Abstract
Objective
Anatomic volar rim locking plates are designed with the aim of treating intraarticular distal radius fractures. When used to treat comminuted distal radius fractures, these plates can damage the flexor tendons.
In this study, we sought to determine the radiological and functional results and rate of complications of these plates.
Methods
We retrospectively reviewed the records of 36 patients (28 males, 8 females; mean age: 46.4 years) with AO/OTA Type C2-C3 distal radius fractures treated with anatomic volar rim distal radius plates between January 2011 and December 2014. Radial length, radial inclination and palmar tilt were compared with the intact wrist. Results were evaluated with the Mayo wrist and Lidstrom scores. Complications were documented throughout the follow-up period of 23.8 (range: 12 to 48) months.
Results
Postoperative measurements of the radial length, inclination and palmar tilt did not differ significantly. Mayo wrist and Lidstrom scores were good and excellent in 27 and 32 patients, respectively. Flexor tenosynovitis was symptomatic in 15 patients and asymptomatic (localized swelling only) in 21. Plates were removed from 15 patients due to symptomatic tenosynovitis and from six patients due to partial rupture of the flexor pollicis longus tendon. The flexor digitorum profundus tendon of the second finger was also partially ruptured in three patients.
Conclusion
Anatomic volar rim locking plates provide satisfying radiological and functional results in treating AO/OTA Type C2-C3 comminuted distal radius fractures. However, if these plates interfere with the union of the fracture, they should be removed to avoid potential tendon problems caused by their placement in the rim region.
Level of Evidence: Level IV, Therapeutic study
Keywords: Distal radius fracture, Flexor tendon complications, Intraarticular fracture, Volar plating
Intra-articular fractures of the distal radius generally have a worse prognosis than unstable extra-articular fractures.1 Due to the anterior tilt of the lunate facet, distal radial fractures involving the watershed line and the volar rim, and the coronal type of lunate facet fractures are hard to support and stabilize against shearing forces after fixation of distal fragments. In these types of fractures, conventional locked plates cannot provide butress effect. Fragment-specific plates and wire loop fixation techniques are used for fixation of small intraarticular fragments.2, 3 Anatomic volar rim plates (2.4-mm, variable angle LCP volar rim distal radius plate; Synthes Inc., Oberdorf, Switzerland) are designed to provide butress effect over the anatomical volar rim as an alternative to these methods.
In addition to providing a stable fixation, volar locking plates may compress and damage the flexor tendons.4, 5, 6 To avoid flexor tendon problems, some surgeons recommend keeping the plates proximal to the volar rim.7 However, this practice may not always be possible in comminuted fractures with multiple intraarticular fragments in the distal bone.8, 9, 10
We retrospectively assessed the radiological and functional results of patients with comminuted AO/OTA Type C2-C3 distal radius fractures treated with anatomic volar rim locking plates in order to determine the rate and nature of complications.
Patients and methods
We reviewed the records of all patients with comminuted AO/OTA Type C2-C3,11 intraarticular, segmental, distal radius fractures treated with open reduction and internal fixation using an anatomic volar rim distal radius plate (2.4-mm, variable angle LCP volar rim distal radius plate) between January 2011 and December 2014.
Of the 55 patients meeting the eligibility criteria, 10 with volar and dorsal plating, two with bilateral distal radius fractures, one with a contralateral forearm fracture, two with ipsilateral radioulnar instability, and four patients lost to follow-up were excluded from the analysis. The 36 evaluable patients (28 males, 8 females) had a mean age of 46.4 (range: 22–69) years.
Informed consent was taken from each patient before enrollment. Standard anteroposterior and lateral radiographs were obtained for both wrists before, immediately after, and at least 12 months after surgery (Fig. 1).
Fig. 1.
(a, b) Preoperative and (c, d) 14-month postoperative anteroposterior and lateral views of the left wrist of a 39-year-old man treated with a volar locking rim plate.
Surgical indications were an intraarticular step-off of more than 1 mm, a dorsal tilt more than 10°, and a radius more than 2 mm shorter than the contralateral one on the radiographs obtained after closed repositioning performed in the emergency department.12 All patients underwent three-dimensional computed tomography (CT) to guide surgical planning. Fracture involving the volar rim and the lunate facet was confirmed by CT imaging.
A flexor carpi radialis approach was taken in all surgeries. After elevating the pronator quadratus muscle and restoring the articulation, the small and main fragments were fixed temporarily with Kirschner wires. Plates were then positioned distal to the volar rim in order to fix and support the fractured fragments. The distal screws were placed as close as possible to the subchondral bone, and potential articular penetrations were avoided by diverting them 15° proximally. Plate placement was done according to the suggested surgical technique (Fig. 2).13 The prominence of screws with the articular and dorsal cortex penetrations was evaluated by dorsal horizontal intraoperative fluoroscopy and by tangential imaging at 20 degrees of elevation.
Fig. 2.
Images of a 36-year-old man with AO/OTA Type C3 distal radius fracture. (a) Peroperative view of the volar rim and (b) position of the plate. (c) A 15-degree Kirschner wire was used as reference for screw angulation by using fluoroscopy.
After fixation, we tried to cover the plate with the pronator quadratus muscle. No patient received bone grafts.
The wrist was immobilized postoperatively with a plaster-splint on the volar surface. Splints were removed after the soft tissue healed, and then active finger and wrist exercises were begun. All patients received physiotherapy after discharge from the hospital.
Functional and radiological findings were recorded during follow-up visits on the 3rd, 6th, and 12th weeks and on the 6th, 12th, and 24th months after discharge. Wrist motions were measured with a goniometer. Functional results were evaluated with the Mayo wrist score.14 Radiological results were evaluated with Lidstrom scores modified by Sarmiento.15 Radius length and inclination and the palmar tilt were compared with the intact wrist. When diagnosing radiological fracture union, bone bridgings on the radial, ulnar, and dorsal cortices were considered. A fracture union time greater than six months was considered to indicate non-union.
Grip strength was measured with a dynamometer (Jamar; Therapeutic Equipment Corp., Clifton, NJ, USA). Symptomatic tenosynovitis was diagnosed due to the presence of localized swelling, sensitivity on palpation, crepitation induced by finger movement, loss of active motion, and weakness in the fingers.16 Patients with only localized swelling were considered to have asymptomatic tenosynovitis. Other complications that developed during follow-up were recorded.
The data were analyzed with the Number Cruncher Statistical System software 2007 (NCSS, LLC, Kaysville, Utah, USA). The data were described with either means and standard deviations or medians and interquartile ranges. The operated and contralateral sides were compared with the Wilcoxon signed-rank test for the non-normally distributed variables.
Results
According to the AO/OTA classification, all fractures were Type C (C3 in 23 and C2 in 13 patients).11 The cause of the fractures was a simple fall on the hand in 26 cases, traffic accidents in five, and fall from height in five.
According to the Gustilo-Anderson open fracture classification, five patients had a Type 1 open fracture and one had a Type 2 open fracture. The dominant hand was involved in 28 patients. In addition, three patients had a proximal femur fracture, two had a tibial plateau fracture, and one had a tibial shaft fracture. The mean time from hospital admission to surgery was 4.4 (range: 1–8) days.
Mean follow-up period was 23.8 (range: 12–48) months. Mayo wrist scores were excellent in 10 patients (28%), good in 17 (47%), moderate in five (14%) and poor in four (11%).
On the final follow-up visit, the grip strength was 76% of the uninvolved hand.
Radiographs indicated that union occurred in all fractures at a mean of 14 (range: 12–16) weeks. There was no statistically significant difference in terms of radial length, radial inclination or palmar tilt (p > 0.05) (Table 1).
Table 1.
Radiological evaluations of both wrists.
| Involved wrist (n = 36) | Intact wrist (n = 36) | p* | ||
|---|---|---|---|---|
| Radius length in mm | Min–Max (Median) | 8–15 (12) | 10–16 (12) | 0.138 |
| Mean ± SD | 11.64 ± 1.53 | 11.73 ± 1.53 | ||
| Radial inclination in degrees | Min–Max (Median) | 17–30 (22) | 18–30 (22) | 0.524 |
| Mean ± SD | 21.86 ± 2.50 | 22.03 ± 2.29 | ||
| Palmar tilt in degrees | Min–Max (Median) | 10–20 (14) | 11–22 (14) | 0.691 |
| Mean ± SD | 14.86 ± 2.94 | 15.13 ± 2.76 | ||
∗Wilcoxon signed-rank test.
The modified Lidstrom radiological scores were excellent in 18 patients (50%), good in 14 (39%), moderate in three (8%) and poor in one (3%).
No patient had early wound problems or superficial or deep infections. No plate breakage, screw loosening, or articular penetration was detected in any patient. Among 15 of 36 patients (42%) with symptomatic flexor tenosynovitis (swelling on the volar side of the wrist and pain during thumb movements), three had active flexion weakness of the thumb and second finger and three had active flexion weakness of the thumb (Fig. 3). Twenty-one of 36 patients (58%) had asymptomatic flexor tenosynovitis, characterized by only localized swelling, without restricted movement or pain. The plates were removed from 15 patients with symptomatic flexor tenosynovitis after a mean period of 20 (range: 10–32) months after surgery. During the plate removal, severe synovitis around the median nerve and flexor tendons was observed in all patients. Degeneration and partial rupture were detected in the flexor pollicis longus (FPL) tendon in six patients, and among them, three had additional partial rupture of the second finger flexor digitorum profundus tendon (Fig. 4).
Fig. 3.

Fourteen months after surgery, swelling on the wrist of the patient from Fig. 1 can be seen as he makes a fist.
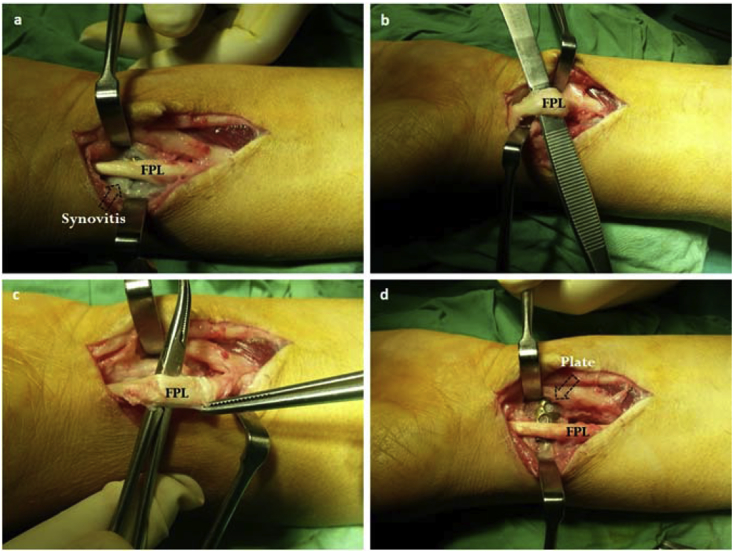
Fig. 4.
Removal of the volar plate from the patient in Fig. 1, 18 months after placement, to reduce symptomatic tenosynovitis. (a) Synovitis around the plate. (b) Synovitis on the flexor pollicis longus (FPL) tendon. (c) Partial rupture on the FPL tendon. (d) Contact of the FPL tendon with the volar plate.
In addition to synovectomy, the FPL tendon was repaired in four patients, with ruptures exceeding 60% of the tendon width (Fig. 5).17 No patient required tendon grafting. Patients who underwent tendon repair wore wrist splints for four weeks, others were followed without splinting throughout the postoperative period. Patients reported that the FPL tendon symptoms had resolved in a mean of 3.9 (range: 2–5) months. Although the plate removal was recommended for patients with asymptomatic tenosynovitis, none chose to have the plate removed. Complex regional pain syndrome developed in two patients who were treated with physiotherapy and oral analgesics. In three patients, carpal tunnel syndrome was diagnosed. All three patients had undergone plate extraction for symptomatic tenosynovitis and were additionally treated with carpal tunnel release which yielded successful results.
Fig. 5.
(a) Loss of flexion in the second finger caused by plate-induced tendon damage. (b) Extensive synovitis around the median neuron and flexor tendons. (c) Synovitis around the deep flexor tendons. (d) Partial tendon damage (>60%) in the second finger flexor.
Discussion
Anatomic reduction and rigid fixation are the main goals in the intraarticular fracture treatment.18 In a review of suitable fixation methods for different types of fractures, volar locking plates have been recommended for comminuted AO/OTA Type C2-C3 fractures.19
Third-generation plates have introduced the distal polyaxial locking screws and fourth-generation plates have provided optimal placement on the radial surface with anatomical structures compatible with the lateral colon in more distal part compared to the medial colon.20, 21 To date, studies on different types of volar locking plates have not addressed the results of anatomic volar rim plates. Volar plates placed distal to the volar rim may cause progressive tenosynovitis and tendon ruptures by compressing the flexor tendons.7, 10, 22 An ultrasonographic study on anatomic volar rim plates revealed 1.3 mm distance between the FPL tendon and volar rim in the intact wrist.23 Because of this close relationship between the tendon and the volar rim, it is highly probable to see tendinous problems with plates used in this region. In our study of distal radius intraarticular comminuted fractures treated with anatomic volar rim distal plates, the short-term follow-up revealed a complication rate related to the flexor tendons in all patients, of which 15 were symptomatic.
In addition to plate location, plate and tendon compression caused by malreduction may cause flexor tendon problems.4 In 15 patients with tendon problems, Lidstrom scores were excellent in nine and good in four. In light of these data, we believe that tendon complications were related to the plate localization.
Although tendon complications from plates located distal to the volar rim have been reported, such placement is inevitable in fractures requiring fragment fixation and support of the volar surface of the lunate fossa, particularly in comminuted intraarticular fractures (AO/OTA Type C2-C3) with small fragments in the distal radial colon.8, 9, 10 A biomechanical study reported that distal screws should be located as distally as possible in the subchondral region to prevent radial shortening.24 In distal radius fractures including the lunate facet and the volar rim, it has been suggested that the plate should be located distally as far as possible to prevent this region from collapsing.25, 26
The distal part of the plates we used in our study was inclined and provided excellent support for distal fragments. This part has a low profile, and the screw heads are flush with the surface, preventing soft tissue compression. Also, a second line of distal screws and the radial styloid allowed fixation of the lunate facet and distal radioulnar joint. The variable-angle option of the distal screws enabled them to be placed far from the joint, even though the plate was placed distally.
We found no radiological evidence of loss of reduction, indicating that these plates provided stabile and rigid fixation in the segmental, intraarticular fractures. We obtained excellent and good functional results at a rate of 75% using the Mayo wrist score. However, in addition to all the advantages mentioned above, problems with these plates may occur after treatment. The most common complications are related to tendons, but complex regional pain syndrome and carpal tunnel syndrome have also been observed. If the fracture requires the implant to be located distally, we recommend close follow-up and plate removal if signs of flexor tendon irritation appear.5, 9
Our study was limited by its retrospective nature and small sample size. Also, we evaluated only the short-term results. Another limitation was that the plates used were not compared with other plates. It should be noted that open fractures in our study caused the poor functional results. Larger scale studies comparing the results of the volar rim plates used in AO/OTA Type C2-C3 distal radius fractures with those of different types of plates are needed.
In conclusion, anatomic volar rim locking plates provide satisfactory radiological and functional results in treating AO/OTA Type C2-C3 comminuted distal radius fractures. However, if these plates interfere with the union of the fracture, they should be removed to avoid potential tendon problems caused by their placement in the rim region.
References
- 1.Cooney W.P., 3rd, Linscheid R.L., Dobyns J.H. External pin fixation for unstable Colles' fractures. J Bone Jt Surg Am. 1979;61:840–845. [PubMed] [Google Scholar]
- 2.Chin K.R., Jupiter J.B. Wire-loop fixation of volar displaced osteochondral fractures of the distal radius. J Hand Surg Am. 1999;24:525–533. doi: 10.1053/jhsu.1999.0525. [DOI] [PubMed] [Google Scholar]
- 3.Bakker A.J., Shin A.Y. Fragment-specific volar hook plate for volar marginal rim fractures. Tech Hand Up Extrem Surg. 2014;18:56–60. doi: 10.1097/BTH.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 4.Asadollahi S., Keith P.P. Flexor tendon injuries following plate fixation of distal radius fractures: a systematic review of the literature. J Orthop Traumatol. 2013;14:227–234. doi: 10.1007/s10195-013-0245-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drobetz H., Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casaletto J.A., Machin D., Leung R., Brown D.J. Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur Vol. 2009;34:471–474. doi: 10.1177/1753193408100964. [DOI] [PubMed] [Google Scholar]
- 7.Jupiter J.B., Marent-Huber M., Group L.C.P.S. Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. Surg Tech J Bone Jt Surg Am. 2010;92(Suppl 1 Pt 1):96–106. doi: 10.2106/JBJS.I.01340. [DOI] [PubMed] [Google Scholar]
- 8.Suganuma S., Tada K., Tsuchiya H. Reducing the risk of flexor pollicis longus tendon rupture after volar plate fixation for distal radius fractures: validation of the tendon irritation test. Eur J Orthop Surg Traumatol. 2014;24:1425–1429. doi: 10.1007/s00590-014-1420-5. [DOI] [PubMed] [Google Scholar]
- 9.Arora R., Lutz M., Hennerbichler A., Krappinger D., Espen D., Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–322. doi: 10.1097/BOT.0b013e318059b993. [DOI] [PubMed] [Google Scholar]
- 10.Konstantinidis L., Helwig P., Strohm P.C., Hirschmuller A., Kron P., Sudkamp N.P. Clinical and radiological outcomes after stabilisation of complex intra-articular fractures of the distal radius with the volar 2.4 mm LCP. Arch Orthop Trauma Surg. 2010;130:751–757. doi: 10.1007/s00402-009-0990-x. [DOI] [PubMed] [Google Scholar]
- 11.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium – 2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 12.Osada D., Kamei S., Masuzaki K., Takai M., Kameda M., Tamai K. Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg Am. 2008;33:691–700. doi: 10.1016/j.jhsa.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 13.http://synthes.vo.llnwd.net/o16/LLNWMB8/US Mobile/Synthes North America/Product Support Materials/Technique Guides/SUTG2.4VALCPVolarRimDRPJ10270C.pdf.
- 14.Amadio P.C., Berquist T.H., Smith D.K., Ilstrup D.M., Cooney W.P., 3rd, Linscheid R.L. Scaphoid malunion. J Hand Surg Am. 1989;14:679–687. doi: 10.1016/0363-5023(89)90191-3. [DOI] [PubMed] [Google Scholar]
- 15.Sarmiento A., Pratt G.W., Berry N.C., Sinclair W.F. Colles' fractures. Functional bracing in supination. J Bone Jt Surg Am. 1975;57:311–317. [PubMed] [Google Scholar]
- 16.Tada K., Ikeda K., Shigemoto K., Suganuma S., Tsuchiya H. Prevention of flexor pollicis longus tendon rupture after volar plate fixation of distal radius fractures. Hand Surg. 2011;16:271–275. doi: 10.1142/S0218810411005539. [DOI] [PubMed] [Google Scholar]
- 17.McGeorge D.D., Stilwell J.H. Partial flexor tendon injuries: to repair or not. J Hand Surg Br. 1992;17:176–177. doi: 10.1016/0266-7681(92)90083-e. [DOI] [PubMed] [Google Scholar]
- 18.Fok M.W., Klausmeyer M.A., Fernandez D.L., Orbay J.L., Bergada A.L. Volar plate fixation of intra-articular distal radius fractures: a retrospective study. J Wrist Surg. 2013;2:247–254. doi: 10.1055/s-0033-1350086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martineau P.A., Berry G.K., Harvey E.J. Plating for distal radius fractures. Hand Clin. 2010;26:61–69. doi: 10.1016/j.hcl.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Gasse N., Lepage D., Pem R. Anatomical and radiological study applied to distal radius surgery. Surg Radiol Anat. 2011;33:485–490. doi: 10.1007/s00276-010-0754-x. [DOI] [PubMed] [Google Scholar]
- 21.Obert L., Loisel F., Huard S., Rochet S., Lepage D., Leclerc G., Garbuio P. Plate fixation of distal radius fracture and related complications. Eur J Orthop Surg Traumatol. 2015 Apr;25(3):457–464. doi: 10.1007/s00590-014-1550-9. PubMed PMID: 25274206. [DOI] [PubMed] [Google Scholar]
- 22.Sugun T.S., Gurbuz Y., Ozaksar K., Toros T., Kayalar M., Bal E. Results of volar locking plating for unstable distal radius fractures. Acta Orthop Traumatol Turc. 2012;46:22–25. [PubMed] [Google Scholar]
- 23.Kara A., Celik H., Bankaoglu M., Oc Y., Bulbul M., Sugun T.S. Ultrasonic evaluation of the flexor pollicis longus tendon following volar plate fixation for distal radius fractures. J Hand Surg Am. 2016;41:374–380. doi: 10.1016/j.jhsa.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 24.Drobetz H., Bryant A.L., Pokorny T., Spitaler R., Leixnering M., Jupiter J.B. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction–a biomechanic study in a cadaveric model. J Hand Surg Am. 2006;31:615–622. doi: 10.1016/j.jhsa.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 25.Harness N.G., Jupiter J.B., Orbay J.L., Raskin K.B., Fernandez D.L. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Jt Surg Am. 2004;86-a:1900–1908. doi: 10.2106/00004623-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Marcano A., Taormina D.P., Karia R., Paksima N., Posner M., Egol K.A. Displaced intra-articular fractures involving the volar rim of the distal radius. J Hand Surg Am. 2015;40:42–48. doi: 10.1016/j.jhsa.2014.09.013. [DOI] [PubMed] [Google Scholar]