Abstract
Rates of suicidal ideation and behavior are extremely high in Bipolar Spectrum Disorders (BSDs). However, relatively little work has evaluated potentially synergistic relationships between cognitive and emotion-regulatory processes proposed by theoretical models of suicidality in BSDs. The present study evaluated whether negative cognitive style and subtypes of rumination would exacerbate the impact of self-criticism on suicidal ideation in a prospective study of individuals with BSDs. Seventy-two young adults with BSDs (bipolar II, bipolar NOS, or cyclothymia) completed diagnostic interviews and trait measures of self-criticism, negative cognitive style, and brooding and reflective rumination at a baseline assessment. The occurrence of suicidal ideation was assessed as part of diagnostic interviews completed every four months for an average of three years of follow-up. Negative cognitive style and reflective rumination strengthened the association between self-criticism and the prospective occurrence of suicidal ideation across follow-up. Individuals with high levels of self-criticism in conjunction with negative cognitive style or reflective rumination were most likely to experience the onset of suicidal ideation. Self-criticism may work synergistically with negative cognitive style and rumination to confer risk for suicidal ideation in bipolar spectrum disorders. These results support theoretical models of suicidality in BSDs and indicate that evaluating and understanding negative cognitive styles may help to identify individuals who are at risk for suicide.
Keywords: bipolar spectrum, bipolar disorder, suicide, suicidal ideation, cognitive styles, self-criticism, rumination
1. Introduction
Bipolar spectrum disorders (BSDs) are characterized by periods of depression and/or mood elevation and are associated with impairment in many areas of functioning (Murray and Lopez, 1996; Peters et al., 2014). In addition, individuals with BSDs experience high rates of suicide (Angst et al., 2002), with previous reports indicating that 25 to 50% of individuals with bipolar I or II disorder have a lifetime history of a suicide attempt (Chen and Dilsaver, 1996; Leverich et al., 2003; Valtonen et al., 2005), twice the rate of individuals with unipolar depression (Chen and Dilsaver, 1996), and twenty to thirty times greater risk than the general population (Pompili et al., 2013). In addition, suicidal ideation (SI), which strongly predicts suicide attempts (Leverich et al., 2003), may occur in greater than 80% of patients with bipolar I and II disorders during their lifetimes (Valtonen et al., 2005). However, the biological, clinical and psychosocial factors leading to SI in BSDs remain understudied (Valtonen et al., 2005). A better understanding of suicide risk in BSDs could lead to improved detection and prevention of suicide.
Malhi et al. (2013) recently developed the Bipolar Suicidality Model (BSM) to address the lack of theoretical approaches in existing studies investigating risk factors for suicide in BSDs. Given that stressful life events are demonstrated risk factors for suicide (e.g., Bagge, Glenn, and Lee, 2013; for review see Liu and Miller, 2014), the BSM proposes that when encountering such events, individuals who appraise situations as being hopeless, futile, or unchangeable are likely to think about suicide as a way of escaping the situation. Similarly, individuals who make appraisals about themselves as being unworthy or flawed are likely to perceive defeat and experience SI. Individuals with BSDs are especially likely to make appraisals of defeat and tend to repeatedly activate and amplify these appraisals because of difficulties disengaging from negative thinking and difficulties with emotion regulation (Malhi et al., 2013).
To date, few studies have evaluated specific psychosocial components of the BSM such as individuals’ appraisals of themselves following stressful life events. One such style of self-appraisal is self-criticism, a cognitive style stemming from perfectionistic beliefs and an inability to derive satisfaction from successes, which results in negative evaluations of oneself (e.g., Blatt et al., 1982), and which has frequently been linked to greater severity of suicidal ideation and behavior (Fazaa and Page, 2003). Self-criticism is elevated among suicide attempters, particularly following stressful events as a result of motivation to escape (e.g., Klomek et al., 2008). It is also associated with SI in clinical and healthy samples (for a review, see O’Connor, 2007), and among suicide attempters, self-criticism is associated with hopelessness (Donaldson, Spirito, and Farnett, 2000), which is a risk factor for suicide in BSDs (Hawton et al., 2005; Valtonen et al., 2005, 2006). Among individuals with BSDs (bipolar II, bipolar NOS, and cyclothymia), self-criticism conferred vulnerability to depressive symptoms following congruent stressful life events (Francis-Raniere et al., 2006), and it predicted the prospective onset of episodes of depression and hypomania (Alloy et al., 2009). However, to our knowledge, no studies to date have investigated self-criticism as a predictor of SI in BSDs.
The BSM proposes that negative self-appraisals such as self-criticism may work synergistically with other types of negative appraisals to lead to SI; however, these specific mechanisms of SI have neither been elaborated nor investigated empirically. One type of appraisal that could exacerbate the impact of self-criticism on SI is negative cognitive style. Negative cognitive style is derived from the hopelessness theory of depression, which proposes that individuals who are vulnerable to hopelessness (and depression) make attributions about the causes of negative events that are stable (always present) and global (affecting many areas of life), with negative consequences and self-implications (Abramson et al., 1989). In addition to empirical studies supporting the role of negative cognitive styles in depression (e.g., Alloy et al., 2006) and bipolar spectrum disorders (Alloy et al., 1999; Reilly-Harrington et al., 1999; Stange et al., 2013a, in press), research also has supported the role of negative cognitive style and hopelessness in the development of suicidal ideation (Kleiman et al., 2014a). Theoretical models of suicide (e.g., O’Connor, 2011), including the BSM, have suggested that making negative appraisals about the future following stressful life events may facilitate the progression of feelings of entrapment toward SI (Malhi et al., 2013). Indeed, studies have demonstrated that negative cognitive style confers vulnerability to the prospective development of SI (Joiner and Rudd, 1995; Kleiman et al., 2014b) via hopelessness (Abramson et al., 1998; Smith et al., 2006). Studies across the bipolar spectrum have suggested that negative cognitive styles are associated with a poorer course of illness (Alloy et al., 1999; Reilly-Harrington et al., 1999; Stange et al., 2013a). Only one study has evaluated negative cognitive style as a predictor of SI in individuals with bipolar I or II disorder, failing to find such a relationship (Stange et al., 2014), but hopelessness has been strongly implicated as a risk factor for SI and suicide attempts in BSDs (e.g., Umamaheswari et al., 2014; Valtonen et al., 2006). Although it seems plausible that negative cognitive styles would be particularly likely to lead to hopelessness and SI among individuals who also engage in self-criticism (as a result of feeling defeated, ineffective, and hopeless; Malhi et al., 2013), no research has integrated these risk factors in evaluating SI in BSDs.
Rumination, the tendency to repetitively think over the causes and consequences of one’s depressed mood (Nolen-Hoeksema, 1991), also may exacerbate the impact of self-critical thinking on SI. Indeed, theories of suicide (e.g., O’Connor, 2011) have suggested that rumination may facilitate the development of SI because of feelings of entrapment and defeat. Rumination has been linked to a greater lifetime depression frequency in bipolar I disorder (Gruber et al., 2011) as well as SI and behaviors (for review see Morrison and O’Connor, 2008; e.g., Smith et al., 2006) including in bipolar I and II disorders (Simon et al., 2007). The BSM proposes that impaired cognition and emotion regulation (such as rumination) may worsen the effect of negative appraisals of the self, such that SI is activated (Malhi et al., 2013). In line with this model, existing empirical research has shown that rumination exacerbates the associations between negative cognitive styles and depression in individuals at risk for BSDs (Stange et al., 2013b) and normative samples (Ciesla and Roberts, 2007; Robinson and Alloy, 2003). Thus, rumination also could exacerbate the link between self-criticism and SI, but no studies to date have evaluated this question.
Rumination has two subtypes: brooding, rumination in a passive form that is thought to be maladaptive and is associated with depression; and reflection, a more active form of rumination thought to be less maladaptive (Treynor et al., 2003). With respect to suicide, findings have been more mixed, with retrospective, cross-sectional, and prospective studies providing evidence that brooding and/or reflection each may be associated with SI and attempts (e.g., Chan et al., 2009; Grassia and Gibb, 2009; Miranda and Nolen-Hoeksema, 2007; Surrence et al., 2009). Thus, it is possible that both forms of rumination are maladaptive in conferring risk for SI. Researchers recently have called for studies to examine the conditions under which reflection predicts SI (Chan et al., 2009; Miranda and Nolen-Hoeksema, 2007; Surrence et al., 2009; Tucker et al., 2013). For example, Miranda and Nolen-Hoeksema (2007) proposed that reflection could lead to SI when individuals are not successful at generating solutions to their problems, which could occur when negative cognitive styles interfere with problem-solving. Similarly, Watkins (2008) proposed that abstract, analytical forms of repetitive thought such as brooding and reflection may be particularly maladaptive in the context of negative thinking or depressed mood. Thus, reflection and brooding could each be particularly likely to lead to SI when the content of the repetitive thinking is negative, such as among individuals who engage in self-criticism.
Although epidemiological and descriptive studies have evaluated risk factors for suicide among treatment-seeking individuals with bipolar I or II disorder, far fewer studies have evaluated risk factors for SI among individuals with less-severe disorders on the bipolar spectrum. This gap in the literature is notable given that individuals with less-severe BSDs are at high risk for transitioning to more severe types of BSDs (e.g., Akiskal et al., 1977; Alloy et al., 2012; Birmaher et al., 2009), with the potential for substantial economic and personal costs for society (Begley et al., 2001; Kessler et al., 2006, 2008; Simon, 2003).
In the present study, we evaluated self-criticism, negative cognitive style, brooding and reflection as predictors of SI in a prospective study of young adults with BSDs (bipolar II, bipolar NOS, and cyclothymia). Specifically, consistent with the BSM of suicidality, we evaluated whether negative cognitive style, brooding, and reflection would exacerbate the association between self-criticism and prospective SI across three years of follow-up.
2. Methods
2.1. Participants and Procedures
The present sample is derived from the Temple University site of the Longitudinal Investigation of Bipolar Spectrum Disorders (LIBS) Project, a prospective investigation of the biological, psychosocial, and cognitive predictors of bipolar spectrum disorders (BSD). Participants were Temple University undergraduates who were selected after a two-phase screening procedure. A total of 7,500 students were administered the revised General Behavior Inventory (GBI; Depue et al., 1989) in Phase I of screening. Employing GBI cutoffs for depressive and manic symptomatology (see below), 12.3% of those who completed Phase I screened into the potential BSD group.
Phase II of the screening involved administration of a semi-structured diagnostic interview using an expanded version of the Schedule for Affective Disorders and Schizophrenia – Lifetime interview (exp-SADS-L; Alloy et al., 2008). Inclusion criteria for the BSD group included meeting the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) (APA, 1994) and/or the Research Diagnostic Criteria (RDC) (Spitzer et al., 1978) criteria for any of the following disorders: bipolar II disorder, cyclothymia, or bipolar disorder NOS. Exclusion criteria for the BSD group included meeting for a current or past manic episode based on DSM-IV and/or RDC criteria, as a goal of the LIBS Project was to determine risk factors for the onset of bipolar I disorder (Alloy et al., 2012).
The sample included 72 participants (58% bipolar II, 42% cyclothymia or bipolar NOS). The sample was 65% female and the mean age was 19.72 years (SD= 1.85). Prior to study enrollment, 15% of the BSD group indicated seeking medication and/or psychotherapy treatment (Alloy et al., 2008). During study enrollment, 31% of the BSD group reported seeking treatment (16% medication-only, 13% psychotherapy-only) and 3% reported psychiatric hospitalization (Alloy et al., 2008).
The LIBS study was approved by Temple University’s IRB and informed consent was obtained from all participants who were screened and enrolled in the study. After screening Phases I and II, individuals were administered a baseline battery of self-report assessments measuring depressive symptoms, self-criticism, negative cognitive style, and rumination. Prospective suicidal ideation was measured by diagnostic interview every four months post-baseline visit over an average period of three years (M = 1099 days; SD= 464 days).
2.2. Measures
2.2.1. Screening Questionnaire
General Behavior Inventory (GBI; Depue et al., 1989). The GBI is a self-report measure administered at Phase I of screening to identify potential bipolar spectrum participants and controls to invite for Phase II screening. The GBI includes 73 items assessing depressive (GBI-D) and hypomanic/biphasic (GBI-HB) symptomatology as well as their frequency, intensity, and duration. Items are measured on a 4-point Likert scale, ranging from 1 (not at all) to 4 (very often or almost constantly). Based on scoring procedures employed by Depue and colleagues (1989), only scores of 3 or 4 on the Likert scales received a score of one point. Additional details about GBI cutoff scores for potential bipolar spectrum and healthy control participants are available elsewhere (Alloy et al., 2008; Depue et al., 1989). The GBI has high internal consistency (α = 0.90–0.96), good test-retest reliability (r = 0.71–0.74), good sensitivity (0.78), and high specificity (0.99) in detecting BSDs (Depue et al., 1981, 1989).
2.2.2. Bipolar Spectrum Diagnoses
Schedule for Affective Disorders and Schizophrenia – Lifetime version (SADS-L; Endicott and Spitzer, 1978). The SADS-L is a semi-structured diagnostic interview administered during Phase II of the screening process. The expanded version of the SADS-L assesses lifetime history of mood, anxiety, eating, psychotic, and substance use disorders (Alloy et al., 2008). The inter-rater reliability observed in our study was strong; an analysis of 105 jointly rated interviews yielded a kappa = 0.96 for bipolar spectrum diagnoses (Alloy et al., 2008).
2.2.3. Depressive Symptoms
The Beck Depression Inventory (BDI; Beck, Steer, and Garbin, 1988) is a 21-item self-report measure inquiring about a range of affective, motivational, cognitive, and somatic symptoms of depression. The BDI has strong psychometric support and has been validated in samples of college students (Bumberry et al., 1978; Hammen, 1980). After eligibility for the study was determined during Phases I and II, participants were administered the BDI at the baseline visit to assess current (prior two weeks) depressive symptoms. In the present study, the internal consistency was excellent (α = 0.94).
2.2.4. Negative Cognitive Style
The Cognitive Style Questionnaire (CSQ; Haeffel et al., 2008) was designed to assess inferential style in regards to negative events. Participants are presented with 12 negative events and are assessed on inferences regarding the cause of each hypothetical event’s (1) stability (“will never again cause [the event]” to “will also cause [the event] in the future”), (2) globality (“will only cause problems with [the event]” to “will cause problems in all areas of my life”), (3) the event’s likely consequences (“nothing bad will happen” to “very bad things will happen”), and (4) the event’s self-implications (“doesn’t mean anything is wrong with me” to “definitely means something is wrong with me”). Each item is rated on a 7-point Likert scale, with higher scores indicating a more negative cognitive style. In the present study, the internal consistency of the CSQ was excellent (α = 0.94).
2.2.5. Brooding and Reflection
The Ruminative Responses Scale (RRS; Treynor et al., 2003) is a 10-item self-report scale measuring to what degree participants react to feeling depressed by engaging in reflection (actively thinking about one’s mood in a reflective manner with an emphasis on problem solving) and brooding (thinking about one’s mood in a passive and judgmental manner; Treynor et al., 2003). The RRS includes 5 items measuring Reflection and 5 items measuring Brooding on a 4-point Likert scale (1= almost never, 4 = almost always). Both subscales have demonstrated retest reliability (r’s = 0.60, 0.62; Treynor et al., 2003) and good internal consistency (α’s = 0.72, 0.77; Treynor et al., 2003). In the present study, the Brooding (α = 0.74) and Reflection (α = 0.75) subscales yielded good internal consistency.
2.2.6. Self-criticism
The Depressive Experiences Questionnaire (DEQ; Blatt et al. 1976) is a scale designed to measure Blatt et al.’s (1976) proposed depressive cognitive styles. This study employed the self-criticism subscale because it has been found to be highly relevant to suicidal ideation and we were interested in elucidating this relationship as opposed to proposing additional relationships. The DEQ has demonstrated high internal and retest reliability (Blatt et al., 1976; Zuroff et al., 1983). In the present study, the self-criticism subscale demonstrated good internal consistency (α = 0.78).
2.2.7. Suicidal Ideation
Suicidal ideation was measured by the expanded Schedule for Affective Disorders – Change version (exp-SADS-C; Endicott and Spitzer, 1978; Alloy et al., 2008). The exp-SADS-C is a semi-structured diagnostic interview administered at all follow-up assessments throughout the study and is designed to track change in mood symptomatology, including the presence of suicidal ideation over the time period since the previous interview. The exp-SADS-C asks about thoughts about dying, wanting to die, killing oneself, or wanting to commit suicide. SI was coded dichotomously as 1 (yes) and 0 (no) for the presence of any suicidal ideation (Aiken and West, 1991). An analysis of 60 jointly rated interviews demonstrated strong inter-rater reliability (α = 0.80).
2.3. Statistical Analyses
To evaluate whether the association between self-criticism and SI was moderated by negative cognitive style, brooding, and reflection, we conducted three hierarchical logistic regressions. In Step 1, we entered Phase II symptoms of depression and the time participants were in the study (number of days from Time 1 to follow-up). The main effects of self-criticism and one of the cognitive styles (negative cognitive style, brooding, or reflection) was entered in Step 2, followed by the interaction term between self-criticism and the cognitive style in Step 3. Simple slopes tests were conducted for significant interactions by evaluating the association between self-criticism and SI at high and low levels (+/− 1 SD) of the cognitive style (Aiken and West, 1991).
3. Results
3.1. Preliminary Analyses
Descriptive statistics and correlations between study measures are presented in Table 1. Sixteen individuals (22%) experienced the onset of SI across follow-up. SI at follow-up was not significantly associated with any of the cognitive styles independently or with initial depressive symptoms. The cognitive styles were significantly positively correlated with each other, with the exception of reflection, which was not correlated with the other cognitive styles.
Table 1.
Descriptive Statistics and Correlations between Study Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Suicidal Ideation | -- | |||||
| 2. Depressive Symptoms (BDI)1 | 0.19 | -- | ||||
| 3. Self-Criticism (DEQ)2 | 0.17 | 0.24* | -- | |||
| 4. Negative Cognitive Style (CSQ)3 | 0.13 | 0.21 | 0.39*** | -- | ||
| 5. Brooding (RRS)4 | 0.11 | 0.05 | 0.60*** | 0.48*** | -- | |
| 6. Reflection (RRS) | 0.22 | 0.11 | 0.07 | 0.06 | 0.16 | -- |
| Mean | -- | 11.39 | 0.43 | 4.20 | 12.30 | 12.41 |
| SD | -- | 10.71 | 0.94 | 1.09 | 3.56 | 2.92 |
p< 0.05;
p < 0.01;
p < 0.001.
Beck Depression Inventory;
DEQ = Depressive Experiences Questionnaire;
CSQ = Cognitive Style Questionnaire;
RRS = Ruminative Response Scale.
3.2. Hypothesis 1: Does Negative Cognitive Style Amplify the Relationship between Self-Criticism and Onset of Suicidal Ideation?
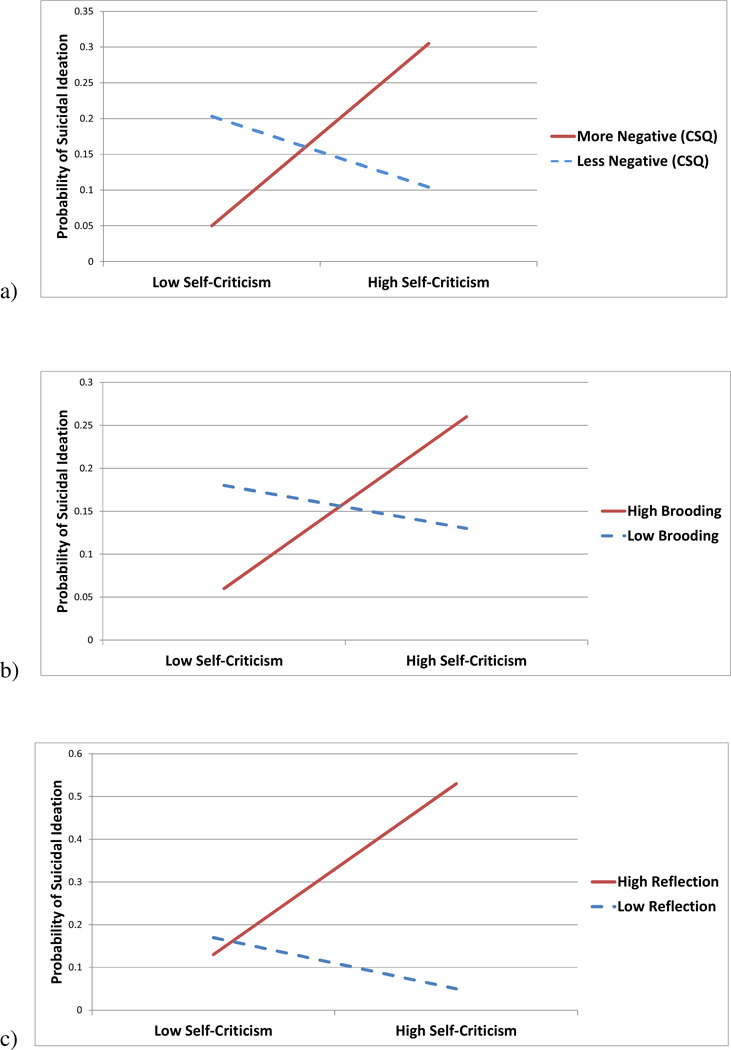
Self-criticism and negative cognitive style interacted significantly to predict the onset of SI (Table 2; Figure 1a). Consistent with hypotheses, self-criticism predicted a significantly greater likelihood of experiencing SI among individuals with higher levels of negative cognitive style (OR = 2.71, 95% CI= 1.01–7.42, p <0.05), but not among individuals with lower levels of negative cognitive style (OR = 0.63, 95% CI = 0.24–1.67, p = 0.35).
Table 2.
Interactions between Self-Criticism and Cognitive Styles Predicting Suicidal Ideation
| Step Variable | Wald | OR | 95% CI | ΔR2 |
|---|---|---|---|---|
| Negative Cognitive Style | ||||
| 1 BDI1 | 1.01 | 1.03 | 0.97–1.09 | 0.12 |
| Time in Study | 5.09 | 1.00* | 1.00–1.01 | |
| 2 Self-Criticism (SC) | 0.46 | 1.31 | 0.60–2.84 | 0.03 |
| Negative Cognitive Style (NCS) | 0.05 | 0.93 | 0.49–1.77 | |
| 3 SC x NCS | 5.38 | 1.96* | 1.11–3.45 | 0.12 |
| Brooding | ||||
| 1 BDI | 2.07 | 1.04 | 0.99–1.10 | 0.12 |
| Time in Study | 4.32 | 1.00* | 1.00–1.01 | |
| 2 Self-Criticism (SC) | 0.54 | 1.41 | 0.56–3.54 | 0.02 |
| Brooding | 0.05 | 0.97 | 0.77–1.23 | |
| 3 SC x Brooding | 3.63 | 1.17† | 1.00–1.37 | 0.07 |
| Reflection | ||||
| 1 BDI | 1.44 | 1.04 | 0.98–1.10 | 0.12 |
| Time in Study | 2.30 | 1.00 | 1.00–1.00 | |
| 2 Self-Criticism (SC) | 0.21 | 1.19† | 0.57–2.46 | 0.06 |
| Reflection | 2.76 | 1.25 | 0.96–1.62 | |
| 3 SC x Reflection | 4.95 | 1.36* | 1.04–1.77 | 0.10 |
p < 0.10;
p < 0.05.
BDI = Beck Depression Inventory.
Figure 1.
Interactions between Self-Criticism and (a) Negative Cognitive Style, (b) Brooding, and (c) Reflection, Predicting Probability of Suicidal Ideation.
3.3. Hypothesis 2: Does Rumination (Brooding or Reflection) Amplify the Relationship between Self-Criticism and Onset of Suicidal Ideation?
In contrast with our hypotheses, the interaction between self-criticism and brooding predicting the onset of SI was only marginally significant, but was in the hypothesized direction (Table 2; Figure 1b). However, self-criticism and reflection interacted significantly to predict the onset of SI (Table 2; Figure 1c). Consistent with hypotheses, self-criticism predicted a significantly greater likelihood of experiencing SI among individuals with higher levels of reflection (OR = 2.88, 95% CI = 1.02–8.12, p < 0.05), but not among individuals with lower levels of reflection (OR = 0.49, 95% CI = 0.16–1.47, p = 0.20).
Notably, all results remained consistent when controlling for lifetime history of SI.
4. Discussion
Individuals with bipolar spectrum disorders (BSDs) are at heightened risk for suicidal ideation and behaviors (e.g., Nock et al., 2009; Pompili et al., 2013); however, the psychosocial processes that confer risk for suicidal ideation among individuals with BSDs remain unclear. The present study extends research on self-criticism and suicidal ideation (O’Conner et al., 2007) by examining whether additional maladaptive cognitive processes amplified the effects of self-criticism on suicidal ideation in BSD individuals across a three-year follow-up period. Consistent with hypotheses, self-criticism predicted a greater likelihood of experiencing suicidal ideation among BSD individuals with more negative cognitive styles. In partial support of hypotheses, reflection, but not brooding, amplified the effects of self-criticism on suicidal ideation among BSD individuals. These findings highlight the detrimental and synergistic effects of self-criticism, negative cognitive style, and rumination on suicidal ideation and the importance of evaluating self-critical tendencies in interaction with other cognitive vulnerabilities for suicide risk among individuals with BSDs.
Although elevated levels of self-criticism have been found among suicidal individuals (O’Connor et al., 2007; Klomek et al., 2008), as well as individuals with BSDs (Nock et al., 2009), our findings suggest that the effects of self-criticism on suicidal ideation may be exacerbated by the presence of other cognitive processes. These findings are consistent with the theoretical framework of the Bipolar Suicidality Model (BSM; Mahli et al., 2013), which posits that individuals with BSDs are particularly vulnerable to making defeatist and hopelessness-inducing appraisals of life events and to perceive suicide as an escape from stressful events. In particular, BSD individuals tend to have higher levels of self-criticism (Fletcher et al., 2012), which includes negative self-representations that may interfere with their ability to cope with stressors (e.g., to manage emotions, acquire social support, problem-solve), and this may be further amplified by negative appraisals of stressful events or dysfunctional emotion regulation strategies.
This was one of the first studies to empirically evaluate aspects of the BSM and to find support for the synergistic associations between negative self-appraisals (i.e. self-criticism) and the tendency to make negative inferences regarding events’ causes, consequences, and meanings (i.e. negative cognitive style) in predicting suicidal ideation. It follows that individuals who are self-critical are more likely to have self-defeatist attitudes and view suicide as an escape (Fazaa and Page, 2003); however, these individuals might be especially likely to do so when they also attribute negative events to stable and global causes (e.g., “things will always be like this and will cause problems in other areas of my life”) with negative consequences and self-implications (e.g., “this means I’m worthless and I will always be miserable”). Thus, individuals who possess self-critical tendencies in conjunction with more negative cognitive styles may be most vulnerable to experiencing suicidal ideation, perhaps as a result of the negative appraisals of both the self and stressful events leading to greater perceptions of defeat.
Additionally, our finding that rumination exacerbates the effects of self-criticism on suicidal ideation is consistent with Mahli et al.’s (2013) BSM. For instance, individuals who are self-critical may be more likely to think about suicide if they have difficulty disengaging from a negative mood (and its possible consequences and meanings), which may amplify emotion dysregulation and increase suicidal thoughts. Further, in accordance with a cognitive catalyst model (Ciesla, Felton, and Roberts, 2011), negative cognitive content may be increased by rumination because it is persistently kept in mind. Thus, self-critical thoughts may be enhanced by the process of repetitive thought (e.g., Stange et al., 2013b), which may subsequently contribute to thoughts of suicide as an escape. Further, given research indicating that abstract and analytical repetitive thought, including brooding and reflection, may impair problem-solving and increase negative self-perceptions (Watkins, 2008), self-criticism may be amplified among individuals who ruminate, thereby leading to a greater likelihood of suicidal ideation.
Surprisingly, our results were only significant for reflection, which is typically considered to be a less maladaptive form of rumination (Treynor et al., 2003), but not for brooding. However, the negative impact of reflection on suicidal ideation is consistent with a growing body of research finding that reflection may be particularly likely to contribute to maladaptive outcomes, including depression and suicidal ideation, among individuals with other vulnerabilities (Chan et al., 2009; Ciesla et al., 2011; Miranda and Nolen-Hoeksema, 2007; Robinson and Alloy, 2003; Surrence et al., 2009; Tucker et al., 2013). Although reflection may be an innocuous process alone, our findings and those of prior studies suggest that reflection may contribute to a downward cognitive spiral among individuals who possess other negative processes (Ciesla et al., 2011; Surrence et al., 2009). In this sense, reflection may not be a uniformly adaptive cognitive response style to depressed mood, and may lead to suicidal ideation among individuals with certain vulnerabilities, such as self-criticism. Thus, among self-critical individuals, the cognitive content of the reflection might be negative, rendering reflection maladaptive and thereby increasing the likelihood of suicidal ideation.
Although we did not find a significant interaction between self-criticism and brooding predicting suicidal ideation, it is possible that limited statistical power prevented us from detecting such effects that actually exist. It is important to note that the interaction between brooding and self-criticism was trending in the expected direction, which is consistent with a number of prior studies that have found a significant influence of brooding on suicidal ideation (e.g., Chan et al., 2009; Miranda and Nolen-Hoeksema, 2007). Future research should further investigate whether the effects of brooding versus reflection depends on specific types of vulnerabilities and experiences (e.g., cognitive versus environmental) in conferring risk for suicidal ideation.
Given the high rates of suicidal ideation and attempts among BSD individuals (Pompili et al., 2013), this study potentially has important implications for the prevention and treatment of SI in BSDs. Our results suggest that evaluating cognitive styles, particularly in combination with one another, may improve our ability to detect BSD individuals at risk for suicidal ideation and suicide attempts. Additionally, our findings highlight the importance of incorporating cognitive elements in the treatment of individuals with bipolar spectrum disorders. Specifically, given that self-criticism is high among BSD individuals (Fletcher et al., 2012; Rosenfarb et al., 1998), it may be particularly important to target self-criticism to reduce the risk of suicidal ideation. However, our findings indicate that it also is important to target the presence of other cognitive vulnerabilities, such as negative cognitive style and repetitive thought processes, which might amplify the effects of self-criticism and contribute to suicidal ideation. Thus, treatments such as cognitive behavioral therapy that involve modifying maladaptive cognitions (Otto et al., 2009), or that involve teaching distanced approaches to noticing negative thoughts rather than engaging with them, such as mindfulness-based cognitive therapy (e.g., Deckersbach et al., 2012), might reduce the impact of self-criticism on negative outcomes such as SI.
Although the present study has several strengths, it is also important to note a number of limitations that will be important for future research to address. First, our sample was relatively small, which might have reduced our ability to detect the significant interaction with brooding and prevented us from having enough power to enter cognitive style interactions into regressions simultaneously. Second, the sample size precluded us from subdividing the sample into bipolar subgroups, which would have provided more information about the generalizability of our findings to different types of BSDs. Third, our study excluded individuals with manic episodes, which limits the extension of implications to individuals with bipolar I. Fourth, our study only evaluated suicidal ideation, but did not examine the severity of suicidal ideation (e.g., frequency, intention, plan) or suicide attempts, which also limits conclusions regarding the role of these synergistic cognitive styles on specific elements of suicidal ideation or suicide attempts in BSD individuals. However, given research documenting that suicidal ideation predicts attempted suicide in individuals with BSDs (Leverich et al., 2003), our study might be important for early detection and prevention of risk for suicide.
Fifth, the rate of suicidal ideation among BSD participants in our study was lower than anticipated. Normative data from a recent surveillance study of college students indicate that twelve percent of college students experienced SI across four years (Wilcox et al., 2010). Thus, although the 22% rate of SI observed in our sample of students with BSDs was lower than expected, this rate of SI is almost twice the normative rate and was obtained across a shorter period of follow-up. Given that SI is less likely to be reported in clinical interviews than in self-report measures (Kaplan et al., 1994), it is possible that SI was under-reported among participants in our study. However, SI also may be somewhat less common among individuals with less-severe bipolar spectrum disorders (e.g., Axelson et al., 2006) as is true for our sample. Thus, our results should be considered within the context of rates of SI that are lower than would be expected in treatment-seeking individuals with bipolar I and II disorders. It is possible that some effects tested (such as the brooding x self-criticism interaction) would be more easily detected in clinical samples with higher rates of SI, or if SI were self-reported.
Finally, the present study only evaluated these relationships within a sample of individuals with BSDs. Thus, it remains unclear whether these processes are specific to BSD individuals or whether they apply more broadly to other clinical or community samples. Given research supporting the cognitive catalyst model of depression in healthy individuals (Ciesla and Roberts, 2007; Ciesla et al., 2011; Robinson and Alloy, 2003), as well as individuals at risk for bipolar disorder (Stange et al., 2013b), it is possible that the effects of these cognitive processes would extend to other samples, but they might be especially acute in individuals with mood dysregulation problems. Future research is needed to replicate these findings in larger samples, which would enable separate examination of different subgroups of BSDs, as well as examination of the interaction of other cognitive styles and emotion regulation strategies in risk for suicidal ideation.
In conclusion, our findings indicate that the effects of self-criticism on suicidal ideation is amplified by both negative cognitive style and reflection, but not brooding, which have important implications for the prevention and treatment of BSD individuals at risk for suicide.
Highlights.
-
-
Suicide rates in bipolar disorders are high and self-criticism is a risk factor for suicidal ideation (SI)
-
-
We examined negative cognitive style and rumination as synergistic predictors of relationship between self-criticism and SI
-
-
Negative cognitive style and reflective rumination moderated self-criticism/SI relationship
-
-
Brooding rumination did not moderate this relationship
Acknowledgments
This work was supported by NIMH grants 52617 and 77908 to Lauren B. Alloy and 52662 to Lyn Y. Abramson. Jonathan P. Stange was supported by National Research Service Award F31MH099761 from NIMH. Jessica L. Hamilton was supported by National Research Service Award F31MH106184 from NIMH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Cornette M, Akhavan S, Chiara A. Suicidality and cognitive vulnerability to depression among college students: A prospective study. Journal of Adolescence. 1998;21(4):473–487. doi: 10.1006/jado.1998.0167. [DOI] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: a theory-based subtype of depression. Psychological Review. 1989;96(2):358–372. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. London: Sage Publication Inc; 1991. [Google Scholar]
- Akiskal HS, Djenderedjian AH, Rosenthal RH, Khani MK. Cyclothymic disorder: validating criteria for inclusion in the bipolar affective group. American Journal of Psychiatry. 1977;134:1227–1233. doi: 10.1176/ajp.134.11.1227. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Walshaw PD, Cogswell A, Grandin LD, Hughes ME, Hogan ME. Behavioral Approach System and Behavioral Inhibition System sensitivities and bipolar spectrum disorders: prospective prediction of bipolar mood episodes. Bipolar Disorders. 2008;10(2):310–322. doi: 10.1111/j.1399-5618.2007.00547.x. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Walshaw PD, Gerstein RK, Keyser JD, Whitehouse WG, Harmon-Jones E. Behavioral approach system (BAS)-relevant cognitive styles and bipolar spectrum disorders: Concurrent and prospective associations. Journal of Abnormal Psychology. 2009;118(3):459–471. doi: 10.1037/a0016604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2006;115(1):145–156. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Reilly-Harrington N, Fresco DM, Whitehouse WG, Zechmeister JS. Cognitive styles and life events in subsyndromal unipolar and bipolar disorders: Stability and prospective prediction of depressive and hypomanic mood swings. Journal of Cognitive Psychotherapy. 1999;13(1):21–40. [Google Scholar]
- Alloy LB, Urošević S, Abramson LY, Jager-Hyman S, Nusslock R, Whitehouse WG, Hogan M. Progression along the bipolar spectrum: A longitudinal study of predictors of conversion from bipolar spectrum conditions to bipolar I and II disorders. Journal of Abnormal Psychology. 2012;121(1):16–27. doi: 10.1037/a0023973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34–38 years. Journal of Affective Disorders. 2002;68(2):167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leornard H, Hunt J, Iyengar S, Bridge J, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Glenn CR, Lee HJ. Quantifying the impact of recent negative life events on suicide attempts. Journal of Abnormal Psychology. 2013;122(2):359–368. doi: 10.1037/a0030371. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Begley CE, Annegers JF, Swann AC, Lewis C, Coan S, Schnapp WB, Bryant-Comstock L. The lifetime cost of bipolar disorder in the US. Pharmacoeconomics. 2001;19(5):483–495. doi: 10.2165/00019053-200119050-00004. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito-Smythers C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorder: The course and outcome of bipolar youth (COBY) study. American Journal of Psychiatry. 2009;166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blatt SJ, D’Afflitti JP, Quinlan DM. Experiences of depression in normal young adults. Journal of Abnormal Psychology. 1976;85:383–389. doi: 10.1037//0021-843x.85.4.383. [DOI] [PubMed] [Google Scholar]
- Blatt SJ, Quinlan DM, Chevron ES, McDonald C, Zuroff D. Dependency and self-criticism: Psychological dimensions of depression. Journal of Consulting and Clinical Psychology. 1982;50:113–124. doi: 10.1037//0022-006x.50.1.113. [DOI] [PubMed] [Google Scholar]
- Bumberry W, Oliver JM, McClure JN. Validation of the Beck Depression Inventory in a university population using psychiatric estimate as the criterion. Journal of Consulting and Clinical Psychology. 1978;46(1):150. [Google Scholar]
- Chan S, Miranda R, Surrence K. Subtypes of rumination in the relationship between negative life events and suicidal ideation. Archives of Suicide Research. 2009;13(2):123–135. doi: 10.1080/13811110902835015. [DOI] [PubMed] [Google Scholar]
- Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other Axis I disorders. Biological Psychiatry. 1996;39(10):896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- Ciesla JA, Felton JW, Roberts JE. Testing the cognitive catalyst model of depression: Does rumination amplify the impact of cognitive diatheses in response to stress? Cognition and Emotion. 2011;25:1349–1357. doi: 10.1080/02699931.2010.543330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciesla JA, Roberts JE. Rumination, negative cognition, and their interactive effects on depressed mood. Emotion. 2007;7(3):555. doi: 10.1037/1528-3542.7.3.555. [DOI] [PubMed] [Google Scholar]
- Deckersbach T, Hölzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, Rauch SL, Lazar S, Nierenberg AA. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neuroscience and Therapeutics. 2012;18(2):133–141. doi: 10.1111/j.1755-5949.2011.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue RA, Krauss S, Spoont MR, Arbisi P. General Behavior Inventory identification of unipolar and bipolar affective conditions in a nonclinical university population. Journal of Abnormal Psychology. 1989;98(2):117. doi: 10.1037//0021-843x.98.2.117. [DOI] [PubMed] [Google Scholar]
- Depue RA, Slater JF, Wolfstetter-Kausch H, Klein D, Goplerud E, Farr D. A behavioral paradigm for identifying persons at risk for bipolar depressive disorder: a conceptual framework and five validation studies. Journal of Abnormal Psychology. 1981;90(5):381. doi: 10.1037//0021-843x.90.5.381. [DOI] [PubMed] [Google Scholar]
- Donaldson D, Spirito A, Farnett E. The role of perfectionism and depressive cognitions in understanding the hopelessness experienced by adolescent suicide attempters. Child Psychiatry and Human Development. 2000;31(2):99–111. doi: 10.1023/a:1001978625339. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry. 1978;35(7):837. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fazaa N, Page S. Dependency and Self-Criticism as Predictors of Suicidal Behavior. Suicide and Life Threatening Behavior. 2003;33(2):172–185. doi: 10.1521/suli.33.2.172.22777. [DOI] [PubMed] [Google Scholar]
- Fletcher K, Parker G, Barrett M, Synnott H, McCraw S. Temperament and personality in bipolar II disorder. Journal of Affective Disorders. 2012;136(3):304–309. doi: 10.1016/j.jad.2011.11.033. [DOI] [PubMed] [Google Scholar]
- Francis-Raniere EL, Alloy LB, Abramson LY. Depressive personality styles and bipolar spectrum disorders: Prospective tests of the event congruency hypothesis. Bipolar Disorders. 2006;8(4):382–399. doi: 10.1111/j.1399-5618.2006.00337.x. [DOI] [PubMed] [Google Scholar]
- Grassia M, Gibb BE. Rumination and lifetime history of suicide attempts. International Journal of Cognitive Therapy. 2009;2(4):400–406. doi: 10.1521/ijct.2009.2.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Eidelman P, Johnson SL, Smith B, Harvey AG. Hooked on a feeling: rumination about positive and negative emotion in inter-episode bipolar disorder. Journal of Abnormal Psychology. 2011;120(4):956–961. doi: 10.1037/a0023667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, Sinclair J, Harriss L. Suicide and attempted suicide in bipolar disorder: a systematic review of risk factors. Journal of Clinical Psychiatry. 2005;66(6):693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Gibb BE, Metalsky GI, Alloy LB, Abramson LY, Hankin BL, Joiner TE, Jr, Swendsen JD. Measuring cognitive vulnerability to depression: Development and validation of the cognitive style questionnaire. Clinical Psychology Review. 2008;28(5):824–836. doi: 10.1016/j.cpr.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen CL. Depression in college students: beyond the Beck Depression Inventory. Journal of Consulting and Clinical Psychology. 1980;48(1):126–128. doi: 10.1037//0022-006x.48.1.126. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Rudd MD. Negative attributional style for interpersonal events and the occurrence of severe interpersonal disruptions as predictors of self-reported suicidal ideation. Suicide and Life Threatening Behavior. 1995;25(2):297–304. [PubMed] [Google Scholar]
- Kaplan ML, Asnis GM, Sanderson WC, Keswani L, de Lecuona JM, Joseph S. Suicide assessment: Clinical interview vs. self-report. Journal of Clinical Psychology. 1994;50(2):294–298. doi: 10.1002/1097-4679(199403)50:2<294::aid-jclp2270500224>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Kessler R, Akiskal H, Ames M, Birnbaum H, Greenberg P, Jin R, Merikangas K, Simon G, Wang P. Prevalence and effects of mood disorders on work performance in a nationally representative sample of US workers. American Journal of Psychiatry. 2006;163(9):1561–1568. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Heeringa S, Lakoma M, Petukhova M, Rupp A, Schoenbaum M, Wang P, Zaslavsky A. Individual and societal effects of mental disorders on earnings in the United States: results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2008;165(6):703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Law KC, Anestis MD. Do theories of suicide play well together? Integrating components of the hopelessness and interpersonal psychological theories of suicide. Comprehensive Psychiatry. 2014b;55(3):431–438. doi: 10.1016/j.comppsych.2013.10.015. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Riskind JH, Stange JP, Hamilton JL, Alloy LB. Cognitive and interpersonal vulnerability to suicidal ideation: A weakest-link approach. Behavior Therapy. 2014a;45(6):778–790. doi: 10.1016/j.beth.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Depue RA, Slater JF. Cyclothymia in the adolescent offspring of parents with bipolar affective disorder. Journal of Abnormal Psychology. 1985;94(2):115. doi: 10.1037//0021-843x.94.2.115. [DOI] [PubMed] [Google Scholar]
- Klomek A, Orbach I, Sher L, Sommerfeld E, Diller R, Apter A, Zalsman G. Quality of depression among suicidal inpatient youth. Arch Suicide Res. 2008;12(2):133–140. doi: 10.1080/13811110701857160. [DOI] [PubMed] [Google Scholar]
- Leverich GS, Altshuler LL, Frye MA, Suppes T, Keck PE, Jr, McElroy SL, Denicoff KD. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. Journal of Clinical Psychiatry. 2003;64(5):506–515. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- Liu RT, Miller I. Life events and suicidal ideation and behavior: A systematic review. Clinical Psychology Review. 2014;34(3):181–192. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Bargh DM, Kuiper S, Coulston CM, Das P. Modeling bipolar disorder suicidality. Bipolar Disorders. 2013;15(5):559–574. doi: 10.1111/bdi.12093. [DOI] [PubMed] [Google Scholar]
- Miranda R, Nolen-Hoeksema S. Brooding and reflection: Rumination predicts suicidal deation at 1-year follow-up in a community sample. Behaviour Research and Therapy. 2007;45(12):3088–3095. doi: 10.1016/j.brat.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison R, O'Connor RC. A systematic review of the relationship between rumination and suicidality. Suicide and Life Threatening Behavior. 2008;38(5):523–538. doi: 10.1521/suli.2008.38.5.523. [DOI] [PubMed] [Google Scholar]
- Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Boston, MA: Harvard University Press; 1996. [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, Williams DR. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Medicine. 2009;6(8) doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100(4):569. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- O'Connor RC. The relations between perfectionism and suicidality: A systematic review. Suicide and Life Threatening Behavior. 2007;37(6):698–714. doi: 10.1521/suli.2007.37.6.698. [DOI] [PubMed] [Google Scholar]
- O'Connor RC. Towards an integrated motivational-volitional model of suicidal behaviour. In: O'Connor RC, Platt S, Gordon J, editors. International handbook of suicide prevention: Research, policy and practice. NY: John Wiley & Sons; 2011. pp. 181–198. [Google Scholar]
- Otto MW, Reilly-Harrington NA, Kogan JN, Henin A, Knauz RO, Sachs GS. Managing bipolar disorder: A cognitive-behavioral approach (Therapist guide) New York, NY: Oxford University Press; 2009. [Google Scholar]
- Peters AT, Peckham AD, Stange JP, Sylvia LG, Hansen NS, Salcedo S, Rauch SL, Nierenberg AA, Dougherty DD, Deckersbach T. Correlates of real world executive dysfunction in bipolar I disorder. Journal of Psychiatric Research. 2014;53:87–93. doi: 10.1016/j.jpsychires.2014.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M, Gonda X, Serafini G, Innamorati M, Sher L, Amore M, Girardi P. Epidemiology of suicide in bipolar disorders: A systematic review of the literature. Bipolar Disorders. 2013;15(5):457–490. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- Reilly-Harrington NA, Alloy LB, Fresco DM, Whitehouse WG. Cognitive styles and life events interact to predict bipolar and unipolar symptomatology. Journal of Abnormal Psychology. 1999;108(4):567–578. doi: 10.1037//0021-843x.108.4.567. [DOI] [PubMed] [Google Scholar]
- Robinson MS, Alloy LB. Negative cognitive styles and stress-reactive rumination interact to predict depression: A prospective study. Cognitive Therapy and Research. 2003;27(3):275–291. [Google Scholar]
- Rosenfarb IS, Becker J, Khan A, Mintz J. Dependency and self-criticism in bipolar and unipolar depressed women. British Journal of Clinical Psychology. 1998;37(4):409–414. doi: 10.1111/j.2044-8260.1998.tb01398.x. [DOI] [PubMed] [Google Scholar]
- Simon GE. Social and economic burden of mood disorders. Biological Psychiatry. 2003;54(3):208–215. doi: 10.1016/s0006-3223(03)00420-7. [DOI] [PubMed] [Google Scholar]
- Simon NM, Zalta AK, Otto MW, Ostacher MJ, Fischmann D, Chow CW, Pollack MH. The association of comorbid anxiety disorders with suicide attempts and suicidal ideation in outpatients with bipolar disorder. Journal of Psychiatric Research. 2007;41(3):255–264. doi: 10.1016/j.jpsychires.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Smith JM, Alloy LB, Abramson LY. Cognitive vulnerability to depression, rumination, hopelessness, and suicidal ideation: Multiple pathways to self-injurious thinking. Suicide and Life Threatening Behavior. 2006;36(4):443–454. doi: 10.1521/suli.2006.36.4.443. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria: rationale and reliability. Archives of General Psychiatry. 1978;35(6):773. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Stange JP, Boccia AS, Shapero BG, Molz AR, Flynn M, Matt LM, Abramson LY, Alloy LB. Emotion regulation characteristics and cognitive vulnerabilities interact to predict depressive symptoms in individuals at risk for bipolar disorder: A prospective behavioural high-risk study. Cognition and Emotion. 2013b;27(1):63–84. doi: 10.1080/02699931.2012.689758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Molz Adams AR, O’Garro-Moore J, Weiss RB, Ong ML, Walshaw PD, Abramson LY, Alloy LB. Extreme cognitions in bipolar spectrum disorders: Associations with personality disorder characteristics and risk for episode recurrence. Behavior Therapy. doi: 10.1016/j.beth.2014.09.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, Magalhaes PV, Miklowitz DJ, Otto MW, Frank E, Berk M, Nierenberg AA, Deckersbach T. Extreme attributions predict the course of bipolar depression: Results from the STEP-BD randomized controlled trial of psychosocial treatment. Journal of Clinical Psychiatry. 2013a;74(3):249–255. doi: 10.4088/JCP.12m08019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, Magalhães PV, Miklowitz DJ, Otto MW, Frank E, Berk M, Hansen NS, Dougherty DD, Nierenberg AA, Deckersbach T. Extreme attributions predict suicide ideation and attempts in bipolar disorder: Prospective data from STEP-BD. World Psychiatry. 2014;13(1):95–96. doi: 10.1002/wps.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surrence K, Miranda R, Marroquín BM, Chan S. Brooding and reflective rumination among suicide attempters: Cognitive vulnerability to suicidal ideation. Behaviour Research and Therapy. 2009;47(9):803–808. doi: 10.1016/j.brat.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]
- Tucker RP, Wingate LR, O'Keefe VM, Mills AC, Rasmussen K, Davidson CL, Grant DM. Rumination and suicidal ideation: The moderating roles of hope and optimism. Personality and Individual Differences. 2013;55(5):606–611. [Google Scholar]
- Umamaheswari V, Avasthi A, Grover S. Risk factors for suicidal ideations in patients with bipolar disorder. Bipolar Disorders. 2014;16(6):642–651. doi: 10.1111/bdi.12179. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Mantere O, Leppamaki S, Arvilommi P, Isometsa ET. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disorders. 2006;8:576–585. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- Valtonen H, Suominen K, Mantere O, Leppamaki S, Arvilommi P, Isometsa ET. Suicidal ideation and attempts in bipolar I and II disorders. Journal of Clinical Psychiatry. 2005;66(11):1456–1462. doi: 10.4088/jcp.v66n1116. [DOI] [PubMed] [Google Scholar]
- Watkins ER. Constructive and unconstructive repetitive thought. Psychological Bulletin. 2008;134(2):163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O'Grady KE. Prevalence and predictors of persistent suicide ideation, plans, and attempts during college. Journal of Affective Disorders. 2010;127(1):287–294. doi: 10.1016/j.jad.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuroff DC, Moskowitz DS, Wielgus MS, Powers TA, Franko DL. Construct validation of the dependency and self-criticism scales of the Depressive Experiences Questionnaire. Journal of Personality Research. 1983;17(2):226–241. [Google Scholar]