Abstract
Objectives
We determined the radiographic osteoarthritic worsening rate prior to knee arthroplasty (TKA) and whether this worsening was associated with worsening pain and function as compared to a non-surgical matched sample.
Methods
We used the Osteoarthritis Initiative 5-year datasets. Extent of knee OA two years prior to TKA was matched to knees of persons who did not undergo TKA. WOMAC Function and KOOS Pain scales were used to quantify functional deficit and functionally relevant pain respectively. A total of 167 persons with isolated TKA and 300 persons with matched symptomatic knee OA but no TKA were studied.
Results
During the two years prior to TKA, worsening by at least one Kellgren and Lawrence (KL) grade occurred in 27.4% (95% CI = 20.6 to 34.2) of the surgical knees compared to 6.6% (95% CI = 3.8 to 9.4) of matched non-surgical knees. Osteoarthritis radiographic progression was strongly associated with WOMAC Function and KOOS Pain worsening (p<0.001) in the two years prior to TKA. KL worsening was strongly associated with future arthroplasty (Odds ratio = 5.0, 95%CI = 2.6 to 9.8) after adjustment for potential confounders.
Conclusions
Persons undergoing TKA two years later had substantial worsening pain and function over the two-year pre-operative period as compared to a non-surgical sample matched based on KL grades. Almost 30% of persons who elect to undergo TKA undergo rapid disease progression and symptom worsening during the 2 years prior to TKA.
Keywords: knee, osteoarthritis, pain, function, arthroplasty
Introduction
The path toward total knee arthroplasty (TKA) for persons with osteoarthritis is an understudied and relatively poorly understood process. Progression to TKA takes many years for most patients (1) and is influenced by multiple patient and surgeon factors (2). Key factors typically considered when recommending TKA surgery are the extent of knee osteoarthritis, pain severity and functional deficits.
We found no assessment of the rate of pre-operative tibiofemoral OA radiographic progression in a sample of persons eventually undergoing TKA. In addition, we found no research that determined if functional or pain related worsening was associated with knee radiographic worsening in a cohort that eventually underwent TKA. Our prior work defined the trajectories of pain and functional status measures in the years leading to TKA (1) but did not address the extent of knee OA, a key factor guiding surgical decisions. Data describing the rate of knee radiographic progression and the potential pain and functional correlates of this progression may assist in identifying patients who are particularly vulnerable to co-occurring radiographic progression, functional loss and pain worsening. Close monitoring of pain, functional loss and radiographic progression may facilitate intervening before a patient’s knee OA status, pain or function has worsened to levels typically expected in patients who undergo TKA. Monitoring and aggressive treatment may help to either delay or prevent TKA surgery or better prepare patients for TKA recovery.
White and colleagues found that persons with worsening knee OA over a 30 month period were at 2.2 times higher risk of developing severe functional loss as compared to persons with no knee radiographic worsening (3). Wesseling and colleagues reported worsening function and pain in persons with knee OA over a 4-year period but only for those whose Kellgren and Lawrence (KL) grades increased by 2 or more scale points (4). No studies were found that examined associations between knee radiographic worsening and worsening pain and function in persons who eventually underwent TKA. Systematic review evidence suggests approximately 4% of osteoarthritic knees worsen by at least one KL grade each year (5) but we found no evidence of preoperative worsening rates for persons who eventually undergo TKA. Given that persons who undergo TKA demonstrate substantial worsening pain and function in the 2 years prior to TKA (1), we suspected the rate of radiographic worsening would be greater as compared to a comparable non-surgical sample with symptomatic knee OA.
Consequently, our primary purpose was to determine the rate of radiographic progression of tibiofemoral osteoarthritis during the 2 years prior to TKA surgery for surgical knees and the pain-related and functional changes associated with radiographic worsening during this critical period. Our secondary purpose was to compare the rate of radiographic progression in our TKA sample to persons with similar ratings of symptomatic knee OA who did not undergo TKA over the study period.
Methods
The Osteoarthritis Initiative (OAI) is an NIH and privately funded natural history multicenter prospective 5-year longitudinal study of persons with or at high risk for knee OA. Two primary subcohorts were studied in the OAI. The progression cohort comprised persons with symptomatic knee OA while the incidence cohort included persons with or at risk for knee OA. The study was approved by the Institutional Review Boards of each site. Subjects were recruited in similar proportions from: (1) the University of Maryland in Baltimore, Maryland, (2) the Ohio State University in Columbus, Ohio, (3) the University of Pittsburgh in Pittsburgh, Pennsylvania, and (4) Memorial Hospital of Rhode Island, in Pawtucket, Rhode Island.
Of 17,457 persons screened, 4,796 were enrolled in OAI. Inclusion criteria included men and women ages 45 to 79 years with, or at risk for, symptomatic tibiofemoral OA. All ethnic minorities were included. More common exclusion criteria were magnetic resonance imaging height and weight limitations (n=2,328), recruitment thresholds for age and gender (n=2,954) and dropouts between the telephone screen and the enrollment visit (n=4,381). The reader is referred to the OAI website for more detailed information (https://oai.epi-ucsf.org/datarelease/default.asp).
Data from n=167 persons (75% from progression cohort and 25% from the incidence cohort) who underwent isolated unilateral TKA surgery over the 5-year study period were included. We excluded persons (n=10) who underwent unicompartmental knee replacement surgery and persons (n=39) who underwent bilateral TKR or hip replacement surgery during the course of study because these persons may have a different trajectory of preoperative worsening than persons undergoing a single primary TKA. A total of 19, 30, 35, 39, 44 TKA surgeries were conducted in years 1 through 5, respectively for a total of 167 TKAs. A total of 87 persons had a left-sided TKA while 80 persons had a right-sided TKA.
For the non-surgical control sample, we recruited persons from the progression cohort of the OAI. Because all patients undergoing TKA were symptomatic, we wanted to select a non-surgical sample that also was symptomatic. Persons in the progression cohort were required to have symptomatic knee OA, defined as at least a definite tibiofemoral osteophyte in at least one knee and corresponding knee pain, aching or stiffness on most days in a month during the past year. Of the 1,116 persons in the progression cohort who did not have either hip or knee arthroplasty over the study period, we used a random number generator and frequency matched to the TKA sample using the 2-year pre-operative knee KL scores. We matched using the maximum number of persons possible using the rate limiting group KL =4. This 2-year pre-operative surgical KL matching to the TKA cohort resulted in the selection of 135 non-surgical subjects with a KL score of 4, 97 with a KL score of 3, 54 with a KL score of 2 and 14 with a KL score of 0 or 1 for a total of 300 subjects in the non-surgical comparison group. The 14 persons classified as having KL grades of 0 or 1 during the radiographic adjudication process were initially screened as having a KL grade of 2 or higher at baseline and were thus included in the progression cohort.
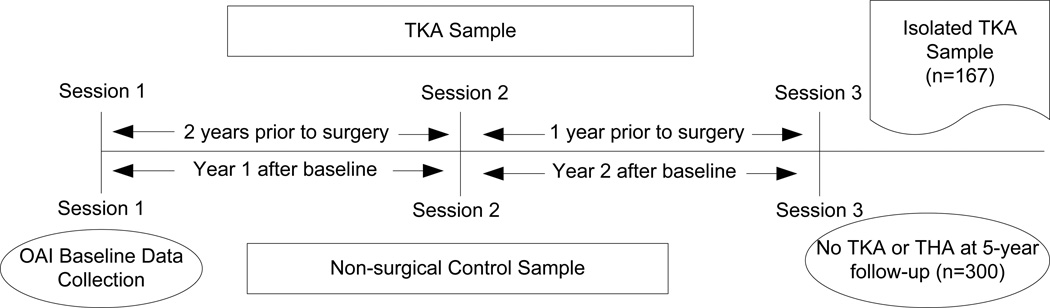
For both samples, we used data from three consecutive yearly data collection sessions (defined for this study as Session 1, Session 2 and Session 3), to examine changes that occurred over two full years. For the TKA sample, Sessions 1 and 2 were used to describe changes that occurred during the second pre-operative year while sessions 2 and 3 described changes during the year prior to TKA. Of note, patients undergoing TKA in year 1 (n= 19) only contributed 1 pre-operative session while persons undergoing surgery in year 2 (n=30) contributed 2 preoperative sessions. The remaining TKA sample (71%) contributed a full complement of pre-operative sessions for analysis. We chose this strategy to take full advantage of data from all isolated unilateral TKAs in the OAI dataset for which radiographic data were available. For the non-surgical sample we also used 3 yearly data collection sessions. Sessions 1 (baseline) and 2 (1-year follow-up) were used to describe changes during the first year while sessions 2 and 3 (2-year follow-up) were used to describe changes during the second year of follow-up. Figure 1 illustrates the timeline for the TKA and non-surgical samples.
Figure 1.
The figure illustrates the temporal sequence and the data collection sessions for the knee arthroplasty sample and the non-surgical control sample.
Radiographic Measures
Radiographs were obtained yearly using a highly standardized approach to position the standing subject’s knees in approximately a 20-degree flexed position and to equally distribute the subject’s body weight (6). More accurate assessment of joint space width is obtained with this approach as compared to knee extended views (6). Technicians at all sites underwent extensive training to enhance consistency.
OAI investigators reported KL grades to quantify the extent of knee arthritis. KL grades were 0 to 4. A grade of 0 was normal, 1 indicated doubtful narrowing of joint space and possible osteophytic lipping, 2 indicated definite osteophytes and possible narrowing of joint space, 3 indicated definite narrowing of joint space and some sclerosis and possible deformity of bone ends, and 4 indicated large osteophytes, marked narrowing of joint space, severe sclerosis and definite deformity of bone ends (7).
We used the radiographic scoring data provided by OAI investigators. An extensive adjudication process was used for KL grades for all knees over all time periods. Two central site readers and a third adjudicator, all either a rheumatologist or a musculoskeletal radiologist with extensive training and experience with KL grading served as radiographic readers. Follow-up films were randomly ordered and then scored while being viewed simultaneously with the baseline film.
Test-retest reliability for the adjudicating readers was substantial to almost perfect (8) with weighted Kappa (Κw) coefficients for both KL grades ranging from 0.70 to 0.80 for repeated independent readings of 300 randomly selected knee films. Missing radiographic data were not imputed and are reported in Table 1. When reporting KL worsening rates, we reported proportions both with KL scores of 4 included and excluded because these knees had already achieved the worst possible score.
Table 1.
Characteristics of the Participants
| TKA Mean (sd) or N(%) (n = 167) |
TKA Missing N |
Non-TKA Mean (sd) or N(%), (n = 300) |
Non-TKA Missing N |
|
|---|---|---|---|---|
| Female Sex | 98 (58.7) | 0 | 160 (51.4), | 0 |
| Age in years * | 64.6 (8.5) | 0 | 63.0 (9.1) | 0 |
| Race | ||||
| Non-white | 28 (16.8) | 90 (29.9) | ||
| Body Mass Index | 29.8 (4.7) | 0 | 30.2 (4.7) | 0 |
| Session 1 KL | 66 | 0 | ||
| Grade+ | ||||
| 0 or 1 | 5 (4.5) | 14 (4.7) | ||
| 2 | 20 (18.0) | 54 (18.0) | ||
| 3 | 36 (32.4) | 97 (32.2) | ||
| 4 | 50 (45) | 135 (45) | ||
| Session 3 KL | 22 | 51 | ||
| Grade + | ||||
| 0 or 1 | 1 (0.7) | 11 (4.4) | ||
| 2 | 12 (8.3) | 40 (16.0) | ||
| 3 | 43 (29.7) | 81 (32.5) | ||
| 4 | 89 (61.4) | 120 (48.2) | ||
| WOMAC | ||||
| Function Score^ | ||||
| Session 1 | 15.2 (10.9) | 56 | 17.5 (12.8) | 3 |
| Session 2 | 18.4 (12.4) | 24 | 15.6 (12.1) | 11 |
| Session 3 | 24.9 (12.9) | 9 | 14.9 (12.1) | 30 |
| KOOS Pain | ||||
| Score^ | ||||
| Session 1 | 69.3 (17.3) | 53 | 65.9 (19.0) | 0 |
| Session 2 | 66.4 (19.0) | 23 | 71.3 (19.1) | 8 |
| Session 3 | 55.8 (18.5) | 6 | 71.2 (20.5) | 26 |
Age in years is reported for the year of surgery.
Values for the surgical sample were taken from yearly visits during the 2 full years prior to knee replacement surgery while the values for the non-surgical sample were taken during baseline, year 1 and year 2 visits. For the immediate pre-surgical visit (Session 3), a total of 22 (13.2%) of the radiographs were missing for the TKA sample.
For the Session #1 KL grades, a total of 17 persons who had TKA 3 or more years after the start of OAI had missing radiographic data 2 full years prior to TKA surgery. A total of 49 patients had TKA surgery during the first two years of OAI data collection. As a result, radiographic data for Session 1 were therefore not available for these persons.
The OAI also obtained yearly WOMAC Function and KOOS Pain scores for both knees of all participants. Both the WOMAC Function and the KOOS Pain scales have been extensively validated (9–12). We chose these two measures because the WOMAC Function Scale, which ranges from 0 to 68 with higher scores equating to worse function, specifically asks patients to rate the extent of difficulty associated with 17 daily activities. The KOOS Pain scale asks patients to rate the severity of pain associated with 9 common activities over the past seven days. The KOOS Pain Scale, ranging from 0 to 100 with higher scores equating to less pain during function, was chosen over the WOMAC Pain Scale because KOOS Pain has 4 additional items which allows for a more comprehensive assessment of the construct. We used the outcome scores for the surgical knees of the TKA patients and the matched non-surgical knees for the control sample.
Data Analysis
Descriptive data for the surgical and non-surgical samples were reported. We used independent t-tests to determine if 2-year KOOS Pain or WOMAC Function change scores were associated with radiographic progression. Surgical and non-surgical samples were examined separately. Missing KL grades for these comparisons were handled in the following way: 1) if a KL score was missing but prior and follow-up KL scores were the same, the missing KL grade also was scored the same. For example, if session 1 was KL = 2 and session 3 was KL=2 but session 2 was missing, the session 2 KL grade of 2 was recorded. 2) If a patient had a KL grade of 4, but had missing follow-up KL score(s), the follow-up session(s) also were scored as 4. WOMAC and KOOS missing values were not imputed. Bonferroni correction was used to interpret p-values for OA/pain and function comparisons such that significant p values were adjusted to p<0.01. Multivariable logistic regression was used to determine if an association exists between our exposure variable of interest (knee OA worsening by at least 1KL grade over the 2-year period) and group (surgical versus non-surgical) after adjustment for potential confounders. We included age, sex, BMI, baseline KOOS Pain, baseline WOMAC Function and race (Caucasian versus other) as potential confounders of the association between knee OA radiographic worsening and group(13). Residuals were checked as were tests for potentially influential observations(14). The Hosmer and Lemeshow goodness of fit was used to assess the final model.
In an a priori power analysis, we determined that a two group t-test with a 0.010 two-sided significance level will have 80% power to detect the difference between a radiographically stable group WOMAC Function mean yearly change of 0.0 points and a radiographic worsening group mean yearly change of 7.0 WOMAC Function points, assuming that the common standard deviation is 8.0, when the sample sizes are 31 in each group. WOMAC Function change and variability estimates were based on our previous work with the OAI(1; 15).
Results
During the two years prior to TKA, a total of 27.4% (95% CI = 20.6 to 34.2) of all surgical knees worsened by at least 1 KL grade. Over this same period, a total of 45.6% (95% CI = 32.7 to 58.5) of knees with KL<4 at baseline had radiographic worsening during the two years prior to surgery. We were unable to measure radiographic worsening for knees with KL grades of 4 due to floor effects of the KL scale. WOMAC Function and KOOS Pain Scores for the TKA sample over the course of study worsened over time and are reported on Table 1. For the non-surgical sample, a total of 6.6% (95% CI = 3.8 to 9.4) of knees worsened by at least 1 KL grade during 2-year period. When considering only knees that had KL<4 at session 1, 11.7% (95% CI = 6.8 to 16.7) of knees worsened. WOMAC Function and KOOS Pain scores for non-surgical knees either stayed approximately the same or improved over the study period. Table 1 summarizes the characteristics of both samples while Table 2 summarizes WOMAC Function and KOOS score changes in relation to radiographic worsening status across the surgical and non-surgical samples.
Table 2.
2-year changes in WOMAC Function and KOOS Pain Scores for the Two Samples
| Surgical Sample | Non-surgical Sample | |||
|---|---|---|---|---|
| KL Worsening Mean (sd) |
No KL Worsening Mean (sd) |
KL Worsening Mean (sd) |
No KL Worsening Mean (sd) |
|
| WOMAC Function | ||||
| Change Scores# | ||||
| Changes from | 18.6 (11.2) | 5.7 (9.2) | −2.4 (13.4) | −2.2 (11.2) |
| Session 1 to 3+ | (n=27) | (n=72) | (n = 13) | (n = 247) |
| KOOS Pain | ||||
| Change Scores* | ||||
| Changes from | −16.7 (14.1) | −5.5 (15.6) | 5.2 (18.4) | 5.0 (17.2) |
| Session 1 to 3+ | (n=28) | (n= 75) | (n = 13) | (n=237) |
WOMAC Function scores range from 0 to 68 with higher scores indicating worse function. Change scores are coded such that positive changes indicate worsening and negative scores indicate improvement in function.
KOOS Pain scores range from 0 to 100 with 100 indicating no pain during functional activities. Change scores are coded such that positive changes indicate improvement and negative scores indicate worsening in pain during functional activities.
p<0.001 for the surgical sample
Associations between radiographic progression and WOMAC Function and KOOS Pain changes
During the two years prior to TKA, the mean difference for KOOS Pain change scores was 11.2 points (95%CI = 4.8 to 17.7) p<0.001 and for WOMAC Function, 12.9 points (95%CI = 8.5 to 17.2) p<0.001 as compared to persons with no radiographic worsening. For both measures, the radiographic worsening group had greater function and pain worsening. Statistical comparisons among those with and without KL worsening among persons in the non-surgical control group indicated no significant differences (p > 0.9) for KOOS or WOMAC change scores. See Table 2 for a summary of WOMAC Function and KOOS Pain change scores in the 2 years prior to TKA.
Yearly rate of radiographic progression in TKA and non-surgical samples
Risk of radiographic progression was substantially greater over the two-year pre-operative period for the TKA sample (Odds ratio = 5.0 (95% CI = 2.6 to 9.8) relative to the non-TKA sample after adjustment for potential confounders. Table 3 summarizes the multivariable logistic regression model. The Hosmer and Lemeshow goodness of fit test was p = 0.11 indicating the model-based probabilities were a reasonable estimation of the actual data-based probabilities(14).
Table 3.
Multivariable Logistic Regression Model of Association Between Group and Progressive Knee OA
| Variable * | Odds | 95% CI for OR | |
|---|---|---|---|
| Ratio | Lower | Upper | |
| Sex (female) | 1.3 | 0.8 | 2.1 |
| Race (white) | 2.7 | 1.3 | 5.6 |
| Age | 1.0 | 0.98 | 1.03 |
| BMI | 1.0 | 0.93 | 1.04 |
| KOOS Pain | 1.01 | 0.99 | 1.03 |
| WOMAC Function | 1.0 | 0.97 | 1.03 |
| OA worsening (yes) | 5.0 | 2.6 | 9.8 |
| Constant | |||
For dichotomous variables, the group of interest is in parentheses. For sex, male is the reference group, for race, non-white persons is the reference group, and for OA worsening, unchanged radiographic OA is the reference group.
Discussion
We examined associations between radiographic worsening and corresponding worsening in pain and function in the two years prior to TKA. We also determined whether the rate of radiographic worsening prior to TKA was significantly higher as compared to persons with similar radiographic severity but who did not undergo TKA over the 5-year study period. These issues have not been explored to our knowledge and they are important given that preoperative worsening in pain and functioning is substantial in the 2 years prior to TKA (1).
Several novel findings emerged from our study. We found that persons whose pre-surgical knee radiographic status worsened also had substantial co-occurring worsening pain and function compared to persons with stable KL scores in the two years prior to surgery. The greater worsening in both KOOS Pain and WOMAC Function scores for the group with progressive radiographic OA was substantial and clinically important (16–18). These data suggest that in the two years prior to surgery, a substantial subgroup of patients experience concomitant knee OA and symptomatic worsening. This high rate of radiographic worsening and associated pain and functional status worsening, in our view, likely contributes to surgeons’ recommendations and patients’ decisions to opt for TKA. The extent of symptomatic worsening in our nonsurgical sample for persons with and without KL worsening was essentially no different and in fact, both those with and without KL worsening in the non-surgical group showed very slight improvement in their KOOS and WOMAC scores.
Prior work has shown that KL scores predict TKR (19–21) but we found no prior evidence that examined correlates of yearly knee radiographic worsening in persons prior to undergoing TKA. Roos and colleagues reported greater pain and functional worsening over a 7-year period in persons with prior history of meniscectomy and who had KL grades of 2 or greater at baseline as compared to meniscectomized persons who had no knee OA at baseline(22). However, these patients did not undergo TKA. White and colleagues (3) and Wesseling et al (4) both examined functional and pain correlates of radiographic worsening over a multiyear period but they did not examine persons who underwent TKA. Our data strongly suggest the rate of radiographic worsening is substantially higher for persons who eventually undergo TKA as compared to persons with similar levels of symptomatic knee OA who do not undergo TKA(5).
The point estimates for rates of pre-operative KL worsening in TKA patients were substantially higher than systematic review-based estimates(5) and much higher than matched OAI patients in our study with no TKA. When excluding knees with KL grades of 4, approximately 46% of our TKA sample worsened by at least 1 KL grade during the 2-year preoperative period compared to approximately 12% over a 2-year period in the non-surgical sample. In post-hoc analyses, we used independent sample t-tests to compare WOMAC and KOOS scores for the surgical and non-surgical KL worsening and non-worsening subgroups for knees with KL scores of 3 or less at baseline. For example, WOMAC Function scores for the surgical sample KL worsening subgroup (n=25) increased (became worse) by 18.5 (sd=10.6) points while the KL non-worsening subgroup worsened by 2.3 (sd=9.2) points (p<0.001). Comparisons for the non-surgical samples were similar to that reported in Table 2 as were comparisons of KOOS Pain scores (data not shown). Our post-hoc findings confirmed estimates from the complete samples.
Patients who undergo TKA within the next few years demonstrate a substantially higher rate of KL worsening as compared to non TKA patients and this elevated rate of radiographic progression was, in our opinion, a likely key contributor to the surgical decision. For example, 81% (30 of 37 persons) with KL worsening for the TKA sample resulted in a KL score of 3 or 4 indicating definite or severe tibiofemoral joint space narrowing, a recommended indication for TKA(23).
Substantial symptomatic worsening coupled with KL progression to grade 3 or 4 would likely trigger the need for surgery. Approximately 25% of the sample of persons who underwent TKA in OAI demonstrated this coupled worsening in the two years prior to surgery. This subgroup runs counter to the traditional suggestion that knee OA is a slowly progressive disorder(24). Our data suggest that additional research should more aggressively study the triggers for both symptomatic and KL based progression in persons with mild to moderate symptomatic knee OA. Given that persons in our non-surgical sample who had KL worsening had no symptomatic worsening, these two clinical events were not coupled and there are apparently factors which trigger both KL and symptomatic worsening in a subset of patients. Interventions designed to slow OA progression and symptomatic worsening have potential to reduce TKA related burden. Of currently available approaches, weight loss interventions would appear to have the greatest potential for these combined effects(25).
We found that patients who eventually undergo TKA in the subsequent two years had an adjusted odds of radiographic OA worsening that is on average, 5.0 times higher than a matched non-surgical sample. The only other predictor of surgical status was race. We found that Caucasians were, on average, 2.7 times more likely to undergo TKR than other races. The evidence linking the role of race and knee TKA utilization is substantial and strongly supports the concept that, for example, African Americans underutilize TKA (26; 27). Our findings echo this evidence.
Our study was not designed to make causative inferences regarding the triggers for symptomatic and radiographic worsening but in our view, this area should be studied further. Symptomatic worsening coupled with radiographic worsening in persons who eventually undergo TKA is likely triggered by a combination of physical, psychological or disease-related factors that, to our knowledge, have not been identified. If causes of more rapid progression could be identified, interventions directed toward these mechanisms may have strong potential for preventing this downward spiral of radiographic and symptomatic worsening for these patients.
Our study has some important limitations. The sample of persons who underwent TKA in OAI is relatively small. The low rate of radiographic worsening in the non-surgical sample, while consistent with published evidence (5) also limited our analyses because we don’t know if the non-surgical sample may have had KL worsening in future years at a similar rate to that of the TKA group. The study also had an inadequate sample size to examine yearly changes more than 2 years prior to TKA. In addition, we only used the progression cohort when randomly selecting persons for the matched non-TKA cohort. This approach likely led to a group that had slightly worse pain and function as compared to the TKA group during session 1. While this approach was conservative (i.e. we elected not to recruit persons from the incidence cohort because many were asymptomatic and had no knee OA) we still found substantial differences in KL progression and co-occurring pain and functional worsening among the two groups. Because the OAI was designed primarily for study of the tibiofemoral joint, we had no radiographic data for the patellofemoral joint. While TKA surgery for isolated patellofemoral disease is rare (28), the lack of data describing the extent of patellofemoral disease potentially affects the interpretability of our findings. In addition, the OAI had fairly restrictive inclusion criteria particularly related to BMI and this further reduced the generalizability of the study.
The KL scale demonstrated an important floor effect with 45% of patients in both groups unable to demonstrate worsening during session 1. This floor effect restricted our ability to assess worsening for a substantial number of patients. An alternative measure of OA worsening that does not exhibit substantial floor effects may have allowed for a more comprehensive assessment of OA worsening. Finally, patients who underwent TKA during year 1 (n=19) or year 2 (n=30) had missing data for either or both sessions 1 and 2. Given that our interest was in radiographic worsening over this period, we may have underestimated the proportion of persons who actually have radiographic worsening in the two years prior to TKA.
In conclusion, symptomatic and functional worsening is strongly associated with radiographic knee OA worsening in the two years prior to TKA. These data provide preliminary evidence to suggest a substantial proportion of persons experience progressive radiographic knee OA worsening coupled with overall symptom worsening during the 2 years prior to surgery. Yearly radiographs in those persons with validated patient reported outcome based symptomatic worsening may be helpful to counsel patients on aggressive knee OA treatment. Additional research needs to examine causative factors for this clinically important symptomatic and radiographic worsening to reduce the rapid downward spiral in knee OA severity, pain and function in these patients.
Acknowledgments
Acknowledgements and Funding Statement: The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. The authors of the current manuscript were not funded by OAI, did not collaborate with OAI investigators and received no other funding for the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Support Statement: The authors disclose no financial support or other benefits from commercial sources for the work reported on in the manuscript, or any other financial interests which could create a potential conflict of interest or the appearance of a conflict of interest with regard to the work.
Contributions: DLR and WAJ conceived of and designed the study, DLR acquired and analyzed the data and DLR and WAJ interpreted the data. DLR and WAJ drafted the article and revised it critically for important intellectual content and both DLR and WAJ gave final approval of the version to be submitted.
Conflict of Interest Statement : The authors declare no conflicts of interest.
Contributor Information
Daniel L. Riddle, Departments of Physical Therapy and Orthopaedic Surgery, Virginia Commonwealth University, Richmond, Virginia, USA, 23298
William A. Jiranek, Department of Orthopaedic Surgery, Virginia Commonwealth University, Richmond, Virginia, USA, 23298
Reference List
- 1.Riddle DL, Perera RA, Stratford PW, Jiranek WA, Dumenci L. Progressing toward, and recovering from, knee replacement surgery: a five-year cohort study. Arthritis Rheum. 2013 Dec;65(12):3304–3313. doi: 10.1002/art.38139. [DOI] [PubMed] [Google Scholar]
- 2.Wright JG, Hawker GA, Hudak PL, Croxford R, Glazier RH, Mahomed NN, et al. Variability in physician opinions about the indications for knee arthroplasty. J Arthroplasty. 2011 Jun;26(4):569–575. doi: 10.1016/j.arth.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 3.White DK, Zhang Y, Niu J, Keysor JJ, Nevitt MC, Lewis CE, et al. Do worsening knee radiographs mean greater chances of severe functional limitation? Arthritis Care Res (Hoboken ) 2010 Oct;62(10):1433–1439. doi: 10.1002/acr.20247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wesseling J, Bierma-Zeinstra SM, Kloppenburg M, Meijer R, Bijlsma JW. Worsening of pain and function over 5 years in individuals with 'early' OA is related to structural damage: data from the Osteoarthritis Initiative and CHECK (Cohort Hip & Cohort Knee) study. Ann Rheum Dis. 2013 Nov 15; doi: 10.1136/annrheumdis-2013-203829. [DOI] [PubMed] [Google Scholar]
- 5.Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE, et al. Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthritis Cartilage. 2008 Aug;16(8):873–882. doi: 10.1016/j.joca.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kothari M, Guermazi A, von IG, Miaux Y, Sieffert M, Block JE, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004 Sep;14(9):1568–1573. doi: 10.1007/s00330-004-2312-6. [DOI] [PubMed] [Google Scholar]
- 7.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957 Dec;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–174. [PubMed] [Google Scholar]
- 9.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833–1840. [PubMed] [Google Scholar]
- 10.Bellamy N, Kirwan J, Boers M, Brooks P, Strand V, Tugwell P, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol. 1997 Apr;24(4):799–802. [PubMed] [Google Scholar]
- 11.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS)-validation and 402 comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003 May 25;1(1):17. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003 Nov 3;1(1):64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2008 Aug;34(3):515–529. doi: 10.1016/j.rdc.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: John Wiley & Sons; 2000. [Google Scholar]
- 15.Riddle DL, Kong X, Fitzgerald GK. Psychological health impact on 2-year changes in pain and function in persons with knee pain: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2011 Sep;19(9):1095–1101. doi: 10.1016/j.joca.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monticone M, Ferrante S, Salvaderi S, Motta L, Cerri C. Responsiveness and minimal important changes for the Knee Injury and Osteoarthritis Outcome Score in subjects undergoing rehabilitation after total knee arthroplasty. Am J Phys Med Rehabil. 2013 Oct;92(10):864–870. doi: 10.1097/PHM.0b013e31829f19d8. [DOI] [PubMed] [Google Scholar]
- 17.Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis. 2001 Sep;60(9):834–840. [PMC free article] [PubMed] [Google Scholar]
- 18.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002 Jan;29(1):131–138. [PubMed] [Google Scholar]
- 19.Riddle DL, Jiranek WA, Neff RS, Whitaker D, Hull JR. Extent of Tibiofemoral Osteoarthritis Before Knee Arthroplasty: Multicenter Data from the Osteoarthritis Initiative. Clin Orthop Relat Res. 2012 Apr 2;470(10):2836–2842. doi: 10.1007/s11999-012-2328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim HA, Kim S, Seo YI, Choi HJ, Seong SC, Song YW, et al. The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology (Oxford) 2008 Jan;47(1):88–91. doi: 10.1093/rheumatology/kem308. [DOI] [PubMed] [Google Scholar]
- 21.Conaghan PG, D'Agostino MA, Le BM, Baron G, Schmidely N, Wakefield R, et al. Clinical and ultrasonographic predictors of joint replacement for knee osteoarthritis: results from a large, 3-year, prospective EULAR study. Ann Rheum Dis. 2010 Apr;69(4):644–647. doi: 10.1136/ard.2008.099564. [DOI] [PubMed] [Google Scholar]
- 22.Roos EM, Bremander AB, Englund M, Lohmander LS. Change in self-reported outcomes and objective physical function over 7 years in middle-aged subjects with or at high risk of knee osteoarthritis. Ann Rheum Dis. 2008 Apr;67(4):505–510. doi: 10.1136/ard.2007.074088. [DOI] [PubMed] [Google Scholar]
- 23.NIH Consensus Panel. NIH Consensus Statement on total knee replacement December 8–10, 2003. J Bone Joint Surg Am. 2004 Jun;86-A(6):1328–1335. doi: 10.2106/00004623-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 24.Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–199. doi: 10.1093/bmb/lds038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage. 2013 Sep;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003 Oct 2;349(14):1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 27.Steel N, Clark A, Lang IA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998–2004. J Gerontol A Biol Sci Med Sci. 2008 Jun;63(6):629–634. doi: 10.1093/gerona/63.6.629. [DOI] [PubMed] [Google Scholar]
- 28.Norwegian Arthroplasty Register. Annual Report June 2010. Annual Reports 11 A.D. Jun 16; (2010 Edition) Available from: URL: http://nrlweb.ihelse.net/eng/default.htm.