Abstract
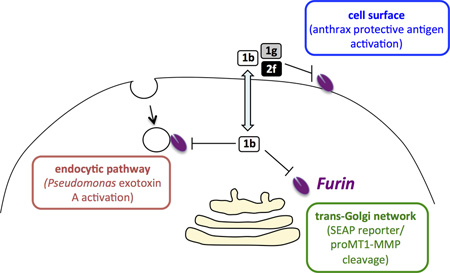
The proprotein convertase furin is implicated in a variety of pathogenic processes such as bacterial toxin activation, viral propagation, and cancer. Several groups have identified non-peptide compounds with high inhibitory potency against furin in vitro, although their efficacy in various cellbased assays is largely unknown. In this study we show that certain guanidinylated 2,5-dideoxystreptamine derivatives exhibit interesting ex vivo properties. Compound 1b (1,1'-(4-((2,4-diguanidino-5-(4-guanidinophenoxy)cyclohexyl)oxy)-1,3-phenylene)diguanidine) is a potent and cell-permeable inhibitor of cellular furin, since it was able to retard tumor cell migration, block release of a Golgi reporter, and protect cells against Bacillus anthracis (anthrax) and Pseudomonas aeruginosa intoxication, with no evident cell toxicity. Other compounds based on the 2,5-dideoxystreptamine scaffold, such as compound 1g (1,1'-(4,6-bis(4-guanidinophenoxy)cyclohexane-1,3-diyl)diguanidine) also efficiently protected cells against anthrax, but displayed only moderate protection against Pseudomonas exotoxin A and did not inhibit cell migration, suggesting poor cell permeability. Certain bisguanidinophenyl ether derivatives such as 2f (1,3-bis(2,4-diguanidinophenoxy) benzene) exhibited micromolar potency against furin in vitro, low cell toxicity, and highly efficient protection against anthrax toxin; this compound only slightly inhibited intracellular furin. Thus, compounds 1g and 2f both represent potent furin inhibitors at the cell surface with low intracellular inhibitory action, and these particular compounds might therefore be of preferred therapeutic interest in the treatment of certain bacterial and viral infections.
Keywords: Furin, Proprotein convertases, Furin inhibitors, Cell-based assays, Protease
Graphical Abstract
1. Introduction
The proprotein convertase (PC) furin is a calcium-dependent serine endoprotease with a neutral pH optimum that is widely distributed in mammalian cells and tissues. The furin protein, encoded by the PCSK3 gene, consists of four different domains: a prodomain, involved in folding and activation; a catalytic domain, which includes the catalytic triad Asp-His-Ser typical of all proprotein convertase family members; the homo B domain (also called the P domain), which is essential for enzyme activity and is known to contribute to enzymatic properties (calcium binding, pH dependence, and substrate specificity); and the C-terminal domain (for reviews see [1, 2]). Furin contains a C-terminal transmembrane domain/cytoplasmic tail within this latter domain, which enables this enzyme to bind cytoplasmic routing proteins and to cleave its substrates within three distinct subcellular compartments, the trans-Golgi network (TGN); the plasma membrane; and the endosomal compartment following its retrieval from the cell surface (reviewed in [3]). Due to this complex cellular itinerary, furin is capable of cleaving a wide range of precursor proteins within the constitutive secretory pathway. Some of the more notable substrates of furin include growth factors and receptors, serum proteins, extracellular matrix components, and protease precursors (e.g. matrix metalloproteinases) [4]. Furin typically processes precursor proteins at sites with the consensus sequence Arg-X-X-Arg, where the middle residues are also often basic residues; the most frequent site is Arg-X-Lys/Arg-Arg [1].
The furin knockout mouse dies early during embryonic development; death is thought to derive from an inability to produce correctly processed vital growth factors [5]. Furin is not, however, required for tissue viability after development, as tissue-specific knockout mice exist ([6]; reviewed in [7]), as do cell lines which do not express furin (e.g. LoVo; [8]). Furin activity contributes to numerous human pathological conditions such as Alzheimer’s disease, arthritis, atherosclerosis, and cancer [9–12]. Overexpression of human furin is correlated with increased carcinogenic potential [4, 13–15]. High furin activity is associated with increased proteolytic processing of the precursor to the membrane type 1-matrix metalloproteinase (MT1-MMP) [16] and insulin-like growth factor-1 (IGF1), as well as of the IGF1 receptor present on the surface of tumor cells [17]; these actions may explain the correlation of increased furin activity with carcinogenesis. Furthermore, host cell furin participates in the activation of many bacterial toxins, such as anthrax, diphtheria, Shiga and Pseudomonas aeruginosa toxins [18, 19] as well as in the activating cleavage of viral envelope glycoproteins necessary for the propagation of many viral pathogens including H5N1 avian influenza, human immunodeficiency, and Ebola viruses [20–22]. Because of its involvement in so many disease-related processes, furin has emerged as a potentially important drug target.
Therapeutic administration of furin inhibitors has been frequently proposed for the treatment of viral and pathogenic infections [23–25]. Additionally, inhibitors of furin and PACE4 (another member of the convertase family) have been used to reduce cancer cell invasiveness [26] and to block tumor growth in mice [17, 27–29]. A number of synthetic inhibitors against furin have been recently generated using the crystal structure of furin [30]. However, most prior studies of non-peptide furin inhibitors have been carried out in vitro, providing only limited information on the potency or toxicity of these compounds within cells. Interestingly, a series of non-peptide small molecules based on a 2,5-dideoxystreptamine scaffold was previously shown to potently inhibit furin in vitro [31]. In the work presented here, we have performed a systematic structure-activity relationship study of these 2,5-dideoxystreptamine derivatives using multiple cell-based assays, identifying the most potent, non-toxic, and compartment-selective inhibitors of cellular furin activity. In addition, we report novel bis-guanidinophenyl ether compounds with high inhibitory potency for furin in vitro; these inhibitors also exhibit low cellular toxicity and efficiently protect cells against anthrax and Pseudomonas toxemias.
2. Material and Methods
2.1. Compound synthesis
All of the compounds in the study were synthesized at Hawaii Biotech, Inc. (Aiea, HI). Compounds 1a–c, e–k, m, and p–r were prepared following the procedures described previously[31]. Compounds 2a–f (a, 1,3-bis(4-guanidinophenoxy)propane; b, cis-1,3-bis(4-guanidinophenoxy)cyclohexane; c, 1,3-bis(4-guanidinophenoxy)benzene; d, 1,3-bis(2,4-diguanidinophenoxy)propane; e, cis-1,3-bis(2,4-diguanidinophenoxy)cyclohexane; f. 1,3-bis(2,4-diguanidinophenoxy)benzene) were synthesized via reaction of 1,3-propanediol, cis-1,3-cyclohexanediol, or 1,3-benzenediol with 1-fluoro-4-nitrobenzene or 1-fluoro-2,4-dinitrobenzene, followed by hydrogenation, guanidination with N,N’-bis(tert-butoxycarbonyl)-N”-tirfluoromethanesulfonylguanidine, and deprotection with trifluoroacetic acid (Fig. 1).
Fig. 1.
Synthesis of bis-guanidinophenyl ether compounds 2a–f.
2.2. Enzyme assays and determination of IC50 values
Soluble human furin was purified from the conditioned medium of methotrexate-amplified, stably transfected CHO DG44 cells as previously described [32]. The furin assay was performed in 96-well polypropylene microtiter plates in a final volume of 100 µl, containing 100 mM HEPES, pH 7.0, 5 mM CaCl2, 0.1% Brij 35, 0.1% NaN3, and 0.1 mg/ml BSA. The substrate Pyr-Arg-Thr-Lys-Arg-4-methylcoumaryl-7-amide (pRTKR-MCA; Peptide Institute, Lexington, KY) was used at a final concentration of 100 µM. Furin was used at a final concentration of 15 nM. Reaction mixtures were incubated at 37°C and fluorescence measurements (380 nm excitation, 460 nm emission) were taken under kinetic conditions every minute for 60 min in a SpectraMax M2 microplate reader. For IC50 assays, serial dilutions of compounds were performed to give final concentrations between 100 nM and 250 µM in 50 µl. After a 30-min preincubation at room temperature, pRTKR-MCA was added, and residual enzyme activities were monitored by measuring aminomethylcoumarin fluorescence intensity. Data were analyzed using Prism 5 as described previously [33].
2.3. Enzyme kinetics
Studies of furin inhibition kinetics were carried out at various concentrations of pRTKR-MCA ranging from 0 to 200 µM in the presence and absence of inhibitors. For all kinetic measurements, the compounds were preincubated with enzyme for 30 min before the addition of substrate. All assays were performed in triplicate in 96-well microplates. Inhibition constants (Ki) were determined using the equation Ki = IC50/(1+([S]/Km)) [32, 34]. The Km value of furin used for this substrate was 8 µM, as described previously [35].
2.4. SEAP activity assays
CHO-GRAPfurin cells were obtained as a kind gift of Dr. A. Rehemtulla (University of Michigan). These cells, expressing the hybrid reporter protein GRAPfurin consisting of the secreted alkaline phosphatase (SEAP) protein fused to a Golgi retention signal via a specific furin recognition/cleavage site [36], were plated in 96-well plates and incubated with OptiMem containing 100 µM of either drug or vehicle for 16 to 20h. The medium was collected, centrifuged, and heated for 30 min at 65°C to inactivate endogenous alkaline phosphatases; SEAP activity remains unaffected after heating. Two and a half µl of heated medium sample were mixed with 100 µl of assay buffer (100 mM Tris-HCl, pH 10, 100 mM NaCl, 5 mM MgCl2) and 100 µl of 36 µM 4-methylumbelliferyl phosphate (MUP) in 50 mM Tris, pH 10. Fluorescence was measured by excitation at 365 nm and recording emission at 460 nm continuously during incubation at 37°C for 1 h. SEAP liberated from the furin reporter is secreted; thus, SEAP levels present in the medium are proportional to the activity of Golgi furin [26].
2.5. Cell migration assays
HT1080 fibrosarcoma cells (ATCC# CCL-121) were cultured to 80% confluence in growth medium (MEM with 2 mM L-glutamine, 10% FBS, 1:100 non-essential amino acids, 1 mM sodium pyruvate, 1% penicillin-streptomycin and 1% gentamicin). Cells were plated in Oris Cell Migration Assay (Platypus Technologies) plates (105 cells per well) following the manufacturer’s protocol. The next day, the growth medium was removed and the wells were rinsed with Dulbecco’s PBS (D-PBS; Ca++- and Mg++-free), and the cells were incubated in assay medium (MEM with 2 mM L-glutamine, 10% heat shocked FBS, 1:100 non-essential amino acids, 1 mM sodium pyruvate, 1% penicillin-streptomycin and 1% gentamicin) in the presence or absence of inhibitor for 20–24 h at 37°C and 5% CO2. After incubation the cells were rinsed with D-PBS (containing calcium and 20 mM HEPES), and incubated with the Live / Dead Cell Stain Kit containing 2 µM calcein AM and 4 µM ethidium homodimer (EthD-1) for 30 min at 37°C and 5% CO2. The fluorescence was measured at 485/528 nm excitation/emission for calcein AM, and 530/645 nm for EthD-1. The experiments were repeated independently 2–3 times for each inhibitor. The results are presented as the percentage of survival ± SD for the mean of all assays.
2.6. Pseudomonas exotoxin A assays
Chinese Hamster Ovary (CHO) DG44 cells were cultured to 80% confluence in growth medium (DMEM:F12 (1:1) with 2 mM L-glutamine, 10% FBS and 1% penicillin-streptomycin). CHO DG44 cells were seeded into microtiter plates (104 per well) and treated 24 h later with 50 ng/ml Pseudomonas aeruginosa exotoxin A (List Biologicals) in the presence or absence of 10 or 100 µM of inhibitor for 20–24 h at 37°C and 5% CO2. Cell viability was monitored by incubation for 2–4 h with the mitochondrial dye WST-1 (Roche). The experiments were repeated independently 3–5 times for the various sets of inhibitors, using triplicate wells each time. The results are presented as the percentage of survival ± SD for the mean of all assays.
2.7. Anthrax toxin assays
The effect of all compounds on anthrax toxemia was studied in the murine macrophage cell line RAW267.7. Cells were grown in RPMI medium with 10% fetal bovine serum, seeded into microtiter plates (104 per well), and treated 12 h later with 400 ng/ml protective antigen (PA) and 200 ng/ml lethal factor (LF) (List Biologicals) in the presence of either 10 or 100 µM of each inhibitor for a 2 h period. Inhibitors were added immediately following treatment of cells with PA + LF. Cell viability was monitored with WST-1. The experiments were repeated independently three times using triplicate wells. The results are presented as the percentage of survival ± SD from the mean of all assays.
2.8. Cytotoxicity assays
In order to assess the ability of each compound to affect cytotoxicity, a 24 h cytotoxicity assay was performed in CHO DG44, HT1080 and RAW267.7 cells using the mitochondrial dye WST-1. Cells were seeded in 96-well plates to achieve 50% confluence the next day, and then incubated with each compound or vehicle in triplicate. After incubation with inhibitors, cells were further incubated for 2–4 h with 10 µl of WST-1 reagent per well, and the absorbance was measured at 450 and 600 nm. To distinguish effects on cell proliferation from effects on cell viability, a 2 h cytotoxicity assay was performed in parallel (not shown). No differences were observed at these two periods of incubation. Independent experiments were performed on at least 3 occasions, with the results presented ± SD for the mean of all assays.
2.9. Molecular modeling
The atomic coordinates of furin were obtained from the X-ray structure of human furin in complex with the competitive inhibitor meta-guanidinomethyl-Phac-RVR-Amba [37] (PDB-entry 4OMC). Enzyme preparation was performed using the program “Molecular Operating Environment” (MOE version 2013). As a validation step, our docking of the co-crystalized ligand was able to closely reproduce the orientation and conformation reported in this X-ray crystal structure. First, each molecule was aligned to the co-crystalized ligand using the flexible alignment methodology implemented in MOE, and then the best alignment was selected for docking into the catalytic pocket.
3. Results
3.1. Structure-activity relationship studies of guanidinylated 2,5-dideoxystreptamine derivatives using cell-based assays
A previous study identified a series of non-peptide small molecules based on the 2,5-dideoxystreptamine scaffold which exhibited great inhibitory activity against furin in vitro [31]. However, in this study only limited data were reported on the cellular potencies of these compounds. Here we have tried to elucidate the structure-activity relationships of these 2,5-dideoxystreptamine derivatives using four different compartment-specific cell-based assays. Table 1 summarizes the cell-based assays and the cell lines used in this work: 1) CHO-GRAPfurin cell/SEAP assay to test furin cleavage within the trans-Golgi network (TGN); 2) HT1080 fibrosarcoma cell migration assay to test the furin-mediated activating cleavage of matrix metalloproteinases in the TGN; 3) CHO-DG44 cell/Pseudomonas exotoxin A assay to test furin activity in the endocytic pathway; and 4) RAW264.7 macrophage cell/anthrax assay to examine furin activity at the cell surface. In order to assess the general cytotoxicity of the compounds under study, control cytotoxicity experiments were also conducted in both CHO and HT1080 cells.
Table 1.
Cell-based assays and cell lines used to test furin activity within different cellular compartments. GRAP: Golgi-retained alkaline phosphatase; SEAP: secreted alkaline phosphatase; TGN: trans-Golgi network.
| SEAP activity | TGN | CHO-GRAPfurin |
| Cell migration | TGN | HT1080 |
| Pseudomonas exotoxin A | Endosomes | CHO DG44 |
| Anthrax | Cell surface | RAW264.7 |
For a better structural understanding, the 2,5-dideoxystreptamine compounds were divided into four structurally similar groups. Fig. 2 shows the structures, effects on cellular furin activity, and the cytotoxicity of a set of guanidinylated 2,5-dideoxystreptamine phenyl ether derivatives. The molecules 1a, 1b and 1g exhibited nanomolar potency against furin in vitro (Fig. 2A) and showed negligible toxicity either in CHO cells (Fig. 2B) or in HT1080 cells (data not shown) at 100 µM. However, only 1a and 1b were able to inhibit intracellular furin, as judged by the release of SEAP from Golgi stores by cleavage of the reporter at the furin consensus site (Fig. 2C). Both of these compounds were also good inhibitors of cell migration (Fig. 2D). Despite its high potency in vitro, compound 1g was unable to inhibit either TGN-associated furin or cell migration (Fig. 2C, 2D). Interestingly, compound 1b was capable of blocking both Pseudomonas and anthrax toxemia at low doses (Fig. 2E, 2F). Compound 1g also potently prevented anthrax toxicity (Fig. 2F). Considering its inability to block furin activity in the TGN, and its modest effect on furin activity in the endocytic pathway (as demonstrated by the Pseudomonas exotoxin A assays (Fig. 2E)), compound 1g might represent a good candidate for selective extracellular inhibition. On the other hand, compound 1h, whose main difference from 1a, 1b and 1g is the absence of guanidino groups at the para position, not only showed no or very weak furin inhibition in vitro and within cells, but also exhibited poor protection against bacterial toxins.
Fig. 2. Effect of guanidinylated 2,5-dideoxystreptamine phenyl ether derivatives 1a, 1b, 1g and 1h on cellular furin activity.
A) The chemical structures and Ki values of compounds 1a, 1b, 1g and 1h. Ki values were taken from the literature [31]. B) CHO cells were incubated with each compound at a final concentration of 100 µM for 24 h at 37°C, and cell viability was monitored by incubation for 2 h with WST-1. C) CHO-GRAPfurin cells, expressing Golgi-retained secreted alkaline phosphatase, was incubated with 100 µM of each inhibitor for 20–24 h at 37°C, and the SEAP activity was measured in the medium. D) Migration of HT1080 cells after incubation with 100 µM of each inhibitor for 24 h at 37°C. E) Protection from Pseudomonas aeruginosa exotoxin A cytotoxicity in CHO DG44 cells in the presence of 10 µM and 100 µM of each inhibitor for 20–24 h at 37°C. F) Protection from anthrax toxin cytotoxicity in RAW264.7 cells incubated in the presence of 10 µM and 100 µM of each inhibitor for 2 h at 37°C. Where no error bar is visible, errors were within the range of the data shown. Compounds showing zero inhibition lack data bars G = guanidino.
In an effort to determine whether modification of the ring structure affects assay selectivity, we assessed the effect of a set of guanidinylated 2,5-dideoxystreptamine pyridinyl ether analogs, the heterocyclic analogs of phenyl ether derivatives, on cellular furin activity (Fig. 3). While none of these compounds were toxic (Fig. 3B), in accord with their poor inhibitory potencies against furin in vitro (Fig. 3A), compounds 1m, 1j and 1k showed no or very weak inhibition of cellular furin (Fig. 3C–F). However, compound 1i exhibited near complete protection against Pseudomonas and anthrax toxins at 100 µM (Fig. 3E, 3F), the former action suggesting its effective uptake by endocytosis. Note that 1i possesses biological properties similar to those of 1g (e.g. protection against exotoxin A and anthrax toxin, and no inhibition of TGN-related furin activity), in agreement with its structural homology with this compound (Fig. 2A). These data indicate that the addition of a nitrogen atom to the aromatic ring at the ortho position improves the protective action against Pseudomonas toxin, but may lessen protection against anthrax toxin.
Fig. 3. Effect of guanidinylated 2,5-dideoxystreptamine pyridinyl ether derivatives 1i, 1m, 1j and 1k on cellular furin activity.
A) Chemical structures and Ki values (taken from [31]). B) CHO cells were incubated with each compound at 100 µM for 24 h at 37°C, and cell viability was monitored by incubation for 2 h with WST-1. C) Inhibition of SEAP secretion in the conditioned medium from CHO-GRAPfurin cells incubated with 100 µM of each inhibitor for 20–24 h at 37°C. D) Inhibition of migration of HT1080 cells after incubation with each inhibitor (100 µM) for 24 h at 37°C. E) Protection from Pseudomonas aeruginosa exotoxin A cytotoxicity in CHO DG44 cells in the presence of 10 µM and 100 µM of each inhibitor for 20–24 h at 37°C. F) Protection from anthrax toxin cytotoxicity in RAW264.7 cells incubated in the presence of 10 µM and 100 µM of each inhibitor for 2 h at 37°C.Where no error bar is visible, errors were within the range of the data shown. Compounds showing zero inhibition lack data bars G = guanidino.
As shown in Fig. 4, the analogs 1c, 1e and 1f, which possess increasing hydrophobicity via replacement of one or two phenyl groups by naphthyl groups, exhibited high in vitro potency against furin (Fig. 4A), although they were also moderately cytotoxic and showed poor inhibitory capacity against intracellular furin (Fig. 4B, 4C). Interestingly, compound 1f significantly inhibited cell migration, protected against Pseudomonas exotoxin A at low concentrations, and effectively blocked anthrax toxemia (Fig. 4D–F). By contrast, 1c was also able to inhibit migration (more efficiently than 1f), but did not protect against exotoxin A, and blocked anthrax toxicity less efficiently than 1f (Fig. 4E, 4F). Compound 1e, which differs from 1c by the absence of a guanidino group at the ortho position, did not possess any inhibitory effect on migration, but exhibited better protection against bacterial toxins (Fig. 4D–F). In general, however, despite their mild cytotoxicity (1c, 1e), compounds in this third set containing the more hydrophobic groups seem to specifically exhibit increased inhibitory potency on cell migration in comparison to similar, more polar, 2,5-dideoxystreptamine derivatives (Fig. 2D, 3D, and 4D).
Fig. 4. Effect of guanidinylated 2,5-dideoxystreptamine phenyl/naphthyl ether derivatives 1c, 1e and 1f on intracellular furin activity.
A) Chemical structures and Ki values (taken from [31]). B) General cytotoxicity. CHO cells were incubated with each compound at 100 µM for 24 h at 37°C, and cell viability was monitored by incubation for 2 h with WST-1. C) Inhibition of intracellular furin activity. CHO-GRAPfurin cells were incubated with 100 µM of each inhibitor for 20–24 h at 37°C, and SEAP activity was measured in the medium. D) Inhibition of migration of HT1080 cells during incubation of 100 µM of each inhibitor for 24 h at 37°C. E) Protection from cytotoxicity of Pseudomonas aeruginosa exotoxin A in CHO DG44 cells in the presence of 10 µM and 100 µM of each inhibitor for 20–24 h at 37°C. F) Protection from cytotoxicity of anthrax toxin in RAW264.7 cells incubated in the presence of 10 µM and 100 µM of each inhibitor for 2 h at 37°C. Where no error bars are visible, errors were within the range of the data shown. Compounds showing zero inhibition lack data bars G = guanidino.
The analogous carbamate compounds 1q and 1p (Fig. 5A), containing guanidino groups at the meta- and para-positions of the phenyl ring respectively, displayed micromolar potency against furin in vitro, but were moderately cytotoxic (1q, 1p) and, except for 1p, did not inhibit intracellular furin even at a concentration of 100 µM (Fig. 5C–D). The analog 1r, which includes guanidino groups at the ortho-position, was totally unable to inhibit furin, either in vitro or intracellularly. In comparison to 1q, the 1p analog was much less toxic (Fig. 5B), inhibited cell migration by almost 40% (Fig. 5D), and completely protected cells against Pseudomonas toxin (Fig. 5E). By contrast, this compound only poorly blocked anthrax toxemia (Fig. 5F). As evidenced by comparing compounds 1p and 1g (Fig. 2), the presence of the carbamate groups appears to decrease both the inhibitory capacity on furin in vitro and the protective effect against anthrax toxin at the cell surface. However, the carbamate groups likely improve cell permeability and/or uptake, as demonstrated by the superior inhibitory effects of this set of compounds on cell migration and on endosomal activation of exotoxin A at 100 µM.
Fig. 5. Effect of guanidinylated 2,5-dideoxystreptamine phenyl carbamate derivatives 1q, 1p and 1r on cellular furin activity.
A) Structures of carbamate derivatives and their Kis (taken from [31]). B) CHO cells were incubated with each compound at 100 µM for 24 h; cell viability was then monitored by incubation for 2 h using WST-1. C) Inhibition of SEAP activity secreted into the conditioned medium by CHO-GRAPfurin cells incubated with 100 µM of each inhibitor for 20–24 h. D) Inhibition of migration of HT1080 cells during incubation with 100 µM of each inhibitor for 24 h at 37°C. E) Protection from cytotoxicity of Pseudomonas aeruginosa exotoxin A in CHO DG44 cells in the presence of 10 µM or 100 µM of each inhibitor for 20–24 h. F) Protection from cytotoxicity of anthrax toxin in RAW264.7 cells incubated in the presence of 10 µM and 100 µM of each inhibitor for 2 h. Where no error bars are visible, errors were within the range of the data shown G = guanidino.
3.2. Inhibition of furin activity in vitro and ex vivo by bis-guanidinophenyl ether compounds
Given the limited inhibition of intracellular furin by guanidinylated 2,5-dideoxystreptamine derivatives, we designed and synthesized a series of compounds in which the guanidino phenyl groups were maintained (for maintaining potency against furin) but the middle linker- the polar 1,3-diguanidinocyclohexane group- was replaced by less polar groups, such as propane (compounds 2a and 2d), cyclohexane (compounds 2b and 2e), or benzene (compounds 2c and 2f), in order to observe whether the cellular activity could be improved. The synthesis of these compounds is described in detail in Fig. 1.
The efficacy of these new molecules in inhibiting furin in vitro was initially characterized by determining IC50 values [38] and further by obtaining Kis, as described in “Materials and Methods”. These data revealed that this series of bis-guanidinophenyl ether compounds inhibited furin in the micromolar range in vitro, substantially less potent than the guanidinylated 2,5-dideoxystreptamine derivatives (Fig. 6). The mechanism of inhibition was competitive (not shown). Interestingly, the addition of two guanidino groups to the phenyl ring improved the inhibitory potency 3–4 times (i.e. 2a vs 2d; 2b vs 2e; 2c vs 2f). The inhibitory potency of these compounds against furin was also dependent on the middle linker group, in the order of benzene > cyclohexane > propane (Fig. 6). Several dideoxystreptamine furin inhibitors- such as compound 1g- are known to exhibit substantial cross-inhibition with the proprotein convertases PC5 and PACE4 [31]. While these two enzymes were not available for testing, the bis-guanidinophenyl ether compounds did not inhibit PC2 even at 100 µM, and of compounds 2b to 2e, only 2d and 2e were found to inhibit PC1/3, and only at high concentrations (51% and 38% inhibition respectively at 100 µM, with no inhibition detected at 10 µM).
Fig. 6. Chemical structures of the bis-guanidinophenyl ether compounds tested as furin inhibitors.
2a: 1,3-bis(4-guanidinophenoxy) propane; 2b: 1,3-bis(4-guanidinophenoxy) cyclohexane; 2c: 1,3-bis(4-guanidinophenoxy) benzene; 2d: 1,3-bis(2,4-diguanidinophenoxy) propane; 2e: 1,3-bis(2,4-diguanidinophenoxy) cyclohexane; 2f: 1,3-bis(2,4-diguanidinophenoxy) benzene. Ki values were calculated as described in the “Materials and Methods” G = guanidino.
Excepting compound 2c, which was slightly toxic at 10 µM and highly toxic at 100 µM, the bis-guanidinophenyl ether compounds were not toxic at 10 µM, and only certain derivatives such as 2a, 2b and 2f showed slight or modest cell toxicity at 100 µM (Fig. 7A). The high cell toxicity of 2c may be due to the presence of the middle aromatic group. In fact, the addition of guanidino groups at the ortho-positions of the phenyl ring significantly alleviated toxicity (2c vs 2f). Fig. 7B shows that compounds 2a, 2b and 2c were able to inhibit 30–50% of cellular furin activity within the TGN, although these results were directly correlated with cytotoxicity and thus may not reflect actual furin inhibition. Compounds 2d, 2e and 2f inhibited only 10–15% of TGN-associated furin activity, suggesting poor entry into this compartment. All of these compounds were able to inhibit the migration of HT1080 fibrosarcoma cells, the most potent inhibitor being 2c (Fig. 7C). Again, however, this effect may be associated with cellular toxicity, since these cells were not viable after a 1-day incubation with 100 µM of this compound (data not shown). The remainder of these compounds effectively inhibited cellular migration, from around 40% (2a, 2b and 2d) to 20–25% (2e and 2f); since only limited cytotoxicity was seen, these compounds represent the second most effective compounds on cell migration, after 1a and 1c (60–70% protection).
Fig. 7. Cell-based assays for bis-guanidinophenyl ether compounds.
A) CHO cells were incubated with each compound at 10 µM and 100 µM for 24 h at 37°C, and cell viability was monitored by incubation for 2 h with WST-1. B) CHO-GRAPfurin cells were incubated with 100 µM of each inhibitor for 20–24 h at 37°C, and the SEAP activity was measured in the medium. C) Migration of HT1080 cells after incubation of 100 µM of each inhibitor for 24 h at 37°C. D) Cell toxicity of Pseudomonas aeruginosa exotoxin A in CHO DG44 cells in the presence of 10 µM and 100 µM of each inhibitor for 20–24 h at 37°C. E) Cytotoxicity of anthrax toxin in RAW264.7 cells incubated in the presence of 10 µM and 100 µM of each inhibitor for 2 h at 37°C.
In the endocytic pathway, compounds 2d, 2e and 2f exhibited good protection against Pseudomonas toxemia, increasing the cell viability to 40% in the case of 2f at 100 µM (Fig. 7D). All of these compounds, except 2c, also showed moderate protection against Pseudomonas exotoxin A at 10 µM, suggesting good uptake into the endosomal system. In agreement with the idea of poor cellular permeability into the TGN of CHO-GRAPfurin cells (Fig. 7B), compounds 2d, 2e and 2f exhibited potent cell activity at the cell surface, with excellent protection against anthrax toxicity at 100 µM inhibitor (Fig. 7E). Interestingly, inhibitor 2f showed almost complete protection at only 10 µM; it was also the most potent of this series in vitro (Ki = 0.4 µM; Fig. 6). Conversely, compound 2a was unable to block anthrax toxicity even at 100 µM, which is likely related to its intrinsically low potency in vitro towards furin (Ki = 8.3 µM, Fig. 6). These data are consistent with the idea that inhibitory potency against anthrax toxemia is most closely correlated with inhibition in in vitro assays.
3.3. Docking of 1,3-bis(2,4-diguanidinophenoxy) benzene (compound 2f) into the catalytic pocket of human furin
In previous studies [39] we emphasized the importance of positively charged groups in furin inhibitors. We also showed a possible binding orientation of 2,5-dideoxystreptamine derivatives into the furin, PC1/3, and PC2 binding sites [33]. Our previously reported binding model of 2,5-dideoxystreptamines into the PC1/3 catalytic site [33] showed a likely preferred orientation of the naphthyl group into the S1 pocket. In this orientation the guanidino group at the para position reaches deep into the S1 subsite, making favorable hydrogen bond interactions with the carbonyl oxygen atoms of Pro256 and Ala292.
An example of this binding pose for the novel compound 2f is shown in Fig. 8. This molecule is the most active amongst the analogous compounds shown in Fig. 6; a comparison with the co-crystallized ligand (guanidinomethyl-phenylacetyl-Arg-Val-Arg-(amidomethyl)-benzamidine (m-guanidinomethyl-Phac-RVR-Amba) [37] shows how compound 2f is able to nicely orient in a similar pose towards the S2, S3, and S4 sites. These subsites have been proposed to be relevant for achieving specificity in the recently published crystal structure of human furin [37]. In the orientation shown in Fig. 8, however, the S1 subsite is unoccupied. This could potentially represent the reason, at least in part, for the decreased inhibitory potency exhibited by this compound as compared to the submicromolar inhibition exhibited by other 2,5-dideoxystreptamine congeners such as compound 1e (assuming similar binding poses).
Fig. 8. Binding orientation of molecule 2f into the furin catalytic pocket.
Molecular surface representation of human furin; residues forming the catalytic triad and subsites S1–S4 are colored. Molecule 2f and the co-crystalized ligand [37] are shown as black and yellow stick representations, respectively.
4. Discussion
The proprotein convertase furin is known to act in various subcellular compartments including the TGN, the cell surface, and the endocytic compartment (reviewed in [3]). Despite the fact that the potency of inhibitors directed to furin action on the cell surface (for example the cleavage of the anthrax toxin PA) correlates well with in vitro inhibitor potency, inhibitory potency for previously published inhibitors in this cell-based assay is generally several orders of magnitude lower than that observed in the test tube [31, 32, 40–43]. This occurs most likely for reasons of inhibitor stability, very low in vivo substrate concentrations, and loss of inhibitor on cell surfaces. Inhibitor access to other subcellular compartments in which furin acts, such as the endosomes and TGN, is likely even more difficult, and the particular biophysical qualities which permit chemical transport across cell membranes or endocytic uptake are still poorly defined. Although reasonably clear structure-activity relationships which generally coincide with prior structural knowledge can be proposed for the 2,5-dideoxystreptamines described in this paper, the challenge of developing structure-activity relationship studies on in vivo data is evident. In the work discussed below, the varying ability of 2,5-dideoxystreptamine derivatives to modulate furin to different extents and to exhibit differing toxicity levels makes these compounds versatile for drug discovery efforts to begin to define compartment-specific furin inhibitors.
The involvement of proprotein convertases, especially furin, in various human pathologies is now well documented (reviewed in [44, 45]). For example, furin expression is elevated in certain kinds of tumors such as those derived from ovary, breast, head and neck, skin, brain and lung compared to normal adjacent tissue [15, 16, 46–49], and furin or furin-like activity contributes to tumor progression, aggressiveness, metastasis, and angiogenesis [27, 50, 51]; reviewed in [12]. Furin processing of substrates such as the metalloproteases stromelysin-3 and pro-membrane type-1 matrix metalloproteinase (proMT1-MMP) facilitates cell invasion and metastasis [14, 52]. In particular, the furin-mediated activation of proMT1-MMP primarily occurs within the TGN, and its mature form, MT1-MMP, is rapidly secreted into the extracellular space [53, 54] where it acts to degrade extracellular macromolecules (e.g. fibronectin, fibrin, vitronectin, laminin-1 and -5, and collagens) and adhesion molecules (e.g. CD44, integrins, and tissue transglutaminase). Furin-mediated activation of other MMPs such as gelatinase and collagenase 3 also contributes to the metastatic potential of tumor cells [14, 55, 56].
In agreement with the idea that convertase overexpression enhances metastasis, administration of peptide-based convertase inhibitors can limit tumor progression. While the non-selective irreversible convertase inhibitor dec-RVKR-CMK decreases skin tumor progression [57], this highly reactive compound exhibits significant cell toxicity [58]. The most potent peptide-based convertase inhibitors are likely the multi-Leu peptides developed by the Day group, which block viral infection [59] as well as tumor growth [28, 29, 60]; and the peptide analogs recently developed by the Steinmetzer group [25, 61] which potently inhibit bacterial toxin activation. However, because peptide-based drugs suffer from potential stability problems, several groups have instead sought small molecule inhibitors.
Many different kinds of small molecule drugs that act as competitive furin inhibitors and that are relatively specific for this enzyme have now been identified [26, 31, 43]. In a compound library screen, the cell-permeable naphthofluorescein disodium salt B3 prevented cell mobility and invasiveness of human fibrosarcoma HT1080 cells by inhibiting proMT1-MMP processing [26]. We found that the guanidinylated 2,5-dideoxystreptamine derivatives 1a and 1b strongly prevented the migration of HT1080 cells (by 60% and 35%, respectively), while showing no significant cell toxicity. Given that these compounds were also able to inhibit TGN furin in GRAPfurin CHO cells, compounds 1a and 1b might represent useful inhibitors to reduce cancer cell metastasis.
Other compounds based on the 2,5-dideoxystreptamine scaffold, including 1c, 1f and 1p, also displayed significant inhibition of cell migration (30–40%) with low general cytotoxicity. In contrast, while the bis-guanidinophenyl ether compounds 2a, 2b and 2c also inhibited migration, they were toxic at high doses. For example, 2c completely inhibited cell mobility, but probably solely as a consequence of a severe decrease in cell viability. In the case of 2d, 2e and 2f, we did not observe cytotoxicity, but these compounds only exhibited a modest 15–35% inhibition of HT1080 cell migration. Taken together, the guanidinylated 2,5-dideoxystreptamine derivatives constitute a promising group of compounds with therapeutic potential in cancer models, and should be subjected to further in vivo testing.
Proprotein convertase cleavages of bacterial and viral proteins are also essential for the pathogenicity of a number of bacteria and viruses [4, 45]. Furin therefore also represents an attractive target for the treatment of certain bacterial and viral infections. In fact, various peptide-based furin inhibitors have been used to block and/or delay anthrax toxemia both in cells and in live animals by inhibiting furin-catalyzed processing of the anthrax PA protein [32, 62, 63]. Additionally, furin has also emerged as a target for the prevention of the cytotoxic activation of Pseudomonas aeruginosa exotoxin A and Shiga toxin [25, 40, 59, 64]. Thus, the general convertase inhibitor nona-D-arginine peptide [65, 66] provides efficient topical treatment of severe corneal keratitis caused by Pseudomonas aeruginosa, particularly when combined with the antibiotic ciprofloxacin [67]. The present results show that the most promising small molecule compounds for the prevention of anthrax toxemia are likely the 2,5-dideoxystreptamine derivatives 1b and 1g, and the bis-guanidinophenyl ether compound 2f, all of which exhibited complete inhibition of anthrax toxicity at 10 µM, and none of which displayed significant cell toxicity at this concentration in a variety of cell lines. Compound 1b was also able to completely prevent Pseudomonas toxin cytotoxicity at this same dose. Since compound 1b also inhibited cell migration, this compound exhibits promise as a potent broad spectrum furin inhibitor for the treatment of furin-related pathologies. Other compounds, including 1i or 1p, also completely prevented Pseudomonas toxemia, but only at 100 µM; 1i was also capable of blocking anthrax toxicity at this same concentration. In general, the compounds based on the bis-guanidinophenyl ether scaffold (except 2a) potently inhibited anthrax toxin activation, and showed relatively good protection against Pseudomonas exotoxin A at 100 µM. Taking into account the lack of toxicity and cell permeability of compound 2f at low doses, its lack of effect on intracellular and endosomal furin, and its potent inhibition of furin at the cell surface, we suggest that this compound might be profitably exploited for selective protection against cell surface furin action (for example as occurs in anthrax infection) with potentially negligible side effects. However, direct evidence for the lack of cell penetrance of this molecule, as well as of other compounds such as 1g, should be confirmed in ex vivo studies using labeled compounds.
In conclusion, we have here elucidated interesting structure-activity relationships for each subgroup of inhibitors; while we could not determine universal molecular characteristics that control the cellular inhibitory activity in each specific compartment, i.e. the TGN, endosome, and cell surface, we have provided “proof of concept” that compartment selectivity of furin inhibitors can be addressed by fine-tuning of molecular structures. We suggest the use of the 2,5-dideoxystreptamine derivative 1b (1,1'-(4-((2,4-diguanidino-5-(4-guanidinophenoxy)cyclohexyl)oxy)-1,3-phenylene)diguanidine) as a general non-peptide small molecule furin inhibitor to combat cancer and/or infectious agents whose mode of action requires intracellular host furin activity. Additional studies in animals will be necessary to corroborate the efficacy of this promising compound. In addition, we have identified the compartment-selective compounds 1g and 2f for the treatment of pathogenic bacterial infections - such as Pseudomonas aeruginosa or Bacillus anthracis - with poor inhibitory capacity for intracellular furin. We suggest that further development of compartment-specific inhibitors in cell-based assays will be helpful to avoid potential side effects caused by the deregulation of normal furin activity and to rule out cytotoxic compounds.
Acknowledgements
We thank Dr. A. Rehemtulla for providing us with the GRAPfurin cell system, and NIH grant R01 DA05084-27 for support. We also thank John Giddens and Zephan Melville for performing preliminary studies of the Grap-furin and anthrax assays respectively.
Grant support KMM thanks Instituto de Quimica for financial support.
This work was supported by the National Institutes of Health Grant R01 DA05084-27.
Abbreviations
- AMC
7-amino-4-methylcoumarin
- CHO
Chinese hamster ovary
- ER
endoplasmic reticulum
- GRAP
Golgi-retained alkaline phosphatase
- LF
lethal factor
- MMP
matrix metalloproteinases
- PA
protective antigen
- PC
proprotein convertase
- pRTKR-MCA
Pyr-Arg-Thr-Lys-Arg-4-methylcoumaryl-7-amide
- SEAP
secreted alkaline phosphatase
- TGN
trans-Golgi network
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure of potential conflicts of interest
No potential conflicts of interest are present.
References
- 1.Nakayama K. Furin: a mammalian subtilisin/Kex2p-like endoprotease involved in processing of a wide variety of precursor proteins. Biochem J. 1997;327(Pt 3):625–635. doi: 10.1042/bj3270625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seidah NG. The proprotein convertases, 20 years later. Methods Mol Biol. 2011;768:23–57. doi: 10.1007/978-1-61779-204-5_3. [DOI] [PubMed] [Google Scholar]
- 3.Molloy SS, Anderson ED, Jean F, Thomas G. Bi-cycling the furin pathway: from TGN localization to pathogen activation and embryogenesis. Trends Cell Biol. 1999;9:28–35. doi: 10.1016/s0962-8924(98)01382-8. [DOI] [PubMed] [Google Scholar]
- 4.Thomas G. Furin at the cutting edge: from protein traffic to embryogenesis and disease. Nat Rev Mol Cell Biol. 2002;3:753–766. doi: 10.1038/nrm934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roebroek AJ, Umans L, Pauli IG, Robertson EJ, van Leuven F, Van de Ven WJ, et al. Failure of ventral closure and axial rotation in embryos lacking the proprotein convertase Furin. Development. 1998;125:4863–4876. doi: 10.1242/dev.125.24.4863. [DOI] [PubMed] [Google Scholar]
- 6.Roebroek AJ, Taylor NA, Louagie E, Pauli I, Smeijers L, Snellinx A, et al. Limited redundancy of the proprotein convertase furin in mouse liver. J Biol Chem. 2004;279:53442–53450. doi: 10.1074/jbc.M407152200. [DOI] [PubMed] [Google Scholar]
- 7.Creemers JW, Khatib AM. Knock-out mouse models of proprotein convertases: unique functions or redundancy? Front Biosci. 2008;13:4960–4971. doi: 10.2741/3055. [DOI] [PubMed] [Google Scholar]
- 8.Takahashi S, Kasai K, Hatsuzawa K, Kitamura N, Misumi Y, Ikehara Y, et al. A mutation of furin causes the lack of precursor-processing activity in human colon carcinoma LoVo cells. Biochem Biophys Res Commun. 1993;195:1019–1026. doi: 10.1006/bbrc.1993.2146. [DOI] [PubMed] [Google Scholar]
- 9.Bennett BD, Denis P, Haniu M, Teplow DB, Kahn S, Louis JC, et al. A Furin-like Convertase Mediates Propeptide Cleavage of BACE, the Alzheimer's β-Secretase. J Biol Chem. 2000;275:37712–37717. doi: 10.1074/jbc.M005339200. [DOI] [PubMed] [Google Scholar]
- 10.Arner EC. Aggrecanase-mediated cartilage degradation. Curr Opin Pharmacol. 2002;2:322–329. doi: 10.1016/s1471-4892(02)00148-0. [DOI] [PubMed] [Google Scholar]
- 11.Stawowy P, Meyborg H, Stibenz D, Borges Pereira Stawowy N, Roser M, Thanabalasingam U, et al. Furin-like proprotein convertases are central regulators of the membrane type matrix metalloproteinase-pro-matrix metalloproteinase-2 proteolytic cascade in atherosclerosis. Circulation. 2005;111:2820–2827. doi: 10.1161/CIRCULATIONAHA.104.502617. [DOI] [PubMed] [Google Scholar]
- 12.Bassi DE, Fu J, Lopez De Cicco R, Klein-Szanto AJ. Proprotein convertases: "master switches" in the regulation of tumor growth and progression. Mol Carcinog. 2005;44:151–161. doi: 10.1002/mc.20134. [DOI] [PubMed] [Google Scholar]
- 13.Mbikay M, Sirois F, Yao J, Seidah NG, Chretien M. Comparative analysis of expression of the proprotein convertases furin, PACE4, PC1 and PC2 in human lung tumours. Br J Cancer. 1997;75:1509–1514. doi: 10.1038/bjc.1997.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bassi DE, Mahloogi H, Klein-Szanto AJ. The proprotein convertases furin and PACE4 play a significant role in tumor progression. Mol Carcinog. 2000;28:63–69. [PubMed] [Google Scholar]
- 15.Fu J, Bassi DE, Zhang J, Li T, Nicolas E, Klein-Szanto AJ. Transgenic overexpression of the proprotein convertase furin enhances skin tumor growth. Neoplasia. 2012;14:271–282. doi: 10.1593/neo.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bassi DE, Mahloogi H, Al-Saleem L, Lopez De Cicco R, Ridge JA, Klein-Szanto AJ. Elevated furin expression in aggressive human head and neck tumors and tumor cell lines. Mol Carcinog. 2001;31:224–232. doi: 10.1002/mc.1057. [DOI] [PubMed] [Google Scholar]
- 17.Khatib AM, Siegfried G, Prat A, Luis J, Chrétien M, Metrakos P, et al. Inhibition of proprotein convertases is associated with loss of growth and tumorigenicity of HT-29 human colon carcinoma cells: importance of insulin-like growth factor-1 (IGF-1) receptor processing in IGF-1-mediated functions. J Biol Chem. 2001;27:30686–30693. doi: 10.1074/jbc.M101725200. [DOI] [PubMed] [Google Scholar]
- 18.Gordon VM, Klimpel KR, Arora N, Henderson MA, Leppla SH. Proteolytic activation of bacterial toxins by eukaryotic cells is performed by furin and by additional cellular proteases. Infect Immun. 1995;63:82–87. doi: 10.1128/iai.63.1.82-87.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garred O, van Deurs B, Sandvig K. Furin-induced cleavage and activation of shiga toxin. J Biol Chem. 1995;270:10817–10821. doi: 10.1074/jbc.270.18.10817. [DOI] [PubMed] [Google Scholar]
- 20.Basak A, Zhong M, Munzer JS, Chretien M, Seidah NG. Implication of the proprotein convertases furin, PC5 and PC7 in the cleavage of surface glycoproteins of Hong Kong, Ebola and respiratory syncytial viruses: a comparative analysis with fluorogenic peptides. Biochem J. 2001;353:537–545. doi: 10.1042/0264-6021:3530537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moulard M, Decroly E. Maturation of HIV envelope glycoprotein precursors by cellular endoproteases. Biochim Biophys Acta. 2000;1469:121–132. doi: 10.1016/s0304-4157(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 22.Volchkov V, Feldmann H, Volchkova VA, Klenk HD. Processing of the Ebola virus glycoprotein by proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komiyama T, Swanson JA, Fuller RS. Protection from anthrax toxin-mediated killing of macrophages by the combined effects of furin inhibitors and chloroquine. Antimicrob Agents Chemother. 2005;49(9):3875–3882. doi: 10.1128/AAC.49.9.3875-3882.2005. 3875–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ozden S, Lucas-Hourani M, Ceccaldi PE, Basak A, Valentine M, Benjannet S, et al. Inhibition of Chikungunya virus infection in cultured human muscle cells by furin inhibitors: impairment of the maturation of the E2 surface glycoprotein. J Biol Chem. 2008;283:21899–21908. doi: 10.1074/jbc.M802444200. [DOI] [PubMed] [Google Scholar]
- 25.Becker GL, Lu Y, Hardes K, Strehlow B, Levesque C, Lindberg I, et al. Highly potent inhibitors of proprotein convertase furin as potential drugs for treatment of infectious diseases. J Biol Chem. 2012;287:21992–22003. doi: 10.1074/jbc.M111.332643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coppola JM, Bhojani MS, Ross BD, Rehemtulla A. A small-molecule furin inhibitor inhibits cancer cell motility and invasiveness. Neoplasia. 2008;10:363–370. doi: 10.1593/neo.08166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bassi D, Lopez de Cicco R, Mahloogi H, Zucker S, Thomas G, Klein-Szanto J. Furin inhibition results in absent or decreased invasiveness and tumorigenicity of human cancer cells. PNAS. 2001;98:10326–10331. doi: 10.1073/pnas.191199198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D'Anjou F, Couture F, Desjardins R, Day R. Knockdown strategies for the study of proprotein convertases and proliferation in prostate cancer cells. Methods Mol Biol. 2014;1103:67–82. doi: 10.1007/978-1-62703-730-3_6. [DOI] [PubMed] [Google Scholar]
- 29.Longuespee R, Couture F, Levesque C, Kwiatkowska A, Desjardins R, Gagnon S, et al. Implications of Proprotein Convertases in Ovarian Cancer Cell Proliferation and Tumor Progression: Insights for PACE4 as a Therapeutic Target. Transl Oncol. 2014 doi: 10.1016/j.tranon.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fugere M, Day R. Cutting back on pro-protein convertases: the latest approaches to pharmacological inhibition. Trends Pharmacol Sci. 2005;26:294–301. doi: 10.1016/j.tips.2005.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiao GS, Cregar L, Wang J, Millis SZ, Tang C, O'Malley S, et al. Synthetic small molecule furin inhibitors derived from 2,5-dideoxystreptamine. Proc Natl Acad Sci U S A. 2006;103:19707–19712. doi: 10.1073/pnas.0606555104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kacprzak MM, Peinado JR, Than ME, Appel J, Henrich S, Lipkind G, et al. Inhibition of furin by polyarginine-containing peptides: nanomolar inhibition by nona-D-arginine. J Biol Chem. 2004;279:36788–36794. doi: 10.1074/jbc.M400484200. [DOI] [PubMed] [Google Scholar]
- 33.Vivoli M, Caulfield TR, Martinez-Mayorga K, Johnson AT, Jiao GS, Lindberg I. Inhibition of prohormone convertases PC1/3 and PC2 by 2,5-dideoxystreptamine derivatives. Mol Pharmacol. 2012;81:440–454. doi: 10.1124/mol.111.077040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Apletalina E, Appel J, Lamango NS, Houghten RA, Lindberg I. Identification of inhibitors of prohormone convertases 1 and 2 using a peptide combinatorial library. J Biol Chem. 1998;273:26589–26595. doi: 10.1074/jbc.273.41.26589. [DOI] [PubMed] [Google Scholar]
- 35.Cameron A, Fortenberry Y, Lindberg I. The SAAS granin exhibits structural and functional homology to 7B2 and contains a highly potent hexapeptide inhibitor of PC1. FEBS Lett. 2000;473:135–138. doi: 10.1016/s0014-5793(00)01511-8. [DOI] [PubMed] [Google Scholar]
- 36.Coppola JM, Hamilton CA, Bhojani MS, Larsen MJ, Ross BD, Rehemtulla A. Identification of inhibitors using a cell-based assay for monitoring Golgi-resident protease activity. Anal Biochem. 2007;364:19–29. doi: 10.1016/j.ab.2007.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dahms SO, Hardes K, Becker GL, Steinmetzer T, Brandstetter H, Than ME. X-ray Structures of Human Furin in Complex with Competitive Inhibitors. ACS Chem Biol. 2014 doi: 10.1021/cb500087x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Motulsky HJ, Christopoulos A. Fitting Models to Biological Data using Linear and Nonlinear Regression: a pratical guide to curve fitting. San Diego, CA: GraphPad Software Inc.; 2003. [Google Scholar]
- 39.Lopez-Vallejo F, Martinez-Mayorga K. Furin inhibitors: Importance of the positive formal charge and beyond. Bioorg Med Chem. 2012;20:4462–4471. doi: 10.1016/j.bmc.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 40.Jean F, Stella K, Thomas L, Liu G, Xiang Y, Reason AJ, et al. alpha1-Antitrypsin Portland, a bioengineered serpin highly selective for furin: application as an antipathogenic agent. Proc Natl Acad Sci U S A. 1998;95:7293–7298. doi: 10.1073/pnas.95.13.7293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiao GS, Cregar L, Goldman ME, Millis SZ, Tang C. Guanidinylated 2,5-dideoxystreptamine derivatives as anthrax lethal factor inhibitors. Bioorg Med Chem Lett. 2006;16:1527–1531. doi: 10.1016/j.bmcl.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 42.Peinado JR, Kacprzak MM, Leppla SH, Lindberg I. Cross-inhibition between furin and lethal factor inhibitors. Biochem Biophys Res Commun. 2004;321:601–605. doi: 10.1016/j.bbrc.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 43.Komiyama T, Coppola JM, Larsen MJ, van Dort ME, Ross BD, Day R, et al. Inhibition of furin/proprotein convertase-catalyzed surface and intracellular processing by small molecules. J Biol Chem. 2009;284:15729–15738. doi: 10.1074/jbc.M901540200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seidah NG, Prat A. The biology and therapeutic targeting of the proprotein convertases. Nat Rev Drug Discov. 2012;11:367–383. doi: 10.1038/nrd3699. [DOI] [PubMed] [Google Scholar]
- 45.Couture F, D'Anjou F, Day R. On the cutting edge of proprotein convertase pharmacology: from molecular concepts to clinical applications. Biomol Concepts. 2011;2:421–438. doi: 10.1515/bmc.2011.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Page RE, Klein-Szanto AJ, Litwin S, Nicolas E, Al-Jumaily R, Alexander P, Godwin AK, et al. Increased expression of the pro-protein convertase furin predicts decreased survival in ovarian cancer. Cell Oncol. 2007;29:289–299. doi: 10.1155/2007/930321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng M, Watson PH, Paterson JA, Seidah N, Chretien M, Shiu RP. Pro-protein convertase gene expression in human breast cancer. Int J Cancer. 1997;71:966–971. doi: 10.1002/(sici)1097-0215(19970611)71:6<966::aid-ijc10>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 48.Mercapide J, Lopez De Cicco R, Bassi DE, Castresana JS, Thomas G, Klein-Szanto AJ. Inhibition of furin-mediated processing results in suppression of astrocytoma cell growth and invasiveness. Clin Cancer Res. 2002;8:1740–1746. [PubMed] [Google Scholar]
- 49.Schalken JA, Roebroek AJ, Oomen PP, Wagenaar SS, Debruyne FM, Bloemers HP, et al. fur gene expression as a discriminating marker for small cell and nonsmall cell lung carcinomas. J Clin Invest. 1987;80:1545–1549. doi: 10.1172/JCI113240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Siegfried G, Basak A, Cromlish JA, Benjannet S, Marcinkiewicz J, Chretien M, et al. The secretory proprotein convertases furin, PC5, and PC7 activate VEGF-C to induce tumorigenesis. J Clin Invest. 2003;111:1723–1732. doi: 10.1172/JCI17220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McColl BK, Paavonen K, Karnezis T, Harris NC, Davydova N, Rothacker J, et al. Proprotein convertases promote processing of VEGF-D, a critical step for binding the angiogenic receptor VEGFR-2. FASEB J. 2007;21:1088–1098. doi: 10.1096/fj.06-7060com. [DOI] [PubMed] [Google Scholar]
- 52.Sato H, Kinoshita TTT, Nakayama K, Seiki M. Activation of a recombinant membrane type 1-matrix metalloproteinase (MT1-MMP) by furin and its interaction with tissue inhibitor of metalloproteinases (TIMP)-2. FEBS Lett. 1996;393:101–104. doi: 10.1016/0014-5793(96)00861-7. [DOI] [PubMed] [Google Scholar]
- 53.Cao J, Rehemtulla A, Bahou W, Zucker S. Membrane type matrix metalloproteinase 1 activates pro-gelatinase A without furin cleavage of the N-terminal domain. J Biol Chem. 1996;271:30174–30180. doi: 10.1074/jbc.271.47.30174. [DOI] [PubMed] [Google Scholar]
- 54.Mazzone M, Baldassarre M, Beznoussenko G, Giacchetti G, Cao J, Zucker S, et al. Intracellular processing and activation of membrane type 1 matrix metalloprotease depends on its partitioning into lipid domains. J Cell Sci. 2004;117:6275–6287. doi: 10.1242/jcs.01563. [DOI] [PubMed] [Google Scholar]
- 55.Yana I, Weiss SJ. Regulation of membrane type-1 matrix metalloproteinase activation by proprotein convertases. Mol Biol Cell. 2000;11:2387–2401. doi: 10.1091/mbc.11.7.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Seiki M. Membrane-type 1 matrix metalloproteinase: a key enzyme for tumor invasion. Cancer Lett. 2003;194:1–11. doi: 10.1016/s0304-3835(02)00699-7. [DOI] [PubMed] [Google Scholar]
- 57.Bassi DE, Zhang J, Cenna J, Litwin S, Cukierman E, Klein-Szanto AJ. Proprotein convertase inhibition results in decreased skin cell proliferation, tumorigenesis, and metastasis. Neoplasia. 2010;12:516–526. doi: 10.1593/neo.92030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Remacle AG, Gawlik K, Golubkov VS, Cadwell GW, Liddington RC, Cieplak P, et al. Selective and potent furin inhibitors protect cells from anthrax without significant toxicity. Int J Biochem Cell Biol. 2010;42:987–995. doi: 10.1016/j.biocel.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gagnon H, Beauchemin S, Kwiatkowska A, Couture F, D'Anjou F, Levesque C, et al. Optimization of furin inhibitors to protect against the activation of influenza hemagglutinin H5 and Shiga toxin. J Med Chem. 2014;57:29–41. doi: 10.1021/jm400633d. [DOI] [PubMed] [Google Scholar]
- 60.Kwiatkowska A, Couture F, Levesque C, Ly K, Desjardins R, Beauchemin S, et al. Design, synthesis, and structure-activity relationship studies of a potent PACE4 inhibitor. J Med Chem. 2014;57:98–109. doi: 10.1021/jm401457n. [DOI] [PubMed] [Google Scholar]
- 61.Becker GL, Sielaff F, Than ME, Lindberg I, Routhier S, Day R, et al. Potent inhibitors of furin and furin-like proprotein convertases containing decarboxylated P1 arginine mimetics. J Med Chem. 2010;53:1067–1075. doi: 10.1021/jm9012455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sarac MS, Peinado JR, Leppla SH, Lindberg I. Protection against anthrax toxemia by hexa-D-arginine in vitro and in vivo. Infect Immun. 2004;72:602–605. doi: 10.1128/IAI.72.1.602-605.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Molloy SS, Bresnahan PA, Leppla SH, Klimpel KR, Thomas G. Human furin is a calcium-dependent serine endoprotease that recognizes the sequence Arg-X-X-Arg and efficiently cleaves anthrax toxin protective antigen. J Biol Chem. 1992;267:16396–16402. [PubMed] [Google Scholar]
- 64.Sarac MS, Cameron A, Lindberg I. The furin inhibitor hexa-D-arginine blocks the activation of Pseudomonas aeruginosa exotoxin A in vivo. Infect Immun. 2002;70:7136–7139. doi: 10.1128/IAI.70.12.7136-7139.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cameron A, Appel J, Houghten RA, Lindberg I. Polyarginines are potent furin inhibitors. J Biol Chem. 2000;275:36741–36749. doi: 10.1074/jbc.M003848200. [DOI] [PubMed] [Google Scholar]
- 66.Fugere M, Appel J, Houghten RA, Lindberg I, Day R. Short polybasic peptide sequences are potent inhibitors of PC5/6 and PC7: Use of positional scanning-synthetic peptide combinatorial libraries as a tool for the optimization of inhibitory sequences. Mol Pharmacol. 2007;71:323–332. doi: 10.1124/mol.106.027946. [DOI] [PubMed] [Google Scholar]
- 67.Karicherla P, Hobden JA. Nona-D-arginine therapy for Pseudomonas aeruginosa keratitis. Invest Ophthalmol Vis Sci. 2009;50:256–262. doi: 10.1167/iovs.08-2344. [DOI] [PubMed] [Google Scholar]










