Abstract
Objectives
Open radical prostatectomy (RP) has been the standard and primary treatment for focal prostate cancer. However, in recent years this view has changed, as robot-assisted laparoscopic RP has gained acceptance among urologists. In this review we evaluate the importance and place of robotics in laparoscopic urological surgery, discussing several techniques that are currently being used and potentially new techniques that might be used in the future.
Methods
We systematically reviewed papers published between 1998 and 2011 using the keywords ‘robotic prostatectomy’ ‘gold standard’ and the Medline database. In addition, after selecting relevant reports we searched ‘related citations’ of the documents to find further supporting published papers.
Results
In all, 50 original papers were identified using the search criteria; we also found 28 through ‘related citations’ browsing. Papers were selected according to their relevance to the current topic (i.e. RP, original articles) and incorporated into this review. These papers were used for their information on the advantages of using robotics, as well as innovative ideas being used in the field of robotic urological surgery.
Conclusion
Almost a decade after the first robotic RP many reports show the benefits and advantages of incorporating robotics into urological surgery. Robotic surgery decreases the learning curve necessary for surgeons when compared with laparoscopic techniques. In addition, patients prefer robotics, as the procedure is less invasive, diminishes the duration of hospitalisation and speeds the return to function.
Abbreviations: (RA)RP, (robot-assisted) radical prostatectomy; 3D, three-dimensional; PNP, primary neural plate; (P)NVB, (predominant) neurovascular bundle; EPE, extraprostatic extension; DVC, dorsal vein complex; LPF, lateral pelvic fascia
Keywords: Robotic, Radical prostatectomy, Standard, Technique
Introduction
Technological advances in the field of laparoscopic surgery have drastically altered the practice of urological surgery. The use of robotics in minimally invasive surgery has enhanced the quality of treatment available to patients. Robotic surgery is beneficial as it allows the surgeon to perform complex surgical procedures with both dexterity and minimal fatigue [1]. In addition, the ergonomic design, filtering of tremors, expanded range of movement, and three-dimensional stereoscopic visualisation of the tissue allows the surgeon to be more accurate and precise during the task, minimising human error and improving the quality of normal human tissue [1]. These benefits, along with the potential to execute any surgical task, are what made robotic surgery a popular treatment option for radical prostatectomy (RP) in the USA [2]. Robotics has also become a staple method for treating other difficult urological procedures, such as pyeloplasty, radical cystectomy, donor nephrectomy, and partial nephrectomy [3–5].
The purpose of this review was to highlight the importance and place of robotics in urological surgery, as well as discuss advances in the field that might play an integral role in the future. We discuss how to operate the robotic equipment used during robotic RP, and advanced techniques that are currently used in the field of robotic urological surgery. We further show that robotics is becoming a more important and better option for treating RP.
Methods
We systematically reviewed published reports to show the importance of robotics in urological surgery. The Medline database was searched for reports published between 1998 and 2011, using the keywords ‘robotic prostatectomy gold standard’. Once the search was completed, 50 reports were found from this criterion. Relevant publications were then selected from the 50 that met the desired criterion for the topic (RP, original articles). From these publications, the use of the ‘related citations’ tool allowed for further reports to be found for incorporation into this review. From the related citations, 28 publications from papers through the search were used in this report (Fig. 1).
Figure 1.
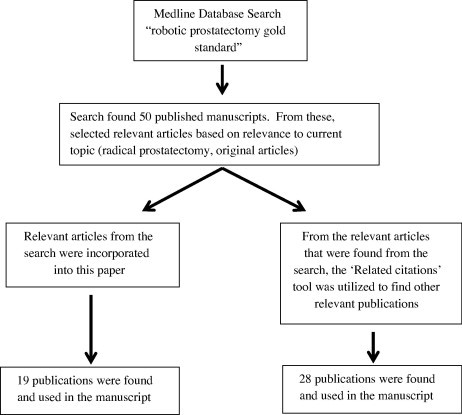
Illustration demonstrating how the articles referenced in the paper were found and selected.
Operative technique
Treatment goals
There are two objectives that need to be met when treating prostate cancer, i.e. eradicate as much of the neoplasm as possible and decrease the morbidity of the patient. However, there are complications that occur during treatment. The term ‘trifecta’ is used to depict a combination of meeting the objectives and minimising the number of complications, i.e. cancer control, continence, and coitus [6]. This is met by use of the da Vinci master–slave robotic system (Intuitive Surgical, Sunnyvale, CA, USA), coupled with a minimally invasive, robotic-assisted RP (RARP) approach. This technique uses a unique standardised surgical procedure, different visual images of the tissue using multiple lenses, optimal retraction strategies, precise suturing, and most importantly, anatomical sparing of the neurovascular structures [7,8]. The RARP approach has been enhanced by increasing the understanding of the local anatomy of the nerves by a thorough dissection of the tissue without using thermal energy to control the patient’s bleeding, termed ‘nerve-sparing’. This allows promising oncological and surgical outcomes while causing minimal bleeding [9]. This procedure allows a quicker recovery, decreased hospitalisation, decreased use of analgesia, less blood transfusion requirement due to less bleeding, and a decreased postoperative scar [10]. There are new approaches to the problem where surgeons have modified their approach to use the following strategies to improve patient outcome and improve the ‘trifecta’ outcomes.
The da Vinci system is a sophisticated master–slave robotic surgical device that incorporates three-dimensional (3D) high-definition visualisation, movement scaling, and wristed instrumentation [11]. A surgeon sits at the main console and controls the surgical field through a binocular port that displays a 3D view of the operated tissue. Two types of lenses are used, 0° or 30°; the 30° lens is used during different parts of the procedure to improve visualisation by allowing the surgeon to look up or down. The da Vinci has four robotic multi-joint arms; the central arm controls the binocular endoscope camera and the other three arms control the articulated instruments [11]. Two finger-controlled handles, known as the ‘masters’, which control the robotic arms and the Endo-wrist instruments, allow for seven degrees of freedom of movement. There are foot pedals operating systems used to control the patient’s bleeding through heat energy. Instrument movements are scaled and range from 1:1, allowing exact finger movements to be transmitted to the instrument tip, to 1: 3 and 1:5, allowing for a more precise and meticulous dissection. The 3D view allows × 10–15 vision with depth perception, which aids in improving tissue delineation and dissection of the neurovascular tissue [11].
The robotic team consists of a console-side and a patient-side surgeon. The surgeon who is operating is positioned at the console and does not need to be ‘scrubbed’ like the patient-side team. Those who are ‘scrubbed’ place the ports, present the operating field to the surgeon who is operating, and use suction to keep the field clean.
Anatomical principles of surgical technique
There are three zones of nerves, known as the trizonal concept, an idea that has been collaborated on by many different urological teams [12–14]. It is important to avoid damage to the primary neural plate (PNP) early in the procedure. The PNP is found on the lateral aspect of the proximal prostate and is vulnerable to injury when the endopelvic fascia is removed. Scissors are used to open the endopelvic fascia medially, and a plane is dissected between the coverings of the prostate; the prostate capsule and prostatic fascia.
The PNP is located lateral to the prostate-bladder junction, so it is best to approach the bladder neck from the centre. Once the bladder is opened, posterior dissection begins by opening a ‘retrotrigonal layer’. This layer is cut, which creates a window where the vasa and seminal vesicles are visible. The PNP is located 5–10 mm lateral to the seminal vesicles and is vulnerable to thermal damage, which thus potentially can affect the recovery of erectile function. This part of the dissection is performed athermally through small pedicles, and controlling them with small 5-mm surgical clips close to the surface of the seminal vesicles.
The next important stage of the surgery is to preserve the predominant neurovascular bundles (PNVBs). The PNVBs are found in a posterolateral groove on the side of the prostate. There is a muscular (levator) branch and anterior rectal component that makes accurate graft anastomosis to the proximal and distal segments difficult, making it important to preserve the nerves. While the PNVBs can have significant anatomical variations, most are well-formed in about half of cases. The neural communications between the PNVBs and PNP are delicate, so any stretch or thermal damage might affect postoperative erectile function, either temporarily or permanently.
Peri-prostatic fascia
There are many layers of fascia that cover the prostate. The outer layer that lines the levator ani muscle is the levator fascia and the inner layer that covers the prostate capsule is the prostatic fascia. In between these layers are the neurovascular structures encompassed within adipose tissue. To ensure maximum nerve-sparing, the prostatic fascia should not be penetrated and the NVBs should not be excised.
Synchronous antegrade and retrograde release of PNVB
Planes of dissection can be obliterated by periprostatic inflammation, tumour-induced desmoplasia, extraprostatic extension (EPE), and haemorrhage. Because of these pitfalls, the prostatic pedicles are approached at the end, when the bundle is free at the apex and of the rest of the nerve. This allows for a clear demarcation of prostatic pedicles and is helpful when the pedicle is wide and problematic to differentiate from the NVB. In situations where tumour growth has prohibited complete nerve-sparing, it is best to do an incremental nerve excision, zone-specific radicality, or excision and nerve advancement with end-to-end anastomosis of the bundles.
Preservation of accessory pathways
There are many accessory nerves found around the prostate, located between the prostatic and lateral prostatic (levator) fascia, posterior to the prostate and in the layers of Denonvilliers’ fascia. They can also be found in planes between the layers of periprostatic fascia and in the layers of the prostatic capsule. The physiological significance of these nerves is unknown; some function as erectile tissue, some function as motor tissue, some innervate the sphincter, and deeper accessory nerves might be involved with prostatic secretions and smooth muscle contraction.
Nerve preservation and apical dissection
Apical dissection is of major importance because this is the area that is the final common pathway for the exit of the cavernous nerves. The PNVB and accessory pathways are associated with the components of the apical-urethral junction, i.e. the distal prostate, dorsal venous plexus, urethral tube, periurethral muscles, puboperinealis, ligaments, fascial layers, and distal vascular pedicle to the prostate and NVB, in an area located behind the pubic bone. Both can be damaged during urethral transection and anastomosis. It is important that there is careful dissection of this region to ensure good preservation of the function of continence.
Surgical steps
The standard procedure begins by incising the peritoneum over the bladder, and then dropping the bladder to enter the space in front of it, allowing the surgeon to approach the prostate from the front. The prostatic veins are secured, and the junction between the prostate and bladder is dissected by using a technique known as the ‘bladder neck pinch’ [9].
Once the bladder neck is transected, the vasa deferentia and seminal vesicles are identified and located behind the retrotrigonal layer. The dissection now continues without cautery (athermal) and is atraumatic. The seminal vesicles and vasa deferentia are enveloped in a fascial compartment (part of the Denonvilliers’ fascia) that is made up of loose areolar tissue, veins, arteries, lymphatics and adipose. Each seminal vesicle has its own compartment and most of its blood supply enters near the tip and anterolateral aspect. Lateral to this compartment is the proximal neurovascular plate, which is part of the inferior hypogastric plexus. This location is important because it has significant implications for nerve-sparing technique, as this crucial neural tissue can be damaged easily. Here is one of the advantages of using robotics as opposed to standard laparoscopy. Robotics allows for increased precision that will allow a greater nerve-sparing technique, thus preserving much more of the vital neural tissue.
Most of the medial wall of the seminal vesicle lies adjacent to an avascular area. This avascular space serves as a good starting point for lateral dissection of the seminal vesicles. Once dissection has begun, the vasa deferentia are mobilised and the proximal end is clipped behind the trigone. The distal ends of the vasa deferentia are separated and held out of the surgical area by one of the robotic arms and pulled anteriorly. This ‘tents’ the Denonvilliers’ fascia. This fascia is incised midline and the opening is enlarged laterally towards the pedicles. Then the undersurface of the prostate is identified, and a plane is developed within the layer of Denonvilliers’ fascia. This creates a large space behind the prostate and the dissection is extended distally to release the apex and urethra from deeper tissue.
The next step is to release the neurovascular tissue by a trizonal-neural-hammock-release technique and athermal approach. It is important to incorporate a grade-specific nerve-sparing approach which aids in preoperative decision making for the best balance between cancer control and functional outcomes. A sharp athermal dissection of the prostatic pedicles is next, after which the surgeon will control the arteries and veins, usually with Hem-o-lok clips (Teleflex Medical Inc., Research Triangle Park, NC, USA) as they enter the prostatic base. The prostate is not attached on either side posterolaterally. This makes the prostate mobile and it can be lifted anteriorly towards the anterior abdominal wall and pubic symphysis. This will open the space behind the urethra and apex. Unfortunately, this also twists and angles the dorsal vein complex (DVC), temporarily occluding it.
At this time it is best to change to a 30° upwards-facing lens for a retro-apical approach to the apical–urethral junction. Care must be taken when moving the lens directly behind the prostate, to avoid getting it smudged by the bladder or the prostate’s undersurface. Once positioned correctly, the surgeon is surprisingly able to differentiate the white surface of the apex from the membranous urethra. This can also be discerned by observing the Foley catheter passing in and out of the apical–urethral junction.
The superficial layers of Denonvilliers’ fascia can then be dissected to expose the prostate–urethral junction. The posterior hemi-circumference of the urethra is incised 1 mm distal to the apex, exposing the Foley catheter and re-positioning it with its tip at the distal urethral opening. This allows the surgeon to now view the urethral mucosa and muscular wall of the urethra. Now the urethra is divided circumferentially, with the muscle fibres then transected and the DVC left attached to the anterior surface of the prostate.
The surgeon must manage the DVC; this depends on the width and thickness of its anterior tissue. If it is broad and thick, the DVC is ligated using a CT-1 needle and 0 polyglactin suture with a slip knot. If the tissue is thin, the pneumoperitoneum pressure is increased to 20 cm H2O and the Foley catheter balloon is inflated to 30 mL behind the prostate. The balloon is placed on caudal traction, which causes partial occlusion of the DVC.
Now the lens is reverted to 0° and the apical dissection of the prostate is continued anteriorly. The prostate is then retracted cephalad. Using robotic Maryland dissectors, the anterior tissue is grasped so that only venous tissue and some parts of the ligament are grabbed; the venous sinus is then cut. This causes minimal bleeding because the inflated balloon is under traction of the DVC, if the DVC is wide and thick. The prostate is then freed, with the ligaments and venous tissue on the prostatic apex.
With the prostate freed, the surgeon can now dissect the pelvic lymph nodes. The lymph nodes are removed just as would be done in the open procedure. Robotic surgery allows for even extended lymph node removal in some high-risk cancer cases. The surgeon ensures that the sphincter, urethra and deeper nerves are not included.
It is important not to damage the muscles surrounding the urethra, to leave the external urethral sphincter intact. Maintaining the external urethral sphincter is important as it helps in the early return of urinary control. Surgeons also preserve the maximum blood supply to the urethra and its surrounding structures by suturing only those vessels that enter the prostate and need to be sutured for safe removal of the prostate. Local cancer spread can then be found by comparing the specimen to frozen sections.
The prostate gland that contains the cancer is then placed in a plastic bag to avoid any tumour spillage. The specimen is removed. The surgeon then closes the surgical incisions using sterile strips.
Extraperitoneal surgical technique
Most RARPs follow the same principles with few modifications. With these procedures, most series use the transperitoneal approach. This is used by many because it provides a larger working space, which is important during lymph-node dissection and urethrovesical anastomosis [15]. There have been studies of the extraperitoneal approach, an alternative method of treatment used because it carries a lower risk of intra-abdominal complications like bowel injury, postoperative ileus, and development of incisional hernia [16–18]. The extraperitoneal technique is similar to the transperitoneal approach but they do not have the same contraindications. Thus patients with a history of laparoscopic abdominal surgery, hernia repair, appendectomy and TURP were not considered contraindicated for the former procedure. While it is debated as to whether or not this approach provides advantages over the traditional procedure, the transperitoneal approach is still successful in removing cancer but preserving continence and potency. Many centres are hesitant to use the extraperitoneal technique because of the risk of unrecognised intra-abdominal injuries from the surgical site [17]. These injuries arise because of the passage of the surgical instruments inside the patient. In addition, other debated disadvantages of the extraperitoneal approach are the limited working space and the increased tension on the vesico-urethral anastomosis [17].
Advanced techniques
Anatomical and athermal robotic technique of nerve sparing
It is vital to have a further understanding of the complexity of the nerves surrounding the prostate. Meticulous dissections of fresh cadavers and observation through robotic surgery have allowed surgeons to enhance their understanding of the pelvic neuroanatomy. It was found that the nerves are arranged around the prostate in a ‘hammock’-like orientation, hence the term ‘trizonal neural hammock’ which describes the structural design of the nerves. On understanding this neuronal arrangement, surgeons have adjusted their nerve-sparing surgical technique to avoid neuronal injury. It was then understood that it was important to not only preserve the dominant (classical) NVBs but also the small, potentially critical, components of the neural hammock, in particular those nerves that travel around and behind the prostate. Nerve sparing can further be increased by avoiding the use of heated cautery instruments during the procedure, as studies showed that nerves cannot withstand heat very well [19–23]. An in-depth step-by-step guide on how to conduct nerve-sparing surgery was published by Menon et al. [24].
Total anatomical reconstruction
The steadfast belief is that on completing the surgical procedure, the closer the corrected tissue is to pre-surgical anatomy, the better the functional results would be [25]. With this basis, the technique of complete vesico-urethral reconstruction was devised, providing critical anterior and posterior support to the urethral sphincter, in an attempt to allow an early return of urinary continence [26]. Tewari et al. [26,27] began using this technique in January 2007 and their patients reported a significant improvement in the return of early continence compared to control patients who were operated on using conventional techniques.
Visual cues to supplement tactile input
A main disadvantage when using robotic surgery is the inability to receive tactile feedback, creating difficulties in the surgeon’s ability to make intraoperative decisions [28]. To ameliorate this disadvantage researchers developed intraoperative visual cues by video-recording RARPs and correlating the anatomy and pathology. The images obtained during the surgery were then matched with histopathology. The visual cues obtained were implemented in following RARPs and the effect of the technical adjustments was assessed. The visual cues function to aid in the smooth transition to using robotics for surgery, in an attempt to decrease the inability to receive tactile feedback. This phenomenon is known as ‘intersensory integration’ where the surgeon is able to ‘feel through the eyes’ during the robotic surgery [28]. Examples of visual cues include changes in colour or texture, bulging and surface irregularities, adhesiveness of planes, and the presence of a mass effect produced by a tumour [28]. Using these visual cues does not compromise the tissue’s safety and it assists surgeons during nerve-sparing RARPs to achieve low positive surgical margin rates [28].
Catheter-less technique
The use of catheters has frequently been hazardous, as they are a source of infection, discomfort, anxiety and embarrassment for patients who undergo RARP [29]. It is for these reasons that surgeons have begun using urethral catheter-less RARP [29]. A urethral splint can also be used instead [30]. The splint drains the bladder, splints the anastomosis, and causes less discomfort for patients after surgery [30]. Research shows that patients being treated without a urethral catheter experience almost no penile pain and achieve continence earlier than patients who use a urethral catheter [30].
Delicate tissue handling during nerve sparing
The most common long-term side-effect of RP that patients complain about is sexual dysfunction [31,32]. This might be attributed to postoperative penile hypoxia, which causes a cascade of biochemical events that ultimately causes erectile dysfunction [33]. A penile oxygen-saturation study showed that by maintaining tissue saturation at >85% during surgery, by using a tissue oximeter, patients had a ⩾95% return to sexual function after 1 year, more than had control patients whose tissue saturation was not monitored [33,34]. During the procedure, if the oxygenation saturation fell below 85%, surgical dissection was altered or FiO2 was increased to ensure that tissue saturation was restored to a minimum of 85% [33]. A landmark article by Walsh and Donker in 1982 [35] showed that the cause of erectile dysfunction after RP was caused by severance of the cavernous nerves. These nerves modulate autonomic function and run along the lateral aspects of the prostate, and are prone to damage during surgery.
Grades of nerve sparing
It is important to preserve as many of the nerves as possible. Tewari et al. [36] showed the importance of nerve-sparing, and developed a risk-stratified approach that centred on the layers of periprostatic fascial dissection. This innovative type of nerve-sparing RP provides an early return of sexual and orgasmic function without compromising cancer control. Tewari et al. [36] described nerve sparing grades as:
Grade 1: The incision of the Denonvilliers’ and lateral pelvic fascia (LPF) is taken just outside the prostatic capsule. We also describe this as medial venous plane for complete hammock preservation. This represents the greatest degree of nerve-sparing possible, and we use this procedure only for patients with no-to-minimal risk of EPE.
Grade 2: The incision through Denonvilliers’ fascia (leaving deeper layers on the rectum) and LPF is taken just outside the layer of veins of the prostate capsule. We also describe this as a peri-venous plane of hammock preservation. This preserves most large neural trunks and ganglia, and is used for patients at low risk of EPE.
Grade 3 (partial/incremental): The incision is taken through the outer compartment of the LPF (leaving some yellow adipose and neural tissue on the specimen), excising all layers of Denonvilliers’ fascia. This is used in patients with a moderate risk of EPE because some of the medial trunks are sacrificed, while the lateral trunks are preserved.
Grade 4 (not nerve-sparing): These patients have a high risk of EPE and are not candidates for nerve-sparing. Here, we use a wide excision of the LPF and Denonvilliers’ fascia, containing most of the periprostatic neurovascular tissue. In selected patients, we attempt nerve advancement of the identifiable ends of the NVBs.
Patient follow-up
Patients report the following concerns to be most influential on prostate cancer therapy: oncological control (margin and PSA recurrence), pain, complications, convenience (catheter duration and length of hospitalisation), and functional outcomes (incontinence and sexual dysfunction) [37]. It is important that each of these concerns be addressed and minimised, so that the patient can enjoy a healthy recovery and improve their quality of life after surgery.
Ou et al. [38] monitored the oncological results of 2200 patients operated using robotic surgery by one surgeon. The study defined margins as positive if there was a tumour present at the inked specimen. The study found that residual positive tumour was detected in <9% of the cases.
Studies show that robotic surgery has allowed patients to have less significant postoperative pain [39]. RARP has allowed a shorter mean hospitalisation stay and duration of catheterisation [39], causing less inconvenience. This can be further improved by using a catheter-less technique [30].
RARP is a safer technique that allows the minor and major complications to be negligible. There are some complications, such as blood transfusions, myocardial infarction, pulmonary embolus, ileus, deep vein thrombosis, anastomotic leakage, etc. [40,41].
Using robotics for surgery is safe but it does have complications. Many reviews have shown the complications that arise from robotic surgery, but the conversion rates from robotic to laparoscopic surgery have been minimal [40,42]. Patients who are at higher risk are those with cardiac problems and those who are obese. Those with cardiac stents must stop using their anticoagulants before surgery. Obese patients are at a greater risk for all complications. Some surgery centres create exercise programmes for these patients to help them reduce weight and enable them to walk sooner after surgery. In addition, when anaesthesia is used, there can be anaesthesia-related complications, including fatal cardiac and thromboembolic events.
Recent advances
Surgeons have begun to expand the use of robotics by changing where they make incisions and how they approach the anatomy. Natural-orifice transluminal endoscopic surgery and laparo-endoscopic single-site surgery have been developed in an attempt to reduce the morbidity and scarring associated with surgical intervention. These procedures reduce the number of transcutaneous incisions (points of access) in an attempt to improve the patient’s postoperative quality of life, as there are fewer complications, a shorter recovery time, less pain and better cosmesis [43]. In addition to these advantages of these procedures, they also attempt to treat patients through scar-less surgery. It has been found that with laparo-endoscopic single-site surgery there is a smaller margin of error and a longer learning curve with the procedure [44]. These difficulties make this procedure not the first choice when it comes to treatment options, but it is promising due to the cosmetic advantages that it provides. In addition, the procedure has mainly been used for pyelonephrectomy, but it is promising that future advances in robotics might allow single-port surgery to be used for laparoscopic RP.
Lasers
In a pilot study, Cheetham et al. [45] evaluated the delivery mechanism of a CO2 laser energy through a fibre to enhance the accuracy of dissection of the NVB during RARP. They used a CO2 laser fibre that transmits energy with minimal absorptive loss. The thermal spread from the energy that CO2 lasers deliver can affect potency and possibly other functions. During the procedure, when the NVB was found, the fibre was inserted into the jaws of the robotic needle driver and the surgeon was able to manipulate the fibre and place it in an optimal position by the NVB. The laser was then activated and used for a bilateral dissection of the NVB. The CO2 laser was able to produce incisions with narrow, well-defined areas. The study showed that using these lasers is a safe and easy technique for dissection of the NVB during nerve-sparing RARP. It also was successful in showing that 70% of the patients regained urinary continence by 6 weeks after the surgery, and 90% regained continence at 3 months after surgery [45].
Another laser-based RARP pilot study was used on 10 dogs. A potassium-titanyl-phosphate laser was used to dissect the prostate, with the addition of a neodymium-doped yttrium–aluminium-garnet laser for coagulation of vessels. The study monitored intracavernosal pressures in response to nerve stimulation as a percentage of the mean arterial pressure before and after RARP. The results were not significantly different and there were no laser-related complications, only catheter-related complications [46]. This type of laser-based procedure is soon to be tested on humans.
Conclusions
RARP is a safe and effective technique for surgery on the prostate; it is becoming the more preferred method of treatment by urologists, because it uses the principles of laparoscopic and open RP. In addition, patients prefer this procedure because they enjoy the benefits of a less-invasive method, minimal pain, and low blood loss that allows them a quicker overall recovery. There are many advanced techniques being implemented to ensure improved quality of treatment to patients, both during and after surgery. Future advances in this field will not only improve the quality of care, but solidify RARP as the new gold standard for treating prostate cancer.
Conflict of interest
The authors have no conflict of interest to declare.
References
- 1.Rocco B., Matei D.V., Melegari S., Ospina J.C., Mazzoleni F., Errico G. Robotic vs open prostatectomy in a laparoscopically naive centre: a matched-pair analysis. BJU Int. 2009;104:991–995. doi: 10.1111/j.1464-410X.2009.08532.x. [DOI] [PubMed] [Google Scholar]
- 2.Dasgupta P., Kirby R.S. The current status of robot-assisted radical prostatectomy. Asian J Androl. 2009;11:90–93. doi: 10.1038/aja.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stoianovici D. Robotic surgery. World J Urol. 2000;18:289–295. doi: 10.1007/pl00007078. [DOI] [PubMed] [Google Scholar]
- 4.Cadeddu J.A., Stoianovici D., Kavoussi L.R. Robotic surgery in urology. Urol Clin North Am. 1998;25:75–85. doi: 10.1016/s0094-0143(05)70434-1. [DOI] [PubMed] [Google Scholar]
- 5.Hubert J. Robotic pyeloplasty. Curr Urol Rep. 2003;4:124–129. doi: 10.1007/s11934-003-0039-6. [DOI] [PubMed] [Google Scholar]
- 6.Bianco F.J., Jr., Scardino P.T., Eastham J.A. Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (‘trifecta’) Urology. 2005;66:83–94. doi: 10.1016/j.urology.2005.06.116. [DOI] [PubMed] [Google Scholar]
- 7.Menon M., Shrivastava A., Sarle R., Hemal A., Tewari A. Vattikuti Institute Prostatectomy: a single-team experience of 100 cases. J Endourol. 2003;17:785–790. doi: 10.1089/089277903770802380. [DOI] [PubMed] [Google Scholar]
- 8.Leak B., Wei J.T., Gabel M., Peabody J.O., Menon M., Demers R. Relevant patient and tumor considerations for early prostate cancer treatment. Semin Urol Oncol. 2002;20:39–44. doi: 10.1053/suro.2002.30397. [DOI] [PubMed] [Google Scholar]
- 9.Tewari A.K., Rao S.R. Anatomical foundations and surgical manoeuvres for precise identification of the prostatovesical junction during robotic radical prostatectomy. BJU Int. 2006;98:833–837. doi: 10.1111/j.1464-410X.2006.06417.x. [DOI] [PubMed] [Google Scholar]
- 10.Duffey B., Varda B., Konety B. Quality of evidence to compare outcomes of open and robot-assisted laparoscopic prostatectomy. Curr Urol Rep. 2011;12:229–236. doi: 10.1007/s11934-011-0180-6. [DOI] [PubMed] [Google Scholar]
- 11.Tewari A., Peabody J., Sarle R., Balakrishnan G., Hemal A., Shrivastava A. Technique of da Vinci robot-assisted anatomic radical prostatectomy. Urology. 2002;60:569–572. doi: 10.1016/s0090-4295(02)01852-6. [DOI] [PubMed] [Google Scholar]
- 12.Tewari A., Takenaka A., Mtui E., Horninger W., Peschel R., Bartsch G. The proximal neurovascular plate and the tri-zonal neural architecture around the prostate gland: importance in the athermal robotic technique of nerve-sparing prostatectomy. BJU Int. 2006;98:314–323. doi: 10.1111/j.1464-410X.2006.06266.x. [DOI] [PubMed] [Google Scholar]
- 13.Takenaka A., Leung R.A., Fujisawa M., Tewari A.K. Anatomy of autonomic nerve component in the male pelvis: the new concept from a perspective for robotic nerve sparing radical prostatectomy. World J Urol. 2006;24:136–143. doi: 10.1007/s00345-006-0102-2. [DOI] [PubMed] [Google Scholar]
- 14.Takenaka A., Murakami G., Soga H., Han S.H., Arai Y., Fujisawa M. Anatomical analysis of the neurovascular bundle supplying penile cavernous tissue to ensure a reliable nerve graft after radical prostatectomy. J Urol. 2004;172:1032–1035. doi: 10.1097/01.ju.0000135648.33110.df. [DOI] [PubMed] [Google Scholar]
- 15.Xylinas E., Ploussard G., Durand X., de la Taille A. Robot-assisted extraperitoneal laparoscopic radical prostatectomy: a review of the current literature. Urol Oncol. 2010 doi: 10.1016/j.urolonc.2010.07.004. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Atug F., Castle E.P., Woods M., Srivastav S.K., Thomas R., Davis R. Transperitoneal versus extraperitoneal robotic-assisted radical prostatectomy: is one better than the other? Urology. 2006;68:1077–1081. doi: 10.1016/j.urology.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Joseph J.V., Rosenbaum R., Madeb R., Erturk E., Patel H.R. Robotic extraperitoneal radical prostatectomy: an alternative approach. J Urol. 2006;175:945–951. doi: 10.1016/S0022-5347(05)00340-X. [DOI] [PubMed] [Google Scholar]
- 18.Esposito M.P., Ilbeigi P., Ahmed M., Lanteri V. Use of fourth arm in da Vinci robot-assisted extraperitoneal laparoscopic prostatectomy: novel technique. Urology. 2005;66:649–652. doi: 10.1016/j.urology.2005.03.061. [DOI] [PubMed] [Google Scholar]
- 19.Ong A.M., Su L.M., Varkarakis I., Inagaki T., Link R.E., Bhayani S.B. Nerve sparing radical prostatectomy: effects of hemostatic energy sources on the recovery of cavernous nerve function in a canine model. J Urol. 2004;172:1318–1322. doi: 10.1097/01.ju.0000139883.08934.86. [DOI] [PubMed] [Google Scholar]
- 20.Ahlering T.E., Eichel L., Edwards R.A., Lee D.I., Skarecky D.W. Robotic radical prostatectomy: a technique to reduce pT2 positive margins. Urology. 2004;64:1224–1228. doi: 10.1016/j.urology.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 21.Tewari A., Rao S., Martinez-Salamanca J.I., Leung R., Ramanathan R., Mandhani A. Cancer control and the preservation of neurovascular tissue: how to meet competing goals during robotic radical prostatectomy. BJU Int. 2008;101:1013–1018. doi: 10.1111/j.1464-410X.2008.07456.x. [DOI] [PubMed] [Google Scholar]
- 22.Gill I.S., Ukimura O. Thermal energy-free laparoscopic nerve-sparing radical prostatectomy: one-year potency outcomes. Urology. 2007;70:309–314. doi: 10.1016/j.urology.2007.03.072. [DOI] [PubMed] [Google Scholar]
- 23.Su L.M., Link R.E., Bhayani S.B., Sullivan W., Pavlovich C.P. Nerve-sparing laparoscopic radical prostatectomy: replicating the open surgical technique. Urology. 2004;64:123–127. doi: 10.1016/j.urology.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Menon M., Tewari A., Peabody J. Vattikuti Institute prostatectomy: technique. J Urol. 2003;169:2289–2292. doi: 10.1097/01.ju.0000067464.53313.dd. [DOI] [PubMed] [Google Scholar]
- 25.Deliveliotis C., Protogerou V., Alargof E., Varkarakis J. Radical prostatectomy: bladder neck preservation and puboprostatic ligament sparing – effects on continence and positive margins. Urology. 2002;60:855–858. doi: 10.1016/s0090-4295(02)01956-8. [DOI] [PubMed] [Google Scholar]
- 26.Tewari A.K., Bigelow K., Rao S., Takenaka A., El-Tabi N., Te A. Anatomic restoration technique of continence mechanism and preservation of puboprostatic collar: a novel modification to achieve early urinary continence in men undergoing robotic prostatectomy. Urology. 2007;69:726–731. doi: 10.1016/j.urology.2006.12.028. [DOI] [PubMed] [Google Scholar]
- 27.Tewari A., Jhaveri J., Rao S., Yadav R., Bartsch G., Te A. Total reconstruction of the vesico–urethral junction. BJU Int. 2008;101:871–877. doi: 10.1111/j.1464-410X.2008.07424.x. [DOI] [PubMed] [Google Scholar]
- 28.Tewari A.K., Patel N.D., Leung R.A., Yadav R., Vaughan E.D., El-Douaihy Y. Visual cues as a surrogate for tactile feedback during robotic-assisted laparoscopic prostatectomy: posterolateral margin rates in 1340 consecutive patients. BJU Int. 2010;106:528–536. doi: 10.1111/j.1464-410X.2009.09176.x. [DOI] [PubMed] [Google Scholar]
- 29.Haute W.V., Dasgupta P. Urethral catheter-less robotic-assisted radical prostatectomy. BJU Int. 2010;105:1201–1203. doi: 10.1111/j.1464-410X.2010.09248.x. [DOI] [PubMed] [Google Scholar]
- 30.Tewari A., Rao S., Mandhani A. Catheter-less robotic radical prostatectomy using a custom-made synchronous anastomotic splint and vesical urinary diversion device: report of the initial series and perioperative outcomes. BJU Int. 2008;102:1000–1004. doi: 10.1111/j.1464-410X.2008.07875.x. [DOI] [PubMed] [Google Scholar]
- 31.Kimura M., Banez L.L., Schroeck F.R., Gerber L., Qi J., Satoh T. Factors predicting early and late phase decline of sexual health-related quality of life following radical prostatectomy. J Sex Med. 2011;8:2935–2943. doi: 10.1111/j.1743-6109.2011.02387.x. [DOI] [PubMed] [Google Scholar]
- 32.Pereira R.F., Daibs Y.S., Tobias-Machado M., Pompeo A.C. Quality of life, behavioral problems, and marital adjustment in the first year after radical prostatectomy. Clin Genitourin Cancer. 2011;9:53–58. doi: 10.1016/j.clgc.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 33.Tewari A., Srivastava A., Sooriakumaran P., Grover S., Dorsey P., Leung R. Technique of traction-free nerve-sparing robotic prostatectomy: delicate tissue handling by real-time penile oxygen monitoring. Int J Impot Res. 2011:1–9. doi: 10.1038/ijir.2011.40. [DOI] [PubMed] [Google Scholar]
- 34.Padmanabhan P., McCullough A.R. Penile oxygen saturation in the flaccid and erect penis in men with and without erectile dysfunction. J Androl. 2007;28:223–228. doi: 10.2164/jandrol.106.001313. [DOI] [PubMed] [Google Scholar]
- 35.Walsh P.C., Donker P.J. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982;128:492–497. doi: 10.1016/s0022-5347(17)53012-8. [DOI] [PubMed] [Google Scholar]
- 36.Tewari A.K., Srivastava A., Huang M.W., Robinson B.D., Shevchuk M.M., Durand M. Anatomical grades of nerve sparing: a risk-stratified approach to neural-hammock sparing during robot-assisted radical prostatectomy (RARP) BJU Int. 2011;108:984–992. doi: 10.1111/j.1464-410X.2011.10565.x. [DOI] [PubMed] [Google Scholar]
- 37.Diefenbach M.A., Dorsey J., Uzzo R.G., Hanks G.E., Greenberg R.E., Horwitz E. Decision-making strategies for patients with localized prostate cancer. Semin Urol Oncol. 2002;20:55–62. doi: 10.1053/suro.2002.30399. [DOI] [PubMed] [Google Scholar]
- 38.Ou Y.C., Yang C.R., Wang J., Yang C.K., Cheng C.L., Patel V.R. The learning curve for reducing complications of robotic-assisted laparoscopic radical prostatectomy by a single surgeon. BJU Int. 2011;108:420–425. doi: 10.1111/j.1464-410X.2010.09847.x. [DOI] [PubMed] [Google Scholar]
- 39.Kenngott H.G., Fischer L., Nickel F., Rom J., Rassweiler J., Muller-Stich B.P. Status of robotic assistance-a less traumatic and more accurate minimally invasive surgery? Langenbecks Arch Surg. 2011 doi: 10.1007/s00423-011-0859-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 40.Coelho R.F., Palmer K.J., Rocco B., Moniz R.R., Chauhan S., Orvieto Ma. Early complication rates in a single-surgeon series of 2500 robotic-assisted radical prostatectomies: report applying a standardized grading system. Eur Urol. 2010;57:945–952. doi: 10.1016/j.eururo.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 41.Patil N., Krane L., Javed K., Williams T., Bhandari M., Menon M. Evaluating and grading cystographic leakage: correlation with clinical outcomes in patients undergoing robotic prostatectomy. BJU Int. 2009;103:1108–1110. doi: 10.1111/j.1464-410X.2008.08168.x. [DOI] [PubMed] [Google Scholar]
- 42.Rotering J., Siemer S., Stockle M. [Robot-assisted laparoscopic radical prostatectomy] Urol A. 2008;47:422–424. doi: 10.1007/s00120-008-1656-y. 420. [DOI] [PubMed] [Google Scholar]
- 43.Autorino R., Cadeddu J.A., Desai M.M., Gettman M., Gill I.S., Kavoussi L.R. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011;59:26–45. doi: 10.1016/j.eururo.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 44.White W.M., Haber G.P., Goel R.K., Crouzet S., Stein R.J., Kaouk J.H. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009;74:801–804. doi: 10.1016/j.urology.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 45.Cheetham P.J., Truesdale M.D., Lee D.J., Landman J.M., Badani K.K. Use of a flexible carbon dioxide laser fiber for precise dissection of the neurovascular bundle during robot-assisted laparoscopic prostatectomy. J Endourol. 2010;24:1091–1096. doi: 10.1089/end.2010.0132. [DOI] [PubMed] [Google Scholar]
- 46.Gianduzzo T., Colombo J.R., Jr., Haber G.P., Hafron J., Magi-Galluzzi C., Aron M. Laser robotically assisted nerve-sparing radical prostatectomy: a pilot study of technical feasibility in the canine model. BJU Int. 2008;102:598–602. doi: 10.1111/j.1464-410X.2008.07708.x. [DOI] [PubMed] [Google Scholar]


