Abstract
Objective
To compare on a population basis the birth outcomes of women treated with Assisted Reproductive Technologies (ART), women with indicators of subfertility but without ART, and fertile women.
Design
Longitudinal cohort study
Setting
Massachusetts
Participants
334,628 births and fetal deaths to Massachusetts mothers giving birth in a Massachusetts hospital between July 1, 2004-December 31, 2008, subdivided into three subgroups for comparison: ART 11,271, subfertile 6,609, and fertile 316,748.
Intervention
None
Main Outcome Measures
Four outcomes: preterm birth, low birthweight, small for gestational age and perinatal death, were modeled separately for singletons and twins using logistic regression with the primary comparison between ART births and those to the newly created population based subgroup of births to women with indicators of subfertility but no ART.
Results
Singletons: The risks for both preterm birth and low birthweight were higher for the ART group (AOR 1.23 and 1.26, respectively) compared to the subfertile group and risks in both the ART and subfertile groups were higher than those among fertile births. Twins: the risk of perinatal death was significantly lower among ART births than fertile (AOR 0.55) or subfertile (AOR 0.15) births.
Conclusions
The use of a population based comparison group of subfertile births without ART demonstrated significantly higher rates of preterm birth and low birthweight in ART singleton births, but these differences are smaller than differences between ART and fertile births. Further refinement of the measurement of subfertile births and examination of the independent risks of subfertile births is warranted.
Keywords: Assisted Reproductive Technologies, Subfertility, Preterm Birth, Low Birthweight, Perinatal Death
INTRODUCTION
In the U.S. in 2012, treatment with assisted reproductive technologies (ART) resulted in 51,267 live births (deliveries of one or more living infants) and 65,160 live born infants representing 1.6% of all U.S. births(1). The growth in the use of ART has raised concerns about a range of perinatal outcomes in the resulting births, including the excess of preterm birth,(2–4) low birthweight,(5–7) small for gestational age(8) and neonatal death.(9) However, research into such outcomes has faced several major constraints:(10) randomization to ART treatment is not feasible; studies from individual ART clinics may lack statistical power; and population based, vital records datasets often lack accurate measurement of ART treatment. Importantly, most studies of outcomes of ART have not distinguished the effect of ART from that of underlying infertility.(10, 11) The outcomes of ART births have been analyzed in comparison to spontaneous conceptions,(12–14) across different treatment parameters,(15) within women themselves across different pregnancies(16) and, within a survey population,(17) to measures of delay in becoming pregnant. In the U.S. context, a population based comparison group of births to women with indicators of subfertility without ART has not been available for comparison in the past.(18) This study utilized a linkage between state records in a national ART clinical database and a statewide longitudinally linked public health database to develop a population based comparison group of births to women with indicators of subfertility who did not receive ART, thus permitting examination of underlying risks associated with these births and providing a more refined assessment of the unique impact of ART on perinatal outcomes.
METHODS
STUDY DATA
Data Sources
This study linked detailed clinical information on ART treatment from all ART clinics in Massachusetts with live births and fetal deaths from July 1, 2004 through December 31, 2008 recorded in the Massachusetts Pregnancy to Early Life Longitudinal (PELL) Data System. Both the PELL (19) and Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS)(20, 21) data systems have been described in previous publications. PELL links data on more than 99% of all births and fetal deaths in Massachusetts from 1998–2009 to corresponding hospital utilization data (admissions, outpatient stays and emergency room visits) and then longitudinally links those data over time, facilitating analysis of maternal hospitalizations prior to a given birth or fetal death. The SART CORS collects data from more than 400 ART clinics across the U.S. (covering 97% of all ART cycles).(22) The SART database includes all Massachusetts clinics, providing the opportunity for a population based examination of outcomes in the state. The national SART CORS database for 2004–08 contains 642,927 records of assisted reproductive technology treatment cycles. The database includes information on demographic characteristics, infertility diagnoses, treatment parameters, treatment outcomes and pregnancy outcomes.
Approval for the study was granted by the Institutional Review Boards at the Massachusetts Department of Public Health and the Boston University School of Medicine as well as the institutions of the project’s co-principal investigators.
Linkage of the Data Sources
We constructed the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART) database by linking the SART CORS and PELL data systems for all children born to Massachusetts resident women in Massachusetts hospitals between July 1, 2004 and December 31, 2008. The starting date was chosen based on the start date of our access to SART CORS (January 1, 2004) to allow us to capture any births associated with ART and the end date reflected the latest available data from both SART and PELL. PELL data from July 1, 2004 through December 31, 2008 included 282,971 women with 334,152 singleton or twin deliveries resulting in 342,035 births and fetal deaths which were linked to 42,649 ART cycles among 18,439 women from SART CORS with a resultant linkage of PELL delivery records to 9,092 ART cycles. We limited our analysis to singletons or twins with complete data on the predictors and outcomes of interest. The linkage process has been previously described. (23)
ANALYSIS
ART group
ART deliveries were identified from the SART CORS database drawing on clinical data from all Massachusetts infertility clinics. We identified 11,271 live births and fetal deaths from 9,092 deliveries.
Subfertility with no ART Comparison Group
The subfertility comparison group was developed using an algorithm that conservatively identified births to women with indicators of subfertility. The goal was to include only cases in which we had clear indication of either diagnosis of infertility through diagnosis codes or maternal report of fertility assistance. The method, which has been described in detail elsewhere, (18) involved identification of subfertile deliveries from three sources:
birth certificates – inclusion if either one of two items on the Massachusetts birth certificate concerning the use of fertility drugs or ART were checked for a delivery from July 1, 2004- December 31, 2008 or on a certificate for an earlier birth to the same woman in the five years prior to an index pregnancy in 2004–2008; or
prior hospital utilization – inclusion if a woman had hospital contact – admission, observational stay or emergency department visit – for a condition specifically indicating infertility (ICD codes 628.0/628.2/628.3/628.8/628.9/V230) associated with an index delivery or in the five years prior to an index pregnancy occurring between 2004–2008. The 628 codes represent “Diminished or absent ability of a female to achieve conception… a term doctors use if a woman hasn’t been able to get pregnant after at least one year of trying.”(24) The V23.0 diagnosis code represents “Supervision of high-risk pregnancy with history of infertility.”(25)
prior ART – inclusion if a woman had an ART cycle in the past as reported to SART CORS between 2004–2008, but did not have an ART cycle associated with the index delivery between 2004–2008.
Prior to cross-checking to eliminate cases that were identified in more than one data set, each source yielded the following number of births: Birth Certificates (9,929); Hospital Utilization (3,321) and SART data (1,641). After eliminating duplication in multiple sources, there were 12,918 cases and after then excluding cases with documented ART use in the index delivery, there were 6,905 births that provided evidence of subfertility without an ART cycle identified in clinic records for that birth. Finally, after limiting our data to births with complete data, the subfertile group included 6,609 live births and fetal deaths to mothers with at least one indicator of infertility with no evidence of an ART cycle for that birth.(18)
Fertile Comparison Group
Births not included in either the ART or Subfertile categories were classified as “Fertile,” since there was no indicator of subfertility or ART use. The Fertile group included 316,748 live births and fetal deaths.
Outcome Measures
Our final analysis was limited to cases with complete data for the variables used in the multivariate model. All analyses were stratified by plurality (singletons and twins) and examined across the three groups of interest. The perinatal outcomes were preterm birth (<37 completed weeks of gestation); low birthweight (< 2500 gms); small for gestational age (lowest 10th percentile among birthweights); and perinatal death (fetal deaths plus neonatal deaths < 7 days).(26) Birthweight Z-scores were calculated to evaluate adequacy of weight for age using Massachusetts population-based standards. In order to determine small for gestational age (SGA) births, we generated gender-, race/ethnicity-, and gestation-specific birthweight means and standard deviations using Massachusetts data for all live births from 1998–2008. Infants with birthweights below the 10th percentile for gestation were classified as small-for-gestational age. We limited our analyses of preterm birth, low birthweight and SGA to live births because of the differing distribution of birthweight by gestational age in fetal deaths (27) and the fact that the distribution used for determining SGA was based on live births only. Our linked data allowed us to identify each twin in a pair and perinatal deaths are based on the death of either twin in a pair.
Covariates
We conducted a series of analyses using logistic regression models to identify potential confounding variables in the association of fertility group and each outcome of interest. First, we ran a model with only the main independent factor, fertility status (as dummy variables, Subfertile vs. Fertile and ART- vs. Fertile). Subsequent models introduced each of the potential confounding variables starting with maternal socio-demographic characteristics. At each stage of modeling, we observed changes in the strength of association between fertility status and the outcome of interest. Variables that did not alter the associations (odds ratios) of either of the fertility group variables with outcome by 10% or more were not retained in the model.
The covariates that remained were maternal age, race/ethnicity, marital status, maternal education, payer for delivery, smoking, prenatal care,(28) parity, chronic and pregnancy associated hypertension, and infant gender. Individual maternal health conditions (e.g. endometriosis, polycystic ovaries, peritoneal adhesions) that were not captured in the subfertility measure were combined into a single dichotomous measure, “other fertility related condition,” which was included in the model. We tested for interaction effects between the main independent variable (fertility status of the delivery) and select demographic characteristics associated with each of the perinatal outcomes. None were deemed significant and as such were not included in the final models. We added propensity scores as covariates to our multivariate logistic models out of the concern that the processes which resulted in being categorized as fertile, subfertile or having received ART were potentially different.(29, 30) Inclusion of the propensity scores did not substantially alter the odds ratios, confidence intervals, or p-values and therefore were not included in the final model. In the multivariate logistic regression models we ran analyses of ART and subfertile outcomes compared to the fertile group, followed by a specific comparison of ART outcomes compared to subfertile births. The data were analyzed using SAS software version 9.2 (SAS Institute Inc., Cary, NC, USA.) and models computed using general estimating equations (GEE) to account for clustering of outcomes within a mother.
Results
Table 1 presents the demographic characteristics of the three fertility groups by plurality. The profile of ART and Subfertile births without ART were much more similar to each other than either group were to the cohort of fertile births. P values in the table are for the comparison of the ART and subfertile groups. Among singletons, mothers in the ART group were more likely to be older, better educated, have private insurance, be nulliparous, and have higher rates of pregnancy induced hypertension and primary cesarean section. Among twin births, mothers with ART tended to be older and more likely to deliver by primary cesarean section.
Table 1.
Maternal and Paternal Characteristics of the Study Population by Maternal Fertility Status
| Singletons | Twins | |||||||
|---|---|---|---|---|---|---|---|---|
| FERTILE | SUBFERTILE – No ART | ART | ART vs Subfertile | FERTILE | SUBFERTILE – No ART | ART | ART vs Subfertile | |
| N (Live births and fetal deaths) | 308,103 | 5,552 | 6,480 | P* | 8,645 | 1,057 | 4,791 | P* |
| % | % | % | % | % | % | |||
| Mother’s Age | <0.01 | <0.01 | ||||||
| ≤ 30 yrs | 54.6 | 16.4 | 11.8 | 47.4 | 20.5 | 15.4 | ||
| 31–34 | 24.2 | 29.3 | 27.0 | 26.9 | 35.2 | 28.9 | ||
| 35–37 | 12.8 | 26.8 | 25.5 | 16.5 | 23.5 | 25.4 | ||
| 38–40 | 6.2 | 18.2 | 20.8 | 7.2 | 15.0 | 17.0 | ||
| 41–42 | 1.6 | 6.0 | 8.1 | 1.3 | 3.6 | 6.4 | ||
| ≥ 43 | 0.7 | 3.4 | 6.9 | 0.8 | 2.7 | 7.0 | ||
| Mother Non-Hisp. White | 67.3 | 85.0 | 86.0 | <0.01 | 70.3 | 88.6 | 87.9 | 0.33 |
| Mother BachDeg. Postgrad | 40.6 | 69.8 | 74.0 | <0.01 | 44.3 | 71.0 | 72.7 | 0.02 |
| Mother U.S. Born | 72.4 | 82.6 | 82.5 | 0.87 | 77.1 | 84.8 | 83.0 | 0.14 |
| Mother Not Married | 33.8 | 5.6 | 4.0 | <0.01 | 29.9 | 4.5 | 3.1 | 0.02 |
| Father’s age 35+ | 36.4 | 66.1 | 71.6 | <0.01 | 40.8 | 60.2 | 67.4 | <0.01 |
| Father Non-Hispan. White | 68.1 | 85.6 | 87.4 | <0.01 | 71.7 | 88.2 | 87.7 | 0.43 |
| Father Bach Deg. Postgrad | 40.5 | 65.6 | 69.4 | <0.01 | 44.2 | 65.6 | 70.7 | <0.01 |
| Father U.S. Born | 71.3 | 81.2 | 81.9 | 0.37 | 74.8 | 83.6 | 82.8 | 0.53 |
| Del. Payer Source Private | 58.7 | 92.0 | 96.8 | <0.01 | 61.4 | 93.8 | 96.2 | <0.01 |
| Nulliparous | 45.7 | 39.4 | 62.4 | <0.01 | 21.7 | 30.8 | 31.6 | 0.08 |
| Gestational Diabetes | 5.4 | 8.3 | 8.1 | 0.67 | 7.9 | 10.8 | 9.9 | 0.36 |
| Other Diabetes | 1.1 | 1.9 | 2.0 | 0.64 | 1.7 | 2.8 | 2.4 | 0.34 |
| Pregnancy-Induced Hypert | 8.3 | 10.2 | 12.8 | <0.01 | 20.6 | 26.9 | 24.7 | 0.15 |
| Chronic Hypertension | 1.6 | 2.7 | 3.2 | 0.07 | 2.6 | 3.6 | 3.0 | 0.32 |
| Smoked During Pregnancy | 7.8 | 1.8 | 0.8 | <0.01 | 6.9 | 0.8 | 0.8 | 0.80 |
| Adequate + Prenatal Care | 37.6 | 48.0 | 48.8 | 0.01 | 75.4 | 82.6 | 84.8 | <0.01 |
| Primary cesarean | 21.5 | 29.0 | 38.6 | <0.01 | 62.9 | 67.3 | 75.4 | <0.01 |
| Infant Gender Male | 51.2 | 50.5 | 50.9 | 0.63 | 50.5 | 50.0 | 51.6 | 0.33 |
| Any Infertility Condition | 2.9 | 7.2 | 8.4 | 0.01 | 2.9 | 6.6 | 9.0 | 0.01 |
p values represent comparison of ART v Subfertile group. ART vs. FERTILE is statistically significantly different in proportion at p<.01 in every comparison except for: infant gender for singleton, and chronic hypertension and infant gender for twins
Table 2 presents the unadjusted prevalence of prematurity, birthweight, small for gestational age and perinatal death for the three fertility groups by plurality. Among singletons, ART births compared to subfertile births were more likely to be preterm (10.2% vs 8.1%), low birthweight (7.8% vs 5.7%) and small for gestational age SGA (8.1% vs 6.5%). Among twins, ART births compared to subfertile births had a longer mean gestational age (35.6 vs 35.0 weeks), lower rate of very premature (<32 weeks) delivery, (8.9% vs 11.6%), very low birthweight (< 1500 grams) births (7.7% vs 10.3%), and much lower rate of perinatal death (11.5 per 1,000 vs 61.5 per 1,000). The ART twin births had the lowest perinatal death rate of the three groups.(31) Comparing the perinatal death rates of singletons versus twins, we see a much smaller disparity between the ART populations (11.5 per 1,000 for twins versus 4.2 for singletons) compared to the difference in perinatal death rate between fertile twins (25.7) and singletons (4.3).
Table 2.
Perinatal Outcomes by Maternal Fertility Status and Plurality
| Singleton | Twins | |||||||
|---|---|---|---|---|---|---|---|---|
| FERTILE | SUBFERTILE – No ART | ART | ART vs Subfertile | FERTILE | SUBFERTILE – No ART | ART | ART vs Subfertile | |
| N* (Live Births) | 307,320 | 5,536 | 6,470 | P** | 8,569 | 1,046 | 4,774 | P** |
| Preterm Birth (%) | <0.01 | 0.03 | ||||||
| <32 completed weeks | 0.9 | 1.1 | 1.7 | 9.7 | 11.6 | 8.9 | ||
| 32–33 | 0.7 | 1.0 | 1.4 | 8.3 | 9.5 | 8.3 | ||
| 34–36 | 4.8 | 6.0 | 7.1 | 35.0 | 35.4 | 36.6 | ||
| Total Preterm (<37 weeks) | 6.4 | 8.1 | 10.2 | 53.0 | 56.5 | 53.8 | ||
| 37–38 completed weeks | 21.7 | 26.1 | 25.8 | 38.4 | 37.9 | 39.2 | ||
| 39–40 | 60.5 | 56.5 | 54.7 | 8.4 | 5.7 | 6.9 | ||
| 41+ | 11.5 | 9.4 | 9.2 | 0.3 | 0.0 | 0.2 | ||
| Gestational Age (mean completed weeks & S.D.) | 39.0 (1.8) | 38.7 (2.0) | 38.6 (2.2) | <0.01 | 35.5 (3.3) | 35.0 (3.9) | 35.6 (3.0) | <0.01 |
| Birthweight (%) | <0.01 | <0.01 | ||||||
| <1,500g | 0.8 | 1.0 | 1.5 | 9.1 | 10.3 | 7.7 | ||
| 1500–2499g | 4.6 | 4.7 | 6.3 | 43.9 | 40.2 | 42.6 | ||
| Low Birthweight (<2500 gms) | 5.4 | 5.7 | 7.8 | 53.0 | 50.5 | 50.3 | ||
| 2500+ g | 94.6 | 94.3 | 92.2 | 47.1 | 49.5 | 49.8 | ||
| Birthweight (average gms & S.D.) | 3362 (552) | 3382 (579) | 3311 (606) | <0.01 | 2383 (636) | 2369 (692) | 2440 (615) | <0.01 |
| Small for Gestational Age (%) | 8.1 | 6.5 | 8.1 | <0.01 | 20.6 | 16.9 | 17.9 | 0.46 |
| N (live births + fetal deaths) | 308,103 | 5,552 | 6,480 | 8,645 | 1,057 | 4,791 | ||
| Perinatal Death (per 1,000) | 4.3 | 5.8 | 4.2 | 0.21 | 25.7 | 61.5 | 11.5 | <0.01 |
N based on live births for gestational age, birthweight. N for and perinatal death based on live births and fetal deaths.
All comparisons between ART vs. FERTILE group significant at p < .01 except SGA and perinatal deaths among singletons and preterm birth, gestational age among twins. Chi square used for categorical variables; t test for continuous.
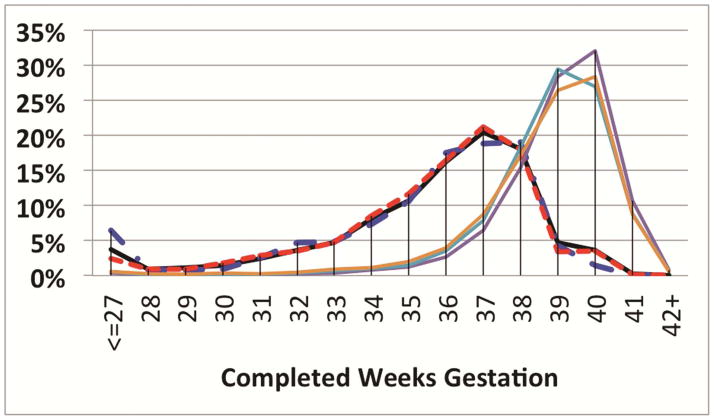
Figure 1 presents gestational age distributions by week for the three groups. Among singletons the ART group had higher proportions of births in weeks 32–37, though the modal week for ART births was week 40, while the subfertile group had a peak at 39 weeks. Among twins, the higher rate of early preterm births for the subfertile group is evident from a distinct tail at less than or equal to 27 weeks while the ART group had a lower rate of early preterm births than the fertile group.
Figure 1.
Gestational Age Distribution, by Fertility Groups, Singletons & Twins
 FERTILE – Twin
FERTILE – Twin
 SUBFERTILE – Twin
SUBFERTILE – Twin
 ART– Twin
ART– Twin
 FERTILE– Singleton
FERTILE– Singleton
 SUBFERTILE– Singleton
SUBFERTILE– Singleton
 ART – Singleton
ART – Singleton
Table 3 presents the adjusted odds ratios and 95% confidence intervals for each outcome by plurality for the three fertility groups controlling for the covariates noted above. We compared the ART and subfertile groups to the fertile group as the reference and then the ART group was compared directly to the subfertile group as a reference. Among singletons, the odds of preterm birth and low birthweight were higher among both the subfertile (AORs 1.24 and 1.20 respectively) and ART (1.53 and 1.51 respectively) groups compared to the fertile group, and the ART group was significantly higher than the subfertile group in each case (AOR 1.23 and 1.26 respectively). The risk for SGA among singletons did not differ significantly between the three fertility groups, nor between the ART and subfertile groups. The odds ratio for perinatal death among the ART group was comparable to the fertile group though the subfertile group had a significantly higher rate (AOR 1.51).
Table 3.
Risks of Adverse Perinatal Outcomes by Fertility Group and Plurality ^
| Singletons | Twins | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome* | AOR | 95% CI | P Value* | AOR | 95% CI | P Value* | AOR | 95% CI | P Value* | AOR | 95% CI | P Value* | |
| Preterm | |||||||||||||
| FERTILE | 1.00 | (Reference) | ---- | 0.80 | (0.72, 0.89) | <0.01 | 1.00 | (Reference) | ---- | 0.74 | (0.31, 1.76) | 0.50 | |
| SUBFERTILE – No ART | 1.24 | (1.12, 1.38) | <0.01 | 1.00 | (Reference) | ---- | 1.35 | (0.57, 3.20) | 0.50 | 1.00 | (Reference) | ---- | |
| ART | 1.53 | (1.40, 1.67) | <0.01 | 1.23 | (1.08, 1.41) | <0.01 | 0.89 | (0.68, 1.18) | 0.43 | 0.66 | (0.23, 1.90) | 0.45 | |
| Low Birthweight | |||||||||||||
| FERTILE | 1.00 | (Reference) | ---- | 0.83 | (0.74, 0.94) | <0.01 | 1.00 | (Reference) | ---- | 0.99 | (0.83, 1.18) | 0.92 | |
| SUBFERTILE – No ART | 1.20 | (1.06, 1.36) | <0.01 | 1.00 | (Reference) | ---- | 1.01 | (0.85, 1.20) | 0.92 | 1.00 | (Reference) | ---- | |
| ART | 1.51 | (1.37, 1.67) | <0.01 | 1.26 | (1.08, 1.47) | <0.01 | 0.98 | (0.89, 1.09) | 0.77 | 0.98 | (0.82, 1.17) | 0.79 | |
| Small-for-Gestation | |||||||||||||
| FERTILE | 1.00 | (Reference) | ---- | 1.05 | (0.94, 1.17) | 0.39 | 1.00 | (Reference) | ---- | 1.25 | (1.02, 1.52) | 0.03 | |
| SUBFERTILE – No ART | 0.95 | (0.85, 1.06) | 0.39 | 1.00 | (Reference) | ---- | 0.80 | (0.66, 0.98) | 0.03 | 1.00 | (Reference) | ---- | |
| ART | 1.05 | (0.96, 1.16) | 0.31 | 1.10 | (0.96, 1.27) | 0.18 | 0.85 | (0.75, 0.96) | <0.01 | 1.06 | (0.86, 1.30) | 0.60 | |
| Perinatal Death | |||||||||||||
| FERTILE | 1.00 | (Reference) | ---- | 0.66 | (0.46, 0.95) | 0.03 | 1.00 | (Reference) | ---- | 0.27 | (0.17, 0.42) | <0.01 | |
| SUBFERTILE – No ART | 1.51 | (1.05, 2.17) | 0.03 | 1.00 | (Reference) | ---- | 3.73 | (2.37, 5.87) | <0.01 | 1.00 | (Reference) | ---- | |
| ART | 1.00 | (0.67, 1.50) | 0.99 | 0.66 | (0.40, 1.11) | 0.12 | 0.55 | (0.34, 0.89) | 0.01 | 0.15 | (0.09, 0.25) | <0.01 | |
Sample based on live births for gestational age, low birthweight and small for gestational age. Sample for perinatal death based on live births and fetal deaths.
Models adjusted for maternal age, race/ethnicity, marital status, maternal education, payer for delivery, smoking, prenatal care, parity, chronic and pregnancy associated hypertension, other fertility related condition and infant gender
Among twin births, there were no significant differences in preterm birth or low birthweight across the three fertility groups. In the case of SGA, the risks for both the subfertile and ART groups were 15–20% lower than the fertile group; there was no difference between the ART and subfertile group. Compared to the fertile group, the subfertile group had a higher risk (AOR 3.73) of perinatal death, while the ART group had half the risk (AOR 0.55). (31, 32) Comparing the subfertile and ART groups, the latter had an 85% lower risk (AOR 0.15). Examination of the perinatal deaths among the subfertile twin births found a higher concentration of very premature births (84% of neonatal deaths prior to 24 weeks in the subfertile vs. 62% in ART group). When we tested models for twin perinatal death that included gestational age, the differences between the fertile and subfertile groups became non- significant, though the odds of a twin death in the ART group remained significantly lower than either the fertile or subfertile group (data not shown).
Sensitivity Analysis
We conducted a sensitivity analysis to examine the potential impact of the use of alternative measures of outcomes and to better understand the reasons behind particular findings. Using early neonatal death (<7 days) as an outcome (i.e. excluding fetal deaths), we found a similarly lower risk of deaths among ART twins compared to subfertile births (AOR 0.12) as in the analysis of perinatal death (AOR 0.15). We also examined whether or not ART births were more likely to have occurred in Level III hospitals and found larger proportions of both ART and “Subfertile without ART” twin births occurring in tertiary centers compared to fertile births. We then tested whether including a variable for hospital level in our models would alter the findings and it did not. One possible explanation for the better outcomes of ART twins could be the higher rate of dichorionic pregnancies among ART births(33, 34) which fare better than monochorionic births, a hypothesis our data do not permit us to examine directly since monozyogsity is not recorded in either of our datasets. However, an analysis restricted to mixed gender twins – by definition dichorionic – found a comparable relative difference between subfertile and ART perinatal deaths (AOR 0.16) as the original model (AOR 0.15).
Discussion
There has long been concern(35) that perinatal outcomes associated with ART births may be compromised. This study has addressed several of the major problems that have limited past research efforts to examine perinatal outcomes, most notably the inability to distinguish between outcomes that may be the result of ART and those resulting from underlying infertility. In this study, we found that preterm birth and low birthweight were increased among ART singletons when compared to singleton deliveries in a fertile population, but that these were also increased in a subfertile population. Further, the risk of perinatal death for ART twins was much lower than in births to fertile mothers and lower still than to mothers with indicators of subfertility without ART.
An important contribution of this paper is the application of our initial approximation of a U.S. based population measure(18) of births to mothers with an indicator of subfertility who did not have an ART cycle associated with the index birth being studied. The addition of this group permits the examination of perinatal outcomes associated with infertility apart from ART as well as the comparison of outcomes associated with ART with those of births to mothers with and without indicators of subfertility. While a number of studies have examined the outcomes of births to mothers with subfertility indicators who gave birth without ART, these have generally been based on non-U.S. data sources(17, 36–38) or systematic reviews that primarily drew on non-U.S. studies.(4, 8) These studies generally found, as we did, higher rates of preterm birth and low birthweight among singleton births to women with indicators of subfertility independent of ART. The importance of the current work is to extend these comparisons to a US population in which ART treatment parameters including amount of ovulation stimulation medication and number of embryos transferred may be different than those of other countries.
Comparing the perinatal outcomes of ART births to spontaneous conceptions, our findings are largely consistent with past research that has found higher rates of preterm birth and low birthweight among singletons born after ART. A meta-analysis by Jackson(13) and systematic reviews by Helmerhorst(12) and Allen(14) all found higher risks for preterm birth and low birth weight when comparing ART births to spontaneous conceptions. While rates of singleton preterm birth and low birth weight were significantly higher in this study, the degree of difference we found was lower than AORs for the same comparison in past research, which might be accounted for by our ability to include substantially more covariates (demographic, social and medical risk) than prior studies. Also, the time frame for our research is more recent than these prior studies and both Klemetti (39) and Kallen(40) reported ART results relative to spontaneous conceptions to be improving over time. Our findings differ somewhat with past findings on SGA. Our more contemporary, U.S. based analysis found no differences between SGA of ART and fertile singleton births, while some prior research(36) has found higher rates of SGA in both subfertile and ART assisted births.
Our findings on perinatal death are of particular interest. Among singletons, we found no difference in risk of perinatal death in births to mothers with ART when compared to births to fertile women while there was a significantly higher risk of perinatal death in the subfertile group without ART. Two prior studies examined perinatal mortality as an outcome in births to subfertile women without ART. Both Basso(9) and Draper(32), relying on different populations and measures of subfertility found, as we did, significantly higher neonatal or perinatal mortality in births to mothers with indicators of subfertility and no ART when compared to spontaneous conceptions (AORs both 3.3). Unlike our findings, both Jackson and Helmerhorst’s reviews found higher rates of perinatal death for singleton ART births, but both drew a large proportion of cases from a single 1990’s Belgian study (41) in which mortality rates were almost double current rates.
Outcomes of twin ART births fared better than comparable fertile births for SGA and perinatal death. These findings are generally consistent with past research, though the literature on outcomes of twin births is less extensive and was limited to the use of spontaneous conceptions as the comparison group.(42–45) Our finding of a lower rate of perinatal death among twins in ART births compared to those from fertile births is comparable to prior research by Fitzsimmons(45) and Boulet,(43) and closely matches the results of Helmerhorst ’s systematic review (AOR 0.58).(31) Our study, relying on state vital statistics data to identify fetal and early neonatal deaths benefitted from much larger populations than prior studies. One suggested explanation for the better outcomes is the “special baby” hypothesis, suggesting that the extra attention given to ART births by both parents and caregivers may contribute to more favorable outcomes.(46) ART mothers had higher rates of primary cesarean section and “adequate plus” prenatal care, though the differences in prenatal care with the “subfertility without ART” group were minimal (Table 1). Nonetheless it may be possible that ART related births involved greater attention to care and more sensitive and comprehensive measures of prenatal care than are currently available on a population basis will be necessary to determine if a “special baby” hypothesis is supported. Considering only the subfertile population, our study found notably higher risks for perinatal death among twins when compared to births to mothers without subfertility indicators. Overall these studies suggest an underlying risk associated with subfertility distinct from that which may result from ART.
Despite the advantages our linked dataset brings to the analysis, limitations remain. Massachusetts was chosen as a site for the study in part because of its policy of mandating private insurers to cover ART and the corresponding high rate of ART use, but the experience in Massachusetts may not be representative of other settings. Our algorithm used to identify “subfertile” births may have missed some cases, misclassifying them as “fertile.” The MOSART dataset does not yet have access to ambulatory care cases, hence those mothers seen by non-hospital healthcare providers for infertility treatment would be missed. As a result, subfertile cases identified through hospital discharge data likely represent an undercount of all cases of treatment for subfertility, though some of the ambulatory care cases were likely identified through the birth certificate items. Ambulatory subfertile patients may be less subfertile, than those found in the subfertile institution population. If true, this would tend to increase the significance of the results. We chose a conservative measure to maximize the positive predictive value of our subfertile designation and sought to avoid misclassification of fertile cases into the much smaller subfertility group.(18) We were also unable to determine definitively how long mothers in the subfertile group had been trying to conceive and whether they conceived spontaneously or used fertility drugs or other non-ART procedures to conceive. Longer infertile intervals have been associated with a greater risk for adverse outcome. This may explain some of the differences between the ART and sub fertile groups. Likewise we were not able to assess time to pregnancy for women in the fertile group. However, our study question focused on the overall impact of the use of ART, rather than an explicit comparison between fertility drug use and ART.
The analysis of the perinatal outcomes of ART births in comparison to births to women with indicators of subfertility is a valuable step forward in our understanding of the reasons for adverse outcomes. Future research on the subfertility group itself can yield important information through refinement of the subfertility measure and further exploration of poor outcomes in this population. The enhancement of our understanding of the outcomes of assisted reproductive technologies will continue to provide information to help clinicians better inform patients of any risks associated with ART treatment.
Acknowledgments
The project described was supported by Award Numbers R01HD064595 and R01HD067270 from the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
Dr. Declercq, Dr. Belanoff, Dr. Cabral, Dr. Diop, Ms. Gopal, and Ms. Hoang have nothing to disclose. Dr. Luke reports grants from National Institutes of Health, during the conduct of the study; personal fees from Society for Assisted Reproductive Technology, outside the submitted work. Dr. Kotelchuck reports grants from NICHD Grants RO1HD06459501 & RO1HD06727001, during the conduct of the study. Dr. Stern reports grants from NIH, during the conduct of the study; grants from ASRM, other from Cooley LLC, outside the submitted work. Dr. Hornstein reports personal fees from WIN Fertility, personal fees from Up to Date, outside the submitted work.
The authors wish to thank additional members of the MOSART team: Bruce Cohen; Dmitri Kissin; Thien Nguyen; and Donna Richard.
SART wishes to thank all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Footnotes
Presented at the 69th annual meeting of the American Society for Reproductive Medicine, Boston, Massachusetts, October 12–17, 2013
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. 2012 ART fertility clinic success rates report. Center for Disease Control and Prevention; 2014. http://www.cdc.gov/art/ARTReports.htm. [Google Scholar]
- 2.Tepper N, Farr S, Cohen B, Nannini A, Zhang Z, Anderson J, et al. Singleton Preterm Birth: Risk Factors and Association with Assisted Reproductive Technology. Maternal and Child Health Journal. 2012;16:807–13. doi: 10.1007/s10995-011-0787-8. [DOI] [PubMed] [Google Scholar]
- 3.Wang YA, Sullivan EA, Black D, Dean J, Bryant J, Chapman M. Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertility and Sterility. 2005;83:1650–8. doi: 10.1016/j.fertnstert.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 4.Pinberg A, Wennerholm U, Romundstad L, Loft A, Aittomaki K, Soderstrrom-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Human Reproduction Update. 2013;19:87–104. doi: 10.1093/humupd/dms044. [DOI] [PubMed] [Google Scholar]
- 5.Kondapalli LA, Perales-Puchalt A. Low birth weight: is it related to assisted reproductive technology or underlying infertility? Fertility and Sterility. 2013;99:303–10. doi: 10.1016/j.fertnstert.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McElrath TF, Wise PH. Fertility therapy and the risk of very low birth weight. Obstetrics & Gynecology. 1997;90:600–5. doi: 10.1016/s0029-7844(97)00362-1. [DOI] [PubMed] [Google Scholar]
- 7.Cooper AR, O’Neill KE, Allsworth JE, Jungheim ES, Odibo AO, Gray DL, et al. Smaller fetal size in singletons after infertility therapies: the influence of technology and the underlying infertility. Fertility and Sterility. 2011;96:1100–6. doi: 10.1016/j.fertnstert.2011.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Messerlian C, Maclagan L, Basso O. Infertility and the risk of adverse pregnancy outcomes: a systematic review and meta-analysis. Human Reproduction. 2013;28:125–37. doi: 10.1093/humrep/des347. [DOI] [PubMed] [Google Scholar]
- 9.Basso O, Olsen J. Subfecundity and neonatal mortality: longitudinal study within the Danish national birth cohort. BMJ. 2005;330:393–4. doi: 10.1136/bmj.38336.616806.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buck Louis GM, Schisterman EF, Dukic VM, Schieve LA. Research hurdles complicating the analysis of infertility treatment and child health. Human Reproduction. 2005;20:12–8. doi: 10.1093/humrep/deh542. [DOI] [PubMed] [Google Scholar]
- 11.Barnhart KT. Assisted reproductive technologies and perinatal morbidity: interrogating the association. Fertility and Sterility. 2013;99:299–302. doi: 10.1016/j.fertnstert.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frans M, Helmerhorst, Perquin DAM, Donker D, Keirse MJNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261. doi: 10.1136/bmj.37957.560278.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstetrics & Gynecology. 2004;103:551–63. doi: 10.1097/01.AOG.0000114989.84822.51. [DOI] [PubMed] [Google Scholar]
- 14.Allen V, Wilson RD. Joint SOGC-CFAS Guideline: Pregnancy Outcomes after Assisted Reproductive Technology. J Obstet Gynaecol Can. 2006;28:220–33. doi: 10.1016/S1701-2163(16)32112-0. [DOI] [PubMed] [Google Scholar]
- 15.Schieve LA, Ferre C, Peterson HB, Macaluso M, Reynolds MA, Wright VC. Perinatal outcome among singleton infants conceived through assisted reproductive technology in the United States. Obstetrics & Gynecology. 2004;103:1144–53. doi: 10.1097/01.AOG.0000127037.12652.76. [DOI] [PubMed] [Google Scholar]
- 16.Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjærven R, Vatten LJ. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Human Reproduction. 2006;21:2353–8. doi: 10.1093/humrep/del153. [DOI] [PubMed] [Google Scholar]
- 17.Brink Henriksen T, Day Baird D, Olsen J, Hedegaard M, Jørgen Secher N, Wilcox AJ. Time to pregnancy and preterm delivery. Obstetrics & Gynecology. 1997;89:594–9. doi: 10.1016/s0029-7844(97)00045-8. [DOI] [PubMed] [Google Scholar]
- 18.Declercq ER, Belanoff C, Diop H, Gopal D, Hornstein MD, Kotelchuck M, et al. Identifying women with indicators of subfertility in a statewide population database: operationalizing the missing link in assisted reproductive technology research. Fertility and Sterility. 2013 doi: 10.1016/j.fertnstert.2013.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Declercq ER, Barger M, Cabral HJ, Evans SR, Kotelchuck M, Simon C, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstetrics & Gynecology. 2007;109:669–77. doi: 10.1097/01.AOG.0000255668.20639.40. [DOI] [PubMed] [Google Scholar]
- 20.Luke B, Brown MB, Wantman E, Lederman A, Gibbons W, Schattman GL, et al. Cumulative birth rates with linked assisted reproductive technology cycles. New England Journal of Medicine. 2012;366:2483–91. doi: 10.1056/NEJMoa1110238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luke B, Brown MB, Stern JE, Missmer SA, Fujimoto VY, Leach R. Racial and ethnic disparities in assisted reproductive technology pregnancy and live birth rates within body mass index categories. Fertility and Sterility. 2011;95:1661–6. doi: 10.1016/j.fertnstert.2010.12.035. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2011 Assisted Reproductive Technology Success Rates: National Summary and Fertility Clinic Reports. Washington, DC: 2013. [Google Scholar]
- 23.Kotelchuck M, Hoang L, Stern J, Diop H, Belanoff C, Declercq E. The MOSART database: Linking the SART CORS clinical database to the population-based Massachusetts PELL reproductive public health data system. MCH Journal. 2014 doi: 10.1007/s10995-014-1465-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ICD9Data.com. 2011 ICD9Data.com.
- 25.Buck C. 2011 ICD-9-CM for Hospitals. St. Louis, Missouri: Elsevier; 2011. Standard Edition. [Google Scholar]
- 26.Barfield WD Fetus tCo Newborn. Standard Terminology for Fetal, Infant, and Perinatal Deaths. Pediatrics. 2011;128:177–81. doi: 10.1542/peds.2011-1037. [DOI] [PubMed] [Google Scholar]
- 27.Zhang X, Joseph K, Cnattingius S, Kramer M. Birth weight differences between preterm stillbirths and live births: analysis of population-based studies from the U.S. and Sweden. BMC Pregnancy and Childbirth. 2012;12:119. doi: 10.1186/1471-2393-12-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barfield W, Clements K, Lee K, Kotelchuck M, Wilber N, Wise P. Using linked data to assess patterns of Early Intervention (EI) referral among very low birth weight infants. Maternal and Child Health Journal. 2008;12:24–33. doi: 10.1007/s10995-007-0227-y. [DOI] [PubMed] [Google Scholar]
- 29.D’Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine. 1998;17:2265–81. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 31.Helmerhorst FM, Perquin DAM, Donker D, Keirse MJNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261. doi: 10.1136/bmj.37957.560278.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Draper E, Kurinczuk JJ, Abrams K, Clarke M. A ssessment of separate contributions to perinatal mortality of infertility history and treatment: a case-control analysis. Lancet. 1999;353:1746–9. doi: 10.1016/S0140-6736(98)08500-6. [DOI] [PubMed] [Google Scholar]
- 33.Chow JS, Benson CB, Racowsky C, Doubilet PMEG. Frequency of a monochorionic pair in multiple gestations: relationship to mode of conception. J Ultrasound Med. 2001;20:757–60. doi: 10.7863/jum.2001.20.7.757. [DOI] [PubMed] [Google Scholar]
- 34.Luke B, Brown MB, Wantman E, Stern JE. Factors associated with monozygosity in assisted reproductive technology pregnancies and the risk of recurrence using linked cycles. Fertility and Sterility. 2014;101:683–9. doi: 10.1016/j.fertnstert.2013.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saunders DM, MMPL The Australian Register: Current Research and Future Role. A Preliminary report. Annals of the New York Academy of Sciences. 1988;21:7–21. doi: 10.1111/j.1749-6632.1988.tb22237.x. [DOI] [PubMed] [Google Scholar]
- 36.Zhu JL, Obel C, Hammer Bech B, Olsen J, Basso O. Infertility, infertility treatment, and fetal growth restriction. Obstetrics & Gynecology. 2007;110:1326–34. doi: 10.1097/01.AOG.0000290330.80256.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basso O, Baird DD. Infertility and preterm delivery, birthweight, and caesarean section: a study within the Danish national birth cohort. Human Reproduction. 2003;18:2478–84. doi: 10.1093/humrep/deg444. [DOI] [PubMed] [Google Scholar]
- 38.Gaudoin M, Dobbie R, Finlayson A, Chalmers J, Cameron IT, Fleming R. Ovulation induction/intrauterine insemination in infertile couples is associated with low-birth-weight infants. American Journal of Obstetrics and Gynecology. 2003;188:611–6. doi: 10.1067/mob.2003.5. [DOI] [PubMed] [Google Scholar]
- 39.Klemetti R, Gissler M, Hemminki E. Comparison of perinatal health of children born from IVF in Finland in the early and late 1990s. Human Reproduction. 2002;17:2192–8. doi: 10.1093/humrep/17.8.2192. [DOI] [PubMed] [Google Scholar]
- 40.Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Otterblad Olausson P. Trends in delivery and neonatal outcome after in vitro fertilization in Sweden: data for 25 years. Human Reproduction. 2010;25:1026–34. doi: 10.1093/humrep/deq003. [DOI] [PubMed] [Google Scholar]
- 41.Dhont M, De Sutter P, Ruyssinck G, Martens G, Bekaert A. Perinatal outcome of pregnancies after assisted reproduction: A case-control study. American Journal of Obstetrics and Gynecology. 1999;181:688–95. doi: 10.1016/s0002-9378(99)70514-4. [DOI] [PubMed] [Google Scholar]
- 42.Nassar AH, Usta IM, Rechdan JB, Harb TS, Adra AM, Abu-Musa AA. Pregnancy outcome in spontaneous twins versus twins who were conceived through in vitro fertilization. American Journal of Obstetrics and Gynecology. 2003;189:513–8. doi: 10.1067/s0002-9378(03)00485-x. [DOI] [PubMed] [Google Scholar]
- 43.Boulet SL, Schieve LA, Nannini A, Ferre C, Devine O, Cohen B, et al. Perinatal outcomes of twin births conceived using assisted reproduction technology: a population-based study. Human Reproduction. 2008;23:1941–8. doi: 10.1093/humrep/den169. [DOI] [PubMed] [Google Scholar]
- 44.Murphy M, Rachel N, Hey K, Seagroatt V, Goldacre M, Vessey M, et al. Pregnancy Outcome Among Twins Conceived After Subfertility Treatment Compared With Natural Twins: A Population-Based Study. Twin Research and Human Genetics. 2006;9:279–84. doi: 10.1375/183242706776382437. [DOI] [PubMed] [Google Scholar]
- 45.Fitzsimmons BP, Bebbington MW, Fluker MR. Perinatal and neonatal outcomes in multiple gestations: Assisted reproduction versus spontaneous conception. American Journal of Obstetrics and Gynecology. 1998;179:1162–7. doi: 10.1016/s0002-9378(98)70125-5. [DOI] [PubMed] [Google Scholar]
- 46.Srebnik N, Miron-Shatz T, Rolison JJ, Hanoch Y, Tsafrir A. Physician recommendation for invasive prenatal testing: the case of the ‘precious baby’. Human Reproduction. 2013;28:3007–11. doi: 10.1093/humrep/det354. [DOI] [PubMed] [Google Scholar]