Highlights
-
•
Insufficiency fractures due to antiepileptic drug use is one of the rare cause.
-
•
Insufficiency fractures should be kept in mind for joint and bone pain with a history of long term anti-epileptic drug use.
-
•
Carbamazepine could be a result of insufficiency fracture.
Keywords: Bilateral femoral neck fracture, Insufficiency fractures, Carbamazepine, Antiepileptic drug, Dynamic hip screw
Abstract
Introduction
Bilateral femoral neck fractures without major trauma are rare and related to several conditions. Insufficiency fractures due to the use of anti-epileptic drug are one of the rare causes. This case study is about bilateral femoral neck insufficiency fractures resulting from chronic use of anti-epileptic drug.
Presentation of case
A 26-year-old woman was referred to our emergency department with a complaint of bilateral groin pain and a 12-year history of irregular carbamazepine use. The diagnosis was bilateral femoral neck insufficiency fractures due to irregular long-term carbamazepine use. One-stage bilateral dynamic hip screw osteosynthesis was performed. After 2 years of follow up, good result was obtained.
Discussion
There are several risk factors for insufficiency fracture, and antiepileptic drug related osteoporosis is one of the reason. These drugs have negative effect on bone methabolism and bone mineral density.
Conclusion
To our knowledge, this is the first case in the literature of bilateral femoral neck insufficiency fracture due to chronic carbamazepine use. Joint and bone pain with a history of long-term use of anti-epileptic drug should be investigated carefully, and insufficiency fractures should be kept in mind.
1. Introduction
Several adverse effects of long-term use of anti-epileptic drug (AED) on bone metabolism have been reported [1–3]. The most common bone metabolism disorders due to AED use are osteoporosis and rickets.
The exact mechanism of the effect of AEDs on bone metabolism is unclear. Vitamin D deficiency may occur with enzyme-inducing AEDs. It has been suggested that inducing the cytochrome p450 enzyme system is associated with vitamin D deficiency because enzyme induction may lead to increased catabolism of vitamin D [4]. Non-enzyme-inducing AEDs have no effect on vitamin D metabolism [5]. It is also reported that direct inhibitor effect on osteoblast proliferation, decreased calcium absorption, and endocrinopathy are the other suggested mechanisms [6].
There are studies about increased fracture risk with AED use. Although these fractures mostly occur during seizures, nontraumatic fractures can be seen [7,8].
In this paper, we present a case of nontraumatic bilateral collum femoris fracture due to chronic carbamazepine use, treated by bilateral dynamic hip screw. To our knowledge, there is no report yet of bilateral femoral neck insufficiency fracture due to carbamazepine use, until now.
2. Presentation of case
A 26-year-old woman was referred to our emergency department with a complaint of ongoing bilateral groin pain for 3 months and with difficulty in walking. Her pain was aggravated by weight bearing and so she was unable to walk.
On examination, both active and passive motions were painful but she had normal range of motion in both hips. Her pain was increased with axial loading to her lower extremities.
In her personal history, it was learned that she was using carbamazepine irregularly for 12 years due to epilepsy, and she did not attempt her neurological controls for a long time. She had her last seizure 6 months ago, and she did not have any complaint just after the seizure; she also had no recent trauma history. Moreover, she does not have smoking history, and she did not use a medication except carbamazepine as well.
Anteroposterior view of both hips was taken and a fracture line on the left femoral neck and an uncertain fracture on right femoral neck was seen (Fig. 1).
Fig. 1.

Anteroposterior view of both hips.
Whereon, computerized tomography (CT) and magnetic resonance imaging (MRI) of both hips were taken. In coronal CT images, fracture lines were seen in the inferomedial border of both femoral necks (Fig. 2). In T2 weighted images, edema and fracture line were seen in the left femoral neck, and a fracture line was seen in the inferomedial border of the right femoral neck (Fig. 3).
Fig. 2.
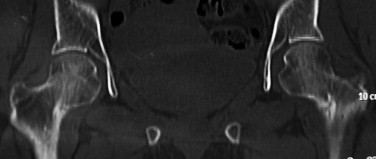
Coronal CT view of both hips.
Fig. 3.
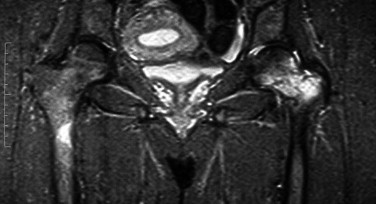
T2 weighted coronal images of both hips.
Bone mineral density of the femoral neck was measured by dual-energy X-ray absorptiometry (DEXA) using a densitometer, and the T score of both hips was −3.
Surgery was done using regional anesthesia with the patient on supine position, and one-stage bilateral dynamic hip screw osteosynthesis was performed.
Osteoporosis therapy was started immediately after surgery. Weight bearing was restricted for 3 months, and after 3 months, she was able to walk without crutches and she had normal range of motions in both hips. After 2 years of follow up, she had no complaint; osteosynthesis was good, and the Harris Hip Score was 96 (Fig. 4).
Fig. 4.

AP view of both hips after 2 years follow-up.
3. Discussion
Fractures resulting from cyclic mechanical stresses can be classified as either fatigue or insufficiency fractures. If the fracture occurs in normal bone of a healthy individual, it is defined as a fatigue fracture. These fractures are common in athletes, dancers, and military personnel [9].
Insufficiency fractures are another type of stress fracture, which is the result of normal stresses on a bone with reduced strength. There are several risk factors for insufficiency fracture and osteoporosis is the most common cause. The other causes for insufficiency fractures are long-term corticosteroid treatment, renal osteodystrophy, amenorrhea, osteomalacia, rheumatoid arthritis, scurvy, fluoride treatment, and pelvic irradiation [10].
Several reports mention unusual causes of insufficiency fractures of femoral neck. Kim et al. reported a patient with a femoral neck insufficiency fracture, who had taken long-time bisphosphonate treatment for osteoporosis [11]. Carpintero et al. reported bilateral insufficiency femoral neck fracture in a male patient with anorexia nervosa [12]. In a pregnant woman, Baki et al. reported a bilateral femoral neck insufficiency fractures due to osteomalacia [13].
It is known that long-term AED usage has several adverse affects on calcium metabolism and bone mineral density. Osteopenia/osteoporosis, osteomalacia, and bone fractures are disorders attributed to the use of these drugs [4,5]. Although hypocalcemia and decreased vitamin D levels are related particularly to children and institutionalized patients with AED usage [14], in mobile and non-institutionalized patients, there is no relation between calcium and vitamin D levels [15]. It was also cited that in young male patients who are taking AEDs, decreased bone density was found without any differences on vitamin D levels [1]. In our case, the patient was active and mobile, and upon analysis of her laboratory tests, calcium and vitamin D levels were normal; however, bone mineral density was decreased.
Simultaneous femoral neck fractures are mostly seen after high-energy trauma; however, they may be associated with repetitive minor trauma, seizure, bone metabolism disorders, and endocrinopathies [16–20], but bilateral collum femoris insufficiency fracture due to AED use is not reported.
The distinctive features of this case include bilateral insufficiency fractures with a strong relation to chronic carbamazepine use and simultaneous surgery of both hips.
4. Conclusion
Joint and bone pain with a history of long-term AED use should be investigated carefully, and insufficiency fractures should be kept in mind. In these conditions, the accurate history of the patient, sufficient imaging, laboratory tests for bone metabolism, and bone mineral density studies must be considered, and adequate treatment should be performed according to the results.
Conflicts of interest
None.
Funding
None.
Ethical approval
None.
Author contribution
KS, corresponding author of the case, did the literature search, manuscript writing, worked in data collection(follow-up data). BG had attended the surgery and also worked in data collecting (follow-up data). OO did the literature search and helped the manuscript writing. FD performed the surgery, made study design and helped in manuscript editing. OY made the initial study design, joined the surgery and made the general supervision of the case report. All authors read and approved the final manuscript.
Consent
This is a statement that the patient had her given informed consent for the case report to be published.
Guarantor
Kerim Sariyilmaz.
Contributor Information
Kerim Sariyilmaz, Email: ksariyilmaz@gmail.com, kerim.sariyilmaz@acibadem.com.tr.
Baris Gulenc, Email: barisgulenc@yahoo.com.
Okan Ozkunt, Email: drdeto@gmail.com.
Fatih Dikici, Email: fatihdikici71@hotmail.com.
References
- 1.Andress D.L. Antiepileptic drug-induced bone loss in young male patients who have seizures. Arch. Neurol. 2002;59(5):781–786. doi: 10.1001/archneur.59.5.781. [DOI] [PubMed] [Google Scholar]
- 2.Farhat G. Effect of antiepileptic drugs on bone density in ambulatory patients. Neurology. 2002;58(9):1348–1353. doi: 10.1212/wnl.58.9.1348. [DOI] [PubMed] [Google Scholar]
- 3.Stephen L.J. Bone density and antiepileptic drugs: a case-controlled study. Seizure. 1999;8(6):339–342. doi: 10.1053/seiz.1999.0301. [DOI] [PubMed] [Google Scholar]
- 4.Pack A.M. Bone mineral density in an outpatient population receiving enzyme-inducing antiepileptic drugs. Epilepsy Behav. 2003;4(2):169–174. doi: 10.1016/s1525-5050(03)00036-2. [DOI] [PubMed] [Google Scholar]
- 5.Kulak C.A. Bone mineral density and serum levels of 25 OH vitamin D in chronic users of antiepileptic drugs. Arq. Neuropsiquiatr. 2004;62(4):940–948. doi: 10.1590/s0004-282x2004000600003. [DOI] [PubMed] [Google Scholar]
- 6.Petty S.J., O'Brien T.J., Wark J.D. Anti-epileptic medication and bone health. Osteoporosis Int. 2007;18(2):129–142. doi: 10.1007/s00198-006-0185-z. [DOI] [PubMed] [Google Scholar]
- 7.Shiek Ahmad B. Falls and fractures in patients chronically treated with antiepileptic drugs. Neurology. 2012;79(2):145–151. doi: 10.1212/WNL.0b013e31825f0466. [DOI] [PubMed] [Google Scholar]
- 8.Jette N. Association of antiepileptic drugs with nontraumatic fractures: a population-based analysis. Arch. Neurol. 2011;68(1):107–112. doi: 10.1001/archneurol.2010.341. [DOI] [PubMed] [Google Scholar]
- 9.Rome K., Handoll H.H., Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst. Rev. 2005;2:CD000450. doi: 10.1002/14651858.CD000450.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egol K.A. Stress fractures of the femoral neck. Clin. Orthop. Relat. Res. 1998;348:72–78. [PubMed] [Google Scholar]
- 11.Kim D.H., Lee E.C., Kang S.K. Insufficiency fracture of ipsilateral femur neck in patient treated with long term bisphosphonate treatment – a case report. J. Bone Metab. 2012;19(2):159–162. doi: 10.11005/jbm.2012.19.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carpintero P. Bilateral insufficiency fracture of the femoral neck in a male patient with anorexia nervosa. Acta Orthop. Belg. 2013;79(1):111–113. [PubMed] [Google Scholar]
- 13.Baki M.E. Bilateral femoral neck insufficiency fractures in pregnancy. Eklem Hastalik Cerrahisi. 2014;25(1):60–62. doi: 10.5606/ehc.2014.13. [DOI] [PubMed] [Google Scholar]
- 14.Fischer M.H. Bone status in nonambulant: epileptic, institutionalized youth: improvement with vitamin D therapy. Clin. Pediatr. (Phila.) 1988;27(10):499–505. doi: 10.1177/000992288802701007. [DOI] [PubMed] [Google Scholar]
- 15.Weinstein R.S. Decreased serum ionized calcium and normal vitamin D metabolite levels with anticonvulsant drug treatment. J. Clin. Endocrinol. Metab. 1984;58(6):1003–1009. doi: 10.1210/jcem-58-6-1003. [DOI] [PubMed] [Google Scholar]
- 16.Schroder J., Marti R.K. Simultaneous bilateral femoral neck fractures: case report. Swiss Surg. 2001;7(5):222–224. doi: 10.1024/1023-9332.7.5.222. [DOI] [PubMed] [Google Scholar]
- 17.Hootkani A., Moradi A., Vahedi E. Neglected simultaneous bilateral femoral neck fractures secondary to narcotic drug abuse treated by bilateral one-staged hemiarthroplasty: a case report. J. Orthop. Surg. Res. 2010;5:41. doi: 10.1186/1749-799X-5-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahman M.M., Awada A. Bilateral simultaneous hip fractures secondary to an epileptic seizure. Saudi Med. J. 2003;24(11):1261–1263. [PubMed] [Google Scholar]
- 19.Chadha M. Spontaneous bilateral displaced femoral neck fractures in nutritional osteomalacia – a case report. Acta Orthop. Scand. 2001;72(1):94–96. doi: 10.1080/000164701753606770. [DOI] [PubMed] [Google Scholar]
- 20.Chen C.E., Kao C.L., Wang C.J. Bilateral pathological femoral neck fractures secondary to ectopic parathyroid adenoma. Arch. Orthop. Trauma Surg. 1998;118(3):164–166. doi: 10.1007/s004020050339. [DOI] [PubMed] [Google Scholar]


