Abstract
Introduction
In contrast to right colectomy, closure of the mesocolic gap after laparoscopic left colectomy is not practiced, and reports of small gut herniation through this gap are scarce.
Presentation of case
A 73 year old male was admitted as an emergency with symptoms and clinical signs, suggesting obstruction of the small bowel. Abdominal imaging, including computed tomography confirmed the diagnosis. The patient had undergone laparoscopic left colectomy for cancer, three years ago. At laparotomy small bowel loops were found to herniate through the mesocolic defect at the level of the colonic anastomosis. The small bowel loops were reduced and their viability was ascertained. Because of an iatrogenic perforation of the colon at the anastomosis during small bowel loops mobilization, the colon was temporarily exteriorized in the form of a double barrel colostomy. The postoperative course was uneventful.
Discussion
Very few cases have been reported in the liteature indicating the need of sutuing the mesenterium. Despite the limited numbe of the reported cases, there is clearly a risk of intenal hernia after laparoscopic left colectomy.
Conclusion
Although rare internal hernia after laparoscopic left colectomy may occur, and this brings forward the question of mesocolic gap closure.
Keywords: Internal hernia, Mesocolic hernia, Laparoscopy, Laparoscopic colectomy, Left colectomy
1. Introduction
Laparoscopic colorectal surgery for the treatment of both benign and malignant pathology of the colon is gaining increased acceptance. The laparoscopic approach offers a faster recovery, with less morbidity and use of narcotic analgesics as compared to the open approach. In addition, long-term oncological results after laparoscopy for colorectal cancer are at least equivalent to conventional surgery.1–7
Immediate postoperative local complications, such as bleeding, anastomotic leak, and wound infection, have been reported after either approach in similar rates.5–7 However, herniation of small bowel loops through the mesocolic gap after laparoscopic colectomy is rarely reported.8–12 We herein present a case with late manifestation of small bowel obstruction (SBO) as a result of jejunal loops herniation through the mesenteric gap of a left colectomy.
2. Case report
A 73 year old male was admitted as an emergency in our department with symptoms and clinical signs suggesting SBO. The patient had undergone laparoscopic left colectomy for cancer of the descending colon, three years before. Abdominal imaging, including computed tomography with i.v. and per-os contrast, confirmed the diagnosis of obstruction of the mid-jejunum, without revealing any possible cause. After a 24-h period of clinical observation and conservative treatment, the patient underwent an exploratory laparatomy. The findings consisted of strangulated jejunal loops herniated through the mesocolic defect at the level of the colo-colonic anastomosis. Viability of the small bowel was ascertained and an intestinal resection was not considered necessary. An iatrogenic perforation of the colon at the level of the anastomosis during mobilization of the small bowel loops necessitated the exteriorization of the anastomosis in the form of a double barrel colostomy. The postoperative course was uneventful, and the patient was discharged on the 6th post-operative day Fig. 1.
Fig. 1.
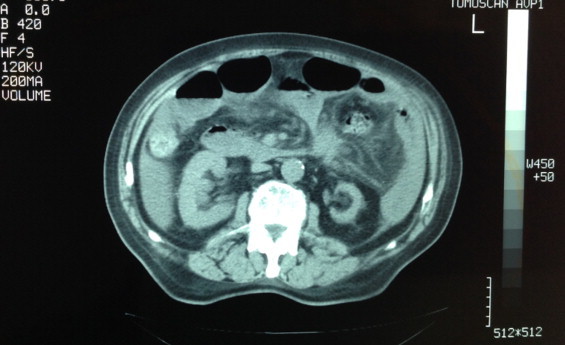
Abdominal CT. Free fluid in the abdominal cavity, turbidity of the mesenteric fat levels, thickening of the small bowel wall, traction of mesenteric helix to suspicious area, and stretching of the bowel central to the pathologic area.
3. Discussion
Internal herniation of jejunal loops through the mesenteric defects has been described as a cause of SBO in rates around 1% after several laparoscopic procedures, such as gastric by-pass, Nissen fundoplication, nephrectomy, or even cholecystectomy.4,5,8 To avoid this complication, meticulous closure of all mesenteric defects with a continuous non-absorbable suture is recommended. SBO after either laparoscopic or open colectomy has been reported in rates of 2–3, 6%, and is most commonly the result of intraperitoneal adhesions formation.13,14 At present, something like eleven (11) cases of small bowel obstruction as a result of herniation of intestinal loops through the mesenteric defect after laparoscopic colectomy have been reported.8,15,16 In an effort to assess the incidence of internal herniation after laparoscopic left colectomy in 436 patients over a 5-year period, Trabaldo et al.12 report five (5) cases of SBO as a result of jejunal loop herniation through the left mesocolic gap, one of which succumbed. However, there is no evidence in the literature on the incidence of asymptomatic internal herniae Fig. 2.
Fig. 2.
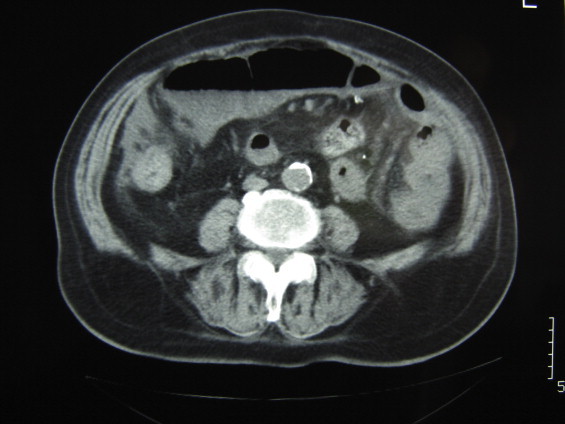
Abdominal CT.
All the aforementioned reported cases were clinically manifested within the first 8 h to 7 days, immediately postoperatively. To our knowledge, the case reported herein is the first in the literature, representing a small bowel herniation through a mesocolic gap after laparoscopic left colectomy, manifested three years postoperatively. Therefore, although extremely rare, one should always suspect the possibility of small bowel loops internal herniation when confronted with a patient presenting with SBO and a past history of laparoscopic colectomy, even years before.
As a result of internal herniation, there are eight (8) SBO cases reported after laparoscopic left colectomy,11,12,15,16 two (2) after laparoscopic transverse colectomy,8,9 and one (1) after laparoscopic right colectomy.10 Most of the authors speculate that the main predisposing factor of internal herniation is a less than 5 cm mesocolic gap that is left behind. Although not supported by any evidence, Trabaldo et al.12 suggest a variety of possible mechanisms to explain internal herniation after laparoscopic left colectomy. These include (i) the reduced formation of adhesions after the laparoscopic approach and thus mobile loops available for herniation, (ii) anatomy of root of small intestine mesentery, leading jejunal loops to fall toward the left ileac fossa, (iii) fixation of the first loop of the jejunum by the Treitz ligament thus predisposing to rotation, (iv) tension or laxity of the left colonic mesentery depending on the degree of the splenic flexure mobilization, and (v) early postoperative mobilization of the patient.
In order to prevent internal herniation of jejuna loops after laparoscopic surgery, closure of the mesenteric defect12,15 and division of the ligament of Treitz12,16 are advocated. However, in the series of Trabaldo et al.12 where five cases of internal herniation and SBO were accounted, obliteration of the mesocolic gap was attempted in two of them. The authors attribute intestinal herniation in these two patients to inadequate closure of the mesocolic defect; they use a tissue sealer (Ligasure™, Valley-lab) in the former and applied endo-clips in the latter case. The authors support the complete closure of the mesocolic gap with a continuous non-absorbable suture. In their study, Cabot et al.18 presented the long-term consequences of not closing the mesenteric defect after laparoscopic right colectomy. In total, 530 patients were studied within a median follow-up period of 20 months and four of them presented with complications attributed to the mesenteric defect: two had small bowel obstruction due to internal herniation and two had torsion of the anastomosis through the defect. The authors concluded that the data they present do not support routinely closing the mesenteric defect after laparoscopic right colectomy for neoplasia while additional studies with extended long-term follow up are needed. Recently in 2013, Masubuchi et al.17 presented an interesting case of an internal hernia projecting through a mesenteric defect following laparoscopic-assisted partial resection of the transverse colon to the lesser omental cleft. They conclude that there is no need to close the mesenteric defect while further research is required to identify the patients who would benefit from closure of the mesenteric defects during laparoscopic-assisted partial colectomy. According to their basic policy, they asses mesenteric defects during the final stages of surgery, and in cases when small intestine has passed into the space, they perform reintegration of the escaped small intestine and fill the space with the greater omentum. In cases of thin patients, it may therefore benefit to close mesenteric defects laparoscopically.
At laparoscopic left colectomy, practicing as in open surgery, the vast majority of surgeons tend to leave the mesenteric defect open, only ensuring lack of mesocolic tension and releasing any jejunal loops from the mesocolic gap. Suture–closure of the mesocolic gap from the ligament of Treitz to the pelvis, in order to prevent a rather very rare complication, seems technically demanding and time consuming at the end of tiresome procedure, while its efficacy is questionable.
4. Conclusion
Despite the limited number of reports, there is clearly a risk of internal hernia after laparoscopic left colectomy. Symptoms are non-specific and range between mild abdominal discomfort and SBO necessitating an emergency operation. SBO is most commonly manifested in the immediate postoperative period, but it may appear as much as 3 years after surgery. Because of the possible adverse outcome associated with this complication, closure of the mesocolic defect is justified.
Conflict of interest
The author(s) declare that they have no competing interests.
Funding
-
•
For this study, we have received NO reimbursements, fees, funding, or salary from an organization that may in any way gain or lose financially from the publication of this manuscript, either now or in the future.
-
•
We hold NO stocks or shares in an organization that may in any way gain or lose financially from the publication of this manuscript, either now or in the future.
-
•
We DO NOT hold any patents relating to the content of the manuscript.
-
•
We have NO other financial competing interests.
-
•
There any NO non-financial competing interests (political, personal, religious, ideological, academic, intellectual, commercial, or any other) to declare in relation to this manuscript.
Ethical approval
Written informed consent was obtained from the patients for publication of these Case reports and any accompanying images/videos.
Author contributions
AD contributed in the collection of the data, creation and design of the manuscript, GK contributed in the collection of the data and design of the manuscript SX contributed in the collection of the data and design of the manuscript, EA participated in the design and coordination and helped to draft the manuscript, GC reviewed the manuscript and was the operating surgeon. All authors read and approved the final manuscript.
Consent
Written informed consent was obtained from the patients for publication of these case reports and any accompanying images/videos. A copy of the written consents is available for review by the editor of this journal.
Key learning points
-
•
Laparoscopic colorectal surgery for the treatment of both benign and malignant pathology of the colon is gaining increased acceptance.
-
•
Immediate postoperative local complications are not that rare However, herniation of small bowel loops through the mesocolic gap after laparoscopic colectomy is rarely reported.
-
•
Symptoms are non-specific and range between mild abdominal discomfort and small bowel obstruction necessitating an emergency operation.
-
•
Because of the possible adverse outcome associated with this complication, closure of the mesocolic defect is justified.
References
- 1.Leung K.L., Kwok S.P., Lam S.C., Lee J.F., Yiu R.Y., Ng S.S. Laparoscopic resection of rectosigmoid carcinoma prospective randomized trial. Lancet. 2004;363:1187–1192. doi: 10.1016/S0140-6736(04)15947-3. [DOI] [PubMed] [Google Scholar]
- 2.Veldkamp R., Kuhry E., Hop W.C., Jeekel J., Kazemier G., Bonjer H.J. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 3.Clinical Outcomes of Surgical Therapy Study Group A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 4.Guillou P.J., Quirke P., Thorpe H., Walker J., Jayne D.G., Smith A.M. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicenter, randomized controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 5.Bonjer H.J., Hop W.C., Nelson H., Sargent D.J., Lacy A.M., Castells A. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298–303. doi: 10.1001/archsurg.142.3.298. [DOI] [PubMed] [Google Scholar]
- 6.Kuhry E., Schwenk W., Gaupset R., Romild U., Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34:498–504. doi: 10.1016/j.ctrv.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Schwenk W., Haase O., Neudecker J., Muller J.M. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;3:CD003145. doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagata K., Tanaka J.I., Endo S., Tatsukawa K., Hidaka E., Kudo S.E. Internal hernia through the mesenteric opening after laparoscopy-assisted transverse colectomy. Surg Laparosc Endosc Percutan Tech. 2005;15:177–179. doi: 10.1097/01.sle.0000166969.38972.fa. [DOI] [PubMed] [Google Scholar]
- 9.Hosono S., Ohtani H., Arimoto Y., Kanamyia Y. Internal hernia with strangulation through a mesenteric defect after laparoscopy-assisted transverse colectomy: report of a case. Surg Today. 2007;37:330–334. doi: 10.1007/s00595-006-3405-4. [DOI] [PubMed] [Google Scholar]
- 10.Jimi S.I., Hotokezaka M., Eto T.A., Hidaka H., Maehara N., Matsumoto K. Internal herniation through the mesenteric opening after laparoscopy-assisted right colectomy: report of a case. Surg Laparosc Endosc Percutan Tech. 2007;17:339–341. doi: 10.1097/SLE.0b013e31806bf493. [DOI] [PubMed] [Google Scholar]
- 11.Kawamura Y.J., Sunami E., Masaki T., Muto T. Transmesenteric hernia after laparoscopic-assisted sigmoid colectomy. J Soc Laparosc Surg. 1999;3:79–81. [PMC free article] [PubMed] [Google Scholar]
- 12.Trabaldo S.S., Anvari M., Leroy J., Marescaux J. Prevalence of internal hernias after laparoscopic colonic surgery. J Gastrointest Surg. 2009;13:1107–1110. doi: 10.1007/s11605-009-0851-5. [DOI] [PubMed] [Google Scholar]
- 13.Duepree H.J., Senagore A., Delaney C.P., Fazio V.W. Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? Laparoscopy versus laparotomy. J Am Coll Surg. 2003;197:177–181. doi: 10.1016/S1072-7515(03)00232-1. [DOI] [PubMed] [Google Scholar]
- 14.Rayan M.D., Wattchow D., Walker M., Hakendorf P. Adhesional small bowel obstruction after colorectal surgery. ANZ J Surg. 2004;74:1010–1012. doi: 10.1111/j.1445-1433.2004.03225.x. [DOI] [PubMed] [Google Scholar]
- 15.Elio A., Veronese E., Frigo F., Residori C., Salvato S., Orcalli F. Ileal volvulus on internal hernia following left laparoscopic-assisted hemicolectomy. Surg Laparosc Endosc. 1998;8:477–478. [PubMed] [Google Scholar]
- 16.Blane P., Delacoste F., Atgar J. A rare cause of intestinal obstruction after laparoscopic colectomy. Ann Chir. 2003;128:619–621. doi: 10.1016/j.anchir.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Masubuchi S., Okuda J., Takanaka K., Kondo K., Asai K., Kayano H. An internal hernia projecting through a mesenteric defect following laparoscopic-assisted partial resection of the transverse colon to the lesser omental cleft: report of a case. Surg Today. 2013;43:814–817. doi: 10.1007/s00595-012-0264-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cabot J.C., Lee S.A., Yoo J., Nasar A., Whelan R.L., Feingold D.L. Long-term consequences of not closing the mesenteric defect after laparoscopic right colectomy. Dis Colon Rectum. 2010;53(3):289–292. doi: 10.1007/DCR.0b013e3181c75f48. [DOI] [PubMed] [Google Scholar]


