs included questions on motivation for quitting (Motivation 1: “I am motivated to AVOID smoking”; Motivation 2: “I am committed to being smoke free”), positive coping expectancies (“I am confident that I could do something OTHER THAN SMOKE to improve my mood”), positive smoking expectancies (“I am confident that SMOKING would improve my mood”), and self-efficacy for quitting (“I am confident in my ability to AVOID smoking”). Participants also answered questions related to their current levels of smoking urges, negative affect [i.e., irritable, frustrated/angry, sad, worried, miserable; see circumplex model of emotion as described in Shiffman and Kirchner (2009)], positive affect (i.e., happy, content; see Shiffman & Kirchner, 2009), restlessness, hostility, and stress. All items were answered on a scale from 1 (strongly disagree) to 5 (strongly agree).
Participants were instructed to initiate a quit attempt at 10:00 p.m. on the night before their second scheduled visit. Thus, abstinent participants would have been abstinent for at least 13hr prior to their quit date clinic visit. Quit date abstinence was assessed via self-report and was confirmed via Vitalograph carbon monoxide monitor. Specifically, participants who self-reported not smoking after 10:00 p.m. (“not even a puff”) on the night prior and had carbon monoxide levels below 10 ppm were considered abstinent. An intention to treat approach was used, whereby participants who did not attend the quit date visit were considered nonabstinent.
Data Analysis
Random effects parameters (i.e., intercepts, slopes, volatility) for 11 EMA variables (i.e., motivation [two items], positive coping expectancies, positive smoking expectancies, quit self-efficacy, smoking urge, negative affect [average of five items], positive affect [average of two items], restlessness, hostility, and stress) for each of the 57 study participants were estimated using the linear multilevel mixed effects modeling (LMM) function in STATA version 12.0 (STATA Corp., College Station, TX). In this step, the repeated measurement of EMA variables was expressed as the regression function of time for each participant. All random effects for EMA variables were then standardized and these standardized parameters were used as predictors of biochemically verified quit date abstinence status in separate logistic regression analyses. Two logistic regression models, unadjusted and adjusted, were tested for each EMA variable. Unadjusted analyses included only the standardized parameters as predictors of quit date abstinence. Adjusted analyses included standardized parameters, treatment group, sex, race/ethnicity, education, and CPD as predictors of quit date abstinence. Notably, some of the adjusted analyses included other relevant baseline measures as covariates (i.e., EMA urge analysis controlled for baseline QSU scores; EMA negative affect analyses controlled for baseline PANAS negative affect subscale; EMA positive affect analyses controlled for baseline PANAS positive affect subscale; EMA motivation analyses controlled for baseline TSAMS score; and EMA stress analyses controlled for baseline PSS score). As used in our previous research, volatility was calculated as the mean absolute deviation over time between a participant’s predicted LMM trajectory and their observed score (Cofta-Woerpel et al., 2011). Thus, this method accounts for within and between day variations in EMA responses.
RESULTS
A minority of study participants (26.3%) achieved biochemically verified smoking abstinence on their scheduled quit date. Participant characteristics and scores on baseline measures are presented by smoking abstinence status in Table 1. A total of 1,368 random EMAs were pushed during the 6 days of prequit assessment (i.e., prequit week), of which 1,132 (82.7%) were completed. On average, participants completed 3.31 random assessments (out of four possible) per day. Most participants (89.5%) completed random EMAs on each day of assessment, 9% completed random EMAs on 4 or 5 days, and one participant completed random EMAs on only one day. On average, participants completed these EMAs within 3.4min (SD = 1.4). Quit date abstainers and nonabstainers completed similar numbers of prequit random EMAs (20.9 vs. 19.5, respectively; p = .35).
Table 1.
Participant Characteristics at Baseline
| Measures | Abstainers (n = 15) % or M (SD) | Nonabstainers (n = 42) % or M (SD) | Full sample (N = 57) % or M (SD) |
|---|---|---|---|
| Male | 60.0% | 59.5% | 59.6% |
| Non-White | 60.0% | 71.4% | 68.4% |
| Years of education | 12.9 (2.1) | 12.5 (1.8) | 12.6 (1.9) |
| Cigarettes per day | 15.1 (5.5) | 19.3 (11.5) | 18.2 (10.4) |
| Brief questionnaire of smoking urges | 4.9 (1.5) | 5.0 (1.7) | 4.9 (1.7) |
| PANAS negative affect | 20.4 (7.5) | 17.7 (6.7) | 18.4 (7.0) |
| PANAS positive affect | 31.2 (9.4) | 30.6 (11.0) | 30.6 (10.5) |
| Perceived stress scale | 5.8 (3.9) | 6.1 (3.2) | 6.0 (3.4) |
| Texas smoking abstinence motivation scale | 21.3 (5.2) | 20.7 (4.8) | 20.9 (4.8) |
Note. PANAS = Positive and Negative Affect Scale. Abstainers and nonabstainers were not significantly different on any baseline participant characteristic.
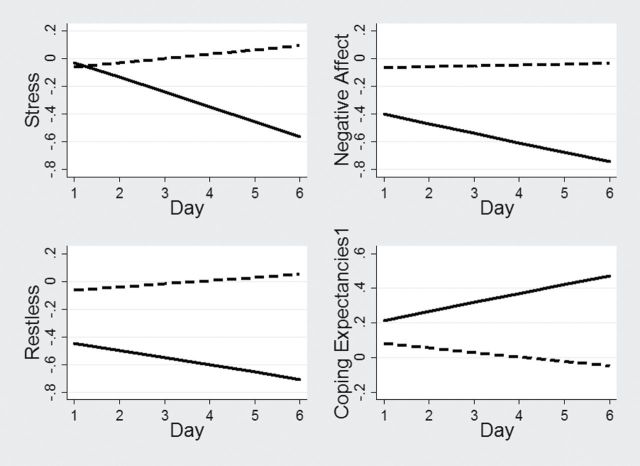
Logistic regression analyses indicated that the prequit slopes of stress (adjusted odds ratio [AOR] = 0.21, 95% confidence interval [CI] = 0.06–0.68, p = .01), negative affect (AOR = 0.21, 95% CI = 0.06–0.77, p = .03), and positive coping expectancies 1 (AOR = 2.91, 95% CI = 1.21–6.96, p = .01) significantly predicted biochemically verified quit date abstinence in unadjusted and adjusted models. Specifically, participants who had greater negative slopes for stress and negative affect, indicating attenuation of these variables across the prequit week, were more likely to quit on their scheduled quit date as compared to those who had flatter or positive slopes on these EMA variables. Those who had more positive slopes on positive coping expectancies were more likely to be abstinent on their quit date compared to those with flatter or negative slopes. Restlessness was a marginally significant predictor of quit date abstinence in the unadjusted model (p = .06), but a significant predictor in the adjusted model (AOR =0.31, 95% CI = 0.11–0.87, p = .03), whereby those with greater negative slopes for restlessness were more likely to be abstinent on the quit date. Logistic regression analyses (adjusted models) also indicated marginally significant relationships between the prequit slopes of both motivation variables and quit date abstinence (Motivation 1: AOR = 2.58, 95% CI = 0.91–7.31, p = .07; Motivation 2: AOR = 2.24, 95% CI = 0.92–5.43, p = .08). Specifically, participants who had gradual increases in motivation to quit smoking were marginally more likely to be abstinent on their scheduled quit date as compared to participants who had flat or decreasing motivation to quit. Figure 1 graphically depicts the slopes for those who were and were not abstinent on their scheduled quit date. Only the slopes of variables that significantly predicted quit date abstinence in adjusted models (i.e., negative affect, stress, positive coping expectancies, and restlessness) are displayed. The slope parameters for smoking urge, quit self-efficacy, hostility, positive affect, and positive smoking expectancies were not significantly associated with quit date abstinence in unadjusted and adjusted models. Notably, none of the calculated volatility parameters were related to quit date abstinence (all ps > .21).
Figure 1.
Random slopes of randomly prompted ecological momentary assessments of stress, negative affect, restlessness, and coping expectancies predict quit date abstinence. The presented slopes are adjusted for treatment group, sex, race/ethnicity, education, cigarettes per day, and baseline questionnaire assessments of the constructs, as available. Note. Dotted lines indicate nonabstainers on the quit date and solid lines indicate abstainers on the quit date.
Follow-up analyses were conducted to further examine the relations between EMA variable parameters and quit date abstinence. First, quadratic terms were calculated to examine potential nonlinear relations between each EMA variable and quit date abstinence. Results indicated no significant relations between quadratic EMA variable parameters and quit date abstinence. Second, we further explored the relation between EMA slope predictors and quit date abstinence after controlling for the slope of CPD (CPD was collected each prequit day via EMA). Adding this covariate did not substantively alter results. Third, in order to determine the relative influence of the four significant EMA slope predictors on quit date abstinence (i.e., stress, negative affect, positive coping expectancies, and restlessness), we conducted a multivariate analysis which included all of these slopes as predictors. No variable significantly predicted quit date abstinence in this multivariate analysis.
DISCUSSION
The identification of variables that predict quit date abstinence in homeless smokers seeking cessation treatment is a critical first step toward the development of novel tailored interventions that may be used to increase cessation rates in this difficult to treat population of smokers. The current study was the first, to our knowledge, to focus on predictors of quit attempt initiation in homeless smokers using EMA methodology. Overall, results indicated that trajectories of negative affect, stress, restlessness, and positive coping expectancy predicted quit date abstinence. Specifically, participants who had declining levels of negative affect, stress, and restlessness and increasing positive coping expectancies across the prequit week were significantly more likely to be abstinent on their scheduled quit date than those with other symptom trajectories. Consequently, homeless smokers whose negative affect, stress, and restlessness fail to attenuate and those who do not experience increases in positive coping expectancies may be at increased risk of failing to initiate a quit attempt.
The current results suggest that interventions initiated prior to the quit date should focus attention on reducing negative affect, stress, and restlessness, while increasing positive coping expectancies (e.g., that mood can be improved by means other than smoking). For example, cognitive-behavioral counseling approaches may help to reduce negative affect, stress, and restlessness, and increase positive coping expectancies. These symptoms might be targeted via clinic-based interventions or potentially by telephone counseling, as the findings from our own recent research with this population suggest that most homeless smokers (i.e., 58.4%) have an active cell phone (Project ADVANCE, heretofore unpublished data). Moreover, the current findings could also be used to inform future smart interventions. Specifically, smart phone delivered EMAs could be used, in real time, to prospectively identify individuals who are unlikely to quit on their scheduled quit date and automatically prompt tailored smart phone applications that aim to help these individuals address identified hurdles. More research is needed to better understand the potential components of and feasibility of such interventions in homeless smokers.
Few studies have examined EMA predictors of successful initiation of a quit attempt. Predicting quit attempt initiation is particularly important in this population because the majority of homeless smokers may be unable to achieve this initial milestone (Businelle et al., 2014). The current findings complement and extend previous EMA research that has focused on predictors of postcessation lapse/relapse among domiciled smokers. For example, previous research has indicated that the trajectory of prequit negative affect predicts relapse (McCarthy et al., 2006), and the current findings highlight the importance of prequit negative affect trajectory on quit attempt initiation as well. In the current study, trajectories of prequit restlessness and stress were also related to quit date abstinence. However, previous research has indicated that momentary changes in stress during the postquit period did not predict lapse and relapse (Shiffman & Waters, 2004). Thus, our findings support the idea that each cessation milestone deserves specific and careful examination. Finally, previous research has linked reductions in positive expectancies about smoking as a means to improve one’s mood (i.e., positive smoking expectancies) with short-term smoking abstinence (Gwaltney, Shiffman, Balabanis, & Paty, 2005; Weinberger, McKee, & George, 2010). Although this variable was not related to the initiation of a quit attempt in this study, our findings indicated that those who experienced increasing positive expectancies about their ability to cope with their mood without smoking (i.e., positive coping expectancies) were more likely to obtain initial abstinence as compared to those with no such improvement.
Although previous studies have indicated that rising nicotine urges/withdrawal predicted relapse among smokers (Piasecki et al., 2002; Piper et al., 2008), prequit smoking urge parameters among homeless smokers were not related to quit attempt initiation in the current study. In addition, the trajectories of a number of other variables were not related or only marginally related to quit date abstinence in this sample. Specifically, trajectories of positive affect, hostility, and self-efficacy did not predict quit date abstinence, and the trajectories of the motivation variables were only marginally related to quit date abstinence. These constructs may be less relevant or variable during the prequit phase, when smokers are still smoking ad libitum.
In the current study, volatility in subject ratings of each of the measured variables was unrelated to quit date abstinence. This finding was unexpected given previous work highlighting the importance of symptom volatility in predicting behaviors related to smoking lapses (e.g., alcohol consumption; Businelle, Lam, et al., 2013) and smoking lapse itself (Cofta-Woerpel et al., 2011; Piasecki et al., 2002) among domiciled populations. However, previous studies in this area have focused on postquit symptom volatility. It may be that symptom volatility may be more important during the postquit period than the prequit period, or may be more pronounced during the postquit period. Also, the methods used to calculate volatility in the current study (Cofta-Woerpel et al., 2011) may have influenced results. However, post-hoc analyses using other published methods of calculating symptom volatility (i.e., Piasecki et al., 2002) yielded similar results.
The current study has several limitations, including that the sample was relatively small and was recruited from one shelter in Texas. Thus, results may not be generalizable to other homeless smokers (e.g., nonsheltered or nontreatment seeking homeless smokers). In addition, small sample size and inclusion of up to six covariates in adjusted analyses may have limited power in univariate and multivariate analysis. Furthermore, analyses were limited to data collected during the prequit week. Data collected via EMA during the postquit week were not analyzed because very few participants (n = 3) were abstinent across the first postquit week. Larger studies that use EMA to assess homeless smokers for longer periods of time are needed in order to gain a better understanding of the barriers to smoking cessation and predictors of smoking lapse and relapse in this understudied and vulnerable population.
The current study has several strengths. Most notably, this is the first study to indicate that EMA methodology is feasible as a means of data collection in homeless smokers, and may yield critical information on the lives and health behaviors of this hard to reach, understudied, and underserved population. In addition, for the majority of variables examined, analyses controlled for baseline/average ratings of these constructs (e.g., average negative affect over the previous 2 weeks was controlled in EMA analyses of momentary ratings of negative affect). This allowed the examination of momentary fluctuations in the background levels of these variables (i.e., assessed at random time points), rather than the overall/average baseline levels of pertinent variables. This is especially important given that people who are experiencing homelessness may have high rates of baseline affective symptomatology (North, Eyrich, Pollio, & Spitznagel, 2004; Reitzel et al., 2014). Future research should identify other hurdles that curtail cessation attempts. This information could be used to improve interventions that aim to increase cessation and long-term abstinence among homeless smokers.
FUNDING
Funding for this research was provided by the UT School of Public Health . Data analysis and manuscript preparation were additionally supported through American Cancer Society grants MRSGT-12-114-01-CPPB (to MSB) and MRSGT-10-104-01-CPHPS (to DEK). Additional support for this study came from the National Institutes of Health through the M. D. Anderson Cancer Center Support Grant (CA016672) and the e-Health Technology Program, a resource of the Duncan Family Institute for Cancer Prevention and Risk Assessment. The funding sources had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENTS
The authors thank the staff at the Bridge Homeless Assistance Center for their work and support throughout the data collection portion of this project. Additionally, the authors thank Jay Dunn (Bridge CEO) and Neil Phillips (Bridge smoking cessation program coordinator and counselor) for their notable efforts that enabled this research.
REFERENCES
- Arnsten J. H., Reid K., Bierer M., Rigotti N. (2004). Smoking behavior and interest in quitting among homeless smokers. Addictive Behaviors, 29, 1155–1161. 10.1016/ j.addbeh.2004.03.010 [DOI] [PubMed] [Google Scholar]
- Baggett T. P., Rigotti N. A. (2010). Cigarette smoking and advice to quit in a national sample of homeless adults. American Journal of Preventive Medicine, 39, 164–172. 10.1016/j.amepre.2010.03.024 [DOI] [PubMed] [Google Scholar]
- Bailey S. R., Bryson S. W., Killen J. D. (2011). Predicting successful 24-hr quit attempt in a smoking cessation intervention. Nicotine & Tobacco Research, 13, 1092–1097. 10.1093/ntr/ntr151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrow S. M., Herman D. B., Cordova P., Struening E. L. (1999). Mortality among homeless shelter residents in New York City. American Journal of Public Health, 89, 529–534. 10.2105/AJPH.89.4.529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blalock J. A., Robinson J. D., Wetter D. W., Schreindorfer L. S., Cinciripini P. M. (2008). Nicotine withdrawal in smokers with current depressive disorders undergoing intensive smoking cessation treatment. Psychology of Addictive Behaviors, 22, 122–128. 10.1037/0893-164x.22.1.122 [DOI] [PubMed] [Google Scholar]
- Bonevski B., Baker A., Twyman L., Paul C., Bryant J. (2012). Addressing smoking and other health risk behaviours using a novel telephone-delivered intervention for homeless people: A proof-of-concept study. Drug & Alcohol Review, 31, 709–713. 10.1111/j.1465-3362.2012.00438.x [DOI] [PubMed] [Google Scholar]
- Businelle M. S., Cuate E. L., Kesh A., Poonawalla I. B., Kendzor D. E. (2013). Comparing homeless smokers to economically disadvantaged domiciled smokers. American Journal of Public Health, 103, S218–S220. 10.2105/AJPH.2013.301336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Businelle M. S., Kendzor D. E., Costello T. J., Cofta-Woerpel L. M., Li Y., Mazas C. A, … Wetter D. W. (2010). Mechanisms linking socioeconomic status to smoking cessation: A structural equation modeling approach. Health Psychology, 29, 262–273. 10.1037/a0019285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Businelle M. S., Kendzor D. E., Kesh A., Cuate E. L., Poonawalla I. B., Reitzel L. R, … Wetter D. W. (2014). Small financial incentives increase smoking cessation in homeless smokers: A pilot study. Addictive Behaviors, 39, 717–720. 10.1016/j.addbeh.2013.11.017 [DOI] [PubMed] [Google Scholar]
- Businelle M. S., Kendzor D. E., Reitzel L. R., Vidrine J. I., Castro Y., Mullen P. D, … Wetter D. W. (2013). Pathways linking socioeconomic status and postpartum smoking relapse. Annals of Behavioral Medicine, 45, 180–191. 10.1007/s12160-012-9434-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Businelle M. S., Lam C., Kendzor D. E., Cofta-Woerpel L., McClure J. B., Cinciripini P. M., Wetter D. W. (2013). Alcohol consumption and urges to smoke during a smoking cessation attempt. Experimental & Clinical Psychopharmacology, 21, 29–37. 10.1037/a0031009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler J., Okuyemi K. S., Jean S., Nazir N., Ahluwalia J. S., Resnicow K. (2002). Smoking characteristics of a homeless population. Substance Abuse, 23, 223–231. 10.1080/08897070209511495 [DOI] [PubMed] [Google Scholar]
- Castro Y., Mazas C., Businelle M. S., Heppner W. L., Correa-Fernandez V., Cofta-Woerpel L., Wetter D. W. (2012). The Texas Smoking Abstinence Motivation Scale (TSAMS): A short scale to assess motivation to quit smoking. Unpublished manuscript.
- Centers for Disease Control and Prevention. (2014). Current cigarette smoking among adults—United States, 2005–2012. Morbidity and Mortality Weekly Report, 63, 29–34. [PMC free article] [PubMed] [Google Scholar]
- Cofta-Woerpel L., McClure J. B., Li Y., Urbauer D., Cinciripini P. M., Wetter D. W. (2011). Early cessation success or failure among women attempting to quit smoking: Trajectories and volatility of urge and negative mood during the first postcessation week. Journal of Abnormal Psychology, 120, 596–606. 10.1037/a0023755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A gobal measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cox L. S., Tiffany S. T., Christen A. G. (2001). Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine & Tobacco Research, 3, 7–16. 10.1080/14622200020032051 [DOI] [PubMed] [Google Scholar]
- Gwaltney C. J., Shiffman S., Balabanis M. H., Paty J. A. (2005). Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. Journal of Abnormal Psychology, 114, 661–675. 10.1037/0021-843X.114.4.661 [DOI] [PubMed] [Google Scholar]
- Hwang S. W., Henderson M. J. (2010). Health care utilization in homeless people: Translating research into policy and practice working paper no. 10002 Retrieved from data_files/publications/workingpapers/wp_10002.pdf
- Hwang S. W., Wilkins R., Tjepkema M., O’Campo P. J., Dunn J. R. (2009). Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. British Medical Journal, 339, b4036. 10.1136/bmj.b4036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor D. E., Businelle M. S., Mazas C. A., Cofta-Woerpel L. M., Reitzel L. R., Irvin Vidrine J, … Wetter D. W. (2009). Pathways between socioeconomic status and health behavior among African American smokers. Journal of Behavioral Medicine, 32, 545–557. 10.1007/s10865-009-9226-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor D. E., Businelle M. S., Poonawalla I. B., Cuate E. L., Kesh A., Rios D. M., Balis D. S. (in press). Adjunctive financial incentives for abstinence among socioeconomically disadvantaged individuals participating in smoking cessation Treatment: A randomized controlled trial. American Journal of Public Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee T. C., Hanlon J. G., Ben-David J., Booth G. L., Cantor W. J., Connelly P. W., Hwang S. W. (2005). Risk factors for cardiovascular disease in homeless adults. Circulation, 111, 2629–2635. 10.1161/CIRCULATIONAHA.104.510826 [DOI] [PubMed] [Google Scholar]
- Matthews K. A., Gallo L. C. (2011). Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology, 62, 501–530. 10.1146/annurev.psych.031809.130711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy D. E., Piasecki T. M., Fiore M. C., Baker T. B. (2006). Life before and after quitting smoking: An electronic diary study. Journal of Abnormal Psychology, 115, 454–466. 10.1037/0021-843X.115.3.454 [DOI] [PubMed] [Google Scholar]
- North C. S., Eyrich K. M., Pollio D. E., Spitznagel E. L. (2004). Are rates of psychiatric disorders in the homeless population changing? American Journal of Public Health, 94, 103–108. 10.2105/AJPH.94.1.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuyemi K. S., Caldwell A. R., Thomas J. L., Born W., Richter K. P., Nollen N, … Ahluwalia J. S. (2006). Homelessness and smoking cessation: Insights from focus groups. Nicotine & Tobacco Research, 8, 287–296. 10.1080/14622200500494971 [DOI] [PubMed] [Google Scholar]
- Okuyemi K. S., Goldade K., Whembolua G., Thomas J. L., Eischen S., Sewali B, … Ahluwalia J. S. (2013). Motivational interviewing to enhance nicotine patch treatment for smoking cessation among homelessl smokers: A randomized controlled trial. Addiction, 108, 1136–1144. 10.1111/add.12140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki T. M., Jorenby D. E., Smith S. S., Fiore M. C., Baker T. B. (2002). Smoking withdrawal dynamics: II. Improved tests of withdrawal-relapse relations. Journal of Abnormal Psychology, 112, 14–27. 10.1037//0021-843X.112.1.14 [PubMed] [Google Scholar]
- Piper M. E., Federmen E. B., McCarthy D. E., Bolt D. M., Smith S. S., Fiore M. C., Baker T. B. (2008). Using mediational models to explore the nature of tobacco motivation and tobacco treatment effects. Journal of Abnormal Psychology, 117, 94–105. 10.1037/0021-843X.117.1.94 [DOI] [PubMed] [Google Scholar]
- Reitzel L. R., Kendzor D. E., Nguyen N., Regan S. D., Okuyemi K. S., Castro Y, … Businelle M. S. (2014). Shelter proximity and affect among homeless smokers making a quit attempt. American Journal of Health Behavior, 38, 161–169. 10.5993/AJHB.38.2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs-Ericsson N., Wise E., Debrody C. P., Paniucki H. B. (1999). Health problems and service utilization in the homeless. Journal of Health Care for the Poor & Underserved, 10, 443–452. 10.1353/hpu.2010.0717 [DOI] [PubMed] [Google Scholar]
- Shelley D., Cantrell J., Wong S., Warn D., Shelley D., Cantrell J, … Warn D. (2010). Smoking cessation among sheltered homeless: A pilot. American Journal of Health Behavior, 34, 544–552. 10.5993/AJHB.34.5.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Hufford M., Hickcox M., Paty J. A., Gnys M., Kassel J. D. (1997). Remember that? A comparison of real-time versus retrospective recall of smoking lapses. Journal of Consulting & Clinical Psychology, 65, 292–300. 10.1037//0022-006X.65.2.292.a [DOI] [PubMed] [Google Scholar]
- Shiffman S., Kirchner T. R. (2009). Cigarette-by-cigarette satisfaction during ad libitum smoking. Journal of Abnormal Psychology, 118, 348–359. 10.1037/a0015620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Scharf D. M., Shadel W. G., Gwaltney C. J., Dang Q., Paton S. M., Clark D. B. (2006). Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult smokers. Journal of Consulting & Clinical Psychology, 74, 276–285. 10.1037/0022-006X.74.2.276 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Waters A. J. (2004). Negative affect and smoking lapses: A prospective analysis. Journal of Consulting & Clinical Psychology, 72, 192–201. 10.1037/0022-006X.72.2.192 [DOI] [PubMed] [Google Scholar]
- Spector A., Alpert H., Karam-Hage M. (2007). Smoking cessation delivered by medical students is helpful to homeless population. Academic Psychiatry, 31, 402–405. 10.1176/appi.ap.31.5.402 [DOI] [PubMed] [Google Scholar]
- Stone A. A., Schwartz J. E., Neale J. M., Shiffman S., Marco C. A., Hickcox M, … Cruise L. J. (1998). A comparison of coping assessed by ecological momentary assessment and retrospective recall. Journal of Personality and Social Psychology, 74, 1670–1680. 10.1037//0022-3514.74.6.1670 [DOI] [PubMed] [Google Scholar]
- Toro P. A., Tompsett C. J., Lombardo S., Philippot P., Nachtergael H., Galand B, … Harvey K. (2007). Homelessness in Europe and the United States: A comparison of prevalence and public opinion. Journal of Social Issues, 63, 505–524. 10.1111/j.1540-4560.2007.00521.x [Google Scholar]
- Watson D., Clark L. A., Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. 10.1037//0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Weinberger A. H., McKee S. A., George T. P. (2010). Changes in smoking expectancies in abstinent, reducing, and non-abstinent participants during a pharmacological trial for smoking cessation. Nicotine & Tobacco Research, 12, 937–943. 10.1093/ntr/ntq120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreb L., Goldberg R., Perloff J. (1998). Health characteristics and medical service use patterns of sheltered homeless and low-income housed mothers. Journal of General Internal Medicine, 13, 389–397. 10.1046/j.1525-1497.1998.00119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter D. W., McClure J. B., Cofta-Woerpel L., Costello T. J., Reitzel L. R., Businelle M. S., Cinciripini P. (2011). A randomized clinical trial of a palmtop computer-delivered treatment for smoking relapse prevention among women. Psychology of Addictive Behaviors, 25, 365–371. 10.1037/a0022797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh V. M., McCarthy D. E., Baker T. B. (2012). An ecological momentary assessment analysis of prequit markers for smoking-cessation failure. Exp Clin Psychopharmacol, 20, 479–488. 10.1037/a0029725 [DOI] [PMC free article] [PubMed] [Google Scholar]