Abstract
Human papillomavirus (HPV) infection is a major risk factor for cervical cancer. However, only some high risk human papillomavirus (HR-HPV)-infected women progress to cervical cancer, host immunogenetic factors human leukocyte antigen (HLA) may account for viral antigens presenting individually or together in the progression to cervical cancer. This study examined the association between the development of invasive cervical cancer (ICC) and the determinant factors including HLA-DRB1*1501 and DQB1*0602, HR-HPV infection among Chinese Uighur and Han populations. Blood samples, cervical swabs and biopsies were obtained from 287 patients with ICC (192 Uighurs and 95 Hans) and 312 healthy controls (218 Uighurs and 94 Hans). HPV DNA was detected by PCR and HLA-DRB1*1501 and DQB1*0602 alleles were performed using PCR-SSP method. HPV16 infection rates was significantly higher among Uighur and Han with ICC as compared to healthy controls (OR = 58.317; 95% CI: 39.663-85.744; OR = 33.778; 95% CI: 12.581-90.691; P < 0.05 for all). HLA-DRB1*1501 (OR = 0.305; 95% CI: 0.115-0.813; P < 0.05) and HLA-DRB1*1501-DQB1*0602 haplotype frequencies (OR = 0.274; 95% CI: 0.086-0.874; P < 0.05) were significantly reduced in Han ICC. The HLA-DQB1*0602 frequency significantly decreased among Uighur women with ICC (OR = 0.482; 95% CI: 0.325-0.716; P < 0.05). Similar tendencies were observed for DQB1*0602 with HPV16-positive ICC (OR = 0.550; 95% CI: 0.362-0.837; P < 0.05). This study suggests that HLA-DRB1*1501 and DQB1*0602 alleles may influence the immune response to HPV16 infection and decrease the risk of ICC among Uighurs and Hans in Xinjiang, China.
Keywords: HLA, invasive cervical cancer, HPV, susceptibility, Uighur
Introduction
Cervical cancer is the second most common type of cancer among women, with 400,000 new cases reported annually worldwide; of this number, 13,000 cases were recorded in China [1]. Uighurs living in Xinjiang are one of the ethnic groups with the highest reported incidence rates of cervical cancer [2]. The rate of cancer incidence among Uighurs is 527/100,000 [3], much higher than the average rate of 126.94/100,000 in China [4].
Research has shown that human papillomaviruses (HPVs) play a central role in cervical cancer etiology [5,6]. However, patients with HPV infection regress spontaneously, and only a small fraction of these cases develop into persistentn infection and cancer, which suggests that other factors are also involved in the pathogenesis of the disease. One potential cofactor is the host cellular immune response to HPV infection and cancer cells mediated by the human leukocyte antigen (HLA)-restricted T lymphocytes [7].
HLA class II (HLA-II) alleles involved in presenting foreign antigens to the immune system cells are important in host immune responses to viruses and other pathogens. Among the most polymorphic human genes, HLA-II polymorphism results in peptide-binding cleft variations, influencing the binding and presentation of antigens to T cells [8]. Given that the host immune response to HPV is an important determinant of HPV persistence and progression to high-grade lesions and cancer [9,10], HLA-II variations, which are also related to ethnicity, may affect cervical cancer pathogenesis through immunological control of HPV.
Many studies have examined the association between HLA-II alleles polymorphism, HPV infection, and cancer development, especially among those with high degrees of DRB1 and DQB1 polymorphism [11-13]. However,HPV infection and cancer cells mediated by the human leukocyte antigen (HLA)-restricted populations. For example, HLA-DRB1*1501 and -DQB1*0602 [14-16] reflect discrepancies under racial differences. Because HLA-II allele frequencies differ in various ethnic and racial groups, which are different in Uighurs compared with Chinese Han and other population groups, and the published data on the distribution of HLA-II alleles among Uighur patient with cervical cancer are not reported as yet. So in this study, we explore the relationship between two HLA-II alleles (HLA-DRB1*1501 and HLA-DQB1*0602) and the occurrence and progression of invasive cervical cancer (ICC) among Uighur and Han people in Xinjiang, China.
Materials and methods
Study subjects
Two hundred eighty-seven specimens were collected between 2000 and 2008, 192 and 95 of which came from Chinese Uighur and Han women, respectively. The patients were evaluated by colposcopy and biopsy to confirm the invasive cervical cancer (ICC), and received neither pre-operative radiotherapy nor chemotherapy. Uighur and Han patients were aged 24 to 65 years and 30 to 63 years, respectively. The control population was selected randomly from an opportunistic screening program in the same hospitals. Cervical smear cytology detection confirmed negative findings of intraepithelial lesion or malignancy, included 218 Uighur and 94 Han women aged 30 to 71 years and 30 to 66 years, respectively. All patients were recruited from the Department of Kashi People’s Hospital and The First Affiliated Hospital of Shihezi University School of Medicine, Xinjiang, China. Peripheral blood samples, cervical scrapings, or biopsy samples were collected from all the participants with written informed consent, used as sources of DNA for HPV and HLA typing.
HPV typing
DNA was extracted from cervical scrapings or biopsy samples using the phenol-chloroform method [17,18]. We used β-globin signals to confirm sample DNA quality; samples with strong signals for HPV and HLA genotypes were chosen. HPV-DNA was detected using primer polymerase chain reaction (PCR). Positive and negative controls were set for each reaction; positive control for the CaSki (HPV 16E6) and Hala (HPV 18 E6) cell DNA (Beijing Institute for Cancer Prevention Laboratory Professor Yang Ke favors). The primers used for HPV16E6 detection were as follows: forward, 5’-GACCCAGAAAGTTACCACAG-3’; reverse, 5’-CACAACGGTTTGTTGT ATTG-3’. To detect HPV18 E6, the following primers were used: forward, 5’-TGCCAGA AACCGTTGAATCC-3’; reverse, 5’-TCTGAGTCGCTTAATTGCTC-3’. The primers for synthesis were sourced from Shanghai Health Industrial Co., Ltd, China. PCR reactions for HPV16 detection were as follows: predegeneration at 94°C for 3 min, degeneration at 94°C for 45 s, annealing at 55°C for 45 s, and an extension at 72°C for 45 s, for a total of 35 cycles. PCR reactions for HPV18 detection were as follows: predegeneration at 94°C for 4 min, degeneration at 94°C for 45 s, annealing at 54°C for 45 s, and an extension at 72°C for 60 s, for a total of 35 cycles. Electrophoresis of HPV16 and HPV18 were performed on a 2% agarose gel, which was then imaged under ultraviolet light and photographed (Figure 1).
Figure 1.
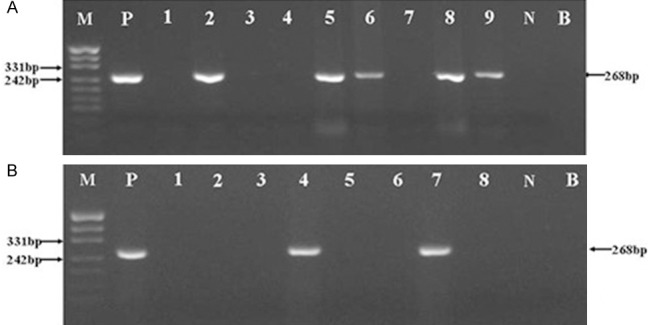
A: HPV16 PCR gel electrophoresis results. M, Mark; P, Positive control (268 bp). 1-9: Cervical tissue samples. N, Negative control; B, Blank. B: HPV18 PCR amplification electrophoresis results. M, Mark; P, Positive control (268 bp). 1-8: Cervical tissue samples. N, Negative control; B, Blank.
Detection of HLA-DRB*1501 and HLA-DQB1*0602
DNA was extracted from blood samples using an automated extractor (QIAamp BioRobot, Qiagen, Hilden). HLA-DRB1*1501 and HLA-DQB1*0602 alleles were identified using sequence-specific primers based on the PCR-SSP method. Positive, negative, and internal controls were set for each reaction (human growth hormone, HGH). Here, we removed false positive and false negative results. The sequence-specific primers are referred to an article by Olerup [19,20]. The primers used for HLA-DRB1*1501 were as follows: forward, 5’-TTCCTGTGGCAGCCTAAGAGG-3’; reverse, 5’-CCGCTGCACTGTGAAGCTCT-3’. The primers used for HLA-DQB1*0602 were as follows: forward, 5’-CGTGCGTCTTCTGACCAGAT-3’; reverse, 5’-GCTGTTCCAGTACTCGGCAT-3’. The primers used for HGH were as follows: forward, 5’-GCCTTCCCAACCATTCCCTTA-3’; reverse, 5’-TCACGGATTTCTGTTGTGTTTC-3’. The primers used for synthesis were sourced from Shanghai Health Industrial Co., Ltd, China. PCR reactions were performed as follows: predegeneration at 94°C for 5 min, denaturation at 94°C for 30 s, annealing at 60°C for 45 s, and an extension at 72°C for 30 s, for a total of 35 cycles. PCR products were electrophoresed in 2% agarose gel, which was then imaged under ultraviolet light and photo-graphed (Figure 2). PCR products were purified and directly sequenced (sent to Shanghai Health Industrial Co., Ltd), and results were homologically analyzed using a BLAST analysis station.
Figure 2.
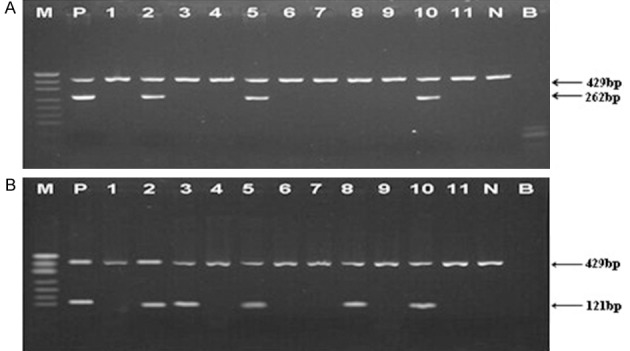
A: HLA DRB1*1501 PCR gel electrophoresis results. M, Mark; P, Positive control (262 bp). 1-11: Cervical tissue samples. N, Negative control; B, Blank; HGH, Internal control (429 bp). B: HLA DQB1*0602 PCR gel electrophoresis results. M, Mark; P, Positive control (121 bp). 1-11: Cervical tissue samples. N, Negative control; B, Blank; HGH, Internal control (429 bp).
Quality control
DNA preparation, PCR, and PCR product detection were carried out in separate spaces. Ultraviolet was used to monitor environmental contamination prior to the experiments, and new sterile gloves and supplies were used to avoid contamination. β-globin signals were used to confirm sample DNA quality, and DNA with sufficient quality was chosen for PCR. Positive and negative controls were set up for each PCR reaction. About 30% of the samples were randomly chosen to repeat the tests, and the same results were obtained.
Statistical analysis
SPSS version 13.0 was employed for all statistical analyses. The t-test and Mantel-Haenszel χ2 test were used for continuous and categorical variables, respectively. Odds ratios (OR) and 95% CI were calculated using logistic regression to estimate the relative likelihood between two HLA-II polymorphisms and the risk of cervical cancer across genotypes. We adjusted multiple comparisons using Bonferroni correction and considered P values less than 0.05 significant.
Results
All test cases were diagnosed as ICC by two pathologists. The case and control groups had similar age ranges (P > 0.05), and beta-globin PCR results showed that all subjects have specimens with sufficient quality for HLA and HPV analyses.
The fractions of HPV16-positive cases among the Uighurs and Hans in the case group were 78.7% and 64.3%, obviously higher than those of Uighurs (6.0%) and Hans (5.3%) control group (OR = 58.937; 95% CI: 22.672-153.208; OR = 33.778; 95% CI: 12.581-90.691; P < 0.05 for all), respectively, and the HPV16 infection rates were higher among Uighurs than Hans (OR = 2.053; 95% CI: 1.192-3.534; P < 0.05). The HPV18 infection rate was only 2% in the case group, no significantly difference in HPV18 infection rate were observed between the case and control groups (P > 0.05).
The distribution of HLA-DRB1*1501 and HLA-DQB1*0602 among Uighurs in the case and control groups is shown in Table 1. The frequency of HLA-DQB1*0602 significantly decreased among Uighur women with ICC (OR = 0.482; 95% CI: 0.325-0.716; P < 0.05) compared with that in the normal control group. Similar patterns were observed between DQB1*0602 and HPV16-positive ICC patients (OR = 0.550; 95% CI: 0.362-0.837; P < 0.05). Unlike Uighur population, the frequency of HLA-DQB1*0602 in Chinese Han ICC population was not significantly changed relative to healthy control group (Table 2). However, the frequency of HLA-DRB1*1501 (OR = 0.305; 95% CI: 0.115-0.813; P < 0.05) significantly decreased among Han women with ICC. Further, similar change was also seen in the frequency of HLA-DRB1*1501-DQB1*0602 haplotype in Han women with ICC relative to healthy control group (OR = 0.274; 95% CI: 0.086-0.874; P < 0.05).
Table 1.
The distribution of HLA-DRB1*1501, DQB1*0602 in Uighur patient and control group
| HLA | ICC (n = 192) | HPV16 ICC (n = 151) | Control (n = 218) | ICC | HPV16 ICC | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| P | OR (95% CI) | P | OR (95% CI) | ||||
| DRB1*1501 | 38 | 34 | 44 | 1.000 | 0.976 (0.601-1.585) | 0.682 | 1.149 (0.693-1.905) |
| DQB1*0602 | 79 | 67 | 129 | 0.000 | 0.482 (0.325-0.716) | 0.007 | 0.550 (0.362-0.837) |
| DRB1*1501-DQB1*0602 | 28 | 27 | 39 | 0.441 | 0.784 (0.461-1.331) | 1.000 | 0.999 (0.582-1.718) |
Table 2.
The distribution of HLA-DRB1*1501, DQB1*0602 in Han patient and control group
| HLA | ICC (n = 95) | HPV16 ICC (n = 61) | Control (n = 94) | ICC | HPV16 ICC | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| P | OR (95% CI) | P | OR (95% CI) | ||||
| DRB1*1501 | 6 | 6 | 17 | 0.024 | 0.305 (0.115-0.813) | 0.238 | 0.494 (0.183-1.334) |
| DQB1*0602 | 33 | 27 | 42 | 0.212 | 0.659 (0.367-1.184) | 1.000 | 0.983 (0.514-1.881) |
| DRB1*1501-DQB1*0602 | 4 | 4 | 13 | 0.04 | 0.274 (0.086-0.874) | 0.294 | 0.437 (0.136-1.410) |
Discussion
Several studies have shown that HPV infection is the primary cervical cancer etiology. HPV typing results of the case group HPV16 was most commonly types (78.7% in Uighur, 64.3% in Han), obviously higher than that of control group. These results are similar to those in a previous report [21]. Hint that HPV16 infection plays a central role in cervical cancer, especially in Uighur women.
Several researchers have considered polymorphisms of HLA-II type alleles to be closely related to HPV infection [10,12,22,23]. HLA-II showed a close relationship with HPV16-positive Kazakh esophageal carcinoma in our previous work [24]. HLA-II genes mainly function in identifying and presenting exogenous antigens, such as HPV. Different HLA-II alleles, capacities of identification, combinations of HPV, and presentations of antigenic peptides to CD4+ T cells have been uncovered. HLA-II alleles that are difficult to identify and clear by the HPV virus are called HPV virus susceptibility alleles; by contrast, those alleles that are easy to identify and clear by the HPV virus can prevent HPV allele infection. Those HPV susceptibility alleles cause persistent HPV infections and are maintained in the body, subsequently causing tumors [8,25].
Some published data on the distribution of HLA-II alleles among cervical cancer are available. However, results among various populations often differ and sometimes even contradict, especially when considering HLA-DRB1*1501 and DQB1*0602 alleles. Beskow [26] examined the distribution of HLA-DRB1 and DQB1 allele frequencies in cervical cancer among Swedish women and found that HLA-DRB1*1501 is related to long-term HPV infection, and this allele particularly increases the risk of developing HPV16-related cervical cancer. Cuzick [27] detected cervical squamous cell carcinoma among women from the United Kingdom and found that HLA DRB1*1501 and HLA-DQB1*0602 do not increase the risk of cervical squamous cell carcinoma but are associated with HPV 16-positive cervical squamous cell carcinoma. Similar reports show the same results among Chinese [28] and Brazilian [29] women. Other studies, however, reported different results. A study by Wu [16] showed that the distributions of HLA DRB1*1501 and HLA-DQB1*0602 decrease among HPV-infected Han women and cervical cancer female patients in China. Ferrera [30] also found that HLA-DQB1*0602 presents decreased risks of cervical cancer among Honduran women. Differences among sampling methods, sensitivity of detection methods, geographic areas and racial factors, and disease status have been cited as potential causes of inconsistency among reports. In this work, highly sensitive HLA detection assays were performed to avoid uncertainty factors. We employed strict quality control measures from DNA preparation to PCR analysis. β-globin primer was used for all ICC sample quality appraisals, and DNA positive and negative controls were set up to avoid the emergence of false positive and false negative results; these controls also ensured experimental accuracy.
In this study, we found that the frequency of HLA-DRB1*1501 decreased among Han patients with ICC compared with Hans in the control group. Similar tendencies were observed in the HLA-DRB1*1501-DQB1*0602 haplotype, consistent with the works of Wu [16] and Hildesheim [31] who studied Han patients with cervical cancer and American patients with high-grade squamous intraepithelial lesions (HSILs), respectively. The HLA-DRB1*1501 and HLA-DRB1*1501-DQB1*0602 haplotypes may inhibit Han ICC cell antigens presented to CD4+ T cells and decrease the risk of HPV infection and ICC occurrence.
The distribution of HLA-DQB1*0602 noticeably decreased in Uighur ICC patients compared with women in the control group. Similar patterns of HLA-DQB1*0602 among HPV16-positive ICC patients were also observed, which agrees with the work of Ferrera on cervical cancer cases in Mexico [29]. Hint HLA-DQB1*0602 may be involved in protecting Uighur cervical tissues from HPV16 infection and cervical cancer occurrence.
A limitation of this study is the lack of epidemiological information, such as smoking status, age at first intercourse, birth control use, and frequency of contraceptive use. Data on these factors may help assess the interaction between high-risk HPV infection and other environmental factors.
Acknowledgements
This work was supported by The Ministry of Science and Technology of China (Grant Nos. 2012AA02A503, 2009BAI82B03 and 2010DFB34100), The National Natural Science Foundation (Grant Nos. 81460363, 81160301 and 81260301), and Shihezi University Science and Technology Research Foundation (Grant No. 2012ZRKXYQYD32).
Disclosure of conflict of interest
None.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Yang BH, Bray FI, Parkin DM, Sellors JW, Zhang ZF. Cervical cancer as a priority for prevention in different world regions: an evaluation using years of life lost. Int J Cancer. 2004;109:418–24. doi: 10.1002/ijc.11719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang SQ, Wang T, Tu SG, Zhou JL, Mairemu ST, Xu X, Hanrini SH, Ruxian GL, Shalai MT, Aimure H, Deng XH. Epideunidogical investigation and analysis of cervical carcinoma in Cele county of XinJiang. Chinese Journal of Practical Gynecology and Obstetrics. 2006;20:379–81. [Google Scholar]
- 4.Chen WB, H X, Huang M. Cervical cancer screening analysis to 8505 cases of married women. Journal of Xinjiang Medical University. 2001;24:252–3. [Google Scholar]
- 5.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 6.zur Hausen H. Papillomavirus infections--a major cause of human cancers. Biochim Biophys Acta. 1996;1288:F55–78. doi: 10.1016/0304-419x(96)00020-0. [DOI] [PubMed] [Google Scholar]
- 7.Mota F, Rayment N, Chong S, Singer A, Chain B. The antigen-presenting environment in normal and human papillomavirus (HPV)-related premalignant cervical epithelium. Clin Exp Immunol. 1999;116:33–40. doi: 10.1046/j.1365-2249.1999.00826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breitburd F, Ramoz N, Salmon J, Orth G. HLA control in the progression of human papillomavirus infections. Semin Cancer Biol. 1996;7:359–71. doi: 10.1006/scbi.1996.0045. [DOI] [PubMed] [Google Scholar]
- 9.Clerici M, Merola M, Ferrario E, Trabattoni D, Villa ML, Stefanon B, Venzon DJ, Shearer GM, De Palo G, Clerici E. Cytokine production patterns in cervical intraepithelial neoplasia: association with human papillomavirus infection. J Natl Cancer Inst. 1997;89:245–50. doi: 10.1093/jnci/89.3.245. [DOI] [PubMed] [Google Scholar]
- 10.Hildesheim A, Schiffman MH, Tsukui T, Swanson CA, Lucci J 3rd, Scott DR, Glass AG, Rush BB, Lorincz AT, Corrigan A, Burk RD, Helgesen K, Houghten RA, Sherman ME, Kurman RJ, Berzofsky JA, Kramer TR. Immune activation in cervical neoplasia: cross-sectional association between plasma soluble interleukin 2 receptor levels and disease. Cancer Epidemiol Biomarkers Prev. 1997;6:807–13. [PubMed] [Google Scholar]
- 11.El-Chennawi FA, Auf FA, Metwally SS, Mosaad YM, El-Wahab MA, Tawhid ZE. HLA-class II alleles in Egyptian patients with hepatocellular carcinoma. Immunol Invest. 2008;37:661–74. doi: 10.1080/08820130802111605. [DOI] [PubMed] [Google Scholar]
- 12.Chan PK, Cheung JL, Cheung TH, Lin CK, Siu SS, Yu MM, Tang JW, Lo KW, Yim SF, Wong YF, To KF, Ng HK, Chung TK. HLA-DQB1 polymorphisms and risk for cervical cancer: a case-control study in a southern Chinese population. Gynecol Oncol. 2007;105:736–41. doi: 10.1016/j.ygyno.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 13.de Araujo Souza PS, Maciag PC, Ribeiro KB, Petzl-Erler ML, Franco EL, Villa LL. Interaction between polymorphisms of the human leukocyte antigen and HPV-16 variants on the risk of invasive cervical cancer. BMC Cancer. 2008;8:246. doi: 10.1186/1471-2407-8-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engelmark M, Beskow A, Magnusson J, Erlich H, Gyllensten U. Affected sib-pair analysis of the contribution of HLA class I and class II loci to development of cervical cancer. Hum Mol Genet. 2004;13:1951–8. doi: 10.1093/hmg/ddh201. [DOI] [PubMed] [Google Scholar]
- 15.Kohaar I, Hussain S, Thakur N, Tiwari P, Nasare V, Batra S, Singh V, Bhambani S, Das BC, Sarkar DP, Bharadwaj M. Association between human leukocyte antigen class II alleles and human papillomavirus-mediated cervical cancer in Indian women. Hum Immunol. 2009;70:222–9. doi: 10.1016/j.humimm.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Wu Y, Liu B, Lin W, Xu Y, Li L, Zhang Y, Chen S, Lin Z, Xu A. Human leukocyte antigen class II alleles and risk of cervical cancer in China. Hum Immunol. 2007;68:192–200. doi: 10.1016/j.humimm.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Shi SR, Cote RJ, Wu L, Liu C, Datar R, Shi Y, Liu D, Lim H, Taylor CR. DNA extraction from archival formalin-fixed, paraffin-embedded tissue sections based on the antigen retrieval principle: heating under the influence of pH. J Histochem Cytochem. 2002;50:1005–11. doi: 10.1177/002215540205000802. [DOI] [PubMed] [Google Scholar]
- 18.Kailash U, Hedau S, Gopalkrishna V, Katiyar S, Das BC. A simple ‘paper smear’ method for dry collection, transport and storage of cervical cytological specimens for rapid screening of HPV infection by PCR. J Med Microbiol. 2002;51:606–10. doi: 10.1099/0022-1317-51-7-606. [DOI] [PubMed] [Google Scholar]
- 19.Olerup O, Aldener A, Fogdell A. HLA-DQB1 and -DQA1 typing by PCR amplification with sequence- specific primers (PCR-SSP) in 2 hours. Tissue Antigens. 1993;41:119–34. doi: 10.1111/j.1399-0039.1993.tb01991.x. [DOI] [PubMed] [Google Scholar]
- 20.Olerup O, Zetterquist H. HLA-DR typing by PCR amplification with sequence-specific primers (PCR-SSP) in 2 hours: an alternative to serological DR typing in clinical practice including donor-recipient matching in cadaveric transplantation. Tissue Antigens. 1992;39:225–35. doi: 10.1111/j.1399-0039.1992.tb01940.x. [DOI] [PubMed] [Google Scholar]
- 21.Zheng XZ, Yang AQ, Pan XL, Zheng LL, Zhou QY, Li XM, Wang XL, Yan LH, Li HA. [Relationship between p53 Arg72Pro polymorphism and cervical carcinoma in Uigur and Han women in Xinjiang] . Zhonghua Bing Li Xue Za Zhi. 2007;36:511–5. [PubMed] [Google Scholar]
- 22.Madeleine MM, Johnson LG, Smith AG, Hansen JA, Nisperos BB, Li S, Zhao LP, Daling JR, Schwartz SM, Galloway DA. Comprehensive analysis of HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1 loci and squamous cell cervical cancer risk. Cancer Res. 2008;68:3532–9. doi: 10.1158/0008-5472.CAN-07-6471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahmud SM, Robinson K, Richardson H, Tellier PP, Ferenczy AS, Roger M, Coutlee F, Franco EL. HLA polymorphisms and cervical human Papillomavirus infection in a cohort of Montreal University students. J Infect Dis. 2007;196:82–90. doi: 10.1086/518612. [DOI] [PubMed] [Google Scholar]
- 24.Hu J, Li L, Pang L, Chen Y, Yang L, Liu C, Zhao J, Chang B, Qi Y, Liang W, Li F. HLA-DRB1*1501 and HLA-DQB1*0301 alleles are positively associated with HPV16 infection-related Kazakh esophageal squamous cell carcinoma in Xinjiang China. Cancer Immunol Immunother. 2012;61:2135–41. doi: 10.1007/s00262-012-1281-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zehbe I, Hohn H, Pilch H, Neukirch C, Freitag K, Maeurer MJ. Differential MHC class II component expression in HPV-positive cervical cancer cells: implication for immune surveillance. Int J Cancer. 2005;117:807–15. doi: 10.1002/ijc.21226. [DOI] [PubMed] [Google Scholar]
- 26.Beskow AH, Josefsson AM, Gyllensten UB. HLA class II alleles associated with infection by HPV16 in cervical cancer in situ. Int J Cancer. 2001;93:817–22. doi: 10.1002/ijc.1412. [DOI] [PubMed] [Google Scholar]
- 27.Cuzick J, Terry G, Ho L, Monaghan J, Lopes A, Clarkson P, Duncan I. Association between high-risk HPV types, HLA DRB1* and DQB1* alleles and cervical cancer in British women. Br J Cancer. 2000;82:1348–52. doi: 10.1054/bjoc.1999.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu Y, Chen Y, Li L, Cao Y, Liu Z, Liu B, Du Z, Zhang Y, Chen S, Lin Z, Xu A. Polymorphic amino acids at codons 9 and 37 of HLA-DQB1 alleles may confer susceptibility to cervical cancer among Chinese women. Int J Cancer. 2006;118:3006–11. doi: 10.1002/ijc.21746. [DOI] [PubMed] [Google Scholar]
- 29.Maciag PC, Schlecht NF, Souza PS, Franco EL, Villa LL, Petzl-Erler ML. Major histocompatibility complex class II polymorphisms and risk of cervical cancer and human papillomavirus infection in Brazilian women. Cancer Epidemiol Biomarkers Prev. 2000;9:1183–91. [PubMed] [Google Scholar]
- 30.Ferrera A, Olivo A, Alaez C, Melchers WJ, Gorodezky C. HLA DOA1 and DOB1 loci in Honduran women with cervical dysplasia and invasive cervical carcinoma and their relationship to human papillomavirus infection. Hum Biol. 1999;71:367–79. [PubMed] [Google Scholar]
- 31.Hildesheim A, Schiffman M, Scott DR, Marti D, Kissner T, Sherman ME, Glass AG, Manos MM, Lorincz AT, Kurman RJ, Buckland J, Rush BB, Carrington M. Human leukocyte antigen class I/II alleles and development of human papillomavirus-related cervical neoplasia: results from a case-control study conducted in the United States. Cancer Epidemiol Biomarkers Prev. 1998;7:1035–41. [PubMed] [Google Scholar]


