Abstract
Introduction:
Myocardial perfusion imaging (MPI) is widely used in the evaluation of known and suspected coronary artery disease (CAD). Imaging of heart in stress and rest enables the comparison of myocardial uptake of radiotracer in proportion to the needs and coronary flow, which is used for detection of perfusion defects. Exercise stress and pharmacologic agents are used for the stressing purpose. Novel pharmacologic stressor regadenoson is A2A selective adenosine agonist, which selectively binds to the adenosine receptors in coronary arteries causing coronary dilatation.
Materials and methods:
We analyzed 50 myocardial perfusion studies performed with regadenoson as a pharmacologic agent that was injected before Tc99m-sestamibi in stress imaging. Stress and rest sets of images were evaluated for relative uptake of Tc99m-sestamibi in order to detect and characterize perfusion defects. After the injection of regadenoson, hemodynamic parameters and potential side-effects were closely monitored. Side-effects were stratified per severity as mild, moderate and severe. Studies were read by nuclear medicine physicians using quantitative perfusion SPECT software. Additional diagnostic information such as wall motion and wall thickening were provided by gating.
Results:
Thirty-three patients (66%) experienced one or more side-effects upon the administration of regadenoson, most commonly warmth and chest discomfort. In all patients but one (98%), the symptoms were mild, of short duration and self-limiting. Out of all side-effects registered, 44 (96%) were mild, and 2 (4%) were moderate. Two moderate side-effects developed in one patient with a prior history of asthma, and included shortness of breath and cough. Heart rate changed by 16 +- 31 bpm. Highest increase in blood pressure was 30 mm Hg for systolic, and 10 mm Hg for diastolic. One case of significant decrease in blood pressure was noted from the hypertensive basal values, 50 mm for systolic, and 30 mm Hg for diastolic. ST segment depression of up to 1 mm occurred in 4 cases (8%), and T-wave changes in 3 cases (6%). No conduction abnormalities, significant hypotension, symptomatic bradycardia or cardiac arrest ocurred.
Conclusion:
Our first institutional experiences proved regadenoson as A2A selective adenosine agonist as a pharmacologic stressor to be safe, tolerable and easily used. Its safety profile enabled the study to be performed in patients with respiratory disease also.
Keywords: myocardial perfusion imaging, regadenoson
1. INTRODUCTION
Myocardial perfusion imaging (MPI) is a well-established non-invasive study used in establishing the diagnosis, prognosis and management of coronary artery disease. In the early stages, only physical exercise was used as a stressor to increase the myocardial blood flow before the injection of radiotracer. Physical exercise still remains most widely used stressor in myocardial perfusion imaging because of the additional diagnostic information provided referring to the hemodynamic response, heart rate recovery, and electrocardiographic changes during exercise (1). Later, the pharmacologically active substances were introduced to myocardial perfusion imaging as stress agents. Pharmacologic stress testing is used whenever a patient cannot exercise or achieve the required cardiac workload for the study. First pharmacologic stressors used to vasodilate the coronary arteries and enhance the myocardial blood flow were dipyridamole and adenosine. Both are non-selective adenosine receptor agonists that bind to adenosine receptors of A1, A2A, A2B and A3 subtypes located on the arteriolar vascular smooth muscle cells. By binding to A2A adenosine receptors, they induce selective dilatation of coronary arteries thus enhancing the myocardial blood flow. However, non-specific binding to A1, A2B and A3 receptors may induce serious adverse events such as bronchospasm, conduction abnormalities (AV block of II and III degree) and peripheral vasodilatation with hypotension (2-7). When vasodilatation is contraindicated, dobutamine as an inotropic agent is used. Stenotic coronary arteries cannot properly dilate so they render distal myocardium ischemic enabling the detection of perfusion defects. A novel generation of adenosine receptor agonists introduced a selective A2A agonist regadenoson. As a pharmacologic stress agent, regadenoson has been used in Europe since 2011. At our Institution, regadenoson was the first pharmacologic stressor introduced in clinical practice in 2013. Applied in a fixed dose of 400 ug/5ml as an intravenous bolus, it dilates coronary arteries reaching peak in circulation within 1-4 minutes increasing blood flow 2,4-fold above the baseline. Hyperemia is maintained long enough for the extraction of Tc-99m-based radiotracer from the blood flow. Potential regadenoson side-effects are reversed with aminophylline (7-9). About 58% of regadenoson has renal clearance by active tubular transport (10).
2. MATERIALS AND METHODS
We analyzed 50 patients who were referred by cardiologists because of their inability to exercise due to age (3), cardiovascular instability (23), neurologic/orthopedic/vascular condition (15) and other reasons (9). All patients underwent myocardial perfusion imaging for evaluation of coronary disease, 29 males and 21 females between 44 and 80 years, median of 59,2 years. 27 patients were imaged in coronary artery disease work-up, 21 patients in follow-up including myocardial infarction, and 2 patients for cardiomyopathy (CMP) (Graph 1). 9 patients had been treated with PCI, and 4 with CABG before the imaging. 19 patients had comorbidity such as chronic obstructive pulmonary disease (3) and/or diabetes.
Graph 1.
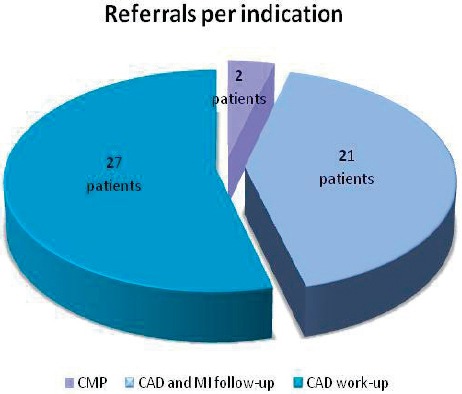
Referrals to myocardial perfusion study per indication
Standard one-day stress-rest protocol with Tc-99m-sestamibi in a weight-adjusted dose was applied. Regadenoson-only method was used for inducing coronary dilatation before stress imaging. 400 ug/5 ml of regadenoson was administered in a bolus after flush of saline. After 30 seconds, Tc-99m-sestamibi was injected followed by the flush of saline, and stress images were acquired 45 minutes later. Clinical signs and hemodynamic parameters with continuous ECG monitoring were closely followed and noted upon the administration of regadenoson for five minutes. SPECT images were acquired per protocol, and the quantitative perfusion SPECT software (QPS), Version 2000, Cedars-Sinai Medical Center, Los Angeles, CA, was used to calculate ischemia on stress and rest images, and the difference between them. After three hours, a rest dose of Tc-99m-sestamibi three times the stress dose was injected, and the imaging was performed after 45 minutes. Additional diagnostic information such as wall motion and wall thickening were provided by gating during stress imaging (Figure 1 and 2).
Figure 1.

Coronary artery disease work-up. Former Dg; Hypertension, Hyperlipoproteinemia. Upper rows of short axis, vertical longitudinal axis and horizontal longitudinal axis of the heart representing stress images are alligned with the rest images in the lower rows
Figure 2.

St. post inferoposterolateral myocardial infarction. St. post CABG. Figure shows residual ishaemia of inferior wall
3. RESULTS
Out of 50 patients, 33 (66%) experienced one or more side-effects upon the administration of regadenoson in the descending order: warmth, chest discomfort, dyspnea, palpitations, vertigo, cough and nausea (Table 1). Side-effects were classified as mild, moderate and severe based on their effect on health, tolerability and the way of resolution. Mild did not pose a threat to health, were of short duration, easily tolerated and spontaneously resolved. Moderate could have posed a threat to health and required some sort of intervention. Severe posed an immediate threat to health, and required intervention. Severe side-effects to consider after the application of regadenoson included AV blocks of II and III degree, hypotension, bradycardia and cardiac arrest.
Table 1.
Frequency and severity of adverse effects per symptoms and signs

In all patients but one (98%), the symptoms were mild and of short duration. Out of all side-effects registered, 44 (96%) were mild, and 2 (4%) were moderate. Moderate symptoms presented in one patient with prior history of asthma, and included shortness of breath and cough. The symptoms were controled by bringing the patient in the upright position and reassurance. No further intervention was necessary, and the study was finished per protocol.
In the studied group, heart rate changed by 16 +- 31 bpm.
No significant changes in blood pressure occurred in all cases when the basal blood pressure was normal (systolic <140 and diastolic <90 mm Hg), and only four cases of mild hypertension were registered. Mild hypertension was defined as systolic BP ranging from 140-159, and diastolic from 90-99 mm Hg. However, in eight cases regadenosone was applied to patients with baseline hypertension, and the highest increase in blood pressure recorded was 30 mm Hg for systolic, and 10 mm Hg for diastolic. In one 80 year-old patient though, a significant sudden decrease in blood pressure was noted but from the hypertensive basal values, and that for 50 mm Hg of systolic, and for 30 mm Hg of diastolic pressure, and the target blood pressure of 110/60. At the same time, heart rate increased from 75 to 80 beats per minute. A described patient was 80 years old, and was referred for the work-up of angina pectoris. No anti-hypotensive medication was applied to the patient who remained asymptomatic.
ST segment depression of up to 1 mm occurred in 4 cases (8%), out of which two were up to 0,5 mm. T-wave changes in a form of inversion ocurred in 3 cases (6%), and were proved to be non-specific.
No AV blocks, significant hypotension, bradycardia or asystole were noted.
All myocardial perfusion studies analyzed were interpretable. 47 (94%) proved to be diagnostic and conclusive while three studies were interpreted with a probability level (2 probably normal and 1 probably abnormal).
Out of 21 myocardial perfusion studies performed for coronary artery disease work-up, the disease was newly diagnosed in eight cases. Two studies were interpreted as probably normal, and one probably abnormal.
Abnormal study showing a reversible defect of the basal and mid-third of the inferior wall, which is compatible with stress-induced ischemia. Regadenoson induced significant increase in heart rate (for 44 bpm) and palpitations. ECG showed sinus tachycardia that resolved in a resting state.
Abnormal study showing a partially reversible defect of the inferolateral wall, which is compatible with residual stress-induced ischemia. Regadenoson induced no symptoms, hemodynamic or significant ECG changes.
4. DISCUSSION
Regadenoson was introduced to clinical practice at our Institution in 2013. It was the first pharmacologic stressor applied so that institutional comparison with other pharmacologic stressors (dipyridamole, adenosine) could not have been done. A manufacturer’s recommended protocol on regadenoson application was used. No combined exercise-pharmacologic stressing protocols have been attempted so far.
Handling and application of regadenoson proved to be easy with a fast throughput of patients through the nuclear medicine department. This resulted in more efficient use of Tc-99m-sestamibi.
Side- effects were common, however, in all cases but one were mild and tolerable, of short duration spontaneously resolving. These side-effects were attributable to the direct stimulation of sympathetic nervous system. In one case, moderate side-effects in the form of shortness of breath and cough caused by bronchospasm were registered in the patient with prior history of athma. Before the study was performed, no active wheezing was present. In this patient, the symptoms spontaneously resolved and required no application of aminophylline. It is our opinion that there was a psychological component of fear of the unknown procedure that contributed to the severity of symptoms. In comparison with a study of 126 patients with COPD and 102 with asthma undergoing regadenoson MPI performed by Husain et al (11) that showed no incidence of clinical exacerbation of COPD or asthma after regadenoson, our cohort remains a small one, and requires further research. Prenner et al recommend that the respiratory condition of the patients with COPD or athma should be as stable as possible prior to MPI with any pharmacologic stress agent (12).
80 year-old patient with a significant sudden decrease in blood pressure (systolic decreased for 50 mm Hg and diastolic for 30 mm Hg) was asymptomatic. Post-regadenoson hypotension was attributed to age and insufficient contractility of myocardium. We considered other possible mechanisms such as vagal stimulation proposed by Underwood et al (13) but in our patient hypotension was isolated sign followed by reflex tachycardia without nausea.
The only disadvantage we noticed in comparison with exercise stressing was more frequent high abdominal activity of Tc-99m-sestamibi, which interefered with interpretatation of the inferior wall. It posed a diagnostic problem in coronary artery disease work-up, when the inferior wall ischemia could have been isolated (such as in uni-vessel disease of right coronary artery) causing symptoms. That is why three studies of coronary artery disease work-up were not interpreted explicitely but with a probability level (2 probably normal and 1 probably abnormal). In reports it was proposed was to the referring cardiologists to make clinical correlations, closely follow-up and repeat the studies in some time. It has been recognized though that increased abdominal activity of radiotracer is not specific for regadenoson but instead has been recognized for all pharmacologic stressors.
We plan to extend our research to the use of regadenoson in patients with chronic renal disease.
5. CONCLUSION
Our first institutional experiences proved A2A selective adenosine agonist regadenoson as a pharmacologic stressor to be safe, tolerable and easily used. Its safety profile enabled the study to be performed in patients with lung diseases as proved in such a small cohort.
REFERENCES
- 1.Boger LA, Volker LL, Hertenstein GK, Bateman TM. Best patient preparation before and during radionuclide myocardial perfusion imaging studies. J Nucl Cardiol. 2006;13:98–110. doi: 10.1016/j.nuclcard.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Buhr C, Goessl M, Erbel R, Eggebrecht H. Regadenoson in the detection of coronary artery disease. Vasc Health Risk Manag. 2008 Apr;4(2):337–40. doi: 10.2147/vhrm.s1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cerqueira MD. The future of pharmacologic stress: selective A2A adenosine receptor agonists. Am J Cardiol. 2004 Jul 22;94(2A):33D–420D. doi: 10.1016/j.amjcard.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Johnson SG, Peters S. Advances in Pharmacologic Stress Agents: Focus on Regadenoson. J Nucl Med Technol. 2010 Sep 1;38(3):163–71. doi: 10.2967/jnmt.109.065581. [DOI] [PubMed] [Google Scholar]
- 5.Iskandrian AS, Verani MS, Heo J. Pharmacologic stress testing: mechanism of action, hemodynamic responses, and results in detection of coronary artery disease. J Nucl Cardiol. 1994;1:94–111. doi: 10.1007/BF02940016. [DOI] [PubMed] [Google Scholar]
- 6.Belardinelli L, Linden J, Berne RM. The cardiac effects of adenosine. Prog Cardiovasc Dis. 1989;32:73–97. doi: 10.1016/0033-0620(89)90015-7. [DOI] [PubMed] [Google Scholar]
- 7.Cerqueira MD. Advances in pharmacologic agents in imaging: new A2A receptor agonists. Curr Cardiol Rep. 2006;8:119–12. doi: 10.1007/s11886-006-0022-1. [DOI] [PubMed] [Google Scholar]
- 8.Brinkert M, Reyes E, Walker S, Latus K, Maenhout A, Mizumoto R, Nkomo C, Standbridge K, Wechalekar K, Underwood SR. Regadenoson in Europe: first-year experience of regadenoson stress combined with submaximal exercise in patients undergoing myocardial perfusion scintigraphy. Eur J Nucl Med Mol Imaging. 2014 Mar;41(3):511–21. doi: 10.1007/s00259-013-2619-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hendel RC, Bateman TM, Cerqueira MD, Iskandrian AE, Leppo JA, Blackburn B, et al. Initial clinical experience with regadenoson, a novel selective A2A agonist for pharmacologic stress single-photon emission computed tomography myocardial perfusion imaging. J Am Coll Cardiol. 2005;46:2069–75. doi: 10.1016/j.jacc.2005.05.097. [DOI] [PubMed] [Google Scholar]
- 10.Gordi T, Frohna P, Sun HL, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet. 2006;45(12):1201–12. doi: 10.2165/00003088-200645120-00005. [DOI] [PubMed] [Google Scholar]
- 11.Husain Z, Palani G, Cabrera R, Karthikeyan AS, Dhanalakota S, Pathmanathan S, Jacobsen G, Ananthasubramaniam K. Hemodynamic response, arrhythmic risk, and overall safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic obstructive pulmonary disease and bronchial asthma patients. Int J Cardiovasc Imaging. 2012 Oct;28(7):1841–9. doi: 10.1007/s10554-011-0003-3. [DOI] [PubMed] [Google Scholar]
- 12.Prenner BM, Bukofzer S, Behm S, Feaheny K, McNutt BE. A randomized, double-blind, placebo-controlled study assessing the safety and tolerability of regadenoson in subjects with asthma or chronic obstructive pulmonary disease. J Nucl Cardiol. 2012 Aug;19(4):681–92. doi: 10.1007/s12350-012-9547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Underwood SR, Latus KA, Reyes E, Standbridge K, Walker S, Wechalekar K. Regadenoson-induced bradycardia and hypotension: possible mechanism and antidote. J Nucl Cardiol. 2014 Oct;21(5):1040. doi: 10.1007/s12350-014-9968-3. [DOI] [PubMed] [Google Scholar]


