Abstract
We report a 69-years-old Iranian HIV negative male patient, with long-standing pulmonary tuberculosis (eleven years) co-infected with non-tuberculosis mycobacteria. Despite of initiation of first line anti-tuberculosis therapy after diagnosis the patient poorly respond because of low compliance with anti-TB treatment. After several incomplete treatments the smear was still positive and thus drug susceptibility tests were performed on isolated organism which revealed that the organisms was resistant not only against isoniazid and rifampin but also against Ofloxacin (OFX), Capreomycin (CAP), p-aminosalicylic acid (PAS), ethionamide (ETH), Kanamycin (KAN), ciprofloxacin (Cip), amikacin (AMK) and cycloserine (CYC). Persistence and resistance of infection had led us to do more investigation using molecular methods, which revealed co-infection with Non-tuberculosis mycobacteria (NTM). The patient is still alive with cough and shortness of breath.
Keywords: NTM, XDR-TB, Mycobacterium tuberculosis
Introduction
There were an estimated 8.7–9 million new cases of tuberculosis annually and 1.4 million people died from TB during 2011. The emergence of drugs resistant strains of Mycobacterium tuberculosis has been considered a serious threat for global health and control of tuberculosis. Extensively drug-resistant Mycobacterium tuberculosis (XDR-TB) is a rare form of drug-resistances which is not susceptible against the second-line anti-tubercular regimen in particular fluoroquinolones and any of injectable drugs (Amikacin, Kanamycin, or Capreomycin) in addition to the first-line anti-TB regimen (resistance to at least isoniazid and rifampin) [1,2]. XDR-TB has been reported by 84 countries with high rate of mortality [3]. XDR-TB raises concerns for restricted treatment options [4]. Individuals with a history of lung damage are susceptible to non-tuberculosis mycobacteria (NTM). Co-existence of TB and NTM led to inaccurate diagnosis and inappropriate treatment [5].
Case report
A 69-years-old male patient was referred to physician with complains of cough for 3 months, tiredness and weight loss during September 2002 in north east of Iran. The patient indicated no history of fever at night and chills and also no family history of pulmonary tuberculosis. In examination no underlying disease and HIV was detected but he was heavy smoker. Three sputum samples were obtained over a 3-day period for acid-fast bacilli (AFB) smears and culture. The direct smears were positive for AFB, and his disease was diagnosed as pulmonary tuberculosis. He received standard anti-TB treatment recommended by WHO, consisting of rifampin (RIF), isoniazid (INH), ethambutol (EMB) and pyrazinamide (PZA) for two months, followed by four months of RIF and INH while his compliance was low. In March 2003, his weight increased and major health improvement was noticed. The smear was negative and consequently the treatment was stopped. In April 2003, because of symptoms recurrence, treatment was begun according to cat II as follow: two months treatment with RIF, INH, EMB, PZA and streptomycin (STR), followed by one month of RIF, INH, EMB and PZA, followed by five months RIF, INH and EMB. In January 2004 patient was admitted with hemoptysis. At this time direct smear was positive and therefore culture of sputum and drug sensitivity test was performed. The exams resulted in positive culture which was resistance against RIF, INH, EMB and STR. The patient was hospitalized for 124 days in the National Research Institute of Tuberculosis and Lung Diseases (NRITLD) (Tehran, Iran) and treatment was started with second-line anti-tubercular regimen consisting ciprofloxacin (Cip), amikacin (AMK), prothionamide (PTH), cycloserine (CYC), clarithromycin (CLR), amoxicillin-clavulanate and vitamin B6. The patient poorly followed his treatment for several years in spite of symptoms. In May 2008, because of no response to treatment, drug sensitivity test was performed for second-line anti-tubercular regimen using two critical proportions of 1% and 10%. The result (after 42 days incubation at 37 °C) showed resistance against Amikacin, Ciprofloxacin, Cycloserine, Ofloxacin (OFX), Capreomycin (CAP), p-aminosalicylic acid (PAS), ethionamide (ETH), Kanamycin (KAN). In August 2012, due to unusual persistence and resistance of infection, more investigation was recommended using biochemical molecular methods and therefore sputum culture and drug sensitivity test was performed in Regional Tuberculosis Reference Laboratory in Mashhad. It showed that direct smear and sputum culture was still positive for AFB. In September 2012, direct smear and culture was repeatedly positive and during this time due to digestive side effects, the patient refused to use regular drugs consumption. Mycobacterium isolated was niacin negative and had smooth colony and was resistance against RIF, INH, EMB and STR. PCR was performed on isolated mycobacterium that revealed NTM (unknown species). For more confirmation, another sputum sample was sent to NRITLD on January 2013. Using molecular methods particularly Spoligotyping, the isolated strain was identified as M. tuberculosis. In March 2013, chest radiography revealed a bilateral infiltration in upper lobes (Fig. 1).
Fig. 1.
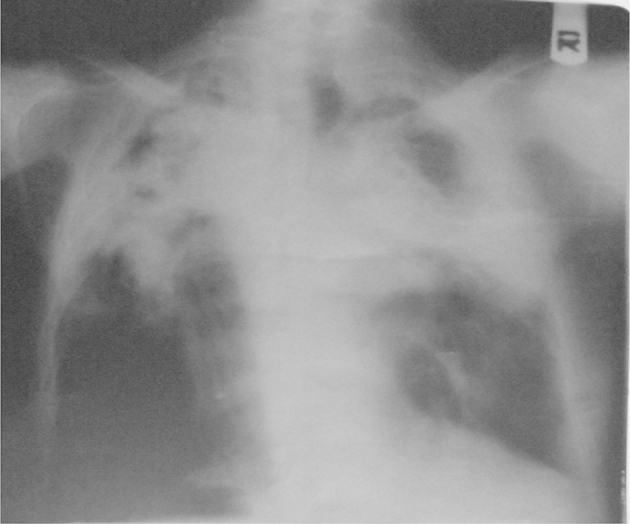
Chest radiography showing bilateral infiltration in upper lobes.
At that time his laboratory values were as follow: white blood cell (70.6% neutrophils) and red blood cell count were normal, Hemoglobin: 18.8 g/dL, Hematocrit: 58.5 mL/dL, urea: 47 mL/dL, Cr: 1.4 mL/dL, Aspartate aminotransferase (AST): 23 IU/L, Alanine aminotransferase (ALT): 19 IU/L. On physical examination, his blood pressure was 90/60 mmHg, his weight was 55 kg. The patient still complained of cough and shortness of breath.
Discussion and conclusion
XDR-TB is a form of tuberculosis that are resistant to most of anti-TB drugs. XDR-TB increases concerns of a tuberculosis due to restricted treatment options, and strongly jeopardizes the achievements made by TB control. It is vital that this form of tuberculosis co-infected with other bacteria, be accurately and rapidly diagnosed. The main concerns and points regarding our case are as follow: The direct smears always were positive except for two times, after initiation of treatment with first-line regimen at first diagnosis and, during treatment with second-line regimen in combination with clarithromycin and amoxicillin-clavulanate. This strain has probably become resistance against first and second line regimen due to poor compliance during these years. Co-existing NTM with M. tuberculosis due to pre-existing lung disease could interpret the symptoms and situation of the patient. Despite lack of sign and symptom, smears remain positive because of NTM. It should be considered that M. tuberculosis may be omitted even if NTM is detected. It must be noticed that NTMs do not show suitable response to anti-tuberculosis drugs. The inaccurate diagnosis of TB co-infected with NTM is still remains a big problem.
Another hypothesis is that NTM infections can diminish progression of M. tuberculosis and thus this theory gives explanation for survival of the patient. And the patient is still alive without any important problems. Another interesting point about the patient was lack of considerable weight loss (53–55 kg) during this period. There are some reports that show XDR-TB cases have died or had serious problems [6–8]. In spite of not using mask protection by the patient, other family members were not infected.
Another possibility in this case is the presence of a new species with characteristics similar to both XDR-TB and NTM. The frequency and clinical significance of NTM isolated from patients during treatment for pulmonary tuberculosis has not been adequately studied ([6,8–10]). More research still needs to be done for more clarifications. Finally it should be remembered that in any tuberculosis patients with poor response to treatment, co-infection with other bacteria especially NTM should be examined.
Acknowledgment
This study was supported by Mashhad University of Medical Sciences (901135), Mashhad, Iran.
References
- 1.Center for Diseases Control and Prevention Emergence of Mycobacterium tuberculosis with extensive resistance to secondline drugs – worldwide, 2000-2004. MMWR Morb Mortal Wkly Rep. 2006;55:301–305. [PubMed] [Google Scholar]
- 2.World Health Organization Case definition for extensively drugresistant tuberculosis. Wkly Epidemiol Rec. 2006;42:408. [PubMed] [Google Scholar]
- 3.World Health Organization . 2011. Global tuberculosis control: WHO report. [Google Scholar]
- 4.Loddenkemper R., Hauer B. Drug-resistant tuberculosis: a worldwide epidemic poses a new challenge. Dtsch Arztebl Int. 2010 Jan;107(1–2):10–19. doi: 10.3238/arztebl.2010.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsing S.C., Weng S.F., Cheng K.C., Shieh J.M., Chen C.H., Chiang S.R. Increased risk of pulmonary tuberculosis in patients with previous non-tuberculous mycobacterial disease. Int J Tuberc Lung Dis. 2013 Jul;17(7):928–933. doi: 10.5588/ijtld.12.0675. [DOI] [PubMed] [Google Scholar]
- 6.Takeda M., Ito W., Kobayashi N., Konno K., Takahashi T., Tatsuko R. Co-existence of Mycobacterium tuberculosis and Mycobacterium intracellulare in one sputum sample. Intern Med. 2008;47(11):1057–1060. doi: 10.2169/internalmedicine.47.0511. [DOI] [PubMed] [Google Scholar]
- 7.Araujo-Filho J.A., Vasconcelos- A.C., Jr., Sousa E.M., Silveira C., Ribeiro E., Kipnis A. Extensively drug-resistant tuberculosis: a case report and literature review. Braz J Infect Dis. 2008 Oct;12(5):447–452. doi: 10.1590/s1413-86702008000500019. [DOI] [PubMed] [Google Scholar]
- 8.Huang H.C., Yu W.L., Shieh C.C., Cheng K.C., Cheng H.H. Unusual mixed infection of thoracic empyema caused by Mycobacteria tuberculosis, nontuberculosis mycobacteria and Nocardia asteroides in a woman with systemic lupus erythematosus. J Infect. 2007 Jan;54(1):e25–e28. doi: 10.1016/j.jinf.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Kobashi Y., Okimoto N., Hara Y., Matsushima T. A case of mixed pulmonary infection with Mycobacterium tuberculosis and M. intracellulare due to familial prevalence. Nihon Kokyuki Gakkai Zasshi. 2002 Jan;40(1):35–39. [PubMed] [Google Scholar]
- 10.Aliyu G., El-Kamary S.S., Abimiku A., Brown C., Tracy K., Hungerford L. Prevalence of non-tuberculous Mycobacterial infections among tuberculosis suspects in Nigeria. PLoS One. 2013;8(5):e6317. doi: 10.1371/journal.pone.0063170. [DOI] [PMC free article] [PubMed] [Google Scholar]


