Abstract
Background
Salivary gland tumours constitute about 3–4 % of all head and neck neoplasms. Approximately 80 % originate in the parotid gland and they are rarely present in the submandibular gland. Basal cell adenoma is a benign epithelial salivary gland tumour that appears to have unique histologic characteristics. The diagnosis of this entity must be established by histological study.
Case report
The literature revealed only four reported cases of basal cell adenoma of submandibular salivary gland. This article presents a rarely occurring basal cell adenoma as a fifth reported case in submandibular salivary gland in a 23 year old female.
Discussion
A rare case of basal cell adenoma of submandibular salivary gland is reported with clinical features, diagnosis, histopathological features and treatment modalities. When there is involvement of submandibular gland with a tumour the histopathological confirmation is mandatory instead of relying on FNAC and it must be differentiated from pleomorphic adenoma, adenoid cystic carcinoma, adenocarcinoma due to its prognostic implications.
Conclusion
Entities like basal cell adenoma can only be established by histopathological examination after excisional biopsy. The treatment done also affects the ultimate prognosis. As such the surgeon has to make his clinical decision based on many factors like history, clinical examination, histopathological examinations, radiological examination and immunohistochemistry study. No single criteria should be relied upon. We recommend to carry out genetic pattern study in a person with basal cell adenoma to rule out pathogenesis and establish a correct diagnosis of it for better understanding and prognosis.
Keywords: Basal cell adenoma, Pleomorphic adenoma, Adenoid cystic carcinoma, Basaloid epithelial cells
Background
Salivary gland tumours constitute a very small number of head and neck neoplasms out of which 80 % occur in the parotid gland whereas they can rarely be found in the submandibular gland [1].
Basal cell adenoma is an uncommon type of monomorphic adenoma with unique histologic characteristics and constitutes 1–2 % of all salivary gland neoplasms. In 1967, Kleinsasser and Klein introduced the term “basal cell adenoma” to describe a benign epithelial salivary gland tumour comprising of uniform-appearing basaloid cells arranged in solid, trabecular, tubular, and membranous patterns but that lacked the myxoid and chondroid mesenchymal-like components of a pleomorphic adenoma. Batsakis reported the first case of basal cell adenoma in American Literature in 1972 [2].
The commonest site for basal cell adenoma is parotid gland with an incidence of 73.1 %. It may occur to involve other sites as upper lip, buccal mucosa, lower lip, palate and nasal septum [3]. It presents as a firm, mobile slow-growing mass usually in patients of 60 years of age or more.
The glandular tumours of maxillofacial region such as pleomorphic adenoma and adenoid cystic carcinoma are considered for its differential diagnosis which have varied prognosis and require specific approaches for their treatment. Hence, it becomes mandatory to consider its proper diagnosis and treatment. Thorough search of literature revealed only four cases of basal cell adenoma of submandibular gland till date. This article reports the fifth case of basal cell adenoma of submandibular salivary gland in a 23 year old female.
Case Report
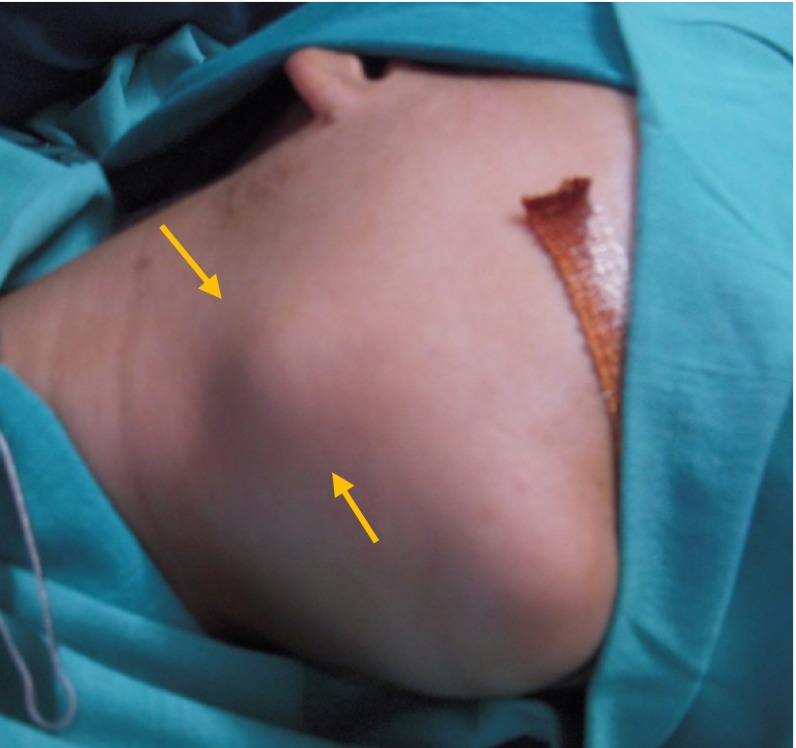
A 23 year old female patient reported with a chief complaint of painless swelling in the right submandibular region since 7 months.
The extra-oral examination revealed a well-defined ovoid, solitary swelling in the right submandibular region measuring approximately 3 cm in diameter. It was normal skin coloured, non-tender and moderately firm in consistency (Fig. 1). The swelling moved on deglutition without any pulsations. The digital orthopantomograph revealed no bony destruction in that region. With suspected diagnosis of right submandibular tumour, a contrast cervicofacial computerised tomography (CT) was performed, considering both bone and soft tissue windows. CT scan showed evidence of a well defined smooth rounded isodense mild to moderately enhancing solid lesion noted at the anterior end of right submandibular gland. There was no evidence of calcification, cysts or necrosis within the nodule (Fig. 2). No signs of mandibular erosion or invasion of other adjacent structures were evident. Due to its radiological features it was suggestive of exophytic submandibular gland neoplasm-adenoma (Fig. 3). Before reporting to us, the patient had undergone a preliminary FNAC procedure at another centre and that report was suggestive of (salivary neoplasm) adenoid cystic carcinoma. Taking into consideration patients age, clinical and radiological findings which did not resemble to be adenoid cystic carcinoma and if so, before proceeding for any radical surgery a second thought was given and FNAC was repeated which gave very different diagnosis from the first one as benign pleomorphic adenoma. So, the decision for surgical treatment was taken considering patients age, history, clinical examination, radiological findings and histopathological reports. In this regard the patient was explained accordingly and the surgery was planned to have total excision and removal of mass along with affected submandibular salivary gland.
Fig. 1.
Clinical photograph showing submandibular swelling
Fig. 2.

CT scan showing a well defined solid lesion at the anterior end of right submandibular gland
Fig. 3.

Intra-operative appearance of tumor mass
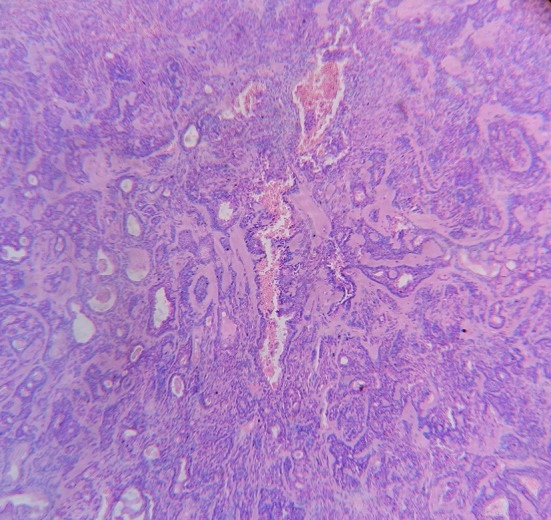
The surgical excision of the mass and submandibular gland was done under general anaesthesia. The excised mass appeared to be well encapsulated (Figs. 2, 4). Keeping previous reports in mind the excised specimen was sent for histopathological diagnosis and immunohistochemistry to have more detailed and accurate histopathological diagnosis. The histopathological report was indicative of basal cell adenoma of submandibular salivary gland. The H & E stained section showed small cuboidal epithelial cells arranged in strands and ducts with eosinophilic coagulum within ducts. The strands are surrounded by hyalinised connective tissue. The stromal connective tissue showed numerous small blood capillaries and few haemorrhagic areas. The capsule appeared intact (Figs. 5, 6, 7). Immunohistochemistry examination showed positivity to S-100 protein. Follow up was done for 2 years 6 months so as to be aware about any changes as the first diagnosis was adenoid cystic carcinoma and there is no sign of recurrence.
Fig. 4.

Excised surgical specimen (2.5 × 3 cm)
Fig. 5.

Histopathological appearance of trabecular–tubular type of basal cell adenoma (×10)
Fig. 6.
Histopathological appearance of trabecular–tubular type of basal cell adenoma (×100)
Fig. 7.
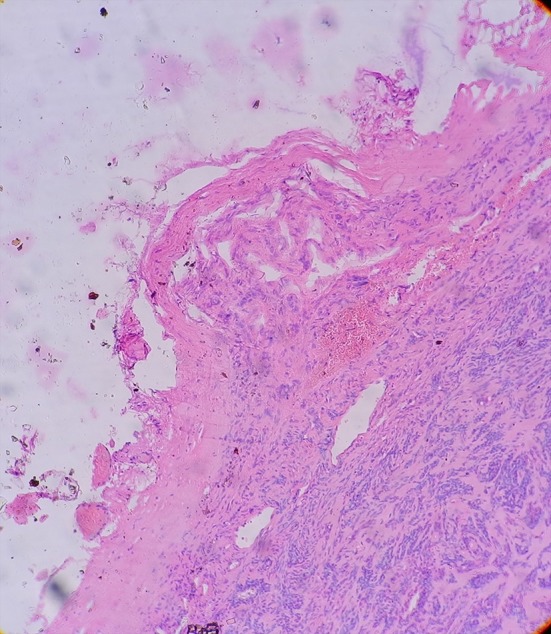
Histopathological appearance of trabecular–tubular type of basal cell adenoma showing intact capsule and basement membrane
Discussion
Basal cell adenoma is a neoplasm of a uniform population of basaloid epithelial cells classified as monomorphic adenoma. Batsakis suggested that the intercalated duct or reserve cell is the histogenetic source of the basal cell adenoma and occur primarily in the major salivary glands. It is predominantly found in the parotid gland and minor salivary glands of the upper lip being the second commonest site. Thorough search of literature revealed only four reported cases of basal cell adenoma of submandibular salivary gland and this particular case becomes distinctly unique as being the fifth case.
Clinically, basal cell adenoma presents as a slow-growing, asymptomatic and freely movable firm swelling that may be cystic and compressible making it indistinguishable from mixed tumour. These encapsulated tumours do not exceed 3 cm in diameter and are superficially located in the glandular body with a brownish appearance. An unusual feature of this case was that the age of patient was 23 years, in contrast to reported age of occurrence–57.7 years–and correlated to its female predilection [4, 5].
The diagnosis of this entity must be established by the histological study. Adenoma is a benign epithelial tumor in which the cells are derived from glandular epithelium [5]. Basal cell adenoma, as defined by WHO, is a distinctive benign neoplasm composed of basaloid cells organized with a prominent basal cell layer and distinct basement membrane-like structure and no myxochondroid stromal component as seen in pleomorphic adenomas. The basal cells in basal cell adenoma are fairly uniform and regular with two morphological forms. One is a small cell with scanty cytoplasm and round deeply basophilic nucleus. The other cell is large with eosinophilic cytoplasm and an ovoid pale staining nucleus. A basal membrane-like structure rounds these tumoral nests, separating them from the surrounding connective tissue [6].
Basal cell adenoma of the salivary glands closely resembles basal cell lesions of the skin. It can show a variety of histologic patterns: tubular, trabecular, cribriform, solid, and membranous [7]. In this case the histological pattern was trabecular–tubular type.
Generally, biopsy is accepted as the most accurate method to obtain the diagnosis, although some authors advocate for fine needle aspiration cytology (FNAC) if physical access to the tumor is available [8]. Cytopathological diagnosis is accurate in over 90–95 % of patients in experienced hands. If histopathological type can be determined preoperatively, this information may be used to determine extent of surgical procedure (with or without neck dissection) [9]. But according to some authors, the primary role of FNAC is only as a diagnostic tool that aids in the evaluation of a salivary gland mass and not a histological procedure on which operative decisions can be based. [10] In our case, the FNAC was done twice with two different diagnosis as adenoid cystic carcinoma and pleomorphic adenoma respectively which makes us to strongly state that this procedure should not be diagnostic preoperatively. We determined our surgical procedure taking into considerations a number of factors as patients age, clinical examination, radiological examination and histopathological reports.
The CT showed evidence of a well-defined smooth rounded isodense mild to moderately enhancing solid lesion at the anterior end of right submandibular gland. There was no evidence of calcification/cysts, necrosis within nodule. No signs of mandibular erosion or invasion of other adjacent structures were seen. In the present case the tumour appeared as well demarcated smooth, solid right submandibular lesion which was suggestive of exophytic submandibular gland neoplasm: adenoma.
Very few immunohistochemistry markers are available for differentiation of tumours. Data suggests that epithelial and glandular origin can be confirmed by immunohistochemistry. In trabecular and ductal subtypes, the cells show intensive S-100 staining which may be due to presence of myoepithelial cells or according to some as a marker of neoplastic cells of BCA, independent of their lineage [8]. The excised specimen was sent for immunohistochemistry to have more detailed and accurate histopathological diagnosis. In our case also, there was positivity to S-100 protein.
For most sporadic basal cell adenomas, the pathogenesis is unclear. Cytogenetic alterations have been only rarely characterized in non-membranous basal cell adenomas, with a trisomy 8 and chromosome 13 alterations being the major abnormalities described [11]. With regards to membranous basal cell adenomas, alterations at the CYLD1 gene locus at chromosome 16q12–13 are seen in both sporadic and familial/syndromic cases, suggesting that this alteration is vital to this subtype’s pathogenesis [12]. CYLD1 is a deubiquitinating enzyme whose loss of activity correlates with activation of the NF-kB pathway, hinting at a mechanism of tumorigenesis [13] and suggests that it should be imperative to carry out genetic study of the patient of basal cell adenoma to rule out pathogenesis for proper conclusion.
Basal cell adenomas are amenable to conservative resection such as local excision or superficial removal of the gland, whereas the membranous subtype requires complete resection of the entire gland. The recurrence rate for the solid and trabecular–tubular variants is almost non-existent. This contrasts with the high recurrence rate (24 %) of the membranous type, which is perhaps a result of the multicentricity of this lesion. Although exceedingly rare, malignant transformation is more common in the membranous type than in the other types [14]. In this case the histological pattern was tubular- trabecular type and there was no recurrence on 2 year follow up.
The differential diagnosis is adenoid cystic carcinoma, basal cell adenocarcinoma, and pleomorphic adenoma. Basal cell adenomas may have a myxoid or hyaline stroma, and rarely a myoepithelial-rich cellular stroma [15]. However, in contrast to pleomorphic adenoma, the stroma, regardless of cellularity, is distinct from the basaloid proliferation, with no intermingling. Mitoses are rare to absent, as is necrosis, and there is no infiltration of surrounding tissue or perineural invasion, which distinguishes basal cell adenomas from their malignant counterparts, basal cell adenocarcinomas [16] (Fig. 7).
The differential diagnosis with these entities has prognostic implications. Also the surgical treatment differs based on preoperative and intraoperative diagnosis. The general guidelines for treatment of basal cell adenoma, adenocarcinoma and adenoid cystic carcinoma are local excision of mass or submandibular gland, level I neck dissection and supraomohyoid neck dissection/comprehensive neck dissection plus postoperative radiotherapy respectively [9] and should be based on continued histopathological diagnosis and immunohistochemistry studies.
Conclusion
The occurrence of basal cell adenoma in submandibular gland is rare and this is the fifth reported case. Entities like basal cell adenoma can only be established by histopathological examination after excisional biopsy. In this case the differential diagnosis of basal cell adenoma was pleomorphic adenoma and adenoid cystic carcinoma so there were prognostic implications. The treatment done also affects the ultimate prognosis. As such the surgeon has to make his clinical decision based on many factors like history, clinical examination, histopathological examinations, radiological examination and immunohistochemistry study. Though we are assisted by many diagnostic aids like FNAC, CT scan etc. no diagnostic method is conclusive. No single criteria should be relied upon. We strongly recommend to carry out genetic pattern study in a person with basal cell adenoma to rule out pathogenesis and establish a correct diagnosis of it for better understanding and prognosis.
Conflict of interest
None.
Contributor Information
Pravin N. Lambade, Email: drpravinlambade@gmail.com
Dilpreet Rajkhokar, Email: dilpreet.rajkhokar@gmail.com.
Dipti Lambade, Email: drdiptilambade@gmail.com.
References
- 1.Lin H-C, Chien C-Y, Huang S-C, Su C-Y. Basal cell adenoma of the sublingual gland. Ann Otol Rhinol Laryngol. 2003;112(12):1066–1068. doi: 10.1177/000348940311201213. [DOI] [PubMed] [Google Scholar]
- 2.Seifert G. The World Health Organization’s histological classification of salivary gland tumors: a commentary on the second edition. Cancer. 1992;70(2):379–385. doi: 10.1002/1097-0142(19920715)70:2<379::AID-CNCR2820700202>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 3.Hiranuma T, Kagamiuch H, Kitamura R. A basal cell adenoma of the sublingual gland. Int J Oral Maxillofac Surg. 2003;32:566–567. doi: 10.1016/S0901-5027(02)90378-4. [DOI] [PubMed] [Google Scholar]
- 4.Bernacki EG, Batsakis JG, Johns ME. Basal cell adenoma: distinctive tumor of salivary glands. Arch Otolaryngol. 1974;99:84–88. doi: 10.1001/archotol.1974.00780030090002. [DOI] [PubMed] [Google Scholar]
- 5.Canalis RF, Mok MW, Fishman SM, Hemenway WG. Congenital basal cell adenoma of the submandibular gland. Arch Otolaryngol Head Neck Surg. 1980;106(5):284–286. doi: 10.1001/archotol.1980.00790290036012. [DOI] [PubMed] [Google Scholar]
- 6.Nagao K, Matsuzaki O, Saiga H, Sugano I, Shigematsu H, Kaneko T, et al. Histopathologic studies of basal cell adenoma of the parotid gland. Cancer. 1982;50:736–745. doi: 10.1002/1097-0142(19820815)50:4<736::AID-CNCR2820500419>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 7.Dardick I, Lytwyn A, Bourne AJ, et al. Trabecular and solid-cribriform types of basal cell adenoma. A morphologic study of two cases of an unusual variant of monomorphic adenoma. Oral Surg Oral Med Oral Pathol. 1992;73:75–83. doi: 10.1016/0030-4220(92)90159-N. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Garcia R, Nam-Cha SH, Munoz-Guerra MF, Gamallo-Amat C. Basal cell adenoma of the parotid gland. Case report and review of the literature. Med Oral Patol Oral Cir Bucal. 2006;11:E206–E209. [PubMed] [Google Scholar]
- 9.Myers EN, Ferris RL. Salivary gland disorders. 1. New York: Springer; 2007. pp. 353–360. [Google Scholar]
- 10.O’dwyer P, Farrar WB, James AG, Finkelmeier W, Mccabe DP. Needle aspiration biopsy of major salivary gland tumors: its value. Cancer. 1986;57:554–557. doi: 10.1002/1097-0142(19860201)57:3<554::AID-CNCR2820570325>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 11.Trompouki E, Hatzivassiliou E, Tsichritzis T, et al. CYLD is a deubiquitinating enzyme that negatively regulates NF-kappaB activation by TNFR family members. Nature. 2003;424:793–796. doi: 10.1038/nature01803. [DOI] [PubMed] [Google Scholar]
- 12.Luna MA, Tortoledo ME, Allen M. Salivary dermal analogue tumors arising in lymph nodes. Cancer. 1987;59:1165–1169. doi: 10.1002/1097-0142(19870315)59:6<1165::AID-CNCR2820590622>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 13.Luna MA, Batsakis JG, Tortoledo ME, et al. Carcinomas ex monomorphic adenoma of salivary glands. J Laryngol Otol. 1989;103:756–759. doi: 10.1017/S0022215100109995. [DOI] [PubMed] [Google Scholar]
- 14.Jang M, Park D, Lee SR, Hahm CK, Kim Y, Kim Y, Park CK, Tae K, Park MH, Park YW. Basal cell adenoma in the parotid gland: CT and MR findings. AJNR Am J Neuroradiol. 2004;25:631–635. [PMC free article] [PubMed] [Google Scholar]
- 15.Weber A, Langhanki L, Schutz A, et al. Expression profiles of p53, p63, and p73 in benign salivary gland tumors. Virchows Arch. 2002;441:428–436. doi: 10.1007/s00428-002-0705-y. [DOI] [PubMed] [Google Scholar]
- 16.Zabaleta M, Mollá FJ, Salazar F, Erdozain E, Sánchez L. Monomorphic adenoma of basal cells in a minor salivary gland. Acta Otorrinolaringol Esp. 1997;48:169–172. [PubMed] [Google Scholar]