Abstract
Obesity is a risk factor for postoperative morbidity in breast reconstruction. Although existing studies about nonbreast reconstruction are limited, previous research has demonstrated that obesity is not an important factor in poor outcomes in nonbreast reconstruction. Our study evaluates the effects of obesity on postoperative morbidity in nonbreast reconstruction in comparison to breast reconstruction. A systematic literature review and meta-analysis was performed using Medline, EMBASE, and Cochrane databases. Obesity was extracted for predictor variables and partial, total loss of flap, and complication were extracted for outcome variables. Subgroup analyses were performed according to reconstruction site. The Newcastle-Ottawa scale (NOS) was used to assess the quality of the studies, and the Cochrane risk of bias tool was used. Publication bias was evaluated using funnel plots. The search strategy identified 944 publications. After screening, 19 articles were selected for review. Partial flap loss, total flap loss, and complications in breast reconstruction occurred significantly more often in obese patients in comparison to nonobese patients (OR = 2.479, P = 0.021 for partial loss, OR = 3.083, P = 0.002 for total loss, OR = 2.666, P = 0.001 for complications). In contrast, partial flap loss, total flap loss, and complications in nonbreast reconstruction were not significantly different in obese patients in comparison to nonobese patients (OR = 0.786, P = 0.629 for partial loss, OR = 0.960, P = 0.961 for total loss, and OR = 1.009, P = 0.536 for complications). In contrast to the relationship between obesity and poor outcomes in breast reconstruction, our study suggests the obesity is not a predisposing factor for poor outcomes in nonbreast reconstruction. Long-term studies are needed to confirm these findings.
Keywords: complications, free flap failure, nonbreast reconstruction, obesity, risk factor
1. Introduction
Free flaps are complex surgeries requiring a lot of experiences on the part of plastic surgeons. The objective of free flap surgeries is to cover various tissue defects owing to cancer or trauma, and this type of surgery has a profound impact on restoring function and improving the quality of life of patients.[1,2] Improvement in microsurgical techniques and technologies over the past several decades have found free flap surgery to be safe and effective.[3–5] Nevertheless, complications, including total flap failure, may occur and may have a significant impact on outcomes of treatment and costs. These complications are frequently attributed to surgical technique. However, several existing studies have investigated the extent to which patient factors may be associated with free flap failure.[6–8]
Among the possible factors potentially leading to postoperative complications, obesity has become a popular a topic of interest. In comparison to patients with normal weight status who undergo surgery, obesity in patients may lead to a sharp increase in morbidity due to perioperative risks, including cardiovascular disease,[9] respirator morbidities,[10] and increased susceptibility to wound infection[11,12] due to complex effects.[13,14] However, the implications of obesity for surgery remain unclear.
It is widely known in the field of plastic surgery that obesity has adverse effects on free flap surgeries when breast reconstruction is performed.[15–17] Although several studies have stated different results according to varying methods of muscle inclusion in reconstructive procedures,[18,19] the majority of existing research suggests that obesity is a critical risk factor for postoperative complications in breast reconstruction.[20,21] However, whether we can define obesity as a risk factor for postoperative complications in general free flap surgery remains controversial. Some past studies investigating risk factors for the reconstruction of sites other than breasts have determined that obesity is not an important predisposing factor for postoperative complications.[22–24]
Accordingly, we hypothesize that a systematic review of existing studies in conjunction with meta-analysis will provide a more comprehensive overview of the impact of obesity in free flap surgeries. Our study estimates the relationship between postoperative complications and obesity in patients undergoing free flap surgery. In addition, it analyzes postoperative morbidity in breast reconstruction and compares the findings with nonbreast reconstruction to determine whether obesity is a risk factor in nonbreast reconstruction.
2. Materials and methods
2.1. Literature search
A search for eligible articles using the PubMed, EMBASE, and Cochrane databases for all studies published prior to October 2015 was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) check list.[25] The purpose of the literature search was to identify various risk factors for free flap failure or complications. The search terms included “risk,” “predisposing,” “free flap,” “free tissue transfer,” “reconstruction,” “obesity,” “body mass index,” “failure,” and “complication.” Only human studies were included, and relevant articles were also examined for references to additional eligible studies.
2.2. Selection criteria
The inclusion criteria were a full-length article that provided sufficient data to enable evaluation of obesity on free flap failure or complications, a brief description of the reconstruction site, prospective or retrospective trials, and a brief explanation of outcome variables (free flap failure or complications). Studies were excluded if they involved incomplete or interim data, they were written in languages other than English, there was no information regarding the effects of obesity on free flap failure or complications, the article described fewer than ten cases, and there were overlapping authors.
2.3. Selection of relevant studies
Two of the authors (JYS and SGR) independently evaluated the eligibility of all the studies yielded by the literature search according to the predetermined selection criteria. The abstracts of all the studies were reviewed to exclude articles according to our exclusion criteria. Full-text reviews were performed to determine whether the remaining studies satisfied the inclusion criteria. Disagreements between the 2 evaluators were resolved by a third author (NHL).
2.4. Data extraction
Two of the authors independently extracted the outcomes from included studies. The predictor variables were obesity of patients (BMI > 30) in need of free flap reconstruction procedures. The outcome variables were partial flap loss, total flap loss, and complications.
2.5. Assessment of methodological quality
The methodological quality of the studies was assessed using the Newcastle-Ottawa scale (NOS) for nonrandomized studies. The parameters of the NOS comprise 3 categories, including selection of the study population, comparability of the groups, and ascertainment of the exposure or outcomes. Each parameter consists of subcategorized questions based on selection, comparability, and exposure or outcomes.[26,27] If the methodology of a study rated the highest quality, then the study was awarded a maximum of 9 stars. Two of the authors independently evaluated the methodological quality of all the studies. Subgroup analyses were performed according to reconstruction sites noted in the studies.
2.6. Statistical evaluation
Comprehensive Meta-Analysis software version 3.3.070 from Biostat (Borenstein M., Hedges L., Higgins J., and Rothstein H., Englewood, NJ) was used for this meta-analysis. The Cochrane Review Manager (RevMan version 5.3: The Cochrane Collaboration, Oxford, England) was also utilized to graphically represent the selected literature. We calculated the rate of both free flap failure and complications according to obesity status. The heterogeneity of each study was assessed using the I2 test, which measures the percentage of total variation across studies.[28] The heterogeneity measure, I2, was calculated as follows: I2 (%) = 100 × (Q − df)/Q, where Q is Cochrane heterogeneity statistic and df is the number of degrees of freedom. The 95% confidence interval (CI) was then computed for each treatment option using both random and fixed effects models. These results were confirmed by I2 tests. Significance was set at a value of P less than 0.05 in both models. We established forest plots to illustrate the effects of study size, and funnel plots to ascertain whether there was evidence of publication bias.
2.7. Ethical review
Institutional review board approval is not required for a meta-analysis.
3. Results
3.1. Identification of relevant studies
Figure 1 shows a flow diagram of how the eligible studies were investigated. Searches of the databases identified 944 publications that potentially met the study criteria. Duplicate records from 394 studies were excluded. The screening process, consisting of a review of titles and abstracts, excluded 263 studies that did not meet the inclusion criteria. A total of 287 articles were reviewed for eligibility by accessing the full text. The reasons for study exclusion during the final review were as follows: review articles (n = 6), incomplete data (n = 179), abstract only (n = 36), letter (n = 16), or case report (n = 31). The remaining 19 nonrandomized studies were included in the final analysis.
Figure 1.

Flow diagram for the identification of relevant studies.
3.2. Characteristics of studies included in the final analysis
Among the 19 studies, we identified a total of 10,269 patients that underwent free flap reconstruction procedures. Enrolled studies were divided into studies about breast reconstruction and nonbreast reconstruction. Each outcome was analyzed. In the included studies, 4770 patients who underwent breast reconstruction and 1684 patients who underwent nonbreast reconstruction were investigated. The clinical data and pooled analysis of the enrolled studies are shown in Tables 1 and 2. Only studies written in English were selected. All studies reported partial flap loss, total flap loss, or complications. In nonrandomized studies, the mean value awarded for quality was 7.3 (Table 3).
Table 1.
Clinical data of included studies.

Table 2.
Pooled analysis according to reconstruction site.

Table 3.
Methodological quality of included studies measured by Newcastle-Ottawa scale.

3.3. Overall impact of obesity in free flap procedures
The partial loss, total loss, and complication of free flap were occurred more frequently in obese patients compared than in nonobese patients. Total loss of free flaps and complications were significantly more common in obese patients (odds ratio = 1.910, P = 0.017 for flap loss, odds ratio = 2.024, P = 0.004 for complications) (Figs. 2–4).
Figure 2.

Forest plot comparing the incidence of partial flap loss between obese and nonobese patients in overall free flap surgeries.
Figure 4.

Forest plot comparing the incidence of complications between obese and nonobese patients in overall free flap surgeries.
Figure 3.

Forest plot comparing the incidence of total flap loss between obese and nonobese patients in overall free flap surgeries.
3.4. Subgroup analysis
3.4.1. Impact of obesity in breast reconstruction
Partial loss, total loss and complications of free flaps in breast reconstruction occurred significantly more frequently in obese patients than in nonobese patients (OR = 2.479, P = 0.021 for partial loss, OR = 3.083, P = 0.002 for total loss, OR = 2.666, P = 0.001 for complications) (Figs. 5–7).
Figure 5.

Forest plot comparing the incidence of partial flap loss between obese and nonobese patients in breast reconstruction.
Figure 7.
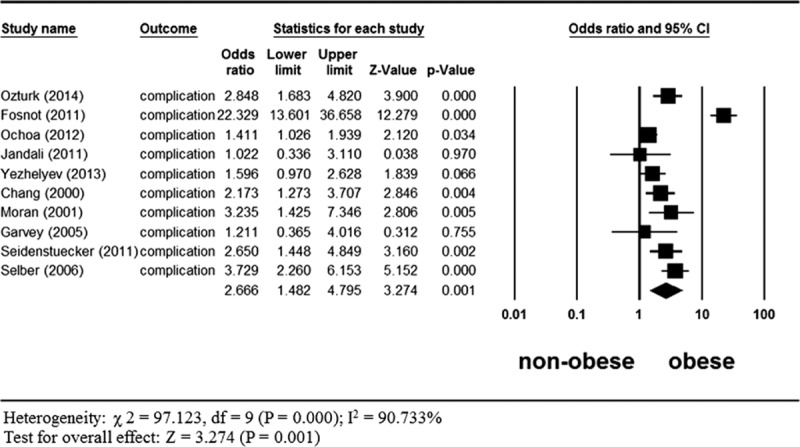
Forest plot comparing the incidence of complications between obese and nonobese patients in breast reconstruction.
Figure 6.

Forest plot comparing the incidence of total flap loss between obese and nonobese patients in breast reconstruction.
3.4.2. Impact of obesity in nonbreast reconstruction
Partial loss, total loss and complications in nonbreast reconstruction were not significantly different in obese patients in comparison to nonobese patients (OR = 0.786, P = 0.629 for partial loss, OR = 0.960, P = 0.961 for total loss, OR = 1.009, P = 0.536 for complications) (Figs. 8–10).
Figure 8.

Forest plot comparing the incidence of partial flap loss between obese and nonobese patients in nonbreast reconstruction.
Figure 10.

Forest plot comparing the incidence of complications between obese and nonobese patients in nonbreast reconstruction.
Figure 9.

Forest plot comparing the incidence of total flap loss between obese and nonobese patients in nonbreast reconstruction.
3.5. Publication bias
Funnel plots for the included studies are depicted in Figs. 11–13. These plots show low levels of asymmetry. Overall, there was no evidence of publication bias in this analysis.
Figure 11.

Funnel plot of direct-comparison meta-analysis for total flap loss in breast reconstruction.
Figure 13.

Funnel plot of direct-comparison meta-analysis for complications in nonbreast reconstruction.
Figure 12.

Funnel plot of direct-comparison meta-analysis for complications in breast reconstruction.
4. Discussion
This study identified the effect of obesity on the outcome of free flap surgeries from 19 studies,[1,15,19,21–24,29–40] which include a total of 10,269 patients. Obesity in overall free flap surgeries is identified as a meaningful risk factor for total flap loss and complications. However, these results reflect findings from a group of studies of which the majority are in breast reconstruction, so we performed subgroup analyses for only breast reconstruction patients and for patients who underwent procedures of reconstruction other than breast reconstruction.
In terms of breast reconstruction only, obesity has an important role as a predisposing factor for partial loss of flaps, total loss of flaps, and complications. These results are consistent with the results of many previous studies[15,17,33,41] and the danger of obesity in this context has been widely discussed. Obese patients frequently have comorbidities such as diabetes, hyperlipidemia, hypertension, and cardiovascular disease.[42,43] These diseases potentially compromise microvascular hemodynamics, which could lead to flap loss and complications. Therefore, we are not able to conclude precisely which factor leads to eventual flap loss and complications. It is clear, however, that surgeons should take particular care with obese patients because of the high rate of flap loss and complications among obese patients. Fortunately, the majority of these complications in obese patients tend to be minor and not to require reoperation.[35,44] In addition, the outcomes of implant-based breast reconstruction in obese patients tend to be poor in comparison to the outcomes of breast reconstruction with free flap surgery.[45,46] Accordingly, free flap surgeries are mainly performed in obese patients in spite of the possible complications.
In the group of patients who underwent nonbreast reconstruction, reconstruction sites included the head, neck, and lower leg. Subgroup analysis was performed in 5 studies[1,22–24,40] representing a total of 1684 patients. This subgroup analysis showed no significant differences in partial loss of flaps, total loss of flaps, and complications between obese and nonobese patients. Several previous studies have asserted that the relationship between obesity and the outcomes of free flap surgeries in nonbreast reconstruction is not relevant, even though the mechanism of the association is unclear. In fact, previous studies acknowledge that a relatively lower body mass index or recent weight loss are independent risk factors for poor outcomes in nonbreast reconstruction,[22] because these variables may be a reflection of poor nutritional status and general health status. In addition, being overweight has been associated with improved long-term survival and recurrence rates in patients with head and neck cancer.[47,48]
According to the results of our meta-analysis, whether or not obesity is a risk factor for free flaps changes according to the site of reconstruction. Our results that identified obesity as a risk factor in breast reconstruction provide necessity of knowing difference between breast and nonbreast reconstruction. Free flap in breast reconstruction was usually performed by abdomen-based autologous free flap compared with nonbreast reconstruction. Large and heavy abdominal flaps in obese patients attenuate the perforators, and thus, may eventually compromise blood supply to the flap.[49] Careful attention in insetting the flap may prevent potential stretching, together with recommended securing of the flap to the chest wall with sutures.[35] In addition, the larger donor site can be technically harder to dissect and prevent tension in harvest process. Furthermore, impaired wound healing owing to decreased myofibroblast activity may predispose obese patients to wound complications.[42]
This is the first meta-analysis relating to obesity as a predisposing factor for outcomes in breast and nonbreast reconstruction. The strength of this study is its rigorous search of recent literature. Subgroup analyses were performed to confirm the robustness of results. Despite the strengths, there are some limitations to the present study. Although all the included studies were high in quality according to their NOS scores, no studies were adequately powered by randomized controlled. Randomized studies on this topic, together with large-scale, well-organized, long-term follow-up studies are needed to confirm our findings. Also, there are fewer studies about nonbreast reconstruction than about breast reconstruction, which is a potential source of bias.
5. Conclusion
This study demonstrates that obesity is not a predisposing factor for poor outcomes in nonbreast reconstruction, unlike the association of obesity and poor outcomes in free flap breast reconstruction. Future large-scale and randomized studies with sufficient follow-up should be conducted to clarify this finding.
Footnotes
Abbreviation: NOS = Newcastle-Ottawa scale.
This paper was supported by research funds of Chonbuk National University In 2016.
The authors have no conflicts of interest to disclose.
References
- 1.Chang EI, Zhang H, Liu J, et al. Analysis of risk factors for flap loss and salvage in free flap head and neck reconstruction. Head Neck 2016; 38 suppl 1:E771–E775. [DOI] [PubMed] [Google Scholar]
- 2.Bourget A, Chang JT, Wu DB, et al. Free flap reconstruction in the head and neck region following radiotherapy: a cohort study identifying negative outcome predictors. Plast Reconstr Surg 2011; 127:1901–1908. [DOI] [PubMed] [Google Scholar]
- 3.Ohtsuka H, Fujita K, Shioya N. Replantations and free flap transfers by microvascular surgery. Plast Reconstr Surg 1976; 58:708–712. [DOI] [PubMed] [Google Scholar]
- 4.Suominen S, Asko-Seljavaara S. Free flap failures. Microsurgery 1995; 16:396–399. [DOI] [PubMed] [Google Scholar]
- 5.Rao SS, Parikh PM, Goldstein JA, et al. Unilateral failures in bilateral microvascular breast reconstruction. Plast Reconstr Surg 2010; 126:17–25. [DOI] [PubMed] [Google Scholar]
- 6.Bozikov K, Arnez ZM. Factors predicting free flap complications in head and neck reconstruction. J Plast Reconstr Aesthet Surg 2006; 59:737–742. [DOI] [PubMed] [Google Scholar]
- 7.Miller RB, Reece G, Kroll SS, et al. Microvascular breast reconstruction in the diabetic patient. Plast Reconstr Surg 2007; 119:38–45.discussion 38–46. [DOI] [PubMed] [Google Scholar]
- 8.Serletti JM, Higgins JP, Moran S, et al. Factors affecting outcome in free-tissue transfer in the elderly. Plast Reconstr Surg 2000; 106:66–70. [DOI] [PubMed] [Google Scholar]
- 9.Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983; 67:968–977. [DOI] [PubMed] [Google Scholar]
- 10.Luder E, Ehrlich RI, Lou WY, et al. Body mass index and the risk of asthma in adults. Respir Med 2004; 98:29–37. [DOI] [PubMed] [Google Scholar]
- 11.Nystrom PO, Jonstam A, Hojer H, et al. Incisional infection after colorectal surgery in obese patients. Acta Chir Scand 1987; 153:225–227. [PubMed] [Google Scholar]
- 12.de Oliveira AC, Ciosak SI, Ferraz EM, et al. Surgical site infection in patients submitted to digestive surgery: risk prediction and the NNIS risk index. Am J Infect Control 2006; 34:201–207. [DOI] [PubMed] [Google Scholar]
- 13.Willett WC, Dietz WH, Colditz GA. Guidelines for healthy weight. N Engl J Med 1999; 341:427–434. [DOI] [PubMed] [Google Scholar]
- 14.Sjostrom LV. Morbidity of severely obese subjects. Am J Clin Nutr 1992; 55 (suppl. 2):508S–515S. [DOI] [PubMed] [Google Scholar]
- 15.Berrino P, Campora E, Leone S, et al. The transverse rectus abdominis musculocutaneous flap for breast reconstruction in obese patients. Ann Plast Surg 1991; 27:221–231. [DOI] [PubMed] [Google Scholar]
- 16.Kroll SS, Netscher DT. Complications of TRAM flap breast reconstruction in obese patients. Plast Reconstr Surg 1989; 84:886–892. [DOI] [PubMed] [Google Scholar]
- 17.Vyas RM, Dickinson BP, Fastekjian JH, et al. Risk factors for abdominal donor-site morbidity in free flap breast reconstruction. Plast Reconstr Surg 2008; 121:1519–1526. [DOI] [PubMed] [Google Scholar]
- 18.Momeni A, Ahdoot MA, Kim RY, et al. Should we continue to consider obesity a relative contraindication for autologous microsurgical breast reconstruction? J Plast Reconstr Aesthet Surg 2012; 65:420–425. [DOI] [PubMed] [Google Scholar]
- 19.Ochoa O, Chrysopoulo M, Nastala C, et al. Abdominal wall stability and flap complications after deep inferior epigastric perforator flap breast reconstruction: does body mass index make a difference? Analysis of 418 patients and 639 flaps. Plast Reconstr Surg 2012; 130:21e–33e. [DOI] [PubMed] [Google Scholar]
- 20.Spear SL, Ducic I, Cuoco F, et al. Effect of obesity on flap and donor-site complications in pedicled TRAM flap breast reconstruction. Plast Reconstr Surg 2007; 119:788–795. [DOI] [PubMed] [Google Scholar]
- 21.Selber JC, Kurichi JE, Vega SJ, et al. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg 2006; 56:492–497. [DOI] [PubMed] [Google Scholar]
- 22.Patel RS, McCluskey SA, Goldstein DP, et al. Clinicopathologic and therapeutic risk factors for perioperative complications and prolonged hospital stay in free flap reconstruction of the head and neck. Head Neck 2010; 32:1345–1353. [DOI] [PubMed] [Google Scholar]
- 23.de la Garza G, Militsakh O, Panwar A, et al. Obesity and perioperative complications in head and neck free tissue reconstruction. Head Neck 2016; 38 suppl 1:E1188–E1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cleveland EC, Fischer JP, Nelson JA, III, et al. Free flap lower extremity reconstruction in the obese population: does weight matter? J Reconstr Microsurg 2014; 30:263–270. [DOI] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25:603–605. [DOI] [PubMed] [Google Scholar]
- 27.Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003; 7:iii–x.1–173. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 29.Wong AK, Joanna Nguyen T, Peric M, et al. Analysis of risk factors associated with microvascular free flap failure using a multi-institutional database. Microsurgery 2015; 35:6–12. [DOI] [PubMed] [Google Scholar]
- 30.Ozturk CN, Kundu N, Bernard S, et al. Breast reconstruction with abdominal-based free flaps in high body mass index population: postoperative complications and impact of weight loss. Ann Plast Surg 2014; 72:13–22. [DOI] [PubMed] [Google Scholar]
- 31.Offodile AC, Aherrera A, II, Wenger J, et al. Impact of increasing operative time on the incidence of early failure and complications following free tissue transfer? A risk factor analysis of 2,008 patients from the ACS-NSQIP database. Microsurgery 2015; doi: 10.1002/micr.22387. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 32.Fosnot J, Jandali S, Low DW, III, et al. Closer to an understanding of fate: the role of vascular complications in free flap breast reconstruction. Plast Reconstr Surg 2011; 128:835–843. [DOI] [PubMed] [Google Scholar]
- 33.Jandali S, Nelson JA, Sonnad SS, et al. Breast reconstruction with free tissue transfer from the abdomen in the morbidly obese. Plast Reconstr Surg 2011; 127:2206–2213. [DOI] [PubMed] [Google Scholar]
- 34.Yezhelyev M, Duggal CS, Carlson GW, et al. Complications of latissimus dorsi flap breast reconstruction in overweight and obese patients. Ann Plast Surg 2013; 70:557–562. [DOI] [PubMed] [Google Scholar]
- 35.Chang DW, Wang B, Robb GL, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg 2000; 105:1640–1648. [DOI] [PubMed] [Google Scholar]
- 36.Moran SL, Serletti JM. Outcome comparison between free and pedicled TRAM flap breast reconstruction in the obese patient. Plast Reconstr Surg 2001; 108:1954–1960.discussion 1952–1961. [DOI] [PubMed] [Google Scholar]
- 37.Mirzabeigi MN, Wilson AJ, Fischer JP, et al. Predicting and managing donor-site wound complications in abdominally based free flap breast reconstruction: improved outcomes with early reoperative closure. Plast Reconstr Surg 2015; 135:14–23. [DOI] [PubMed] [Google Scholar]
- 38.Garvey PB, Buchel EW, Pockaj BA, et al. The deep inferior epigastric perforator flap for breast reconstruction in overweight and obese patients. Plast Reconstr Surg 2005; 115:447–457. [DOI] [PubMed] [Google Scholar]
- 39.Seidenstuecker K, Munder B, Mahajan AL, et al. Morbidity of microsurgical breast reconstruction in patients with comorbid conditions. Plast Reconstr Surg 2011; 127:1086–1092. [DOI] [PubMed] [Google Scholar]
- 40.Lim YS, Kim JS, Kim NG, et al. Free flap reconstruction of head and neck defects after oncologic ablation: one surgeon's outcomes in 42 cases. Arch Plast Surg 2014; 41:148–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paige KT, Bostwick J, Bried JT, III, et al. A comparison of morbidity from bilateral, unipedicled and unilateral, unipedicled TRAM flap breast reconstructions. Plast Reconstr Surg 1998; 101:1819–1827. [DOI] [PubMed] [Google Scholar]
- 42.Fischer JP, Nelson JA, Sieber B, et al. Free tissue transfer in the obese patient: an outcome and cost analysis in 1258 consecutive abdominally based reconstructions. Plast Reconstr Surg 2013; 131:681e–692e. [DOI] [PubMed] [Google Scholar]
- 43.Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg 2013; 217:656–664. [DOI] [PubMed] [Google Scholar]
- 44.Garvey PB, Villa MT, Rozanski AT, et al. The advantages of free abdominal-based flaps over implants for breast reconstruction in obese patients. Plast Reconstr Surg 2012; 130:991–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Atisha DM, Alderman AK, Kuhn LE, et al. The impact of obesity on patient satisfaction with breast reconstruction. Plast Reconstr Surg 2008; 121:1893–1899. [DOI] [PubMed] [Google Scholar]
- 46.McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008; 121:1886–1892. [DOI] [PubMed] [Google Scholar]
- 47.Gaudet MM, Patel AV, Sun J, et al. Prospective studies of body mass index with head and neck cancer incidence and mortality. Cancer Epidemiol Biomarkers Prev 2012; 21:497–503. [DOI] [PubMed] [Google Scholar]
- 48.Arthur AE, Peterson KE, Rozek LS, et al. Pretreatment dietary patterns, weight status, and head and neck squamous cell carcinoma prognosis. Am J Clin Nutr 2013; 97:360–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scheflan M, Kalisman M. Complications of breast reconstruction. Clin Plast Surg 1984; 11:343–350. [PubMed] [Google Scholar]


