Abstract
Background
The admission cardiotocograph (CTG) is a commonly used screening test consisting of a short (usually 20 minutes) recording of the fetal heart rate (FHR) and uterine activity performed on the mother's admission to the labour ward. This is an update of a review published in 2012.
Objectives
To compare the effects of admission cardiotocography with intermittent auscultation of the FHR on maternal and infant outcomes for pregnant women without risk factors on their admission to the labour ward.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register to 30 November 2016 and we planned to review the reference list of retrieved papers.
Selection criteria
All randomised and quasi‐randomised trials comparing admission CTG with intermittent auscultation of the FHR for pregnant women between 37 and 42 completed weeks of pregnancy and considered to be at low risk of intrapartum fetal hypoxia and of developing complications during labour.
Data collection and analysis
Two authors independently assessed trial eligibility and quality, and extracted data. Data were checked for accuracy.
Main results
We included no new trials in this update. We included four trials involving more than 13,000 women which were conducted in the UK and Ireland and included women in labour. Three trials were funded by the hospitals where the trials took place and one trial was funded by the Scottish government. No declarations of interest were made in two trials; the remaining two trials did not mention declarations of interest. Overall, the studies were assessed as low risk of bias. Results reported in the 2012 review remain unchanged.
Although not statistically significant using a strict P < 0.05 criterion, data were consistent with women allocated to admission CTG having, on average, a higher probability of an increase in incidence of caesarean section than women allocated to intermittent auscultation (risk ratio (RR) 1.20, 95% confidence interval (CI) 1.00 to 1.44, 4 trials, 11,338 women, I² = 0%, moderate quality evidence). There was no clear difference in the average treatment effect across included trials between women allocated to admission CTG and women allocated to intermittent auscultation in instrumental vaginal birth (RR 1.10, 95% CI 0.95 to 1.27, 4 trials, 11,338 women, I² = 38%, low quality evidence) and perinatal mortality rate (RR 1.01, 95% CI 0.30 to 3.47, 4 trials, 11,339 infants, I² = 0%, moderate quality evidence).
Women allocated to admission CTG had, on average, higher rates of continuous electronic fetal monitoring during labour (RR 1.30, 95% CI 1.14 to 1.48, 3 trials, 10,753 women, I² = 79%, low quality evidence) and fetal blood sampling (RR 1.28, 95% CI 1.13 to 1.45, 3 trials, 10,757 women, I² = 0%) than women allocated to intermittent auscultation. There were no differences between groups in other secondary outcome measures including incidence and severity of hypoxic ischaemic encephalopathy (incidence only reported) (RR 1.19, 95% CI 0.37 to 3.90; 2367 infants; 1 trial; very low quality evidence) and incidence of seizures in the neonatal period (RR 0.72, 95% CI 0.32 to 1.61; 8056 infants; 1 trial; low quality evidence). There were no data reported for severe neurodevelopmental disability assessed at greater than, or equal to, 12 months of age.
Authors' conclusions
Contrary to continued use in some clinical areas, we found no evidence of benefit for the use of the admission CTG for low‐risk women on admission in labour.
Furthermore, the probability is that admission CTG increases the caesarean section rate by approximately 20%. The data lacked power to detect possible important differences in perinatal mortality. However, it is unlikely that any trial, or meta‐analysis, will be adequately powered to detect such differences. The findings of this review support recommendations that the admission CTG not be used for women who are low risk on admission in labour. Women should be informed that admission CTG is likely associated with an increase in the incidence of caesarean section without evidence of benefit.
Evidence quality ranged from moderate to very low, with downgrading decisions based on imprecision, inconsistency and a lack of blinding for participants and personnel. All four included trials were conducted in developed Western European countries. One additional study is ongoing.
The usefulness of the findings of this review for developing countries will depend on FHR monitoring practices. However, an absence of benefit and likely harm associated with admission CTG will have relevance for countries where questions are being asked about the role of the admission CTG.
Future studies evaluating the effects of the admission CTG should consider including women admitted with signs of labour and before a formal diagnosis of labour. This would include a cohort of women currently having admission CTGs and not included in current trials.
Keywords: Adult; Female; Humans; Pregnancy; Cardiotocography; Cardiotocography/methods; Cardiotocography/statistics & numerical data; Diagnostic Tests, Routine; Diagnostic Tests, Routine/methods; Echocardiography, Doppler; Echocardiography, Doppler/methods; Heart Auscultation; Heart Auscultation/methods; Heart Auscultation/statistics & numerical data; Heart Rate, Fetal; Heart Rate, Fetal/physiology; Labor, Obstetric; Randomized Controlled Trials as Topic
Plain language summary
Comparing electronic monitoring of the baby's heartbeat on a woman's admission in labour using cardiotocography (CTG) with intermittent monitoring
What is the issue?
When healthy women with low‐risk pregnancies are admitted to labour wards, does a cardiotocograph (CTG) or listening to the fetal heart rate (FHR) for one minute following a contraction lead to better outcomes for mothers and their babies?
Why is this important?
Monitoring of the FHR is one of the most common methods for checking a baby's wellbeing. The two most common ways of monitoring the FHR are by listening to the heart beat using a fetal stethoscope, Pinard (special trumpet shaped device), hand‐held Doppler ultrasound device (known as intermittent auscultation) or by an electronic fetal monitoring (EFM) machine that produces a printout of the baby’s heart rate and the mother’s contractions, called a CTG.
The admission CTG is a commonly used test consisting of a short, usually 20 minute, recording of the FHR and uterine activity that is performed when the woman is admitted to the labour ward with signs of labour. The admission CTG was introduced to try and identify those babies who were at greatest risk of becoming compromised with a lack of oxygen during labour. These babies could be monitored more intensively by continuous EFM, or they may benefit from an immediate intervention such as being delivered by caesarean section.
What evidence did we find?
We compared the admission CTG with intermittent auscultation of the FHR performed on the woman's admission to the labour ward. We searched for evidence to 30 November 2016 but found no new studies for this updated review (previously published in 2012). This review includes four studies and there is one study that is not yet complete. The included studies (carried out in the UK and Ireland) involved more than 13,000 women with low‐risk pregnancies. Three trials were funded by the hospitals were the trials took place and one trial was funded by the Scottish government.
Women allocated to admission CTG were probably more likely to have a caesarean section than women allocated to intermittent auscultation (moderate quality evidence). There was no difference in the number of instrumental vaginal births (low quality evidence) or in numbers of babies who died during or shortly after labour (moderate quality evidence) between women in the two groups. Admission CTG was associated with an increase in the use of continuous EFM (with an electrode placed on the baby’s scalp) (low quality evidence) and fetal blood sampling (a small blood sample taken from a baby's scalp) during labour. There were no differences in other outcomes measured such as artificial rupture of the membranes, augmentation of labour, use of an epidural, damage to the baby's brain due to lack of oxygen (very low quality evidence), or the baby having fits or seizures just after birth (low quality evidence). No studies reported if the babies developed any severe problems in brain or central nervous system growth and development after one year of age.
What does this mean?
Although many hospitals carry out CTGs on women when they are admitted to hospital in labour, we found no evidence that this benefits women with low‐risk pregnancies. We found that admission CTGs may increase numbers of women having a caesarean section by about 20%.
The included studies did not include enough women to show if admission CTGs or intermittent auscultation were better at keeping babies safe. However, studies to show which is better at keeping babies safe would have to be very large. Based on this review, low‐risk pregnant women who have an admission CTG could be more likely to have a caesarean section. The benefits to these women of having an admission CTG are not certain.
All of the included studies took place in developed Western European countries. The review findings might not be useful to people in very different countries or where different ways of FHR monitoring are used. However, countries that use admission CTGs should start to question why, because there are not clear benefits to using admission CTGs, and they could be causing women harm by making them more likely to have a caesarean section.
Summary of findings
Summary of findings for the main comparison. Admission cardiotocography compared to Intermittent auscultation (low‐risk women) for assessment of fetal wellbeing.
| Admission cardiotocography compared to Intermittent auscultation (low‐risk women) for assessment of fetal wellbeing | ||||||
| Patient or population: Low risk pregnant women. All of the women were in labour. Setting: Ireland and UK Intervention: Admission cardiotocography ‐ women received a routine 15‐minute (1 trial) or 20‐minute (3 trials) tracing. Comparison: Intermittent auscultation (low‐risk women) ‐ women received intermittent auscultation of the fetal heart for at least one full minute (4 trials), during and after a contraction (2 trials) or after a contraction only (2 trials). | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with Intermittent auscultation (low‐risk women) | Risk with admission cardiotocography | |||||
| Incidence of caesarean section | Study population | RR 1.20 (1.00 to 1.44) | 11338 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 2 | ||
| 36 per 1000 | 44 per 1000 (36 to 52) | |||||
| Incidence of operative vaginal birth | Study population | RR 1.10 (0.95 to 1.27) | 11338 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 3 | ||
| 126 per 1000 | 139 per 1000 (120 to 160) | |||||
| Perinatal mortality rate (fetal and neonatal deaths excluding lethal congenital anomalies) | Study population | RR 1.01 (0.30 to 3.47) | 11339 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 4 5 6 | ||
| 1 per 1000 | 1 per 1000 (0 to 3) | |||||
| Severe neurodevelopmental disability assessed ≥ 12 months of age | Study population | ‐ | (0 RCTs) | ‐ | None of the included studies reported data for the outcome | |
| see comment | see comment | |||||
| Incidence of continuous electronic fetal monitoring during labour | Study population | RR 1.30 (1.14 to 1.48) | 10753 (3 RCTs) | ⊕⊕⊝⊝ LOW 1 7 | ||
| 417 per 1000 | 542 per 1000 (475 to 617) | |||||
| Incidence and severity of hypoxic ischaemic encephalopathy (incidence only reported) | Study population | RR 1.19 (0.37 to 3.90) | 2367 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 8 | ||
| 4 per 1000 | 5 per 1000 (2 to 17) | |||||
| Incidence of seizures in the neonatal period | Study population | RR 0.72 (0.32 to 1.61) | 8056 (1 RCT) | ⊕⊕⊝⊝ LOW 1 9 | ||
| 3 per 1000 | 2 per 1000 (1 to 6) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Most studies contributing data had design limitations: outcome may have been affected by lack of blinding as all studies judged to be at high risk of performance bias (‐1)
2 Good sample size (> 3000), no measurable heterogeneity (I² = 0%), however 95% confidence interval touches the line of no effect (not downgraded)
3 Good sample size (> 3000), though wide confidence intervals cross the line of no effect (‐1)
4 Studies contributing data had design limitations: unlikely this outcome was affected by lack of blinding (not downgraded)
5 Few events but good sample size (not downgraded)
6 Very wide confidence intervals crossing the line of no effect (‐1)
7 Statistical heterogeneity (I² = 79%) (‐1)
8 Wide confidence interval crossing the line of no effect, few events & small sample size (based on one study) (‐2)
9 Wide confidence intervals crossing the line of no effect, large sample size with data from one study (‐1)
Background
Assessment of fetal wellbeing throughout pregnancy, labour and birth is widely regarded as a fundamental component of maternity care and essential for optimising fetal outcomes. Although a variety of methods are used to assess fetal wellbeing, including fetal movement counting and biophysical tests such as Doppler ultrasound, monitoring of the fetal heart rate (FHR) remains the most common method for the assessment of fetal wellbeing (Alfirevic 2013; NCCWCH 2007).
The FHR undergoes constant changes in response to changes in the intrauterine environment and to other stimuli such as uterine contractions. These changes in the FHR can be monitored to assess the wellbeing of the fetus during pregnancy and labour.
Description of the condition
Two common methods of monitoring the FHR are by intermittent auscultation and by an electronic fetal monitoring (EFM) machine that produces a printout called a cardiotocograph (CTG) (Ayres‐de‐Campos 2015). Intermittent auscultation involves listening to the fetal heart at predetermined intervals using either a Pinard stethoscope or a hand‐held Doppler ultrasound device. The CTG is a graphical printout of the FHR and uterine contractions. The FHR recorded on a CTG may be captured externally via an ultrasound transducer attached to the mother's abdomen, or internally via a fetal scalp electrode placed directly on the baby's head. Uterine contractions are recorded via a pressure transducer attached to the mother's abdomen or, less commonly, by an intrauterine pressure device placed in the uterine cavity (Ayres‐de‐Campos 2015).
Description of the intervention
The admission CTG is a commonly‐used screening test consisting of a short, usually 20 minute, recording of the FHR and uterine activity performed on the mother's admission to the labour ward with signs of labour (Cheyne 2003; Impey 2003; Mires 2001). Anecdotally, some women will have an admission CTG performed before assessments aimed at diagnosing the onset of labour, while others will not have the admission CTG until a diagnosis of labour has been established. The implications of this are that some women will have an admission CTG performed on admission to the labour ward or labour assessment room where, on subsequent assessment, a diagnosis of not being in labour is made. Differences in timing of the admission CTG with respect to the onset of labour may result in differences in outcomes assessed. We planned to explore this through subgroup analysis (see Subgroup analysis and investigation of heterogeneity).
How the intervention might work
Pioneered in the 1950s and 1960s as an alternative to intermittent auscultation of the FHR by stethoscope or Pinard (Caldeyro‐Barcia 1966; Hammacher 1968; Hon 1958), EFM was introduced into widespread clinical practice in the 1970s to 1980s on the premise that it would facilitate early detection of abnormal FHR patterns thought to be associated with hypoxia (lack of oxygen), to enable earlier intervention to prevent fetal neurological damage and death or both (Nelson 1996).
However, because antenatal risk factors do not identify all fetuses who will subsequently experience morbidity, mortality, or both, the admission CTG was introduced as a means of attempting to identify those fetuses of low‐risk mothers at greatest risk of intrapartum hypoxia (Arulkumaran 2000; RCOG 2001) who might benefit from more intensive monitoring by continuous EFM and fetal scalp blood gas analysis or both, or from immediate intervention (e.g. expedited birth).
Current prevalence rates of perinatal mortality, neonatal encephalopathy and cerebral palsy are relatively low and, of those, only a small proportion are thought to be attributable directly to intrapartum causes (RCOG 2001). Changes in FHR patterns are neither sensitive (the ability of a test to identify those who have the disease or condition) nor specific (the ability of the test to correctly identify those without the disease or condition) to any particular cause (MacLennan 1999). Multiple late decelerations and decreased FHR variability have been shown to be associated with an increased risk of cerebral palsy (Nelson 1996). However, the associated false positive rate is reported as high as 99.8% in the presence of tracings displaying these abnormalities in the FHR pattern (Nelson 1996). This poor positive predictive value implies that to identify the fetus who may be compromised, EFM identifies abnormal FHR patterns in many healthy fetuses who are not truly compromised.
Why it is important to do this review
There is a lack of evidence of benefit supporting the use of the admission CTG in low‐risk pregnancy. Despite recommendations that it should not be recommended for this group of women (Liston 2007; NCCWCH 2007; RCOG 2001), the admission CTG was used by approximately 79% of maternity units in the UK in 2000 (CESDI 2001), by 96% of units in Ireland in 2004 (Devane 2007) and by approximately 76% of Canadian hospitals (Kaczorowski 1998). More recently, the admission CTG was used in all (100%, n = 42) labour units in Sweden in 2008 (Holzmann 2010).
Although the admission CTG remains in widespread use, several issues remain controversial. These include whether the admission CTG (a) should be offered routinely to all women without risk factors for intrapartum hypoxia; (b) whether the admission CTG is effective at predicting those fetuses who will subsequently develop intrapartum hypoxia; and (c) the effect of the admission CTG on neonatal mortality and on maternal and neonatal morbidity.
It was important to undertake this systematic review to explore these issues and to evaluate the efficacy of admission CTG compared to intermittent auscultation as a method of assessing fetal wellbeing in women on admission to the labour ward, or labour assessment room, with signs of possible labour. This review complements other Cochrane systematic reviews evaluating the effectiveness of other interventions for the assessment of fetal wellbeing including the following.
Amniotic fluid index versus single deepest vertical pocket as a screening test for predicting adverse pregnancy outcomes (Nabhan 2008).
Antenatal cardiotocography for fetal assessment (Grivell 2015).
Biochemical tests for placental function for assessment in pregnancy (Neilson 2012).
Biophysical profile for fetal assessment in high‐risk pregnancies (Lalor 2008).
Fetal and umbilical Doppler ultrasound in high‐risk pregnancies (Alfirevic 2013).
Fetal manipulation for facilitating tests of fetal wellbeing (Tan 2013a).
Fetal movement counting for assessment of fetal wellbeing (Mangesi 2015).
Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing (Tan 2013b).
Maternal glucose administration for facilitating tests of fetal wellbeing (Tan 2012).
Regimens of fetal surveillance for impaired fetal growth (Grivell 2012).
Utero‐placental Doppler ultrasound for improving pregnancy outcome (Stampalija 2010).
Vibroacoustic stimulation for fetal assessment in labour in the presence of a non‐reassuring FHR trace (East 2013).
Objectives
To compare the effects of admission cardiotocograph with intermittent auscultation of the fetal heart rate on maternal and infant outcomes for pregnant women without risk factors for intrapartum hypoxia on their admission to the labour ward.
Methods
Criteria for considering studies for this review
Types of studies
All randomised and quasi randomised trials comparing admission cardiotocograph (CTG) with intermittent auscultation of the fetal heart rate (FHR).
Types of participants
Pregnant women between 37 and 42 completed weeks of pregnancy and considered to be at low risk of intrapartum fetal hypoxia and of developing complications during labour were included. It is recognised that there is much debate surrounding the definition of what constitutes 'normality' and concerns have been expressed at what some regard as the disempowering concept of risk classification (Gail‐Thomas 2003). In addition, the predictive value of risk scoring during pregnancy is poor (WHO 1999). However, given the consensus of opinion that continuous electronic fetal monitoring (EFM) should be reserved for women whose fetuses are at high or increased risk of cerebral palsy, neonatal encephalopathy or perinatal death (Liston 2007; NCCWCH 2007; RANZCOG 2002; RCOG 2001), where sufficient detail was provided by trial authors, we determined eligibility of participants based on absence of risk factors identified in international guidelines for EFM (Characteristics of included studies).
Types of interventions
Admission CTG compared with intermittent auscultation of the FHR on admission to the labour ward.
For the purpose of this review we used the following operational definitions.
Admission CTG is defined as a commonly‐used screening test consisting of a short, usually 20 minute, recording of the FHR and uterine activity performed on the mother's admission to the labour ward.
Intermittent auscultation is defined as intermittent surveillance of the FHR at predetermined intervals, using either a Pinard stethoscope or a hand‐held Doppler, performed on the mother's admission to the labour ward.
Types of outcome measures
Main outcomes
Maternal
Incidence of caesarean section.
Incidence of operative vaginal delivery.
Infant
Perinatal mortality rate (fetal and neonatal deaths excluding lethal congenital anomalies).
Severe neurodevelopmental disability assessed at 12 months of age or more. We defined severe neurodevelopmental disability as any one or a combination of the following: non‐ambulant cerebral palsy, developmental delay (developmental quotient less than 70), auditory and visual impairment. Development should have been assessed by means of a previously validated tool, such as Bayley Scales of Infant Development (Psychomotor Developmental Index and Mental Developmental Index (Bayley 1993)).
Other important outcomes
Maternal
Incidence of serious maternal complications (e.g. admission to intensive care unit, septicaemia (a form of blood infection), organ failure).
Incidence of continuous EFM during labour.
Incidence of artificial rupture of membranes during labour.
Incidence of oxytocin augmentation of labour.
Mobility during labour.
Perceived control and self‐confidence or both during labour.
Incidence of use of pharmacological analgesia including regional analgesia.
Incidence of use of non‐pharmacological methods of coping with labour and birth, e.g. transcutaneous electrical nerve stimulation (TENS), hydrotherapy.
Satisfaction with labour experience.
Incidence of fetal blood sampling.
Length of hospital stay.
Infant
Cardiorespiratory and neurological depression or both at birth as demonstrated by an Apgar score less than seven for longer than five minutes, or evidence of acidaemia indicated by a pH less than 7.0 or base deficit greater than 12 mmol/L in umbilical arterial cord blood, or neonatal blood sample within the first hour of life, or both.
-
Incidence and severity of hypoxic ischaemic encephalopathy. Severity of hypoxic ischaemic encephalopathy assessed using Sarnat staging (Sarnat 1976):
stage 1 (mild): hyperalertness, hyper‐reflexia, dilated pupils, tachycardia, absence of seizures;
stage 2 (moderate): lethargy, hyper‐reflexia, miosis, bradycardia, seizures, hypotonia with weak suck and Moro reflexes;
stage 3 (severe): stupor, flaccidity, small to midposition pupils which react poorly to light, decreased stretch reflexes, hypothermia and absent Moro reflex.
Incidence of seizures in the neonatal period, either apparent clinically or detected by electro‐encephalographic recordings.
Evidence of multi‐organ compromise within the first 24 hours after birth: for example, renal failure, hepatic injury, cardiac damage, respiratory complications, or haematological insult.
Incidence of admission to neonatal special care and intensive care unit or both.
Length of stay to neonatal special care and neonatal intensive care unit or both.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (30 November 2016).
The Register is a database containing over 22,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth in the Cochrane Library and select the "Specialized Register" section from the options on the left side of the screen.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by the group's Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included studies; Ongoing studies).
For details of additional author searching carried out in the previous version of the review, please see Devane 2012.
Searching other resources
We planned to search the reference list of papers identified using the search strategy described to assess their suitability for inclusion in the review. However, we did not find any new studies for inclusion in this update.
We did not apply any language or date restrictions.
Data collection and analysis
No new reports were identified from the updated search for this update. For methods used in the previous version of this review, see Devane 2012.
The Methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors (DD, JGL) assessed independently for inclusion all the potential studies identified as a result of the search strategy. We did not encounter any disagreement and therefore did not need to consult a third review author (SD, WM or VS).
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors (DD, JGL) extracted data using the data extraction form. We resolved any discrepancies through discussion and did not need to consult a third review author. Two review authors (DD, JGL) entered all data into the Review Manager (RevMan) software (RevMan 2014) and checked for accuracy. When information regarding any of the steps was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
Given the nature of the intervention, we did not expect blinding or participants or personnel to have been likely.
(4) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(5) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(6) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(7) Other bias (checking for bias due to problems not covered by criteria (1) to (6))
We described for each included study any important concerns we had about other possible sources of bias.
Assessment of the quality of the evidence using the GRADE approach
We assessed evidence quality using the GRADE approach as outlined in the GRADE handbook to assess the quality of the body of evidence relating to the following outcomes for the main comparison: Admission cardiotocography versus Intermittent auscultation (low‐risk women).
Incidence of caesarean section.
Incidence of operative vaginal delivery.
Perinatal mortality rate (fetal and neonatal deaths excluding lethal congenital anomalies).
Severe neurodevelopmental disability assessed at or after 12 months of age. We defined severe neurodevelopmental disability as any one or a combination of the following: non‐ambulant cerebral palsy, developmental delay (developmental quotient less than 70), auditory and visual impairment. Development should have been assessed by means of a previously validated tool, such as Bayley Scales of Infant Development (Psychomotor Developmental Index and Mental Developmental Index (Bayley 1993)).
Incidence of continuous EFM during labour.
Incidence and severity of hypoxic ischaemic encephalopathy (incidence only reported)
Incidence of seizures in the neonatal period, either apparent clinically or detected by electro‐encephalographic recordings.
GRADEpro Guideline Development Tool was used to import data from Review Manager 5.3 (RevMan 2014) in order to create ’Summary of findings’ tables. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from high quality by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. We used the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
We did not find any cluster‐randomised trials from our search. In future updates, if we identify cluster‐randomised trials we will include them in the analyses along with individually randomised trials. We will adjust their sample sizes using the methods described in the Handbook using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
We did not plan to include cross‐over design trials in this review.
Other unit of analysis issues
Multiple pregnancies
As this review is based on women experiencing low‐risk pregnancies, we did not plan to include women with multiple pregnancies.
Multiple‐armed studies
No multiple‐armed studies have been included in this update. In future updates, if multiple‐armed trials are identified, we will combine all relevant intervention and control groups together to create a single pair‐wise comparison (see section 16.5.4 of Cochrane Handbook for Systematic Reviews of Interventions) (Higgins 2011).
Dealing with missing data
For included studies, levels of attrition were noted. In future updates, if more eligible studies are included, the impact of including studies with high levels of missing data in the overall assessment of treatment effect will be explored by using sensitivity analysis.
For all outcomes, analyses were carried out, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if I² was greater than 30% and either Tau² was greater than zero, or there was a low P value (< 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (> 30%), we planned to explore it by pre‐specified subgroup analysis.
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analyses using the Review Manager software (RevMan 2014). The largest of the four included trials (Impey 2003) included women in whom the liquor was known to be clear (i.e. only women who had either a spontaneous rupture of the membranes or an amniotomy were included in the study). This knowledge of the presence of clear liquor would have given clinicians an additional clinical feature used in the assessment of fetal well being that would not have been available for all women included in the other three trials (Cheyne 2003; Mires 2001; Mitchell 2008) where membrane rupture and clear liquor were not inclusion criteria. Because of this, we believed that there was clinical heterogeneity sufficient to expect that the underlying treatment effects would differ between the included trials (and in particular between the Impey 2003 trial and the other three trials (Cheyne 2003; Mires 2001; Mitchell 2008)). We therefore used random‐effects meta‐analysis to produce an overall summary of the average treatment effect across the four included trials. We have treated this random‐effects summary as the average range of possible treatment effects. For each outcome reported, we present the results of the random‐effects analyses as the average treatment effect with its 95% confidence interval, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
In future updates, if we identify substantial heterogeneity, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it is, we will use random‐effects analysis to produce it.
We planned to carry out the following subgroup analysis using a priori outcomes.
Women in‐labour versus women not in‐labour on clinical assessment post admission CTG.
However, all four studies included only women in labour (at point of intervention) and therefore this subgroup analysis was not possible.
In future updates, if subgroup analysis is possible, we will assess subgroup differences by interaction tests available within RevMan (RevMan 2014). We will report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
In future updates of the review, we plan to carry out sensitivity analyses to explore the effect of trial quality assessed by concealment of allocation, high attrition rates, or both, with poor quality studies being excluded from the analyses in order to assess whether this makes any difference to the overall result. If we include cluster‐RCTs, along with the individually‐randomised trials, we will carry out sensitivity analysis to investigate the effect of the variation randomisation unit.
Results
Description of studies
Results of the search
An updated search of the Cochrane Pregnancy and Childbirth Group's Trials Register (30 November 2016) found no new studies for consideration. The original search in Devane 2012 found seven reports and our search of the other databases did not identify any additional reports. These seven reports related to four completed (Cheyne 2003; Impey 2003; Mires 2001; Mitchell 2008) and one ongoing trial (Devane 2008). At the time of this update, Devane 2008 is ongoing (see Figure 1).
1.

Study flow diagram
Included studies
Methods
We included four randomised controlled trials (RCTs) with 13,296 women (Cheyne 2003; Impey 2003; Mires 2001; Mitchell 2008) (see Characteristics of included studies). We did not exclude any study and found one ongoing study (Devane 2008, see Characteristics of ongoing studies).
Settings
The studies were conducted in hospitals in Scotland (Cheyne 2003; Mires 2001), Ireland (Impey 2003) and England (Mitchell 2008).
Participants
The number of pregnant women included in each study ranged from 334 (Cheyne 2003) to 8628 (Impey 2003). All four studies included women in labour. Therefore, we were unable to perform our planned subgroup analysis by whether or not women were in labour or not on clinical assessment post the admission cardiotocograph (CTG) (see Subgroup analysis and investigation of heterogeneity).
Three studies included women in spontaneous labour only (Cheyne 2003; Mitchell 2008; Mires 2001) and one included women who were in spontaneous or induced labour (Impey 2003). All studies included women who were regarded as being at "low risk" of maternal and fetal complications with the exception of Impey 2003 who included a relatively small (approximately 5%) proportion of women with a previous caesarean section and prior to 37 completed weeks' gestation. Details on participant inclusion criteria, including what constituted low risk are given in Characteristics of included studies.
Interventions and controls
Women allocated to admission CTG received a routine 15‐minute (Mitchell 2008) or 20‐minute (Cheyne 2003; Impey 2003; Mires 2001) tracing. Women allocated to intermittent auscultation received intermittent auscultation of the fetal heart for at least one full minute (Cheyne 2003; Impey 2003; Mires 2001; Mitchell 2008) during and after a contraction (Cheyne 2003; Mires 2001) or after a contraction only (Impey 2003; Mitchell 2008).
Outcomes
Outcomes reported were: caesarean section; instrumental vaginal birth; continuous electronic fetal monitoring (EFM) during labour; amniotomy; oxytocin for augmentation of labour; epidural; fetal blood sampling; fetal and neonatal deaths; Apgar score less than seven at or after five minutes; admission to neonatal intensive care; neonatal seizures; length of stay in neonatal intensive care (hours); hypoxic ischaemic encephalopathy; evidence of fetal multi‐organ compromise within the first 24 hours after birth.
Funding
Cheyne 2003, Impey 2003 and Mitchell 2008 were funded by the hospitals or NHS Trusts where the trials took place (North Glasgow University Hospitals NHS Trust, Research Committee of the National Maternity Hospital, Holles St, Dublin, Ireland, and Buckinghamshire Hospitals NHS Trust's Research Department, respectively). Mires 2001 was funded by Chief Scientists Office of the Scottish Executive, Edinburgh.
Impey 2003 and Mires 2001 declared no conflicts of interest. The remaining two trials (Cheyne 2003; Mitchell 2008) did not include declarations of interest.
Excluded studies
We did not exclude any studies.
Risk of bias in included studies
We assessed the risk of bias in included studies within the domains of (i) random sequence generation (selection bias) (ii) allocation concealment (selection bias) (iii) blinding of participants and personnel (performance bias)(iv) blinding of outcome assessment (detection bias) (v) incomplete outcome data (attrition bias) (vi) selective reporting (reporting bias) and (vii) other bias (see Assessment of risk of bias in included studies above). Overall, the studies were assessed at low risk of bias across most domains with some exceptions, which are detailed below.
Allocation
We assessed all four included studies as having low risk of bias in random sequence generation and in allocation concealment.
Blinding
We felt it unreasonable to expect blinding of participants and professionals providing care (see Assessment of risk of bias in included studies). Nevertheless, due to knowledge of the allocated interventions by participants and personnel during the study, all four studies were rated high risk for performance bias. Risk of bias for blinding for outcome assessors was assessed as low for two studies (Impey 2003; Mires 2001), unclear for one (Mitchell 2008) and high risk in one where outcome assessment was not blinded (Cheyne 2003).
Incomplete outcome data
Overall, loss to follow‐up was low across all outcomes for all four studies with the exception of umbilical cord blood gas analyses (arterial pH, venous pH and base deficit/base excess (BD/BE)). Two studies included this outcome (Impey 2003; Mires 2001) but the range of values used for this outcome in both these studies differed from that prespecified in this review, and therefore, we have not used these data. For information, Impey 2003 reports missing data for the outcome "pH less than seven or BD/E greater than 12 mmol/L" of 7.5% and 7.8% for admission CTG and intermittent ausculation respectively. Mires 2001 reports missing data for their primary outcome of metabolic acidosis defined as "pH less than 7.20 or BD greater than 8 mmol/L" of 26% and 27% for admission CTG and intermittent ausculation respectively. One study reported a loss to follow‐up of 7% (N = 22) of women (Cheyne 2003). However, data were identified and extracted subsequently for 21 of these 22 women by the trial author and kindly provided to the review team.
Selective reporting
All four studies reported all outcomes mentioned in the methods section in the results section of the trial publication(s) and were therefore assessed as being at low risk of selective reporting.
Other potential sources of bias
We identified no other sources of potential bias in three of the four studies (Cheyne 2003; Impey 2003; Mitchell 2008). One study (Mires 2001) recruited women (N = 3752) to the study and randomised them to admission CTG or intermittent auscultation during the third trimester. However, some women developed an obstetric complication between randomisation and admission in labour that warranted continuous fetal heart rate (FHR) monitoring in labour, such that only 2367 women were judged to be low risk when in labour (1186 admission CTG, 1181 intermittent auscultation). Of the 1885 women randomised to intermittent auscultation in the third trimester, 704 (37%) developed complications during pregnancy and required admission CTG on admission. This is addressed further under Sensitivity analysis.
Effects of interventions
See: Table 1
Admission cardiotocography versus intermittent auscultation (low‐risk women, four studies, 11,339 women)
For this comparison, we included all women as randomised in the Cheyne 2003 and Mitchell 2008 studies and the subgroups of low‐risk women in the Impey 2003; Mires 2001 studies (see Characteristics of included studies and Sensitivity analysis for details).
Main outcomes
The difference in the average treatment effect across included trials between women allocated to admission CTG and women allocated to intermittent auscultation in caesarean section has a risk ratio (RR) of 1.20 and a 95% confidence interval (CI) of 1.00 to 1.44, four trials, 11,338 women (Analysis 1.1). Given that the 95% CI just reaches 1.00 and the absence of measurable heterogeneity in this outcome analysis (T² = 0.00, I² = 0%), the probability is that admission CTG increases the caesarean section rate by approximately 20%. There was no significant difference in the average treatment effect across included trials between women allocated to admission CTG and women allocated to intermittent auscultation in instrumental vaginal birth (RR 1.10, 95% CI 0.95 to 1.27, 4 trials, 11,338 women, T² = 0.01, I² = 38%, Analysis 1.2) and fetal and neonatal deaths (RR 1.01, 95% CI 0.30 to 3.47, 4 trials, 11,339 infants, T² = 0.00, I² = 0%, Analysis 1.8). None of the included studies reported data for the outcome 'Severe neurodevelopmental disability assessed at greater than, or equal to 12 months of age'.
1.1. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 1 Caesarean section.
1.2. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 2 Instrumental vaginal birth.
1.8. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 8 Fetal and neonatal deaths.
Other important outcomes
Women allocated to admission CTG had, on average, significantly higher rates of continuous EFM during labour (RR 1.30, 95% CI 1.14 to 1.48, 3 trials, 10,753 women, T² = 0.01, I² = 79%, Analysis 1.3) and fetal blood sampling (RR 1.28, 95% CI 1.13 to 1.45, 3 trials, 10,757 women, T² = 0.00, I² = 0%, Analysis 1.7) than women allocated to intermittent auscultation.
1.3. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 3 Continuous EFM during labour.
1.7. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 7 Fetal blood sampling.
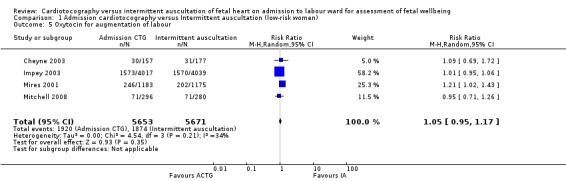
There was no significant difference in the average treatment effect across included trials between women allocated to admission CTG and women allocated to intermittent auscultation in amniotomy (RR 1.04, 95% CI 0.97 to 1.12, 2 trials, 2694 women, T² = 0.00, I² = 0%, Analysis 1.4), oxytocin for augmentation of labour (RR 1.05, 95% CI 0.95 to 1.17, 4 trials, 11,324 women, T² = 0.00, I² = 34%, Analysis 1.5), epidural (RR 1.11, 95% CI 0.87 to 1.41, 3 trials, 10,757 women, T² = 0.03, I² = 86%, Analysis 1.6), Apgar score less than seven at or after five minutes (RR 1.00, 95% CI 0.54 to 1.85, 4 trials, 11,324 infants, T² = 0.10, I² = 25%, Analysis 1.11), hypoxic ischaemic encephalopathy (RR 1.19, 95% CI 0.37 to 3.90, 1 trial, 2367 infants, heterogeneity not applicable, Analysis 1.12), admission to neonatal intensive care units (RR 1.03, 95% CI 0.86 to 1.24, 4 trials, 11,331 infants, T² = 0.00, I² = 0%, Analysis 1.10), neonatal seizures (RR 0.72, 95% CI 0.32 to 1.61, 1 trial, 8056 infants, heterogeneity not applicable, Analysis 1.13), evidence of fetal multi‐organ compromise within the first 24 hours after birth (RR 0.56, 95% CI 0.19 to 1.67, 1 trial, 8056 infants, heterogeneity not applicable, Analysis 1.9), length of stay in neonatal intensive care (hours) (mean difference (MD) 6.20 hours, 95% CI ‐8.70 to 21.10, 1 trial, 318 infants, heterogeneity not applicable, Analysis 1.15) and length of stay in neonatal intensive care (days) (MD 1.80, 95% CI ‐0.59 to 4.19, 1 trial, 91 infants, heterogeneity not applicable, Analysis 1.14).
1.4. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 4 Amniotomy.
1.5. Analysis.
Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 5 Oxytocin for augmentation of labour.
1.6. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 6 Epidural.
1.11. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 11 Apgar score < 7 at or after 5 minutes.
1.12. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 12 Hypoxic ischaemic encephalopathy.
1.10. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 10 Admission to neonatal intensive care.
1.13. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 13 Neonatal seizures.
1.9. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 9 Evidence of fetal multi‐organ compromise within the first 24 hours after birth.
1.15. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 15 Length of stay in neonatal intensive care (hours).
1.14. Analysis.

Comparison 1 Admission cardiotocography versus Intermittent auscultation (low‐risk women), Outcome 14 Length of stay in neonatal intensive care (days).
Data were not reported, were unavailable or were unavailable in a format that could be used in this review for the following other important outcomes.
Maternal
Incidence of serious maternal complications (e.g. admission to intensive care unit, septicaemia (a form of blood infection), organ failure).
Mobility during labour.
Perceived control and self‐confidence or both during labour.
Incidence of use of non‐pharmacological methods of coping with labour, e.g. transcutaneous electrical nerve stimulation, hydrotherapy.
Satisfaction with labour experience.
Length of hospital stay.
Sensitivity analyses
One study (Mires 2001) recruited women (N = 3752) to the study and randomised them to admission CTG or intermittent auscultation during the third trimester. However, some women developed an obstetric complication between randomisation and admission in labour that warranted continuous FHR monitoring in labour, such that only 2367 women were judged to be at low risk when in labour (1186 admission CTG, 1181 intermittent auscultation). Of the 1881 women randomised to intermittent auscultation in the third trimester, 704 (37%) developed complications during pregnancy and required an admission CTG on admission to the labour ward. However, the proportion of women who developed complications were similar in each group, suggesting an absence of differential treatment of women post‐randomisation. The trial author kindly provided data separately for the outcomes in this subgroup of women, and we have included these data in the main analyses in this review (Characteristics of included studies).
A second study (Impey 2003) randomised women at the point of labour. However, this study included a relatively small number (fewer than 5%) of women who had a previous lower segment caesarean section and who went into labour prior to 37 completed weeks' gestation. The trial author kindly provided data separately for the outcomes for women between 37 and 42 completed weeks with no previous caesarean section and we have included these data in the main analyses in this review. We explored the dependency of the findings of this review on the decision to use data from the low‐risk subgroups of women in both the Impey 2003 and Mires 2001 studies through a post‐hoc sensitivity analysis in which the primary analysis was repeated with data from the whole groups as randomised in both studies. Results for this were consistent with primary comparison effects for the low‐risk subgroup of women with the exception of two outcomes. Caesarean section became statistically significant, with significantly more women allocated to admission CTG having, on average, a caesarean section compared with women allocated to intermittent auscultation (RR 1.17, 95% CI 1.02 to 1.34, 4 trials, 13,247 women, T² = 0.00, I² = 0%, Analysis 2.1). Epidural also became significant, with significantly more women allocated to intermittent auscultation having, on average, an epidural compared with women allocated to admission CTG (RR 1.11, 95% CI 1.01 to 1.22, 2 trials, 4085 women, T² = 0.00, I² = 0%, Analysis 2.6).
In the main comparison, three outcomes (instrumental vaginal birth, continuous EFM during labour and epidurals) had significant statistical heterogeneity where T² was greater than zero and either I² was greater than 30% or there was a low P value (< 0.10) in the Chi² test for heterogeneity. On investigating this heterogeneity, we found that the Mires 2001 study appeared to drive the heterogeneity for instrumental vaginal birth and continuous EFM during labour. When Mires 2001 was removed from analyses for each of these two outcomes, the heterogeneity was no longer substantial. Removal of Mires 2001 from analyses for each of these two outcomes did not alter the direction or significance of the effect. Heterogentity for the third outcome, epidural, seemed to be driven by Impey 2003, which in contrast to the direction of effect of the other two studies included in this outcome, found a non‐significant reduction in epidurals in women allocated to admission CTG.
Discussion
Summary of main results
This updated review included four trials (Cheyne 2003; Impey 2003; Mires 2001; Mitchell 2008) involving more than 13,000 women. All four studies included women in labour. No new studies were included in the update.
The admission cardiotocograph (CTG) was introduced as a means of attempting to identify those fetuses at greatest risk of intrapartum hypoxia (Arulkumaran 2000; RCOG 2001) who might benefit from more intensive monitoring by continuous electronic fetal monitoring and fetal scalp blood gas analysis, or both, or from immediate intervention (e.g. expedited birth). Although there was no significant difference in caesarean sections (using a strict P = 0.05 criterion) between women allocated to admission CTG and women allocated to intermittent auscultation, on average the probability is that admission CTG increases the caesarean section rate by approximately 20%. This is reinforced by the 95% confidence interval (CI) just reaching 1.00 and by the absence of measurable heterogeneity in this outcome analysis. Further, all four included studies found fewer caesarean sections associated with intermittent auscultation, although no individual study showed a statistically significant difference. Although numbers needed to treat/harm (NNT/H) analyses remain controversial in the context of meta‐analysis, and should be interpreted with caution, we estimated that overall, one additional caesarean section was performed for every 136 women monitored continuously (risk difference (RD) (controls‐treated) = ‐0.0074 (‐0.015 to ‐0.0002), 95% CI 69 to 5641).
On average, women allocated to admission CTG had a significantly higher rate of continuous electronic fetal monitoring during labour and fetal blood sampling than women allocated to intermittent auscultation.
Overall completeness and applicability of evidence
All four included studies provide relevant evidence on the effects of the admission CTG compared with intermittent auscultation on maternal and infant outcomes for pregnant women without risk factors on their admission to the labour ward. There are three important points in discussing how the results of the review fit into the context of current practice. Firstly, the largest study in this review (Impey 2003) included women in which the colour of the liquor was known to be clear. As such, clinicians caring for these women had an additional, and important, feature used in the overall assessment of fetal wellbeing. Secondly, all four studies included women in either spontaneous or induced labour. In some practice contexts, the admission CTG is performed in the absence of a diagnosis of labour, that is, an admission CTG is done before an assessment to diagnose labour is made. Thirdly, in Mitchell 2008, women allocated to admission CTG received a routine 15‐minute CTG. This is less than the 20 minutes recommended for visual assessment of fetal heart rate (FHR) reactivity by some guidelines (RCOG 2001). These points should be considered in determining the applicability of the evidence presented here to different practice contexts.
It is reasonable to assume that outcomes related to perinatal death are perhaps those of most importance to women and maternity care professionals. In this review, there was no significant difference in perinatal mortality between admission CTG and intermittent auscultation. However, to identify correctly a 20% reduction in proportion of perinatal deaths (assuming a developed world rate of seven per 1000) between admission CTG and intermittent auscultation, a sample size of more than 100,000 is required (with α = 0.05, β‐1 = 20%) and even then a 20% reduction might be regarded as optimistic, with lower effect sizes requiring higher sample sizes. Such sample sizes are unlikely, except perhaps in the largest of mega‐trials, and therefore, typical randomised trials and systematic reviews of these trials, including this review, are insufficiently powered to evaluate the effects of different fetal monitoring modalities on fetal and neonatal mortality measures. Therefore, while this review found no evidence of an effect for admission CTG on perinatal mortality, this should not be confused with evidence of no effect.
There are other important outcomes, which are not reported, are unavailable or are not in a suitable format to be included in the analysis; these include perceived control and satisfaction with labour. This reflects a widespread tendency among the clinical and research community to frame outcomes in a non‐salutogenic or pathological manner (e.g. operative birth) rather than in a salutogenic, wellbeing‐orientated manner (e.g. normal birth). It may also reflect the relative difficulty of quantifying outcomes that are subjective and difficult, although important, to measure.
In addition to statistical heterogeneity, there was evidence of clinical heterogeneity between studies in the numbers of women having an epidural. In Impey 2003, significantly more women allocated to intermittent auscultation had an epidural compared with women allocated to admission CTG. This contrasts with Mires 2001, who found significantly fewer epidurals in women allocated to intermittent auscultation. The third study reporting on this outcome, Cheyne 2003, found no significant difference in epidurals between groups. It is difficult to explain such heterogeneity. All three studies found an increased rate of continuous electronic fetal monitoring for women allocated to admission CTG, making it unlikely that differing practices in use of continuous electronic fetal monitoring indications give rise to differential effects on epidural use. Futhermore, although the labours of nulliparous women in Impey 2003 were managed actively, the package of care for active management in labour has not been shown to impact on epidural rates (Brown 2008).
Quality of the evidence
Overall, risk of bias of the four included studies was assessed as low across all domains (Figure 2) with the exception of performance bias, which was judged to be high risk across all included outcomes for all studies, and blinded outcome assessment (detection bias), which was unclear in Mitchell 2008 and not carried out in Cheyne 2003. Of the 3752 women randomised during the third trimester in the study by Mires 2001, 37% developed an obstetric complication between randomisation and admission in labour that warranted continuous FHR monitoring in labour. Specific complications are given and these are in line with clinical norms reported in the literature. The study by Impey 2003 also included a small proportion of women with risk factors. Both Impey 2003 and Mires 2001 provided data for the subgroup of low‐risk women, and these data were used in the main analyses in this review. Sensitivity analyses were done in which the outcomes for all randomised women were used. Results were consistent with the main comparison effects, with the exception of two outcomes. Caesarean section became statistically significant, with significantly more women allocated to admission CTG having, on average, a caesarean section compared with women allocated to intermittent auscultation. Epidural also became significant, with significantly more women allocated to intermittent auscultation having, on average, an epidural compared with women allocated to admission CTG. However, these findings should be interpreted with caution. For the outcome caesarean section in whole‐group comparison, Mires 2001 contributes most weight to the meta‐analysis. However, in this study 37% (N = 704) of women randomised to intermittent auscultation developed complications during pregnancy and required admission CTG on admission.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Funding was provided by the hospitals where the trials took place (Cheyne 2003; Impey 2003; Mitchell 2008) or by government grants (Mires 2001). There were no declarations of interest made in Impey 2003 and Mires 2001. The other two trials (Cheyne 2003; Mitchell 2008) did not mention any declarations of interest.
The GRADE approach was used to assess evidence quality. All outcomes, with the exception of perinatal mortality rate, were downgraded for lack of blinding because it was felt that knowledge of allocation could affect the outcomes. The level of evidence for incidence of caesarean section was graded moderate. The other maternal outcomes (incidence of operative vaginal birth and of continuous electronic fetal monitoring during labour) were downgraded for imprecision and inconsistency respectively; the level of evidence for both outcomes was graded low. The evidence for perinatal mortality rate was graded moderate for imprecision due to wide confidence intervals crossing the line of no effect. Incidence of seizures in the neonatal period was graded low for imprecision. Incidence of hypoxic ischaemic encephalopathy was downgraded for wide confidence intervals crossing the line of no effect, few events and having data contributed from one small study meaning its level of evidence was graded very low. One main outcome (severe neurodevelopmental disability assessed at 12 months of age or more) selected for the 'Summary of findings' table was not reported. See Table 1.
Potential biases in the review process
It is possible that we introduced bias during the review process. However, we attempted to minimise bias by applying the following approaches: two review authors (DD, JGL) independently assessed for inclusion all the potential studies identified as a result of the search strategy. We attempted to identify all relevant trials by conducting a comprehensive search of the literature.
Declan Devane and Valerie Smith are currently conducting a trial, known as the ADCAR Trial, evaluating the effectiveness of the admission CTG compared with intermittent auscultation. This study is ongoing; however, if it is completed for future review updates, neither author will be involved in assessing the trial for inclusion, assessing risk of bias, or data extraction.
Agreements and disagreements with other studies or reviews
An earlier review on the effects of admission CTG compared with intermittent auscultation of the fetal heart rate (Gourounti 2007), which included three (Cheyne 2003; Impey 2003; Mires 2001) of the four trials included in our review found an increased relative risk of caesarean section and instrumental delivery associated with admission CTG group. Our finding supports the likelihood of an increased risk for caesarean section associated with admission CTG but we did not find a significant increase in instrumental delivery with admission CTG.
Authors' conclusions
Implications for practice.
Contrary to continued use in some clinical areas, we found no evidence of benefit for the use of the admission cardiotocograph (CTG) for low‐risk women on admission in labour. Furthermore, the probability is that admission CTG increases the caesarean section rate by approximately 20%. The data lacked power to detect possible important differences in perinatal mortality. However, it is unlikely that any trial, or meta‐analysis, will be adequately powered to detect such differences. The findings of this review support recommendations that the admission CTG not be used for women who are low risk on admission in labour (Liston 2007; NCCWCH 2007; RCOG 2001). Women should be informed that admission CTG is likely associated with an increase in the incidence of caesarean section without evidence of benefit.
It is important to note that all four trials included in this review were conducted in developed Western European countries. The usefulness of the findings of this review for developing countries will depend on FHR monitoring practices. However, an absence of benefit and likely harm associated with admission CTG will have relevance for countries where questions are being asked about the role of the admission CTG.
Implications for research.
All four included studies used the admission CTG on women in spontaneous or induced labour. Future studies evaluating the effects of the admission CTG should consider including women admitted with signs of labour and prior to a formal diagnosis of labour. This would include a cohort of women currently having admission CTGs and not included in current trials. The largest study in this review includes women where the colour of the liquor was known to be clear. Additional studies that evaluate the effects of the admission CTG on women where the colour of the amniotic fluid is not known are needed. Should future trials, including the ongoing ADCAR trial, identify differences in short term perinatal outcomes, information about long term neurodevelopmental outcomes will become important.
What's new
| Date | Event | Description |
|---|---|---|
| 10 May 2019 | Amended | Edited Declarations of interest |
History
Protocol first published: Issue 1, 2005 Review first published: Issue 2, 2012
| Date | Event | Description |
|---|---|---|
| 30 November 2016 | New search has been performed | Search updated and no new studies identified. |
| 30 November 2016 | New citation required but conclusions have not changed | For this no new studies update, GRADEpro Guideline Development Tool was used to import data from Review Manager 5.3 (RevMan 2014) in order to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for selected outcomes was produced using the GRADE approach. |
| 7 July 2010 | New citation required and major changes | Protocol substantially updated and reinstated. |
| 11 November 2009 | Amended | Protocol withdrawn from publication. |
| 12 May 2009 | Amended | Contact details updated. |
| 31 October 2008 | Amended | Converted to new review format. |
Acknowledgements
Our thanks to Mr Lawrence Impey who provided additional data for Impey 2003, to Dr Helen Cheyne who provided additional data for Cheyne 2003 and to Dr Fiona Williams who provided additional data for Mires 2001.
Our thanks also to Prof Mike Clarke for helpful discussions around group comparisons that informed this review methodology.
This project was supported by the National Institute for Health research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1. Admission cardiotocography versus Intermittent auscultation (low‐risk women).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caesarean section | 4 | 11338 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.00, 1.44] |
| 2 Instrumental vaginal birth | 4 | 11338 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.95, 1.27] |
| 3 Continuous EFM during labour | 3 | 10753 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.14, 1.48] |
| 4 Amniotomy | 2 | 2694 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.97, 1.12] |
| 5 Oxytocin for augmentation of labour | 4 | 11324 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.95, 1.17] |
| 6 Epidural | 3 | 10757 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.87, 1.41] |
| 7 Fetal blood sampling | 3 | 10757 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.13, 1.45] |
| 8 Fetal and neonatal deaths | 4 | 11339 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.30, 3.47] |
| 9 Evidence of fetal multi‐organ compromise within the first 24 hours after birth | 1 | 8056 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.19, 1.67] |
| 10 Admission to neonatal intensive care | 4 | 11331 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.86, 1.24] |
| 11 Apgar score < 7 at or after 5 minutes | 4 | 11324 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.54, 1.85] |
| 12 Hypoxic ischaemic encephalopathy | 1 | 2367 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.37, 3.90] |
| 13 Neonatal seizures | 1 | 8056 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.32, 1.61] |
| 14 Length of stay in neonatal intensive care (days) | 1 | 91 | Mean Difference (IV, Random, 95% CI) | 1.80 [‐0.59, 4.19] |
| 15 Length of stay in neonatal intensive care (hours) | 1 | 318 | Mean Difference (IV, Random, 95% CI) | 6.20 [‐8.70, 21.10] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cheyne 2003.
| Methods |
Study design: RCT. Duration of study: 1999. |
|
| Participants |
Setting: Glasgow Royal Maternity Hospital, Scotland. Inclusion criteria: healthy women who had experienced a normal pregnancy, presented at term in spontaneous labour and were eligible for admission to the Midwives Birth Unit. Exclusion criteria: women with risk factors. Participants randomised: 334 women (157 admission CTG (referred to as 'control group' in paper), 177 intermittent auscultation (referred to as 'study group' in paper)). Randomisation on admission in labour. |
|
| Interventions |
Admission CTG: a routine 20‐minute period of EFM at the time of admission. Intermittent auscultation: the fetal heart was auscultated during and immediately following a contraction for a minimum of 60 seconds. |
|
| Outcomes | Outcomes considered in the review and reported in or extracted from the study:
|
|
| Notes | Unpublished data to permit re‐inclusion of women to groups as randomised kindly provided by author. This study was funded by North Glasgow University Hospitals NHS Trust. Declaration of interest were not mentioned in the trial. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...computer‐generated in order to allocate participants equally between the two groups..." |
| Allocation concealment (selection bias) | Low risk | "...sequentially numbered, sealed opaque envelopes, which contained allocation to the appropriate group." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although not documented, we judged, given nature of intervention, that women and clinicians were not blind to the interventions used. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: in the trial report 22 women (7%) are excluded from the analysis (21 women entered into the study and found not to be in labour and 1 randomisation card missing). However, data for these 21 of 22 women were identified and extracted subsequently by the trial author and kindly provided to the review team. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods section were reported adequately in results. |
| Other bias | Low risk | None identified. |
Impey 2003.
| Methods |
Study design: RCT. Duration of study: 1997 to 2001. |
|
| Participants |
Setting: National Maternity Hospital in Dublin, Ireland. Inclusion criteria: women were eligible for inclusion if they were admitted in labour, a singleton pregnancy, fewer than 42 completed weeks of gestation, no suspicion or evidence of antenatal fetal compromise, no adverse obstetric history, clear amniotic fluid, and maternal temperature of 37.5°C or less at admission. Participants randomised: 8628 women (4320 admission CTG, 4308 intermittent auscultation). Randomisation on admission in labour. A relatively small number (fewer than 5%) of women who had a previous caesarean section and who went into labour prior to 37 completed weeks' gestation were included in this study and were randomised. The trial author kindly provided data separately for the outcomes for women (i) between 37 and 42 completed weeks with (ii) an absence of previous caesarean section and these data were used in the main analyses for this review. Sensitivity analyses were conducted in which the outcomes for all randomised women were used. |
|
| Interventions |
Admission CTG: a 20‐minute admission CTG immediately after early amniotomy done on diagnosis of labour in women presenting to the delivery ward. Intermittent auscultation: intermittent auscultation was used for 1 minute after a contraction every 15 minutes in the first stage and every 5 minutes in the second stage of labour. This was done after early amniotomy on diagnosis of labour in women presenting to the delivery ward. |
|
| Outcomes | Outcomes considered in the review and reported in or extracted from the study:
|
|
| Notes | See Participants (above) The study was funded by the Research Committee of the National Maternity Hospital, Holles St, Dublin, Ireland. Declarations of interest: none declared. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...the randomisation sequence was from a commercial package 10 and used a fixed block size of 100. It was changed after 2621 patients had been recruited, and was generated by the National Perinatal Epidemiology Unit with random block sizes of 100–250." |
| Allocation concealment (selection bias) | Low risk | "...sealed, opaque, sequentially numbered envelope." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although not documented, we judged, given nature of intervention, that women and clinicians were not blind to the interventions used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "...Data were entered and neonatal assessment was made without knowledge of the randomised assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up = 22 (0.5%); admission CTG 26 (0.6%). Intermittent auscultation. For outcome 'pH less than 7 or BD/E > than 12 mmol/L' 7.5% and 7.8% data missing for admission CTG and intermittent auscultation respectively. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods section were reported adequately in results. |
| Other bias | Low risk | None identified. |
Mires 2001.
| Methods |
Study design: RCT. Duration of study: not stated. |
|
| Participants |
Setting: Dundee, Scotland. Inclusion criteria: "Women were eligible to join the study if they were booked for hospital delivery, attended a hospital or community based consultant led clinic in the third trimester of pregnancy, and had no obstetric complications at that visit that would warrant continuous intrapartum monitoring of FHR (pre eclampsia or hypertension in previous or index pregnancy; essential hypertension; diabetes (insulin dependent or gestational); suspected intrauterine growth restriction; placental abruption or praevia or vaginal bleeding of unknown origin; multiple pregnancy; fetal malformation; previous caesarean section; breech presentation; or rhesus isoimmunisation)." Participants randomised: 3752 women randomised. "No data collected n = 1" (1866 admission CTG, 1885 intermittent auscultation). A total of 3752 women were recruited to the study and randomised during the third trimester. However, some women developed an obstetric complication between randomisation and admission in labour that warranted continuous FHR monitoring in labour, such that only 2367 women were judged to be low‐risk when in labour (1186 admission CTG, 1181 intermittent auscultation). The trial author kindly provided data separately for the outcomes in this subgroup of women and these data are used in the main analyses in this review. Sensitivity analyses were done in which the outcomes for all randomised women were used. |
|
| Interventions |
Admission CTG: a 20‐minute CTG on admission in spontaneous uncomplicated labour. Intermittent auscultation: auscultation of the fetal heart with a hand‐held Doppler device during and immediately after at least 1 contraction. |
|
| Outcomes | Outcomes considered in the review and reported in or extracted from the study:
|
|
| Notes | See Participants (above) This study was funded by Chief Scientists Office of the Scottish Executive, Edinburgh. Declarations of interest: none declared. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...commercially available computer randomisation program." |
| Allocation concealment (selection bias) | Low risk | "The allocation was placed in a sealed envelope..." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although not documented, we judged, given nature of intervention, that women and clinicians were not blind to the interventions used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The data analysts were blind to the randomisation code." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up for the primary outcome of metabolic acidosis was high (admission CTG N = 310, 26% and intermittent auscultation N = 321, 27%). However, metabolic acidosis was defined as "pH less than 7.20 or BD (Base Deficit) > than 8 mmol/L". Data were unavailable for the outcome metabolic acidosis as defined in this review, i.e. 'pH less than 7 or BD/E > than 12 mmol/L', therefore this study does not provide data for this outcome in this review. All other outcomes had low rates of missing data, hence rating as low risk of bias. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods section were reported adequately in results. |
| Other bias | Low risk | "Between randomisation during the third trimester of pregnancy and admission in labour, 1384 women (37%) developed an obstetric complication that warranted continuous fetal heart rate monitoring in labour". A total of 3752 women were recruited to the study and randomised during the third trimester. However, some women developed complications between randomisation and admission in labour, such that only 2367 women were judged to be low risk when in labour (1186 admission CTG, 1181 intermittent auscultation). There are similar levels of attrition in both groups due to development of complications suggesting that allocation concealment remained intact. The trial author kindly provided data separately for the outcomes in this low‐risk subgroup of women and these data are used in the main analyses in this review. |
Mitchell 2008.
| Methods |
Study design: RCT. Duration of study: 2002 to 2006. |
|
| Participants |
Setting: Buckinghamshire, England. Inclusion criteria: labouring women considered to be "low risk" of fetal or maternal complications on admission. Exclusion criteria: any minor maternal medical complication, e.g. diabetes or essential hypertension; previous caesarean section; preterm labour (< 37 completed weeks); multiple pregnancy; prolonged pregnancy (> 42 completed weeks); prolonged membrane rupture (more than 24 hours); induction of labour; meconium‐stained liquor; maternal pyrexia; rhesus sensitisation; polyhydramnios; oligohydramnios; pre‐eclampsia or blood pressure over 140/90 mmHg; abnormal presentation or lie (e.g. breech, transverse); high head (5/5ths palpable per abdomen); antepartum or intrapartum haemorrhage; known or suspected intrauterine growth retardation; any known or suspected fetal medical complication; abnormal Doppler artery velocimetry; known fetal malformation; poor obstetric history (e.g. history of stillbirth); un‐booked. Participants randomised: 582 women randomised (298 admission CTG, 284 intermittent auscultation). Randomisation on admission in labour. |
|
| Interventions |
Admission CTG: a 15‐minute CTG on admission in spontaneous uncomplicated labour. Intermittent auscultation: auscultation of the fetal heart for one continuous minute using a Pinard stethoscope or Doppler ultrasound device, after a contraction, at least every 15 minutes in the first stage of labour, and every 5 minutes in the second stage of labour. |
|
| Outcomes | Outcomes considered in the review and reported in or extracted from the study:
|
|
| Notes | See Participants. The study was funded by Buckinghamshire Hospitals NHS Trust's Research Department and through the establishment of a research midwife role within the maternity unit. Declaration of interest not mentioned. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...via a random number table." |
| Allocation concealment (selection bias) | Low risk | "Allocation to control and experimental arms was via opening of the next envelope in a series of sequentially numbered envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although not documented, we judged, given nature of intervention, that women and clinicians were not blind to the interventions used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data reported with exception of "augmentation with oxytocin" where missing data were low (admission CTG N = 2, 0.7% and intermittent auscultation N = 4, 1.4%). |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods section were reported adequately in results. |
| Other bias | Low risk | None identified. |
BD: base deficit BD/E: base deficit/excess CTG: cardiotocograph EFM: electronic fetal monitoring FHR: fetal heart rate RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Devane 2008.
| Trial name or title | Foetal cardiotocography versus intermittent auscultation during labour ward admission: a randomised controlled trial (the ADCAR trial) |
| Methods | RCT |
| Participants |
|
| Interventions |
|
| Outcomes | Primary: incidence of caesarean section |
| Starting date | 2008 |
| Contact information | Declan Devane declan.devane@nuigalway.ie |
| Notes |
CTG: cardiotocograph EFM: electronic fetal monitoring RCT: randomised controlled trial
Differences between protocol and review
Additional post‐hoc sensitivity analyses have been conduced beyond those stated in the protocol. These have been identified clearly as post‐hoc analyses.
Contributions of authors
Declan Devane (DD) and Valerie Smith (VS) drafted the background section and all other authors contributed to editing the text. All authors contributed to the drafting of the inclusion criteria for the review. DD added the methodology section with other authors commenting. DD, VS and Joan G. Lalor (JGL) abstracted and pooled data. DD wrote the results section, discussion and implications sections with input from all authors. Declan Devane is the guarantor of this review.
Anna Cuthbert prepared this 'no new studies' update and it was reviewed by all other authors.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Health Research Board, Ireland.
Declan Devane and Valerie Smith are currently conducting a trial, known as the ADCAR Trial, evaluating the effectiveness of the admission CTG compared with intermittent auscultation.
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Declan Devane is currently conducting a trial, known as the ADCAR Trial, evaluating the effectiveness of the admission cardiotocograph (CTG) compared with intermittent auscultation. This study is funded by the Health Research Board (Ireland). If this trial is eligible for inclusion in the full review, or a subsequent review update, the investigators will not be involved in assessing the trial for inclusion, assessing risk of bias, or data extraction. These tasks will be carried out by two other members of the review team who are not directly involved with the ADCAR Trial.
Joan G Lalor: none known.
Sean Daly: none known.
William McGuire: none known.
Anna Cuthbert: none known.
Valerie Smith: is currently conducting a trial, known as the ADCAR Trial, evaluating the effectiveness of the admission cardiotocograph (CTG) compared with intermittent auscultation. This study is funded by the Health Research Board (Ireland). If this trial is eligible for inclusion in the full review, or a subsequent review update, the investigators will not be involved in assessing the trial for inclusion, assessing risk of bias, or data extraction. These tasks will be carried out by two other members of the review team who are not directly involved with the ADCAR Trial.
Edited (no change to conclusions)
References
References to studies included in this review
Cheyne 2003 {published data only}
- Cheyne H, Dunlop A, Shields N, Mathers AM. A randomised controlled trial of admission electronic fetal monitoring in normal labour. Midwifery 2003;19(3):221‐9. [DOI] [PubMed] [Google Scholar]
Impey 2003 {published data only}
- Impey L, Reynolds M, MacQuillan K, Gates S, Murphy J, Sheil O. Admission cardiotocography: a randomised controlled trial. Lancet 2003;361(9356):465‐70. [DOI] [PubMed] [Google Scholar]
Mires 2001 {published data only}
- Mires G, Williams F, Howie P. Randomised controlled trial of cardiotocography versus doppler auscultation of fetal heart at admission in labour in low risk obstetric population. BMJ 2001;322(7300):1457‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mires GJ, Williams FLR, Howie PW. Randomised controlled trial of cardiotocography versus doppler auscultation of the fetal heart at admission in labour in a low risk obstetric population [abstract]. Journal of Perinatal Medicine 2001;29 Suppl 1(Pt 2):295. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2008 {published data only}
- ISRCTN28370122. A randomised controlled trial evaluating the relationship between the labour electronic fetal monitoring (EFM) admission test and obstetric intervention in low risk mothers. isrctn.com/ISRCTN28370122 Date first received: 12 September 2003.
- Mitchell K. The effect of the labour electronic fetal monitoring admission test on operative delivery in low‐risk women: a randomised controlled trial. Evidence Based Midwifery 2008;6(1):18‐26. [Google Scholar]
References to ongoing studies
Devane 2008 {published data only}
- ISRCTN96340041. A randomised controlled trial comparing the effect of admission cardiotocography versus intermittent auscultation of the foetal heart rate on low‐risk women on admission to labour ward showing signs of possible labour. isrctn.com/ISRCTN96340041 Date first received: 25 March 2008.
Additional references
Alfirevic 2013
- Alfirevic Z, Stampalija T, Gyte GML. Fetal and umbilical Doppler ultrasound in high‐risk pregnancies. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD007529] [DOI] [PMC free article] [PubMed] [Google Scholar]
Arulkumaran 2000
- Arulkumaran S, Jenkins HML. Perinatal Asphyxia. Chennai: Orient Longman Ltd, 2000. [Google Scholar]
Ayres‐de‐Campos 2015
- Ayres‐de‐Campos D, Spong CY, Chandraharan E. FIGO consensus guidelines on intrapartum fetal monitoring: Cardiotocography. International Journal of Gynaecology and Obstetrics 2015;131(1):13‐24. [DOI] [PubMed] [Google Scholar]
Bayley 1993
- Bayley N. Manual for the Bayley Scales of Infant Development. 2nd Edition. San Antonio: The Psychological Corporation, 1993. [Google Scholar]
Brown 2008
- Brown HC, Paranjothy S, Dowswell T, Thomas J. Package of care for active management in labour for reducing caesarean section rates in low‐risk women. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD004907.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caldeyro‐Barcia 1966
- Caldeyro‐Barcia R, Mendez‐Bauer C, Poseiro JJ, Escarcena LA, Pose SV, Bieniarz J, et al. Control of human fetal heart rate during labour. In: Cassels DE editor(s). The Heart and Circulation in the Newborn and Infant. New York: Grune and Stratton, 1966:7‐36. [Google Scholar]
CESDI 2001
- Maternal and Child Health Research Consortium. Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI): 8th Annual Report. London: Maternal and Child Health Research Consortium, 2001. [Google Scholar]
Devane 2007
- Devane D, Lalor J, Bonnar J. The use of intrapartum electronic fetal heart rate monitoring: a national survey. Irish Medical Journal 2007;100(2):360‐2. [PUBMED: 17432809] [PubMed] [Google Scholar]
East 2013
- East CE, Smyth RMD, Leader LR, Henshall NE, Colditz PB, Lau R, et al. Vibroacoustic stimulation for fetal assessment in labour in the presence of a nonreassuring fetal heart rate trace. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD004664] [DOI] [Google Scholar]
Gail‐Thomas 2003
- Gail‐Thomas B. The disempowering concept of risk. In: Wickham S editor(s). Midwifery Best Practice. London: Books for Midwives Press, 2003:3‐6. [Google Scholar]
Gourounti 2007
- Gourounti K, Sandall J. Admission cardiotocography versus intermittent auscultation of fetal heart rate: effects on neonatal Apgar score, on the rate of Caesarean sections and on the rate of instrumental delivery. A systematic review. International Journal of Nursing Studies 2007;44(6):1029‐1035. [DOI] [PubMed] [Google Scholar]
Grivell 2012
- Grivell RM, Wong L, Bhatia V. Regimens of fetal surveillance for impaired fetal growth. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD007113] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grivell 2015
- Grivell RM, Alfirevic Z, Gyte GML, Devane D. Antenatal cardiotocography for fetal assessment. Cochrane Database of Systematic Reviews 2015, Issue 9. [DOI: 10.1002/14651858.CD007863] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hammacher 1968
- Hammacher K, Hūter K, Bokelmann J, Werners P. Foetal heart frequency and perinatal condition of the foetus and newborn. Gynecologica 1968;166(4):349‐60. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Holzmann 2010
- Holzmann M, Nordström L. Follow‐up national survey (Sweden) of routines for intrapartum fetal surveillance. Acta Obstetricia et Gynecologica Scandinavica 2010;89(5):712‐4. [DOI] [PubMed] [Google Scholar]
Hon 1958
- Hon EH. The electronic evaluation of the fetal heart rate; preliminary report. American Journal of Obstetrics and Gynecology 1958;75(6):1215‐30. [DOI] [PubMed] [Google Scholar]
Kaczorowski 1998
- Kaczorowski J, Levitt C, Hanvey L, Avard D, Chance G. A national survey of use of obstetric procedures and technologies in Canadian hospitals: routine or based on existing evidence?. Birth 1998;25(1):11‐8. [DOI] [PubMed] [Google Scholar]
Lalor 2008
- Lalor JG, Fawole B, Alfirevic Z, Devane D. Biophysical profile for fetal assessment in high risk pregnancies. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD000038.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liston 2007
- Liston R, Sawchuck D, Young D, Society of Obstetrics and Gynaecologists of Canada, British Columbia Perinatal Health Program. Fetal health surveillance: antepartum and intrapartum consensus guideline. Journal of Obstetrics and Gynaecology Canada 2007;29(9 Suppl 4):S3‐56. [PubMed] [Google Scholar]
MacLennan 1999
- MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. BMJ 1999;319(7216):1054‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mangesi 2015
- Mangesi L, Hofmeyr GJ, Smith V, Smyth RMD. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD004909] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nabhan 2008
- Nabhan AF, Abdelmoula YA. Amniotic fluid index versus single deepest vertical pocket as a screening test for preventing adverse pregnancy outcome. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD006593.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCCWCH 2007
- National Collaborating Centre for Women’s and Children’s Health. Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. London: RCOG Press, 2007. [PubMed] [Google Scholar]
Neilson 2012
- Neilson JP. Biochemical tests of placental function for assessment in pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD000108] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 1996
- Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. New England Journal of Medicine 1996;334(10):613‐8. [DOI] [PubMed] [Google Scholar]
RANZCOG 2002
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Clinical Guidelines: Intrapartum Surveillance. East Melbourne: RANZCOG, 2002. [Google Scholar]
RCOG 2001
- Royal College of Obstetricians and Gynaecologists. The Use of Electronic Fetal Monitoring: the Use and Interpretation of Cardiotocography in Intrapartum Fetal Surveillance. Evidence‐based Clinical Guideline Number 8. London: Royal College of Obstetricians and Gynaecologists, 2001. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sarnat 1976
- Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress: a clinical and electrographic study. Archives of Neurology 1976;33(10):696‐705. [DOI] [PubMed] [Google Scholar]
Stampalija 2010
- Stampalija T, Alfirevic Z, Gyte GML. Utero‐placental Doppler ultrasound for improving pregnancy outcome. Cochrane Database of Systematic Reviews 2010, Issue 2. [DOI: 10.1002/14651858.CD008363] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2012
- Tan KH, Sabapathy A. Maternal glucose administration for facilitating tests of fetal wellbeing. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD003397] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2013a
- Tan KH, Sabapathy A, Wei X. Fetal manipulation for facilitating tests of fetal wellbeing. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD003396] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2013b
- Tan KH, Smyth RMD, Wei X. Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD002963] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1999
- World Health Organization. Care in Normal Birth: a Practical Guide. Report of a Technical Working Group. Geneva: World Health Organization, 1999. [Google Scholar]
References to other published versions of this review
Devane 2010
- Devane D, Lalor JG, Daly S, McGuire W, Smith V. Cardiotocography versus intermittent auscultation of fetal heart on admission to labour ward for assessment of fetal wellbeing. Cochrane Database of Systematic Reviews 2010, Issue 8. [DOI: 10.1002/14651858.CD005122.pub3] [DOI] [PubMed] [Google Scholar]
Devane 2012
- Devane D, Lalor JG, Daly S, McGuire W, Smith V. Cardiotocography versus intermittent auscultation of fetal heart on admission to labour ward for assessment of fetal wellbeing. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD005122.pub4] [DOI] [PubMed] [Google Scholar]


