Abstract
Background: Compared with men, women have poorer lipid control. Although potential causes of this disparity have been explored, it is unknown whether patient-centered factors such as satisfaction and confidence contribute. We evaluated (1) whether satisfaction with lipid control and confidence in ability to improve it vary by gender and (2) whether sociodemographic characteristics modify the association.
Materials and Methods: We evaluated baseline survey responses from the Cardiovascular Intervention Improvement Telemedicine Study, including self-rated satisfaction with cholesterol levels and confidence in controlling cholesterol. Participants had poorly controlled hypertension and/or hypercholesterolemia.
Results: A total of 428 veterans (15% women) participated. Compared with men, women had higher low-density lipoprotein values at 141.2 versus 121.7 mg/dL, respectively (p < 0.05), higher health literacy, and were less likely to have someone to help track their medications (all p < 0.05). In an adjusted model, women were less satisfied with their cholesterol levels than men with estimated mean scores of 4.3 versus 5.6 on a 1–10 Likert scale (p < 0.05). There was no significant difference in confidence by gender. Participants with support for tracking medications reported higher confidence levels than those without, estimated mean 7.8 versus 7.2 (p < 0.05).
Conclusions: Women veterans at high risk for cardiovascular disease were less satisfied with their lipid control than men; however, confidence in ability to improve lipid levels was similar. Veterans without someone to help to track medications were less confident, and women were less likely to have this type of social support. Lack of social support for medication tracking may be a factor in lingering gender-based disparities in hyperlipidemia.
Keywords: : disparities, women's health, chronic disease, health behavior
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality among women in the United States and, compared with men, more women die annually from CVD.1 Although there have been significant improvements in overall CVD-related mortality in recent decades, this trend has not been realized in women <55 years.2
Not only does the physiology and clinical presentation of CVD differ between men and women, but also current risk stratification systems appear to be less accurate for women.3 Women are more likely than men to have certain nontraditional CVD risk factors, such as depression4 or rheumatoid arthritis,5 which are typically not accounted for in standard risk calculations. Compared with men, women are less likely to be physically active,1 less likely to have their hypertension controlled when older,6 may have a greater adverse health effects from smoking,7 have more difficulty with smoking cessation,8,9 and incur a greater increase in CVD risk because of diabetes.10 In addition to these differences and disparities in CVD risk factors between the sexes, women have worse lipid control than men.11–16
The reason for this disparity in lipid control is not fully understood. Until recently, women have been under-represented in CVD clinical trials17,18 including trials of statin use. Recent findings19 and guidelines20,21 support statin use in primary and secondary prevention of CVD among women; however, the application in clinical practice continues to be complicated and variable.22 Women are less likely to receive appropriate statin regimens than men,16,23 particularly for secondary prevention and treatment intensification.15,24,25 Multiple other contributing factors for the gender disparity in lipid control have been put forth, including gender disparities in medication adherence,15,26–28 treatment escalation,16,23,29,30 awareness of CVD risk,31,32 lifestyle factors,33 and gender differences in statin side effect profiles.15 However, little attention has been paid to the potential impact of patient-centered factors in gender-based lipid disparities.
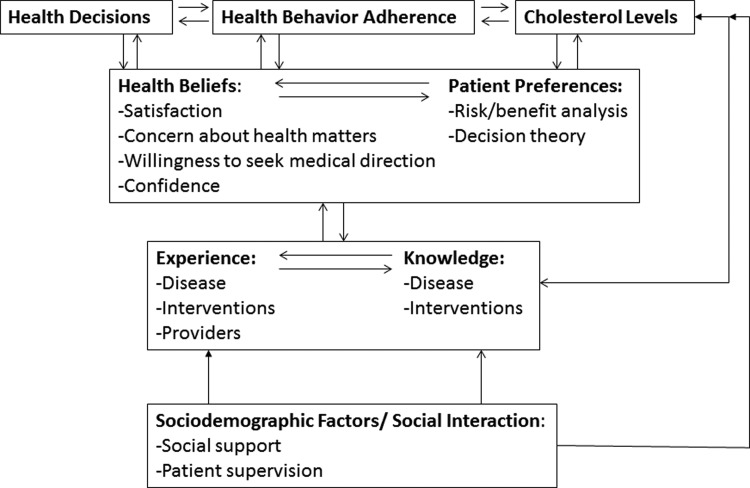
To frame an evaluation of patient-centered factors in gender-based disparities in lipid control, we use key constructs from the Health Decision Model (HDM).34 The HDM highlights the influence of health beliefs, patient experience, sociodemographic factors, and social interactions on health decisions, behaviors, and outcomes.34 As applied to gender disparities in lipid control, the patient-centered HDM constructs of particular interest include patients' satisfaction and confidence. Although not explicitly defined by the HDM, we conceptualize confidence as a health belief that is similarly influenced by patient experience and knowledge (Fig. 1).
FIG. 1.
Patient-centered factors in lipid control (adapted from Eraker et al.34).
Patient satisfaction and confidence have been shown to relate to health outcomes. Higher levels of satisfaction with treatment impact decisions made about health-related behaviors, improve motivation to adhere to recommended treatment,35–37 and improve quality of life in certain chronic conditions.35 Similarly, higher levels of self-efficacy, a construct with similarities to confidence, have been associated with better self-management behaviors such as medication adherence in hypertension38,39 and diabetes outcomes.40 Gender disparities in satisfaction and confidence may exist. In the context of diabetes, women have been found to have lower levels of self-efficacy than men, which is related to worse biological disease markers.41,42
Examining patient-centered factors could fill an important gap in our understanding of gender-based differences in lipid control. If gender differences exist for satisfaction and confidence related to hyperlipidemia, then those differences may also contribute to disparities in lipid control. Subsequently, understanding the role of patient-centered factors among women in lipid control could inform future targeted interventions. Therefore, we surveyed male and female patients at high risk for CVD to evaluate (1) whether satisfaction with lipid control and confidence in ability to improve it vary by gender and (2) whether sociodemographic characteristics (e.g., health literacy and work status) modify the association.
Materials and Methods
We examined baseline survey responses from veterans who participated in a clinical trial to improve cardiovascular risk, Cardiovascular Intervention Improvement Telemedicine Study (CITIES; ClinicalTrials.gov Identifier NCT01142908). CITIES has been previously described.43,44 In brief, this is a telephone-based, 12-month, clinical pharmacist-delivered medication and behavioral management intervention to reduce CVD risk for veterans with existing poorly controlled hypertension and/or hyperlipidemia. Participants were randomized to a usual care or an intervention arm. Those randomized to the usual care arm received education materials in print format, whereas those randomized to the intervention received monthly phone calls to discuss home-based self-monitoring results of blood pressure and blood glucose (if diagnosed with diabetes) and to receive guidance on medication adjustment and specific health behavior recommendations (e.g., smoking cessation and dietary adjustments) from a clinical pharmacist. For the remainder of this article, we discuss the results from the baseline assessment for participants in both arms of the study. The Durham Veterans Affairs Medical Center (VAMC) Institutional Review Board approved the study. All participants completed informed consent.
Participants
We enrolled participants from November 2011 to April 2014. To be eligible for CITIES, patients had to (1) reside in North Carolina or Virginia, (2) be of age 40 years or older, (3) attend one of three Durham VAMC-affiliated primary care clinics and have at least one primary care visit within the last year, and (4) have poorly controlled hypertension (defined as blood pressure [BP] >150/100 mmHg) and/or hyperlipidemia (defined as low-density lipoprotein [LDL] >130 mg/dL) within the preceding year as documented in the medical record. Of note, at the time of this study, the VA recommended lipid screening every 5 years starting at age 45 years for women and age 35 years for men, and annually for those with known coronary artery disease, diabetes, or peripheral vascular disease. The frequency of repeat screening was encouraged through electronic medical record clinical reminders. Cutoff levels were based on clinical guidelines available at the time of study initiation; for hypertension, mean BP had to be >150/100 mmHg, and for hypercholesterolemia, the mean LDL had to be >130 mg/dL in the previous year. ICD-9 codes were used to establish diagnoses, specifically, we used 401.0, 401.1, and 401.9 for hypertension and 272.0–272.9 for hyperlipidemia. Individuals were excluded if they had any of the following: (1) metastatic cancer, dementia, active psychosis, or significant renal dysfunction as defined by a serum creatinine of >2.5 mg/dL or dialysis; (2) no laboratory values on file in the last year; (3) reside in a nursing home; (4) unable to use the telephone because of lack of access or difficulty hearing; (5) recent hospitalization for myocardial infarction, stroke, or cardiac surgery within the preceding 3 months; or (6) were actively enrolled in another clinical trial or clinical pharmacy service.
Potential study participants were identified in the electronic medical record using the stated screening eligibility criteria and sorted by gender to over-sample women who are underrepresented in the VA. Before an upcoming clinic appointment, eligible patients were mailed an introduction letter that included a toll-free opt-out number and that was signed by their primary care provider. Individuals who did not opt out were then contacted by a research assistant on the study team to review additional eligibility criteria and schedule an inperson visit. At the inperson visit, participants completed informed consent.
Data collection and outcomes
At the time of study enrollment, the participant completed a survey and underwent a medical assessment by a study team member. Participants were determined to have diabetes at the time of randomization based on self-report and administrative data. Baseline laboratory work was obtained within 30 days of the initial study visit, but the results were not necessarily available to subjects at the time of the baseline survey. The baseline survey included multiple self-report variables, including age, race, marital status, education level, financial status, and current medication cost. Weight, height, and BP were also measured at the baseline visit. Participants were also asked to complete the Rapid Estimate of Adult Literacy in Medicine (REALM) test.45 We dichotomized the REALM scores into a binary measure identifying low literacy (equivalent to an eighth-grade reading level) using a total score <60 as has been done previously.45
To assess aspects of social support, participants were asked the following questions: (1) “If needed, is there someone who could help you with tasks such as taking you to the doctor, fixing lunch, or home repairs?” with yes/no response and (2) “There is no one to help me keep track of when to take pills” with responses ranging from definitely true to definitely false. The responses to this question were dichotomized into the following categories: “definitely true/probably true” and “definitely false/probably false.”
Patients were asked to rate on a scale of 1–10 “how confident are you that you can control your cholesterol?” (1 = not at all confident, 10 = completely confident) and “how satisfied are you with your cholesterol levels?” (1 = definitely not satisfied, 10 = definitely satisfied).
Data analysis
We describe sociodemographic characteristics for the participants who completed the baseline survey both overall and by gender using means and proportions. Differences between groups were analyzed using t-tests and Chi-squared tests. Unadjusted and adjusted multivariable linear regression models were used to examine the relationship between levels of satisfaction with cholesterol levels and confidence in controlling cholesterol and key factors, including gender and social support. Based on earlier stated objectives, models were fit for each of the outcomes, satisfaction, and confidence, separately. Sociodemographic characteristics and medical diagnosis variables of interest, including cholesterol diagnosis, were identified for inclusion in the model a priori. All selected variables were looked at in unadjusted models, then inputted into the adjusted models. All data analyses were completed using SAS software version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Overall, 428 veterans completed the baseline survey, including 65 women (15%) (Table 1). Of those patients who were contacted and eligible for the study, 42% of women and 37% of men completed consent. For the satisfaction measure, 40 participants were missing responses (36 men and 4 women) because of reporting “don't know.” For confidence, there were 11 participants with missing response (nine men and two women) for the same reason. Compared with men, women were significantly younger (54.2 years [standard deviation (SD) 7.5] vs. 62.4 years [SD 8.2]), less likely to be married (35.4% vs. 60.6%), less likely to have low health literacy (13.8% vs. 36.9%), and were more likely to report that they had no one to help track their medications (33.3% vs. 20.6%). Six women (and seven men) were 44 years of age or younger (i.e., likely of child-bearing age). There were no gender differences in work status, financial status, out-of-pocket prescription costs, or having someone to help with tasks such as being taken to the doctor, fixing lunch, or home repairs. Although men and women had similar rates of diagnosis of hyperlipidemia, women had higher mean LDL values at baseline visit than male participants, 141.2 versus 121.7 mg/dL, respectively (p < 0.01). Men were more likely than women to have a diagnosis of hypertension (92.3% vs. 78.5%) and diabetes (42.1% vs. 27.7%); however men and women had similar body mass indices. Among men and women with diabetes, hemoglobin A1cs were similar. Diastolic BP was similar between all men and women at baseline, although men had a higher systolic BP than women (mean 131.2 vs. 124.4 mmHg) at baseline. Overall mean for satisfaction with cholesterol levels was 5.1 (SD 3.2), mean confidence in ability to control cholesterol was 7.8 (SD 2.6).
Table 1.
Baseline Characteristics of Participants Overall and by Gender
| Characteristic | Overall N = 428 | Women N = 65 | Men N = 363 | p valuea |
|---|---|---|---|---|
| Age, mean (SD) | 61.2 (8.7) | 54.2 (7.5) | 62.4 (8.2) | <0.01 |
| Non-Hispanic white,bn (%) | 195 (45.8) | 23 (35.9) | 172 (47.5) | 0.10 |
| Married, n (%) | 243 (56.8) | 23 (35.4) | 220 (60.6) | <0.01 |
| ≤High school education | 128 (29.9) | 9 (13.8) | 119 (32.8) | <0.01 |
| Low health literacy, n (%) | 143 (33.4) | 9 (13.8) | 134 (36.9) | <0.01 |
| Inadequate financial status,bn (%) | 103 (24.2) | 22 (34.4) | 81 (22.4) | 0.06 |
| Working at least part-time, n (%) | 128 (29.9) | 13 (20.0) | 115 (31.7) | 0.08 |
| Out-of-pocket medication costs ≥$51 per month, n (%) | 89 (20.8) | 13 (20.0) | 76 (20.9) | 0.87 |
| No one to help with tasks if needed,bn (%) | 42 (9.8) | 8 (12.3) | 34 (9.4) | 0.50 |
| No one to help track medications,bn (%) | 95 (22.5) | 21 (33.3) | 74 (20.6) | 0.03 |
| Current smoker, n (%) | 124 (29.0) | 21 (32.3) | 103 (28.4) | 0.55 |
| Diabetes, n (%) | 171 (40.0) | 18 (27.7) | 153 (42.1) | 0.04 |
| Hyperlipidemia, n (%) | 317 (74.1) | 48 (73.8) | 269 (74.1) | 1.00 |
| Hypertension, n (%) | 386 (90.2) | 51 (78.5) | 335 (92.3) | <0.01 |
| LDL cholesterol,b mean (SD) | 124.7 (36.7) | 141.2 (34.6) | 121.7 (36.3) | <0.01 |
| SBP,b,c mean (SD) | 130.1 (18.7) | 124.4 (19.7) | 131.2 (18.3) | <0.01 |
| DBP,b,c mean (SD) | 75.8 (12.0) | 76.8 (10.1) | 75.6 (12.3) | 0.49 |
| BMI,b mean (SD) | 31.8 (5.7) | 31.1 (5.9) | 31.9 (5.7) | 0.32 |
| HbA1c,b,d mean (SD) | 7.8 (2.0) | 8.1 (2.6) | 7.8 (1.9) | 0.53 |
t-tests and Chi-squared tests.
Missing data: two patients have missing race data, three have missing data for inadequate financial status, one has missing help with tasks if needed, five have missing data for help track medications, six have missing data for LDL cholesterol, one has missing data for blood pressure measurements, six have missing data for BMI, six have missing data for HbA1c.
Blood pressure values were averaged over three measurements obtained at the baseline assessment visit.
Restricted to patients with diabetes.
LDL, low density lipoprotein (mg/dL); SD, standard deviation; SBP, systolic blood pressure (mmHg); DBP, diastolic blood pressure (mmHg); BMI, body mass index; HbA1c, hemoglobin A1c.
Unadjusted results indicated that the measure of satisfaction with cholesterol levels was significantly lower among female participants with estimated means of 3.6 versus 5.4 (p < 0.01), a finding that persisted in the adjusted model with estimated means of 4.3 versus 5.6 (p < 0.01). There was no association between satisfaction and measures of social support, race/ethnicity, financial status, or medication costs. Lower education level, working at least part time, and low health literacy were significantly associated with higher levels of satisfaction in the unadjusted models only (see Table 2).
Table 2.
Satisfaction with Cholesterol Levels
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Least square means (standard error) | p value | Least square means (standard error) | p value | |
| Gender | ||||
| Women | 3.6 (0.4) | <0.01 | 4.3 (0.5) | <0.01 |
| Men | 5.4 (0.2) | 5.6 (0.3) | ||
| Race | ||||
| Non-Hispanic white | 5.1 (0.2) | 0.93 | 5.1 (0.4) | 0.45 |
| Other | 5.1 (0.2) | 4.8 (0.4) | ||
| Married | ||||
| Yes | 5.2 (0.2) | 0.31 | 4.8 (0.4) | 0.40 |
| No | 4.9 (0.2) | 5.1 (0.4) | ||
| Highest level of education | ||||
| ≤High school | 5.9 (0.3) | <0.01 | 5.3 (0.5) | 0.10 |
| >High school | 4.8 (0.2) | 4.7 (0.4) | ||
| Low health literacy | ||||
| Yes | 5.6 (0.3) | 0.04 | 5.2 (0.4) | 0.22 |
| No | 4.9 (0.2) | 4.7 (0.4) | ||
| Inadequate financial status | ||||
| Yes | 4.8 (0.3) | 0.33 | 4.8 (0.4) | 0.27 |
| No | 5.2 (0.2) | 5.2 (0.4) | ||
| Working at least part-time | ||||
| Yes | 5.7 (0.3) | <0.01 | 5.2 (0.5) | 0.12 |
| No | 4.8 (0.2) | 4.7 (0.4) | ||
| Out-of-pocket medication costs ≥$51 per month | ||||
| Yes | 4.9 (0.4) | 0.48 | 4.8 (0.4) | 0.43 |
| No | 5.1 (0.2) | 5.1 (0.4) | ||
| Have task help when needed | ||||
| Yes | 5.2 (0.2) | 0.10 | 5.2 (0.3) | 0.37 |
| No | 4.3 (0.5) | 4.7 (0.6) | ||
| No one to help track medications | ||||
| Definitely/probably true | 4.6 (0.3) | 0.08 | 4.7 (0.4) | 0.28 |
| Definitely/probably false | 5.2 (0.2) | 5.2 (0.4) | ||
| Diabetes | ||||
| Yes | 4.9 (0.3) | 0.43 | 4.9 (0.4) | 0.89 |
| No | 5.2 (0.2) | 5.0 (0.4) | ||
| Cholesterol diagnosis | ||||
| Yes | 4.5 (0.2) | <0.01 | 3.9 (0.4) | <0.01 |
| No | 6.7 (0.3) | 6.0 (0.4) | ||
Satisfaction with cholesterol levels rated on a scale of 1–10, with 1 = definitely not satisfied and 10 = definitely satisfied. Adjusted model: R-square = 0.16; 380 out of 428 participants included in the model (48 participants removed because of missing data for the outcome and/or explanatory variables).
With respect to confidence in ability to control their cholesterol, there was no significant difference between women and men in unadjusted or adjusted results, specifically, unadjusted estimated means were 7.2 versus 7.9 (p = 0.05), and adjusted estimated means were 7.2 versus 7.8 (p = 0.12) (see Table 3). Non-Hispanic white participants had lower levels of confidence than those of other racial/ethnic identity in both unadjusted and adjusted models with estimated means of 7.3 and 8.2 (p < 0.01) and 7.1 and 7.9 (p < 0.01), respectively. Those participants who reported having someone to help keep track of when to take their medications reported higher confidence in controlling cholesterol levels than those without such support in both the unadjusted model with estimated means of 7.9 and 7.3 (p = 0.04) and in the adjusted model with estimated means of 7.8 versus 7.2 (p < 0.05). Lower education levels were associated with higher confidence levels in the unadjusted model only, whereas having a diagnosis of high cholesterol was associated with lower confidence levels in both the unadjusted and adjusted models.
Table 3.
Confidence in Ability to Control Cholesterol Levels
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Least square means (standard error) | p value | Least square means (standard error) | p value | |
| Gender | ||||
| Women | 7.2 (0.3) | 0.05 | 7.2 (0.4) | 0.12 |
| Men | 7.9 (0.1) | 7.8 (0.3) | ||
| Race | ||||
| Non-Hispanic white | 7.3 (0.2) | <0.01 | 7.1 (0.3) | <0.01 |
| Other | 8.2 (0.2) | 7.9 (0.3) | ||
| Married | ||||
| Yes | 7.7 (0.2) | 0.69 | 7.3 (0.3) | 0.14 |
| No | 7.8 (0.2) | 7.7 (0.3) | ||
| Highest level of education | ||||
| ≤High school | 8.2 (0.2) | 0.02 | 7.7 (0.4) | 0.14 |
| >High school | 7.6 (0.1) | 7.3 (0.3) | ||
| Low health literacy | ||||
| Yes | 8.0 (0.2) | 0.17 | 7.5 (0.4) | 0.95 |
| No | 7.7 (0.2) | 7.5 (0.3) | ||
| Inadequate financial Status | ||||
| Yes | 7.7 (0.3) | 0.84 | 7.4 (0.4) | 0.44 |
| No | 7.8 (0.1) | 7.6 (0.3) | ||
| Working at least part-time | ||||
| Yes | 7.9 (0.2) | 0.44 | 7.6 (0.4) | 0.69 |
| No | 7.7 (0.2) | 7.4 (0.3) | ||
| Out-of-pocket medication costs ≥$51 per month | ||||
| Yes | 7.7 (0.3) | 0.65 | 7.5 (0.4) | 0.91 |
| No | 7.8 (0.1) | 7.5 (0.3) | ||
| Have task help when needed | ||||
| Yes | 7.8 (0.1) | 0.26 | 7.7 (0.3) | 0.49 |
| No | 7.4 (0.4) | 7.3 (0.5) | ||
| No one to help track medications | ||||
| Definitely/probably true | 7.3 (0.3) | 0.04 | 7.2 (0.4) | <0.05 |
| Definitely/probably false | 7.9 (0.1) | 7.8 (0.3) | ||
| Diabetes | ||||
| Yes | 7.8 (0.2) | 0.87 | 7.5 (0.3) | 0.87 |
| No | 7.8 (0.2) | 7.5 (0.3) | ||
| Cholesterol diagnosis | ||||
| Yes | 7.6 (0.1) | <0.01 | 7.1 (0.3) | 0.02 |
| No | 8.4 (0.2) | 7.9 (0.4) | ||
Confidence in controlling cholesterol rated on a scale of 1–10, with 1 = not at all confident and 10 = completely confident. Adjusted model: R-square = 0.07; 407 out of 428 participants included in the model (21 participants removed because of missing data for the outcome and/or explanatory variables).
Discussion
Among this group of patients at high risk for CVD, we found that women were less satisfied with their lipid control than men. This dissatisfaction appears justified as women in this study had significantly higher LDL values than men. Confidence in ability to improve cholesterol levels was similar between men and women after adjustment for sociodemographic characteristics. Notably, individuals without someone to help with medication tracking were less confident in controlling their lipid levels than those who had someone to fulfill this role, and women were less likely to have this type of instrumental social support.
Our finding that women had higher LDL values than men align with previous findings,15,46,47 including data from VA-based studies.23,30,48 Because this study targeted patients with uncontrolled CVD risk factors (specifically hypertension and/or hyperlipidemia), they are a high risk population and one that likely had previous conversations with their providers about lipid control and CVD and may have been more likely to receive lipid testing. However, in general, fewer than 50% of women report having conversations with their providers about CVD.31 Moreover, compared with men, women are less likely to be identified as high risk for CVD49,50 and less likely to undergo LDL testing.51 Recent findings by Villablanca et al. note that only 53.8% of women know what their cholesterol values are.52 Efforts within the VA to promote preventative care and eradicate gender disparities through universal gender-specific clinical reminders pertaining to lipid screening may lessen these disparities; for example, among diabetic patients, women and men undergo lipid testing equally,30 despite persistence LDL disparities.
Although our results demonstrate no association between levels of satisfaction and social support, they do demonstrate that higher levels of social support were associated with greater confidence in ability to control cholesterol. Social support has positive health benefits in the context of chronic disease.53 Social isolation is known to predict mortality at levels similar to known clinical risk factors such as smoking.54 Conversely, better social support has been found to be associated with improved hypertension adherence,55,56 increased physical activity,57 and to be protective after first myocardial infarction.58 National studies of CVD prevention find that lack of support directly contributes to an inability to engage in prevention-related behavior.31 Similarly, previous analyses from this study cohort found that lacking someone to assist tracking medications is associated with higher medication barriers.45 For men, being married or cohabiting appears to be an important factor in lowering CVD risk.59 With respect to hyperlipidemia, spousal involvement can help patients adhere to needed behavior change60 and dietary adherence.61 Most studies that examined spousal support predominantly included men as the index participant, which limits our ability to draw conclusions about its impact on women. However, among women, lower levels of social support have been found to be associated with higher rates of CVD risk,62 myocardial infarction and stroke,63 and heart failure-related mortality.64
Social support and CVD risk is especially relevant to the women veteran population who are less likely to be married and have less social support than male veterans.65 Female veterans are also less likely to have someone accompany them to a doctor's visit,65 more likely to live alone,65 and more likely to be homeless.66 Among veterans, disparities in LDL goal achievement persist67 despite overall improvements in gender inequities within the VA48; these disparities are most notable among older women veterans and those women with known ischemic heart disease.11 Understanding the impact of poor social support in the veteran population can help provide insights for other high risk groups and possible underlying causes of disparities in their hyperlipidemia control.
To eliminate gender disparities in CVD and inform gender-tailored prevention efforts, we need the purposeful inclusion of women into CVD clinical trials, explicitly designed to address gender-based treatment effects.17 If social support has a differential effect on CVD-related behaviors and outcomes for women than for men, then further deliberate examination of the mechanism of this gender-based difference is needed. A better understanding of the impact of poor social support on CVD risk could inform the design of possible intervention strategies for both women and men. Potential strategies to augment social support in the context of hyperlipidemia treatment could include nursing support, pharmacist-based interventions, or peer support.
As a cross-sectional analysis of survey data, this study has limitations. The measures of satisfaction and confidence are limited to one point in time, and thus the discussed associations should be considered exploratory. In addition, only measures of instrumental social support (e.g., informational support) were included in this analysis. A better understanding of which aspects of the all types of social support (informational, emotional, instrumental, and appraisal68) are most impactful on CVD risk-reduction behaviors would be helpful. For example, research in the general population suggests that perceived social support may be more important than functional support in the context of CVD outcomes.69 A more comprehensive measure of social support could clarify the nuances of the impact to confidence and satisfaction in the context of hyperlipidemia. As 9.2% of female participants were of reproductive age (less than or equal to age 44), it is possible that levels of satisfaction and confidence in ability to lipid control may have been influenced by limitations on the safety of statin medications as these medications are considered teratogenic.70 We did not assess the specific impact of reproductive contraindications to lipid control medication on the patient-centered measures. In addition, gender differences in characteristics such as marital status, education, and age may contribute to the gender differences reported in our findings. However, these sociodemographic differences reflect those found in the underlying veteran population receiving care in the VA.71 Given that these analyses are secondary, we were limited in the assessment of potential comorbid diseases. Given the relatively small number of women included in this study, we were also limited in our ability to further adjust for these baseline differences in our analysis. Patients in this study were at high risk for CVD by design and may not fully apply to a patient population at average risk. Finally, this study took place at a single site in the veteran's health administration, which may see a different patient population from other U.S. patient populations.
Conclusions
In a population at high risk for CVD, lack of social support for medication tracking is associated with lower confidence in ability to control lipids, and women were less likely to have this type of social support. Lack of social support may be a potential contributing factor to lingering gender disparities in the treatment of hyperlipidemia and warrants further investigation as a potential target for future tailored CVD risk-reduction interventions.
Acknowledgments
We would like to thank Susanne Danus and Jill Blakeney for their work on this project.
Funding
This study was funded by a grant from the VA Health Service Research and Development to Dr. H.B.B. (VA HSR&D IIR (#08-297). Drs. K.M.G. (CDA #13-263) and L.L.Z. (CDA#13-025) were supported by VA HSR&D Career Development Awards. Dr. BCB was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR001115. In addition, this work was supported by the Center of Innovation for Health Services Research in Primary Care (CIN 13-410) at the Durham VA Medical Center.
Prior Presentations
Findings presented here were previously presented at the VA HSR&D/QUERI Conference, Philadelphia, PA, in July 2015 and at the Society for Women's Health Research conference “Transforming Cardiovascular Disease Prevention for Millennial Women: Beyond Traditional Risk Factors,” Winston-Salem, NC in October 2015. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the NIH.
Disclosure Statement
No competing financial interests exist.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015;131:e29–e322 [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: Concealed leveling of mortality rates. J Am Coll Cardiol 2007;50:2128–2132 [DOI] [PubMed] [Google Scholar]
- 3.Agrawal S, Van Eyk J, Sobhani K, Wei J, Bairey Merz CN. Sex, myocardial infarction, and the failure of risk scores in women. J Womens Health (Larchmt) 2015;24:859–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah AJ, Ghasemzadeh N, Zaragoza-Macias E, et al. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc 2014;3:e000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J, Chen L, Delzell E, et al. The association between inflammatory markers, serum lipids and the risk of cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis 2014;73:1301–1308 [DOI] [PubMed] [Google Scholar]
- 6.Doumas M, Papademetriou V, Faselis C, Kokkinos P. Gender differences in hypertension: Myths and reality. Curr Hypertens Rep 2013;15:321–330 [DOI] [PubMed] [Google Scholar]
- 7.Mucha L, Stephenson J, Morandi N, Dirani R. Meta-analysis of disease risk associated with smoking, by gender and intensity of smoking. Gend Med 2006;3:279–291 [DOI] [PubMed] [Google Scholar]
- 8.Smith PH, Kasza KA, Hyland A, et al. Gender differences in medication use and cigarette smoking cessation: Results from the International Tobacco Control Four Country Survey. Nicotine Tob Res 2015;17:463–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender differences in smoking cessation. J Consult Clin Psychol 1999;67:555–562 [DOI] [PubMed] [Google Scholar]
- 10.Ballotari P, Ranieri SC, Luberto F, et al. Sex differences in cardiovascular mortality in diabetics and nondiabetic subjects: A population-based study (Italy). Int J Endocrinol 2015;2015:914057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vimalananda VG, Miller DR, Hofer TP, Holleman RG, Klamerus ML, Kerr EA. Accounting for clinical action reduces estimates of gender disparities in lipid management for diabetic veterans. Journal of general internal medicine 2013;28 Suppl 2:S529–S535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chou AF, Scholle SH, Weisman CS, Bierman AS, Correa-de-Araujo R, Mosca L. Gender disparities in the quality of cardiovascular disease care in private managed care plans. Womens Health Issues 2007;17:120–130 [DOI] [PubMed] [Google Scholar]
- 13.Chou AF, Wong L, Weisman CS, et al. Gender disparities in cardiovascular disease care among commercial and medicare managed care plans. Womens Health Issues 2007;17:139–149 [DOI] [PubMed] [Google Scholar]
- 14.Cone C, Murata G, Myers O. Demographic determinants of response to statin medications. Am J Health Syst Pharm 2011;68:511–517 [DOI] [PubMed] [Google Scholar]
- 15.Billimek J, Malik S, Sorkin DH, et al. Understanding disparities in lipid management among patients with type 2 diabetes: Gender differences in medication nonadherence after treatment intensification. Womens Health Issues 2015;25:6–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Victor BM, Teal V, Ahedor L, Karalis DG. Gender differences in achieving optimal lipid goals in patients with coronary artery disease. Am J Cardiol 2014;113:1611–1615 [DOI] [PubMed] [Google Scholar]
- 17.Bucholz EM, Krumholz HM. Women in clinical research: What we need for progress. Circ Cardiovasc Qual Outcomes 2015;8(2 Suppl 1):S1–S3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim ES, Carrigan TP, Menon V. Enrollment of women in National Heart, Lung, and Blood Institute-funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J Am Coll Cardiol 2008;52:672–673 [DOI] [PubMed] [Google Scholar]
- 19.Fulcher J, O'Connell R, Voysey M, et al. Efficacy and safety of LDL-lowering therapy among men and women: Meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet (London, England) 2015;385:1397–1405 [DOI] [PubMed] [Google Scholar]
- 20.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25 Suppl 2):S1–S45 [DOI] [PubMed] [Google Scholar]
- 21.Downs JR, O'Malley PG. Management of dyslipidemia for cardiovascular disease risk reduction: Synopsis of the 2014 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guideline. Ann Intern Med 2015;163:291–297 [DOI] [PubMed] [Google Scholar]
- 22.Mittleman MA, Taylor WC, Smetana G, Burns RB. Treatment of blood cholesterol to reduce risk for atherosclerotic cardiovascular disease: Grand rounds discussion from the beth Israel Deaconess Medical Center. Ann Intern Med 2015;163:280–290 [DOI] [PubMed] [Google Scholar]
- 23.Sambamoorthi U, Mitra S, Findley PA, Pogach LM. Decomposing gender differences in low-density lipoprotein cholesterol among veterans with or at risk for cardiovascular illness. Womens Health Issues 2012;22:e201–e208 [DOI] [PubMed] [Google Scholar]
- 24.Sheppard JP, Fletcher K, McManus RJ, Mant J. Missed opportunities in prevention of cardiovascular disease in primary care: A cross-sectional study. Br J Gen Pract 2014;64:e38–e46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wallach-Kildemoes H, Andersen M, Diderichsen F, Lange T. Adherence to preventive statin therapy according to socioeconomic position. Eur J Clin Pharmacol 2013;69:1553–1563 [DOI] [PubMed] [Google Scholar]
- 26.Stulc T, Ceska R, Gotto AM., Jr. Statin intolerance: The clinician's perspective. Curr Atheroscler Rep 2015;17:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmad Z. Statin intolerance. Am J Cardiol 2014;113:1765–1771 [DOI] [PubMed] [Google Scholar]
- 28.Lewey J, Shrank WH, Bowry AD, Kilabuk E, Brennan TA, Choudhry NK. Gender and racial disparities in adherence to statin therapy: A meta-analysis. Am Heart J 2013;165:665–678, 678.e1 [DOI] [PubMed] [Google Scholar]
- 29.Virani SS, Woodard LD, Chitwood SS, et al. Frequency and correlates of treatment intensification for elevated cholesterol levels in patients with cardiovascular disease. Am Heart J 2011;162:725–732.e1 [DOI] [PubMed] [Google Scholar]
- 30.Vimalananda VG, Miller DR, Palnati M, Christiansen CL, Fincke BG. Gender disparities in lipid-lowering therapy among veterans with diabetes. Womens Health Issues 2011;21(4 Suppl):S176–S181 [DOI] [PubMed] [Google Scholar]
- 31.Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women's awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes 2010;3:120–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biswas MS, Calhoun PS, Bosworth HB, Bastian LA. Are women worrying about heart disease? Womens Health Issues 2002;12:204–211 [DOI] [PubMed] [Google Scholar]
- 33.Bhattacharjee S, Findley PA, Sambamoorthi U. Understanding gender differences in statin use among elderly Medicare beneficiaries: An application of decomposition technique. Drugs Aging 2012;29:971–980 [DOI] [PubMed] [Google Scholar]
- 34.Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med 1984;100:258–268 [DOI] [PubMed] [Google Scholar]
- 35.Chen H, Rosenzweig EB, Gotzkowsky SK, Arneson C, Nelsen AC, Bourge RC. Treatment satisfaction is associated with improved quality of life in patients treated with inhaled treprostinil for pulmonary arterial hypertension. Health Qual Life Outcomes 2013;11:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saarti S, Hajj A, Karam L, et al. Association between adherence, treatment satisfaction and illness perception in hypertensive patients. J Hum Hypertens 2016;30:341–345 [DOI] [PubMed] [Google Scholar]
- 37.Aljumah K, Ahmad Hassali A, AlQhatani S. Examining the relationship between adherence and satisfaction with antidepressant treatment. Neuropsychiatr Dis Treat 2014;10:1433–1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Criswell TJ, Weber CA, Xu Y, Carter BL. Effect of self-efficacy and social support on adherence to antihypertensive drugs. Pharmacotherapy 2010;30:432–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health 2012;37:15–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ku GM, Kegels G. Knowledge, attitudes and perceptions of people with type 2 diabetes as related to self-management practices: Results of a cross-sectional study conducted in Luzon, Philippines. Chronic Illn 2015;11:93–107 [DOI] [PubMed] [Google Scholar]
- 41.Chiu CJ, Wray LA. Gender differences in functional limitations in adults living with type 2 diabetes: Biobehavioral and psychosocial mediators. Ann Behav Med 2011;41:71–82 [DOI] [PubMed] [Google Scholar]
- 42.Centis E, Trento M, Dei Cas A, et al. Stage of change and motivation to healthy diet and habitual physical activity in type 2 diabetes. Acta Diabetol 2014;51:559–566 [DOI] [PubMed] [Google Scholar]
- 43.Melnyk SD, Zullig LL, McCant F, et al. Telemedicine cardiovascular risk reduction in veterans. Am Heart J 2013;165:501–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zullig LL, Melnyk SD, Stechuchak KM, et al. The Cardiovascular Intervention Improvement Telemedicine Study (CITIES): Rationale for a tailored behavioral and educational pharmacist-administered intervention for achieving cardiovascular disease risk reduction. Telemed J E Health 2014;20:135–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zullig LL, Stechuchak KM, Goldstein KM, et al. Patient-reported medication adherence barriers among patients with cardiovascular risk factors. J Manage Care Spec Pharm 2015;21:479–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schoen MW, Tabak RG, Salas J, Scherrer JF, Buckhold FR. Comparison of adherence to guideline-based cholesterol treatment goals in men versus women. Am J Cardiol 2016;117:48–53 [DOI] [PubMed] [Google Scholar]
- 47.Hammond G, Mochari-Greenberger H, Liao M, Mosca L. Effect of gender, caregiver, on cholesterol control and statin use for secondary prevention among hospitalized patients with coronary heart disease. Am J Cardiol 2012;110:1613–1618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whitehead AM, Czarnogorski M, Wright SM, Hayes PM, Haskell SG. Improving trends in gender disparities in the Department of Veterans Affairs: 2008–2013. Am J Public Health 2014;104 Suppl 4:S529–S531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abuful A, Gidron Y, Henkin Y. Physicians' attitudes toward preventive therapy for coronary artery disease: Is there a gender bias? Clin Cardiol 2005;28:389–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hemal K, Pagidipati NJ, Coles A, et al. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease: Insights from the PROMISE trial. JACC Cardiovasc Imaging 2016;9:337–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Manteuffel M, Williams S, Chen W, Verbrugge RR, Pittman DG, Steinkellner A. Influence of patient sex and gender on medication use, adherence, and prescribing alignment with guidelines. J Womens Health (Larchmt) 2014;23:112–119 [DOI] [PubMed] [Google Scholar]
- 52.Villablanca AC, Slee C, Lianov L, Tancredi D. Outcomes of a clinic-based educational intervention for cardiovascular disease prevention by race, ethnicity, and urban/rural status. J Womens Health (Larchmt) 2016;25:1174–1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gallant MP. The influence of social support on chronic illness self-management: A review and directions for research. Health Educ Behav 2003;30:170–195 [DOI] [PubMed] [Google Scholar]
- 54.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: A predictor of mortality comparable to traditional clinical risk factors. Am J Public Health 2013;103:2056–2062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hu HH, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens 2015;29:198–203 [DOI] [PubMed] [Google Scholar]
- 56.Magrin ME, D'Addario M, Greco A, et al. Social support and adherence to treatment in hypertensive patients: A meta-analysis. Ann Behav Med 2015;49:307–318 [DOI] [PubMed] [Google Scholar]
- 57.Coghill N, Cooper AR. Motivators and de-motivators for adherence to a program of sustained walking. Prev Med 2009;49:24–27 [DOI] [PubMed] [Google Scholar]
- 58.Quinones PA, Kirchberger I, Heier M, et al. Marital status shows a strong protective effect on long-term mortality among first acute myocardial infarction-survivors with diagnosed hyperlipidemia—findings from the MONICA/KORA myocardial infarction registry. BMC Public Health 2014;14:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mols RE, Sand NP, Jensen JM, Thomsen K, Diederichsen AC, Norgaard BL. Social factors and coping status in asymptomatic middle-aged Danes: Association to coronary artery calcification. Scand J Public Health 2013;41:737–743 [DOI] [PubMed] [Google Scholar]
- 60.Sperber NR, Sandelowski M, Voils CI. Spousal support in a behavior change intervention for cholesterol management. Patient Educ Couns 2013;92:121–126 [DOI] [PubMed] [Google Scholar]
- 61.Bovbjerg VE, McCann BS, Brief DJ, et al. Spouse support and long-term adherence to lipid-lowering diets. Am J Epidemiol 1995;141:451–460 [DOI] [PubMed] [Google Scholar]
- 62.Piwonski J, Piwonska A, Sygnowska E. Is level of social support associated with health behaviours modifying cardiovascular risk? Results of the WOBASZ study. Kardiol Pol 2012;70:803–809 [PubMed] [Google Scholar]
- 63.Gafarov VV, Panov DO, Gromova EA, Gagulin IV, Gafarova AV. The influence of social support on risk of acute cardiovascular diseases in female population aged 25–64 in Russia. Int J Circumpolar Health 2013;72 [Epub ahead of print]; DOI: 10.3402/ijch.v72i0.21210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 2006;152:940.e1–e8 [DOI] [PubMed] [Google Scholar]
- 65.Frayne SM, Parker VA, Christiansen CL, et al. Health status among 28,000 women veterans. The VA Women's Health Program Evaluation Project. J Gen Intern Med 2006;21 Suppl 3:S40–S46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Washington DL, Yano EM, McGuire J, Hines V, Lee M, Gelberg L. Risk factors for homelessness among women veterans. J Health Care Poor Underserved 2010;21:82–91 [DOI] [PubMed] [Google Scholar]
- 67.Goldstein KM, Melnyk SD, Zullig LL, et al. Heart matters: Gender and racial differences cardiovascular disease risk factor control among veterans. Womens Health Issues 2014;24:477–483 [DOI] [PubMed] [Google Scholar]
- 68.Dennis CL. Peer support within a health care context: A concept analysis. Int J Nurs Stud 2003;40:321–332 [DOI] [PubMed] [Google Scholar]
- 69.Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosom Med 2010;72:229–238 [DOI] [PubMed] [Google Scholar]
- 70.Godfrey LM, Erramouspe J, Cleveland KW. Teratogenic risk of statins in pregnancy. Ann Pharmacother 2012;46:1419–1424 [DOI] [PubMed] [Google Scholar]
- 71.Frayne SM PC, Saecho F, Maisel NC, et al. Sourcebook: Women veterans in the veterans health administration. Volume 3 Sociodemographics, utilization, costs of care, and health profile. Washington, DC: Women's Health Evaluation Initiative, Women's Health Services, Veterans Health Administration, Department of Veterans Affairs, 2014;21–38 [Google Scholar]