Abstract
Background:
Q-switched neodymium: yttrium aluminum garnet (Nd: YAG) laser at a wavelength of 1064 nm primarily targets dermal melanin and black tattoo ink. Recent studies have shown that this laser is effective in treating black tattoos. There are few studies conducted in India for the same.
Aim:
The aim was to assess the effectiveness of Q-switched Nd: YAG laser (QSNYL) in the treatment of blue-black tattoos following 3 treatment sessions.
Materials and Methods:
This study, a prospective interventional study included a total of 12 blue-black tattoos. Following informed consent for the procedure, as well as for photographs, a questionnaire was administered, and improvement perceived by the patient was recorded. In addition, global assessment score (GAS) by a blinded physician was also recorded. Photographs were taken at baseline and at every follow-up. Each patient underwent three treatment sessions with 1064 nm QSNYL at 4–6 weekly intervals. Fluences ranged from 1.8 to 9 J/cm2. The follow-up was done monthly for 4 months from the first treatment session. The response was assessed by patient assessment (PA) and GAS by comparing photographs.
Results:
After three treatment sessions, although no patient achieved clearance, most patients showed good response with few adverse effects. An average of 64.1% (GAS) and 54.2% (PA) improvement was observed in 12 tattoos. Tattoos more than 10-year-old showed quicker clearing than those less than 10-year-old. Amateur tattoos also showed a better response in comparison to professional tattoos.
Conclusion:
Totally, 1064 nm QSNYL is safe and effective for lightening blue-black tattoos in pigmented Indian skin. All patients achieved near complete clearance following the continuation of treatment (an average of six sessions) although this was spaced at longer intervals.
Keywords: Blue-black tattoos, pigmented skin, Q-switched neodymium:yttrium aluminum garnet laser
What was known?
The 1064 nm Q-switched neodymium: yttrium aluminum garnet laser is safe and effective in treating blue-black tattoos in the dark skin though multiple sessions are often required.
Introduction
Laser treatment in dermatology was started about 40 years ago but was limited due to the formation of scars over the treated areas. Only in the past 20 years have there been a major breakthrough in laser therapy of dermatological problems.[1]
Tattoos are exogenously placed chromophores either by a tattoo artist, cosmetologist (decorative tattoo), physician (delineating a radiation port) or a traumatic event. They are permanent because they are too big to be removed by the body. Laser treatment causes tattoo pigment particles to heat up and fragment into smaller pieces, which are removed by the body processes. Amateur tattoos are less dense and may be placed at variable depths (more superficial) and composed of carbon-based ink and usually require fewer laser sessions as compared to professional tattoos which are characterized by densely packed colored pigments at a uniform depth (usually deeper). Rapidly pulsed Q-switched lasers produce ultrashort bursts of light (pulses) useful for treating pigment-containing lesions. These pulses have a ultrashort pulse duration in the nanosecond range which matches the size of the target-melanosomes or tattoo ink particles. In addition, these ultrashort pulse duration results in a photoacoustic effect, which ruptures these pigment laden cells eliciting a “shock wave.”
Recent studies have shown that 1064 nm Q-switched neodymium:yttrium aluminum garnet (Nd: YAG) laser is effective in treating blue-black tattoos and has one of the best safety profiles in darker skin types.[2,3,4,5,6,7,8,9,10] This laser with a near infrared light is poorly absorbed by melanin, making it suitable for use in dark skin types. It is well-absorbed by dark tattoo pigments and is the wavelength of choice in the removal of black ink and tattoo removal in darker skin. This study highlights the safety and efficacy of Q-switched Nd: YAG laser (QSNYL) in the treatment of blue-black tattoos in the dark skin (Fitzpatrick skin types III-VI).
Materials and Methods
Twelve patients with blue-black tattoos were treated with three sessions of 1064 nm QSNYL.
Males and females, 18 years and older with unwanted blue-black tattoos were included. Pregnant and lactating mothers, patients with herpes, keloidal tendencies, and melasma were excluded.
After obtaining an informed written consent prior to starting the procedure and prior to taking photographs, a questionnaire was administered to each patient to be filled. At each review, the percentage of improvement perceived by the patient was recorded. This was a comparison of the baseline lesion and the lesion at the current visit. Photographs of each lesion were taken at baseline and before each treatment session using a DSLR Nikon D5100 in the same room with similar lighting conditions. The study was initiated following approval by the local Institutional Human Ethics Committee.
Procedure
Before initiating treatment, individual assessment including the patient's skin type and the nature and size of their lesions were recorded. Photographs were taken at baseline and before each treatment session. The subjects were of Fitzpatrick skin type III-VI.
Tattoos were categorized as amateur or professional and also based on age (<10 years and > 10 years).
Small lesions were targeted using a phototherapy stencil or were surrounded with micropore tape to protect the surrounding skin. Topical anesthesia is containing a eutectic mixture of lidocaine 25 mg and prilocaine 25 mg/g, was applied and kept under occlusion over the area to be treated, 1 h prior to treatment. Prior to the laser session, the topical anesthetic was wiped off, and ice packs were applied over the area. Cooling minimized pain and ensured optimal patient co-operation. Proper eye protection was given to the patient, as well as the treating doctor. Three sessions of 1064 nm using MedLite C6 QSNYL at 4–6 weekly intervals were administered. (Ideally tattoos would require longer intervals of 6–8 weeks).
Laser parameters
Laser parameters were selected according to the patient's Fitzpatrick skin type, type of lesion, and the site of the lesion. The wavelength used for all lesions in this study was 1064 nm as it has demonstrated a good safety profile on pigmented skin. The spot size varied depending on the size of the lesion. Initially, test fluence was tried to see the reaction of the laser on each patient. This fluence was dependent on the patient's skin type. A patient with Fitzpatrick skin type III-IV was started with a test fluence of 5 J/cm2, and a patient with skin type V-VI was started with a fluence of 3 J/cm2. If the patient tolerated the test fluence, the procedure was carried out at the same fluence level. If the patient could not tolerate the test fluence (as evidenced by pain), it was lowered to a level tolerable by the patient, and the procedure was carried out at that fluence.
The laser was given in 1–2 passes for tattoos so as to achieve “frosting” (brisk whitening of the lesion). Tattoos showed frosting with fewer passes. The end point was taken when the lesion showed frosting.
At subsequent treatment sessions, the fluence was increased in increments of 0.5–1 J/cm2.
Each patient underwent 3 treatment sessions at 4 weeks intervals with QSNYL with the following settings:
1064 nm wavelength
Fluences ranging from 1.8 to 9 J/cm2
Spot size of 3–6 mm, the majority being treated with 4 mm spot size
The repetition rate of 2–10 Hz.
The topical steroid was advised immediately following the procedure and for 3 consecutive days (at night) following the procedure. Sunscreens were advised to be applied throughout the entire course of treatment. All patients were followed up monthly for 4 months after the first treatment session.
Assessment
Patients’ self-assessment
The patients were asked to give a percentage value based on their improvement from the baseline lesion.
Global assessment score
Global assessment scoring (GAS) was done by a blinded physician by comparing photographs of each lesion at each follow-up. A numeric score of 0–10 (0 – no improvement/10 - complete clearance) was assigned to each follow-up photograph after comparing the follow-up photograph to the baseline photograph.
The results of each lesion were analyzed based on the patient's assessment (PA) and the GAS. The GASs were converted into a percentage, and the mean percentage improvement was calculated. The PA scores were similarly computed.
Results
A total of 12 patients (3 males and 12 females) aged between 19 and 48 years with Fitzpatrick skin types III-VI with blue-black tattoos were treated.
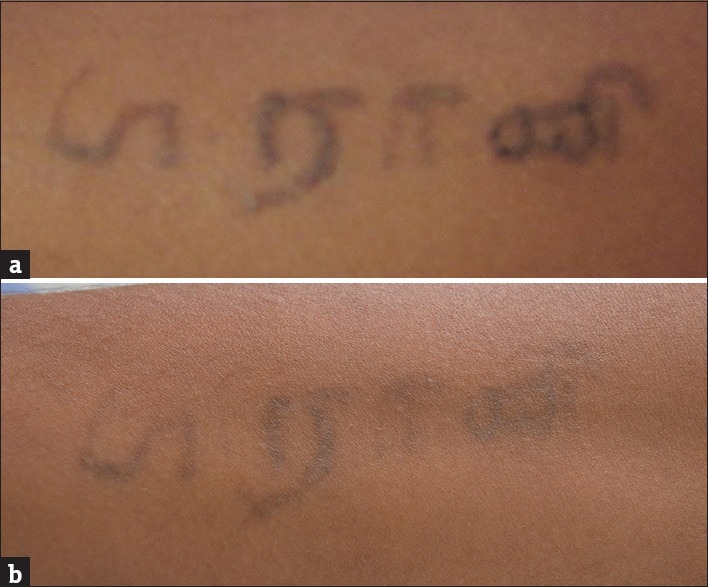
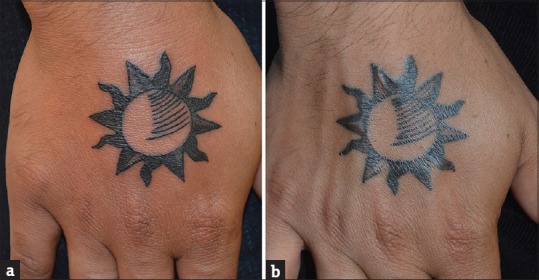
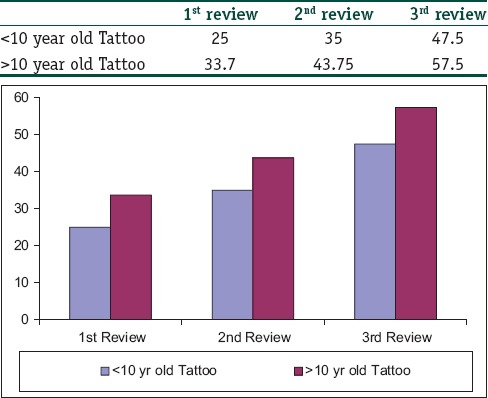
Of the tattoos treated in this study, two were professional tattoos, and the remaining 10 tattoos were amateur tattoos. Of 12 tattoos, four tattoos were applied within the last 10 years, and 8 were applied more than 10 years back. Tattoos more than 10-year-old showed quicker clearing than those less than 10-year-old. Amateur tattoos also showed a better response in comparison to professional tattoos [Table 1]. An average of 64.1% (GAS) and 54.2% (PA) improvement was observed in 12 tattoos [Table 2] Please refer to Figures 1a and b, 2a and b, and 3a and b. One of the tattoos was only a day old and showed only a 30% (GAS) and 20% (PA) improvement following three sessions [Figure 4a and b]. Tables 3 and 4 show an overall improvement of the tattoos by (GAS) scoring and (PA), respectively.
Table 1.
Comparison of results between Professional and Amateur Tattoos and according to age of the Tattoo
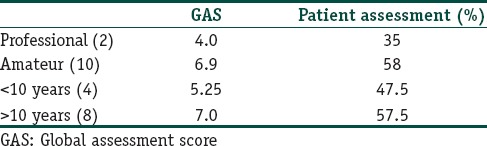
Table 2.
Overall improvement of tattoos at each review

Figure 1.

(a) Tattoo over forehead - before treatment (b) Tattoo forehead after laser treatment
Figure 2.

(a) Tattoo dorsum of hand - before laser treatment (b) Tattoo dorsum of hand - after laser treatment
Figure 3.
(a) Tattoo forearm- before laser (b) Tattoo forearm - after laser
Figure 4.
(a) Professional tattoo dorsum of hand - before laser (b) Professional tattoo dorsum of hand - after laser
Table 3.
Overview of improvement of lesions by global assessment score
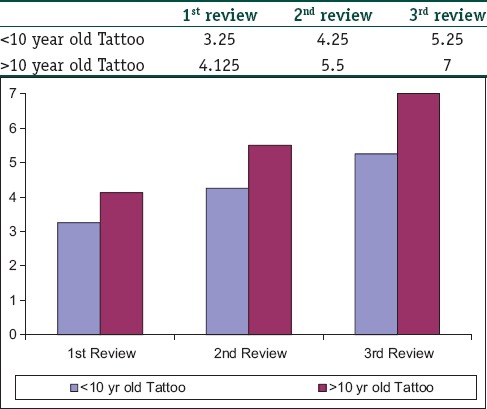
Table 4.
Overview of improvement of lesions by patient assessment
Discussion
The QSNYL system was developed by Geusic et al. in 1964. Now a laser in common use, it operates with two wavelengths (532 and 1064 nm). Totally, 532 nm is highly absorbed by melanin, whereas 1064 nm is a longer wavelength which is poorly absorbed by melanin but well-absorbed by blue-black tattoo ink making it the wavelength of choice for tattoo removal in darker skin and for black ink. The depth of penetration ranges from 3 to 6 mm in human skin.[4,5]
Tissue interactions are a major point of consideration when using lasers. They include the scatter, absorption, and transmission of energy. A major reason for tissue damage around the focused area is the scattering of energy. Scatter of light is said to be more with shorter wavelengths than with longer wavelengths. The spot size for the treatment area should be optimal to reduce the surrounding tissue damage. A minimum spot size of 3 mm is advocated for treatment using the QSNYL while treating tattoos, the largest possible spot size (because light scatters at the margin of the field), should be used in order to minimize the percentage of scatter of the incident beam.[4] Ideally, the initial fluence should be 3.5–4 J/cm2 and should be adjusted according to the patient's response. The desired clinical endpoint is brisk whitening (“frosting”) of the treated area, which typically resolves within 20–30 min after the procedure.[4] The fluence should be increased if frosting is not achieved and reduced if there is visible bleeding over the treated area. It is recommended that the treatment sessions should be carried out at intervals of 6–8 weeks, as melanophages may continue slow clearance of the tattoo pigment. The number of treatment sessions required is dependent on the skin type, type of pigment, location, color, amount of ink, scarring or tissue change, and the rate of lymphatic clearance.[5,6,7,8,9]
QSNYL (1064 nm) targets black pigment injected into the dermis such as India ink commonly used in blue-black tattoos. There are several studies from abroad and India reporting the efficacy of 1064 nm QSNYL on blue-black tattoo removal.[3,4,5,6,7,8,9] Kilmer et al. reported an excellent response (>75% of ink removal) in 77% of patients with black tattoos after 4 treatment sessions at 3–4 weeks intervals using 10–12 J/cm2. They also observed that colored ink was not successfully removed by this laser.[7]
In our study, an average of 54% improvement was observed after three sessions in 12 tattoos treated. According to the PA scoring, seven out of 12 patients (58%) showed 60–70% improvement after three sessions. By GAS, 50% of patients showed 70–80% lightening of the tattoo.
One patient had a tattoo containing black ink and green ink. As observed in earlier reports, there was no lightening of the green pigment, whereas, the black pigment showed excellent response to QSNYL.[5,7]
Amateur tattoos had a quicker clearance rate than professional tattoos.[3,4,5,6,7,8,9,10] Professional tattoos may require 4–6 sessions more for clearance as compared to amateur tattoos.
Our study had ten amateur tattoos and two professional tattoos. Of these, amateur tattoos showed an improvement of 69% by GAS and 58% by the PA. In contrast, professional tattoos showed a 40% lightening by GAS scoring and 35% improvement by PA. Amateur tattoos are less dense with more superficial location of pigment, which is easier to clear. However, few amateur tattoos have deeply placed ink and may be difficult to remove.
Similar findings were recorded in a study was conducted in 15 dark skinned individuals with amateur tattoos. Eight of the 15 tattoos showed 75–95% clearance after three or four sittings at 2 months intervals.[3] Our study showed a 69% clearance of the amateur tattoos after three treatment sessions.
The age of the tattoo may be relevant as older tattoos are thought to be easier to remove than newer tattoos, as over time the body disperses the ink via lymphatic drainage.[10] New tattoos have a higher concentration of ink and require extra sessions. Tattoos in acral locations are more difficult to remove than those placed on truncal sites, which is related to the lymphatic drainage. In our study, four tattoos were less than 10-year-old, and eight tattoos were more than 10-year-old. When comparing these groups, the older tattoos showed an average of 70% clearance whereas the newer tattoos (<10 years) showed only 52.5% clearance. One patient presented with a tattoo that was only a day old. In this patient, lower fluences had to be used initially to minimize pain. The highest tolerable fluence was 1.8 J/cm2, which was subsequently hiked to 5 J/cm2 in later sessions. This patient achieved only 30% clearance after undergoing three laser sessions [Figure 4a and b]. The interval between sessions was increased to 8 weeks. Amateur tattoos generally require four to six treatments and professional tattoos may need eight or more sessions. Complete removal may be difficult to achieve in professional tattoos. Although we found older tattoos easier to treat, and this phenomenon has been reported by few authors,[10] a contrary trend between duration of tattoo and success rate with a worse outcome of laser therapy in older tattoos, has been reported without any explanation.[11] They propose the “sooner the better strategy” in the removal of tattoos. It is also important to record a history of hypertrophic scars/keloids or prior gold therapy. Q-switched laser treatments are contraindicated in patients who have received gold therapy as they induce chrysiasis.[10] Paradoxical darkening can occur in cosmetic tattoos (pink, tan, white, yellow or other light-colored tattoos) used as permanent makeup as the titanium dioxide or iron oxide pigment is reduced by the Q-switched laser treatment.[10]
The “Kirby-Desai Scale,” a predictive scale developed by Kirby et al. could help in evaluating the potential success and number of treatments necessary for laser tattoo removal applicable when using a Q-switched Nd: YAG with an interval of 6 weeks between sessions.[12] This study did not however utilize this predictive scale. It would be very useful to incorporate this in further studies.
Minimal erythema and localized swelling over the treated area shortly after the procedure was observed in all patients, which were relieved with topical steroids. One patient developed a blister at the site of treatment after the first treatment session. This patient had undergone “double tattooing” or “cover art.” This describes the application of a second tattoo over an already existing tattoo, often to camouflage an undesirable tattoo. The blister developed over the area that was overlapped by the new tattoo [Figure 5]. This resolved following the application of topical steroid, an antibiotic combination for 5–7 days. On follow-up, there was no hypertrophic scarring or further blistering as reported in two cases with “double tattoos” who developed hypertrophic scarring following a single treatment with QSNYL.[13]
Figure 5.

Blister formation over double tattooed area following laser treatment
A novel technique by Sardana et al. combining the ultrapulse CO2 laser and Q-switched Nd: YAG is effective in lightening of amateur blue-black tattoos with reduced number of sessions.[5] Other combined protocols using Erb: YAG and QSNYLs have reported good results.[14] Nanosecond lasers like QSNYLs are thought to be the “gold standard” for tattoo removal, but newer picosecond lasers promise effective clearance of newer, vibrant multicolored tattoos. The picoseconds pulse width is 100 times shorter than the nanosecond technology resulting in greater photomechanical impact and subsequent clearance in fewer sessions using lower fluences.[10] Modified techniques like R0 and R20 would enable the number of sessions to be decreased to even a single session.[15] Topical perfluorodecalin rapidly resolves immediate whitening reaction and permits multiple passes without resorting to the R20 technique, which is time-consuming.[16]
Conclusion
Although quality-switched lasers remain the gold standard for tattoo removal, the appropriate device and technique does not always guarantee successful results. Q-switched Nd: YAG 1064 nm is the safest for use in patients with darker complexion with minimal adverse reactions as the longer wavelength is minimally absorbed by epidermal melanin. Although it may take up to 3 months for the effect of one treatment session to be realized, laser sessions are ideally spaced 6–8 weeks apart for tattoos and dermal pigmented lesions. Efficient cooling of the site to be treated and initially starting with lower fluences would lower the incidence of epidermal injury and attendant complications such as pigmentary changes, blistering, and scarring. It is important to utilize the largest spot size possible when treating tattoos, as smaller spot sizes result in greater beam scatter, with resultant decreased depth of penetration. Amateur tattoos generally require four to six treatments and professional tattoos may need eight or more sessions. Since initial fluencies are lower in pigmented skin tattoos in acral locations are more difficult to remove than those placed on truncal sites and older tattoos are easier to treat than newer ones. Although three sessions are inadequate for complete removal of tattoos, with patients showing only partial clearance this study endeavors to study the response of blue-black tattoos to the QSNYL in these sessions. Using the Kirby-Desai Scale may help in predicting the number of treatment sessions required and would be advisable in larger studies. All the patients were followed up and had a better response after more than six sessions, the amateur tattoos showing near complete removal in 6–8 sessions, and professional tattoos requiring 8–10 sessions.
What is new?
There are few published studies from India on the use of a monotherapy of Q-switched neodymium: yttrium aluminum garnet laser in type IV skin for blue-black tattoos.
Footnotes
Source of support: PSG Hospitals and PSGIMSR
Conflict of Interest: Nil.
References
- 1.Tanzi EL, Lupton JR, Alster TS. Lasers in dermatology: Four decades of progress. J Am Acad Dermatol. 2003;49:1–31. doi: 10.1067/mjd.2003.582. [DOI] [PubMed] [Google Scholar]
- 2.Kilmer SL, Lee MS, Grevelink JM, Flotte TJ, Anderson RR. The Q-switched Nd: YAG laser effectively treats tattoos. A controlled, dose-response study. Arch Dermatol. 1993;129:971–8. [PubMed] [Google Scholar]
- 3.Jones A, Roddey P, Orengo I, Rosen T. The Q-switched ND: YAG laser effectively treats tattoos in darkly pigmented skin. Dermatol Surg. 1996;22:999–1001. doi: 10.1111/j.1524-4725.1996.tb00651.x. [DOI] [PubMed] [Google Scholar]
- 4.Bernstein EF. Laser tattoo removal. Semin Plast Surg. 2007;21:175–92. doi: 10.1055/s-2007-991186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sardana K, Garg VK, Bansal S, Goel K. A promising split-lesion technique for rapid tattoo removal using a novel sequential approach of a single sitting of pulsed CO (2) followed by Q-switched Nd: YAG laser (1064 nm) J Cosmet Dermatol. 2013;12:296–305. doi: 10.1111/jocd.12060. [DOI] [PubMed] [Google Scholar]
- 6.Kilmer SL. Laser treatment of tattoos. Dermatol Ther. 2000;13:69–79. [Google Scholar]
- 7.Kilmer SL, Alexiades-Armenakas MR, Levine VJ, Ashinoff R. The Q-switched Nd: YAG (1064 + 532 nm) laser. In: Kauvar AN, Hruza GJ, editors. Principles and Practices in Cutaneous Laser Surgery. Boca Raton: Taylor and Francis Group, LLC; 2005. pp. 265–84. [Google Scholar]
- 8.Ferguson JE, August PJ. Evaluation of the Nd/YAG laser for treatment of amateur and professional tattoos. Br J Dermatol. 1996;135:586–91. [PubMed] [Google Scholar]
- 9.Kuperman-Beade M, Levine VJ, Ashinoff R. Laser removal of tattoos. Am J Clin Dermatol. 2001;2:21–5. doi: 10.2165/00128071-200102010-00004. [DOI] [PubMed] [Google Scholar]
- 10.Green JB, Metelitsa AI. Optimizing outcomes of laser tattoo removal. Skin Therapy Lett. 2011;16:1–3. [PubMed] [Google Scholar]
- 11.Prinz BM, Vavricka SR, Graf P, Burg G, Dummer R. Efficacy of laser treatment of tattoos using lasers emitting wavelengths of 532 nm, 755 nm and 1064 nm. Br J Dermatol. 2004;150:245–51. doi: 10.1111/j.1365-2133.2004.05658.x. [DOI] [PubMed] [Google Scholar]
- 12.Kirby W, Desai A, Desai T, Kartono F, Geeta P. The kirby-desai scale: A proposed scale to assess tattoo-removal treatments. J Clin Aesthet Dermatol. 2009;2:32–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Alora MB, Arndt KA, Taylor CR. Scarring following Q-switched laser treatment of double tattoos. Arch Dermatol. 2000;136:269–70. doi: 10.1001/archderm.136.2.269. [DOI] [PubMed] [Google Scholar]
- 14.Sardana K, Ranjan R, Kochhar AM, Mahajan KG, Garg VK. A rapid tattoo removal technique using a combination of pulsed Er: YAG and Q-Switched Nd: YAG in a split lesion protocol. J Cosmet Laser Ther. 2015 Feb;20:1–7. doi: 10.3109/14764172.2015.1007066. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Kossida T, Rigopoulos D, Katsambas A, Anderson RR. Optimal tattoo removal in a single laser session based on the method of repeated exposures. J Am Acad Dermatol. 2012;66:271–7. doi: 10.1016/j.jaad.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 16.Reddy KK, Brauer JA, Anolik R, Bernstein L, Brightman L, Hale E, et al. Topical perfluorodecalin resolves immediate whitening reactions and allows rapid effective multiple pass treatment of tattoos. Lasers Surg Med. 2013;45:76–80. doi: 10.1002/lsm.22106. [DOI] [PubMed] [Google Scholar]


