Introduction
Frostbite is a feared manifestation of cold injury to the troops deployed in extreme cold areas. We report two cases of severe frost bite affecting the face. The rarity of such cases and their unique management prompted us to report these cases.
Case 1
A 36 year old serving officer, deployed at a forward post in high altitude reported to the hospital with the history of sustaining cold injury following exposure to his face. The officer had been on a night patrol and inadvertently exposed both face and ears to the chilly winds. He reported that when he got up the next day he noticed black discoloration of both the ears as well as parts of the face. There were few blisters on the ears. On arrival he was suffering from second to third degree frostbite of the pinna (Fig. 1) and first-degree frostbite of the face. There was no evidence of any gangrenous areas. The sensation was lost on most of the pinna. The patient was started on oral antibiotics and vasodilators (tablet pentoxyphylline). Frequent dressings of the wounds and debridement of the necrotic areas was also undertaken. The blisters were left untouched. Antioxidants and thromboxane inhibitors in the form of brufen were added. An ointment of 10% aloe vera and vitamin E were applied topically thrice a day. The patient showed good response and most of the blisters and wounds had resolved by the end of three weeks. On follow up after four weeks, both ears and face were normal except for marginal reduction in size of ear lobule.
Fig. 1.

Frostbite of the right pinna showing gangrenous area along the helix before (left) and after treatment (right).
Case 2
A 22 year old serving non commissioned officer performing duties in a helicopter base was constantly exposed to chilly gusts of icy subzero winds thrown up by the rotors of the helicopters. He often felt pain and numbness in his hands and toes but was surprised to notice a blister on the tip of his nose one day. After another two days of exposure, he saw a painless raw area on the tip of his nose. He reported to the hospital where he was found to be suffering from second degree frostbite of the nasal tip. On examination, there was a 5 × 5mm shallow ulcer with sero-sanguinous discharge (Fig. 2). There was pain on deep pressure only. The sensory sensation was blunted over the nasal tip area. The patient was given oral antibiotics along with antiinflammatory drugs and oral vasodilators (tablet pentoxyphylline). An ointment of 10% aloe vera and vitamin E was applied topically. Frequent warm saline dressings were done though no debridement was required. The patient showed good response and most of the blisters and wounds had resolved at the end of three weeks with no residual disfigurement.
Fig. 2.
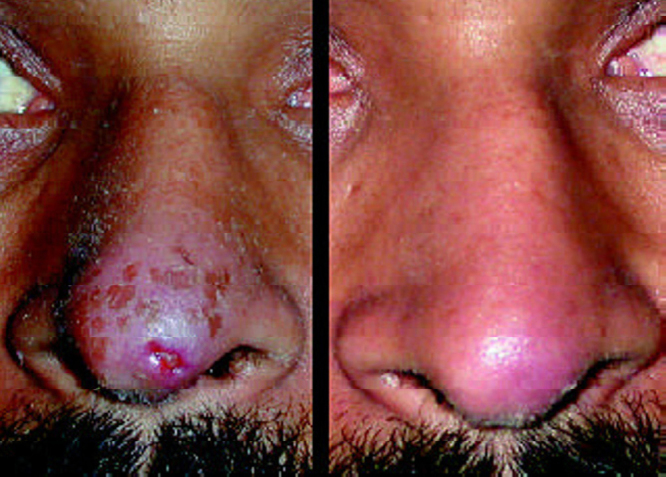
Frostbite on the tip of the nose showing a shallow ulcer before (left) and after treatment (right).
Discussion
Cold injuries are a significant cause of morbidity amongst soldiers deployed in extreme cold climate. Most of these injuries take the form of frostbite of the extremities. Though the head and neck region are constantly exposed to the cold climate and chilly winds, second and third degree frostbite of this region is uncommon. Hashmi et al [1], have reported a 3% incidence for frostbite in the head and neck region in a retrospective study of over 1500 cases of frostbite in the Karakoram mountains over ten years. The tip of the nose and the pinna are commonly affected with frostnip, a condition characterised by painful swelling and erythematous discoloration. Current methods used to treat cases of frostbite include gradual rewarming, antiinflammatory drugs, hyperbaric oxygen, vasodilators and surgical debridement. The role of nonconventional treatment modalities in the form of topical applications of aloe vera extracts has not been fully established though scientific evidence exists towards its protective role. The mechanism of action and active ingredient responsible for the results remains debatable. Aloe vera is known to contain several pharmacologically active ingredients, including a carboxypeptidase that inactivates bradykinin in vitro, salicylates, and a substance(s) that inhibit thromboxane formation in vivo [2]. Vazquez et al [3], demonstrated anti-inflammatory responses on aloe vera extract and suggested its inhibitory action on the arachidonic acid pathway via cyclo-oxygenase. Others have suggested aloe gel as a thromboxane inhibitor and therefore considered beneficial in frost bite cases [4].
The use of pentoxyphylline in frostbite is not supported by controlled human clinical trials but is a commonly used agent in cases of frostbite. Hayes et al [5], have mentioned it as an important adjunctive treatment in frostbite and attribute it to increased RBC flexibility allowing easier vascularisation. Miller et al [6], studied the efficacy of aloe vera cream and pentoxyphylline on experimentally induced frostbites in rabbit ears. Tissue survival was notably improved with pentoxifylline (20%), better with aloe vera cream (24%), and the best results obtained with the combination therapy (30%) as compared to only 6% in controls.
We combined systemic synthetic pentoxyfylline with topical administration of 10% ointment of aloe vera and vitamin E in an effort to minimize tissue loss and scarring. Both the cases showed excellent healing response with minimal scarring and no residual deformity. Aloe vera thus offers an exciting option in treatment of this condition. Though minimal evidence exists in using it as a stand-alone treatment modality, it can be an excellent adjunctive measure. The additional advantage gained by aloe vera and pentoxyfylline cannot be conclusively proved in the absence of a controlled clinical trial. The role of topical aloe vera extracts therfore needs consideration in management of frostbite of the face.
Conflicts of Interest
None identified
References
- 1.Hashmi MA, Rashid M, Haleem A, Bokhari SA, Hussain T. Frostbite: Epidemiology at high altitude in the Karakoram mountains. Ann R Coll Surg Engl. 1998;80:91–95. [PMC free article] [PubMed] [Google Scholar]
- 2.Klien AD, Penneys NS. Aloe Vera. J Am Acad Dermatol. 1998;19:82. doi: 10.1016/s0190-9622(88)70095-x. [DOI] [PubMed] [Google Scholar]
- 3.Vazquez B, Avila G, Segura D, Escalante B. Anti-inflammatory activity of extracts from Aloe vera gel. J Ethnopharmacol. 1996;55:69–75. doi: 10.1016/s0378-8741(96)01476-6. [DOI] [PubMed] [Google Scholar]
- 4.McCauley RL, Heggers JP, Robson MC. Frostbite. Methods to minimize tissue loss. Postgrad Med. 1990;88:67–68. doi: 10.1080/00325481.1990.11704769. [DOI] [PubMed] [Google Scholar]
- 5.Hayes DW, Jr, Mandracchia VJ, Considine C, Webb GE. Pentoxifylline Adjunctive therapy in the treatment of pedal frostbite. Clin Podiatr Med Surg. 2000;17:715–722. [PubMed] [Google Scholar]
- 6.Miller MB, Koltai PJ. Treatment of experimental frostbite with pentoxifylline and aloe vera cream. Arch Otolaryngol Head Neck Surg. 1995;121:678–680. doi: 10.1001/archotol.1995.01890060076015. [DOI] [PubMed] [Google Scholar]


