Abstract
Background
The recommendation for using posterior-stabilized (PS) implants in patellectomy patients undergoing total knee arthroplasty (TKA) is based on older case series with heterogeneous patient populations. The use of cruciate-retaining implants in these patients has not been evaluated with more contemporary implant designs.
Questions/purposes
The purpose of this study was to evaluate the survivorship and functional outcomes (Knee Society score, presence of an extensor lag, and range of motion) of cruciate-retaining (CR) TKA in patients with prior patellectomy.
Methods
Between 1986 and 2012, we performed 27 CR TKAs in 25 patients after patellectomy. Of those, 23 CR TKAs in 21 patients were available for followup at a minimum of 2 years (mean, 11.2 years; range, 2.3–25.1 years). In this retrospective study, we queried a prospectively maintained database to assess functional outcomes and survivorship.
Results
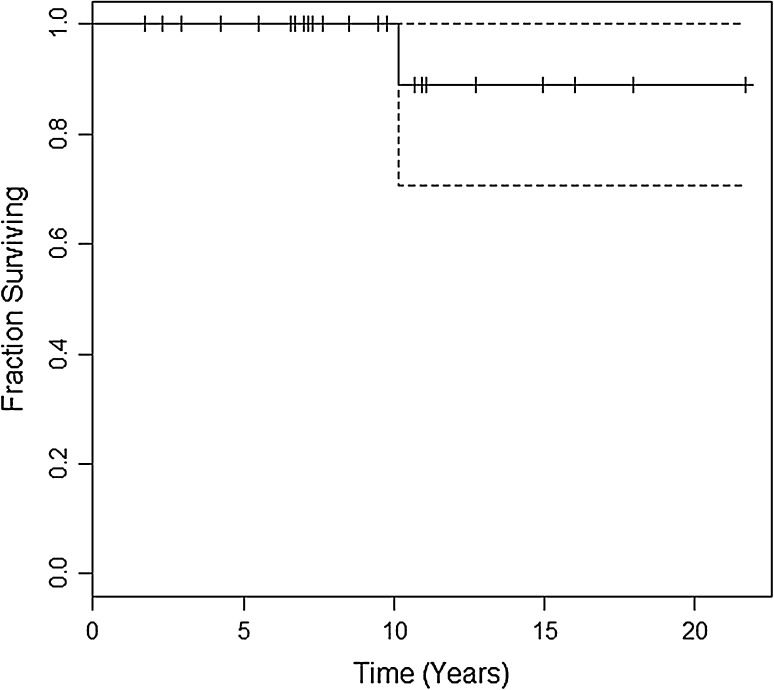
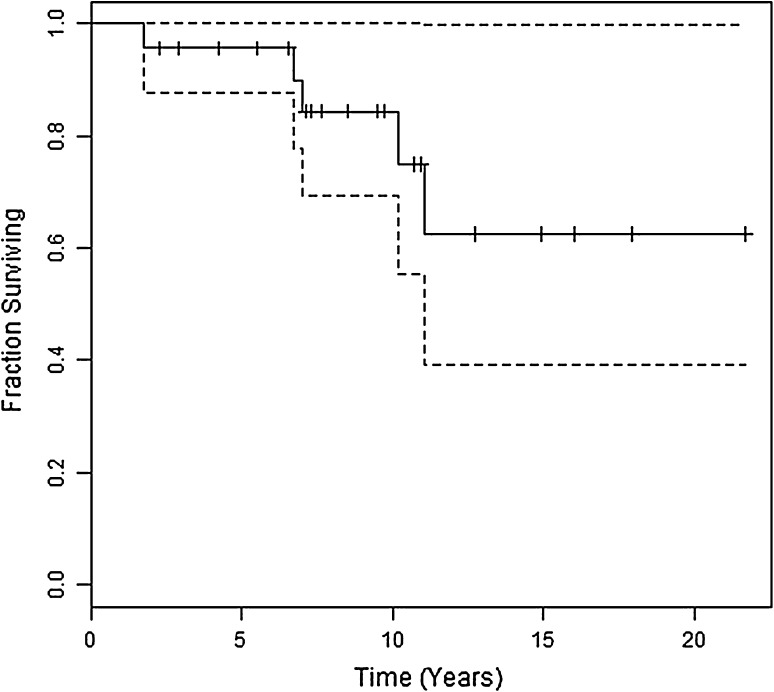
Aseptic loosening-free survival was 100% at 5 and 10 years, and survival with revision for any reason as the outcome was 96% at 5 years (95% confidence interval [CI], 87.7%–100%) and 84% at 10 years (95% CI, 69.5%–100%). One patient was revised for aseptic loosening at 10.2 years postoperatively. Mean Knee Society scores improved from 36 ± 13 preoperatively to 92 ± 9.6 at followup. Extensor lag was present in seven patients preoperatively and only three at followup. Average knee flexion at followup was 112° ± 12.5°.
Conclusions
In this study we found good long-term survivorship and functional outcomes with a CR implant design in patients following patellectomy. Earlier studies have favored PS over CR implants for patients with patellectomies. We believe this series suggests that CR TKA is indeed an option in patients with patellectomy.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
It has been proposed that the AP intrinsic stability of the knee is a result of a four-bar linkage system consisting of the patella and quadriceps tendons and the anterior and posterior cruciate ligaments [15]. This mechanism affords AP knee stability during knee flexion but is contingent on a normal extensor mechanism. The patella serves to position the quadriceps and patella tendons such that they are parallel to the anterior and posterior cruciate ligaments, respectively. This allows those pairs of ligaments to work in concert to afford stability to the knee. When the patella is absent such as in a patellectomized patient, the four-bar linkage system is disrupted [4, 15].
In a patient with knee osteoarthritis, often the anterior cruciate ligament is absent or deficient, which, when combined with a disrupted four-bar linkage system in a patellectomized patient, can result in a loss of intrinsic AP stability of the knee. For patients undergoing TKA in this setting, increased stresses may theoretically be transferred to the prosthetic components [10]. It has been suggested that posterior-stabilized (PS) designs are preferred over cruciate-retaining (CR) prostheses in patellectomy patients undergoing TKA because of intrinsic AP stability provided by the PS prosthesis itself [10, 11, 15]. Most of the early literature in the 1980s and 1990s on TKA in patients with prior patellectomy has supported the use of PS implants over CR designs [2, 3, 5, 10, 12, 14]. However, most of those studies had very small sample sizes, heterogeneous patient populations with both revisions and primary knee arthroplasties included, and multiple implant designs, making it difficult to draw any meaningful conclusions. Furthermore, most of the implant designs used in those studies are no longer in clinical practice.
The purposes of this study, therefore, were (1) to evaluate the survivorship of CR TKA in patients with prior patellectomy at a mean of 11 years (range, 2–25 years); and (2) to evaluate the functional outcomes (Knee Society score, presence of an extensor lag, and ROM) of those same patients.
Patients and Methods
A prospectively maintained database of two senior arthroplasty surgeons (TST, RDS) was searched for all patients who underwent a primary CR TKA after a previous ipsilateral patellectomy. Between 1986 and 2012, 27 CR TKAs in 25 patients were identified with a minimum followup of 2 years (mean, 11 years; range, 2–25 years). During this time period we did not identify any patients with a prior patellectomy who underwent a PS TKA. Three patients were lost to followup before their 2-year visit, and one patient had surgery less than 2 years before data collection began for the present study. None of the excluded patients had undergone revision before being lost. The one patient who underwent surgery less than 2 years ago had not undergone revision at the time of this study. The study population, therefore, consisted of 23 CR TKAs in 21 patients. There were six deaths; because all six had been followed for at least 2 years, the data from those patients were included in the analysis.
The CR implants used were 11 PFC (DePuy Orthopaedics Inc, Warsaw, IN, USA) (all done before 1995), seven Sigma fixed-bearing (DePuy Orthopaedics Inc), and five Sigma rotating platform (DePuy Orthopaedics Inc).
Demographic data were recorded from the database for each patient. The patients had a mean age of 57.8 ± 9.4 years. Mean preoperative Knee Society score (KSS) was 36.4 ± 13 and mean preoperative Knee Society functional score was 51.1 ± 16. The mean time interval between patellectomy and TKA was 23.4 years (range, 3–52 years). Reasons for patellectomy included recurrent patella instability in eight, patella fracture in seven, patella infection in three, severe patellofemoral osteoarthrosis in one, and unclear reasons in the remaining four who each reported childhood patella problems without specific details.
Clinical outcomes were assessed by comparing preoperative and postoperative KSS for each patient, which were graded according to the following scoring system: 85 to 100 excellent, 70 to 84 good, 60 to 69 fair, and < 60 poor [7]. The ability of the patient to ascend and descend stairs was recorded from the KSS functional outcome score questionnaire [7]. Preoperative and postoperative knee ROM was assessed using a goniometer or at the operating surgeon’s discretion. All revision surgeries were recorded as well as the specific reason for each revision. An attempt to contact all patients by telephone was performed to confirm accuracy of all revisions recorded in the database.
Survivorship analysis was conducted using the Kaplan-Meier survival method through the “survival” package in R [16, 17]. Survival curves were calculated for patients undergoing revision for aseptic loosening and/or instability alone with other indications for revision treated as censored data. Additional survival analysis was performed for all patients undergoing revision for any reason (uncensored revisions). Ninety-five percent confidence intervals were estimated through the survival model and given as log-based percentages.
Results
Aseptic loosening-free survival was 100% at 5 and 10 years postoperatively (Fig. 1). Total revision-free survival for any reason was 96% at 5 years (95% confidence interval [CI], 87.7%–100%) and 84% at 10 years (95% CI, 69.5%–100%) (Fig. 2). Five patients underwent revision during followup. Two patients underwent polyethylene exchange at 6.75 years and 11 years postoperatively for wear and osteolysis without loosening of the components. One patient developed a late infection 7 years postoperatively and underwent a two-stage exchange. One patient had repeat falls during the first postoperative year with resultant collateral ligament instability requiring revision with increased component constraint. One patient was revised for aseptic loosening of the tibial component at 10.2 years postoperatively.
Fig. 1.
Kaplan-Meier survivorship curve with revision for aseptic loosening as the endpoint with 95% CIs (dotted lines) is demonstrated.
Fig. 2.
Kaplan-Meier survivorship curve with revision for any reason as the endpoint with 95% CIs (dotted lines) is demonstrated.
Mean KSS improved from 36.4 ± 13 preoperatively to 92.1 ± 9.6 at 11.2 years average followup. Preoperative KSS were all classified as poor, and at latest followup (including after any revision surgery), there were 18 excellent, four good, and one fair result. Seven patients had a preoperative extensor lag ranging from 5° to 15°. At latest followup, three patients had a persistent extensor lag: one each measuring 5°, 10°, and 15°. Average knee flexion at followup was 112° ± 12.5° (range, 90°–135°).
Discussion
The recommendation that patellectomy patients undergoing TKA should have a PS design has been based on limited evidence from prior studies, which evaluated heterogeneous groups [3–5, 7, 12, 14]. It has been theorized that the loss of intrinsic knee AP stability in a patellectomy patient would predispose a CR TKA to early failure secondary to aseptic loosening and/or instability. However, this has never been shown convincingly in the literature. Prior comparative studies such as that by Paletta and Laskin had very small sample sizes with only nine patients in their PS group [14]. Despite being a comparative study, it is difficult with such small numbers to draw meaningful conclusions regarding superiority of one type of TKA over another in patellectomy patients. In the current study, with CR implants, patients with a prior patellectomy demonstrated excellent survivorship and functional outcomes at a mean of 11 years.
This study is subject to a number of limitations. As a result of a retrospective design, the current study is subject to selection bias; however, all patellectomy patients who underwent TKA were considered for inclusion, and we were unable to find any patients with prior patellectomy who underwent a primary PS TKA in the senior authors’ database. The lack of a comparison group is another weakness, but the relative infrequency of patellectomy poses a logistical challenge to conducting such a randomized or even comparative study. The few comparative data available on this topic involve smaller groups than the group we evaluated [14] or evaluations of more heterogeneous (or no longer available) implants [12]. Even so, as a result of a lack of a comparison group, we are unable to comment on the comparativeness of CR and PS TKA in this series of patellectomy patients. The authors would suggest a multiinstitutional comparative study as a future possibility. Additionally, the patients in this study did not undergo objective AP knee translation measurement to more accurately delineate AP stability of the knee, and this study is subject to assessor bias, which may be relevant to surgeon-assessed outcomes such as ROM and extensor lag. Finally, three patients were lost to followup before the 2-year minimum. If they have undergone revision elsewhere, that would diminish the survivorship reported here.
In this study, CR TKA in patellectomized patients demonstrated survivorship of 100% at 10 years with revision for aseptic loosening as the endpoint. There are no prior studies on survivorship of CR TKA postpatellectomy with which to compare. The only other series on CR TKA postpatellectomy recently reported no cases of revision at midterm followup [6]. When considering revision for any reason as the outcome, we found 10-year survivorship to be 84%. Comparatively, Yao et al. [18] reported a large series of TKA after patellectomy, in which 48 of 52 implants were PS, and found an overall 19.2% revision rate at mean 5.75-year followup. Although survivorship of PS and CR implants is similar in patellectomy patients, they are both worse when compared with primary TKA in patients with intact patellae, which has been shown to have 10-year survivorship ranging from 93% to 98% [1, 9, 13].
In general, studies have shown inferior functional outcomes of TKA in patellectomy patients when compared with those with an intact patella [8, 12, 18]. Some have reported inferior functional outcomes of CR TKA when compared with PS TKA in patellectomy patients [14], whereas others have not shown a difference in functional outcomes between implant designs [18]. Paletta and Laskin [14] reported an average KSS score of 67 with cruciate retention compared with 89 with PS TKA in patellectomized patients at mean 5-year followup. By contrast, Kang et al. [8] reported a mean KSS score of 82.5 in their CR group and found no difference compared with PS patients. In the current study, the average KSS score was 92.1 at mean 11.2 years followup, which is comparable to prior PS cohorts. We also found mean knee flexion to be 111° at followup, which is comparable to the 118° of knee flexion shown in the recent midterm report on CR TKA after patellectomy by Dahiya et al. [6]. Similar knee flexion arcs of 104° and 110° have been shown in PS TKA for patellectomy and intact patellae, respectively [18].
In this case series of TKA in patients with prior patellectomy, we found good survivorship and functional outcomes with a CR implant design at mean 11.2 years followup. Although we cannot recommend this approach—or discount an alternative treatment such as PS TKA—we believe that these data suggest that CR TKA is a potentially viable option, and multicenter studies will be needed to draw firmer conclusions in terms of its efficacy relative to PS TKA in patients who have had patellectomies.
Footnotes
Two of the authors certify that he (TST, RDS), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001 from DePuy (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Brigham and Women’s Hospital, Boston, MA, USA.
References
- 1.Argenson JN, Parratte S, Ashour A, Saintmard B, Aubaniac JM. The outcome of rotating-platform total knee arthroplasty with cement at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2012;94:638–644. doi: 10.2106/JBJS.K.00263. [DOI] [PubMed] [Google Scholar]
- 2.Bayne O, Cameru HU. Total knee arthroplasty following patellectomy. Clin Orthop Relat Res. 1984;186:112–114. [PubMed] [Google Scholar]
- 3.Cameron HU, Cungen HU, Vyamont D. Posterior stabilized knee prosthesis for total knee replacement in patients with prior patellectomy. Can J Surg. 1996;39:469–473. [PMC free article] [PubMed] [Google Scholar]
- 4.Cameron HU, Fedorkow DM. The patella in total knee arthroplasty. Clin Orthop Relat Res. 1982;165:197. [PubMed] [Google Scholar]
- 5.Cameron HU, Jung YB. Prosthetic replacement of the arthritic knee after patellectomy. Can J Surg. 1990;33:119–121. [PubMed] [Google Scholar]
- 6.Dahiya V, Gupta H, Rajgopal A, Vasdev A. Midterm results of cruciate retaining total knee arthroplasty in patellectomized patients. Indian J Orthop. 2013;47:31–34. doi: 10.4103/0019-5413.106891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 8.Kang JD, Papas SN, Rubash HE, McClain EJ., Jr Total knee arthroplasty in patellectomized patients. J Arthroplasty. 1993;8:489–501. doi: 10.1016/S0883-5403(06)80214-7. [DOI] [PubMed] [Google Scholar]
- 9.Keenan AC, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ. Ten-year survival of cemented total knee replacement in patients aged less than 55 years. J Bone Joint Surg Br. 2012;94:928–931. doi: 10.1302/0301-620X.94B7.27031. [DOI] [PubMed] [Google Scholar]
- 10.Larson KR, Cracchiolo A, Dorey FJ, Finerman GAM. Total knee arthroplasty in patients after patellectomy. Clin Orthop Relat Res. 1991;264:243–254. [PubMed] [Google Scholar]
- 11.Lennox DW, Hungerford DS, Krackow KA. Total knee arthroplasty following patellectomy. Clin Orthop Relat Res. 1987;223:220–224. [PubMed] [Google Scholar]
- 12.Martin SD, Haas SB, Insall JN. Primary total knee arthroplasty after patellectomy. J Bone Joint Surg Am. 1995;77:1323–1330. doi: 10.2106/00004623-199509000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res. 2013 Nov 19 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 14.Paletta GA, Jr, Laskin RS. Total knee arthroplasty after a previous patellectomy. J Bone Joint Surg Am. 1995;77:1708–1712. doi: 10.2106/00004623-199511000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Sledge C, Ewald F. Total knee arthroplasty experience at the Robert Breck Brigham Hospital. Clin Orthop Relat Res. 1979;145:78. [PubMed] [Google Scholar]
- 16.Therneau T. A package for survival analysis in S. R package version 2.37-4. 2013. Available at: http://CRAN.R-project.org/package=survival. Accessed July 2013.
- 17.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, NY, USA: Springer; 2000. [Google Scholar]
- 18.Yao R, Lyons MC, Howard JL, McAuley JP. Does patellectomy jeopardize function after TKA? Clin Orthop Relat Res. 2013;417:544–553. doi: 10.1007/s11999-012-2653-4. [DOI] [PMC free article] [PubMed] [Google Scholar]